Abstract
Background
Gap-junctional intercellular communication (GJIC) is implicated in physicological processes and it is vitally important for granulosa cell (GC) differentiation and oocyte growth. We investigated the expression of connexin 43 (Cx43), a gap junctional protein, in normal and androstenedione-induced polycystic ovary (PCO), the effects of androstenedione on Cx43 expression, GJIC and progesterone production in granulosa cells in vitro.
Methods
Isolated GCs from rat ovary were supplemented with FSH and dripped with EHS-matrix (EHS-drip) in culture media, were treated with physiological (10−7 M) or pathological (10−5 M) androstenedione concentrations to induce differentiation. Cx43 protein levels were assessed by Western blotting. Immunohistochemistry was also used to determine the localization of Cx43 in GCs and corpus luteum (CL) of controls and PCOs. Differentiation of GCs was determined by progesterone assay and Lucifer yellow dye transfer for GJIC status. The degree of significance of variations between the results was analyzed by ANOVA using SPSS (version 11.5; 2002).
Results
Cx43 localized in the GC layer of both the control and PCOs. Its protein levels were upregulated in PCO rat ovaries. GCs in culture with or without androstenedione had a punctate membranous distribution of Cx43. However, androstenedione increased GJIC and upregulated progesterone and Cx43 protein levels. Inhibiting GJIC by 18-α GA in androstenedione-treated GCs caused partial inhibition of progesterone production, suggesting a possible role of GJIC in mediating the action of androstenedione on GC differentiation.
Conclusion
This study presented a suitable culture model for polycystic ovary syndrome and showed that Cx43 and GJIC might contribute to the pathogenesis of polycystic ovary syndrome.
Keywords: Androstenedione, Connexins, Extracellular matrix, Gap junction intercellular communication, Granulosa cell, Ovary, Polycystic ovary
Introduction
The Polycystic Ovary Syndrome (PCOS) first identified in 1935 (1), accounts for 75% of anovulatory infertility cases in women which makes it one of the most common humandisorders and particularly a major endocrinopathy in women of reproductive age (2). PCOS is a complex and heterogeneous genetic disorder characterized by androgen excess and ovulatory dysfunction (1). Follicular growth is disrupted as a result of ovarian hyperandrogenism, hyperinsulinemia due to insulin resistance and distorted intraovarian paracrine signaling (3). In PCOS, folliculogensis occurs normally throughout the preantral stage; beyond which the progression of the follicle into a preovulatory one will be disturbed. In addition to the role of the endocrine control in the development of the preantral follicle, there are various paracrine and autocrine factors identified in small follicles, playing roles during early follicular growth not to mention a critical role of the oocyte in this process (4–7). Studies have shown that granulosa cells (GCs) in antral follicles in PCOs exhibit decreased aromatase activity, altered response to growth factors, hormones and early leutinization (8−10).
Normally, inactive primordial follicles undergo arrest at prophase I and contain nongrowing oocytes and squamous pregranulosa cells supported by a basal lamina. As these follicles get activated the squamous pregranulosa cells will develop to form a single layer of cuboidal granulosa cells that will later divide to form a multilayered follicle (11). It is clear that tissue remodeling is essential for follicular maturation; as such, the communication between GCs and the extracellular matrix (ECM) is inevitable for normal folliculogenesis. The role of ECM in GC function has been investigated since early 1980s and continues with the improvement in the in vitro culture systems (12). Attempts to study GC differentiation in vitro has focused on the effects of soluble mediators such as hormones, growth factors, cytokines and neurotransmitters (13–15); however, the crucial role of the microenvironment in GC differentiation is poorly understood. It has been shown that antibodies which block cell-ECM interactions have resulted in the loss of progesterone synthesis in cultured rat GCs in vitro (16). In addition, studies have revealed that ECM rescues primary GCs from apoptosis (17). Consistent with this, it has been shown that gonadotrophins and ECM synergize to regulate GC differentiation, as measured by progesterone production, and induction of gap junction formation (18).
Gap-junctional intercellular communication (GJIC) is implicated in many normal physiological and pathological processes. GYIC has been documented to play a crucial role in the physiology of the ovarian follicle. GJIC has been also implicated in the control of steroidogenesis (19). In ovaries, connexin 43 (Cx43), encoded by Gja1, has been found to be the main connexin expressed in developing follicles forming the gap junctions coupling granulosa cells (20–23). In agreement with the role of gap junctions in folliculogenesis, Cx43 knockout mice have had folliculogenesis arrest in their primary stage and developed incompetent oocytes (24, 25). Furthermore; GCs lacking Cx43 have displayed lower proliferation rate and reduced response to oocyte-derived mitogens resulting in an impaired function of these cells (26, 27).
The regulation of GJIC and connexin protein expression by steroids has been documented in several cell types (28–30), including ovarian cells (31); causing either a downregulation or an elevation in the expression of gap junctional proteins. An in vitro study revealed that GJIC up-regulation in granulosa-oocyte complex is independent of gonadotropins (32). However, its breakdown is gonadotropin dependent and occurs by the clustering of Cx43 in lipid raft microdomains of the cells.
Taking into account the importance of GJIC for GC differentiation and oocyte growth, in addition to the important role of steroids in controlling GJIC, the current study was designed to study GJIC in GCs of androstenedione-induced PCOS in rats using in vivo and in vitro models. Specifically, we investigated the expression of Cx43, a gap junctional protein, in normal and androstene-dione-induced PCO, the effects of androstenedione on Cx43 expression, GJIC, and progesterone production in vitro.
Methods
Materials
Androstenedione, Diethylstilbestrol (DES), equine chorionic gonadotrophic (eCG) and human chorionic gonadotrophic (hCG) hormones, follicle stimulating hormone (FSH), Hanks Balanced Salt Solution (HBSS), Dulbecco's Minimal Essential Medium (DMEM-F12), penicillin/ streptomycin, trypsin-EDTA, poly-L-lysine and 18α glycyrrhetinic acid (18αGA) were purchased from Sigma Chemical Co. (St Louis, Missouri, USA). Protease inhibitors, CompleteTM, were obtained from Boehringer (Mannheim, Germany). Fetal bovine serum (FBS) was purchased from Gibco (Paisely, Scotland). The source of growth factor reduced EHS (Engelberth-Holm-Swarm tumor)-matrix, Matrigel™, was from Collaborative Biomedical Products (Bedford, MA, USA). PVDF membranes and α-32PdCTP were supplied by Amersham Pharmacia Biotech (Uppsala, Sweden), and rat-specific progesterone RIA kits were obtained from Immunotech (France). Rabbit anticonnexin 43 was obtained from Zymed (San Francisco, CA, USA). Anti-rabbit and anti-goat IgG HRP conjugated antibodies, β actin antibodies, Enhanced Chemiluminescence (ECL) kit and ECL markers were obtained from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Lucifer Yellow CH (LY), Secondary goat anti-rabbit IgG FITC-conjugate, propidium iodide, and Prolong AntifadeTM kit were purchased from Molecular Probes (Leiden, Netherlands). Biorad DC protein assay reagent was obtained from Biorad (Hercules, CA, USA). All other material used was of molecular biology grade.
Animals, hormone treatments and tissue sections
Immature 21−24 day old female Sprague Dawley rats were obtained from the animal care facility at the American University of Beirut. All animal care requirements were fulfilled, and animals were given food and water ad libitum. Rats were sacrificed by cervical dislocation. For in vivo studies, rats were divided into five groups. The control group received injections of corn oil (100 µl/day for 3 days, subcutaneously [s.c.]) and ovaries were subsequently removed one day after the last injection. Another group of rats received injections of DES (1 mg/day, for 3 days, s.c.); the rats were then either sacrificed (DES group; ovaries enriched in preantral follicle-undifferentiated GCs) or subsequently received injections of eCG (15 IU, intraperitoneal injection [i.p.]). Forty-eight hours later, the latter group of animals were either sacrificed (eCG group; ovaries enriched in antral follicle-differentiated GCs) or administered hCG (15 IU; i.p.) and sacrificed eight hours, thereafter (hCG group; ovaries enriched in luteal cells). This protocol was used to mimic the different follicular developmental stages in the rat ovary (33). The PCOS group received daily injecttions of androstenedione at a concentration of 6 mg/100 g body weight dissolved in 200 µl corn oil for 21 days. It is established that this treatment is sufficient to induce PCOS in 24 day-old female rats (34–39). The ovaries were removed, fixed in 4% buffered formaldehyde, embedded in paraffin, and sectioned at 5 µm and mounted onto Vectabond coated slides. Sections were used for immuunofluorescence as described later. For GC culture, rats received daily injections of DES (l mg/day, s.c.) for three consecutive days. Ovarieswere excised and surrounding tissues were removed.
Cell culture
For GC culture, ovaries were washed in cell culture medium (DMEM-F 12) containing 5% FBS. GCs were harvested in DMEM-F 12 containing 5% FBS by follicle puncture using 25-gauge needle fitted to a 1 ml insulin syringe. The GCs were isolated from the excised ovaries using gentle pressure with a blunt microspatula. The culture medium was collected and the cells were sedimented by centrifugation at 150 g for 5 min at 4 °C. The pellet was then washed with DMEM-F12 and resuspended in l ml of DMEM-F 12. The cells were counted using a hemocytometer and plated in a 24-well cell culture plate at a seeding density of l.5x105 cells/ml. Cells were maintained in a humidified incubator (95% air, 5% C02) at 37 °C. GCs were plated on serum precoated tissue culture plates in serum supplemented (5% FBS) DMEM-F12 media in the presence of 20 ng/ml FSH and 1% penicillin/streptomycin. The medium was changed on the first day after plating and on subsequent days as needed. Serum was removed on day 1 after plating and diluted MatrigelTM (1.5% vol/vol) was dripped (hereafter referred to as EHS-drip), onto cells (40). After washing, cells were grown on plastic without matrigel.
GCs were cultured with or without androstenedione at 10−7 or 10−5 M (dissolved in 100% ethanol) as of day 1 after plating. Cells were trypsinized and counted (Trypan blue viable counts) using a hemocytometer, and the conditioned medium was collected for progesterone quantification using a radioimmunoassay kit according to the manufacturer's instructions.
In experiments where 18αGA was added to GCs, 50 µM 18αGA (dissolved in DMSO) was added to the cultured GCs on day l of culture. Media were changed on a daily basis and accompanied with repeated androstenedione treatments.
Progesterone assay
Cells were cultured on plastic, EHS-drip in 24-well plates. Media conditioned beta cells were collected on daily basis until day 6 of culture. Upon collection, 40 µl of diluted protease inhibitors cocktail was added to the media. The sampled media were stored at −70 °C for subsequent analysis. Progesterone concentration in the media was quantified using a solidphase radioimmunoassay (RIA) kit. The assay was performed according to the manufacturer's instructions. Samples from each treatment were run in duplicates and the values were converted to concentrations by extrapolation from a standard curve.
Western blot analysis
Total proteins extracted either from ovaries or GCs in culture were analyzed by western blotting for Cx43 as described by El-Sabban et al. Briefly, ovaries were homogenized for 2 min, into RIPA buffer supplemented with protease inhibitors (40 µl/l ml of RIPA). The homogenate was then centrifuged at 10,000 g for 30 min where the supernatant was removed and stored at −70 °C. For GCs in culture, protein extraction was performed on day 4 of culture by scraping the cells in RIPA buffer supplemented with protease inhibitors. The scraped cells were then sheared, centrifuged at 10,000 g for 30 min and the supernatant was removed and stored in aliquots at −70 °C. Biorad assay was used for quantification of protein content of samples extracted from both cells and ovaries. Twenty µg of protein were run on a 12% SDS-PAGE and blotted. Membranes were then blocked in 3% skimmed milk for 1 hr, incubated with primary rabbit anti-connexin 43 according to the supplier's suggestion in 5% skimmed milk for 1 hr at room temperature then for 1 hr at room temperature in 3% skimmed milk solution containing goat antirabbit IgG conjugated to horse raddish peroxidase (1:5000). Immunoreactivity was detected using enhanced chemiluminescence.
Immunohistochemistry
GCs were cultured on poly-L-lysine coated EHS-dripped coverslips in 24-well plates as described previously. On day 4 of culture, cells were washed with warm HBSS and fixed in cold (−20 °C) 70% ethanol. Fixed cells were rinsed twice with phosphate-buffered saline (PBS), blocked for 1 hr with 3% normal goat serum and incubated for 2 hr at room temperature with rabbit anti-connexin 43. The cells were then incubated for 1 hr with secondary goat anti-rabbit IgG (H + L) FITC-conjugate. Concentrations of the primary and secondary antibodies were used as recommended by the supplier. Nuclei were counterstained with propidium iodide (5 µg/ml). Washing with PBS was performed twice between incubations. Cells were then mounted on slides and staining was preserved by adding AntifadeTM to the stained cells. Cells were observed using a fluorescence microscope (Zeiss LSM 410, Germany). Same procedure was followed for the immunohistochemistry of the ovarian sections, except that deparafinization and rehydration in an ethanol gradient were needed before proceeding in the immunostaining. All incubations and washings were done at room temperature.
Lucjfer yellow dye transfer assay
GCs were grown on EHS-drip in 8-chamber polystyrene tissue culture treated glass slides at 3.0x105 cells/ chamber. Scrape-loading technique was performed using Lucifer Yellow (LY) dye (41, 42).
Statistics
The degree of significance of variations between average levels of progesterone from triplicate wells was determined after appropriate Analysis of Variance (ANOVA) using Least Significant Difference (LSD) test. All analyses were performed using SPSS version; 11.5 for windows SPSS Inc., Chicago, IL, USA).
Results
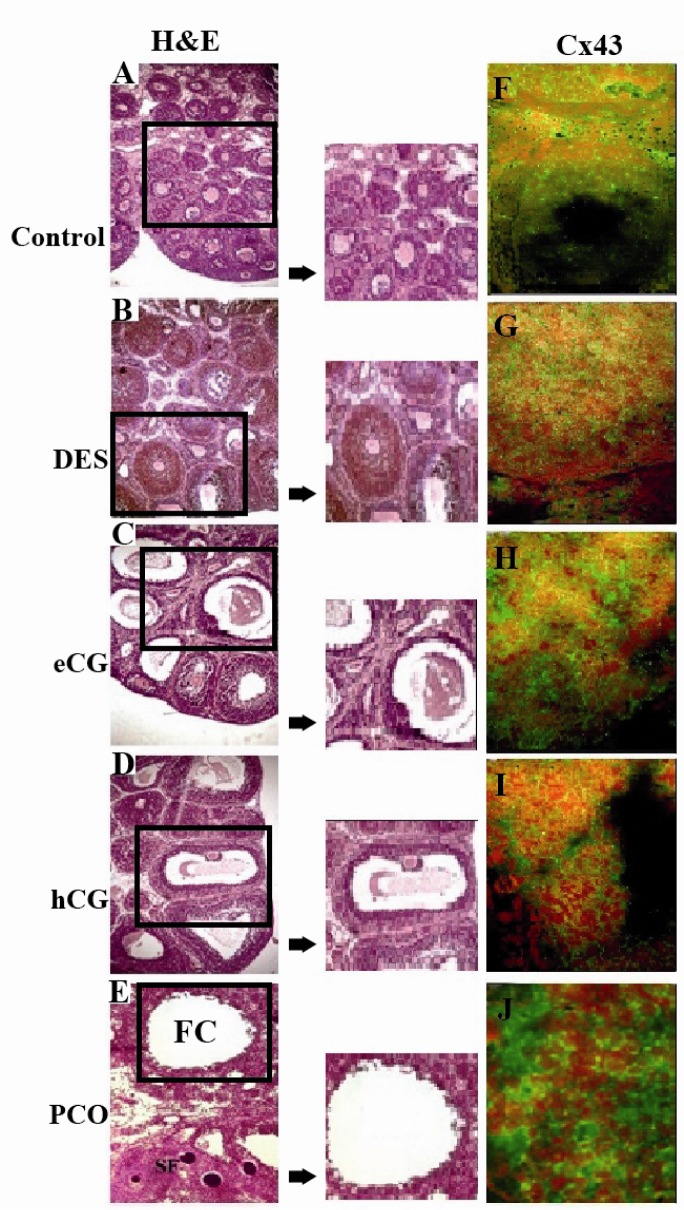
To reveal a potential role of Cx43 in GC function, we aimed to characterize its distribution in rat ovaries from hormone-treated animals with different follicular developmental stages and in those from rats with PCOs after androstenedione induction. Sections were by stained H&E to reveal follicular development in each of control, treated and PCOs groups. As (Figure 1A-E) indicates, control ovaries had mostly primordial and primary follicles (Figure 1A). The DES-treated group had their ovaries filled with preantral follicles (Figure 1B). Follicles were at the early antral to late antral stage in ovaries of the eCG group (Figure 1C). The hCG ovaries were filled with follicles at the preovulatory stage having the oocyte in an eccentric position (Figure 1D). Polycystic ovaries were enlarged and occupied with follicular cysts that were either devoid from oocytes or had their oocytes surrounded with a maximum of two layers of GCs. Immunolocalization of Cx43 in rat ovaries of DES, eCG, hCG, and PCO groups stained with H&E stains (Figure 1A-E) revealed that Cx43 localized to the GCs of all animal groups (Figure 1F-J). Cx43 was not detected at the thecal cell layer or at the border between GCs and oocytes where Cx26 and Cx32 were found to be predominant, respectively (data not shown).
Figure 1.
Hematoxylin and Eosin stains and Cx43 immunolocalization for rat ovarian sections of control (A & F), DES (B & G), eCG (C & H), hCG (D & I) and androstenedione (PCO; E & J) treated rats where section in the squares are magnified to reveal the clear structure of the follicle. Image (E) shows a section of polycystic ovary with a follicular cyst (FC) in addition to small follicles (SF). Middle panel represents enlarged areas of similar sizes representing the follicle features in every condition. Cx43 localizes to the GCs in all stained sections. Micrographs are taken at 5X magnification
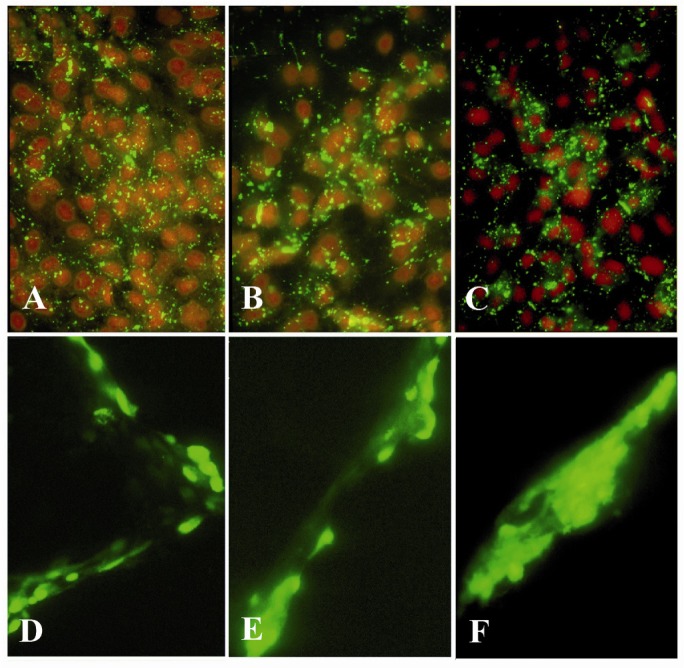
To assess the effect of androstenedione on Cx43 expression and localization and GJIC functionality, GCs’ expression and localization of Cx43 were examined. When GCs were plated on EHS-drip with or without androstenedione, they expressed Cx43 as indicated in (Figure 2A-C). To further analyze the effect of androstenedione on Cx43 cellular distribution in GCs culture immunelocalization studies were performed. Cx43 expression was evident at 4 days in culture and had a punctate membranous appearance in the absence or presence of androstenedione at both 10−7 M and 10−5 M concentrations (Figure 2A-C). Neverthe-less, the functionality of GJIC between GCs on day 4 of culture was enhanced upon androstenedione treatment. Confluent cultures of GCs plated on EHS-drip alone displayed limited dye transfer to neighboring cell layers (Figure 2D), although these cells showed increased dye transfer when compared to cells cultured on plastic alone (data not shown). Similar transfer of the fluorescent dye was observed with GCs cultured on EHS-drip with 10−7 M androstenedione when compared to control untreated cultures, however, appreciable increase in LY transfer to cell layers away from the scrape sites was noted when GCs were cultured on EHS-drip with 10−5 M androstenedione (Figure 2F), suggesting enhanced GJIC in PCO-like conditions (34).
Figure 2.
Immunolocalization of Cx43 (A-C) and lucifer yellow dye transfer (D-F) in GCs on day 4 of culture. GCs were plated on EHS-drip without androstenedione (A & D), with 10−7 M (B & E) or 10−5 M (C & F) androstenedione. Although Cx43 distribution was not altered in either of the cultured conditions, GJIC was markedly enhanced when cells were treated with 10−5 M (F) androstenedione. Fluorescent microscopy images were obtained at 10X (A-C) and 20X magnifications (D-F)
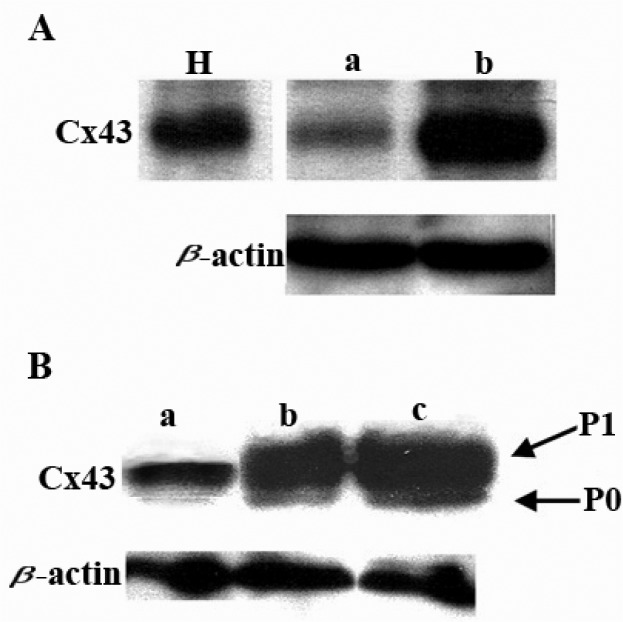
Since Cx43 has been shown to be the major Cx expressed in GCs in vivo in both control and PCOs, we examined the localization and levels of expression of Cx43 in GCs in response to androstenedione dosages. Western blot analysis showed that the treatment of rats with 10−5 M concentration of androstenedione upregulated Cx43 expression in their PCOs (Figure 3A). Similarly, and parallel to enhanced GJIC noted in culture, androstenedione also enhanced Cx43 expression at 10−7 and 10−5 M by cultured GC in a dose-dependent manner. Enhanced phosphorylation of Cx43 was also noted in androstenedione treated cells (Figure 3B).
Figure 3.
Effect of androstenedione on Cx43 expression. A. Western blot analysis of Cx43 protein in normal rat ovaries (lane a) and in androstenedione treated rats’ PCO ovaries (lane b). Lane H: heart sample Cx43 control. B. Western blot analysis of Cx43 protein in GCs on day 4 of culture. Cx43 proteins expressed in GCs cultured on EHS-drip (lane a), in the presence of 10−7 M (lane b) or 10−5 M (lane c) androstenedione. P0, unphosphorylated form of Cx43 protein, P1 phosphorylated active form of Cx43. β-actin protein shows for equal loading
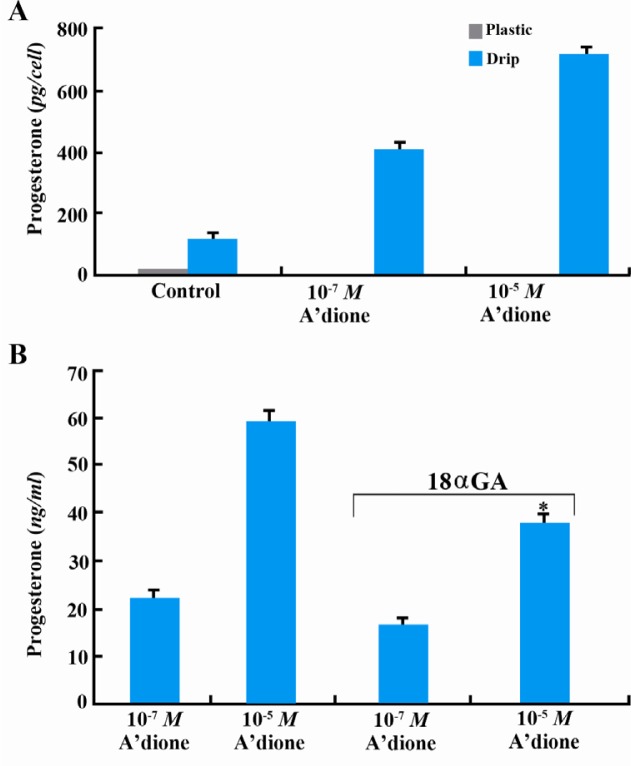
Progesterone production was used as an indicator of the extent of differentiation of GCs. We showed that the enhanced GJIC and Cx43 expression in androstenedione-treated cells was paralleled by an increase in progesterone production. To assess the effect of androstenedione on progesterone levels produced by GCs on day 4 of culture, RIA analysis was performed. Whereas GCs on p lastic produced very low levels of progesterone (<20 pg/cell), cells on EHS-drip produced significantly (p <0.05) higher progesterone levels (> 100 pg/cell). Furthermore, EHS-dripped GCs cultured with 10−7 M and 10−5 M androstenedione, significantly increased their progesterone levels, in a dose dependent manner, as compared to the controls. GCs cultured with 10−5 M androstenedione produced more than 700 pg/cell of progesterone (Figure 4A).
Figure 4.
Androstenedione induces progesterone production in GC cultures in a GJIC-dependent manner. A. GCs on day 4 of culture on EHS-drip in the absence (control) or presence of 10−7 M or 10−5 M androstenedione. Progesterone production is enhanced by androstenedione in a dose-dependent manner. Note: minimal levels of progesterone (<20 pg/cell) are produced by GC cultured on plastic. The amount of progesterone (pg) secreted into the media was normalized per one cell. B. Effect of 18αGA on progesterone production by GCs on EHS-drip and treated with 10−5 M and 10−7 M androstenedione and 50 µM of 18αGA show marked downregulation of progesterone production on day 4 of culture. Statistical analysis obtained from these experiments reveals statistical significance at p <0.05 represented by asterisk (*). In (A) all results are significantly different from each other
In order to study the role of GJIC in facilitating progesterone production in GCs in response to androstenedione 18αGA, a gap junction inhibitor, was used. Increased progesterone production was at least partly a consequence of increased GJIC since 18αGA decreased progesterone production by GCs in culture. Compared to control untreated cells, progesterone production by GCs cultured on EHS-drip in the presence of 10−5 M androstenedione was inhibited by about 40% in the presence of 18αGA with no significant difference (p <0.05) in its levels in the 10−7 M androstenedione (Figure 4B).
Discussion
GJIC has been shown to regulate major cellular programs such as growth, differentiation, and apoptosis (41, 43–45). More specifically in the ovary, cell-cell communication between GCs allows transport of metabolites and signal molecules between them and also with oocytes. This cellular communication is crucial for follicular development and oocyte growth and maturation (46). Mice with disrupted GJs were infertile and the communication between oocytes and the neighboring GCs was greatly reduced (47). Aberrant GJIC is involved in ovulatory dysfunction, results in interrupted folliculogenesis and prevents formation of GC layers around the oocyte in Cx43 null mice. Ackert et al. demonstrated that the mutant oocytes obtained from Cx43 null mice failed to undergo meiotic maturation and could not be fertilized. This correlation between abnormal folliculogenesis, Cx43 expression and aberrant GJIC prompted our laboratory to investigate the regulation of Cx43 in the PCO.
In vivo rat PCO model has long been established, and could be experimentally induced through prolonged injections of androgens in immature female rats (38, 39, 48). In the current study, androstenedione was successfully used to induce PCOs in rats as verified by H&E staining of PCO sections. These ovaries had evident follicular cysts, and lacked corpora lutea, as most follicles developed into early follicular stages but did not develop to ovulatory stages in PCOs (49, 50). In the ovary of a control 41-day old rat, Cx43 was localized to GCs of small and large follicles and the corpus luteum (CL). In androstenedioneinduced PCO rats, Cx43 was also localized in follicular GCs. This is consistent with previous data indicating that Cx43 was present in follicular GCs of rat (51), mouse (24, 52), ewe (53), cow (54), and pig (55, 56). Cx43 has also been previously detected in rat CL (57, 58).
In this study, GCs were grown in the culture media under differentiation-permissive conditions, supplemented with FSH and dripped with EHS-matrix. GCs cultured on plastic in media lacking androstenedione produced very low amounts of progesterone while those cultured on EHS-drip produced appreciable amounts. More so, increased progesterone production by GCs on EHS-drip was noted in response to androstenedione in a dose-dependent manner. This suggested that EHS-drip and androstenedione together synergistically promoted progesterone production by GCs. It has previously been shown that growing mammary epithelial cells enhanced their differentiation phenotype and GJIC with EHS-drip and lactogenic hormones (41, 59). During the follicular phase of ovarian cycle, androstenedione produced by theca cells reaches a level of 10−7 M in the follicular fluid. In PCO syndrome, androstenedione levels rise from 10−7 M to 10−5 M, which is the androgen concentration that reaches the GCs (60, 61). The mechanism of this rise in androgen levels is unclear. Nevertheless, this excess clearly adds up to the complexity of PCOS and is mediated by both intrinsic and extrinsic factors (62). The rise in androstenedione levels is either due to increased activity of theca cells, or decreased GC ability to aromatize the accumulating androgens into estrogens (63, 64). Given that, 10−7 M (moderate) and 10−5 M (high) androstenedione concentrations were used to study the effects of androstenedione on Cx43 expression, GJIC and subsequently GC differentiation.
Cx43 is the major Cx expressed by GCs that contributes to intercellular coupling; hence playing role in GC development, maturation, differentiation and leutinization (46, 65). As such, we intended to characterize the effect of androstenedione on Cx43 expression, localization and GJIC to further understand how GJs display PCO phenotype through their effects on GC differentiation. Cx43 immunolocalization showed punctate membranous distribution in GCs when cultured on EHS-drip, in the presence of both 10−7 and 10−5 M androstenedione, or in androstenedione free medium. However, scrape loading of LY showed a significant increase in GJIC in the presence of 10−5 M androstenedione. Increased LY dye transfer in the presence of 10−7 M androstenedione was not as evident. In parallel experiments we showed that no LY transfer was noted in GC cultured on plastic compared to those on EHS-drip (not shown). Taken together, the data suggests a possible synergistic role of both hormones, androstenedione in this case and ECM, in promoting GJIC. A similar observation was reported earlier in mammary epithelial cells (41). In fact, in human GCs, hCG and ECM synergize to enhance gap junction formation and progesterone production (18). As for GJIC, androstenedione could be acting directly on increasing Cx gene expression in GCs, since it has been shown previously that Cx43 promoter is responsive to estrogens (66), and that estrogen upregulated Cx43 expression in GCs in vivo (57). Though, estradiol and progesterone have been shown to decrease Cx43 protein levels when administered together into cultured rat endometrial cells (28). Alternatively, androstenedione could be activated by several kinases, such as MAP kinase which is also activated by ECM (67), and it has been shown to regulate GJIC (68–70). Direct regulation of GJIC in GCs by either estrogens or androgens has not been previously studied. It was found that Cx43 protein levels were highly upregulated in the PCOs as compared to the controls. This trend is not noted in the immunohistochemistry as it only reveals the distribution and localization of Cx43.
Quantification of fluorescence was not attempted and Western blotting for Cx43 protein was used for quantification purposes instead.
The elevation of Cx43 protein levels observed in PCOs in this study cannot be attributed to an increase in the number of ovarian blood vessels expressing Cx43, since H&E staining of both PC and control ovaries did not reveal any difference in vascularization (not shown). GJIC is at least partly mediated by Cx43 post-translational modification through kinase activation (41, 71) because an increase in Cx43 protein levels and phosphorylation in the presence of 10−7 M and 10−5 M androstenedione were noted. It has been documented that GJIC in porcine granulosa cells was enhanced by protein kinase A (PKA) phosphorylation but decreased by protein kinase C (PKC) (72). Other studies indicated that FSH-stimulated Cx43 phosphorylation was attributable to PKA (73), and that casein kinase 1 induced Cx43 gap-junction assembly (74).
Androstenedione treatment of GCs on EHS-drip promoted increased GJIC in GCs, in addition to increased progesterone production. Yet, under physiological concentrations (10−7 M) of androstenedione, inhibiting GJIC did not lead to a significant decrease in progesterone production levels suggesting that GJIC is not the sole mediator but could contribute along with ECM to progesterone production. Cx43 effect on progesterone production is only prominent under non-physiological doses of androstenedione (10−5 M). The effect of ECM, androstenedione and FSH on GC differentiation and progesterone production is likely due to the collective effects of enhanced activity and expression of the steroidogenic enzymes (75), deposition of some basement membrane components like fibronectin and proteoglycans, maintenance of FSH receptors under optimal culture conditions (75) and/or an increase in c-AMP production (76). Treating cultured rat GCs with cAMP increases GJIC (77, and unpublished data), since cAMP, apart from being a second messenger, has been known to enhance GJIC and induce differentiation in several cell types (41, 78). Knowing that GJIC may play a role in increasing progesterone and consequently mediating GC differentiation, the effect of inhibiting GJIC on GC differentiation had to be examined. When treating GCs with 18αGA, an inhibitor of GJIC (41, 79–81), progesterone production was downregulated. It is worth noting that the androstenedione-induced differentiated phenotype, as evident by increased progesterone production, was unlikely due to changes in cell morphology since GCs cultured on EHS-drip with or without androstenedione did not show marked altered morphology. Therefore, the effect of androstenedione on progesterone production may be partially mediated by increased GJIC, either through upregulating Cx43 levels of protein expression, as seen in our study, or through promoting Cx43 phosphorylation by activating several kinases.
The involvement of other connexins in regulating GC function cannot be ruled out (46). In fact, Cx45 has been shown previously to be expressed by rat ovarian GCs (82). Similarly, we showed Cx45 immunolocalization in GCs of normal rat ovaries and PCOs, and Cx45 protein levels were upregulated in PCOs as compared to normal ones (unpublished data), further suggesting the involvement of Cx45 in addition to Cx43 in modulating GJIC in GCs following androgen stimulation. The role of Cx45 in PCO syndrome needs further investigation.
Conclusion
Gap junctions form a network of bonded interconnecting GCs that surround the oocyte, and the loss of these junctions may facilitate the dissociation of the oocyte and disrupt normal folliculogenesis. In conclusion, this work demonstrates for the first time the modulation of Cx43 in androstenedione-induced rat PCO. Moreover, androstenedione induced luteinization of cultured GCs together with enhanced GJIC, and Cx43 expression suggest a role for gap junctions in partially mediating the effect of androstenedione on progesterone production. Further studies are required to understand the androstenedione-induced GJIC dependent signaling pathways mediating a PCO-like phenotype in vitro.
Acknowledgement
The authors are grateful to doctors. Medhat Khattar and Joana Kogan for critical reading of the manuscript. Wissam Mehio is acknowledged for assisting in the preparation of the manuscript. This work is supported by the University Research Board (RST, CGT and MES). Medical Practice Plan, Diana Tamari Sabbagh Research Fund, Terry Fox Cancer Research fund (MES), and Lebanese National Council for Scientific Research (CGT, and RST).
Declaration of conflict of interest: The authors declare no conflict of interest.
To cite this article: Talhouk R, Tarraf C, Kobrossy L, Shaito A, Bazzi S, Bazzoun D, El-Sabban M. Modulation of Cx43 and Gap Junctional Intercellular Communication by Androstenedione in Rat Polycystic Ovary and Granulosa Cells in vitro. J Reprod Infertil. 2012;13(1):21-32.
References
- 1.Stein IF, Leventhal ML. Amenorrhea associated with bilateral polycystic ovaries. Am J Obstet Gynecol. 1935;29:181–91. [Google Scholar]
- 2.Jones MR, Chua A, Chen YD, Li X, Krauss RM, Rotter JI, et al. Harnessing expression data to identify novel candidate genes in polycystic ovary syndrome. PLoS One. 2011;6(5):e20120. doi: 10.1371/journal.pone.0020120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pigny P, Merlen E, Robert Y, Cortet-Rudelli C, Decanter C, Jonard S, et al. Elevated serum level of anti-mullerian hormone in patients with polycystic ovary syndrome: relationship to the ovarian follicle excess and to the follicular arrest. J Clin Endocrinol Metab. 2003;88(12):5957–62. doi: 10.1210/jc.2003-030727. [DOI] [PubMed] [Google Scholar]
- 4.Dong J, Albertini DF, Nishimori K, Kumar TR, Lu N, Matzuk MM. Growth differentiation factor-9 is required during early ovarian folliculogenesis. Nature. 1996;383(6600):531–5. doi: 10.1038/383531a0. [DOI] [PubMed] [Google Scholar]
- 5.Matzuk MM. Revelations of ovarian follicle biology from gene knockout mice. Mol Cell Endocrinol. 2000;163(1-2):61–6. doi: 10.1016/s0303-7207(99)00241-5. [DOI] [PubMed] [Google Scholar]
- 6.Gougeon A, Busso D. Morphologic and functional determinants of primordial and primary follicles in the monkey ovary. Mol Cell Endocrinol. 2000;163(1-2):33–42. doi: 10.1016/s0303-7207(00)00220-3. [DOI] [PubMed] [Google Scholar]
- 7.McNatty KP, Fidler AE, Juengel JL, Quirke LD, Smith PR, Heath DA, et al. Growth and paracrine factors regulating follicular formation and cellular function. Mol Cell Endocrinol. 2000;163(1-2):11–20. doi: 10.1016/s0303-7207(99)00235-x. [DOI] [PubMed] [Google Scholar]
- 8.Samoto T, Maruo T, Matsuo H, Katayama K, Barnea ER, Mochizuki M. Altered expression of insulin and insulin-like growth factor-I receptors in follicular and stromal compartments of polycystic ovaries. Endocr J. 1993;40(4):413–24. doi: 10.1507/endocrj.40.413. [DOI] [PubMed] [Google Scholar]
- 9.Pierro E, Andreani CL, Lazzarin N, Cento R, Lanzone A, Caruso A, et al. Further evidence of increased aromatase activity in granulosa luteal cells from polycystic ovary. Hum Reprod. 1997;12(9):1890–6. doi: 10.1093/humrep/12.9.1890. [DOI] [PubMed] [Google Scholar]
- 10.Doldi N, Grossi D, Destefani A, Gessi A, Ferrari A. Polycystic ovary syndrome: evidence for reduced 3 beta-hydroxysteroid dehydrogenase gene expression in human luteinizing granulosa cells. Gynecol Endocrinol. 2000;14(1):32–7. doi: 10.3109/09513590009167657. [DOI] [PubMed] [Google Scholar]
- 11.Hirshfield AN. Development of follicles in the mammalian ovary. Int Rev Cytol. 1991;124:43–101. doi: 10.1016/s0074-7696(08)61524-7. [DOI] [PubMed] [Google Scholar]
- 12.Vlodavsky I, Lui GM, Gospodarowicz D. Morphological appearance, growth behavior and migratory activity of human tumor cells maintained on extracellular matrix versus plastic. Cell. 1980;19(3):607–16. doi: 10.1016/s0092-8674(80)80037-7. [DOI] [PubMed] [Google Scholar]
- 13.Ben-Rafael Z, Orvieto R. Cytokines--involvement in reproduction. Fertil Steril. 1992;58(6):1093–9. doi: 10.1016/s0015-0282(16)55548-4. [DOI] [PubMed] [Google Scholar]
- 14.Giudice LC, Chandrasekher YA, Cataldo NA. The potential roles of intraovarian peptides in normal and abnormal mechanisms of reproductive physiology. Curr Opin Obstet Gynecol. 1993;5(3):350–9. [PubMed] [Google Scholar]
- 15.Kol S, Adashi EY. Intraovarian factors regulating ovarian function. Curr Opin Obstet Gynecol. 1995;7(3):209–13. doi: 10.1097/00001703-199506000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Aten RF, Kolodecik TR, Behrman HR. A cell adhesion receptor antiserum abolishes, whereas laminin and fibronectin glycoprotein components of extracellular matrix promote, luteinization of cultured rat granulosa cells. Endocrinology. 1995;136(4):1753–8. doi: 10.1210/endo.136.4.7895687. [DOI] [PubMed] [Google Scholar]
- 17.Aharoni D, Meiri I, Atzmon R, Vlodavsky I, Amsterdam A. Differential effect of components of the extracellular matrix on differentiation and apoptosis. Curr Biol. 1997;7(1):43–51. doi: 10.1016/s0960-9822(06)00026-1. [DOI] [PubMed] [Google Scholar]
- 18.Amsterdam A, Rotmensch S, Furman A, Venter EA, Vlodavsky I. Synergistic effect of human chorionic gonadotropin and extracellular matrix on in vitro differentiation of human granulosa cells: progesterone production and gap junction formation. Endocrinology. 1989;124(4):1956–64. doi: 10.1210/endo-124-4-1956. [DOI] [PubMed] [Google Scholar]
- 19.Grazul-Bilska AT, Redmer DA, Reynolds LP. Cellular interactions in the corpus luteum. Semin Reprod Endocrinol. 1997;15(4):383–93. doi: 10.1055/s-2008-1068376. [DOI] [PubMed] [Google Scholar]
- 20.Munari-Silem Y, Lebrethon MC, Morand I, Rousset B, Saez JM. Gap junction-mediated cell-to-cell communication in bovine and human adrenal cells. A process whereby cells increase their responsiveness to physiological corticotropin concentrations. J Clin Invest. 1995;95(4):1429–39. doi: 10.1172/JCI117813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wiesen JF, Midgley AR., Jr Changes in expression of connexin 43 gap junction messenger ribonucleic acid and protein during ovarian follicular growth. Endocrinology. 1993;133(2):741–6. doi: 10.1210/endo.133.2.8393773. [DOI] [PubMed] [Google Scholar]
- 22.Gittens JE, Mhawi AA, Lidington D, Ouellette Y, Kidder GM. Functional analysis of gap junctions in ovarian granulosa cells: distinct role for connexin 43 in early stages of folliculogenesis. Am J Physiol Cell Physiol. 2003;284(4):C880–7. doi: 10.1152/ajpcell.00277.2002. [DOI] [PubMed] [Google Scholar]
- 23.Tong D, Gittens JE, Kidder GM, Bai D. Patchclamp study reveals that the importance of connexin43-mediated gap junctional communication for ovarian folliculogenesis is strain specific in the mouse. Am J Physiol Cell Physiol. 2006;290(1):C290–7. doi: 10.1152/ajpcell.00297.2005. [DOI] [PubMed] [Google Scholar]
- 24.Juneja SC, Barr KJ, Enders GC, Kidder GM. Defects in the germ line and gonads of mice lacking connexin43. Biol Reprod. 1999;60(5):1263–70. doi: 10.1095/biolreprod60.5.1263. [DOI] [PubMed] [Google Scholar]
- 25.Ackert CL, Gittens JE, O'Brien MJ, Eppig JJ, Kidder GM. Intercellular communication via connexin 43 gap junctions is required for ovarian folliculogenesis in the mouse. Dev Biol. 2001;233(2):258–70. doi: 10.1006/dbio.2001.0216. [DOI] [PubMed] [Google Scholar]
- 26.Gittens JE, Barr KJ, Vanderhyden BC, Kidder GM. Interplay between paracrine signaling and gap junctional communication in ovarian follicles. J Cell Sci. 2005;118(Pt 1):113–22. doi: 10.1242/jcs.01587. [DOI] [PubMed] [Google Scholar]
- 27.Gittens JE, Kidder GM. Differential contributions of connexin37 and connexin43 to oogenesis revealed in chimeric reaggregated mouse ovaries. J Cell Sci. 2005;118(Pt 21):5071–8. doi: 10.1242/jcs.02624. [DOI] [PubMed] [Google Scholar]
- 28.Grümmer R, Traub O, Winterhager E. Gap junction connexin genes cx26 and cx43 are differentially regulated by ovarian steroid hormones in rat endometrium. Endocrinology. 1999;140(6):2509–16. doi: 10.1210/endo.140.6.6640. [DOI] [PubMed] [Google Scholar]
- 29.Kilarski WM, Hongpaisan J, Semik D, Roomans GM. Effect of progesterone and oestradiol on expression of connexin43 in cultured human myometrium cells. Folia Histochem Cytobiol. 2000;38(1):3–9. [PubMed] [Google Scholar]
- 30.Habermann H, Chang WY, Birch L, Mehta P, Prins GS. Developmental exposure to estrogens alters epithelial cell adhesion and gap junction proteins in the adult rat prostate. Endocrinology. 2001;142(1):359–69. doi: 10.1210/endo.142.1.7893. [DOI] [PubMed] [Google Scholar]
- 31.Chang X, Patiño R, Yoshizaki G, Thomas P, Lee VH. Hormonal regulation and cellular distribution of connexin 32.2 and connexin 32.7 RNAs in the ovary of Atlantic croaker. Gen Comp Endocrinol. 2000;120(2):146–56. doi: 10.1006/gcen.2000.7549. [DOI] [PubMed] [Google Scholar]
- 32.Sasseville' M, Gagnon MC, Guillemette C, Sullivan R, Gilchrist RB, Richard FJ. Regulation of gap junctions in porcine cumulus-oocyte complexes: contributions of granulosa cell contact, gonadotropins, and lipid rafts. Mol Endocrinol. 2009;23(5):700–10. doi: 10.1210/me.2008-0320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boone DL, Tsang BK. Identification and localization of deoxyribonuclease I in the rat ovary. Biol Reprod. 1997;57(4):813–21. doi: 10.1095/biolreprod57.4.813. [DOI] [PubMed] [Google Scholar]
- 34.Anderson E, Little B, Lee GS. Androgen-induced changes in rat ovarian granulosa cells in vitro. Tissue Cell. 1987;19(2):217–34. doi: 10.1016/0040-8166(87)90007-3. [DOI] [PubMed] [Google Scholar]
- 35.Henmi H, Endo T, Nagasawa K, Hayashi T, Chida M, Akutagawa N, et al. Lysyl oxidase and MMP-2 expression in dehydroepiandrosterone-induced polycystic ovary in rats. Biol Reprod. 2001;64(1):157–62. doi: 10.1095/biolreprod64.1.157. [DOI] [PubMed] [Google Scholar]
- 36.Stener-Victorin E, Lundeberg T, Waldenström U, Manni L, Aloe L, Gunnarsson S, et al. Effects of electro-acupuncture on nerve growth factor and ovarian morphology in rats with experimentally induced polycystic ovaries. Biol Reprod. 2000;63(5):1497–503. doi: 10.1095/biolreprod63.5.1497. [DOI] [PubMed] [Google Scholar]
- 37.Lee MT, Anderson E, Lee GY. Changes in ovarian morphology and serum hormones in the rat after treatment with dehydroepiandrosterone. Anat Rec. 1991;231(2):185–92. doi: 10.1002/ar.1092310206. [DOI] [PubMed] [Google Scholar]
- 38.Mahesh VB, Mills TM, Bagnell CA, Conway BA. Animal models for study of polycystic ovaries and ovarian atresia. Adv Exp Med Biol. 1987;219:237–57. doi: 10.1007/978-1-4684-5395-9_12. [DOI] [PubMed] [Google Scholar]
- 39.Roy S, Mahesh VB, Greenblatt RB. Effect of dehydroepiandrosterone and delta4-androstenedione on the reproductive organs of female rats: production of cystic changes in the ovary. Nature. 1962;196:42–3. doi: 10.1038/196042a0. [DOI] [PubMed] [Google Scholar]
- 40.Streuli CH, Edwards GM, Delcommenne M, Whitelaw CB, Burdon TG, Schindler C, et al. Stat5 as a target for regulation by extracellular matrix. J Biol Chem. 1995;270(37):21639–44. doi: 10.1074/jbc.270.37.21639. [DOI] [PubMed] [Google Scholar]
- 41.El-Sabban ME, Sfeir AJ, Daher MH, Kalaany NY, Bassam RA, Talhouk RS. ECM-induced gap junctional communication enhances mammary epithelial cell differentiation. J Cell Sci. 2003;116(Pt 17):3531–41. doi: 10.1242/jcs.00656. [DOI] [PubMed] [Google Scholar]
- 42.el-Fouly MH, Trosko JE, Chang CC. Scrape-loading and dye transfer. A rapid and simple technique to study gap junctional intercellular communication. Exp Cell Res. 1987;168(2):422–30. doi: 10.1016/0014-4827(87)90014-0. [DOI] [PubMed] [Google Scholar]
- 43.Rana B, Mischoulon D, Xie Y, Bucher NL, Farmer SR. Cell-extracellular matrix interactions can regulate the switch between growth and differentiation in rat hepatocytes: reciprocal expression of C/EBP alpha and immediate-early growth response transcription factors. Mol Cell Biol. 1994;14(9):5858–69. doi: 10.1128/mcb.14.9.5858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rosenkranz HS, Pollack N, Cunningham AR. Exploring the relationship between the inhibition of gap junctional intercellular communication and other biological phenomena. Carcinogenesis. 2000;21(5):1007–11. doi: 10.1093/carcin/21.5.1007. [DOI] [PubMed] [Google Scholar]
- 45.Moorby CD. A connexin 43 mutant lacking the carboxyl cytoplasmic domain inhibits both growth and motility of mouse 3T3 fibroblasts. Mol Carcinog. 2000;28(1):23–30. [PubMed] [Google Scholar]
- 46.Kidder GM, Mhawi AA. Gap junctions and ovarian folliculogenesis. Reproduction. 2002;123(5):613–20. doi: 10.1530/rep.0.1230613. [DOI] [PubMed] [Google Scholar]
- 47.Simon AM, Goodenough DA, Li E, Paul DL. Female infertility in mice lacking connexin 37. Nature. 1997;385(6616):525–9. doi: 10.1038/385525a0. [DOI] [PubMed] [Google Scholar]
- 48.Yen SS. The polycystic ovary syndrome. Clin Endocrinol (Oxf) 1980;12(2):177–207. doi: 10.1111/j.1365-2265.1980.tb02132.x. [DOI] [PubMed] [Google Scholar]
- 49.Anderson E, Lee MT, Lee GY. Cystogenesis of the ovarian antral follicle of the rat: ultrastructural changes and hormonal profile following the administration of dehydroepiandrosterone. Anat Rec. 1992;234(3):359–82. doi: 10.1002/ar.1092340307. [DOI] [PubMed] [Google Scholar]
- 50.Dunaif A. Adrenal disorders and polycystic ovary syndrome. Horm Res. 1992;37(Suppl 3):39–44. doi: 10.1159/000182399. [DOI] [PubMed] [Google Scholar]
- 51.Beyer EC, Kistler J, Paul DL, Goodenough DA. Antisera directed against connexin43 peptides react with a 43-kD protein localized to gap junctions in myocardium and other tissues. J Cell Biol. 1989;108(2):595–605. doi: 10.1083/jcb.108.2.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Goodenough DA, Simon AM, Paul DL. Gap junctional intercellular communication in the mouse ovarian follicle. Novartis Found Symp. 1999;219:226–35. doi: 10.1002/9780470515587.ch14. discussion 235–40. [DOI] [PubMed] [Google Scholar]
- 53.Huet C, Monget P, Pisselet C, Hennequet C, Locatelli A, Monniaux D. Chronology of events accompanying follicular atresia in hypophysectomized ewes. Changes in levels of steroidogenic enzymes, connexin 43, insulin-like growth factor II/mannose 6 phosphate receptor, extracellular matrix components, and matrix metalloproteinases. Biol Reprod. 1998;58(1):175–85. doi: 10.1095/biolreprod58.1.175. [DOI] [PubMed] [Google Scholar]
- 54.Grazul-Bilska AT, Redmer DA, Johnson ML, Jablonka-Shariff A, Bilski JJ, Reynolds LP. Gap junctional protein connexin 43 in bovine corpora lutea throughout the estrous cycle. Biol Reprod. 1996;54(6):1279–87. doi: 10.1095/biolreprod54.6.1279. [DOI] [PubMed] [Google Scholar]
- 55.Itahana K, Morikazu Y, Takeya T. Differential expression of four connexin genes, Cx-26, Cx-30.3, Cx-32, and Cx-43, in the porcine ovarian follicle. Endocrinology. 1996;137(11):5036–44. doi: 10.1210/endo.137.11.8895378. [DOI] [PubMed] [Google Scholar]
- 56.Lenhart JA, Downey BR, Bagnell CA. Connexin 43 gap junction protein expression during follicular development in the porcine ovary. Biol Reprod. 1998;58(2):583–90. doi: 10.1095/biolreprod58.2.583. [DOI] [PubMed] [Google Scholar]
- 57.Schreiber JR, Beckmann MW, Polacek D, Davies PF. Changes in gap junction connexin-43 messenger ribonucleic acid levels associated with rat ovarian follicular development as demonstrated by in situ hybridization. Am J Obstet Gynecol. 1993;168(4):1094–102. doi: 10.1016/0002-9378(93)90352-j. discussion 1102–4. [DOI] [PubMed] [Google Scholar]
- 58.Mayerhofer A, Garfield RE. Immunocytochemical analysis of the expression of gap junction protein connexin 43 in the rat ovary. Mol Reprod Dev. 1995;41(3):331–8. doi: 10.1002/mrd.1080410308. [DOI] [PubMed] [Google Scholar]
- 59.Safieh-Garabedian B, Mouneimne GM, El-Jouni W, Khattar M, Talhouk R. The effect of endotoxin on functional parameters of mammary CID-9 cells. Reproduction. 2004;127(3):397–406. doi: 10.1530/rep.1.00135. [DOI] [PubMed] [Google Scholar]
- 60.Mahesh VB, Greenblatt RB. Isolation of dehydro-epiandrosterone and 17alphahydroxy-delta5-pregenolone from the polycystic ovaries of the Stein-Leventhal syndrome. J Clin Endocrinol Metab. 1962;22:441–8. doi: 10.1210/jcem-22-4-441. [DOI] [PubMed] [Google Scholar]
- 61.Anderson E, Selig M, Lee G, Little B. Androgen-induced changes in ovarian granulosa cells from immature rats in vitro. Adv Exp Med Biol. 1987;219:259–74. doi: 10.1007/978-1-4684-5395-9_13. [DOI] [PubMed] [Google Scholar]
- 62.Yildiz BO, Azziz R. The adrenal and polycystic ovary syndrome. Rev Endocr Metab Disord. 2007;8(4):331–42. doi: 10.1007/s11154-007-9054-0. [DOI] [PubMed] [Google Scholar]
- 63.Ehrmann DA, Barnes RB, Rosenfield RL. Polycystic ovary syndrome as a form of functional ovarian hyperandrogenism due to dysregulation of androgen secretion. Endocr Rev. 1995;16(3):322–53. doi: 10.1210/edrv-16-3-322. [DOI] [PubMed] [Google Scholar]
- 64.Rosenfield RL, Barnes RB, Cara JF, Lucky AW. Dysregulation of cytochrome P450c 17 alpha as the cause of polycystic ovarian syndrome. Fertil Steril. 1990;53(5):785–91. [PubMed] [Google Scholar]
- 65.Rosenfeld CS, Wagner JS, Roberts RM, Lubahn DB. Intraovarian actions of oestrogen. Reproduction. 2001;122(2):215–26. doi: 10.1530/rep.0.1220215. [DOI] [PubMed] [Google Scholar]
- 66.Yu W, Dahl G, Werner R. The connexin43 gene is responsive to oestrogen. Proc Biol Sci. 1994;255(1343):125–32. doi: 10.1098/rspb.1994.0018. [DOI] [PubMed] [Google Scholar]
- 67.Hillier SG. Intrafollicular paracrine function of ovarian androgen. J Steroid Biochem. 1987;27(1-3):351–7. doi: 10.1016/0022-4731(87)90327-x. [DOI] [PubMed] [Google Scholar]
- 68.Kanemitsu MY, Lau AF. Epidermal growth factor stimulates the disruption of gap junctional communication and connexin43 phosphorylation independent of 12-0-tetradecanoylphorbol 13-acetatesensitive protein kinase C: the possible involvement of mitogen-activated protein kinase. Mol Biol Cell. 1993;4(8):837–48. doi: 10.1091/mbc.4.8.837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wood KW, Sarnecki C, Roberts TM, Blenis J. Ras mediates nerve growth factor receptor modulation of three signal-transducing protein kinases: MAP kinase, Raf-1, and RSK. Cell. 1992;68(6):1041–50. doi: 10.1016/0092-8674(92)90076-o. [DOI] [PubMed] [Google Scholar]
- 70.Kim DY, Kam Y, Koo SK, Joe CO. Gating connexin 43 channels reconstituted in lipid vesicles by mitogen-activated protein kinase phosphorylation. J Biol Chem. 1999;274(9):5581–7. doi: 10.1074/jbc.274.9.5581. [DOI] [PubMed] [Google Scholar]
- 71.El-Sabban ME, Abi-Mosleh LF, Talhouk RS. Developmental regulation of gap junctions and their role in mammary epithelial cell differentiation. J Mammary Gland Biol Neoplasia. 2003;8(4):463–73. doi: 10.1023/B:JOMG.0000017432.04930.76. [DOI] [PubMed] [Google Scholar]
- 72.Godwin AJ, Green LM, Walsh MP, McDonald JR, Walsh DA, Fletcher WH. In situ regulation of cell-cell communication by the cAMP-dependent protein kinase and protein kinase C. Mol Cell Biochem. 1993;127-128:293–307. doi: 10.1007/BF01076779. [DOI] [PubMed] [Google Scholar]
- 73.Yogo K, Ogawa T, Akiyama M, Ishida-Kitagawa N, Sasada H, Sato E, et al. PKA implicated in the phosphorylation of Cx43 induced by stimulation with FSH in rat granulosa cells. J Reprod Dev. 2006;52(3):321–8. doi: 10.1262/jrd.17107. [DOI] [PubMed] [Google Scholar]
- 74.Cooper CD, Lampe PD. Casein kinase 1 regulates connexin-43 gap junction assembly. J Biol Chem. 2002;277(47):44962–8. doi: 10.1074/jbc.M209427200. [DOI] [PubMed] [Google Scholar]
- 75.Hsueh AJ, Adashi EY, Jones PB, Welsh TH., Jr Hormonal regulation of the differentiation of cultured ovarian granulosa cells. Endocr Rev. 1984;5(1):76–127. doi: 10.1210/edrv-5-1-76. [DOI] [PubMed] [Google Scholar]
- 76.Furman A, Rotmensch S, Kohen F, Mashiach S, Amsterdam A. Regulation of rat granulosa cell differentiation by extracellular matrix produced by bovine corneal endothelial cells. Endocrinology. 1986;118(5):1878–85. doi: 10.1210/endo-118-5-1878. [DOI] [PubMed] [Google Scholar]
- 77.Furger C, Cronier L, Poirot C, Pouchelet M. Human granulosa cells in culture exhibit functional cyclic AMP-regulated gap junctions. Mol Hum Reprod. 1996;2(8):541–8. doi: 10.1093/molehr/2.8.541. [DOI] [PubMed] [Google Scholar]
- 78.Romanello M, Moro L, Pirulli D, Crovella S, D'Andrea P. Effects of cAMP on intercellular coupling and osteoblast differentiation. Biochem Biophys Res Commun. 2001;282(5):1138–44. doi: 10.1006/bbrc.2001.4710. [DOI] [PubMed] [Google Scholar]
- 79.Martin W, Zempel G, Hülser D, Willecke K. Growth inhibition of oncogene-transformed rat fibroblasts by cocultured normal cells: relevance of metabolic cooperation mediated by gap junctions. Cancer Res. 1991;51(19):5348–51. [PubMed] [Google Scholar]
- 80.Munari-Silem Y, Rousset B. Gap junction-mediated cell-to-cell communication in endocrine glands--molecular and functional aspects: a review. Eur J Endocrinol. 1996;135(3):251–64. doi: 10.1530/eje.0.1350251. [DOI] [PubMed] [Google Scholar]
- 81.D'Andrea P, Paschini V, Vittur F. Dual mechanism for cAMP-dependent modulation of Ca2+ signalling in articular chondrocytes. Biochem J. 1996;318(Pt 2):569–73. doi: 10.1042/bj3180569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Okuma A, Kuraoka A, Iida H, Inai T, Wasano K, Shibata Y. Colocalization of connexin 43 and connexin 45 but absence of connexin 40 in granulosa cell gap junctions of rat ovary. J Reprod Fertil. 1996;107(2):255–64. doi: 10.1530/jrf.0.1070255. [DOI] [PubMed] [Google Scholar]