Abstract
Introduction
This article compares the prevalence of primary infertility in Iran estimates provided by different studies. No other study had provided a review about the researches related to epidemiology of infertility in the country.
Materials and Methods
A literature review was undertaken using the scientific resources on the internet and the list of national projects obtained from Deputy of Research and Technology, of Iran Ministry of Health and Medical Education (MOH & ME) and relevant research centers. These resources were attentively reviewed to find about national studies on the epidemiology of primary infertility in Iran during the last decade. Based on their design quality, the National Infertility Study (NIS) (2004-2005), National Health Survey (NHS) (2001) and Tehran Study (1997) were considered for the research.
Results
Current primary infertility estimated by National Health Survey (NHS) was 2.8% and by National Infertility Survey (NIS) 3.4%. Tehran study and NIS estimated the prevalence of lifetime primary infertility to be 21.9% and 24.9%, respectively. The minimum prevalence of lifetime primary infertility was found to be 15.8% for the marriage age of 19-27 by Tehran study and 17.2% for the marriage age of 21-26 by NIS.
Conclusion
On the average, 21-22% of women experience primary infertility during their marital life. The best age of marriage for women in Iran seems to be 20-27 years. At this age group, the lowest number of women (16-18%) would experience primary infertility.
Keywords: Infertility, Iran, Primary infertility
Introduction
Infertility has been recognized as a potentially serious, costly and burdensome problem on affected families. Infertility may have far-reaching consequences, including marital conflicts, violence, stigmatization, isolation and divorce (1). The consequences are more serious in societies where women are primarily stereotyped as mothers.
Epidemiological study of infertility might assist public health policy-makers in making efficient decisions by estimating the potential users of health services for infertility work up or treatment. The terminology and definitions of infertility and its kinds have always been controversial and they could cause many differences in interpretations and estimations. In this article, we review the epidemiology of primary infertility based on the national surveys that have been conducted earlier in Iran.
Materials and Methods
We conducted an internet-based search through Google Scholar, PubMed and IranMedex to find about previous primary infertility studies in Iran. The key words included in the search were Iran, infertility, epidemiology and prevalence. A comprehensive search of the Deputy of Research and Technology of MOH & ME and relevant research centers was also carried out on previously undertaken national projects in Iran regarding the subject.
We only included national studies regarding the epidemiology of infertility. The only exception was a research that had been conducted in Tehran, Iran because of its a) design quality and b) taking into account the variable of age at the first marriage. Eventually, the following three studies were considered for the review:
Research on Primary Infertility in Tehran (Tehran Study), which had been carried out on 1,992 women aging 15-49 years, who were married for at least one year, in Tehran and suburban areas during 1997.
The National Infertility Study (NIS) (2004-2005), supported by the National Research Center for Medical Sciences of Iran (NRCMSI), had studied 10,783 women aging 19-49 years.
The National Health Survey (NHS) (2001), conducted by Iran Ministry of Health and Medical Education (MOH & ME).
All the above studies had defined primary infertility as inability to conceive upon one year of unprotected intercourse.
Regarding the definitions, lifetime primary infertility refers to couples who experience the problem at some time during their married life (2), while current primary infertility indicates the number of couples who have the problem at the time of study.
Results
The 2001 National Health Survey (NHS) estimated the prevalence of current infertility to be 2.8%, based on self-reports of infertility by 10,418 non-menopausal married women aging 15-49 years (3). The number of cases had been proportional to that of the population in respective provinces.
Tehran Study was carried out by Barouti et al. on 1992 women who had been married for at least one year and were 15-49 years old in Tehran and its suburban areas in 1997 (4). The prevalence of lifetime infertility was estimated to be 21.9% while the lowest prevalence (15.8%) was observed in the age group between 19-27 years.
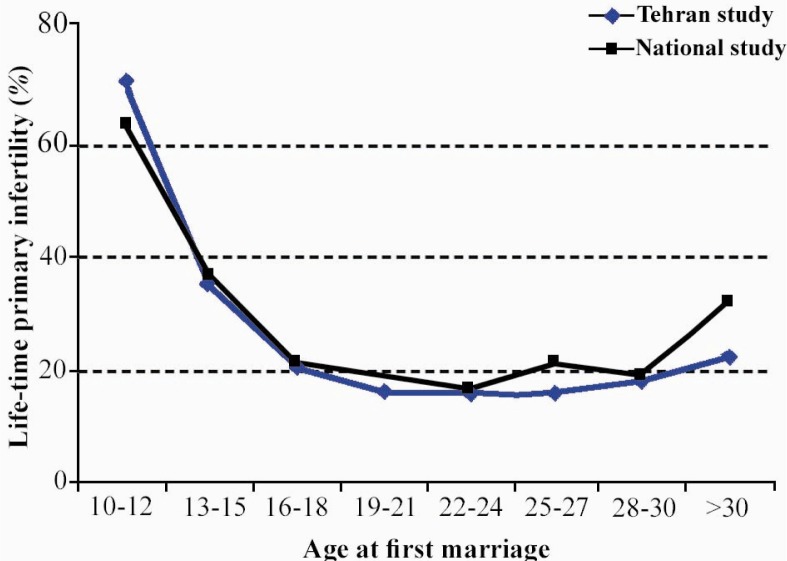
Vahidi et al. studied the prevalence of current and lifetime primary infertility in all provinces of Iran, in sample sizes proportionate to the size of populations there during 2004-2005 (5). The project supported by the NRCMSI, studied 10,783 women aging 19-49 years. A history of lifetime primary infertility was found in 24.9% of the subjects and the prevalence of current primary infertility was 3.4%. The lowest prevalence (17.2%) was seen in the age group of 21-26 years. Figure 1 compares the prevalence of primary infertilities according to age at the first marriage between the NIS and the Tehran Study.
Figure 1.
The prevalence of primary infertility by age at the first marriage; estimated by National Infertility and Tehran Studies.
Discussion
All the three aforementioned studies included considerable sample sizes that led to acceptable precision of estimation. All the three studies had employed inability to conceive upon one-year of unprotected sex for defining primary infertility. While the other two studies had only considered current primary infertility for the definition of infertility, the NIS had considered both definitions. The prevalence of lifetime primary infertility shows the proportion of couples who have experienced this problem at some time during their married life, while prevalence of current primary infertility indicates the number of couples who may be the potential users of infertility services.
Regarding the prevalence of life-time primary infertility, we observed a higher estimate in NIS report compared to that of Tehran Study (24.1% versus 21.9%). This could be due to an older age at the time of marriage for people in Tehran compared to the average age of marriage for other women in the country . The highest prevalence rate of primary infertility was observed in individuals with the youngest age at the time of marriage in NIS and Tehran Study; although NIS reported higher estimates (17.2% versus 15.8%). The prevalence of primary infertility can be affected by age at the time of marriage, which is a surrogate for other indicators of conception such as the number of successful ovulatory cycles. The differences between the average prevalence of primary infertility between the aforementioned studies can be explained by the difference in age eligibility to have been included in the studies, as the minimum inclusion age had been 15 and 19 years in Tehran study and NIS, respectively. The trend for primary infertility in both studies showed that highest rates of infertility were more likely to be seen with youngest age at the time of marriage.
Appropriate sets of questions are critical in measuring the prevalence of primary infertility. The definition of infertility and its different categories has always been a controversial issue in clinical and epidemiological studies (6, 7), causing wide variations in prevalence estimates and in the time threshold for the initiation of its treatment.
Furthermore, the precise definition of numerators and denominators of the equation for the calculation of primary infertility is a crucial point. The numerator has to be the number of infertile couples over a certain period of time. In all the three studies, the definition of “infertile couples” was based on inability to conceive upon one year of unprotected intercourse (8). The appropriate duration for unprotected intercourse is the most important element in this definition. Increasing this period to 24 months can result in underestimating the prevalence of primary infertility (9). The denominator for the calculation of primary infertility is the number of couples to be at the study for the whole duration of the period.
Overestimating the number of women at risk of infertility leads to the underestimation of infertility prevalence rates (10). Omitting both the women who have become pregnant despite contraception and those who have been on contraceptives since marriage will cause biased estimates. Nevertheless, it is not clear whether a woman who is on contraceptives is infertile or not. NIS omits both groups from its calculations and overestimates the related lifetime and current primary infertilities of the first group as 0.8% and 0.6%, respectively. There is no information on the estimation bias in the second group, because it is expected that some of the women who had been using contraception at the time of the interview had been experiencing infertility (5).
The prevalence of current primary infertility is estimated to be 3.4% by NIS and 2.8% by NHS. NHS does not exclude the following groups from the denominator, leading to the underestimation of current primary infertility: a) the newly married women who have not discontinued contraceptive use and b) women who have stopped contraceptive use for at least one year, but have not become pregnant.
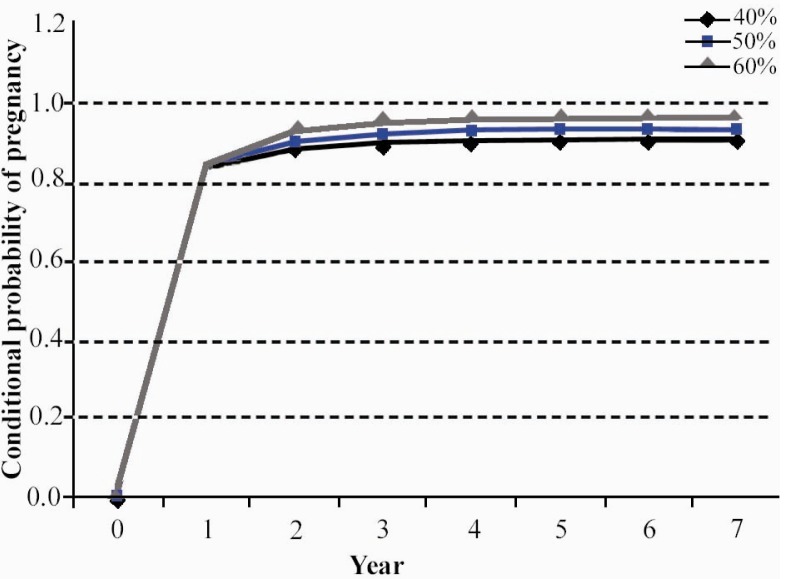
Figure 2 presents the conditional probability of pregnancy without intervention, given the primary infertility of 16.0% in the first year of marriage and the three scenarios for pregnancy reduction rates of 40%, 50% and 60% per year. Assuming that the conditional probability of pregnancy is reduced by half per year, after seven years of unprotected sex, only about 6.0% of couples would remain infertile without any intervention. This figure is 8.7 and 3.9% for the reduction rates of 40% and 60%, respectively. Increasing chances of pregnancy without intervention over time raises the question of the effectiveness of therapeutic measures.
Figure 2.
The conditional probability of pregnancy without intervention, assuming pregnancy reduction rates of 40%, 50% and 60% per year.
Conclusion
Almost 21-22% of Iranian women experience primary infertility at some time during their married life. The best age of marriage for women to minimize the chances for primary infertility is thought to be 20-27. In this age group, 16-18% of women experienced primary infertility. Appropriate sets of questions seem to be critical to measuring the prevalence of primary infertility. Precise definition of numerator and denominator is also a crucial issue in estimating the prevalence of primary infertility.
To cite this article: Mohammad K, Ardalan A. An Overview of the Epidemiology of Primary Infertility in Iran. J Reprod Infertil. 2009;10(3):213-216.
References
- 1.Vayena E, Rowe PJ, Griffin PD. Geneva: World Health Organization; 2002. Current practices and controversies in assisted reproduction: Report of a meeting on “Medical, Ethical and Social Aspects of Assisted Reproduction” held at WHO; p. 369. [Google Scholar]
- 2.Schmidt L, Munster K, Helm P. Infertility and the seeking of infertility treatment in a representative population. Br J Obstet Gynaecol. 1995;102(12):978–84. doi: 10.1111/j.1471-0528.1995.tb10905.x. [DOI] [PubMed] [Google Scholar]
- 3.Noorbala AA, Mohammad K. [Health survey in Iran] Tehran: Deputy of research, Ministry of Health & Medical Education; 2001. Persian. [Google Scholar]
- 4.Barouti E, Ramezani Tehrani F, Heydari Seradj M, Khalajabadi Farahani F, Mohammad K. [Primary infertility based on marriage age in Tehran] Hakim. 1999;2:88–93. Persian. [Google Scholar]
- 5.Vahidi S, Ardalan A, Mohammad K. Prevalence of primary infertility in the Islamic Republic of Iran in 2004-5. Asia Pac J Public Health. 2009;21(3):287–93. doi: 10.1177/1010539509336009. [DOI] [PubMed] [Google Scholar]
- 6.Rutstein SO, SHah IH. Infecundity, infertility, and childlessness in developing countries; Calverton, Maryland, USA: ORC Macro and the World Health Organization; 2004. DHS comparative reports No.9. [Google Scholar]
- 7.Habbema JD, Collins J, Leridon H, Evers JL, Lunenfeld B, te Velde ER. Towards less confusing terminology in reproductive medicine: a proposal. Hum Reprod. 2004;19(7):1497–501. doi: 10.1093/humrep/deh303. [DOI] [PubMed] [Google Scholar]
- 8.Larsen U. Research on infertility: which definition should we use? Fertil Steril. 2005;83(4):846–52. doi: 10.1016/j.fertnstert.2004.11.033. [DOI] [PubMed] [Google Scholar]
- 9.Rowe PJ. WHO manual for the standardized investigation and diagnosis of the infertile couple. 1st ed. Geneva: Cambridge University Press; 1993. p. 83. [Google Scholar]
- 10.Che Y, Cleland J. Infertility in Shanghai: prevalence, treatment seeking and impact. J Obstet Gynaecol. 2002;22(6):643–8. doi: 10.1080/0144361021000020457. [DOI] [PubMed] [Google Scholar]
- 11.Thonneau P, Spira A. Prevalence of infertility: international data and problems of measurement. Eur J Obstet Gynecol Reprod Biol. 1991;38(1):43–52. doi: 10.1016/0028-2243(91)90206-z. [DOI] [PubMed] [Google Scholar]