Abstract
Background: Alcohol-exposed pregnancy (AEP) is a leading cause of birth defects. Effective face-to-face preconception interventions based on motivational interviewing (MI) exist and should be translated into remote formats for maximum public health impact. This study investigated the feasibility and promise of a one-session, remote-delivered, preconception, MI-based AEP intervention (EARLY Remote) for non–treatment-seeking community women. Subjects and Methods: This was a single-arm, prospective pilot intervention study. All participants received the intervention via telephone and mail. Feasibility of remote-delivery methods, treatment engagement, treatment credibility, MI treatment integrity, and therapeutic alliance were examined. Outcomes were 3- and 6-month drinks per drinking day (DDD), rate of unreliable contraception, and proportion of women at risk for AEP due to continued risk drinking and no or unreliable contraception use. Results: Feasibility of remote delivery was established; participants were engaged by the intervention and rated it as credible. Integrity to MI and therapeutic alliance were good. Both DDD and rate of unreliable contraception decreased significantly over time. Proportions of women who drank at risk levels, used unreliable or no contraception, and/or were at risk for AEP in the past 90 days decreased significantly from baseline to 6 months. Conclusions: Remote delivery was feasible, and the translated remote intervention may reduce AEP risk. Refinement of EARLY Remote may facilitate its placement within a spectrum of effective MI-based preconception AEP interventions as part of a stepped-care approach. EARLY Remote may have an important role within a stepped-care model for dissemination to geographically disperse women at risk for AEP. This could result in substantial public health impact through reduction of AEP on a larger scale.
Key words: e-health, telehealth, telemedicine, telepsychiatry
Introduction
Fetal alcohol exposure can result in neurological and behavioral problems known as fetal alcohol spectrum disorders.1 Between 9% and 20% of sexually active women of childbearing age drink alcohol and use no or unreliable contraception. These dual risk behaviors place them at risk for alcohol-exposed pregnancy (AEP).2–5 Although most women cease drinking when they find out they are pregnant, over half of pregnancies are unplanned and unrecognized for 4–6 weeks following conception, when key neurological developments occur.2,3
Preconception interventions to change one or more risk behaviors contributing to AEP risk are needed. Two such interventions have been developed and found efficacious in randomized controlled trials (RCTs): a four-session intervention for community women (CHOICES6) and a two-session intervention for university women (BALANCE7). Both CHOICES and BALANCE provide contraception and are delivered in face-to-face format. Additionally, a one-session intervention for community women, also delivered in a face-to-face format but without contraception provided, called EARLY, was developed. An RCT found significant risk improvement associated with passage of time but no significant differences between groups.8
These three interventions use a counseling style called motivational interviewing (MI), a directive, patient-centered approach grounded in compassion, acceptance, partnership, and evocation.9 In MI, counselors utilize reflective listening, open questioning, and exploring and resolving ambivalence surrounding specific behavior changes. For AEP intervention, the dual targets are contraception and drinking.9 Using the MI counseling style, counselors deliver personalized feedback about risk for AEP and facilitate exploration of risks, resolution of ambivalence, goal setting, and behavioral change planning through a menu of MI activities.10
While the EARLY RCT was underway, investigators translated EARLY from face-to-face delivery format to a telemedicine format or remote-delivery format via telephone and mail. Investigators named the translated intervention EARLY Remote. A remote-delivered intervention could increase reach and convenience for geographically dispersed community women. Remote formats may even be preferred by women who are reluctant to discuss drinking and sexual behaviors face-to-face. Studies have found remote-delivered MI interventions incorporating personalized feedback and telephone counseling have yielded health behavior change, yet no such AEP interventions have been developed to date.11,12 To this end, we explored feasibility and preliminary promise of EARLY Remote, by conducting a single-arm, prospective pilot intervention study.
Subjects and Methods
Study Design
This single-arm, prospective pilot intervention study investigated feasibility and promise of EARLY Remote. Non–treatment-seeking community women at risk for AEP were recruited, screened, consented, assessed at baseline, provided the EARLY Remote intervention (hereafter referred to as “intervention”), and followed up at 3 and 6 months after baseline (3M and 6M, respectively). Feasibility of remote recruitment and data collection as well as treatment engagement, treatment credibility, MI treatment integrity, and therapeutic alliance were examined. To explore the promise of the intervention to reduce AEP risk, outcomes (i.e., drinks per drinking day [DDD], rate of unreliable contraception, and proportion of women at risk for AEP) were assessed at baseline, 3M, and 6M and then compared.
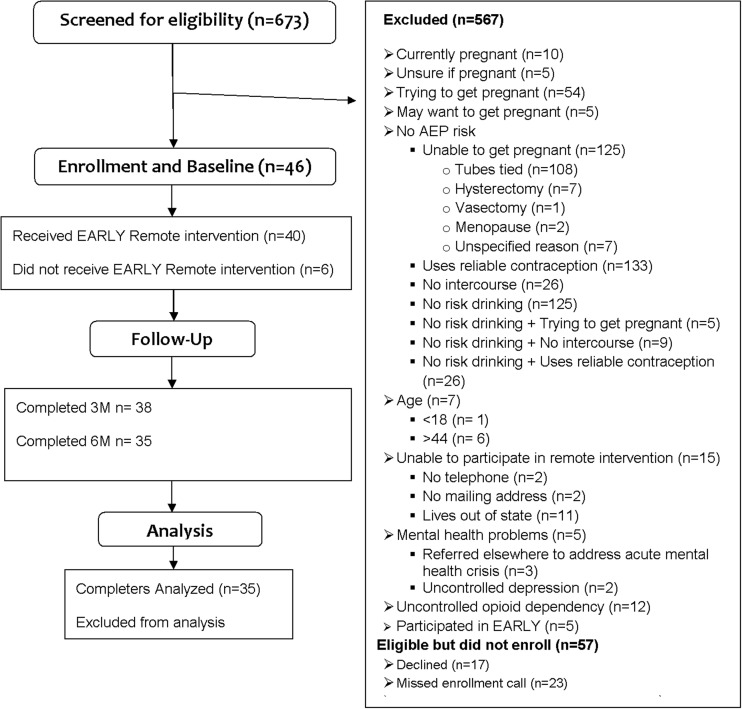
This study was approved by the University of Virginia Institutional Review Board on December 15, 2009. All contact with participants was remote via mail and telephone. Data were collected from 2009 to 2011, and analyses were conducted in 2011–2012. The study flow is shown in Figure 1.
Fig. 1.
Study flow diagram. 3M, 3-month follow-up; 6M, 6-month follow-up; AEP, alcohol-exposed pregnancy.
Procedures
Remote recruitment, screening, and enrollment
The study was advertised on Craigslist in three Virginia population centers, seeking “women between the ages of 18 and 44 years who drink and who also have sex for a research study.” Potential participants telephoned the center and researchers used a 5-min structured screening interview to assess inclusion and exclusion criteria as described below.
Women who spoke and read English, were sexually active (at least one instance of sexual intercourse with a man in the last 90 days), fertile (18–44 years old, with no known infertility), and at risk for AEP were included in this study. Risk for AEP was (1) current risk drinking (i.e., more than 7 standard drinks per week on average and/or more than 3 standard drinks on at least one occasion in the past 90 days13) and (2) no or unreliable contraception (i.e., nonexistent, inconsistent, or unreliable methods of contraception paired with vaginal intercourse during the past 90 days). Examples of inconsistent contraception methods included missing two birth control pills in 1 month without using an effective back-up method (e.g., condom) or not using a condom during all or part of any vaginal sexual encounter for condom users. Unreliable contraception methods included any that have been found to result in 20 or more new pregnancies in a year per 100 women (e.g., withdrawal, rhythm, use of spermicides alone, etc.).14 Other eligibility requirements included planning to remain in the area for the follow-up period and having a current mailing address, telephone, and DVD player through which to participate in data collection and intervention. Exclusion criteria were (1) current pregnancy or hopes for pregnancy in the follow-up period, (2) severe cognitive disorders that could impair ability to provide informed consent or understand the intervention, (3) current untreated major depression that could diminish reponse to the intervention, (4) active suicidality, (5) current untreated opioid dependence, and (6) current participation in another intervention study targeting drinking or contraception use.
After screening, researchers scheduled an enrollment call for eligible and interested women and mailed them a copy of the informed consent form. The University of Virginia Institutional Review Board waived written consent and allowed provision of verbal consent.
Remote assessment
Baseline, 3M, and 6M assessments were performed during scheduled 60-min calls. Prior to calls, participants were mailed questionnaires and visual aids (e.g., a chart displaying standard drinks). Participants received up to $180 for time spent completing assessments, prorated by time point completed.
Measures
Demographic and baseline characteristics
A structured interview from the EARLY study was adapted and used to obtain information on demographic and risk characteristics during the baseline assessment. Demographic characteristics included age, race, ethnicity, education, marital status, living situation, and employment. Risk characteristics included sexual health and contraception use and current drinking behavior. Alcohol abuse and dependence at baseline was assessed with the M.I.N.I. International Neuropsychiatric Interview Module J.15,16
AEP risk
Drinking and contraception use were measured during baseline, 3M, and 6M assessment calls using the Time Line Follow-Back (TLFB). The TLFB is a guided method that uses a calendar to prompt accurate recollection of daily behavior. The instrument has excellent validity and reliability among substance users for in-person and telephone data collection17,18 and has been used in previous AEP intervention studies.6–8,10
Treatment engagement
Engagement with the intervention was assessed. During the intervention call, counselors asked participants if and when they watched the DVD, read personalized feedback, and completed the mailed MI activity worksheets (i.e., before, during, and or after the intervention).
Treatment credibility
Participants completed a four-item Treatment Credibility Form after the intervention call and mailed completed forms to researchers (adapted from Dennis Turk, 2000, pers. commun.). This form assessed participants' ratings of intervention clarity, how successful they believed the intervention would be in helping them use contraception effectively and reduce risk drinking, and how confident they would be in recommending the intervention to a friend at risk for AEP. Scores on each item ranged from 1 to 10, with higher scores indicating higher credibility (Dennis Turk, 2000, pers. commun.).
Therapeutic alliance
Participants and counselors completed parallel forms of the Helping Alliance Questionnaire (HAQ-II) after the intervention call. The HAQ-II is a 19-item measure of counselor and patient alliance that correlates well with treatment response.19 Participants mailed completed forms to researchers. Respondents provided ratings, on a scale of 1–5 (from 1=strongly disagree to 5=strongly agree), to statements such as “The patient believes I am experienced in helping people” or “The counselor and I have meaningful exchanges.” Scores on the HAQ-II range from 19 to 114, with higher scores indicating more positive alliance.
Treatment integrity
All intervention calls were audio recorded to enable assessment of integrity to MI. The principal investigator randomly selected 25% of sessions (n=10) for coding. Following the Motivational Interviewing Treatment Integrity instrument version 3.1. instructions, a trained coder randomly selected one 20-min segment of each session and coded. 20 The coder scored five global variables (i.e., empathy, evocation, collaboration, autonomy/support, and direction) and counted frequency of verbal behaviors (i.e., giving information, asking open and closed-ended questions, providing simple and complex reflections, and making other statements categorized as MI adherent or not). A judgment about a session's MI fidelity can be made through comparison with recommended standards for global scores and ratios that are based upon expert opinion.20
EARLY Remote intervention
The intervention was conducted during one 60-min telephone call and consisted of the EARLY intervention8 translated into a mail and telephone-administered format. Specific intervention components are shown in Table 1. Counselors have doctoral degrees in clinical psychology and extensive training in MI. Prior to the intervention, researchers prepared and mailed a package including personalized feedback, using the information gathered in the baseline assessment, with other materials needed to conduct the intervention (i.e., agenda, DVD about fetal alcohol spectrum disorders and AEP risk, educational brochures, and MI activity worksheets) and post-intervention measures. Participants were instructed to access the package and a DVD player and be in a quiet and private place during the intervention call.
Table 1.
EARLY Remote Intervention Components
| Therapists used a collaborative, evocative style to acknowledge autonomy and provide support while completing the following: |
| • Build rapport and induce role |
| • Provide overview of EARLY Remote intervention |
| • Discuss reactions to baseline assessment |
| • Elicit views of drinking and contraception use |
| • Provide personalized feedback, including |
| ∘ Comparison of drinking level with national average |
| ∘ Average and peak alcohol consumption |
| ∘ Financial costs associated with drinking |
| ∘ Specific reasons for pregnancy risk coupled with information about effective contraception methods |
| • Introduce and ask participant to view videotape26 |
| • Elicit participant's response to video |
| • If relevant, discuss her other drug use and/or other mental health issues in relation to AEP prevention |
| • Select and perform one MI activity: |
| ∘ Use a Decisional Balance activity to explore ambivalence about change |
| ∘ Use a Importance, Confidence, and Readiness Ruler activity to explore motivation to change and to elicit thoughts on next steps |
| ∘ Use the Temptation and Confidence activity to elicit and explore the participant's thoughts about situational temptation to engage in risk behavior and confidence not to |
| ∘ Use a Change Plan activity to create a goal statement and plans to achieve goal(s) |
| • Encourage a contraception visit by encouraging the participant to schedule an appointment with her reproductive health practitioner to explore contraception options. Refer participants without practitioners to the list of community resources provided. If relevant, refer participant to brochure with information about contraception. |
| • Summarize intervention |
AEP, alcohol-exposed pregnancy; MI, motivational interviewing.
Data Analysis
We used descriptive statistics, t tests, and chi-squared tests to characterize sample demographics, characteristics, contraceptive behaviors, drinking behaviors, AEP risk, and feasibility variables. We investigated the promise of the intervention by evaluating change in outcome variables. Outcome variables were DDD, unreliable contraception rate (percentage of days with one or more episodes of unprotected intercourse), and the presence or absence of risk for AEP in the past 90 days at 3M and 6M derived from the TLFB. Reduced risk for AEP was defined as (1) no longer at risk for pregnancy because of perfectly reliable contraception or sexual abstinence and/or (2) no risk drinking. Secondary outcome variables included the proportion of participants engaging in risk drinking (>3 drinks per occasion and/or >7 per week) and unprotected intercourse in the 90-day time frame preceding 3M and 6M. For the categorical outcomes of risk for AEP, unreliable contraception, and risk drinking at 3M and 6M, chi-squared tests were applied to determine if there was a difference between baseline and follow-up points. Paired t tests compared the continuous outcomes of DDD and unreliable contraception rate from baseline to each follow-up point. For each outcome variable, within-group unbiased estimators of effect size (d) and 95% confidence intervals were computed comparing each follow-up point to baseline values.21 For continuous outcome variables, pre–post mean and standard deviation (SD) values and the pre–post correlation were used. For categorical outcome variables, proportions and sample sizes were used.22
Results
Demographic and Baseline Characteristics
Demographic characteristics of the sample are shown in Table 2 for the sample at baseline (n=46), 3M (n=38), and 6M (n=35); these characteristics were similar to those observed in EARLY.8 On average, at baseline, participants were 27 years old (SD=5.5 years); most were African American (67.4%), employed (43.5 %), and living with a spouse or male partner (52.2%). Most participants (71.8%) used mobile rather than landline telephones during calls. Select AEP risk characteristics at baseline are presented in Table 3. All participants were at risk for AEP, reported unreliable contraception, and drank at risk levels at baseline. There were no significant differences in characteristics between the baseline and follow-up samples.
Table 2.
Demographic Characteristics of the Sample and Comparison of 3-Month and 6-Month Completers with Noncompleters
| |
SAMPLE |
||
|---|---|---|---|
| CHARACTERISTIC | BASELINE (N=46) | 3M COMPLETERS (N=38) | 6M COMPLETERS (N=35) |
| Age (years) [mean (SD)] | 27.1 (5.5) | 26.8 (5.7) | 27.3 (5.6) |
| Education (years) [mean (SD)] | 12.4 (4.3) | 12 (4.7) | 11.9 (4.9) |
| Race [n (%)] | |||
| African American | 31 (67.4) | 26 (70.3) | 24 (70.6) |
| White | 12 (26.1) | 9 (24.3) | 9 (26.5) |
| Native American | 2 (4.4) | 1 (2.7) | 1 (2.9) |
| Other | 1 (2.2) | 1 (2.7) | 0 |
| Marital status [n (%)] | |||
| Single | 18 (39.1) | 15 (40.5) | 15 (44.1) |
| Living together | 18 (39.1) | 14 (37.8) | 11 (32.4) |
| Married | 4 (8.7) | 4 (10.8) | 4 (11.8) |
| Separated | 4 (8.7) | 3 (8.1) | 3 (8.8) |
| Divorced | 2 (4.4) | 1 (2.7) | 1 (2.9) |
| Employment [n (%)] | |||
| Unemployed | 14 (30.4) | 11 (29.7) | 10 (29.4) |
| Full-time | 13 (28.3) | 11 (29.7) | 9 (26.5) |
| Part-time | 7 (15.2) | 6 (16.2) | 6 (17.7) |
| Self-employed | 3 (6.5) | 1 (2.7) | 1 (2.9) |
| Full-time student | 6 (13.0) | 5 (13.5) | 5 (14.7) |
| Part-time student | 3 (6.5) | 3 (8.1) | 4 (8.8) |
| Living with [n (%)] | |||
| Male | 24 (52.2) | 18 (48.7) | 15 (44.1) |
| Partner/spouse | 10 (21.7) | 8 (21.6) | 8 (23.5) |
| Parent | 5 (10.9) | 5 (13.5) | 5 (14.7) |
| Roommate | 3 (6.5) | 3 (8.1) | 3 (8.8) |
| Children | 2 (4.4) | 1 (2.7) | 1 (2.9) |
| No one | 1 (2.2) | 1 (2.7) | 1 (2.9) |
| Relatives | 1 (2.2) | 1 (2.7) | 1 (2.9) |
| Female partner | 0 | 0 | 0 |
t tests and chi-squared tests revealed no differences in any variables between those completing versus those not completing each follow-up and the baseline sample (data not shown).
SD, standard deviation.
Table 3.
Alcohol-Exposed Pregnancy Risk Characteristics at Baseline (n=46)
| |
SAMPLE |
|
|---|---|---|
| CHARACTERISTIC | N | % |
| Reproductive health | ||
| Lifetime unplanned pregnancies | ||
| 0 | 16 | 34.8 |
| 1 | 13 | 28.3 |
| 2 | 5 | 10.9 |
| 3 or more | 12 | 26.1 |
| Lifetime miscarriages | ||
| 0 | 35 | 76.1 |
| 1 | 7 | 15.2 |
| 2 or more | 4 | 8.7 |
| Lifetime abortions | ||
| 0 | 28 | 60.9 |
| 1 | 12 | 26.1 |
| 2 or more | 6 | 13.0 |
| Lifetime births | ||
| 0 | 24 | 52.2 |
| 1 | 7 | 15.2 |
| 2 or more | 15 | 32.6 |
| Primary method of contraception | ||
| Condoms | 20 | 44.4 |
| Withdrawal | 15 | 33.3 |
| Not using any contraceptive method | 8 | 11.1 |
| Birth control pills | 2 | 4.4 |
| Last Pap smear | ||
| Within last year | 32 | 71.1 |
| Within 2 years | 7 | 15.6 |
| More than 2 years ago | 6 | 13.3 |
| Drinking severity | ||
| DSM-IV alcohol disorders by M.I.N.I. | ||
| Abuse | 6 | 13.3 |
| Dependence | 27 | 60 |
| Neither | 12 | 26.7 |
The n values reflect the number of participants who provided responses to the variable.
DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, 4th edition; M.I.N.I., M.I.N.I. International Neuropsychiatric Interview Module J.
Feasibility
Remote recruitment, screening, enrollment, and retention
Figure 1 shows that 673 individuals were screened, resulting in 106 potentially eligible women, which is a 15.8% gross eligibility rate. The accrual rate was approximately 5 new enrolled participants per month, with approximately 74 screened per month. Of those enrolled, 82.6% and 76% completed 3M and 6M follow-ups, respectively.
Treatment engagement
A high level of treatment engagement was observed. Counselors reviewed personalized feedback during the intervention with all participants. All participants completed at least one MI activity worksheet. Ten participants stated plans to complete additional MI activity worksheets after the call. Thirty-four participants viewed the DVD before or during the call. Three did not have access to a DVD player during the call but stated plans to view it after the call.
Treatment credibility
Post-intervention treatment credibility scores were available for 39 of 40 participants, who rated the intervention favorably as follows: with a mean score of 9.6 (SD=0.7) out of 10 that the intervention made sense, with a mean score of 8.6 (SD=1.7) out of 10 that the intervention was likely to help them improve contraception effectiveness, with a mean score of 9.3 (SD=1.1) out of 10 that they would recommend the intervention to a friend, and with a mean score of 8.3 (SD=2.1) out of 10 that the intervention was likely to help them to reduce risk drinking. These scores indicate that participants found the treatment to be very credible (Dennis Turk, 2000, pers. commun.).
Therapeutic alliance
The HAQ-II had excellent internal consistency in this sample, with a standardized Cronbach's alpha of 0.87 for participants (n=39) and 0.89 for counselors (n=40). Participants' mean helping alliance total score was 94.6 (SD=8.8) with a minimum of 74 and maximum of 111. Counselors' mean helping alliance total score was 88.7 (SD=6.1) with a minimum of 74 and a maximum of 104. Scores indicated development of strong therapeutic alliance.19
Treatment integrity
Mean global scores were calculated: empathy, mean of 4.9 (SD=0.32); evocation, mean of 4.6 (SD=0.52); collaboration, mean of 4.9 (SD=0.32); autonomy/support, mean of 4.7 (SD=0.48); and direction, mean of 5 (SD=0). The mean percentage of reflections to questions ratio was 100% (SD=0.19%). The mean percentage of open questions to all open- and close-ended questions combined was 60% (SD=0.11%). The mean percentage of complex reflections to all simple and complex reflections combined was 51% (SD=0.07%). The mean percentage of MI-adherent out of MI-adherent and not MI-adherent combined was 96% (SD=0.07%). All scores were above recommended standards for proficiency and therefore demonstrate adequate MI treatment integrity.20
Early Remote Intervention Promise
Table 4 shows the primary and secondary AEP risk variables across time points including within-group effect sizes for changes from baseline to follow-up. DDD decreased from 5.3 (SD=4.4) at baseline to 4.6 (SD=3.3) at 3M (paired t=1.26, not significant) and 4.1 (SD=2.2) at 6M (paired t=0.2.35; p<0.05). The unreliable contraception rate on days decreased significantly from 83.7% (SD=23.5%) at baseline to 64.5% (SD=42.0%) at 3M (paired t=21.36; p<0.01). This improvement was maintained at 6M, when the unreliable contraception rate was 65.3% (SD=43.0%), significantly less than baseline (paired t=19.7, p<0.01). AEP risk declined significantly from 100% at baseline to 68.5% at 3M (χ2 with 1 degree of freedom=15.8, p<0.01) and remained significantly lower at 6M with 68.8% at risk for AEP (χ2 with 1 degree of freedom=14.57, p<0.01). The proportion of participants who engaged in risk drinking declined significantly from 100% at baseline to 85.7% at 3M (χ2 with 1 degree of freedom=6.53, p<0.01) and remained significantly lower at 6M (87.5%); χ2 with 1 degree of freedom=6.58, p<0.01). The proportion of women continuing to use unreliable contraception or no contraception decreased from 100% at baseline to 80.0% at 3M (χ2 with 1 degree of freedom=9.66, p<0.01) and 75.0% at 6M (χ2 with 1 degree of freedom=12.3, p<0.01).
Table 4.
Alcohol-Exposed Pregnancy Risk Variables over Time
| |
BASELINE |
3-MONTH FOLLOW-UP |
6-MONTH FOLLOW-UP |
|||||
|---|---|---|---|---|---|---|---|---|
| PRIMARY AND SECONDARY OUTCOMES | MEAN | SD | MEAN | SD | EFFECT SIZE (95% CI)a | MEAN | SD | EFFECT SIZE (95% CI)a |
| Drinks per drinking day | 5.3 (n=44) | 4.3 | 4.6 (n=35) | 3.3 | d=0.018 (–0.13, 0.49) | 4.1 (n=30) | 2.2 | d=0.32 (−0.04, 0.68) |
| Unreliable contraception rate | 84.5% (n=44) | 23.2% | 63.7% (n=35) | 42.6% | d=0.60 (0.12, 1.08) | 64.3% (n=32) | 43.7% | d=0.57 (0.07, 1.07) |
| N | % | N | % | EFFECT SIZE (95% CI)a | N | % | EFFECT SIZE (95% CI)a | |
|---|---|---|---|---|---|---|---|---|
| At risk for AEP | 44/44 | 100% | 24/34 | 68.5% | d=2.01 (0.42, 3.60) | 22/32 | 68.8% | d=2.06 (0.47, 3.64) |
| Used unreliable contraception | 44/44 | 100% | 28/35 | 80.0% | d=1.74 (0.14, 3.34) | 24/32 | 75.0% | d=1.89 (0.30, 3.49) |
| Risk drinking | 44/44 | 100% | 30/35 | 85.7% | d=1.53 (–0.09, 3.15) | 28/32 | 87.5% | d=1.46 (−0.18, 3.09) |
The n values reflect the number of participants who provided responses to the variable.
From baseline.
AEP, alcohol-exposed pregnancy; CI, confidence interval; SD, standard deviation.
Discussion
This pilot study found that remote recruitment, data collection, and the EARLY Remote intervention targeting drinking and contraception behaviors were feasible. Participants indicated the intervention was credible and engaging. A very strong therapeutic alliance was developed. It is important that results suggest counselors can conduct the intervention over the telephone while demonstrating good MI treatment fidelity and adherence to the study protocol.
Additionally, the intervention showed promise. Significant changes in both risk behaviors and absolute AEP risk occurred between baseline and follow-up. Although mean DDD did not decrease below risk levels, the proportion of women who used unreliable or no contraception and/or drank at risk levels in the past 90 days decreased significantly, contributing to significant reductions in AEP risk.
It is important to contextualize results, especially change in absolute AEP risk, within the spectrum of face-to-face preconception MI-based AEP interventions tested in RCTs (i.e., CHOICES, BALANCE, and the face-to-face version of EARLY). CHOICES5 resulted in only 36% of women still at risk at 3M. BALANCE7 achieved similar results, with only 31% at risk at the 4-month follow-up. Both CHOICES and BALANCE significantly outperformed comparison conditions. However, EARLY resulted in 65% and 62% of women still at risk at 3M and 6M, respectively, and improvements did not differ from those observed in the comparison conditions. In EARLY Remote, 69% of women were still at risk for AEP at 3M and 6M, which is similar to changes found in association with information control conditions tested in the CHOICES, BALANCE, and EARLY RCTs.5–7,10 Results from this study, in comparison with previous studies' results, suggest that CHOICES and BALANCE are the most potent of the MI-based preconception interventions developed to date. Furthermore, the remote-delivered version of EARLY may be slightly less potent than the same intervention delivered face-to-face.
Limitations
This was an uncontrolled pilot study with a small sample. Although we observed statistically significant, yet clinically modest, changes in AEP risk, these could be unrelated to intervention effects. The informed consent and assessment process may have sensitized women to risk for AEP and exerted an intervention effect. Also, improvements could be related to the passage of time. Additionally, we used self-report measures of target behaviors and treatment engagement, which can be susceptible to social desirability and recall biases.23,24 However, this is consistent with other studies in the AEP risk reduction literature that use self-reported data collection methods, despite their potential flaws.5–7,10
Strengths
This pilot study adds to a small literature on MI-based preconceptional AEP prevention interventions and is the first study to explore the feasibility and promise of a one-session, remote-delivered, MI-based, AEP risk reduction intervention. A remote-delivered intervention, even if it has a lower possible effect than face-to-face interventions, could impact public health by reaching larger samples of women at risk and may even be preferred by women for its convenience and privacy. Of note is that, in the current investigation, most of the sample were African American women, showing the utility of a remote intervention to reach populations at risk for health disparities. Future research might focus on refining the EARLY Remote intervention to enhance treatment effects by adding sessions and/or facilitating access to contraception. Once refined, a remote-delivered intervention could have an important place within the existing spectrum of MI-based preconception AEP interventions and then taken to scale as part of a stepped-care model.25
Conclusions
The one-session EARLY Remote intervention was feasible and associated with reduction in risk behaviors that compose AEP risk (drinking and unreliable use or nonuse of contraception). Although the intervention may not be as potent as lengthier face-to-face interventions that also provide contraception, this relatively low-resource intense intervention might be appropriate as part of a stepped-care model or to reach women at risk who are unable or unwilling to attend face to face counseling interventions, especially after future research and development.25 Dissemination of an improved intervention could result in a substantial public health impact through reduction of AEP risk on a large scale.
Acknowledgments
This study was funded by grant 3RO1 AA014356-S from the National Institutes of Health/National Institute on Alcoholism and Alcohol Abuse to K.S.I. We thank the staff of the University of Virginia Center for Addiction Research and Education in both Richmond and Charlottesville, VA, for their assistance with study logistics. In particular, we thank Sandra Foster for exceptional administrative assistance. We thank Wendy Cohn for her consultation regarding selection of measures. Finally, we thank the Writers' Task Force of the McGuire Veterans Affairs Medical Center in Richmond, VA, for their careful review of two drafts of this manuscript; in particular, we thank Laura Manning, Nicole Kelly, Karen Stewart, and Scott McDonald for their reviews.
Disclosure Statement
No competing financial interests exist. L.F.-C. and J.H. served as counselors. K.S.I. and J.H. served as clinical supervisors. S.K. and J.J. served as recruiters, research assistants, and interviewers. L.M.R. lent his expertise in the area of remote-delivered behavioral health interventions to the study design.
References
- 1.Eaton B. Gangluff D. Mengel M. Fetal alcohol spectrum disorders: Flying under the radar. Ark Med Soc. 2011;107:260–262. [PubMed] [Google Scholar]
- 2.Floyd R. Decoufle P. Hungerford D. Alcohol use prior to pregnancy recognition. Am J Prev Med. 1999;17:101–107. doi: 10.1016/s0749-3797(99)00059-8. [DOI] [PubMed] [Google Scholar]
- 3.Floyd R. Ebrahim S. Boyle C. Observations from the CDC—Preventing alcohol-exposed pregnancies among women of childbearing age: The necessity of a preconceptional approach. J Womens Health Gender Based Med. 1999;8:733–736. doi: 10.1089/152460999319048. [DOI] [PubMed] [Google Scholar]
- 4.Anderson A. Baio J. Ebrahim S. Floyd R. Gould D. Luman E, et al. Alcohol-exposed pregnancy—Characteristics associated with risk. Am J Prev Med. 2002;23:166–173. doi: 10.1016/s0749-3797(02)00495-6. [DOI] [PubMed] [Google Scholar]
- 5.Ingersoll K. Ceperich S. Nettleman M. Johnson B. Binge drinking and risk for pregnancy and STDs among college women. Psychol Health. 2008;23:965–981. doi: 10.1080/08870440701596569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Floyd RL. Sobell M. Velasquez MM. Ingersoll K. Nettleman M. Sobell L, et al. Preventing alcohol-exposed pregnancies—A randomized controlled trial. Am J Prev Med. 2007;32:1–10. doi: 10.1016/j.amepre.2006.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ceperich SD. Ingersoll KS. Motivational interviewing plus feedback intervention to reduce alcohol-exposed pregnancy risk among college binge drinkers: Determinants and patterns of response. J Behav Med. 2011;34:381–395. doi: 10.1007/s10865-010-9308-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ingersoll KS. Ceperich SD. Hettema JE. Farrell-Carnahan L. Penberthy JK. Preconception motivational interviewing interventions to reduce alcohol-exposed pregnancy risk. J Subst Abuse Treat. 2013;44:407–416. doi: 10.1016/j.jsat.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller W. Rollnick S. 2nd. New York: Guilford Press; 2002. Motivational interviewing: Preparing people for change. [Google Scholar]
- 10.Velasquez MM. Ingersoll KS. Sobell MB. Floyd RL. Sobel LC. von Sternberg K. A dual-focus motivational intervention to reduce the risk of alcohol-exposed pregnancy. Cogn Behav Pract. 2010;17:203–212. doi: 10.1016/j.cbpra.2009.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Keulen HM. Mesters I. Ausems M. van Breukelen G. Campbell M. Resnicow K, et al. Tailored print communication and telephone motivational interviewing are equally successful in improving multiple lifestyle behaviors in a randomized controlled trial. Ann Behav Med. 2011;41:104–118. doi: 10.1007/s12160-010-9231-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McBride C. Rimer B. Using the telephone to improve health behavior and health service delivery. Patient Educ Couns. 1999;37:3–18. doi: 10.1016/s0738-3991(98)00098-6. [DOI] [PubMed] [Google Scholar]
- 13.National Institute of Alcohol Abuse and Alcoholism. Bethesda, MD: National Institutes of Health; 2005. Helping patients who drink too much: A clinician's guide. Report Number 05-3769. [Google Scholar]
- 14.Planned Parenthood Federation of America. New York: Planned Parenthood Federation of America; 2011. Facts about birth control. [Google Scholar]
- 15.Sheehan D. Lecrubier Y. Sheehan K. Amorim P. Janavs J. Weiller E, et al. The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 16.Sheehan D. Lecrubier Y. Sheehan K. Janavs J. Weiller E. Keskiner A, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. Eur Psychiatry. 1997;12:232–241. [Google Scholar]
- 17.Sobell L. Brown J. Leo G. Sobell M. The reliability of the alcohol timeline followback when administered by telephone and by computer. Drug Alcohol Depend. 1996;42:49–54. doi: 10.1016/0376-8716(96)01263-x. [DOI] [PubMed] [Google Scholar]
- 18.Sobell L. Sobell M. Timeline follow-back: A technique for assessing self-reported alcohol-consumption. In: Litten RZ, editor; Allen J, editor. Measuring alcohol consumption: Psychosocial and biological methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- 19.Luborsky L. Barber J. Siqueland L. Johnson S. Najavits L. Frank A, et al. The revised helping alliance questionnaire (HAQ-II): Psychometric properties. J Psychother Pract Res. 1996;5:260–271. [PMC free article] [PubMed] [Google Scholar]
- 20.Moyers TB. Martin T. Manuel J, et al. Albuquerque, NM: University of New Mexico Center on Alcoholism, Substance Abuse and Addictions; 2007. Revised global scales: Motivational interviewing treatment integrity 3.0 (MITI3.0) [Google Scholar]
- 21.Hedges L. Olkin I. Orlando, FL; Academic Press; 1985. Statistical methods for meta-analysis. [Google Scholar]
- 22.Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med. 2000;19:3127–3131. doi: 10.1002/1097-0258(20001130)19:22<3127::aid-sim784>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 23.Graham C. Catania J. Brand R. Duong B. Canchola J. Recalling sexual behavior: A methodological analysis of memory recall bias via interview using the diary as the gold standard. J Sex Res. 2003;40:325–332. doi: 10.1080/00224490209552198. [DOI] [PubMed] [Google Scholar]
- 24.Paulhus DL. Measurement and control of response bias. In: Robinson JP, editor; Shaver PR, editor; Wrightsman LS, editor. Measures of personality and social psychological attitudes. San Diego: Academic Press; 1991. pp. 17–59. [Google Scholar]
- 25.Bower P. Gilbody S. Stepped care in psychological therapies: Access, effectiveness and efficiency—Narrative literature review. Br J Psychiatry. 2005;186:11–17. doi: 10.1192/bjp.186.1.11. [DOI] [PubMed] [Google Scholar]
- 26.National Organization on Fetal Alcohol Spectrum Disorders. Fetal alcohol spectrum disorders (FASD): An overview [DVD] 2011. www.youtube.com/watch?v=RHZ6-Tq3YAc. [Jun 6;2013 ]. www.youtube.com/watch?v=RHZ6-Tq3YAc