Abstract
Background:
Juveniles in custody are affected by sexually transmitted infections due to risky behaviors. Therefore, they have a disproportionate burden of hepatitis B virus (HBV) and human immunodeficiency virus (HIV). In this study, the prevalence and associated characteristics of hepatitis B and HIV infections were assessed in young prisoners.
Materials and Methods:
In this cross-sectional study, prevalence of HBV and HIV infections was assessed among young prisoners during 2008-2009. A checklist consisting of demographic, social, and risk factors was filled out and blood was drawn for their tests. Sera were analyzed for hepatitis B surface antigen (HBs Ag), hepatitis B surface antibody (HBs Ab), hepatitis B core antibody (HBc Ab) and HIV Ab, and Western blot test was performed on antibody-positive HIV.
Results:
A total number of 160 young prisoners (147 boys and 13 girls) were evaluated. The mean age of the subjects was 16.59 ± 1.24 year. HBs Ag, HBc Ab, HBs Ab, and HIV Ab were detected in 1 (0.63%), 1 (0.63%), 52 (32.5%), and 1 (0.63%), respectively.
Conclusion:
With respect to national vaccination program against HBV infection, the juvenile prisoners had low prevalence of HBs Ab.
Keywords: Hepatitis B virus, human immunodeficiency virus, young prisoners
INTRODUCTION
High-risk behaviors are normal part of maturity. These risky activities are associated with predictable, although often unforeseen, consequences.[1] Young inmates, compared with their peers, begin high risk sexual activity earlier; have more partners, initiation of injection drug use, and higher rates of sexually transmitted diseases.[2] Health studies of juvenile inmates indicate rates of risk behaviors affecting physical health.[3] Factors such as low socioeconomic status, high risky sexual behaviors, injection drug use may be evolved in them before incarceration. After entrance to prison, it may be connected to additional risk factors such as sexual harassment, non-professional tattooing, psychological stress, poor ventilation systems, and crowded living conditions.[4]
Hepatitis B virus (HBV) and human immunodeficiency virus (HIV) are blood borne pathogens, which are efficiently transmitted by percutaneous or per mucosal exposure to infectious blood or body fluids.[5] The prevalence of HBV infection worldwide is 5%, which makes it a global health problem.[6] It is estimated that 50 million new cases are being detected annually with 5-10% of adults and up to 90% of infants becoming chronically infected.[7] Among prisoners, the prevalence of serological markers HBV infection is 13-47%, and varies among different regions.[5]
Young inmates are at heightened risk for HIV infection due to higher prevalence of psychopathology and substance use disorders, compared with their no offending peers. Young ones with psychiatric disorders are at greater risk because of unprotected sexual behaviors than their peers who are not coping with mental health issues.[2] Therefore, young offenders are particularly at risk for HBV and HIV.
We undertook a survey to determine the seroprevalence of HBV and HIV in young prisoners.
MATERIALS AND METHODS
During 2008-2009, the cross-sectional study was conducted among prisoners in Isfahan, Iran. All the 160 prisoners, who were younger than 19 years of age, after signed a written informed consent form was enrolled voluntarily by census method. Researchers recorded a check-list for each participant through a face-to-face interview. Any question could be skipped by inmates. The checklist included socio-demographic data, drug and sexual history, and duration of incarceration.
Having a history of at least one time injection was considered as intravenous drug use. This study was approved by the Ethical Committee of Isfahan University of Medical Sciences, Isfahan, Iran.
Five milliliter blood sample was obtained from each participant. Serum samples were stored at –20°C until analyzing. HBV antibody was assayed with commercial enzyme-linked immunosorbent assays (ELISA) for hepatitis B surface antigen (HBs Ag) kit (Diapro, Italy), total hepatitis B core antibody (HBc Ab) kit (Diapro, Italy) and hepatitis B surface antibody (HBs Ab) kit (Diapro, Italy). Testing for antibody to HIV was performed with commercial ELISA (Diapro, Italy) confirmed by Western blot (INNO-LIA HIV I/II Score), which assessed p24, p31, gp41, p120, gp 36, p105, and p17 antigens.
Samples were tested for HBs Ag to estimate recent infection. A specimen was considered HIV seropositive if it was reactive to both ELISA and Western blot. The data was analyzed with descriptive statistical methods by Statistical Package for the Social Sciences software, version 15.
RESULTS
The age range of subjects was from 12 to 19 years old with the mean age of 16.59 ± 1.24. Most of the subjects were boy (91.9%) and had a low-level of education (77.5%) [Table 1]. Sixty from 160 inmates self-reported a history of illegal sex. The finding showed that 29.4% of cases had a history of drug abuse. Of the 160 participants, 44 had the history of being incarcerated before the present time.
Table 1.
Demographic characteristics of subjects
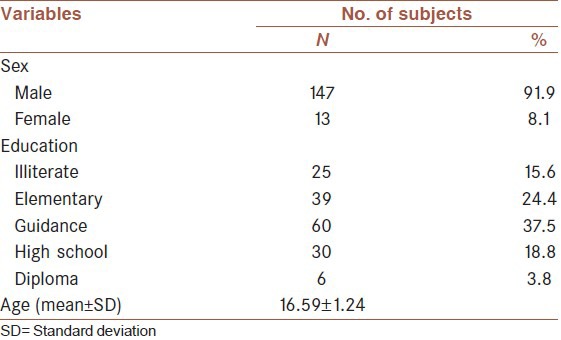
Table 2 shows the results of serological test. The seroprevalence of HBs Ag, HBc Ab, and HIV was 0.6%. HBs Ag and HBc Ab were detected in one 17-year-old boy with 2 times incarcerations and more than 1 year of duration of being in prison.
Table 2.
Serological tests
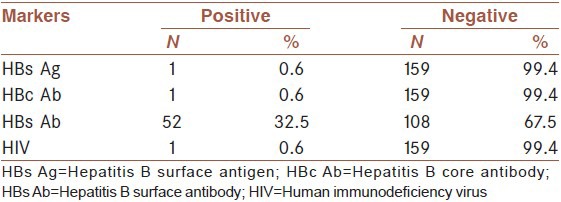
A 15-year-old boy was HIV positive, one number of incarceration and less than 60 days of being in prison. Among 160 juveniles, 52 (32.5%) individuals were positive for HBs Ab.
According to the small number of HBs Ag, HBc Ab, and HIV (one case), no test of association with risk factors could be performed.
DISCUSSION
In this study we evaluated the seroprevalence of HBs Ag, HBc Ab, HBs Ab, and HIV among juveniles in a prison in Isfahan. Such studies have been undertaken in some of countries but reports on these infections among young prisoners are scarce in our country.n comparison with other studies, we found low seropositivity of HBs Ag and HBc Ab. Butler et al.[3] reported 11% of young offenders tested positive for HBc Ab. The prevalence of HBc Ab was 4% among young prisoner in England and Wales.[8] HBc Ab and HBs Ag were reported 11% and 4% among juvenile detainees in Australia.[9] A study which was done in Melborne juvenile justice center[1] reported 8% had been exposed to HBV. In a study in Taiwan, the prevalence of HBs Ag was 24.5% in participants aged 10-20 years.[10] Adoga reported HBs Ag seroprevalence rate of 10% in the age group 15-20 year in a prison in Nigeria.[11]
More than 65% of these juveniles had no immunity against hepatitis B. In Iran mass vaccination of neonates against HBV infection started in 1993 as a national program.[12] Therefore, this program has not covered some of these young people who were born before 1993. Although our finding shows the HBV prevalence is still low in this group but many studies[13,14,15] showed that the prevalence of HBV infection is generally higher in prisoners than in non-prisoners. These researches indicate that prisons could be also high-risk places for infection transmission and they can have an important effect on rate of infection. Therefore, antibody testing for immunity against HBV and performing of hepatitis B vaccination programs in prison and correctional setting should be conducted in our country.
Our results indicated prevalence of HIV seropositivity is 0.6% in this population. In Butler et al. study[3] none of young prisoners were positive for HIV. In comparison with other studies in Brazil,[16] Maryland,[17] and Argentina[18] we found low seropositivity of HIV. However, it was similar to finding from UK,[19] USA,[20] and Australia.[9] According to the absence of risk factors for this patient, HIV infection can be due to vertical transmission.
Unfortunately, we did not assessed the knowledge and understanding of risks related to transmission of these infections in this study. However, we know more than 75% of this population had less than high school education and it could be acceptable that the most of them did not know about transmission routes of these infections. Therefore, educating inmates about prominent potential route for transmission of these blood borne disease is very important.
Our study had several limitations. First, it included a low number of cases and only a positive case for HBV and HIV, and thus, it is difficult to make a clear statement about the risk factors. Second, data was collected by means self-report questionnaire through an interview.
According to the prevalence rate of HBS Ab and doing high-risk behaviors in this high-risk group, implementation program on immunization of this population should be considered. Since education programs are the most important and effective way of preventing such disease, such programs should be performed constantly for all prisoners.
CONCLUSION
With respect to national vaccination program against HBV infection in Iran, the juvenile prisoners had low prevalence of HBs Ab.
ACKNOWLEDGMENTS
This study was supported by Isfahan University of Medical Sciences (The University Research Project Number 185063).
Footnotes
Source of Support: This paper is extracted from the research project no: 185063 research chancellor, Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Ogilvie EL, Veit F, Crofts N, Thompson SC. Hepatitis infection among adolescents resident in Melbourne Juvenile Justice Centre: Risk factors and challenges. J Adolesc Health. 1999;25:46–51. doi: 10.1016/s1054-139x(98)00086-x. [DOI] [PubMed] [Google Scholar]
- 2.Tolou-Shams M, Stewart A, Fasciano J, Brown LK. A review of HIV prevention interventions for juvenile offenders. J Pediatr Psychol. 2010;35:250–61. doi: 10.1093/jpepsy/jsp069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Butler T, Belcher JM, Champion U, Kenny D, Allerton M, Fasher M. The physical health status of young Australian offenders. Aust N Z J Public Health. 2008;32:73–80. doi: 10.1111/j.1753-6405.2008.00169.x. [DOI] [PubMed] [Google Scholar]
- 4.Marques NM, Margalho R, Melo MJ, Cunha JG, Meliço-Silvestre AA. Seroepidemiological survey of transmissible infectious diseases in a Portuguese prison establishment. Braz J Infect Dis. 2011;15:272–5. doi: 10.1016/s1413-8670(11)70188-x. [DOI] [PubMed] [Google Scholar]
- 5.Weinbaum CM, Sabin KM, Santibanez SS. Hepatitis B, hepatitis C, and HIV in correctional populations: A review of epidemiology and prevention. AIDS. 2005;19:S41–6. doi: 10.1097/01.aids.0000192069.95819.aa. [DOI] [PubMed] [Google Scholar]
- 6.Alizadeh AH, Ranjbar M, Ansari S, MirArab A, Alavian SM, Mohammad K, et al. Seroprevalence of hepatitis B in Nahavand, Islamic Republic of Iran. East Mediterr Health J. 2006;12:528–37. [PubMed] [Google Scholar]
- 7.Merican I, Guan R, Amarapuka D, Alexander MJ, Chutaputti A, Chien RN, et al. Chronic hepatitis B virus infection in Asian countries. J Gastroenterol Hepatol. 2000;15:1356–61. doi: 10.1046/j.1440-1746.2000.0150121356.x. [DOI] [PubMed] [Google Scholar]
- 8.Weild AR, Gill ON, Bennett D, Livingstone SJ, Parry JV, Curran L. Prevalence of HIV, hepatitis B, and hepatitis C antibodies in prisoners in England and Wales: A national survey. Commun Dis Public Health. 2000;3:121–6. [PubMed] [Google Scholar]
- 9.Templeton DJ. Sexually transmitted infection and blood-borne virus screening in juvenile correctional facilities: A review of the literature and recommendations for Australian centres. J Clin Forensic Med. 2006;13:30–6. doi: 10.1016/j.jcfm.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 10.Lin CF, Twu SJ, Chen PH, Cheng JS, Wang JD. Prevalence and determinants of hepatitis B antigenemia in 15,007 inmates in Taiwan. J Epidemiol. 2010;20:231–6. doi: 10.2188/jea.JE20081045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adoga MP, Banwat EB, Forbi JC, Nimzing L, Pam CR, Gyar SD, et al. Human immunonodeficiency virus, hepatitis B virus and hepatitis C virus: Sero-prevalence, co-infection and risk factors among prison inmates in Nasarawa State, Nigeria. J Infect Dev Ctries. 2009;3:539–47. doi: 10.3855/jidc.472. [DOI] [PubMed] [Google Scholar]
- 12.Alavian SM, Hajarizadeh B, Ahmadzad-Asl M, Kabir A, Bagheri Lankarani K. Hepatitis B virus infection in Iran: A systematic review. Hepat Mon. 2008;8:281–94. [Google Scholar]
- 13.Weinbaum C, Lyerla R, Margolis HS. Centers for Disease Control and Prevention. Prevention and control of infections with hepatitis viruses in correctional settings. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2003;52:1–36. [PubMed] [Google Scholar]
- 14.Pallás J, Fariñas-Alvarez C, Prieto D, Llorca J, Delgado-Rodríguez M. Risk factors for monoinfections and coinfections with HIV, hepatitis B and hepatitis C viruses in northern Spanish prisoners. Epidemiol Infect. 1999;123:95–102. doi: 10.1017/s0950268899002538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mir-Nasseri MM, Mohammadkhani A, Tavakkoli H, Ansari E, Poustchi H. Incarceration is a major risk factor for blood-borne infection among intravenous drug users: Incarceration and blood borne infection among intravenous drug users. Hepat Mon. 2011;11:19–22. [PMC free article] [PubMed] [Google Scholar]
- 16.Zanetta DM, Strazza L, Azevedo RS, Carvalho HB, Massad E, Menezes RX, et al. HIV infection and related risk behaviours in a disadvantaged youth institution of São Paulo, Brazil. Int J STD AIDS. 1999;10:98–104. doi: 10.1258/0956462991913718. [DOI] [PubMed] [Google Scholar]
- 17.Kassira EN, Bauserman RL, Tomoyasu N, Caldeira E, Swetz A, Solomon L. HIV and AIDS surveillance among inmates in Maryland prisons. J Urban Health. 2001;78:256–63. doi: 10.1093/jurban/78.2.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Avila MM, Casanueva E, Piccardo C, Liberatore D, Cammarieri G, Cervellini M, et al. HIV-1 and hepatitis B virus infections in adolescents lodged in security institutes of Buenos Aires. Pediatr AIDS HIV Infect. 1996;7:346–9. [PubMed] [Google Scholar]
- 19.Bird AG, Gore SM, Burns SM, Duggie JG. Study of infection with HIV and related risk factors in young offenders’ institution. BMJ. 1993;307:228–31. doi: 10.1136/bmj.307.6898.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morris RE, Baker CJ, Valentine M, Pennisi AJ. Variations in HIV risk behaviors of incarcerated juveniles during a four-year period: 1989-1992. J Adolesc Health. 1998;23:39–48. doi: 10.1016/s1054-139x(97)00268-1. [DOI] [PubMed] [Google Scholar]


