Abstract
SUMMARY
In a world where most emerging and reemerging infectious diseases are zoonotic in nature and our contacts with both domestic and wild animals abound, there is growing awareness of the potential for human acquisition of animal diseases. Like other Pasteurellaceae, Pasteurella species are highly prevalent among animal populations, where they are often found as part of the normal microbiota of the oral, nasopharyngeal, and upper respiratory tracts. Many Pasteurella species are opportunistic pathogens that can cause endemic disease and are associated increasingly with epizootic outbreaks. Zoonotic transmission to humans usually occurs through animal bites or contact with nasal secretions, with P. multocida being the most prevalent isolate observed in human infections. Here we review recent comparative genomics and molecular pathogenesis studies that have advanced our understanding of the multiple virulence mechanisms employed by Pasteurella species to establish acute and chronic infections. We also summarize efforts being explored to enhance our ability to rapidly and accurately identify and distinguish among clinical isolates and to control pasteurellosis by improved development of new vaccines and treatment regimens.
INTRODUCTION
We now live in an era where two-thirds of human infectious diseases and three-quarters of emerging or reemerging infectious diseases are zoonotic in origin, i.e., diseases caused by animal-associated pathogens that can be shared with humans (1–4). Coupled with the globalization of air travel and commerce and the megamobilization of the food and trade industries, the spread of zoonotic diseases poses a threat to global public health and biosecurity (2, 4–10). With this backdrop, there are rising concerns among health care officials, policy makers, and the general public about human acquisition of zoonotic diseases from close encounters with pets and other wild or domestic animals (5, 8, 10–16). Over 60% of U.S. households have at least one pet (17, 18). Although cats and dogs still rank highest in the U.S. pet population (17), the popularity of nontraditional or exotic pets is growing (9, 19–21). Combined with the expanding impact of changes in land usage and other anthropogenic activities affecting wildlife habitats (22) and the associated movement of and exposure to animals and animal products (11, 12, 23, 24), these trends are thought to contribute to the increased risk of transmission of known and novel zoonoses (9, 14, 22–30).
Of the hundreds of bacterial species known to commonly reside in the oral, nasal, and respiratory cavities of animals (31–33), Pasteurella species are among the most prevalent commensal and opportunistic pathogens found worldwide in domestic and wild animals (34). Pasteurellosis (symptomatic infection with Pasteurella) is a high-impact disease in livestock, according to the World Animal Health Organization (OIE) (www.oie.int). In both animals and humans, Pasteurella species, most notably P. multocida, are often associated with chronic as well as acute infections that can lead to significant morbidity (manifested as pasteurellosis, pneumonia, atrophic rhinitis, dermonecrosis, cellulitis, abscesses, meningitis, and/or hemorrhagic septicemia [HS]) and mortality, particularly in animals (34–36).
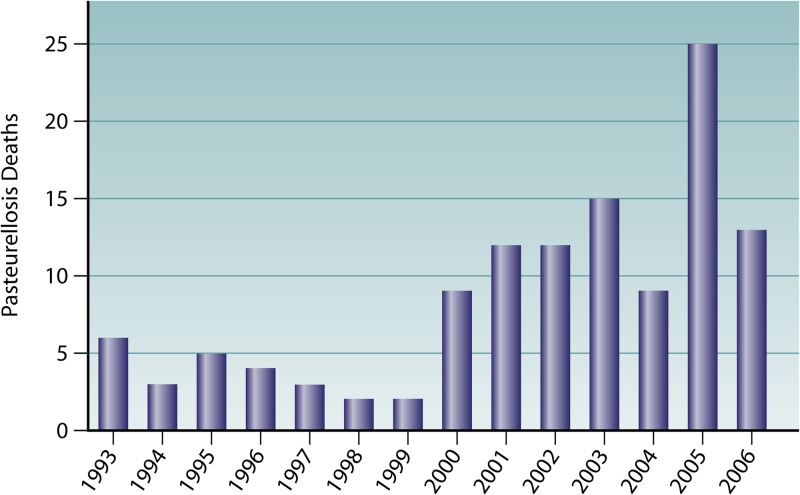
Most likely due to routine prompt prophylactic treatment of animal bite wounds with antibiotics, pasteurellosis is still a relatively uncommon cause of mortality in humans (37, 38), even though deaths due to pasteurellosis have increased in recent years in the United States (Fig. 1). Nevertheless, pasteurellosis is often associated with significant morbidity due to complications resulting from animal bite or scratch wounds or from respiratory exposure (39–46). Roughly 300,000 (1%) annual visits to the emergency rooms in the United States are due to animal bite or scratch wounds (45, 47). Pasteurella species are isolated from infections resulting from 50% of dog bites and 75% of cat bites (48–50), and indeed, it has been observed “… that seemingly trivial animal bites can result in severe complications and that P. multocida is an important cause of infection …” (49). Other contact with animals, such as kissing or licking of skin abrasions or mucosal surfaces (eyes, nose, and mouth), can also result in infection with P. multocida (20, 38, 51–53). In nearly all reported cases of P. multocida infection, evidence of prior animal exposure or contact was indicated.
Fig 1.
Pasteurellosis deaths in the United States, 1993 to 2006. Data are based on CDC general mortality tables (http://www.cdc.gov/nchs/nvss/mortality_tables.htm).
In this review, we provide an overview of the prevalence and pathogenic potential of P. multocida, particularly how it relates to animal infections, human-animal interactions, transmission from animal reservoirs, and subsequent human disease. We also summarize what is currently known about the phylogenetic relationships of P. multocida with other members of the Pasteurellaceae and the pathogenomics, cellular microbiology, and molecular virulence mechanisms that enable P. multocida to cause both acute and chronic disease in animals and humans. Finally, we summarize current antibiotic treatment modalities and efforts toward increasing our options for prevention and control of transmission through animal vaccine development.
PASTEURELLA AND THE PASTEURELLACEAE FAMILY
Comparative Genomics of the Pasteurellaceae
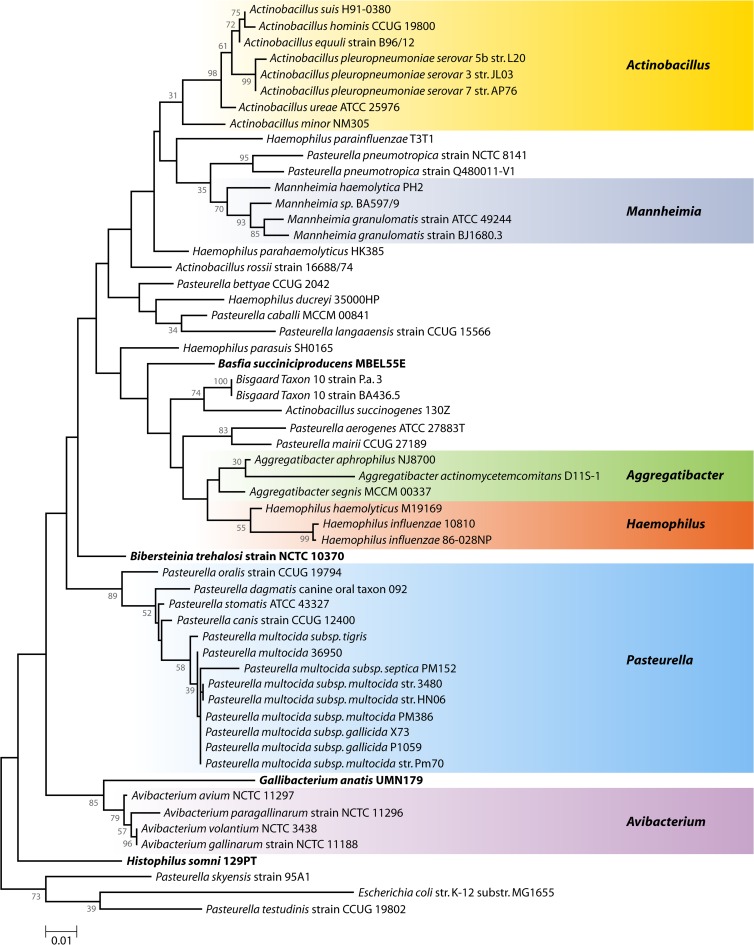
The genus Pasteurella is a member of the Pasteurellaceae family, which includes a large and diverse group of Gram-negative Gammaproteobacteria, whose members are not only human or animal commensals and/or opportunistic pathogens but also outright pathogens (34, 54, 55). Ancestral relationships among bacterial taxa within the Pasteurellaceae family can be inferred by comparing their 16S rRNA genes (Fig. 2). Comparative genomic and phylogenetic analyses of the Pasteurellaceae have revealed that many members of this highly diverse family were poorly classified (54, 56). Indeed, a number of the Pasteurellaceae have already been renamed: Histophilus somni (formerly Haemophilus somnus, H. agni, and H. ovis) (57), Mannheimia (formerly Pasteurella) haemolytica (58), Bibersteinia (formerly Pasteurella) trehalosi (59), Actinobacillus (formerly Haemophilus) pleuropneumoniae (60), Actinobacillus (formerly Pasteurella) ureae (61), Aggregatibacter (formerly Actinobacillus) actinomycetemcomitans (62), Aggregatibacter aphrophilus (formerly Haemophilus aphrophilus and H. paraphrophilus) (62), Aggregatibacter (formerly Haemophilus) segnis (62), Avibacterium (formerly Haemophilus) paragallinarum (63), Avibacterium (formerly Pasteurella) gallinarum (63), Avibacterium (formerly Pasteurella) volantium (63), Avibacterium (formerly Pasteurella) avium (63), Basfia (formerly Mannheimia) succiniciproducens (64), and Gallibacterium (formerly Pasteurella) anatis (65). However, as can been seen from the 16S rRNA phylogenetic tree shown in Fig. 2, further reclassification or renaming may be warranted.
Fig 2.
Phylogenetic relationships of Pasteurella multocida and related Pasteurellaceae bacteria based on 16S rRNA genes. The maximum-likelihood phylogenetic tree was calculated by using MEGA5 (575), based on full-length 16S rRNA gene sequences. Nodes with bootstrap values of greater than 30% after 1,000 replicates are indicated.
Based on conserved signature sequence insertions and deletions (indels) that are specific for certain subgroups of Pasteurellaceae species, it has been proposed that the Pasteurellaceae family be divided into at least two clades (66). Two other independent studies produced similar but not identical 2-clade clustering of the Pasteurellaceae by using 12 intracellular proteins (67) or 50 conserved proteins (68). However, this attempt to classify the Pasteurellaceae into two clades reflects only the phylogenetic relationships of the genes examined resulting from more recent events such as horizontal gene transfer. Such clustering is not congruent with the phylogenetic tree derived from 16S rRNA gene comparison (as shown in Fig. 2), and it is also not reflective of known host specificities or disease manifestations.
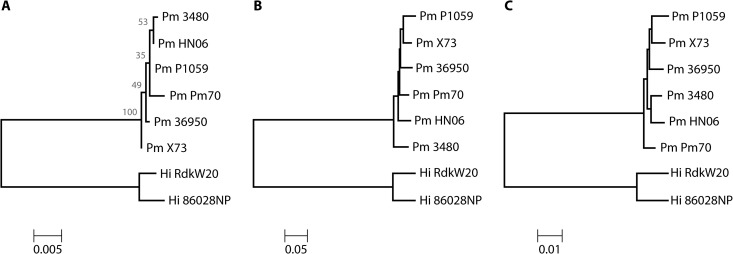
The first Pasteurellaceae member to be genome sequenced was Haemophilus influenzae strain Rd KW20 (69). Since then, the complete or nearly complete genomes of over 28 members of the Pasteurellaceae family have been sequenced, including at least six complete genomes from the species Pasteurella multocida. Phylogenetic analysis of 16S rRNA genes alone shows that these six P. multocida strains tightly cluster and are distant from H. influenzae (Fig. 3A). Genome-wide comparison based on the fractions of common genes (Fig. 3B) or based on similarity among the common genes (Fig. 3C) revealed subtle differences in relatedness among these six P. multocida strains. This likely reflects the dynamics of frequent gene transfer events among the pool of P. multocida strains. While phylogenetic analysis can readily distinguish P. multocida strains from other Pasteurellaceae, ancestral relationships among P. multocida strains are more difficult to define. Consequently, comprehensive genome-wide comparisons (i.e., pathogenomics) are necessary to account for the extent of diversity observed for pathogenic phenotypes among the P. multocida isolates (Table 1).
Fig 3.
Phylogenetic comparison among selected Pasteurella multocida and Haemophilus influenzae species with completed genome sequences. (A) Phylogenetic relationships among the strains based on 16S rRNA genes. The maximum-likelihood tree was calculated by using MEGA5 (575), based on the 16S rRNA genes from each of the indicated strains of P. multocida (Pm) or H. influenzae (Hi) with complete genome sequences. Nodes with bootstrap values of greater than 30% after 1,000 replicates are indicated. (B) Genome-wide comparison based on the fractions of common genes among the strains. The neighbor-joining tree was calculated by using MEGA5 with distances derived from the fraction of genes that are common between each pair of genomes and have >90% coverage in BLASTN alignment. (C) Genome-wide comparison based on the similarity among the common genes among the strains. The neighbor-joining tree was calculated by using MEGA5 with distances derived from the average BLASTN identity for common genes with >90% coverage in alignment.
Table 1.
Genome features and phenotypes of sequenced P. multocida strains
| Strain | Source | Typing | GenBank accession no., size (Mbp) | No. of: | |
|---|---|---|---|---|---|
| Genes | Proteins | ||||
| P. multocida subsp. multocida Pm70 | Oviduct of chicken with fowl cholera | Capsular serotype F:3, nontoxinogenica | AE004439.1, 2.26 | 2,089 | 2,012 |
| P. multocida subsp. gallicida X73 | Fowl cholera | Capsular serotype A:1, nontoxinogenica | CM001580.1, 2.27 | 2,128 | 2,069 |
| P. multocida subsp. gallicida P1059 | Turkey liver | Capsular serotype A:3, nontoxinogenica | CM001581.1, 2.31 | 2,168 | 2,111 |
| P. multocida 36950 | Bovine respiratory infection | Capsular serotype A,b nontoxinogenic,a ICEPmu1c | CP003022.1, 2.35 | 2,202 | 2,098 |
| P. multocida 3480 | Lung of swine with pneumonia | Capsular serotype A,b nontoxinogenica | CP001409.1, 2.38 | 2,296 | 2,223 |
| P. multocida subsp. multocida HN06 | Diseased swine | Capsular serotype D, toxinogenica | CP003313.1, 2.41 (pHN06, 5,360 bp) | 2,361 | 2,265 |
Pathogenomics of P. multocida
A number of genes or gene clusters, identified through signature-tagged transposon mutagenesis (70, 71), in vivo expression technology (72), and whole-genome expression profiling (73–75), have been implicated as important for virulence of P. multocida (76). Some of these genes encoding putative virulence factors are universally present in all six P. multocida genomes, and these include genes encoding outer membrane proteins (ompA, ompH, and ompW), iron acquisition genes (exbB-exbD-tonB, hgbA, and fur), thiamine metabolism genes (tbpA, thiP, and thiQ), and the adhesion/Flp pilus assembly gene cluster (tadZABCDEFG). Homologs of the tad gene locus are also present in many other Pasteurellaceae and Gram-negative bacteria, where they play key roles in biofilm formation, colonization, and pathogenesis (77). Potential virulence genes in P. multocida can also be inferred from a list of virulence genes found in the phylogenetically related H. influenzae (78).
Unique genes correlated with virulence are present in almost each of the sequenced P. multocida genomes. For instance, P. multocida strain 36950, isolated from bovine lung, contains the large integrative conjugative element (ICE) ICEPmu1 of 82 kbp that carries 88 genes, including 12 antimicrobial resistance genes (79, 80). This ICE is not found in any of the other five sequenced genomes; however, a similar ICE was found in Histophilus somni 2336 and Mannheimia haemolytica PHL213, both of which are bovine respiratory pathogens and thus share the same host niche as P. multocida strain 36950. Strain 36950 also has a DNA segment of 9.5 kbp that contains several genes involved in xylose metabolism (xylA, xylF, xylG, xylH, and xylR). Homologs of this region are present in P. multocida strains P1059, P52VAC, HN06, and 3840 but are absent in strains Pm70 and X73.
P. multocida strain Pm70 contains a unique 13.9-kbp region, carrying genes PM1935 to PM1949, that is homologous to a gene cluster found in members of other Pasteurellaceae genera, including H. influenzae R2846 (13 kbp), H. somni 2336 (5 kbp), and Gallibacterium anatis UMN179 (5 kbp). However, strain 36950 is the only other strain of P. multocida that contains a partial sequence (2.1 kbp) homologous to this gene cluster.
The genome of the toxinogenic P. multocida strain HN06 has a unique 18-kbp region carrying 14 genes (PMCN06_2106 to PMCN06_2119), including the toxA gene for P. multocida toxin (PMT) (the toxin responsible for atrophic rhinitis) and several phage-related genes. A 6.7-kbp segment of this sequence lacking the toxA gene is present in the genome of the nontoxinogenic strain 3480. Additionally, there are two regions, a 4.8-kbp region carrying 53 genes (NT08PM_0048 to NT08PM_0100) and a 16-kbp region carrying 22 genes (NT08PM_0622 to NT08PM_0643), in strain 3480 that are also found in strain HN06, albeit fragmented and displaced in multiple loci around the chromosome, further supporting the close relatedness of these two strains. However, there is a 37-kbp fragment (NT08PM_1283 to NT08PM_1334) that is so far unique to strain 3480 and another 33-kbp fragment (PMCN06_1378 to PMCN06_1438) that is so far unique to strain HN06, for which no homologous sequences are found in any of the other strains. It is noteworthy that multiple phage-related genes are present in all of these strain-specific unique sequences, including the segment harboring the toxA gene.
Detection, Identification, and Typing of P. multocida
Selective culturing and phenotyping of P. multocida.
Until very recently, conventional methods for detection and diagnosis of infection with Pasteurella (pasteurellosis) relied on observation of the bacterium by microscopy using staining and/or isolation by in vitro culturing on selective media, followed by phenotypic and/or serological characterization (54). P. multocida is a small, pleomorphic, Gram-negative, nonflagellated coccobacillus. Microscopic analysis of fresh cultures or clinical specimens using Leishman's stain, methylene blue, or Giemsa stain shows bipolar-staining rods. P. multocida isolates are aerobic or facultative anaerobic and grow well at 37°C on 5% sheep's blood (the preferred culture medium) in dextrose-starch, casein-sucrose-yeast (CSY), chocolate, Mueller-Hinton, or brain heart infusion (BHI) agar (81, 82); however, there is no growth on MacConkey agar. Most clinical isolates are catalase, oxidase, indole, and ornithine decarboxylase positive. Most isolates also ferment sucrose, glucose, and maltose. Media containing vancomycin, clindamycin, gentamicin, neomycin, kanamycin, and/or amikacin, either singly or in combination, have been used to select for Pasteurella (83–86), but the results are not always consistent.
Although P. multocida grows well on blood agar and chocolate agar, it is easily overgrown by other microbiota in sputum and might be easily misidentified, as it resembles other Gram-negative bacteria such as Francisella tularensis, Yersinia species, and other Pasteurellaceae species (87–89), such as Haemophilus influenzae (90) and on first examination even Neisseria species (91). Phenotypic characterization of P. multocida, based on morphology, carbohydrate fermentation patterns, and serology, is also challenging (92, 93). Identification of P. multocida using biochemical strips (such as API 20E/20NE, Minitek, or Oxi/Ferm strips) remains a rapid method commonly used in diagnostic laboratories, but it has limited accuracy (94, 95) and can lead to confusion of P. multocida with Mannheimia (Pasteurella) haemolytica (95), H. influenzae, or other Pasteurellaceae species (90, 96, 97). For example, two reports of identification of P. gallinarum as a possible cause of disease in humans were later suspected as possible misidentification as Haemophilus aphrophilus due to similarities in phenotype and/or biochemical properties (98). The authors concluded that the API 20NE system does not differentiate among P. gallinarum, H. aphrophilus, and A. actinomycetemcomitans. Most Haemophilus species, particularly H. influenzae, require chocolate agar or some other source for X and V factors, which Pasteurella species do not. However, a number of Haemophilus species will grow sufficiently on most blood agar media for growth to be discernible, thus necessitating further differentiation from Pasteurella by testing for X and V factor dependency (97). In all, no conclusive diagnostic identification is possible through selective culturing, phenotyping, or direct microscopic examination alone.
Serotyping and ribotyping of P. multocida.
P. multocida isolates are classified based on a combination of capsular polysaccharide serotyping, which distinguishes isolates into one of the five capsular serogroups A (hyaluronic acid) (99), B (arabinose, mannose, and galactose) (100), D (heparin) (101, 102), E (uncharacterized), or F (chondroitin) (101, 102). Isolates are also subtyped based on their lipopolysaccharide (LPS), which separates isolates further into 16 serovars (103, 104). Isolate designations usually consist of a capsular serogroup letter followed by a somatic serovar number (e.g., A:1, A:2, A:3, B:2, etc.). The polysaccharide structure and biosynthetic genes have been determined for three of the capsular serotypes (99, 101, 102, 105, 106), as well as for the LPSs from a number of isolates (103, 107–117).
PCR- plus sequence-based ribotyping analysis using universal primers for 16S rRNA genes, genomics, and other DNA sequence-based molecular techniques have now superseded phenotypic methods for identification, characterization, and differentiation of P. multocida and other Pasteurellaceae (54, 55, 92, 106, 118–120). Conventional ribotyping based on PCR amplification alone is still generally considered a reliable and discriminative method for characterizing clinical isolates of P. multocida (54, 121). However, PCR amplification of 16S rRNA genes, followed by sequencing and sequence comparison against known ribosomal databases, such as the NCBI or the RDP (http://rdp.cme.msu.edu) database, is now the predominant and most reliable method of taxonomically identifying isolates at the genus and species levels.
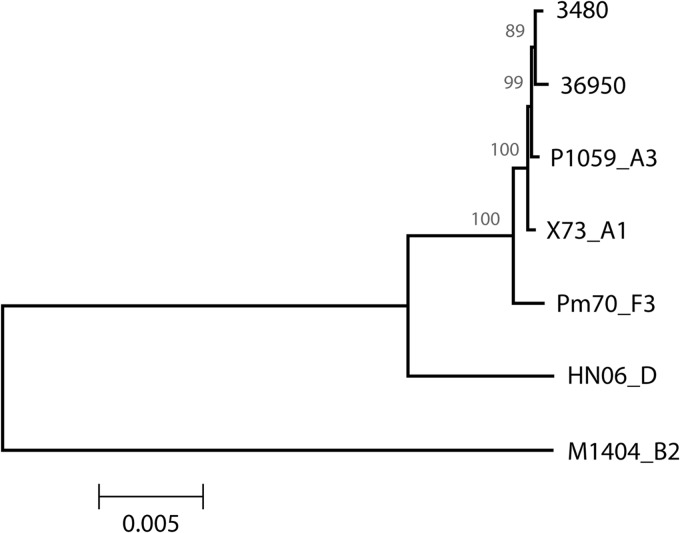
The availability of additional sequence data for comparing various non-16S rRNA gene clusters has enabled the design of more sophisticated PCR methods for taxonomic identification (16S rRNA gene sequence-based ribotyping) and subtyping (virotyping using non-16S rRNA genes such as those associated with virulence traits) of P. multocida isolates (120–122). For example, the cap locus has been sequenced for capsule serotypes B:2 (strain M1404), A:1 (strain X73), A:3 (strain P1590), and D (strain HN06) (Fig. 4) and has been used as a basis for serotyping (106, 118). As a consequence, the cap loci of previously untyped P. multocida strains can now be subtyped based on clustering with the corresponding loci of known serotypes (118, 123–125).
Fig 4.
Phylogenetic comparison of the capsule biosynthesis (cap) gene locus among selected Pasteurella multocida strains. The maximum-likelihood tree was calculated by using MEGA5 (575) with distances derived from genes within the cap locus of P. multocida serotypes B:2 (strain M1404), A:1 (strain X73), A:3 (strain P1590), and D (strain HN06), as well as the cap loci from serotype A strains 3480 and 36950.
PASTEURELLA DISEASE IN ANIMALS
Pasteurellosis Prevalence
Pasteurella species cause numerous endemic and epizootic diseases of economic importance in a wide range of domestic and wild animals and birds. P. multocida is a common commensal or opportunistic pathogen found in the upper respiratory tracts of most livestock, domestic, and wild animals (34), including chickens (126–131), turkeys (132, 133), and other wild birds (123, 134–144), cattle and bison (121, 145–147), swine (34, 148–151), rabbits (152–154), dogs (41, 155–157), cats (domestic house cats as well as large wild cats, such as tigers, leopards, cougars, and lions) (39, 42–46, 49, 157–166), goats (125, 139, 167, 168), chimpanzees (169), marine mammals (seals, sea lions, and walruses) (170), and even komodo dragons (171, 172). The manifestation and pathological symptoms associated with Pasteurella infection, or “pasteurellosis,” range from asymptomatic or mild chronic upper respiratory inflammation to acute, often fatal, pneumonic and/or disseminated disease.
Transmission is through direct contact with nasal secretions, where a chronic infection ensues in the nasal cavity, paranasal sinuses, middle ears, lacrimal and thoracic ducts of the lymph system, and lungs (173, 174). Preexisting or coinfection with other respiratory pathogens, particularly Bordetella bronchiseptica (149, 150, 175–180) or Mannheimia haemolytica (147), significantly enhances colonization by P. multocida, leading to more severe disease. Interestingly, a recent report showed that P. multocida inhibits the growth of M. haemolytica in vitro (181). Primary infection with respiratory viruses or with Mycoplasma species also predisposes animals to secondary infection with P. multocida and/or M. haemolytica (176, 182–186). Environmental conditions, stress, and the overall health of the animal also appear to play important roles in disease severity and likelihood of transmission (147, 187, 188).
Pasteurellosis Pneumonia and Atrophic Rhinitis
The predominant syndrome of pasteurellosis in endemic and epizootic infections of wild and domestic animal populations is upper respiratory disease in the form of rhinitis (irritation and inflammation of nasal mucosa and nasal secretions) and lower respiratory disease in the form of pneumonia (in cattle also referred to as bovine respiratory distress syndrome). Symptoms of pasteurellosis in most animals range from mild to severe (44, 178, 189–198). Mild symptoms include sneezing, copious mucous secretions, mild rhinitis, mild pneumonia with labored breathing, and fever but can progress to disseminated disease (hemorrhagic septicemia [further discussed in “Pasteurellosis and Hemorrhagic Septicemia” below]) and/or atrophic rhinitis (atrophy of nasal mucosa, seromucinous glands, and turbinate bones) associated with toxinogenic strains. Pasteurellosis pneumonia without symptoms of atrophic rhinitis is most often caused by nontoxinogenic capsular type A strains of P. multocida (147, 151, 199, 200).
P. multocida is often endemic in rabbit colonies and swine herds, where the pneumonia and rhinitis disease is commonly called “snuffles” (148, 154). In more severe cases, symptoms progress toward atrophic rhinitis and, in rare cases, renal impairment, testicular and splenic atrophy, and hepatic necrosis. Atrophic rhinitis in rabbits can also result in overall weight loss, growth retardation, and frequently death. Toxinogenic capsular serotype D and some serotype A strains of P. multocida are associated with more severe symptoms of atrophic rhinitis in rabbits and swine (34, 148, 178, 194, 195, 201), with serotype D more prevalent in swine and serotype A more prevalent in rabbits.
The primary overt symptom of atrophic rhinitis in swine and rabbits is twisting or distortion of the snout due to atrophic rhinitis (148, 202–204), manifested as bone resorption characterized by atrophy of the nasal turbinate bones (Fig. 5). Pathological changes may be mild and restricted to the snout with no overt clinical signs other than shrinkage of the ventral turbinates. However, infection can develop into more severe and progressive disease with complete loss of all turbinate bone structures and septum deviation, which often results in twisting, wrinkling, distortion or shortening of the snout, sneezing, snuffling, nasal discharge, and teary eyes (205–207).
Fig 5.

Atrophic rhinitis in swine. Shown are transverse sections of the nasal cavities of pigs exhibiting pathological symptoms of atrophic rhinitis ranging from mild (left panel) to moderate (middle panel) to severe (right panel) caused by infection with toxinogenic P. multocida. (Photos courtesy of the University of Illinois Veterinary Diagnostics Laboratory, Urbana, IL; reproduced with permission.)
Pasteurellosis and Hemorrhagic Septicemia
In cattle and other hoofed animals (ungulates), P. multocida causes predominantly respiratory disease. Along with Mannheimia haemolytica, Histophilus somni, Mycoplasma bovis, and Arcanobacterium pyogenes, P. multocida is implicated as a common pathogen associated with bovine respiratory disease (BRD), or “shipping fever” (nonsepticemic pneumonia) (208, 209). M. haemolytica is the most predominant isolate from cases of BRD and is associated with acute fulminating, fibrinopurulent pleuropneumonia with hemorrhage or coagulation necrosis due to intense LPS-induced inflammation and production of a ruminant-specific, pore-forming leukotoxin (208). P. multocida serotype A:3 is isolated from about 35% of shipping fever cases in the United States (209), manifesting usually as chronic bovine fibrinopurulent bronchopneumonia and occasionally with fibrinonecrosis (Fig. 6) (147, 208). Hemorrhagic septicemia caused by serotype A strains is only occasionally seen in North America (147, 210, 211); however, the proportion of severe hemorrhagic BRD incidences attributed to P. multocida, particularly as coinfection with M. haemolytica or other pathogens, appears to be rising (121, 146, 176, 183, 208, 209, 212). External stressors such as poor food supply, close confinement, and wet climate conditions are also thought to enhance transmission through contact with nasal secretions of infected animals or fomites (147).
Fig 6.
Bovine pasteurellosis bronchopneumonia lung. Shown is an image of a lung lobe from a calf exhibiting pathological symptoms of bronchopneumonia, including extensive hemorrhagic lesions (dark areas), caused by infection with P. multocida. (Courtesy of Peter G. Moisan, Veterinary Diagnostic Laboratory, Kansas State University; reproduced with permission.)
Hemorrhagic septicemia (HS) is a serious acute, highly fatal, and highly prevalent disease in livestock, especially cattle and buffalo, in tropical regions of the world, including Asia, India, Africa, southern Europe, and the Middle East (93, 147, 210, 211, 213–220). HS is caused primarily by P. multocida serotypes B:2 and E:2 and is thought to occur at the later stages of pasteurellosis disease (reviewed in reference 221). HS is observed less commonly in swine, sheep, goats, deer, and elk and then is mostly associated with serotype B:2 strains (214, 221). HS may be asymptomatic or unnoticed until onset of the acute stage, which is characterized by rapid onset (within a few hours) and progression. Symptoms usually begin with fever, lethargy, and edema with copious salivation, lacrimation (teary eyes), and nasal discharge, rapidly followed by respiratory distress, septic shock with widespread hemorrhaging, and death within 1 to 3 days. Antibiotic treatment can be effective at early stages, but since acute clinical signs of sepsis manifest so quickly, mortality is nearly 100% after onset (221).
Despite extensive research, very little is known to date about the virulence factors and mechanisms involved in the transition from mild chronic pasteurellosis to acute severe disseminated disease. Recently, a mouse model of HS caused by P. multocida serotype B:2 has been developed (222), which might enable further exploration of the roles of different host immune cells and host factors as well as bacterial factors in dissemination of the bacteria in the host.
Pasteurellosis and Fowl Cholera
P. multocida subsp. multocida is the most predominant cause of fowl cholera worldwide in a variety of avian species (34, 134, 223), although P. multocida subsp. septica and P. multocida subsp. gallicida are also sometimes isolated (223). Capsular serotype A (mainly A:1, A:3, and A:4) is highly correlated to disease predilection for strains associated with fowl cholera (105, 224–227), although capsular serotypes F and D have also been reported (123, 124, 227, 228). Serotype B:3 is often isolated from avian disease cases that manifest as sinusitis (229, 230) with symptoms of nasal discharge, increased lacrimation, swelling, and inflammation. The respiratory tract appears to be the primary site of infection for fowl cholera (126, 129, 223, 231), but isolation of P. multocida subsp. multocida from avian salpingitis has also been reported (232).
Fowl cholera tends to be an asymptomatic or mild chronic sinusitis and conjunctivitis (229, 230) or pneumonia-like pasteurellosis, but it can suddenly and rapidly develop into a fatal disseminated disease (223). To date, no single bacterial virulence trait or mechanism has been identified as correlating with observed disease incidence or severity (223, 233), but environmental and host factors appear to contribute to onset and outcome severity.
PASTEURELLA AND OTHER PASTEURELLACEAE DISEASES IN HUMANS
Pasteurellosis as a Zoonotic Infection in Humans
Humans acquire Pasteurella infection primarily through contact with animals, most usually through animal bites, scratches, licks on skin abrasions, or contact with mucous secretions derived from pets (19, 20, 36, 40–42, 46, 48, 90, 158, 160, 163, 165, 185, 234–244). The prevalence of antisera to P. multocida was 2-fold higher in healthy individuals with occupational or pet exposure than in a control group with no reported exposure (245), indicating that animal exposure increases the likelihood of subclinical carriage or infection. A survey of the literature over the past 30 years suggests that 20 to 30 human deaths due to pasteurellosis occur annually worldwide, but as mentioned above, this rate appears to be rising (Fig. 1), and in nearly all cases death appears to result as a complication from infection acquired through animal exposure. Among the Pasteurella species, P. multocida is the predominant human pathogen encountered, especially in severe disease cases (235, 239), although P. canis may be more prevalent with dog bites (48, 246–248).
Common symptoms of pasteurellosis in humans from animal bite wounds are swelling (edema), cellulitis (diffuse, localized inflammation with redness and pain), and bloody or suppurative/purulent exudate (drainage) at the wound site (39, 41, 48, 49, 160, 165, 241, 249–255). Leukocyte and neutrophil counts are typically high at the infection site, and inflammation develops very rapidly. In more severe cases, pasteurellosis can rapidly progress to bacteremia (fulminant sepsis) (41, 161, 235, 241, 251, 256–266) and other complications such as osteomyelitis (inflammation of the bone) (155, 165, 267–269), endocarditis (inflammation of the heart) (256, 263, 270–285), and meningitis (inflammation of the meninges) (53, 90, 159, 163, 165, 264, 286–293).
Respiratory infection in humans is relatively uncommon but can occur in patients with chronic pulmonary disease (44, 48, 152, 239, 247, 294–296). In these instances, pasteurellosis can present as severe bilateral consolidating pneumonia and also can cause lymphadenopathy (swelling of the lymph nodes), epiglottitis, and abscess formation (295, 297).
Transmission and Prevalence through Contact with Pets
Infections with Pasteurella requiring medical intervention commonly arise as a result of bite or scratch wounds from pets, predominantly cats and dogs (39, 41, 45, 48, 49, 155–157, 161, 240, 242, 243, 249–251, 254, 255, 257, 258, 267, 298–304), but also from other domestic animals (305–308). Bite wound infections with Pasteurella tend to be highly aggressive with skin or soft tissue inflammation, erythema, local lymphadenopathy, fever, pain, and swelling often manifesting within 24 h, but they can present as early as 8 to 12 h (41, 48, 159, 166, 309). Pasteurellosis has an overall mortality rate of 25 to 30% among reported human cases of animal bite wounds (38, 90, 163, 288, 289, 310), with bacteremia found in 40 to 63% of all pasteurellosis patients and meningitis plus neurological complications found in 17 to 29% of patients.
Pasteurella infections that do not result from bite wounds are likewise most often associated with P. multocida strains (44, 90, 163, 310) and usually involve contact of skin lesions or naso-oropharynx or other upper respiratory mucosa with animals or animal secretions, particularly in young children, the elderly, or pregnant or immunocompromised individuals (40, 44, 53, 87, 90, 165, 235, 240, 241, 244, 255, 257, 258, 261, 277, 288, 289, 291, 307, 311–339).
Neonatal meningitis (usually with septicemia) has been reported (90, 91, 288, 313, 340–342), but in nearly all cases the most likely route of transmission was attributed to direct exposure to pets or other domestic animals. Vertical transmission from mother to child was reported rarely (291, 341). Only three instances of human-to-human horizontal transmission have been reported. In two cases transmission was likely from the father, who had exposure to chickens (286) or sheep (343), and in the third case the mother tested negative for P. multocida colonization but the grandmother tested positive, as did her pet dog (344).
Patients with underlying diseases that contribute to an immunocompromised condition, such as cirrhosis (liver dysfunction) (39, 43, 241, 244, 249, 255–257, 260, 262, 263, 265, 266, 273, 275–280, 292, 312, 314, 316, 317, 321, 322, 328, 329, 335, 337, 345–359), renal failure (kidney dysfunction requiring dialysis or indwelling catheters) (253, 267, 300, 302, 303, 318, 324, 326, 327, 360–366), or HIV-positive status (especially if taking immunosuppressive drugs or experiencing other disease conditions) (290, 310, 315, 367–369), have an increased risk of peritonitis, endocarditis, and/or septicemia caused by P. multocida. This is particularly the case if there is a history of exposure to pets. Indeed, in almost all of the above-mentioned reports, the authors caution patients with these conditions about the risks associated with exposure to pets and/or alert clinicians to consider possible complications with P. multocida infection for cases with pet ownership or a history of animal exposure.
It is noteworthy that in human infection cases the subspecies or serotype of the P. multocida clinical isolate is rarely reported (370). However, there are a few studies where this has been examined retrospectively. In one study, 143 isolates collected from human patients over a 12-year period (1983 to 1994) were biochemically characterized for distribution at the species and subspecies levels as well as capsular groups (239). Most of the isolates were determined to be P. multocida subsp. multocida, with the remaining being P. multocida subsp. septica, P. multocida subsp. gallicida, P. canis, P. dogmatis, and P. stomatis. While P. multocida strains were associated with cat and dog bites, P. canis, P. dogmatis, and P. stomatis strains were recovered only from dog bites, and P. multocida subsp. multocida and P. multocida subsp. septica were most frequently associated with cat bites. Most of the animal bite isolates were non-group A capsular strains (serogroup D) and were associated more with disseminated disease. Capsular serogroup A strains were associated more with respiratory infections. Similar findings were observed for isolates recovered from infected patients in four other studies involving 159 strains (247), 107 strains (48), 54 strains (294), and 20 strains (296).
Rare Cases of Zoonotic Transmission through Wild Animals
Although zoonotic transmission from wild animals is relatively rare, Pasteurella infection is a serious concern in cases of bite wounds from wild animals. Similar to that for bites from their smaller domestic relatives, Pasteurella infection is a high risk for bites from large cats, including lions, tigers, cougars, and others (159, 162, 164, 166, 293, 371–375). Cases of Pasteurella infections have also been reported for bites or exposure to mucous secretions from other wild and domestic animals, including rats, opossums, horses, and rabbits (166, 259, 287, 295, 376). Although these incidents of severe outcome from zoonotic exposure appear to be relatively uncommon, it has been proposed based on historical precedence that there is a potential threat for any pathogen that exclusively infects animals to evolve into a pathogen that more readily transmits among animals and humans and then converts into a bona fide human-specific pathogen (377). It is not hard to speculate that there is potential for a zoonotic pathogen such as Pasteurella, which is highly prevalent in animals and can transmit to humans, to convert into a human pathogen upon acquisition of additional virulence traits.
Human Diseases Caused by Other Pasteurellaceae
In contrast to Pasteurella, most of the other members of the Pasteurellaceae family are primarily animal commensals or enzootic or epizootic pathogens, with a few notable exceptions which are primarily human pathogens. These will be discussed in this section.
Haemophilus.
Haemophilus influenzae is frequently found as a commensal in healthy adult humans but can cause invasive infections in humans, which present as cellulitis, arthritis, pneumonia, sepsis, or meningitis and can often become life threatening. There are six identifiable types and some nontypeable strains of H. influenzae associated with human disease. H. influenzae type b (Hib) is the most prominent form (378). Before introduction of the Hib vaccine, Hib was responsible for about 20,000 cases of and about 1,000 deaths from severe disease in children annually, but invasive Hib disease has nearly been eradicated since the introduction of the Hib conjugate vaccine (379). Other strains of H. influenzae, particularly noncapsular (nontypeable) strains, remain important pathogens in humans worldwide (379–381).
H. influenzae biogroup aegyptius is responsible for recurring outbreaks of seasonal acute, purulent conjunctivitis, more commonly known as pink eye (382). In 1984, a new, highly virulent strain emerged in Brazil that caused a highly lethal disseminated disease in young children, called Brazilian purpuric fever (BPF) (382, 383). The infection presented as an acute, purulent conjunctivitis before rapid onset of bacteremia and progression to septic shock, with mortality rates as high as 70% (383). A pan-genomic analysis of the invasive BPF isolate with other noninvasive H. influenzae isolates responsible for conjunctivitis identified significant differences in the repertoire of autotransporter adhesins as well as new fimbrial proteins, which were suggested to contribute to virulence through altered host-pathogen interactions (382).
Haemophilus haemolyticus is closely related to H. influenzae but is generally considered to be a nonpathogenic human commensal found in the pharynges of some individuals (384). However, H. haemolyticus can be mistaken as nontypeable H. influenzae due to its lack of a capsule and its variable hemolytic properties on blood agar (384, 385). Cases associated with invasive clinical disease in postsurgical patients have been identified using 16S rRNA sequencing (386).
Haemophilus ducreyi is a strict human pathogen that naturally infects genital and nongenital skin (387), causing genital ulcerative disease known as chancroid (388–390). Interestingly, H. ducreyi is more closely related to the animal pathogens M. haemolytica and Actinobacillus pleuropneumoniae than to other human pathogens of the Pasteurellaceae family (Fig. 2) (68). Identification of virulence genes and elucidation of the molecular basis of pathogenesis in H. ducreyi may provide insight into how a pathogen could adapt to occupy a unique niche in a human host (390).
Actinobacillus.
Most Actinobacillus species are enzootic or epizootic pathogens; A. hominis and A. ureae are the only known exceptions, being highly adapted to humans. Both are relatively uncommon commensals of the human respiratory tract but can cause infections. A. hominis can cause lower respiratory tract infections that can progress to bacteremia, sepsis, or meningitis and in severe cases can result in death, particularly in immunocompromised individuals (391). Most cases of A. ureae infections are associated with predisposing factors, such as head trauma, a neurosurgical procedure, liver cirrhosis, alcoholism, diabetes, malnutrition, or immunosuppression (392–395). For example, A. ureae meningitis was found in a number of immunocompromised patients (392, 394). A. ureae has also been associated with bone marrow infection and septic arthritis in a patient with rheumatoid arthritis taking a tumor necrosis factor alpha (TNF-α) inhibitor (395).
Aggregatibacter.
Aggregatibacter actinomycetemcomitans is a common periodontal pathogen responsible for periodontitis, a chronic inflammatory disease that manifests as loss of supporting connective tissue and alveolar bone around teeth with symptoms of malodor, gingival bleeding, pain, and swelling (396). It is also a major pathogen causing endocarditis (397) and brain abscesses (398). A. actinomycetemcomitans produces two toxins as major virulence factors responsible for pathogenesis: a pore-forming leukotoxin (LtxA) that kills white blood cells in gingiva and thereby helps evade the host immune response during infection (399) and a cytolethal distending toxin (Cdt) that enters host cells to cause cell cycle arrest or apoptosis through its DNase activity and thereby causes extensive damage to gingival tissue (400, 401).
Aggregatibacter aphrophilus is also an oral commensal occasionally found in humans that causes bone and joint infections and endocarditis in some cases (402). Its genome contains genes that encode a type VI secretion system (T6SS) as well as several putative T6SS effector proteins that may contribute to virulence (403).
PASTEURELLA VIRULENCE MECHANISMS
Survival in the Host Environment
Extensive research activities, including a number of genome and transcriptome analyses, are beginning to shed light on the virulence mechanisms of P. multocida (reviewed in reference 233). Several factors appear to be involved enhancing survival in the host environment: iron acquisition mechanisms that enable in vivo growth; membrane lipopolysaccharide (LPS) that confers serum resistance; capsule that prevents phagocytosis; surface components that provide adherence properties; extracellular matrix-degrading enzymes such as hyaluronidase, neuraminidase, and proteases that facilitate colonization and/or dissemination; and in some highly virulent strains a dermonecrotic toxin (PMT) that causes atrophic rhinitis and dermonecrosis and modulates the immune response. This section will explore what is currently known about the role of each of these mechanisms in P. multocida pathogenesis.
Nutrient acquisition.
During later stages of infection, Pasteurella encounters host niches that require changes in gene expression for pathways involved in central energy metabolism and in uptake of various nutrients such as iron and amino acids. Most P. multocida genes shown to be upregulated during infection are involved in nutrient acquisition and metabolic processes (404). Highly virulent strains of P. multocida often secrete various hydrolytic enzymes that presumably facilitate nutrient acquisition or dissemination. Virulent serotype B strains, particularly serotype B:2 isolates from hemorrhagic septicemia cases, produce a hyaluronidase (405, 406). Production of sialidases (neuraminidases), which scavenge sialic acid from host membrane components and serve to evade host defenses by blocking mucin action, is also prevalent in virulent strains of P. multocida (407–410).
Iron acquisition.
Iron is an important nutrient for nearly all life forms. Bacterial pathogens, when in a vertebrate host environment, will encounter a depletion of iron, triggering release of the transcriptional control of ferric uptake regulator (Fur), which represses genes under its control in the presence of iron (411). It is possible that iron acquisition in P. multocida plays an important role in its survival and pathogenesis in the host, particularly considering that more than 2.5% (53 coding DNA sequences) of the Pm70 genes are predicted to encode proteins homologous to known proteins involved in iron uptake or acquisition (412). Gene expression profiling under iron-limiting conditions have identified several iron acquisition genes at increased expression levels (413), and indeed, different sets of genes appear to be expressed in response to the nature of the iron source (414). Many iron acquisition-related genes have been predicted to be part of the outer membrane proteome (415). Although iron-dependent expression profiling of the outer membrane proteome still needs to be investigated, most of these membrane proteins were shown to be protective antigens (416).
Some Pasteurellaceae species have strict host specificity. Iron acquisition system requirements are considered to be an important restricting factor for host specificity. For example, the porcine pathogen A. pleuropneumoniae utilizes porcine transferrin as an iron acquisition vehicle through binding to a bacterial surface receptor, which is comprised of the transferrin-binding proteins TbpA and TbpB. A. pleuropneumoniae binds only porcine transferrin and not bovine or human transferrin (417). Similarly, the bovine pathogen M. haemolytica has a transferrin-binding receptor that binds only bovine transferrin (417, 418). It has also been reported that most strains of H. somni are capable of acquiring iron only from bovine transferrin through binding to the bipartite TbpA-TbpB transferrin receptor, but some strains can also utilize ovine or caprine transferrin through a single-component TbpA2 transferrin receptor (419). Although no TbpA-TbpB homologs are encoded in the six complete genomes of P. multocida, they all have genes coding for homologs of the single-component transferrin receptor and other hemoglobulin/transferrin/lactoferrin receptor family proteins. In addition, P. multocida strains have siderophore-independent iron acquisition systems homologous to the Actinobacillus AfeABCD system (420) and the periplasmic binding protein-dependent iron transport systems homologous to E. coli FecBCDE (421), Neisseria FbpABC (422), and Actinobacillus AfuABC systems (423), which can utilize xenosiderophores for iron acquisition. The presence of multiple iron acquisition systems in Pasteurella species may account for their ability to infect multiple hosts.
Surface components.
(i) LPS.
P. multocida lipopolysaccharide (LPS) confers resistance to serum complement and is a major virulence determinant (113, 114, 117, 424). Avian strains with mutations in LPS are highly attenuated in chickens (109, 117). P. multocida strains express two LPS glycoforms (A and B) that differ in their inner core structure (114, 117), whereas the outer antigen structure varies among strains and has been classified into 16 different LPS serovars (107, 109). Protection against P. multocida infection appears to be serovar specific (108).
(ii) Capsule.
P. multocida expresses a hydrophilic capsule that inhibits phagocytosis and complement-mediated opsonization (224, 425–427). Loss of capsule biosynthesis results in highly attenuated strains that are no longer serum resistant (105, 224). The major polysaccharide component of serotype A capsule is hyaluronic acid, which is consistent with its structural properties (99) and sensitivity to hyaluronidase (226, 428). The hexA gene responsible for capsule export, located in an 11-gene cap locus in the P. multocida strain X73 (serotype A:1) (226), is required for growth in both chickens and mice (224). The apparent predominance of serotype A strains in zoonotic respiratory carriage and infections in humans (48, 85, 152, 239, 294) has been attributed to the antiphagocytic properties of the mucoid capsular hyaluronic acid components (239, 429), which prevent phagocytic clearing and promote mucosal colonization of the lower respiratory tract in humans.
In contrast to the serotype A capsule, the serotype B polysaccharide capsule consists of arabinose, mannose, and galactose sugar residues with as-yet-unclear linkages (427). The cexA gene, a homolog of hexA, is part of a 15-gene capsule (cap) biosynthesis locus and has been shown to be a virulence determinant for P. multocida strain M1404 (serotype B:2) in mice (426). Serotype B and E isolates are infrequently recovered from human infections (239).
Based on sensitivity to mucopolysaccharidases, structural composition analysis, and cloning and sequencing of the capsule biosynthesis genes, serotype D capsules are comprised of heparin or heparin sulfate (101, 102, 430), and serotype F capsules are made of chondroitin (101, 430, 431). The capsule biosynthesis gene loci for serotypes A, D, and F appear to have high similarity with each other but can be distinguished by multiplex PCR-based typing analysis (106, 118). Human clinical isolates with serotype D capsules are most often associated with systemic infections resulting from skin and soft tissue exposure (48, 85, 152, 239, 247, 294, 296).
Although noncapsular variants may arise through mutational events, there is evidence that capsule biosynthesis might be transcriptionally regulated (105). Through study of acapsular strains of P. multocida, a single-site mutation in the fis gene outside the cap locus was found to prevent capsule production despite the strains having an intact biosynthetic locus (432), suggesting that regulation of capsule production is possible through the Fis protein, a known transcriptional regulator in other bacteria.
(iii) OMPs.
Putative adhesins that enhance colonization by P. multocida have been reported (34, 433–442). OmpA is an outer membrane protein (OMP) that serves as an adhesin by binding to host extracellular matrix proteins, such as fibronectin (437, 438, 443). OmpH is a major outer membrane porin that forms a homotrimeric channel and has shown some potential as a protective antigen (444). OmpH and Pasteurella lipoprotein E (PlpE) are protective surface antigens associated with P. multocida serotype A:1, A:3, and A:4 strains isolated from cattle with shipping fever (445, 446) and from birds with fowl cholera (416). OmpA and OmpH proteins show considerable heterogeneity, and at least among avian P. multocida strains, a number of different variants appear to be associated with certain capsular serotypes (B, D, or F) (200, 227).
Oma87, an 87-kDa outer membrane protein present in all P. multocida strains that is expressed in vivo, shares sequence similarity with the surface D15 protective surface antigen of H. influenzae (447). Another protective surface antigen that has been identified is a 39-kDa adhesion protein (Cp39) present in avian P. multocida strains P-1059 (serotype A:3) and X-73 (serotype A:1) (436, 448).
The type IV fimbrial subunit PtfA has been identified and characterized from serotype A, B, D, and F strains (439, 449–451); however, the role of type IV fimbriae in adhesion, host specificity, and colonization is not yet clear. On the other hand, an analogous type IV pilin protein, Tfp, of Pseudomonas aeruginosa has been shown to bind lung epithelial cells, leading to pathogenic effects in the host (452).
Growth of P. multocida strains under iron-limited versus iron-rich conditions showed iron-dependent changes in iron acquisition genes (413, 414), several of which were identified as encoding OMPs (453). Further insights about the role of these iron acquisition OMPs in the pathogenic potential of P. multocida could be gained by more comprehensive outer membrane proteomic analysis of these proteins in response to various iron and nutrient conditions. Despite all these reports and studies showing their potential use as protective antigens for component vaccines (see below), no OMP has yet been shown to be an essential virulence factor.
(iv) Filamentous hemagglutinin.
P. multocida possesses two filamentous hemagglutinins, FhaB1 and FhaB2 (also named PfhB1 and PfhB2, respectively) (70, 412). These proteins are similar to the LspA1 and LspA2 filamentous hemagglutinins from H. ducreyi (454), mutations of which have been shown to affect virulence (455). A similar filamentous hemagglutinin in Bordetella pertussis and B. bronchiseptica is required for biofilm formation and colonization of the nose and trachea in mice (456, 457). FhaB2 in P. multocida has been implicated in virulence (70, 458), and expression of FhaB2 was found to be reduced by 4-fold in a nonmucoid P. multocida variant, AL1114 (432). FhaB and its transporter FhaC form a two-partner secretion system that is similar to the FhaB-FhaC system in Bordetella species (456, 459), LspA-LspB in H. ducreyi (455), and IbpA-IbpB in the pathogenic Histophilus somni strain 2336 (460), which act to inhibit phagocytosis. Genome-wide comparison showed that the IbpA-IbpB system and two other immunoglobulin-binding proteins, p76 and p120, are absent in the avirulent H. somni strain PT129 (460).
PMT.
Once it was discovered that only certain capsular serotype D and A strains of P. multocida were responsible for chronic turbinate atrophy, a large protein toxin was identified, isolated, and cloned from these strains (148, 194, 196, 461, 462). The purified, 146-kDa P. multocida toxin (PMT), encoded by the toxA gene located on a putative lysogenic bacteriophage (463), was subsequently demonstrated to be the primary agent responsible for the symptoms of atrophic rhinitis (461, 464–471), as well as a number of other clinical symptoms associated with P. multocida infection (189, 190, 192, 461, 464, 470, 472–475). PMT-mediated bone atrophy appears to occur through disruption of normal cell signaling processes in bone-generating osteoblasts and macrophage-like osteoclasts (205, 206, 466, 476–482). In humans, toxin-producing strains are often isolated from respiratory carriage or infections (483), but a role for PMT in human pulmonary disease has not yet been established.
PMT is a member of the dermonecrotic toxin family of G-protein-deamidating toxins, whose molecular mechanism of action has been thoroughly reviewed (201, 484–487). Mounting evidence suggests that PMT enters mammalian cells (reviewed in reference 486) and exerts its pathogenic effect on cells through modulation of multiple signaling pathways (reviewed in reference 485). Recent studies have revealed that in addition to the α subunit of the heterotrimeric Gq protein (488–490), PMT also acts on other G proteins, i.e., G11, Gi, and G12/13 (488–494). A number of studies have implicated PMT as a modulator of host immunity (475, 495–498) and cellular differentiation and proliferation (476, 477, 485, 499–507). Interestingly, because of its potent mitogenic and proliferative properties, there has been speculation that exposure to PMT might play a role in cancer predisposition as a long-term consequence of infection with toxinogenic P. multocida (485, 495, 499, 504, 505, 508–510).
DNA Uptake
A number of the Pasteurellaceae are competent for DNA uptake, and two high-frequency uptake signal sequences (USS) have been identified for members of the Pasteurellaceae (67): the USS (AAGTGCGGT) found in P. multocida, H. influenzae, Aggregatibacter actinomycetemcomitans, Histophilus somni, and Mannheimia succiniciproducens and the closely related USS (ACAAGCGGT) found in Haemophilus ducreyi, Actinobacillus pleuropneumoniae, and M. haemolytica. The common USS and conservation of all competence genes among these family members suggest a common ancestral origin of competence.
The mechanism for DNA uptake and organization of the competence apparatus of P. multocida can be inferred from the better-characterized H. influenzae system (511). All six completed P. multocida genomes harbor the entire set of competence-related genes, including comABCDE, comF, comEA, comEC/rec2, and orfJ. The presence of competence as well as a universal USS favors the ready exchange of virulence traits through horizontal gene transfer among these family members and accounts for many of their similar pathogenic properties. It is interesting that only four family members (H. somni, H. ducreyi, M. succiniciproducens, and M. haemolytica) appear to have recently acquired mutations resulting in defective competence systems (67).
Transformation of P. multocida usually requires P. multocida-specific vectors (512). Most effective transformation methods for genetic manipulation of P. multocida involve conjugation using shuttle vectors (513–515) or the use of transposons (70, 516). The capsules of some P. multocida strains are known to hinder transformation of nonspecific vectors, but the presence of mucolytic enzymes or coculturing with bacteria producing capsule lytic enzymes has been reported to enhance the competence of capsulated P. multocida X73 (513). This finding implies that enhanced competence and acquisition of new virulence genes could occur under various infection conditions, including coinfections or polymicrobial infections.
Antibiotic Resistance
While not all strains of P. multocida harbor plasmids, plasmids of various sizes (usually 1 to 6 kb but up to 100 kb) have been identified in isolates from various sources (517). Most of these plasmids confer resistance to various and often multiple antibiotics (517–531), most frequently β-lactams, tetracycline, chloramphenicol, streptomycin, and sulfonamides. In addition to the antibiotic resistance genes, a few of these plasmids have also been found to carry genes with other functions, such as plasmid mobilization, segregation, or replication genes (522) and putative cation transporter genes (80, 532). Many of the plasmids carrying antibiotic resistance determinants are transferrable among the Pasteurellaceae members, as well as other Gram-negative bacteria (517, 518, 522, 529, 533–536).
Multiple antibiotic resistance genes have been identified on mobilizable or conjugative elements integrated into the chromosomes of some strains. For example, genes encoding multiple antibiotic resistances have been identified integrated into the chromosome of the genome-sequenced P. multocida strain 36950 isolated from a case of BRD that exhibited resistance to all the antibiotics commonly used to control BRD (80, 537). Interestingly, the 85-kb ICEPmu1 element carried 88 genes, including 12 different resistance genes that were distributed between two regions of resistance (80), a 15.7-kb region at one end of the element and a 9.8-kb region at the other end. ICEPmu1 also contains genes involved in conjugative transfer of the element and its chromosomal excision/integration, genes encoding putative metabolic enzymes involved in alcohol, aldehyde, and ketone catabolism, and genes encoding a lysozyme-like protein and a copper-oxidase-like protein (79). A 5.2-kb mobilizable plasmid, pCCK647, encoding spectinomycin/streptomycin resistance was identified in a capsular serotype F strain isolated from a case of bovine peritonitis (520).
TREATMENT AND PREVENTION
Antibiotics
Broad-spectrum antibiotics that target Pasteurella, as well as other Gram-negative and Gram-positive bacteria, are the preferred prophylaxis for animal bites, which tend to be polymicrobial in nature (32, 41, 48, 309). Pasteurella species are not very susceptible to erythromycin, lincosamides (such as clindamycin), or certain β-lactams (such as dicloxacillin or cephalexin), so these antibiotics are not recommended as monovalent treatments for animal bites. Instead, a combination of amoxicillin and the β-lactamase inhibitor clavulanic acid (Augmentin), doxycycline plus metronidazole for patients with penicillin allergies, or clindamycin plus a fluoroquinolone (ciprofloxacin, or trimethoprim-sulfamethoxazole combination for children or ceftriaxone for pregnant women) is the recommended treatment regimen (41, 48, 309).
Vaccination
The relatively low incidence of human pasteurellosis, despite the high prevalence of Pasteurella species in domestic and wild animals, supports the premise that Pasteurella is an opportunistic pathogen for humans. Further support for this comes from studies examining the carriage and anti-Pasteurella antibody levels in individuals with occupational or other extensive exposure to animals (85, 152). Because of the relatively low incidence of human infection, most immunization or vaccination studies against Pasteurella infection have been geared toward controlling animal disease. Despite considerable effort and ample experimental animal models, mechanisms of protective immunity against Pasteurella remain elusive, and so development and evaluation of effective vaccines have been challenging (34, 449, 538).
Detection of high serum levels of IgG antibodies is not indicative of clearance of or resistance to Pasteurella infection but rather is indicative of chronic infection (178, 475, 539, 540). Vaccination using toxin-based component vaccines, bacterins, or live attenuated bacteria is effective against toxin-mediated disease, such as atrophic rhinitis (449, 471, 541–552). A commercial swine vaccine based on P. multocida bacterin-toxoid (BT) conferred protective immunity in rabbits against PMT challenge (553). To prevent vertical transmission of P. multocida from sows to suckling pigs or laterally among young weaned animals, sows are often vaccinated once or twice prior to farrowing to induce passive immunity through colostrum (542, 554–557). However, despite the benefits of PMT-based vaccination for prevention of atrophic rhinitis and other disease symptoms in swine and rabbits (543, 544, 553, 555, 557–559), current commercial and experimental vaccines do not confer complete immunity to P. multocida infection and are not effective in clearing the bacteria (542, 551, 555). Although PMT activates dendritic cells, it is a poor adjuvant and appears to suppress the antibody response in vivo (497). PMT is nonetheless an effective immunogen, and mutant derivatives have shown potential for vaccine development against atrophic rhinitis (543, 544, 549–551, 555, 557, 560, 561).
Several of the Pasteurella outer membrane proteins are putative virulence factors and potential targets for vaccine development (reviewed in reference 433). For example, antisera against the outer membrane protein Oma87 protected mice against a lethal-dose challenge of P. multocida (447). Vaccination with recombinant adhesion protein Cp39 from P. multocida strain P-1059 protected chickens from challenge with strain P-1059 (serotype A:3) and strain X-73 (serotype A:1) (436, 448). OmpH-specific antibodies were more effective than OmpA-specific antibodies in curbing P. multocida growth in mice, presumably by enhancing PMN phagocytosis (562). Full-length OmpH was more effective than shorter fragments as a vaccine against a swine strain of P. multocida (isolated from a case of atrophic rhinitis) in a mouse challenge model (563). Although OmpA elicits a strong antibody response, vaccination is not protective in a mouse model of infection (435). The type 4 fimbrial subunit of serotype A, B, and D strains has been identified as a potential vaccine candidate (439, 449); however, efficacy as a vaccine has been reported only for the fimbrial protein from serotype B:2 against hemorrhagic septicemia in goats (564).
Using a bioinformatics approach, 98 genes in avian strain Pm70 and 107 genes in the nontoxinogenic porcine strain 3480 were identified as encoding putative OMPs (415). Of this combined list, 71 recombinant proteins were expressed and purified, albeit most as insoluble proteins, and tested as vaccine candidates. Only one protein, lipoprotein E (PlpE), was found to protect against P. multocida challenge in chickens and mice, which confirmed previously reported results using the PlpE cloned from the avian serotype A:1 strain X-73 (446). However, a plpE knockout mutant strain retained full virulence (416). Conjugated vaccines comprised of multiple antigens, such as OmpH plus PlpE peptides, have also shown promise (445, 565).
Additional vaccine candidates include the filamentous hemagglutinin protein (FhaB2) (566), iron-regulated Omps (567–570), and LPS (109). Vaccination with peptides derived from FhaB2 protected turkeys from fowl cholera upon challenge with P. multocida P1059 (566). LPS is a major virulence factor and immunogen of P. multocida, but its potential use and efficacy as a vaccine candidate is complicated by the structural heterogeneity of the 16 different serovars (109). Several in vivo-expressed surface antigens have been identified as potential vaccine candidates (72, 538, 571). A number of these are iron-regulated Omps expressed during P. multocida infection and have been characterized as potential immunogens in challenge studies (568–573). For example, the 96-kDa heme acquisition system receptor (HasR) protein is a surface-exposed Omp conserved among most P. multocida isolates. HasR is expressed under low-iron conditions in vivo and confers protection against challenge with bovine P. multocida serotype A:3 strain 232 (568). A whole-cell vaccine based on a serotype A:1 strain of P. multocida that has been inactivated by treatment with high iron concentrations has also been explored (574).
A few bacterin- and/or toxin-based vaccines are available commercially. For example, Porcillis AR-T DF is a PMT-based vaccine comprised of a deletion mutant of PMT (Δ28-148) plus inactivated Bordetella bronchiseptica bacterin. A commercial vaccine against fowl cholera (chickens and turkeys), sold as CholeramuneM, Multimunem, or M-Ninevax-C, is available and is based on a freeze-dried preparation of a live, avirulent avian isolate of P. multocida M-9 strain (a serotype A:3-A:4 cross). A trivalent combination vaccine against fowl cholera (for ducks, chickens, and other poultry) and rabbit pasteurellosis, sold as Landavax, is available as an inactivated bacterin oil emulsion of P. multocida serotype A:1, A:3, and A:4 strains. A tetravalent combination vaccine, sold as Rhini ShieldTX4, provides four-way protection against swine PMT-mediated atrophic rhinitis and respiratory diseases through a bacterin containing inactivated B. bronchiseptica, Erysipelothrix rhusiopathiae (the causative agent of erysipelas), P. multocida serotype A, and toxinogenic P. multocida serotype D. A tetravalent Pasteurella OBP vaccine for cattle that is a formalinized bacterin of P. multocida serotypes A, D, and E plus M. haemolytica serotype A:1 is also commercially available.
FUTURE PERSPECTIVES
Extensive genetic, biochemical, and virulence studies of P. multocida and other Pasteurellaceae have provided valuable insights into the disease processes of these organisms in their natural hosts and have led to the development of new non-bacterin-based vaccines, several of which are now available commercially for animal use. With the impressive advances that have been made, we are at a cusp in regard to our understanding of the molecular virulence mechanisms of P. multocida pathogenesis. Pathogenomics and ribotyping, in particular, have greatly contributed to our ability to distinguish among the various clinical isolates for diagnostic purposes and epidemiological studies and have provided glimpses of the relatedness among the Pasteurellaceae.
In addition to furthering our understanding of the role of capsule and LPS biosynthesis, antibiotic resistance, and PMT production in pasteurellosis, genome comparison has begun to identify additional virulence genes responsible for host specificity and other phenotypes. Major advances are on the horizon with the information gleaned from comparison of existing and additional genomes of P. multocida and other related Pasteurellaceae in the pipeline, as well as from in vivo transcriptional and protein expression profiling studies such as RNA-seq and proteomics technologies. Greater understanding of the molecular and immunologic mechanisms of pathogenesis will provide insights into the host-microbe interactions involved in chronic infection and the molecular basis of the transition from subclinical or chronic disease to acute, disseminated disease. These studies will also provide clues about the long-term sequelae of exposure to chronic or acute infections with these organisms.
Our interactions with pets and other domestic and wild animals are unlikely to diminish in the future. Mounting evidence suggests that such contacts that result in P. multocida infection can lead to outcomes ranging from benign to disastrous. Considering the high prevalence of Pasteurella species as part of the microbiota of domestic and wild animals, it would be prudent for us to consider zoonotic transmission of P. multocida as a serious risk for infection.
ACKNOWLEDGMENTS
Some of the work reported here was supported by grants from the National Institutes of Health (NIH/NIAID AI038396) and the U.S. Department of Agriculture (NRI 1999-02295) (to B.A.W.).
Biographies

Brenda Anne Wilson, Ph.D., is Associate Professor of Microbiology at the University of Illinois, Urbana, IL. She received her doctorate degree in chemistry in 1989 from the Johns Hopkins University in Baltimore, MD, where she worked on β-lactam antibiotic biosynthesis. She began her studies on bacterial protein toxins as a postdoctoral fellow at Harvard Medical School. In 1993, she joined the Department of Biochemistry at Wright State University in Dayton, OH. As an Associate Professor, she then moved to her current position in 1999. Dr. Wilson's research involves studying the molecular interactions and biochemical mechanisms by which protein toxins produced by pathogenic bacteria cause their toxic effects on mammalian cells, understanding how the toxins can be used as potent selective cell biology tools for studying signal transduction pathways and physiological processes within cells, designing and developing novel postexposure antitoxin therapeutics, and exploiting comparative and functional genomic technologies to study the dynamic interactions between the hosts (humans and nonhuman primates) and their microbiomes.
Mengfei Ho, Ph.D., is a Research Assistant Professor of Microbiology at the University of Illinois, Urbana, IL. He received his doctorate degree in chemistry in 1984 from the Johns Hopkins University in Baltimore, MD, where he worked on β-lactam antibiotic biosynthesis. After his postdoctoral training in protein chemistry at Rockefeller University in New York, he taught medicinal chemistry at the State University of New York at Buffalo and biochemistry at Wright State University in Dayton, OH. He has worked in various areas, including the protein chemistry and structure-function relationships of protein kinases, G-proteins, Pasteurella multocida toxin, and other bacterial protein toxins. He is currently also a Jinshan Scholar at Fujian Agricultural and Forestry University in Fuzhou, China.
REFERENCES
- 1. Cleaveland S, Haydon DT, Taylor L. 2007. Overviews of pathogen emergence: which pathogens emerge, when and why? Curr. Top. Microbiol. Immunol. 315:85–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jones KE, Patel NG, Levy MA, Storeygard A, Balk D, Gittleman JL, Daszak P. 2008. Global trends in emerging infectious diseases. Nature 451:990–993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kuiken T, Leighton FA, Fouchier RA, LeDuc JW, Peiris JS, Schudel A, Stohr K, Osterhaus AD. 2005. Public health. Pathogen surveillance in animals. Science 309:1680–1681 [DOI] [PubMed] [Google Scholar]
- 4. Taylor LH, Latham SM, Woolhouse ME. 2001. Risk factors for human disease emergence. Philos. Trans. R. Soc. Lond. B Biol. Sci. 356:983–989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Karesh WB, Dobson A, Lloyd-Smith JO, Lubroth J, Dixon MA, Bennett M, Aldrich S, Harrington T, Formenty P, Loh EH, Machalaba CC, Thomas MJ, Heymann DL. 2012. Ecology of zoonoses: natural and unnatural histories. Lancet 380:1936–1945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Morse SS, Mazet JA, Woolhouse M, Parrish CR, Carroll D, Karesh WB, Zambrana-Torrelio C, Lipkin WI, Daszak P. 2012. Prediction and prevention of the next pandemic zoonosis. Lancet 380:1956–1965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Woolhouse ME. 2002. Population biology of emerging and re-emerging pathogens. Trends Microbiol. 10:S3–S7 [DOI] [PubMed] [Google Scholar]
- 8. Woolhouse ME, Gowtage-Sequeria S. 2005. Host range and emerging and reemerging pathogens. Emerg. Infect. Dis. 11:1842–1847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cutler SJ, Fooks AR, van der Poel WH. 2010. Public health threat of new, reemerging, and neglected zoonoses in the industrialized world. Emerg. Infect. Dis. 16:1–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wilson BA. 2008. Global biosecurity in a complex, dynamic world. Complexity 14:71–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Karesh WB, Cook RA, Bennett EL, Newcomb J. 2005. Wildlife trade and global disease emergence. Emerg. Infect. Dis. 11:1000–1002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Karesh WB, Noble E. 2009. The bushmeat trade: increased opportunities for transmission of zoonotic disease. Mt. Sinai J. Med. 76:429–434 [DOI] [PubMed] [Google Scholar]
- 13. Smith KM, Anthony SJ, Switzer WM, Epstein JH, Seimon T, Jia H, Sanchez MD, Huynh TT, Galland GG, Shapiro SE, Sleeman JM, McAloose D, Stuchin M, Amato G, Kolokotronis SO, Lipkin WI, Karesh WB, Daszak P, Marano N. 2012. Zoonotic viruses associated with illegally imported wildlife products. PLoS One 7:e29505. 10.1371/journal.pone.0029505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Reaser JK, Clark EE, Jr, Meyers NM. 2008. All creatures great and minute: a public policy primer for companion animal zoonoses. Zoonoses Public Health 55:385–401 [DOI] [PubMed] [Google Scholar]
- 15. Woodford MH. 2009. Veterinary aspects of ecological monitoring: the natural history of emerging infectious diseases of humans, domestic animals and wildlife. Trop. Anim. Health Prod. 41:1023–1033 [DOI] [PubMed] [Google Scholar]
- 16. Weese JS, McCarthy L, Mossop M, Martin H, Lefebvre S. 2007. Observation of practices at petting zoos and the potential impact on zoonotic disease transmission. Clin. Infect. Dis. 45:10–15 [DOI] [PubMed] [Google Scholar]
- 17.American Veterinary Medical Association 2012. U.S. pet ownership and demographics sourcebook. American Veterinary Medical Association, Schaumburg, IL [Google Scholar]
- 18.Humane Society of the United States 2012. American Pet Products Manufacturers Association (APPMA) 2011-2012 national pet owners survey. http://www.americanpetproducts.org/press_industrytrends.asp [Google Scholar]
- 19. Chomel BB, Belotto A, Meslin FX. 2007. Wildlife, exotic pets, and emerging zoonoses. Emerg. Infect. Dis. 13:6–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chomel BB, Sun B. 2011. Zoonoses in the bedroom. Emerg. Infect. Dis. 17:167–172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Souza MJ. 2011. One health: zoonoses in the exotic animal practice. Vet. Clin. North Am. Exot. Anim. Pract. 14:421–426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Patz JA, Daszak P, Tabor GM, Aguirre AA, Pearl M, Epstein J, Wolfe ND, Kilpatrick AM, Foufopoulos J, Molyneux D, Bradley DJ. 2004. Unhealthy landscapes: policy recommendations on land use change and infectious disease emergence. Environ. Health Perspect. 112:1092–1098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fevre EM, Bronsvoort BM, Hamilton KA, Cleaveland S. 2006. Animal movements and the spread of infectious diseases. Trends Microbiol. 14:125–131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Greger M. 2007. The long haul: risks associated with livestock transport. Biosecur. Bioterror. 5:301–311 [DOI] [PubMed] [Google Scholar]
- 25. Bengis RG, Leighton FA, Fischer JR, Artois M, Morner T, Tate CM. 2004. The role of wildlife in emerging and re-emerging zoonoses. Rev. Sci. Tech. 23:497–511 [PubMed] [Google Scholar]
- 26. Greger M. 2007. The human/animal interface: emergence and resurgence of zoonotic infectious diseases. Crit. Rev. Microbiol. 33:243–299 [DOI] [PubMed] [Google Scholar]
- 27. Merianos A. 2007. Surveillance and response to disease emergence. Curr. Top. Microbiol. Immunol. 315:477–509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pike BL, Saylors KE, Fair JN, Lebreton M, Tamoufe U, Djoko CF, Rimoin AW, Wolfe ND. 2010. The origin and prevention of pandemics. Clin. Infect. Dis. 50:1636–1640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rostal MK, Olival KJ, Loh EH, Karesh WB. Wildlife: the need to better understand the linkages. Curr. Top. Microbiol. Immunol., in press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Stone AB, Hautala JA. 2008. Meeting report: panel on the potential utility and strategies for design and implementation of a national companion animal infectious disease surveillance system. Zoonoses Public Health 55:378–384 [DOI] [PubMed] [Google Scholar]
- 31. Dewhirst FE, Klein EA, Thompson EC, Blanton JM, Chen T, Milella L, Buckley CM, Davis IJ, Bennett ML, Marshall-Jones ZV. 2012. The canine oral microbiome. PLoS One 7:e36067. 10.1371/journal.pone.0036067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Goldstein EJ, Citron DM, Merriam CV, Tyrrell KL. 2012. Ceftaroline versus isolates from animal bite wounds: comparative in vitro activities against 243 isolates, including 156 Pasteurella species isolates. Antimicrob. Agents Chemother. 56:6319–6323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lowe BA, Marsh TL, Isaacs-Cosgrove N, Kirkwood RN, Kiupel M, Mulks MH. 2012. Defining the “core microbiome” of the microbial communities in the tonsils of healthy pigs. BMC Microbiol. 12:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Harper M, Boyce JD, Adler B. 2006. Pasteurella multocida pathogenesis: 125 years after Pasteur FEMS Microbiol. Lett. 265:1–10 [DOI] [PubMed] [Google Scholar]
- 35. Hill WA, Brown JP. 2011. Zoonoses of rabbits and rodents. Vet. Clin. North Am. Exot. Anim. Pract. 14:519–531 [DOI] [PubMed] [Google Scholar]
- 36. Souza MJ. 2009. Bacterial and parasitic zoonoses of exotic pets. Vet. Clin. North Am. Exot. Anim. Pract. 12:401–415 [DOI] [PubMed] [Google Scholar]
- 37. Cheah AE, Chong AK. 2011. Bites to the hand: are they more than we can chew? Singapore Med. J. 52:715–718 [PubMed] [Google Scholar]
- 38. Velez M, Casanasa B, Greene JN, Morey J, Mastroianni D, Oehler R. 2010. Pasteurella multocida infections in cancer patients. Asian Biomed. 4:449–455 [Google Scholar]
- 39. Adler AC, Cestero C, Brown RB. 2011. Septic shock from Pasturella multocida following a cat bite: case report and review of literature. Conn. Med. 75:603–605 [PubMed] [Google Scholar]
- 40. Heydemann J, Heydemann JS, Antony S. 2010. Acute infection of a total knee arthroplasty caused by Pasteurella multocida: a case report and a comprehensive review of the literature in the last 10 years. Int. J. Infect. Dis. 14:e242–e245 [DOI] [PubMed] [Google Scholar]
- 41. Oehler RL, Velez AP, Mizrachi M, Lamarche J, Gompf S. 2009. Bite-related and septic syndromes caused by cats and dogs. Lancet Infect. Dis. 9:439–447 [DOI] [PubMed] [Google Scholar]
- 42. Dendle C, Looke D. 2008. Animal bites: an update for management with a focus on infections. Emerg. Med. Australasia 20:458–467 [DOI] [PubMed] [Google Scholar]
- 43. Correira K. 2003. Managing dog, cat, and human bite wounds. J. Am. Acad. Physician Assistants 16:28–37 [PubMed] [Google Scholar]
- 44. Klein NC, Cunha BA. 1997. Pasteurella multocida pneumonia. Semin. Respir. Infect. 12:54–56 [PubMed] [Google Scholar]
- 45. Griego RD, Rosen T, Orengo IF, Wolf JE. 1995. Dog, cat, and human bites: a review. J. Am. Acad. Dermatol. 33:1019–1029 [DOI] [PubMed] [Google Scholar]
- 46. Goldstein EJ. 1992. Bite wounds and infection. Clin. Infect. Dis. 14:633–638 [DOI] [PubMed] [Google Scholar]
- 47. Weiss HB, Friedman DI, Coben JH. 1998. Incidence of dog bite injuries treated in emergency departments. JAMA 279:51–53 [DOI] [PubMed] [Google Scholar]
- 48. Talan DA, Citron DM, Abrahamian FM, Moran GJ, Goldstein EJ. 1999. Bacteriologic analysis of infected dog and cat bites. Emergency Medicine Animal Bite Infection Study Group. N. Engl. J. Med. 340:85–92 [DOI] [PubMed] [Google Scholar]
- 49. Jones N, Khoosal M. 1999. Infected dog and cat bites. N. Engl. J. Med. 340:1841–1842 [DOI] [PubMed] [Google Scholar]
- 50. Rempe B, Aloi M, Iskyan K. 2009. Evidence-based management of mammalian bite wounds. Pediatr. Emerg. Med. Pract. 6:1–22 [PubMed] [Google Scholar]
- 51. Arashima Y, Kumasaka K. 2005. Pasteurellosis as zoonosis. Intern. Med. 44:692–693 [DOI] [PubMed] [Google Scholar]
- 52. Iaria C, Cascio A. 2007. Please, do not forget Pasteurella multocida. Clin. Infect. Dis. 45:940. [DOI] [PubMed] [Google Scholar]
- 53. Kawashima S, Matsukawa N, Ueki Y, Hattori M, Ojika K. 2010. Pasteurella multocida meningitis caused by kissing animals: a case report and review of the literature. J. Neurol. 257:653–654 [DOI] [PubMed] [Google Scholar]
- 54. Christensen H, Bisgaard M. 2010. Molecular classification and its impact on diagnostics and understanding the phylogeny and epidemiology of selected members of Pasteurellaceae of veterinary importance. Berl. Munch. Tierarztl. Wochenschr. 123:20–30 [PubMed] [Google Scholar]
- 55. Kuhnert P, Christensen H. 2008. Pasteurellaceae: biology, genomics and molecular aspects. Caister Academic Press, Norfolk, United Kingdom [Google Scholar]
- 56. Bonaventura MP, Lee EK, Desalle R, Planet PJ. 2010. A whole-genome phylogeny of the family Pasteurellaceae. Mol. Phylogenet. Evol. 54:950–956 [DOI] [PubMed] [Google Scholar]
- 57. Angen O, Ahrens P, Kuhnert P, Christensen H, Mutters R. 2003. Proposal of Histophilus somni gen. nov., sp. nov. for the three species incertae sedis ‘Haemophilus somnus', ‘Haemophilus agni’ and ‘Histophilus ovis’. Int. J. Syst. Evol. Microbiol. 53:1449–1456 [DOI] [PubMed] [Google Scholar]
- 58. Angen O, Mutters R, Caugant DA, Olsen JE, Bisgaard M. 1999. Taxonomic relationships of the [Pasteurella] haemolytica complex as evaluated by DNA-DNA hybridizations and 16S rRNA sequencing with proposal of Mannheimia haemolytica gen. nov., comb. nov., Mannheimia granulomatis comb. nov., Mannheimia glucosida sp. nov., Mannheimia ruminalis sp. nov. and Mannheimia varigena sp. nov. Int. J. Syst. Bacteriol. 49:67–86 [DOI] [PubMed] [Google Scholar]
- 59. Blackall PJ, Bojesen AM, Christensen H, Bisgaard M. 2007. Reclassification of [Pasteurella] trehalosi as Bibersteinia trehalosi gen. nov., comb. nov. Int. J. Syst. Evol. Microbiol. 57:666–674 [DOI] [PubMed] [Google Scholar]
- 60. Pohl S, Bertschinger HU, Frederiksen W, Mannheim W. 1983. Transfer of Haemophilus pleuropneumoniae and the Pasteurella haemolytica-like organism causing porcine necrotic pleuropneumonia to the genus Actinobacillus (Actinobacillus pleuropneumoniae comb. nov.) on the basis of phenotypic and deoxyribonucleic acid relatedness. Int. J. Syst. Evol. Microbiol. 33:510–514 [Google Scholar]
- 61. Mutters R, Pohl S, Mannheim W. 1986. Transfer of Pasteurella ureae Jones 1962 to the genus Actinobacillus Brumpt 1910: Actinobacillus ureae comb. nov. Int. J. Syst. Evol. Microbiol. 36:343–344 [Google Scholar]
- 62. Norskov-Lauritsen N, Kilian M. 2006. Reclassification of Actinobacillus actinomycetemcomitans, Haemophilus aphrophilus, Haemophilus paraphrophilus and Haemophilus segnis as Aggregatibacter actinomycetemcomitans gen. nov., comb. nov., Aggregatibacter aphrophilus comb. nov. and Aggregatibacter segnis comb. nov., and emended description of Aggregatibacter aphrophilus to include V factor-dependent and V factor-independent isolates. Int. J. Syst. Evol. Microbiol. 56:2135–2146 [DOI] [PubMed] [Google Scholar]
- 63. Blackall PJ, Christensen H, Beckenham T, Blackall LL, Bisgaard M. 2005. Reclassification of Pasteurella gallinarum, [Haemophilus] paragallinarum, Pasteurella avium and Pasteurella volantium as Avibacterium gallinarum gen. nov., comb. nov., Avibacterium paragallinarum comb. nov., Avibacterium avium comb. nov. and Avibacterium volantium comb. nov. Int. J. Syst. Evol. Microbiol. 55:353–362 [DOI] [PubMed] [Google Scholar]
- 64. Kuhnert P, Scholten E, Haefner S, Mayor D, Frey J. 2010. Basfia succiniciproducens gen. nov., sp. nov., a new member of the family Pasteurellaceae isolated from bovine rumen. Int. J. Syst. Evol. Microbiol. 60:44–50 [DOI] [PubMed] [Google Scholar]
- 65. Christensen H, Bisgaard M, Bojesen AM, Mutters R, Olsen JE. 2003. Genetic relationships among avian isolates classified as Pasteurella haemolytica, ‘Actinobacillus salpingitidis' or Pasteurella anatis with proposal of Gallibacterium anatis gen. nov., comb. nov. and description of additional genomospecies within Gallibacterium gen. nov. Int. J. Syst. Evol. Microbiol. 53:275–287 [DOI] [PubMed] [Google Scholar]
- 66. Naushad HS, Gupta RS. 2012. Molecular signatures (conserved indels) in protein sequences that are specific for the order Pasteurellales and distinguish two of its main clades. Antonie Van Leeuwenhoek 101:105–124 [DOI] [PubMed] [Google Scholar]
- 67. Redfield RJ, Findlay WA, Bosse J, Kroll JS, Cameron AD, Nash JH. 2006. Evolution of competence and DNA uptake specificity in the Pasteurellaceae. BMC Evol. Biol. 6:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Gioia J, Qin X, Jiang H, Clinkenbeard K, Lo R, Liu Y, Fox GE, Yerrapragada S, McLeod MP, McNeill TZ, Hemphill L, Sodergren E, Wang Q, Muzny DM, Homsi FJ, Weinstock GM, Highlander SK. 2006. The genome sequence of Mannheimia haemolytica A1: insights into virulence, natural competence, and Pasteurellaceae phylogeny. J. Bacteriol. 188:7257–7266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Fleischmann RD, Adams MD, White O, Clayton RA, Kirkness EF, Kerlavage AR, Bult CJ, Tomb JF, Dougherty BA, Merrick JM, et al. 1995. Whole-genome random sequencing and assembly of Haemophilus influenzae Rd. Science 269:496–512 [DOI] [PubMed] [Google Scholar]
- 70. Fuller TE, Kennedy MJ, Lowery DE. 2000. Identification of Pasteurella multocida virulence genes in a septicemic mouse model using signature-tagged mutagenesis. Microb. Pathog. 29:25–38 [DOI] [PubMed] [Google Scholar]
- 71. Harper M, Boyce JD, Wilkie IW, Adler B. 2003. Signature-tagged mutagenesis of Pasteurella multocida identifies mutants displaying differential virulence characteristics in mice and chickens. Infect. Immun. 71:5440–5446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Hunt ML, Boucher DJ, Boyce JD, Adler B. 2001. In vivo-expressed genes of Pasteurella multocida. Infect. Immun. 69:3004–3012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Boyce JD, Wilkie I, Harper M, Paustian ML, Kapur V, Adler B. 2002. Genomic scale analysis of Pasteurella multocida gene expression during growth within the natural chicken host. Infect. Immun. 70:6871–6879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Boyce JD, Wilkie I, Harper M, Paustian ML, Kapur V, Adler B. 2004. Genomic-scale analysis of Pasteurella multocida gene expression during growth within liver tissue of chickens with fowl cholera. Microbes Infect. 6:290–298 [DOI] [PubMed] [Google Scholar]
- 75. Guo D, Lu Y, Zhang A, Liu J, Yuan D, Jiang Q, Lin H, Si C, Qu L. 2012. Identification of genes transcribed by Pasteurella multocida in rabbit livers through the selective capture of transcribed sequences. FEMS Microbiol. Lett. 331:105–112 [DOI] [PubMed] [Google Scholar]
- 76. Boyce JD, Seemann T, Adler B, Harper M. 2012. Pathogenomics of Pasteurella multocida. Curr. Top. Microbiol. Immunol. 361:23–38 [DOI] [PubMed] [Google Scholar]
- 77. Tomich M, Planet PJ, Figurski DH. 2007. The tad locus: postcards from the widespread colonization island. Nat. Rev. Microbiol. 5:363–375 [DOI] [PubMed] [Google Scholar]
- 78. Wong SM, Akerley BJ. 2012. Genome-scale approaches to identify genes essential for Haemophilus influenzae pathogenesis. Front. Cell Infect. Microbiol. 2:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Michael GB, Kadlec K, Sweeney MT, Brzuszkiewicz E, Liesegang H, Daniel R, Murray RW, Watts JL, Schwarz S. 2012. ICEPmu1, an integrative conjugative element (ICE) of Pasteurella multocida: structure and transfer. J. Antimicrob. Chemother. 67:91–100 [DOI] [PubMed] [Google Scholar]
- 80. Michael GB, Kadlec K, Sweeney MT, Brzuszkiewicz E, Liesegang H, Daniel R, Murray RW, Watts JL, Schwarz S. 2012. ICEPmu1, an integrative conjugative element (ICE) of Pasteurella multocida: analysis of the regions that comprise 12 antimicrobial resistance genes. J. Antimicrob. Chemother. 67:84–90 [DOI] [PubMed] [Google Scholar]
- 81.OIE, World Organisation for Animal Health 2012, posting date. Manual of diagnostic tests and vaccines for terrestrial animals. http://www.oie.int/international-standard-setting/terrestrial-manual/access-online [Google Scholar]
- 82. Lariviere S, Leblanc L, Mittal KR, Martineau GP. 1993. Comparison of isolation methods for the recovery of Bordetella bronchiseptica and Pasteurella multocida from the nasal cavities of piglets. J. Clin. Microbiol. 31:364–367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Smith IM, Baskerville AJ. 1983. A selective medium for the isolation of P. multocida in nasal specimens from pigs. Br Vet. J. 139:476–486 [DOI] [PubMed] [Google Scholar]
- 84. Morris EJ. 1958. Selective media for some Pasteurella species. J. Gen. Microbiol. 19:305–311 [DOI] [PubMed] [Google Scholar]
- 85. Avril JL, Donnio PY, Pouedras P. 1990. Selective medium for Pasteurella multocida and its use to detect oropharyngeal carriage in pig breeders. J. Clin. Microbiol. 28:1438–1440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Garlinghouse LE, Jr, DiGiacomo RF, Van Hoosier GL, Jr, Condon J. 1981. Selective media for Pasteurella multocida and Bordetella bronchiseptica. Lab. Anim. Sci. 31:39–42 [PubMed] [Google Scholar]
- 87. Kofteridis DP, Christofaki M, Mantadakis E, Maraki S, Drygiannakis I, Papadakis JA, Samonis G. 2009. Bacteremic community-acquired pneumonia due to Pasteurella multocida. Int. J. Infect. Dis. 13:e81–83 [DOI] [PubMed] [Google Scholar]
- 88. Steinbach WJ, Shetty AK. 2001. Use of the diagnostic bacteriology laboratory: a practical review for the clinician. Postgrad. Med. J. 77:148–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Ewers C, Lubke-Becker A, Wieler LH. 2004. Pasteurella: insights into the virulence determinants of a heterogenous bacterial type. Berl. Munch. Tierarztl. Wochenschr. 117:367–386 [PubMed] [Google Scholar]
- 90. Wade T, Booy R, Teare EL, Kroll S. 1999. Pasteurella multocida meningitis in infancy (a lick may be as bad as a bite). Eur. J. Pediatr. 158:875–878 [DOI] [PubMed] [Google Scholar]
- 91. Koranyi KI, Barson WJ, Studley JK. 2005. Meningitis in a young infant. Pediatr. Infect. Dis. J. 24:387. [DOI] [PubMed] [Google Scholar]
- 92. Hunt ML, Adler B, Townsend KM. 2000. The molecular biology of Pasteurella multocida. Vet. Microbiol. 72:3–25 [DOI] [PubMed] [Google Scholar]
- 93. Wilson MA, Rimler RB, Hoffman LJ. 1992. Comparison of DNA fingerprints and somatic serotypes of serogroup B and E Pasteurella multocida isolates. J. Clin. Microbiol. 30:1518–1524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Collins MT, Swanson EC. 1981. Use of the API 20E system to identify non-Enterobacteriaceae from veterinary medical sources. Am. J. Vet. Res. 42:1269–1273 [PubMed] [Google Scholar]
- 95. Collins MT, Weaver N, Ellis RP. 1981. Identification of Pasteurella multocida and Pasteurella haemolytica by API 20E, Minitek, and Oxi/Ferm systems. J. Clin. Microbiol. 13:433–437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Myhrvold V, Brondz I, Olsen I. 1992. Application of multivariate analyses of enzymic data to classification of members of the Actinobacillus-Haemophilus-Pasteurella group. Int. J. Syst. Bacteriol. 42:12–18 [DOI] [PubMed] [Google Scholar]
- 97. Hamilton-Miller JM. 1993. A possible pitfall in the identification of Pasteurella spp. with the API system. J. Med. Microbiol. 39:78–79 [DOI] [PubMed] [Google Scholar]
- 98. Frederiksen W, Tonning B. 2001. Possible misidentification of Haemophilus aphrophilus as Pasteurella gallinarum. Clin. Infect. Dis. 32:987–989 [DOI] [PubMed] [Google Scholar]
- 99. Rosner H, Grimmecke HD, Knirel YA, Shashkov AS. 1992. Hyaluronic acid and a (1-4)-beta-d-xylan, extracellular polysaccharides of Pasteurella multocida (Carter type A) strain 880. Carbohydr. Res. 223:329–333 [DOI] [PubMed] [Google Scholar]
- 100. Boyce JD, Chung JY, Adler B. 2000. Genetic organisation of the capsule biosynthetic locus of Pasteurella multocida M1404 (B:2). Vet. Microbiol. 72:121–134 [DOI] [PubMed] [Google Scholar]
- 101. DeAngelis PL, Gunay NS, Toida T, Mao WJ, Linhardt RJ. 2002. Identification of the capsular polysaccharides of Type D and F Pasteurella multocida as unmodified heparin and chondroitin, respectively. Carbohydr. Res. 337:1547–1552 [DOI] [PubMed] [Google Scholar]
- 102. DeAngelis PL, White CL. 2002. Identification and molecular cloning of a heparosan synthase from Pasteurella multocida type D. The J. Biol. Chem. 277:7209–7213 [DOI] [PubMed] [Google Scholar]
- 103. Harper M, Boyce JD, Adler B. 2012. The key surface components of Pasteurella multocida: capsule and lipopolysaccharide. Curr. Top. Microbiol. Immunol. 361:39–51 [DOI] [PubMed] [Google Scholar]
- 104. Heddleston KL, Gallagher JE, Rebers PA. 1972. Fowl cholera: gel diffusion precipitin test for serotyping Pasteruella multocida from avian species. Avian Dis. 16:925–936 [PubMed] [Google Scholar]
- 105. Watt JM, Swiatlo E, Wade MM, Champlin FR. 2003. Regulation of capsule biosynthesis in serotype A strains of Pasteurella multocida. FEMS Microbiol. Lett. 225:9–14 [DOI] [PubMed] [Google Scholar]
- 106. Townsend KM, Boyce JD, Chung JY, Frost AJ, Adler B. 2001. Genetic organization of Pasteurella multocida cap loci and development of a multiplex capsular PCR typing system. J. Clin. Microbiol. 39:924–929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Harper M, St Michael F, Vinogradov E, John M, Boyce JD, Adler B, Cox AD. 2012. Characterization of the lipopolysaccharide from Pasteurella multocida Heddleston serovar 9: identification of a proposed bi-functional dTDP-3-acetamido-3,6-dideoxy-alpha-d-glucose biosynthesis enzyme. Glycobiology 22:332–344 [DOI] [PubMed] [Google Scholar]
- 108. Harper M, St Michael F, John M, Vinogradov E, Adler B, Boyce JD, Cox AD. 2011. Pasteurella multocida Heddleston serovars 1 and 14 express different lipopolysaccharide structures but share the same lipopolysaccharide biosynthesis outer core locus. Vet. Microbiol. 150:289–296 [DOI] [PubMed] [Google Scholar]
- 109. Harper M, Cox AD, Adler B, Boyce JD. 2011. Pasteurella multocida lipopolysaccharide: the long and the short of it. Vet. Microbiol. 153:109–115 [DOI] [PubMed] [Google Scholar]
- 110. Harper M, Cox AD, St Michael F, Ford M, Wilkie IW, Adler B, Boyce JD. 2010. Natural selection in the chicken host identifies 3-deoxy-d-manno-octulosonic acid kinase residues essential for phosphorylation of Pasteurella multocida lipopolysaccharide. Infect. Immun. 78:3669–3677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. St Michael F, Harper M, Parnas H, John M, Stupak J, Vinogradov E, Adler B, Boyce JD, Cox AD. 2009. Structural and genetic basis for the serological differentiation of Pasteurella multocida Heddleston serotypes 2 and 5. J. Bacteriol. 191:6950–6959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Boyce JD, Harper M, St Michael F, John M, Aubry A, Parnas H, Logan SM, Wilkie IW, Ford M, Cox AD, Adler B. 2009. Identification of novel glycosyltransferases required for assembly of the Pasteurella multocida A:1 lipopolysaccharide and their involvement in virulence. Infect. Immun. 77:1532–1542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Harper M, Cox A, St Michael F, Parnas H, Wilkie I, Blackall PJ, Adler B, Boyce JD. 2007. Decoration of Pasteurella multocida lipopolysaccharide with phosphocholine is important for virulence. J. Bacteriol. 189:7384–7391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Harper M, Boyce JD, Cox AD, St Michael F, Wilkie IW, Blackall PJ, Adler B. 2007. Pasteurella multocida expresses two lipopolysaccharide glycoforms simultaneously, but only a single form is required for virulence: identification of two acceptor-specific heptosyl I transferases. Infect. Immun. 75:3885–3893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. St Michael F, Vinogradov E, Li J, Cox AD. 2005. Structural analysis of the lipopolysaccharide from Pasteurella multocida genome strain Pm70 and identification of the putative lipopolysaccharide glycosyltransferases. Glycobiology 15:323–333 [DOI] [PubMed] [Google Scholar]
- 116. St Michael F, Li J, Vinogradov E, Larocque S, Harper M, Cox AD. 2005. Structural analysis of the lipopolysaccharide of Pasteurella multocida strain VP161: identification of both Kdo-P and Kdo-Kdo species in the lipopolysaccharide. Carbohydr. Res. 340:59–68 [DOI] [PubMed] [Google Scholar]
- 117. Harper M, Cox AD, St Michael F, Wilkie IW, Boyce JD, Adler B. 2004. A heptosyltransferase mutant of Pasteurella multocida produces a truncated lipopolysaccharide structure and is attenuated in virulence. Infect. Immun. 72:3436–3443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Arumugam ND, Ajam N, Blackall PJ, Asiah NM, Ramlan M, Maria J, Yuslan S, Thong KL. 2011. Capsular serotyping of Pasteurella multocida from various animal hosts—a comparison of phenotypic and genotypic methods. Trop. Biomed. 28:55–63 [PubMed] [Google Scholar]
- 119. Blackall PJ, Miflin JK. 2000. Identification and typing of Pasteurella multocida: a review. Avian Pathol. 29:271–287 [DOI] [PubMed] [Google Scholar]
- 120. Dziva F, Muhairwa AP, Bisgaard M, Christensen H. 2008. Diagnostic and typing options for investigating diseases associated with Pasteurella multocida. Vet. Microbiol. 128:1–22 [DOI] [PubMed] [Google Scholar]
- 121. Taylor JD, Fulton RW, Dabo SM, Lehenbauer TW, Confer AW. 2010. Comparison of genotypic and phenotypic characterization methods for Pasteurella multocida isolates from fatal cases of bovine respiratory disease. J. Vet. Diagn. Invest. 22:366–375 [DOI] [PubMed] [Google Scholar]
- 122. Bethe A, Wieler LH, Selbitz HJ, Ewers C. 2009. Genetic diversity of porcine Pasteurella multocida strains from the respiratory tract of healthy and diseased swine. Vet. Microbiol. 139:97–105 [DOI] [PubMed] [Google Scholar]
- 123. Strugnell BW, Dagleish MP, Bayne CW, Brown M, Ainsworth HL, Nicholas RA, Wood A, Hodgson JC. 2011. Investigations into an outbreak of corvid respiratory disease associated with Pasteurella multocida. Avian Pathol. 40:329–336 [DOI] [PubMed] [Google Scholar]
- 124. Mohamed MA, Mohamed MW, Ahmed AI, Ibrahim AA, Ahmed MS. 2012. Pasteurella multocida in backyard chickens in Upper Egypt: incidence with polymerase chain reaction analysis for capsule type, virulence in chicken embryos and antimicrobial resistance. Vet. Ital. 48:77–86 [PubMed] [Google Scholar]
- 125. Soriano-Vargas E, Vega-Sanchez V, Zamora-Espinosa JL, Acosta-Dibarrat J, Aguilar-Romero F, Negrete-Abascal E. 2012. Identification of Pasteurella multocida capsular types isolated from rabbits and other domestic animals in Mexico with respiratory diseases. Trop. Anim. Health Prod. 44:935–937 [DOI] [PubMed] [Google Scholar]
- 126. Woo YK, Kim JH. 2006. Fowl cholera outbreak in domestic poultry and epidemiological properties of Pasteurella multocida isolate. J. Microbiol. 44:344–353 [PubMed] [Google Scholar]
- 127. Zhang P, Fegan N, Fraser I, Duffy P, Bowles RE, Gordon A, Ketterer PJ, Shinwari W, Blackall PJ. 2004. Molecular epidemiology of two fowl cholera outbreaks on a free-range chicken layer farm. J. Vet. Diagn. Invest. 16:458–460 [DOI] [PubMed] [Google Scholar]
- 128. Petersen KD, Christensen JP, Permin A, Bisgaard M. 2001. Virulence of Pasteurella multocida subsp. multocida isolated from outbreaks of fowl cholera in wild birds for domestic poultry and game birds. Avian Pathol. 30:27–31 [DOI] [PubMed] [Google Scholar]
- 129. Muhairwa AP, Christensen JP, Bisgaard M. 2000. Investigations on the carrier rate of Pasteurella multocida in healthy commercial poultry flocks and flocks affected by fowl cholera. Avian Pathol. 29:133–142 [DOI] [PubMed] [Google Scholar]
- 130. Waltman WD, Horne AM. 1993. Characteristics of fowl cholera diagnosed in Georgia, 1989-91. Avian Dis. 37:616–621 [PubMed] [Google Scholar]
- 131. Sander JE, Glisson JR. 1989. Fowl cholera in broilers. Avian Dis. 33:816–819 [PubMed] [Google Scholar]
- 132. Blackall PJ, Pahoff JL, Marks D, Fegan N, Morrow CJ. 1995. Characterisation of Pasteurella multocida isolated from fowl cholera outbreaks on turkey farms. Aust. Vet. J. 72:135–138 [DOI] [PubMed] [Google Scholar]
- 133. Christiansen KH, Carpenter TE, Snipes KP, Hird DW. 1992. Transmission of Pasteurella multocida on California turkey premises in 1988-89. Avian Dis. 36:262–271 [PubMed] [Google Scholar]
- 134. Blanchong JA, Samuel MD, Goldberg DR, Shadduck DJ, Lehr MA. 2006. Persistence of Pasteurella multocida in wetlands following avian cholera outbreaks. J. Wildl. Dis. 42:33–39 [DOI] [PubMed] [Google Scholar]
- 135. Blanchong JA, Samuel MD, Mack G. 2006. Multi-species patterns of avian cholera mortality in Nebraska's Rainwater Basin. J. Wildl. Dis. 42:81–91 [DOI] [PubMed] [Google Scholar]
- 136. Descamps S, Jenouvrier S, Gilchrist HG, Forbes MR. 2012. Avian cholera, a threat to the viability of an Arctic seabird colony? PLoS One 7:e29659. 10.1371/journal.pone.0029659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Fallacara DM, Monahan CM, Morishita TY, Bremer CA, Wack RF. 2004. Survey of parasites and bacterial pathogens from free-living waterfowl in zoological settings. Avian Dis. 48:759–767 [DOI] [PubMed] [Google Scholar]
- 138. Hubalek Z. 2004. An annotated checklist of pathogenic microorganisms associated with migratory birds. J. Wildl. Dis. 40:639–659 [DOI] [PubMed] [Google Scholar]
- 139. Kumar AA, Shivachandra SB, Biswas A, Singh VP, Srivastava SK. 2004. Prevalent serotypes of Pasteurella multocida isolated from different animal and avian species in India. Vet. Res. Commun. 28:657–667 [DOI] [PubMed] [Google Scholar]
- 140. Lehr MA, Botzler RG, Samuel MD, Shadduck DJ. 2005. Associations between water quality, Pasteurella multocida, and avian cholera at Sacramento National Wildlife Refuge. J. Wildl. Dis. 41:291–297 [DOI] [PubMed] [Google Scholar]
- 141. Leotta GA, Chinen I, Vigo GB, Pecoraro M, Rivas M. 2006. Outbreaks of avian cholera in Hope Bay, Antarctica. J. Wildl. Dis. 42:259–270 [DOI] [PubMed] [Google Scholar]
- 142. Samuel MD, Shadduck DJ, Goldberg DR. 2004. Are wetlands the reservoir for avian cholera? J. Wildl. Dis. 40:377–382 [DOI] [PubMed] [Google Scholar]
- 143. Samuel MD, Shadduck DJ, Goldberg DR, Johnson WP. 2005. Avian cholera in waterfowl: the role of lesser snow and ross's geese as disease carriers in the Playa Lakes Region. J. Wildl. Dis. 41:48–57 [DOI] [PubMed] [Google Scholar]
- 144. Wang C, Wu Y, Xing X, Hu G, Dai J, He H. 2009. An outbreak of avian cholera in wild waterfowl in Ordos wetland, Inner Mongolia, China. J. Wildl. Dis. 45:1194–1197 [DOI] [PubMed] [Google Scholar]
- 145. Dyer NW, Ward AC, Weiser GC, White DG. 2001. Seasonal incidence and antibiotic susceptibility patterns of Pasteurellaceae isolated from American bison (Bison bison). Can. J. Vet. Res. 65:7–14 [PMC free article] [PubMed] [Google Scholar]
- 146. Taylor JD, Fulton RW, Lehenbauer TW, Step DL, Confer AW. 2010. The epidemiology of bovine respiratory disease: what is the evidence for preventive measures? Can. Vet. J. 51:1351–1359 [PMC free article] [PubMed] [Google Scholar]
- 147. Dabo SM, Taylor JD, Confer AW. 2007. Pasteurella multocida and bovine respiratory disease. Anim. Health Res. Rev. 8:129–150 [DOI] [PubMed] [Google Scholar]
- 148. Foged NT. 1992. Pasteurella multocida toxin. The characterisation of the toxin and its significance in the diagnosis and prevention of progressive atrophic rhinitis in pigs. APMIS Suppl. 25:1–56 [PubMed] [Google Scholar]
- 149. Cowart RP, Backstrom L, Brim TA. 1989. Pasteurella multocida and Bordetella bronchiseptica in atrophic rhinitis and pneumonia in swine. Can. J. Vet. Res. 53:295–300 [PMC free article] [PubMed] [Google Scholar]
- 150. Rhodes MB, New CW, Jr, Baker PK, Hogg A, Underdahl NR. 1987. Bordetella bronchiseptica and toxigenic type D Pasteurella multocida as agents of severe atrophic rhinitis of swine. Vet. Microbiol. 13:179–187 [DOI] [PubMed] [Google Scholar]
- 151. Kielstein P. 1986. On the occurrence of toxin-producing Pasteurella multocida strains in atrophic rhinitis and in pneumonias of swine and cattle. Zentralbl. Veterinarmed. B 33:418–424 [DOI] [PubMed] [Google Scholar]
- 152. Donnio PY, Le Goff C, Avril JL, Pouedras P, Gras-Rouzet S. 1994. Pasteurella multocida: oropharyngeal carriage and antibody response in breeders. Vet. Res. 25:8–15 [PubMed] [Google Scholar]
- 153. Kawamoto E, Sawada T, Maruyama T. 1990. Prevalence and characterization of Pasteurella multocida in rabbits and their environment in Japan. Nihon Juigaku Zasshi 52:915–921 [DOI] [PubMed] [Google Scholar]
- 154. DiGiacomo RF, Garlinghouse LE, Jr, Van Hoosier GL., Jr 1983. Natural history of infection with Pasteurella multocida in rabbits. J. Am. Vet. Med. Assoc. 183:1172–1175 [PubMed] [Google Scholar]
- 155. Desai SS, Groves RJ, Glew R. 1990. Subacute Pasteurella osteomyelitis of the hand following dog bite. Orthopedics 13:653–656 [DOI] [PubMed] [Google Scholar]
- 156. Rodriguez-Escot C, Hernandez Medina E, Santana-Cabrera L, Sanchez-Palacios M. 2012. Severe Pasteurella multocida infection after a dog bite. J. Emerg. Med. 43:717–718 [DOI] [PubMed] [Google Scholar]
- 157. Lewis KT, Stiles M. 1995. Management of cat and dog bites. Am. Family Phys. 52:479–490 [PubMed] [Google Scholar]
- 158. Brue C, Chosidow O. 1994. Pasteurella multocida wound infection and cellulitis. Int. J. Dermatol. 33:471–473 [DOI] [PubMed] [Google Scholar]
- 159. Burdge DR, Scheifele D, Speert DP. 1985. Serious Pasteurella multocida infections from lion and tiger bites. J. Am. Med. Assoc. 253:3296–3297 [PubMed] [Google Scholar]
- 160. Garcia VF. 1997. Animal bites and Pasturella infections. Pediatr. Rev. 18:127–130 [DOI] [PubMed] [Google Scholar]
- 161. Jones AG, Lockton JA. 1987. Fatal Pasteurella multocida septicaemia following a cat bite in a man without liver disease. J. Infect. 15:229–235 [DOI] [PubMed] [Google Scholar]
- 162. Kizer KW. 1989. Pasteurella multocida infection from a cougar bite. A review of cougar attacks. West. J. Med. 150:87–90 [PMC free article] [PubMed] [Google Scholar]
- 163. Kumar A, Devlin HR, Vellend H. 1990. Pasteurella multocida meningitis in an adult: case report and review. Rev. Infect. Dis. 12:440–448 [DOI] [PubMed] [Google Scholar]
- 164. Morgan MS. 1999. Tiger bites. J. R Soc. Med. 92:545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Weber DJ, Wolfson JS, Swartz MN, Hooper DC. 1984. Pasteurella multocida infections. Report of 34 cases and review of the literature. Medicine 63:133–154 [PubMed] [Google Scholar]
- 166. Woolfrey BF, Quall CO, Lally RT. 1985. Pasteurella multocida in an infected tiger bite. Arch. Pathol. Lab Med. 109:744–746 [PubMed] [Google Scholar]
- 167. Baalsrud KJ. 1987. Atrophic rhinitis in goats in Norway. Vet. Rec. 121:350–353 [DOI] [PubMed] [Google Scholar]
- 168. Shafarin MS, Zamri-Saad M, Khairani BS, Saharee AA. 2008. Proliferation and transmission patterns of Pasteurella multocida B:2 in goats. Trop. Anim. Health Prod. 40:335–340 [DOI] [PubMed] [Google Scholar]
- 169. Kondgen S, Leider M, Lankester F, Bethe A, Lubke-Becker A, Leendertz FH, Ewers C. 2011. Pasteurella multocida involved in respiratory disease of wild chimpanzees. PLoS One 6:e24236. 10.1371/journal.pone.0024236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Hansen MJ, Bertelsen MF, Christensen H, Bisgaard M, Bojesen AM. 2012. Occurrence of Pasteurellaceae bacteria in the oral cavity of selected marine mammal species. J. Zoo Wildl. Med. 43:828–835 [DOI] [PubMed] [Google Scholar]
- 171. Bull JJ, Jessop TS, Whiteley M. 2010. Deathly drool: evolutionary and ecological basis of septic bacteria in Komodo dragon mouths. PLoS One 5:e11097. 10.1371/journal.pone.0011097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Montgomery JM, Gillespie D, Sastrawan P, Fredeking TM, Stewart GL. 2002. Aerobic salivary bacteria in wild and captive Komodo dragons. J. Wildl. Dis. 38:545–551 [DOI] [PubMed] [Google Scholar]
- 173. DiGiacomo RF, Jones CD, Wathes CM. 1987. Transmission of Pasteurella multocida in rabbits. Lab. Anim. Sci. 37:621–623 [PubMed] [Google Scholar]
- 174. DiGiacomo RF, Xu YM, Allen V, Hinton MH, Pearson GR. 1991. Naturally acquired Pasteurella multocida infection in rabbits: clinicopathological aspects. Can. J. Vet. Res. 55:234–238 [PMC free article] [PubMed] [Google Scholar]
- 175. Brockmeier SL, Register KB, Magyar T, Lax AJ, Pullinger GD, Kunkle RA. 2002. Role of the dermonecrotic toxin of Bordetella bronchiseptica in the pathogenesis of respiratory disease in swine. Infect. Immun. 70:481–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Fulton RW. 2009. Bovine respiratory disease research (1983-2009). Anim. Health Res. Rev. 10:131–139 [DOI] [PubMed] [Google Scholar]
- 177. Chanter N, Magyar T, Rutter JM. 1989. Interactions between Bordetella bronchiseptica and toxigenic Pasteurella multocida in atrophic rhinitis of pigs. Res. Vet. Sci. 47:48–53 [PubMed] [Google Scholar]
- 178. Deeb BJ, DiGiacomo RF, Bernard BL, Silbernagel SM. 1990. Pasteurella multocida and Bordetella bronchiseptica infections in rabbits. J. Clin. Microbiol. 28:70–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Pedersen KB, Barfod K. 1981. The aetiological significance of Bordetella bronchiseptica and Pasteurella multocida in atrophic rhinitis of swine. Nord Vet. Med. 33:513–522 [PubMed] [Google Scholar]
- 180. Gagne S, Martineau-Doize B. 1993. Nasal epithelial changes induced in piglets by acetic acid and by Bordetella bronchiseptica. J. Comp. Pathol. 109:71–81 [DOI] [PubMed] [Google Scholar]
- 181. Bavananthasivam J, Dassanayake RP, Kugadas A, Shanthalingam S, Call DR, Knowles DP, Srikumaran S. 2012. Proximity-dependent inhibition of growth of Mannheimia haemolytica by Pasteurella multocida. Appl. Environ. Microbiol. 78:6683–6688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Pardon B, De Bleecker K, Dewulf J, Callens J, Boyen F, Catry B, Deprez P. 2011. Prevalence of respiratory pathogens in diseased, non-vaccinated, routinely medicated veal calves. Vet. Rec. 169:278. [DOI] [PubMed] [Google Scholar]
- 183. Fulton RW, Blood KS, Panciera RJ, Payton ME, Ridpath JF, Confer AW, Saliki JT, Burge LT, Welsh RD, Johnson BJ, Reck A. 2009. Lung pathology and infectious agents in fatal feedlot pneumonias and relationship with mortality, disease onset, and treatments. J. Vet. Diagn. Invest. 21:464–477 [DOI] [PubMed] [Google Scholar]
- 184. Srikumaran S, Kelling CL, Ambagala A. 2007. Immune evasion by pathogens of bovine respiratory disease complex. Anim. Health Res. Rev. 8:215–229 [DOI] [PubMed] [Google Scholar]
- 185. Hartel H, Nikunen S, Neuvonen E, Tanskanen R, Kivela SL, Aho R, Soveri T, Saloniemi H. 2004. Viral and bacterial pathogens in bovine respiratory disease in Finland. Acta Vet. Scand. 45:193–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Galdiero M, Pisciotta MG, Marinelli A, Petrillo G, Galdiero E. 2002. Coinfection with BHV-1 modulates cell adhesion and invasion by P. multocida and Mannheimia (Pasteurella) haemolytica. New Microbiol. 25:427–436 [PubMed] [Google Scholar]
- 187. Simensen E, Olson LD. 1981. Influence of prior hauling on pathogenesis of Pasteurella multocida in turkeys. Poult. Sci. 60:2221–2225 [DOI] [PubMed] [Google Scholar]
- 188. Simensen E, Olson LD, Hahn GL. 1980. Effects of high and low environmental temperatures on clinical course of fowl cholera in turkeys. Avian Dis. 24:816–832 [PubMed] [Google Scholar]
- 189. Ackermann MR, Register KB, Stabel JR, Gwaltney SM, Howe TS, Rimler RB. 1996. Effect of Pasteurella multocida toxin on physeal growth in young pigs. Am. J. Vet. Res. 57:848–852 [PubMed] [Google Scholar]
- 190. Ackermann MR, Stabel JR, Pettit RK, Jacobson CD, Elmquist JK, Register KB, Rimler RB, Hilton JH. 1995. Reduced physeal area and chondrocyte proliferation in Pasteurella multocida toxin-treated rats. Vet. Pathol. 32:674–682 [DOI] [PubMed] [Google Scholar]
- 191. Al-Haddawi MH, Jasni S, Israf DA, Zamri-Saad M, Mutalib AR, Sheikh-Omar AR. 2001. Ultrastructural pathology of nasal and tracheal mucosa of rabbits experimentally infected with Pasteurella multocida serotype D:1. Res. Vet. Sci. 70:191–197 [DOI] [PubMed] [Google Scholar]
- 192. Cheville NF, Rimler RB. 1989. A protein toxin from Pasteurella multocida type D causes acute and chronic hepatic toxicity in rats. Vet. Pathol. 26:148–157 [DOI] [PubMed] [Google Scholar]
- 193. DiGiacomo RF, Allen V, Hinton MH. 1991. Naturally acquired Pasteurella multocida subsp. multocida infection in a closed colony of rabbits: characteristics of isolates. Lab Anim. 25:236–241 [DOI] [PubMed] [Google Scholar]
- 194. DiGiacomo RF, Deeb BJ, Brodie SJ, Zimmerman TE, Veltkamp ER, Chrisp CE. 1993. Toxin production by Pasteurella multocida isolated from rabbits with atrophic rhinitis. Am. J. Vet. Res. 54:1280–1286 [PubMed] [Google Scholar]
- 195. DiGiacomo RF, Deeb BJ, Giddens WE, Jr, Bernard BL, Chengappa MM. 1989. Atrophic rhinitis in New Zealand white rabbits infected with Pasteurella multocida. Am. J. Vet. Res. 50:1460–1465 [PubMed] [Google Scholar]
- 196. Frymus T, Bielecki W, Jakubowski T. 1991. Toxigenic Pasteurella multocida in rabbits with naturally occurring atrophic rhinitis. Zentralbl. Veterinarmed. B 38:265–268 [DOI] [PubMed] [Google Scholar]
- 197. Hoskins IC, Thomas LH, Lax AJ. 1997. Nasal infection with Pasteurella multocida causes proliferation of bladder epithelium in gnotobiotic pigs. Vet. Rec. 140:22. [DOI] [PubMed] [Google Scholar]
- 198. Thurston JR, Rimler RB, Ackermann MR, Cheville NF. 1992. Use of rats to compare atrophic rhinitis vaccines for protection against effects of heat-labile protein toxin produced by Pasteurella multocida serogroup D. Vet. Immunol. Immunopathol. 33:155–162 [DOI] [PubMed] [Google Scholar]
- 199. Davies RL, Watson PJ, Caffrey B. 2003. Comparative analyses of Pasteurella multocida strains associated with the ovine respiratory and vaginal tracts. Vet. Rec. 152:7–10 [DOI] [PubMed] [Google Scholar]
- 200. Davies RL, MacCorquodale R, Baillie S, Caffrey B. 2003. Characterization and comparison of Pasteurella multocida strains associated with porcine pneumonia and atrophic rhinitis. J. Med. Microbiol. 52:59–67 [DOI] [PubMed] [Google Scholar]
- 201. Wilson BA, Ho M. 2006. Pasteurella multocida toxin, p 430–447 Alouf JE, Popoff MR. (ed), The comprehensive sourcebook of bacterial protein toxins. Elsevier Science Publishers B. V., Amsterdam, Netherlands [Google Scholar]
- 202. Chanter N, Rutter JM. 1990. Colonisation by Pasteurella multocida in atrophic rhinitis of pigs and immunity to the osteolytic toxin. Vet. Microbiol. 25:253–265 [DOI] [PubMed] [Google Scholar]
- 203. Frymus T. 1990. Atrophic rhinitis in swine and other animal species. Dtsche. Wochenschr. 97:364–366 [PubMed] [Google Scholar]
- 204. Rutter JM. 1985. Atrophic rhinitis in swine. Adv. Vet. Sci. Comp. Med. 29:239–279 [PubMed] [Google Scholar]
- 205. Felix R, Fleisch H, Frandsen PL. 1992. Effect of Pasteurella multocida toxin on bone resorption in vitro. Infect. Immun. 60:4984–4988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Mullan PB, Lax AJ. 1998. Pasteurella multocida toxin stimulates bone resorption by osteoclasts via interaction with osteoblasts. Calcif. Tissue Int. 63:340–345 [DOI] [PubMed] [Google Scholar]
- 207. Williams PP, Hall MR, Rimler RB. 1990. Host response to Pasteurella multocida turbinate atrophy toxin in swine. Can. J. Vet. Res. 54:157–163 [PMC free article] [PubMed] [Google Scholar]
- 208. Confer AW. 2009. Update on bacterial pathogenesis in BRD. Anim. Health Res. Rev. 10:145–148 [DOI] [PubMed] [Google Scholar]
- 209. Welsh RD, Dye LB, Payton ME, Confer AW. 2004. Isolation and antimicrobial susceptibilities of bacterial pathogens from bovine pneumonia: 1994-2002. J. Vet. Diagn. Invest. 16:426–431 [DOI] [PubMed] [Google Scholar]
- 210. Rimler RB, Wilson MA. 1994. Re-examination of Pasteurella multocida serotypes that caused haemorrhagic septicaemia in North America. Vet. Rec. 134:256. [DOI] [PubMed] [Google Scholar]
- 211. Taylor SK, Ward AC, Hunter DL, Gunther K, Kortge L. 1996. Isolation of Pasteurella spp. from free-ranging American bison (Bison bison). J. Wildl. Dis. 32:322–325 [DOI] [PubMed] [Google Scholar]
- 212. Ames TR, Markham RJ, Opuda-Asibo J, Leininger JR, Maheswaran SK. 1985. Pulmonary response to intratracheal challenge with Pasteurella haemolytica and Pasteurella multocida. Can. J. Comp. Med. 49:395–400 [PMC free article] [PubMed] [Google Scholar]
- 213. Bastianello SS, Jonker MR. 1981. A report on the occurrence of septicaemia caused by Pasteurella multocida type E in cattle from Southern Africa. J. S. Afr. Vet. Assoc. 52:99–104 [PubMed] [Google Scholar]
- 214. Dey S, Singh VP, Kumar AA, Sharma B, Srivastava SK, Singh N. 2007. Comparative sequence analysis of 16S rRNA gene of Pasteurella multocida serogroup B isolates from different animal species. Res. Vet. Sci. 83:1–4 [DOI] [PubMed] [Google Scholar]
- 215. Rani SS, Chaturvedi VK, Gupta PK, Joseph S, Nair BC, Pandey KD. 2006. Cloning and characterisation of the ahpA gene of Pasteurella multocida serogroup b:2 (strain P52): short communication. Acta Vet. Hung. 54:449–453 [DOI] [PubMed] [Google Scholar]
- 216. Tomer P, Chaturvedi GC, Minakshi Malik P, Monga DP. 2002. Comparative analysis of the outer membrane protein profiles of isolates of the Pasteurella multocida (B:2) associated with haemorrhagic septicaemia. Vet. Res. Commun. 26:513–522 [DOI] [PubMed] [Google Scholar]
- 217. Townsend KM, Dawkins HJ, Papadimitriou JM. 1997. REP-PCR analysis of Pasteurella multocida isolates that cause haemorrhagic septicaemia. Res. Vet. Sci. 63:151–155 [DOI] [PubMed] [Google Scholar]
- 218. Kumar P, Singh VP, Agrawal RK, Singh S. 2009. Identification of Pasteurella multocida isolates of ruminant origin using polymerase chain reaction and their antibiogram study. Trop. Anim. Health Prod. 41:573–578 [DOI] [PubMed] [Google Scholar]
- 219. Biswas A, Shivachandra SB, Saxena MK, Kumar AA, Singh VP, Srivastava SK. 2004. Molecular variability among strains of Pasteurella multocida isolated from an outbreak of haemorrhagic septicaemia in India. Vet. Res. Commun. 28:287–298 [DOI] [PubMed] [Google Scholar]
- 220. Verma ND. 1988. Pasteurella multocida B:2 in haemorrhagic septicaemia outbreak in pigs in India. Vet. Rec. 123:63. [DOI] [PubMed] [Google Scholar]
- 221. Shivachandra SB, Viswas KN, Kumar AA. 2011. A review of hemorrhagic septicemia in cattle and buffalo. Anim. Health Res. Rev. 12:67–82 [DOI] [PubMed] [Google Scholar]
- 222. Kharb S, Charan S. 2013. Mouse model of haemorrhagic septicaemia: dissemination and multiplication of Pasteurella multocida B:2 in vital organs after intranasal and subcutaneous challenge in mice. Vet. Res. Commun. 37:59–63 [DOI] [PubMed] [Google Scholar]
- 223. Christensen JP, Bisgaard M. 2000. Fowl cholera. Rev. Sci. Tech. 19:626–637 [DOI] [PubMed] [Google Scholar]
- 224. Chung JY, Wilkie I, Boyce JD, Townsend KM, Frost AJ, Ghoddusi M, Adler B. 2001. Role of capsule in the pathogenesis of fowl cholera caused by Pasteurella multocida serogroup A. Infect. Immun. 69:2487–2492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225. Hirsh DC, Jessup DA, Snipes KP, Carpenter TE, Hird DW, McCapes RH. 1990. Characteristics of Pasteurella multocida isolated from waterfowl and associated avian species in California. J. Wildl. Dis. 26:204–209 [DOI] [PubMed] [Google Scholar]
- 226. Chung JY, Zhang Y, Adler B. 1998. The capsule biosynthetic locus of Pasteurella multocida A:1. FEMS Microbiol. Lett. 166:289–296 [DOI] [PubMed] [Google Scholar]
- 227. Davies RL, MacCorquodale R, Caffrey B. 2003. Diversity of avian Pasteurella multocida strains based on capsular PCR typing and variation of the OmpA and OmpH outer membrane proteins. Vet. Microbiol. 91:169–182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Wilson MA, Duncan RM, Nordholm GE, Berlowski BM. 1995. Pasteurella multocida isolated from wild birds of North America: a serotype and DNA fingerprint study of isolates from 1978 to 1993. Avian Dis. 39:587–593 [PubMed] [Google Scholar]
- 229. Songserm T, Viriyarampa AS, Sae-Heng N, Chamsingh W, Bootdee O, Pathanasophon P. 2003. Pasteurella multocida-associated sinusitis in khaki Campbell ducks (Anas platyrhynchos). Avian Dis. 47:649–655 [DOI] [PubMed] [Google Scholar]
- 230. Gustafson CR, Cooper GL, Charlton BR, Bickford AA. 1998. Pasteurella multocida infection involving cranial air spaces in White Leghorn chickens. Avian Dis. 42:413–417 [PubMed] [Google Scholar]
- 231. Mbuthia PG, Christensen H, Boye M, Petersen KM, Bisgaard M, Nyaga PN, Olsen JE. 2001. Specific detection of Pasteurella multocida in chickens with fowl cholera and in pig lung tissues using fluorescent rRNA in situ hybridization. J. Clin. Microbiol. 39:2627–2633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232. Bisgaard M. 1995. Salpingitis in web-footed birds: prevalence, aetiology and significance. Avian Pathol. 24:443–452 [DOI] [PubMed] [Google Scholar]
- 233. Wilkie IW, Harper M, Boyce JD, Adler B. 2012. Pasteurella multocida: diseases and pathogenesis. Curr. Top. Microbiol. Immunol. 361:1–22 [DOI] [PubMed] [Google Scholar]
- 234. Abrahamian FM, Goldstein EJ. 2011. Microbiology of animal bite wound infections. Clin. Microbiol. Rev. 24:231–246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235. Felix M, Tallon P, Salavert M, Navarro V, Breton JR, Perez-Belles C, Gobernado M. 2003. Bacteremia due to Pasteurella spp.: a rare process in our hospital over the last 8 years. Enferm. Infecc. Microbiol. Clin. 21:334–339 [DOI] [PubMed] [Google Scholar]
- 236. Mayr B. 1993. Pets as permanent excretors of zoonoses pathogens. Int. J. Hyg. Environ. Med. 194:214–222 [PubMed] [Google Scholar]
- 237. Nelson JD. 1983. Diseases acquired from pets. Pediatr. Infect. Dis. 2:S56–S60 [PubMed] [Google Scholar]
- 238. Rondon-Berrios H, Trevejo-Nunez GJ. 2010. Pets or pest: peritoneal dialysis-related peritonitis due to Pasteurella multocida. J. Microbiol. Immunol. Infect. 43:155–158 [DOI] [PubMed] [Google Scholar]
- 239. Donnio PY, Lerestif-Gautier AL, Avril JL. 2004. Characterization of Pasteurella spp. strains isolated from human infections. J. Comp. Pathol. 130:137–142 [DOI] [PubMed] [Google Scholar]
- 240. Mat O, Moenens F, Beauwens R, Rossi C, Muniz-Martinez MC, Mestrez F, Dhaene M. 2005. Indolent Pasteurella multocida peritonitis in a CCPD patient. 25 years of “cat-bite peritonitis”: a review. Perit. Dial. Int. 25:88–90 [PubMed] [Google Scholar]
- 241. Migliore E, Serraino C, Brignone C, Ferrigno D, Cardellicchio A, Pomero F, Castagna E, Osenda M, Fenoglio L. 2009. Pasteurella multocida infection in a cirrhotic patient: case report, microbiological aspects and a review of literature. Adv. Med. Sci. 54:109–112 [DOI] [PubMed] [Google Scholar]
- 242. Peeples E, Boswick JA, Jr, Scott FA. 1980. Wounds of the hand contaminated by human or animal saliva. J. Trauma 20:383–389 [PubMed] [Google Scholar]
- 243. Stefanopoulos PK, Tarantzopoulou AD. 2005. Facial bite wounds: management update. Int. J. Oral Maxillofac. Surg. 34:464–472 [DOI] [PubMed] [Google Scholar]
- 244. Tamaskar I, Ravakhah K. 2004. Spontaneous bacterial peritonitis with Pasteurella multocida in cirrhosis: case report and review of literature. South. Med. J. 97:1113–1115 [DOI] [PubMed] [Google Scholar]
- 245. Choudat D, Le Goff C, Delemotte B, Paul G, Mady V, Fages J, Conso F. 1987. Occupational exposure to animals and antibodies against Pasteurella multocida. Br. J. Ind. Med. 44:829–833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246. Biberstein EL, Jang SS, Kass PH, Hirsh DC. 1991. Distribution of indole-producing urease-negative Pasteurellas in animals. J. Vet. Diagn. Invest. 3:319–323 [DOI] [PubMed] [Google Scholar]
- 247. Holst E, Rollof J, Larsson L, Nielsen JP. 1992. Characterization and distribution of Pasteurella species recovered from infected humans. J. Clin. Microbiol. 30:2984–2987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248. Mohan K, Kelly PJ, Hill FW, Muvavarirwa P, Pawandiwa A. 1997. Phenotype and serotype of Pasteurella multocida isolates from diseases of dogs and cats in Zimbabwe. Comp. Immunol. Microbiol. Infect. Dis. 20:29–34 [DOI] [PubMed] [Google Scholar]
- 249. Hey P, Gow P, Torresi J, Testro A. 2012. Cirrhosis, cellulitis and cats: a ‘purrfect’ combination for life-threatening spontaneous bacterial peritonitis from Pasteurella multocida. BMJ Case Rep. 10.1136/bcr-2012-007397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250. Perez Garcia J, Candel Gonzalez FJ, Baos Munoz E, Gonzalez Romo F, Picazo JJ. 2009. Cellulitis after a cat bite. Rev. Espan. Quimioter. 22:221–223 [PubMed] [Google Scholar]
- 251. Fukuchi T, Morisawa Y. 2009. A case of cat-scratch-induced Pasteurella multocida infection presenting with disseminated intravascular coagulation and acute renal failure. J. Jpn. Assoc. Infect. Dis. 83:557–560 [DOI] [PubMed] [Google Scholar]
- 252. Brook I. 2009. Management of human and animal bite wound infection: an overview. Curr. Infect. Dis. Rep. 11:389–395 [DOI] [PubMed] [Google Scholar]
- 253. Cooke FJ, Kodjo A, Clutterbuck EJ, Bamford KB. 2004. A case of Pasteurella multocida peritoneal dialysis-associated peritonitis and review of the literature. Int. J. Infect. Dis. 8:171–174 [DOI] [PubMed] [Google Scholar]
- 254. Butt TS, Khan A, Ahmad A, Khan MA, Parke A, Hill DR. 1997. Pasteurella multocida infectious arthritis with acute gout after a cat bite. J. Rheumatol. 24:1649–1652 [PubMed] [Google Scholar]
- 255. Koch CA, Mabee CL, Robyn JA, Koletar SL, Metz EN. 1996. Exposure to domestic cats: risk factor for Pasteurella multocida peritonitis in liver cirrhosis? Am. J. Gastroenterol. 91:1447–1449 [PubMed] [Google Scholar]
- 256. Khan MF, Movahed MR, Jung J. 2012. Pasteurella multocida endocarditis. J. Heart Valve Dis. 21:260–262 [PubMed] [Google Scholar]
- 257. Drenjancevic IH, Ivic D, Drenjancevic D, Ivic J, Pelc B, Vukovic D. 2008. Fatal fulminant sepsis due to a cat bite in an immunocompromised patient. Wiener Klin. Wochenschr. 120:504–506 [DOI] [PubMed] [Google Scholar]
- 258. Yokose N, Dan K. 2007. Pasteurella multocida sepsis, due to a scratch from a pet cat, in a post-chemotherapy neutropenic patient with non-Hodgkin lymphoma. Int. J. Hematol. 85:146–148 [DOI] [PubMed] [Google Scholar]
- 259. Stiehl JB, Sterkin LA, Brummitt CF. 2004. Acute Pasteurella multocida in total knee arthroplasty. J. Arthroplasty 19:244–247 [DOI] [PubMed] [Google Scholar]
- 260. Ashley BD, Noone M, Dwarakanath AD, Malnick H. 2004. Fatal Pasteurella dagmatis peritonitis and septicaemia in a patient with cirrhosis: a case report and review of the literature. J. Clin. Pathol. 57:210–212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261. Schlichthaar H, Rohrer T, Schuster G, Lehnert H. 1995. Interstitial pneumonia and sepsis due to a Pasteurella multocida infection. Dtsch. Med. Wochenschr. 120:1582–1586 [DOI] [PubMed] [Google Scholar]
- 262. Morris JT, McAllister CK. 1992. Bacteremia due to Pasteurella multocida. South. Med. J. 85:442–443 [DOI] [PubMed] [Google Scholar]
- 263. Hombal SM, Dincsoy HP. 1992. Pasteurella multocida endocarditis. Am. J. Clin. Pathol. 98:565–568 [DOI] [PubMed] [Google Scholar]
- 264. Levin JM, Talan DA. 1990. Erythromycin failure with subsequent Pasteurella multocida meningitis and septic arthritis in a cat-bite victim. Ann. Emerg. Med. 19:1458–1461 [DOI] [PubMed] [Google Scholar]
- 265. Palutke WA, Boyd CB, Carter GR. 1973. Pasteurella multocida septicemia in a patient with cirrhosis. Report of a case. Am. J. Med. Sci. 266:305–308 [DOI] [PubMed] [Google Scholar]
- 266. Normann B, Nilehn B, Rajs J, Karlberg B. 1971. A fatal human case of Pasteurella multocida septicaemia after cat bite. Scand. J. Infect. Dis. 3:251–254 [DOI] [PubMed] [Google Scholar]
- 267. Guion TL, Sculco TP. 1992. Pasteurella multocida infection in total knee arthroplasty. Case report and literature review. J. Arthroplasty 7:157–160 [DOI] [PubMed] [Google Scholar]
- 268. Tan CC, Ti TY, Lee EJ. 1990. Pasteurella multocida osteomyelitis of the cervical spine in a patient on chronic haemodialysis. Singapore Med. J. 31:400–402 [PubMed] [Google Scholar]
- 269. Pestana OA. 1974. Mycotic aneurysm and osteomyelitis secondary to infection with Pasteurella multocida. Am. J. Clin. Pathol. 62:355–360 [DOI] [PubMed] [Google Scholar]
- 270. Naba MR, Araj GF, Kanafani ZA, Kanj SS. 2009. First case of Pasteurella multocida endocarditis of the tricuspid valve: a favorable outcome following medical treatment. Int. J. Infect. Dis. 13:e267–e269 [DOI] [PubMed] [Google Scholar]
- 271. Reinsch N, Plicht B, Lind A, Janosi RA, Buck T, Kamler M, Jakob H, Naber CK, Erbel R. 2008. Recurrent infective endocarditis with uncommon Gram-negative Pasteurella multocida and Pseudomonas aeruginosa: a case report. J. Heart Valve Dis. 17:710–713 [PubMed] [Google Scholar]
- 272. Graf S, Binder T, Heger M, Apfalter P, Simon N, Winkler S. 2007. Isolated endocarditis of the pulmonary valve caused by Pasteurella multocida. Infection 35:43–45 [DOI] [PubMed] [Google Scholar]
- 273. Al-Ghonaim MA, Abba AA, Al-Nozha M. 2006. Endocarditis caused by Pasteurella multocida. Ann. Saudi Med. 26:147–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274. Camou F, Guisset O, Pereyre S, Gabinski C, Viallard JF, Mercie P, Pellegrin JL. 2005. Endocarditis due to Pasteurella sp. Two cases. Med. Malad. Infect. 35:556–559 [DOI] [PubMed] [Google Scholar]
- 275. Fayad G, Modine T, Mokhtari S, Legout L, Decoene C, Azzaoui R, Al-Ruzzeh S, Naja G, Larrue B, Lecomte F, Senneville E, Warembourg H. 2003. Pasteurella multocida aortic valve endocarditis: case report and literature review. J. Heart Valve Dis. 12:261–263 [PubMed] [Google Scholar]
- 276. Fukumoto Y, Moriyama Y, Iguro Y, Toda R, Taira A. 2002. Pasteurella multocida endocarditis: report of a case. Surg. Today 32:513–515 [DOI] [PubMed] [Google Scholar]
- 277. Vasquez JE, Ferguson DA, Jr, Bin-Sagheer S, Myers JW, Ramsak A, Wilson MA, Sarubbi FA. 1998. Pasteurella multocida endocarditis: a molecular epidemiological study. Clin. Infect. Dis. 26:518–520 [DOI] [PubMed] [Google Scholar]
- 278. Elsaghier AA, Kibbler CC, Hamilton-Miller JM. 1998. Pasteurella multocida as an infectious cause of endocarditis. Clin. Infect. Dis. 27:410–411 [DOI] [PubMed] [Google Scholar]
- 279. Nettles RE, Sexton DJ. 1997. Pasteurella multocida prosthetic valve endocarditis: case report and review. Clin. Infect. Dis. 25:920–921 [DOI] [PubMed] [Google Scholar]
- 280. Genne D, Siegrist HH, Monnier P, Nobel M, Humair L, de Torrente A. 1996. Pasteurella multocida endocarditis: report of a case and review of the literature. Scand. J. Infect. Dis. 28:95–97 [DOI] [PubMed] [Google Scholar]
- 281. Thamlikitkul V, Sangruchi T. 1990. Pasteurella multocida infective endocarditis: a case report. J. Med. Assoc. Thai. 73:704–706 [PubMed] [Google Scholar]
- 282. Salmon D, Fantin B, Bricaire F, Vilde JL, Pangon B, Ferand D. 1989. Endocarditis due to Pasteurella multocida with glomerulonephritis. Am. J. Med. 86:493. [DOI] [PubMed] [Google Scholar]
- 283. Singh CP, Spurrell JR. 1983. Pasteurella multocida endocarditis. Br. Med. J. 286:1862–1863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284. Guerain JM, Segrestaa JM, Lamotte M. 1980. Pasteurella multocida endocarditis. Nouv. Presse Med. 9:2735–2736 [PubMed] [Google Scholar]
- 285. Lehmann V, Knutsen SB, Ragnhildstveit E, Skagseth E, Solberg CO. 1977. Endocarditis caused by Pasteurella multocida. Scand. J. Infect. Dis. 9:247–248 [DOI] [PubMed] [Google Scholar]
- 286. Spadafora R, Pomero G, Delogu A, Gozzoli L, Gancia P. 2011. A rare case of neonatal sepsis/meningitis caused by Pasteurella multocida complicated with status epilepticus and focal cerebritis. Pediatr. Med. Chir. 33:199–202 [PubMed] [Google Scholar]
- 287. Per H, Kumandas S, Gumus H, Ozturk MK, Coskun A. 2010. Meningitis and subgaleal, subdural, epidural empyema due to Pasteurella multocida. J. Emerg. Med. 39:35–38 [DOI] [PubMed] [Google Scholar]
- 288. Kobayaa H, Souki RR, Trust S, Domachowske JB. 2009. Pasteurella multocida meningitis in newborns after incidental animal exposure. Pediatr. Infect. Dis. J. 28:928–929 [DOI] [PubMed] [Google Scholar]
- 289. Green BT, Ramsey KM, Nolan PE. 2002. Pasteurella multocida meningitis: case report and review of the last 11 y. Scand. J. Infect. Dis. 34:213–217 [DOI] [PubMed] [Google Scholar]
- 290. Guerin JM, Mofredj A, Raskine L, Leibinger F. 1994. Septicemia and purulent meningitis caused by Pasteurella multocida in a HIV positive patient. Presse Med. 23:631. [PubMed] [Google Scholar]
- 291. Hillery S, Reiss-Levy EA, Browne C, Au T, Lemmon J. 1993. Pasteurella multocida meningitis in a two-day old neonate. Scand. J. Infect. Dis. 25:655–658 [DOI] [PubMed] [Google Scholar]
- 292. Levy CE, Irino K, Funayama CR, Moura-Ribeiro MV. 1989. Meningoencephalitis due to Pasteurella multocida: clinico-laboratory study of a case in an infant. Arq. Neuropsiquiatr. 47:468–470 [DOI] [PubMed] [Google Scholar]
- 293. Steinbok P, Flodmark O, Scheifele DW. 1985. Animal bites causing central nervous system injury in children. A report of three cases. Pediatr. Neurosci. 12:96–100 [DOI] [PubMed] [Google Scholar]
- 294. Avril JL, Donnio PY. 1987. Characterization of Pasteurella species isolated from man. Pathol. Biol. (Paris) 35:169–172 [PubMed] [Google Scholar]
- 295. Beyt BE, Jr, Sondag J, Roosevelt TS, Bruce R. 1979. Human pulmonary pasteurellosis. JAMA 242:1647–1648 [PubMed] [Google Scholar]
- 296. Chen HI, Hulten K, Clarridge JE., III 2002. Taxonomic subgroups of Pasteurella multocida correlate with clinical presentation. J. Clin. Microbiol. 40:3438–3441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297. Myers EM, Ward SL, Myers JP. 2012. Life-threatening respiratory pasteurellosis associated with palliative pet care. Clin. Infect. Dis. 54:e55–e57 [DOI] [PubMed] [Google Scholar]
- 298. Freshwater A. 2008. Why your housecat's trite little bite could cause you quite a fright: a study of domestic felines on the occurrence and antibiotic susceptibility of Pasteurella multocida. Zoonoses Public Health 55:507–513 [DOI] [PubMed] [Google Scholar]
- 299. Hutcheson KA, Magbalon M. 1999. Periocular abscess and cellulitis from Pasteurella multocida in a healthy child. Am. J. Ophthalmol. 128:514–515 [DOI] [PubMed] [Google Scholar]
- 300. Joh J, Padmanabhan R, Bastani B. 1998. Pasteurella multocida peritonitis following cat bite of peritoneal dialysis tubing. With a brief review of the literature. Am. J. Nephrol. 18:258–259 [DOI] [PubMed] [Google Scholar]
- 301. Love DN, Malik R, Norris JM. 2000. Bacteriological warfare amongst cats: what have we learned about cat bite infections? Vet. Microbiol. 74:179–193 [DOI] [PubMed] [Google Scholar]
- 302. Luchansky M, Bergman M, Djaldetti R, Salman H. 2003. Cat bite in an old patient: is it a simple injury? Eur. J. Emerg. Med. 10:130–132 [DOI] [PubMed] [Google Scholar]
- 303. Mayo RR, Lipschutz D. 1996. An interesting case of failed renal transplant complicated by a lymphocele infected with Pasteurella multocida and a review of the literature. Am. J. Nephrol. 16:361–366 [DOI] [PubMed] [Google Scholar]
- 304. Paul RV, Rostand SG. 1987. Cat-bite peritonitis: Pasteurella multocida peritonitis following feline contamination of peritoneal dialysis tubing. Am. J. Kidney Diseases. 10:318–319 [DOI] [PubMed] [Google Scholar]
- 305. Campos A, Taylor JH, Campbell M. 2000. Hamster bite peritonitis: Pasteurella pneumotropica peritonitis in a dialysis patient. Pediatr. Nephrol. 15:31–32 [DOI] [PubMed] [Google Scholar]
- 306. Yefet E, Abozaid S, Nasser W, Peretz A, Zarfin Y. 2011. Unusual infection-Pasteurella canis bacteremia in a child after exposure to rabbit secretions. Harefuah 150:13–70 [PubMed] [Google Scholar]
- 307. Henderson SR, Shah A, Banford KB, Howard LS. 2010. Pig trotters lung—novel domestic transmission of Pasteurella multocida. Clin. Med. 10:517–518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308. Lion C, Conroy MC, Dupuy ML, Escande F. 1995. Pasteurella “SP” group infection after a guinea pig bite. Lancet 346:901–902 [DOI] [PubMed] [Google Scholar]
- 309. Fleisher GR. 1999. The management of bite wounds. N. Engl. J. Med. 340:138–140 [DOI] [PubMed] [Google Scholar]
- 310. Koch CA, Robyn JA. 1998. Risk of animal contact in immunocompromised hosts. Arch. Intern. Med. 158:1036. [DOI] [PubMed] [Google Scholar]
- 311. Baud D, Bizzini A, Jaton K, Achtari C, Prod'hom G, Greub G. 2012. Pasteurella multocida zoonotic ascending infection: an unusual cause of tubo-ovarian abscess. Vector Borne Zoonotic Dis. 12:84–85 [DOI] [PubMed] [Google Scholar]
- 312. Bilbao Garay J, Zapatero Gaviria A, Perea Lopez B, Lopez Jimenez M, Ruiz Galiana J. 1997. Spontaneous peritonitis in a cirrhotic patient with a cat: Pasteurella multocida infection of the ascitic fluid. Rev. Espan. Enferm. Dig. 89:786–789 [PubMed] [Google Scholar]
- 313. Breen D, Schonell M, Au T, Reiss-Levy E. 2000. Pasteurella multocida: a case report of bacteremic pneumonia and 10-year laboratory review. Pathology 32:152–153 [DOI] [PubMed] [Google Scholar]
- 314. Brivet F, Guibert M, Barthelemy P, Lepicard A, Naveau S, Dormont J. 1994. Pasteurella multocida sepsis after hemorrhagic shock in a cirrhotic patient: possible role of endoscopic procedures and gastrointestinal translocation. Clin. Infect. Dis. 18:842–843 [DOI] [PubMed] [Google Scholar]
- 315. Elsey RM, Carson RW, DuBose TD., Jr 1991. Pasteurella multocida peritonitis in an HIV-positive patient on continuous cycling peritoneal dialysis. Am. J. Nephrol. 11:61–63 [DOI] [PubMed] [Google Scholar]
- 316. Espinosa MD, Nogueras F, Garcia Montero M, Martin-Vivaldi R. 1996. Pasteurella multocida as a cause of spontaneous bacterial peritonitis in a cirrhotic patient. Rev. Espan. Enferm. Dig. 88:644–645 [PubMed] [Google Scholar]
- 317. Fernandez-Esparrach G, Mascaro J, Rota R, Valerio L. 1994. Septicemia, peritonitis, and empyema due to Pasteurella multocida in a cirrhotic patient. Clin. Infect. Dis. 18:486. [DOI] [PubMed] [Google Scholar]
- 318. Frankel AH, Cassidy MJ. 1991. Pasteurella multocida peritonitis in CAPD: beware of the cats. Perit. Dial. Int. 11:184–185 [PubMed] [Google Scholar]
- 319. Furie RA, Cohen RP, Hartman BJ, Roberts RB. 1980. Pasteurella multocida infection; report in urban setting and review of spectrum of human disease. N. Y. State J. Med. 80:1597–1602 [PubMed] [Google Scholar]
- 320. Glickman M, Klein RS. 1997. Acute epiglottitis due to Pasteurella multocida in an adult without animal exposure. Emerg. Infect. Dis. 3:408–409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321. Honberg PZ, Frederiksen W. 1986. Isolation of Pasteurella multocida in a patient with spontaneous peritonitis and liver cirrhosis. Eur. J. Clin. Microbiol. 5:340–342 [DOI] [PubMed] [Google Scholar]
- 322. Jacobson JA, Miner P, Duffy O. 1977. Pasteurella multocida bacteremia associated with peritonitis and cirrhosis. Am. J. Gastroenterol. 68:489–491 [PubMed] [Google Scholar]
- 323. Kam WK, Haverkos HW, Rodman HM, Schmeltz R, Van Thiel DH. 1980. Human pasteurellosis: The first reported case of Pasteurella multocida septicemia and peritonitis during pregnancy. Am. J. Obstet. Gynecol. 138:351–352 [DOI] [PubMed] [Google Scholar]
- 324. Kitching AR, Macdonald A, Hatfield PJ. 1996. Pasteurella multocida infection in continuous ambulatory peritoneal dialysis. N. Z. Med. J. 109:59. [PubMed] [Google Scholar]
- 325. Loghman-Adham M. 1997. Pasteurella multocida peritonitis in patients undergoing peritoneal dialysis. Pediatr. Nephrol. 11:353–354 [DOI] [PubMed] [Google Scholar]
- 326. London RD, Bottone EJ. 1991. Pasteurella multocida: zoonotic cause of peritonitis in a patient undergoing peritoneal dialysis. Am. J. Med. 91:202–204 [DOI] [PubMed] [Google Scholar]
- 327. Musio F, Tiu A. 1998. Pasteurella multocida peritonitis in peritoneal dialysis. Clin. Nephrol. 49:258–261 [PubMed] [Google Scholar]
- 328. Navarro V, Ferreruela R, Berbegal J, Lopez-Benito I. 1994. Spontaneous primary peritonitis due to Pasteurella multocida. Ann. Med. Interna. 11:297–298 [PubMed] [Google Scholar]
- 329. Patton F, Dumas M, Cannon NJ. 1980. Pasteurella multocida septicemia and peritonitis in a cirrhotic cock trainer with a pet pig. N. Engl. J. Med. 303:1126–1127 [PubMed] [Google Scholar]
- 330. Purcell JJ, Jr, Krachmer JH. 1977. Corneal ulcer caused by Pasteurella multocida. Am. J. Ophthalmol. 83:540–542 [DOI] [PubMed] [Google Scholar]
- 331. Quentin R, Fignon A, Lansac J, Goudeau A. 1991. Pasteurella multocida and female genital carcinoma; a case report to dispute the concept of genital opportunistic pathogen. Eur. J. Obstet. Gynecol. Reprod. Biol. 41:243–244 [DOI] [PubMed] [Google Scholar]
- 332. Raffi F, David A, Mouzard A, Le Neel JC, Baron D, Courtieu AL. 1986. Pasteurella multocida appendiceal peritonitis: report of three cases and review of the literature. Pediatr. Infect. Dis. 5:695–698 [PubMed] [Google Scholar]
- 333. Rollof J, Johansson PJ, Holst E. 1992. Severe Pasteurella multocida infections in pregnant women. Scand. J. Infect. Dis. 24:453–456 [DOI] [PubMed] [Google Scholar]
- 334. Strand CL, Helfman L. 1971. Pasteurella multocida chorioamnionitis associated with premature delivery and neonatal ssepsis and death. Am. J. Clin. Pathol. 55:713–716 [DOI] [PubMed] [Google Scholar]
- 335. Szpak CA, Woodard BH, White JO, Zwadyk P. 1980. Bacterial peritonitis and bacteremia associated with Pasteurella multocida. South. Med. J. 73:801–803 [DOI] [PubMed] [Google Scholar]
- 336. Uribarri J, Bottone EJ, London RD. 1996. Pasteurella multocida peritonitis: are peritoneal dialysis patients on cyclers at increased risk? Perit. Dial. Int. 16:648–649 [PubMed] [Google Scholar]
- 337. Vakil N, Adiyody J, Treser G, Lue Y. 1985. Pasteurella multocida septicemia and peritonitis in a patient with cirrhosis: case report and review of the literature. Am. J. Gastroenterol. 80:565–568 [PubMed] [Google Scholar]
- 338. Waghorn DJ, Robson M. 2003. Occupational risk of Pasteurella multocida septicaemia and premature labour in a pregnant vet. Int. J. Obstet. Gynaecol. 110:780–781 [PubMed] [Google Scholar]
- 339. Wong GP, Cimolai N, Dimmick JE, Martin TR. 1992. Pasteurella multocida chorioamnionitis from vaginal transmission. Acta Obstet. Gynecol. Scand. 71:384–387 [DOI] [PubMed] [Google Scholar]
- 340. Best EJ, Lahra MM, Palasanthiran P. 2005. An unusual neonatal zoonosis. Med. J. Aust. 182:137. [DOI] [PubMed] [Google Scholar]
- 341. Zaramella P, Zamorani E, Freato F, Cattai M, Meloni GA. 1999. Neonatal meningitis due to a vertical transmission of Pasteurella multocida. Pediatr. Int. 41:307–310 [DOI] [PubMed] [Google Scholar]
- 342. Perrin I, Blanc P, Karam T, Carbajal R. 2003. Meningitis and osteitis caused by Pasteurella multocida in a three-month-old infant. Arch. Pediatr. 10:439–441 [DOI] [PubMed] [Google Scholar]
- 343. Guillet C, Join-Lambert O, Carbonnelle E, Ferroni A, Vachee A. 2007. Pasteurella multocida sepsis and meningitis in 2-month-old twin infants after household exposure to a slaughtered sheep. Clin. Infect. Dis. 45:e80–e81 [DOI] [PubMed] [Google Scholar]
- 344. Siahanidou T, Gika G, Skiathitou AV, Oikonomopoulos T, Alexandrou-Athanassoulis H, Koutouzis EI, Syriopoulou VP. 2012. Pasteurella multocida infection in a neonate: evidence for a human-to-human horizontal transmission. Pediat. Infect. Dis. J. 31:536–537 [DOI] [PubMed] [Google Scholar]
- 345. Tezer Tekae AY, Kalkan IH, Mert Dina B, Onder FO, Etik DO, Suvak B, Akdogan M. 2012. A catastrophic event caused by Pasteurella multocida in an alcoholic cirrhotic patient. Acta Gastroenterol. Belg. 75:64. [PubMed] [Google Scholar]
- 346. Tekce AY, Kalkan IH, Ding BM, Onder FO, Etik DO, Suvak B, Akdogan M. 2012. A catastrophic event caused by Pasteurella multocida in an alcoholic cirrhotic patient. Acta Gastroenterol. Belg. 75:366. [PubMed] [Google Scholar]
- 347. Laupland KB, Rimmer KP, Gregson DB, Megran DW. 2003. Spontaneous empyema and overwhelming septic shock due to Pasteurella multocida. Scand. J. Infect. Dis. 35:132–133 [DOI] [PubMed] [Google Scholar]
- 348. Tseng HK, Su SC, Liu CP, Lee CM. 2001. Pasteurella multocida bacteremia due to non-bite animal exposure in cirrhotic patients: report of two cases. J. Microbiol. Immunol. Infect. 34:293–296 [PubMed] [Google Scholar]
- 349. Hazouard E, Ferrandiere M, Lanotte P, Le Marcis L, Cattier B, Ginies G. 2000. Septic shock caused by Pasteurella multocida in alcoholic patients. Probable contamination of leg ulcers by the saliva of the domestic cats. Presse Medicale 29:1455–1457 [PubMed] [Google Scholar]
- 350. Shimizu T, Hasegawa K, Mitsuhashi Y, Kojima S, Ishikawa K, Hayashi N, Sawada T. 1995. A case of Pasteurella multocida subsp. multocida septicemia due to cat bites in liver cirrhosis patient. Jpn. Assoc. Infect. Dis. 69:1302–1306 [DOI] [PubMed] [Google Scholar]
- 351. Di Martino V, Cadranel JF, Chosidow O, Rogeaux O, Herson S. 1994. Pasteurella multocida septicemia and infections of ascitic fluid in patients with liver cirrhosis. Ann. Med. Int. (Paris) 145:441–444 [PubMed] [Google Scholar]
- 352. Di Martino V, Cadranel JF, Chosidow O, Heym B, Rogeaux O, Khosrovani C, Herson S, Bousquet O. 1994. Pasteurella multocida septicemia in a patient with liver cirrhosis. Ann. Med. Int. (Paris) 145:445–446 [PubMed] [Google Scholar]
- 353. Iseni MC, Desaint B, Guivarch P, Florent C, Levy VG. 1988. A rare etiology of ascitic fluid infection in cirrhosis: Pasteurella multocida. Gastroenterol. Clin. Biol. 12:294. [PubMed] [Google Scholar]
- 354. Raffi F, Barrier J, Baron D, Drugeon HB, Nicolas F, Courtieu AL. 1987. Pasteurella multocida bacteremia: report of thirteen cases over twelve years and review of the literature. Scand. J. Infect. Dis. 19:385–393 [DOI] [PubMed] [Google Scholar]
- 355. Nadler JP, Freedman MS, Berger SA. 1979. Pasteurella multocida septicemia. N. Y. State J. Med. 79:1581–1583 [PubMed] [Google Scholar]
- 356. Gerding DN, Khan MY, Ewing JW, Hall WH. 1976. Pasteurella multocida peritonitis in hepatic cirrhosis with ascites. Gastroenterology 70:413–415 [PubMed] [Google Scholar]
- 357. Heyworth MF, Stainforth JN, Wright R, Graham JM. 1975. Pasteurella multocida septicaemia associated with chronic liver disease. Br. Med. J. 4:733–734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358. Neumann A, Rohricht C. 1972. Septicemia caused by Pasteurella multocida in postnecrotic liver cirrhosis. Dtsch. Gesundheitsw. 27:2341–2343 [PubMed] [Google Scholar]
- 359. Yaneza AL, Jivan H, Kumari P, Togoo MS. 1991. Pasteurella haemolytica endocarditis. J. Infect. 23:65–67 [DOI] [PubMed] [Google Scholar]
- 360. Antony SJ, Oglesby KA. 2007. Peritonitis associated with Pasteurella multocida in peritoneal dialysis patients—case report and review of the literature. Clin. Nephrol. 68:52–56 [DOI] [PubMed] [Google Scholar]
- 361. Castellano I, Marin JP, Gallego S, Mora M, Rangel G, Suarez MA, Deira JL, Garcia-Bernalt V, Novillo R, Gomez-Martino JR. 2011. Pasteurella canis peritonitis in a peritoneal dialysis patient. Perit. Dial. Int. 31:503–504 [DOI] [PubMed] [Google Scholar]
- 362. Cortez JM, Imam AA, Ang JY. 2007. Pasteurella multocida urinary tract infection in a pediatric patient with end-stage renal disease. Pediatr. Infect. Dis. J. 26:183–185 [DOI] [PubMed] [Google Scholar]
- 363. Kanaan N, Gavage P, Janssens M, Avesani V, Gigi J, Goffin E. 2002. Pasteurella multocida in peritoneal dialysis: a rare cause of peritonitis associated with exposure to domestic cats. Acta Clin. Belg. 57:254–256 [DOI] [PubMed] [Google Scholar]
- 364. MacKay K, Brown L, Hudson F. 1997. Pasteurella multocida peritonitis in peritoneal dialysis patients: beware of the cat. Perit. Dial. Int. 17:608–610 [PubMed] [Google Scholar]
- 365. Mugambi SM, Ullian ME. 2010. Bacteremia, sepsis, and peritonitis with Pasteurella multocida in a peritoneal dialysis patient. Perit. Dial. Int. 30:381–383 [DOI] [PubMed] [Google Scholar]
- 366. Schmulewitz L, Chandesris MO, Mainardi JL, Poiree S, Viard JP, Lecuit M, Mamzer-Bruneel MF, Lortholary O. 2008. Invasive Pasteurella multocida sinusitis in a renal transplant patient. Transplant. Infect. Disease 10:206–208 [DOI] [PubMed] [Google Scholar]
- 367. Bernier C, Bouvard E, Saidi F, Parrot A, Meyniel D. 1999. Bacteremia and Pasteurella multocida pneumonia revealing HIV infection. Rev. Pneumol. Clin. 55:403–406 [PubMed] [Google Scholar]
- 368. Garavelli PL. 1997. Sepsis due to Pasteurella multocida in an HIV-positive patient. Recent Prog. Med. 88:226. [PubMed] [Google Scholar]
- 369. Raguin G, Guiot JD, Aerts J, Dehaye B, Desplaces N. 1993. Pasteurellosis in an HIV infected patient. Presse Med. 22:1366. [PubMed] [Google Scholar]
- 370. Tay L, Tey BH, Lim YS, Chew LS, Seng ST. 1992. Pasteurella multocida infection in Singapore. Trop. Geogr. Med. 44:359–361 [PubMed] [Google Scholar]
- 371. Anderson M, Utter P, Szatkowski J, Patrick T, Duncan W, Turner N, Dekutoski M. 2008. Cervical spine injury: tiger attack. Orthopedics 31:December. [PubMed] [Google Scholar]
- 372. Kadesky KM, Manarey C, Blair GK, Murphy JJ, III, Verchere C, Atkinson K. 1998. Cougar attacks on children: injury patterns and treatment. J. Pediatr. Surg. 33:863–865 [DOI] [PubMed] [Google Scholar]
- 373. McGeachie J. 1958. Isolation of Pasteurella septica from a lion-bite wound and lion's mouth. J. Pathol. Bacteriol. 75:467–470 [DOI] [PubMed] [Google Scholar]
- 374. Mellado E, Martin-Luengo F, Lopez-Egido A, Sanchez-Canizares MA, Aguilera A. 1990. Infection caused by Pasteurella multocida after a lion bite. Enferm. Infecc. Microbiol. Clin. 8:322–323 [PubMed] [Google Scholar]
- 375. Isotalo PA, Edgar D, Toye B. 2000. Polymicrobial tenosynovitis with Pasteurella multocida and other gram negative bacilli after a Siberian tiger bite. J. Clin. Pathol. 53:871–872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376. Silberfein EJ, Lin PH, Bush RL, Zhou W, Lumsden AB. 2006. Aortic endograft infection due to Pasteurella multocida following a rabbit bite. J. Vasc. Surg. 43:393–395 [DOI] [PubMed] [Google Scholar]
- 377. Wolfe ND, Dunavan CP, Diamond J. 2007. Origins of major human infectious diseases. Nature 447:279–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378. Broome CV. 1987. Epidemiology of Haemophilus influenzae type b infections in the United States. Pediatr. Infect. Dis. J. 6:779–782 [DOI] [PubMed] [Google Scholar]
- 379. Agrawal A, Murphy TF. 2011. Haemophilus influenzae infections in the H. influenzae type b conjugate vaccine era. J. Clin. Microbiol. 49:3728–3732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380. Albritton WL. 1982. Infections due to Haemophilus species other than H. influenzae. Annu. Rev. Microbiol. 36:199–216 [DOI] [PubMed] [Google Scholar]
- 381. Livorsi DJ, Macneil JR, Cohn AC, Bareta J, Zansky S, Petit S, Gershman K, Harrison LH, Lynfield R, Reingold A, Schaffner W, Thomas A, Farley MM. 2012. Invasive Haemophilus influenzae in the United States, 1999-2008: epidemiology and outcomes. J. Infect. 65:496–504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382. Strouts FR, Power P, Croucher NJ, Corton N, van Tonder A, Quail MA, Langford PR, Hudson MJ, Parkhill J, Kroll JS, Bentley SD. 2012. Lineage-specific virulence determinants of Haemophilus influenzae biogroup aegyptius. Emerg. Infect. Dis. 18:449–457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383. Harrison LH, Simonsen V, Waldman EA. 2008. Emergence and disappearance of a virulent clone of Haemophilus influenzae biogroup aegyptius, cause of Brazilian purpuric fever. Clin. Microbiol. Rev. 21:594–605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384. McCrea KW, Xie J, LaCross N, Patel M, Mukundan D, Murphy TF, Marrs CF, Gilsdorf JR. 2008. Relationships of nontypeable Haemophilus influenzae strains to hemolytic and nonhemolytic Haemophilus haemolyticus strains. J. Clin. Microbiol. 46:406–416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385. Murphy TF, Brauer AL, Sethi S, Kilian M, Cai X, Lesse AJ. 2007. Haemophilus haemolyticus: a human respiratory tract commensal to be distinguished from Haemophilus influenzae. J. Infect. Dis. 195:81–89 [DOI] [PubMed] [Google Scholar]
- 386. Anderson R, Wang X, Briere EC, Katz LS, Cohn AC, Clark TA, Messonnier NE, Mayer LW. 2012. Haemophilus haemolyticus isolates causing clinical disease. J. Clin. Microbiol. 50:2462–2465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387. Bong CT, Bauer ME, Spinola SM. 2002. Haemophilus ducreyi: clinical features, epidemiology, and prospects for disease control. Microbes Infect. 4:1141–1148 [DOI] [PubMed] [Google Scholar]
- 388. Morse SA. 1989. Chancroid and Haemophilus ducreyi. Clin. Microbiol. Rev. 2:137–157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389. Albritton WL. 1989. Biology of Haemophilus ducreyi. Microbiol. Rev. 53:377–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390. Janowicz DM, Ofner S, Katz BP, Spinola SM. 2009. Experimental infection of human volunteers with Haemophilus ducreyi: fifteen years of clinical data and experience. J. Infect. Dis. 199:1671–1679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391. Friis-Moller A, Christensen JJ, Fussing V, Hesselbjerg A, Christiansen J, Bruun B. 2001. Clinical significance and taxonomy of Actinobacillus hominis. J. Clin. Microbiol. 39:930–935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392. de Castro N, Pavie J, Lagrange-Xelot M, Bouvry D, Delisle F, Parrot A, Molina JM. 2007. Severe Actinobacillus ureae meningitis in an immunocompromised patient: report of one case and review of the literature. Scand. J. Infect. Dis. 39:1076–1079 [DOI] [PubMed] [Google Scholar]
- 393. Kingsland RC, Guss DA. 1995. Actinobacillus ureae meningitis: case report and review of the literature. J. Emerg. Med. 13:623–627 [DOI] [PubMed] [Google Scholar]
- 394. Kaka S, Lunz R, Klugman KP. 1994. Actinobacillus (Pasteurella) ureae meningitis in a HIV-positive patient. Diagn. Microbiol. Infect. Dis. 20:105–107 [DOI] [PubMed] [Google Scholar]
- 395. Kaur PP, Derk CT, Chatterji M, Dehoratius RJ. 2004. Septic arthritis caused by Actinobacillus ureae in a patient with rheumatoid arthritis receiving anti-tumor necrosis factor-alpha therapy. J. Rheumatol. 31:1663–1665 [PubMed] [Google Scholar]
- 396. Henderson B, Ward JM, Ready D. 2010. Aggregatibacter (Actinobacillus) actinomycetemcomitans: a triple A* periodontopathogen? Periodontology 2000 54:78–105 [DOI] [PubMed] [Google Scholar]
- 397. Paturel L, Casalta JP, Habib G, Nezri M, Raoult D. 2004. Actinobacillus actinomycetemcomitans endocarditis. Clin. Microbiol. Infect. 10:98–118 [DOI] [PubMed] [Google Scholar]
- 398. Rahamat-Langendoen JC, van Vonderen MG, Engstrom LJ, Manson WL, van Winkelhoff AJ, Mooi-Kokenberg EA. 2011. Brain abscess associated with Aggregatibacter actinomycetemcomitans: case report and review of literature. J. Clin. Periodontol. 38:702–706 [DOI] [PubMed] [Google Scholar]
- 399. Kachlany SC. 2010. Aggregatibacter actinomycetemcomitans leukotoxin: from threat to therapy. J. Dent. Res. 89:561–570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400. Damek-Poprawa M, Korostoff J, Gill R, Dirienzo JM. 2013. Cell junction remodeling in gingival tissue exposed to a microbial toxin. J. Dent. Res. 92:518–523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401. Damek-Poprawa M, Jang JY, Volgina A, Korostoff J, DiRienzo JM. 2012. Localization of Aggregatibacter actinomycetemcomitans cytolethal distending toxin subunits during intoxication of live cells. Infect. Immun. 80:2761–2770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402. Huang ST, Lee HC, Lee NY, Liu KH, Ko WC. 2005. Clinical characteristics of invasive Haemophilus aphrophilus infections. J. Microbiol. Immunol. Infect. 38:271–276 [PubMed] [Google Scholar]
- 403. Di Bonaventura MP, DeSalle R, Pop M, Nagarajan N, Figurski DH, Fine DH, Kaplan JB, Planet PJ. 2009. Complete genome sequence of Aggregatibacter (Haemophilus) aphrophilus NJ8700. J. Bacteriol. 191:4693–4694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404. Boyce JD, Adler B. 2006. How does Pasteurella multocida respond to the host environment? Curr. Opin. Microbiol. 9:117–122 [DOI] [PubMed] [Google Scholar]
- 405. Rimler RB, Rhoades KR. 1994. Hyaluronidase and chondroitinase activity of Pasteurella multocida serotype B:2 involved in hemorrhagic septicaemia. Vet. Rec. 134:67–68 [DOI] [PubMed] [Google Scholar]
- 406. Carter GR, Chengappa MM. 1980. Hyaluronidase production by type B Pasteurella multocida from cases of hemorrhagic septicemia. J. Clin. Microbiol. 11:94–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407. Straus DC, Purdy CW, Loan RW, Briggs RF, Frank GH. 1998. In vivo production of neuraminidase by Pasteurella haemolytica in market stressed cattle after natural infection. Curr. Microbiol. 37:240–244 [DOI] [PubMed] [Google Scholar]
- 408. Straus DC, Cooley JD, Purdy CW. 1996. In vivo production of neuraminidase by Pasteurella multocida A:3 in goats after transthoracic challenge. Curr. Microbiol. 33:266–269 [DOI] [PubMed] [Google Scholar]
- 409. Muller HE, Mannheim W. 1995. Occurrence of sialidase and N-acetylneuraminate lyase in Pasteurella species. Zentralbl. Bakteriol. Mikrobiol. Hyg. B 283:105–114 [DOI] [PubMed] [Google Scholar]
- 410. White DJ, Jolley WL, Purdy CW, Straus DC. 1995. Extracellular neuraminidase production by a Pasteurella multocida A:3 strain associated with bovine pneumonia. Infect. Immun. 63:1703–1709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411. Skaar EP. 2010. The battle for iron between bacterial pathogens and their vertebrate hosts. PLoS Pathog. 6:e1000949. 10.1371/journal.ppat.1000949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412. May BJ, Zhang Q, Li LL, Paustian ML, Whittam TS, Kapur V. 2001. Complete genomic sequence of Pasteurella multocida, Pm70. Proc. Natl. Acad. Sci. U. S. A. 98:3460–3465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413. Paustian ML, May BJ, Kapur V. 2001. Pasteurella multocida gene expression in response to iron limitation. Infect. Immun. 69:4109–4115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414. Paustian ML, May BJ, Kapur V. 2002. Transcriptional response of Pasteurella multocida to nutrient limitation. J. Bacteriol. 184:3734–3739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415. E-komon T, Burchmore R, Herzyk P, Davies R. 2012. Predicting the outer membrane proteome of Pasteurella multocida based on consensus prediction enhanced by results integration and manual confirmation. BMC Bioinformatics 13:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416. Hatfaludi T, Al-Hasani K, Gong L, Boyce JD, Ford M, Wilkie IW, Quinsey N, Dunstone MA, Hoke DE, Adler B. 2012. Screening of 71 P. multocida proteins for protective efficacy in a fowl cholera infection model and characterization of the protective antigen PlpE. PLoS One 7:e39973. 10.1371/journal.pone.0039973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417. Schryvers AB, Gonzalez GC. 1990. Receptors for transferrin in pathogenic bacteria are specific for the host's protein. Can. J. Microbiol. 36:145–147 [DOI] [PubMed] [Google Scholar]
- 418. Ogunnariwo JA, Schryvers AB. 1990. Iron acquisition in Pasteurella haemolytica: expression and identification of a bovine-specific transferrin receptor. Infect. Immun. 58:2091–2097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419. Ekins A, Bahrami F, Sijercic A, Maret D, Niven DF. 2004. Haemophilus somnus possesses two systems for acquisition of transferrin-bound iron. J. Bacteriol. 186:4407–4411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420. Rhodes ER, Tomaras AP, McGillivary G, Connerly PL, Actis LA. 2005. Genetic and functional analyses of the Actinobacillus actinomycetemcomitans AfeABCD siderophore-independent iron acquisition system. Infect. Immun. 73:3758–3763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421. Staudenmaier H, Van Hove B, Yaraghi Z, Braun V. 1989. Nucleotide sequences of the fecBCDE genes and locations of the proteins suggest a periplasmic-binding-protein-dependent transport mechanism for iron(III) dicitrate in Escherichia coli. J. Bacteriol. 171:2626–2633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422. Strange HR, Zola TA, Cornelissen CN. 2011. The fbpABC operon is required for Ton-independent utilization of xenosiderophores by Neisseria gonorrhoeae strain FA19. Infect. Immun. 79:267–278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423. Chin N, Frey J, Chang CF, Chang YF. 1996. Identification of a locus involved in the utilization of iron by Actinobacillus pleuropneumoniae. FEMS Microbiol. Lett. 143:1–6 [DOI] [PubMed] [Google Scholar]
- 424. Muhairwa AP, Christensen JP, Bisgaard M. 2002. Serum resistance of Pasteurella multocida in avian and porcine sera, and comparative virulence investigations of selected serum-sensitive and resistant strains in chickens. Avian Pathol. 31:183–191 [DOI] [PubMed] [Google Scholar]
- 425. Borrathybay E, Sawada T, Kataoka Y, Okiyama E, Kawamoto E, Amao H. 2003. Capsule thickness and amounts of a 39 kDa capsular protein of avian Pasteurella multocida type A strains correlate with their pathogenicity for chickens. Vet. Microbiol. 97:215–227 [DOI] [PubMed] [Google Scholar]
- 426. Boyce JD, Adler B. 2000. The capsule is a virulence determinant in the pathogenesis of Pasteurella multocida M1404 (B:2). Infect. Immun. 68:3463–3468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427. Boyce JD, Chung JY, Adler B. 2000. Pasteurella multocida capsule: composition, function and genetics. J. Biotechnol. 83:153–160 [DOI] [PubMed] [Google Scholar]
- 428. Carter GR, Annau E. 1953. Isolation of capsular polysaccharides from colonial variants of Pasteurella multocida. Am. J. Vet. Res. 14:475–478 [PubMed] [Google Scholar]
- 429. Maheswaran SK, Thies ES. 1979. Influence of encapsulation on phagocytosis of Pasteurella multocida by bovine neutrophils. Infect. Immun. 26:76–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430. Rimler RB. 1994. Presumptive identification of Pasteurella multocida serogroups A, D and F by capsule depolymerisation with mucopolysaccharidases. Vet. Rec. 134:191–192 [DOI] [PubMed] [Google Scholar]
- 431. DeAngelis PL, Padgett-McCue AJ. 2000. Identification and molecular cloning of a chondroitin synthase from Pasteurella multocida type F. J. Biol. Chem. 275:24124–24129 [DOI] [PubMed] [Google Scholar]
- 432. Steen JA, Harrison P, Seemann T, Wilkie I, Harper M, Adler B, Boyce JD. 2010. Fis is essential for capsule production in Pasteurella multocida and regulates expression of other important virulence factors. PLoS Pathog. 6:e1000750. 10.1371/journal.ppat.1000750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433. Hatfaludi T, Al-Hasani K, Boyce JD, Adler B. 2010. Outer membrane proteins of Pasteurella multocida. Vet. Microbiol. 144:1–17 [DOI] [PubMed] [Google Scholar]
- 434. Nazierbieke W, Yan F, He C, Zhang L, Borrathybay E. 2008. Expression and purification of an adhesive protein of rabbit Pasteurella multocida C51-3 and detection of its antigenicity. Chin. J. Biotechnol. 24:1446–1453 [PubMed] [Google Scholar]
- 435. Dabo SM, Confer A, Montelongo M, York P, Wyckoff JH., III 2008. Vaccination with Pasteurella multocida recombinant OmpA induces strong but non-protective and deleterious Th2-type immune response in mice. Vaccine 26:4345–4351 [DOI] [PubMed] [Google Scholar]
- 436. Sthitmatee N, Numee S, Kawamoto E, Sasaki H, Yamashita K, Takahashi N, Kataoka Y, Sawada T. 2008. Protection of chickens from fowl cholera by vaccination with recombinant adhesive protein of Pasteurella multocida. Vaccine 26:2398–2407 [DOI] [PubMed] [Google Scholar]
- 437. Mullen LM, Nair SP, Ward JM, Rycroft AN, Williams RJ, Robertson G, Mordan NJ, Henderson B. 2008. Novel adhesin from Pasteurella multocida that binds to the integrin-binding fibronectin FnIII9-10 repeats. Infect. Immun. 76:1093–1104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438. Dabo SM, Confer AW, Hartson SD. 2005. Adherence of Pasteurella multocida to fibronectin. Vet. Microbiol. 110:265–275 [DOI] [PubMed] [Google Scholar]
- 439. Doughty SW, Ruffolo CG, Adler B. 2000. The type 4 fimbrial subunit gene of Pasteurella multocida. Vet. Microbiol. 72:79–90 [DOI] [PubMed] [Google Scholar]
- 440. Grund S, Schoss P, Thiesen B. 1990. Pasteurella multocida (type D and A) and atrophic rhinitis of swine—hemagglutination, fimbriae and adhesion in vitro in the nasal mucosa of swine fetuses. Berl. Munch. Tierarztl. Wochenschr. 103:365–371 [PubMed] [Google Scholar]
- 441. Chung WB, Collins MT, Backstrom LR. 1990. Adherence of Bordetella bronchiseptica and Pasteurella multocida to swine nasal ciliated epithelial cells in vitro. Acta Pathol. Microbiol. Immunol. Scand. 98:453–461 [PubMed] [Google Scholar]
- 442. Pijoan C, Trigo F. 1990. Bacterial adhesion to mucosal surfaces with special reference to Pasteurella multocida isolates from atrophic rhinitis. Can. J. Vet. Res. 54(Suppl):S16–S21 [PubMed] [Google Scholar]
- 443. Dabo SM, Confer AW, Quijano-Blas RA. 2003. Molecular and immunological characterization of Pasteurella multocida serotype A:3 OmpA: evidence of its role in P. multocida interaction with extracellular matrix molecules. Microb. Pathog. 35:147–157 [DOI] [PubMed] [Google Scholar]
- 444. Chevalier G, Duclohier H, Thomas D, Shechter E, Wroblewski H. 1993. Purification and characterization of protein H, the major porin of Pasteurella multocida. J. Bacteriol. 175:266–276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 445. Okay S, Ozcengiz E, Ozcengiz G. 2012. Immune responses against chimeric DNA and protein vaccines composed of PlpEN-OmpH and PlpEC-OmpH from Pasteurella multocida A:3 in mice. Acta Microbiol. Immunol. Hung. 59:485–498 [DOI] [PubMed] [Google Scholar]
- 446. Wu JR, Shien JH, Shieh HK, Chen CF, Chang PC. 2007. Protective immunity conferred by recombinant Pasteurella multocida lipoprotein E (PlpE). Vaccine 25:4140–4148 [DOI] [PubMed] [Google Scholar]
- 447. Ruffolo CG, Adler B. 1996. Cloning, sequencing, expression, and protective capacity of the oma87 gene encoding the Pasteurella multocida 87-kilodalton outer membrane antigen. Infect. Immun. 64:3161–3167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 448. Ali HA, Sawada T, Noda K. 2004. Protectivity of an immunoaffinity-purified 39 kDa capsular protein of avian Pasteurella multocida in mice. J. Vet. Med. Sci. 66:1603–1604 [DOI] [PubMed] [Google Scholar]
- 449. Adler B, Bulach D, Chung J, Doughty S, Hunt M, Rajakumar K, Serrano M, van Zanden A, Zhang Y, Ruffolo C. 1999. Candidate vaccine antigens and genes in Pasteurella multocida. J. Biotechnol. 73:83–90 [DOI] [PubMed] [Google Scholar]
- 450. Ruffolo CG, Tennent JM, Michalski WP, Adler B. 1997. Identification, purification, and characterization of the type 4 fimbriae of Pasteurella multocida. Infect. Immun. 65:339–343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 451. Siju J, Kumar AA, Shivachandra SB, Chaudhuri P, Srivastava SK, Singh VP. 2007. Cloning and characterization of type 4 fimbrial gene (ptfA) of Pasteurella multocida serogroup B:2 (strain P52). Vet. Res. Commun. 31:397–404 [DOI] [PubMed] [Google Scholar]
- 452. Bucior I, Pielage JF, Engel JN. 2012. Pseudomonas aeruginosa pili and flagella mediate distinct binding and signaling events at the apical and basolateral surface of airway epithelium. PLoS Pathog. 8:e1002616. 10.1371/journal.ppat.1002616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 453. Wheeler R. 2009. Outer membrane proteomics of Pasteurella multocida isolates to identify putative host-specificity determinants. Biosci. Horiz. 2:1–12 [Google Scholar]
- 454. Ward CK, Lumbley SR, Latimer JL, Cope LD, Hansen EJ. 1998. Haemophilus ducreyi secretes a filamentous hemagglutinin-like protein. J. Bacteriol. 180:6013–6022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 455. Ward CK, Latimer JL, Nika J, Vakevainen M, Mock JR, Deng K, Blick RJ, Hansen EJ. 2003. Mutations in the lspA1 and lspA2 genes of Haemophilus ducreyi affect the virulence of this pathogen in an animal model system. Infect. Immun. 71:2478–2486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456. Blom J, Hansen GA, Poulsen FM. 1983. Morphology of cells and hemagglutinogens of Bordetella species: resolution of substructural units in fimbriae of Bordetella pertussis. Infect. Immun. 42:308–317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 457. Serra DO, Conover MS, Arnal L, Sloan GP, Rodriguez ME, Yantorno OM, Deora R. 2011. FHA-mediated cell-substrate and cell-cell adhesions are critical for Bordetella pertussis biofilm formation on abiotic surfaces and in the mouse nose and the trachea. PLoS One 6:e28811. 10.1371/journal.pone.0028811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458. Tatum FM, Yersin AG, Briggs RE. 2005. Construction and virulence of a Pasteurella multocida fhaB2 mutant in turkeys. Microb. Pathog. 39:9–17 [DOI] [PubMed] [Google Scholar]
- 459. Jacob-Dubuisson F, Kehoe B, Willery E, Reveneau N, Locht C, Relman DA. 2000. Molecular characterization of Bordetella bronchiseptica filamentous haemagglutinin and its secretion machinery. Microbiology 146:1211–1221 [DOI] [PubMed] [Google Scholar]
- 460. Sandal I, Inzana TJ. 2010. A genomic window into the virulence of Histophilus somni. Trends Microbiol. 18:90–99 [DOI] [PubMed] [Google Scholar]
- 461. Lax AJ, Chanter N. 1990. Cloning of the toxin gene from Pasteurella multocida and its role in atrophic rhinitis. J. Gen. Microbiol. 136:81–87 [DOI] [PubMed] [Google Scholar]
- 462. Petersen SK, Foged NT. 1989. Cloning and expression of the Pasteurella multocida toxin gene, toxA, in Escherichia coli. Infect. Immun. 57:3907–3913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 463. Pullinger GD, Bevir T, Lax AJ. 2004. The Pasteurella multocida toxin is encoded within a lysogenic bacteriophage. Mol. Microbiol. 51:255–269 [DOI] [PubMed] [Google Scholar]
- 464. Nakai T, Sawata A, Tsuji M, Samejima Y, Kume K. 1984. Purification of dermonecrotic toxin from a sonic extract of Pasteurella multocida SP-72 serotype D. Infect. Immun. 46:429–434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 465. Chanter N, Rutter JM, Mackenzie A. 1986. Partial purification of an osteolytic toxin from Pasteurella multocida. J. Gen. Microbiol. 132:1089–1097 [DOI] [PubMed] [Google Scholar]
- 466. Kimman TG, Lowik CW, van de Wee-Pals LJ, Thesingh CW, Defize P, Kamp EM, Bijvoet OL. 1987. Stimulation of bone resorption by inflamed nasal mucosa, dermonecrotic toxin-containing conditioned medium from Pasteurella multocida, and purified dermonecrotic toxin from P. multocida. Infect. Immun. 55:2110–2116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 467. Elling F, Pedersen KB, Hogh P, Foged NT. 1988. Characterization of the dermal lesions induced by a purified protein from toxigenic Pasteurella multocida. APMIS 96:50–55 [DOI] [PubMed] [Google Scholar]
- 468. Kamp EM, Kimman TG. 1988. Induction of nasal turbinate atrophy in germ-free pigs, using Pasteurella multocida as well as bacterium-free crude and purified dermonecrotic toxin of P. multocida. Am. J. Vet. Res. 49:1844–1849 [PubMed] [Google Scholar]
- 469. Kamps AM, Kamp EM, Smits MA. 1990. Cloning and expression of the dermonecrotic toxin gene of Pasteurella multocida ssp. multocida in Escherichia coli. FEMS Microbiol. Lett. 55:187–190 [DOI] [PubMed] [Google Scholar]
- 470. Chrisp CE, Foged NT. 1991. Induction of pneumonia in rabbits by use of a purified protein toxin from Pasteurella multocida. Am. J. Vet. Res. 52:56–61 [PubMed] [Google Scholar]
- 471. Kim TJ, Lee JI, Lee BJ. 2006. Development of a toxA gene knock-out mutant of Pasteurella multocida and evaluation of its protective effects. J. Microbiol. 44:320–326 [PubMed] [Google Scholar]
- 472. Cheville NF, Rimler RB, Thurston JR. 1988. A toxin from Pasteurella multocida type D causes acute hepatic necrosis in pigs. Vet. Pathol. 25:518–520 [DOI] [PubMed] [Google Scholar]
- 473. Nakai T, Sawata A, Tsuji M, Kume K. 1984. Characterization of dermonecrotic toxin produced by serotype D strains of Pasteurella multocida. Am. J. Vet. Res. 45:2410–2413 [PubMed] [Google Scholar]
- 474. van Diemen PM, de Vries Reilingh G, Parmentier HK. 1994. Immune responses of piglets to Pasteurella multocida toxin and toxoid. Vet. Immunol. Immunopathol. 41:307–321 [DOI] [PubMed] [Google Scholar]
- 475. van Diemen PM, de Vries Reilingh G, Parmentier HK. 1996. Effect of Pasteurella multocida toxin on in vivo immune responses in piglets. Vet. Q. 18:141–146 [DOI] [PubMed] [Google Scholar]
- 476. Gwaltney SM, Galvin RJ, Register KB, Rimler RB, Ackermann MR. 1997. Effects of Pasteurella multocida toxin on porcine bone marrow cell differentiation into osteoclasts and osteoblasts. Vet. Pathol. 34:421–430 [DOI] [PubMed] [Google Scholar]
- 477. Harmey D, Stenbeck G, Nobes CD, Lax AJ, Grigoriadis AE. 2004. Regulation of osteoblast differentiation by Pasteurella multocida toxin (PMT): a role for Rho GTPase in bone formation. J. Bone Miner. Res. 19:661–670 [DOI] [PubMed] [Google Scholar]
- 478. Jutras I, Martineau-Doize B. 1996. Stimulation of osteoclast-like cell formation by Pasteurella multocida toxin from hemopoietic progenitor cells in mouse bone marrow cultures. Can. J. Vet. Res. 60:34–39 [PMC free article] [PubMed] [Google Scholar]
- 479. Kimman TG, Kamp EM. 1986. Induced atrophic rhinitis in rats. Am. J. Vet. Res. 47:2426–2430 [PubMed] [Google Scholar]
- 480. Martineau-Doize B, Caya I, Gagne S, Jutras I, Dumas G. 1993. Effects of Pasteurella multocida toxin on the osteoclast population of the rat. J. Comp. Pathol. 108:81–91 [DOI] [PubMed] [Google Scholar]
- 481. Mullan PB, Lax AJ. 1996. Pasteurella multocida toxin is a mitogen for bone cells in primary culture. Infect. Immun. 64:959–965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 482. Sterner-Kock A, Lanske B, Uberschar S, Atkinson MJ. 1995. Effects of the Pasteurella multocida toxin on osteoblastic cells in vitro. Vet. Pathol. 32:274–279 [DOI] [PubMed] [Google Scholar]
- 483. Donnio PY, Avril JL, Andre PM, Vaucel J. 1991. Dermonecrotic toxin production by strains of Pasteurella multocida isolated from man. J. Med. Microbiol. 34:333–337 [DOI] [PubMed] [Google Scholar]
- 484. Wilson BA, Ho M. 2010. Recent insights into Pasteurella multocida toxin and other G-protein-modulating bacterial toxins. Future Microbiol. 5:1185–1201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 485. Wilson BA, Ho M. 2011. Cellular and molecular action of the mitogenic protein-deamidating toxin from Pasteurella multocida. FEBS J. 278:4616–4632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 486. Wilson BA, Ho M. 2012. Pasteurella multocida toxin interaction with host cells: entry and cellular effects. Curr. Top. Microbiol. Immunol. 361:93–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 487. Orth JH, Aktories K. 2012. Molecular biology of Pasteurella multocida toxin. Curr. Top. Microbiol. Immunol. 361:73–92 [DOI] [PubMed] [Google Scholar]
- 488. Orth JH, Preuss I, Fester I, Schlosser A, Wilson BA, Aktories K. 2009. Pasteurella multocida toxin activation of heterotrimeric G proteins by deamidation. Proc. Natl. Acad. Sci. U. S. A. 106:7179–7184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 489. Zywietz A, Gohla A, Schmelz M, Schultz G, Offermanns S. 2001. Pleiotropic effects of Pasteurella multocida toxin are mediated by Gq-dependent and -independent mechanisms. involvement of Gq but not G11. J. Biol. Chem. 276:3840–3845 [DOI] [PubMed] [Google Scholar]
- 490. Wilson BA, Zhu X, Ho M, Lu L. 1997. Pasteurella multocida toxin activates the inositol triphosphate signaling pathway in Xenopus oocytes via G(q)alpha-coupled phospholipase C-beta1. J. Biol. Chem. 272:1268–1275 [DOI] [PubMed] [Google Scholar]
- 491. Orth JH, Fester I, Siegert P, Weise M, Lanner U, Kamitani S, Tachibana T, Wilson BA, Schlosser A, Horiguchi Y, Aktories K. 2013. Substrate specificity of Pasteurella multocida toxin for alpha subunits of heterotrimeric G proteins. FASEB J. 27:832–842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 492. Orth JH, Aktories K. 2010. Pasteurella multocida toxin activates various heterotrimeric G proteins by deamidation. Toxins 2:205–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 493. Orth JH, Fester I, Preuss I, Agnoletto L, Wilson BA, Aktories K. 2008. Activation of Galpha (i) and subsequent uncoupling of receptor-Galpha (i) signaling by Pasteurella multocida toxin. J. Biol. Chem. 283:23288–23294 [DOI] [PubMed] [Google Scholar]
- 494. Orth JH, Lang S, Taniguchi M, Aktories K. 2005. Pasteurella multocida toxin-induced activation of RhoA is mediated via two families of Gα proteins, Gαq and Gα12/13. J. Biol. Chem. 280:36701–36707 [DOI] [PubMed] [Google Scholar]
- 495. Hildebrand D, Walker P, Dalpke A, Heeg K, Kubatzky KF. 2010. Pasteurella multocida Toxin-induced Pim-1 expression disrupts suppressor of cytokine signalling (SOCS)-1 activity. Cell. Microbiol. 12:1732–1745 [DOI] [PubMed] [Google Scholar]
- 496. Blocker D, Berod L, Fluhr JW, Orth J, Idzko M, Aktories K, Norgauer J. 2006. Pasteurella multocida toxin (PMT) activates RhoGTPases, induces actin polymerization and inhibits migration of human dendritic cells, but does not influence macropinocytosis. Int. Immunol. 18:459–464 [DOI] [PubMed] [Google Scholar]
- 497. Bagley KC, Abdelwahab SF, Tuskan RG, Lewis GK. 2005. Pasteurella multocida toxin activates human monocyte-derived and murine bone marrow-derived dendritic cells in vitro but suppresses antibody production in vivo. Infect. Immun. 73:413–421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 498. Jordan RW, Hamilton TD, Hayes CM, Patel D, Jones PH, Roe JM, Williams NA. 2003. Modulation of the humoral immune response of swine and mice mediated by toxigenic Pasteurella multocida. FEMS Immunol. Med. Microbiol. 39:51–59 [DOI] [PubMed] [Google Scholar]
- 499. Aminova LR, Wilson BA. 2007. Calcineurin-independent inhibition of 3T3-L1 adipogenesis by Pasteurella multocida toxin: suppression of Notch1, stabilization of beta-catenin and pre-adipocyte factor 1. Cell. Microbiol. 9:2485–2496 [DOI] [PubMed] [Google Scholar]
- 500. Bannai Y, Aminova LR, Faulkner MJ, Ho M, Wilson BA. 2012. Rho/ROCK-dependent inhibition of 3T3-L1 adipogenesis by G-protein-deamidating dermonecrotic toxins: differential regulation of Notch1, Pref1/Dlk1, and beta-catenin signaling. Front. Cell Infect. Microbiol. 2:80e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 501. Hildebrand D, Heeg K, Kubatzky KF. 2011. Pasteurella multocida toxin-stimulated osteoclast differentiation is B cell dependent. Infect. Immun. 79:220–228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 502. Lax AJ, Grigoriadis AE. 2001. Pasteurella multocida toxin: the mitogenic toxin that stimulates signalling cascades to regulate growth and differentiation. Int. J. Med. Microbiol. 291:261–268 [DOI] [PubMed] [Google Scholar]
- 503. Wilson BA, Aminova LR, Ponferrada VG, Ho M. 2000. Differential modulation and subsequent blockade of mitogenic signaling and cell cycle progression by Pasteurella multocida toxin. Infect. Immun. 68:4531–4538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 504. Orth JH, Aktories K, Kubatzky KF. 2007. Modulation of host cell gene expression through activation of STAT transcription factors by Pasteurella multocida toxin. J. Biol. Chem. 282:3050–3057 [DOI] [PubMed] [Google Scholar]
- 505. Preuss I, Hildebrand D, Orth JH, Aktories K, Kubatzky KF. 2010. Pasteurella multocida toxin is a potent activator of anti-apoptotic signalling pathways. Cell. Microbiol. 12:1174–1185 [DOI] [PubMed] [Google Scholar]
- 506. Oubrahim H, Wong A, Wilson BA, Chock PB. 2013. Mammalian target of rapamycin complex 1 (mTORC1) plays a role in Pasteurella multocida toxin (PMT)-induced protein synthesis and proliferation in Swiss 3T3 cells. J. Biol. Chem. 288:2805–2815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 507. Oubrahim H, Wong A, Wilson BA, Chock PB. 2013. Pasteurella multocida toxin (PMT) upregulates CTGF which leads to mTORC1 activation in Swiss 3T3 cells. Cell. Signal. 25:1136–1148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 508. Lax A. 2012. The Pasteurella multocida toxin: a new paradigm for the link between bacterial infection and cancer. Curr. Top. Microbiol. Immunol. 361:131–144 [DOI] [PubMed] [Google Scholar]
- 509. Lax AJ, Pullinger GD, Baldwin MR, Harmey D, Grigoriadis AE, Lakey JH. 2004. The pasteurella multocida toxin interacts with signalling pathways to perturb cell growth and differentiation. Int. J. Med. Microbiol. 293:505–512 [DOI] [PubMed] [Google Scholar]
- 510. Oswald E, Nougayrede JP, Taieb F, Sugai M. 2005. Bacterial toxins that modulate host cell-cycle progression. Curr. Opin. Microbiol. 8:83–91 [DOI] [PubMed] [Google Scholar]
- 511. Mell JC, Hall IM, Redfield RJ. 2012. Defining the DNA uptake specificity of naturally competent Haemophilus influenzae cells. Nucleic Acids Res. 40:8536–8549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 512. Jablonski L, Sriranganathan N, Boyle SM, Carter GR. 1992. Conditions for transformation of Pasteurella multocida by electroporation. Microb. Pathog. 12:63–68 [DOI] [PubMed] [Google Scholar]
- 513. Abdelhak D. 2009. Alternative method for genetic transformation of Pasteurella multocida X73 using a hyaluronidase-producing Staphylococcus aureus strain. J. Microbiol. Methods 78:25–27 [DOI] [PubMed] [Google Scholar]
- 514. Bills MM, Medd JM, Chappel RJ, Adler B. 1993. Construction of a shuttle vector for use between Pasteurella multocida and Escherichia coli. Plasmid 30:268–273 [DOI] [PubMed] [Google Scholar]
- 515. Lee MD, Henk AD. 1997. RSF1010-based shuttle vectors for cloning and expression in Pasteurella multocida. Vet. Microbiol. 54:369–374 [DOI] [PubMed] [Google Scholar]
- 516. DeAngelis PL. 1998. Transposon Tn916 insertional mutagenesis of Pasteurella multocida and direct sequencing of disruption site. Microb. Pathog. 24:203–209 [DOI] [PubMed] [Google Scholar]
- 517. San Millan A, Giufre M, Escudero JA, Hidalgo L, Gutierrez B, Cerquetti M, Gonzalez-Zorn B. 2011. Contribution of ROB-1 and PBP3 mutations to the resistance phenotype of a beta-lactamase-positive amoxicillin/clavulanic acid-resistant Haemophilus influenzae carrying plasmid pB1000 in Italy. J. Antimicrob. Chemother. 66:96–99 [DOI] [PubMed] [Google Scholar]
- 518. San Millan A, Escudero JA, Gutierrez B, Hidalgo L, Garcia N, Llagostera M, Dominguez L, Gonzalez-Zorn B. 2009. Multiresistance in Pasteurella multocida is mediated by coexistence of small plasmids. Antimicrob. Agents Chemother. 53:3399–3404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 519. Kehrenberg C, Wallmann J, Schwarz S. 2008. Molecular analysis of florfenicol-resistant Pasteurella multocida isolates in Germany. J. Antimicrob. Chemother. 62:951–955 [DOI] [PubMed] [Google Scholar]
- 520. Kehrenberg C, Catry B, Haesebrouck F, de Kruif A, Schwarz S. 2005. Novel spectinomycin/streptomycin resistance gene, aadA14, from Pasteurella multocida. Antimicrob. Agents Chemother. 49:3046–3049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 521. Kehrenberg C, Schwarz S. 2005. dfrA20, A novel trimethoprim resistance gene from Pasteurella multocida. Antimicrob. Agents Chemother. 49:414–417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 522. Wu JR, Shieh HK, Shien JH, Gong SR, Chang PC. 2003. Molecular characterization of plasmids with antimicrobial resistant genes in avian isolates of Pasteurella multocida. Avian Dis. 47:1384–1392 [DOI] [PubMed] [Google Scholar]
- 523. Kehrenberg C, Schwarz S. 2000. Identification of a truncated, but functionally active tet(H) tetracycline resistance gene in Pasteurella aerogenes and Pasteurella multocida. FEMS Microbiol. Lett. 188:191–195 [DOI] [PubMed] [Google Scholar]
- 524. Vassort-Bruneau C, Lesage-Descauses MC, Martel JL, Lafont JP, Chaslus-Dancla E. 1996. CAT III chloramphenicol resistance in Pasteurella haemolytica and Pasteurella multocida isolated from calves. J. Antimicrob. Chemother. 38:205–213 [DOI] [PubMed] [Google Scholar]
- 525. Hansen LM, McMurry LM, Levy SB, Hirsh DC. 1993. A new tetracycline resistance determinant, Tet H, from Pasteurella multocida specifying active efflux of tetracycline. Antimicrob. Agents Chemother. 37:2699–2705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 526. Rosenau A, Labigne A, Escande F, Courcoux P, Philippon A. 1991. Plasmid-mediated ROB-1 beta-lactamase in Pasteurella multocida from a human specimen. Antimicrob. Agents Chemother. 35:2419–2422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 527. Cote S, Harel J, Higgins R, Jacques M. 1991. Resistance to antimicrobial agents and prevalence of R plasmids in Pasteurella multocida from swine. Am. J. Vet. Res. 52:1653–1657 [PubMed] [Google Scholar]
- 528. Yamamoto J, Sakano T, Shimizu M. 1990. Drug resistance and R plasmids in Pasteurella multocida isolates from swine. Microbiol. Immunology 34:715–721 [DOI] [PubMed] [Google Scholar]
- 529. Schwarz S, Spies U, Schafer F, Blobel H. 1989. Isolation and interspecies-transfer of a plasmid from Pasteurella multocida encoding for streptomycin resistance. Med. Microbiol. Immunol. 178:121–125 [DOI] [PubMed] [Google Scholar]
- 530. Wright CL, Strugnell RA, Hodgson AL. 1997. Characterization of a Pasteurella multocida plasmid and its use to express recombinant proteins in P. multocida. Plasmid 37:65–79 [DOI] [PubMed] [Google Scholar]
- 531. Hirsh DC, Martin LD, Rhoades KR. 1981. Conjugal transfer of an R-plasmid in Pasteurella multocida. Antimicrob. Agents Chemother. 20:415–417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 532. McGee JE, Bejcek BE. 2001. A cryptic plasmid from Pasteurella multocida has a predicted protein nearly identical to a transport protein from Actinobacillus actinomycetemcomitans. Plasmid 46:60–64 [DOI] [PubMed] [Google Scholar]
- 533. Kehrenberg C, Salmon SA, Watts JL, Schwarz S. 2001. Tetracycline resistance genes in isolates of Pasteurella multocida, Mannheimia haemolytica, Mannheimia glucosida and Mannheimia varigena from bovine and swine respiratory disease: intergeneric spread of the tet(H) plasmid pMHT1. J. Antimicrob. Chemother. 48:631–640 [DOI] [PubMed] [Google Scholar]
- 534. Kehrenberg C, Schulze-Tanzil G, Martel JL, Chaslus-Dancla E, Schwarz S. 2001. Antimicrobial resistance in Pasteurella and Mannheimia: epidemiology and genetic basis. Vet. Res. 32:323–339 [DOI] [PubMed] [Google Scholar]
- 535. Livrelli VO, Darfeuille-Richaud A, Rich CD, Joly BH, Martel JL. 1988. Genetic determinant of the ROB-1 beta-lactamase in bovine and porcine Pasteurella strains. Antimicrob. Agents Chemother. 32:1282–1284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 536. San Millan A, Garcia-Cobos S, Escudero JA, Hidalgo L, Gutierrez B, Carrilero L, Campos J, Gonzalez-Zorn B. 2010. Haemophilus influenzae clinical isolates with plasmid pB1000 bearing blaROB-1: fitness cost and interspecies dissemination. Antimicrob. Agents Chemother. 54:1506–1511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 537. Kadlec K, Brenner Michael G, Sweeney MT, Brzuszkiewicz E, Liesegang H, Daniel R, Watts JL, Schwarz S. 2011. Molecular basis of macrolide, triamilide, and lincosamide resistance in Pasteurella multocida from bovine respiratory disease. Antimicrob. Agents Chemother. 55:2475–2477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 538. Confer AW. 1993. Immunogens of Pasteurella. Vet. Microbiol. 37:353–368 [DOI] [PubMed] [Google Scholar]
- 539. Zimmerman TE, Deeb BJ, DiGiacomo RF. 1992. Polypeptides associated with Pasteurella multocida infection in rabbits. Am. J. Vet. Res. 53:1108–1112 [PubMed] [Google Scholar]
- 540. Li Z, Nestor KE, Saif YM, Anderson JW, Patterson RA. 2000. Serum immunoglobulin G and M concentrations did not appear to be associated with resistance to Pasteurella multocida in a large-bodied turkey line and a randombred control population. Poult. Sci. 79:163–166 [DOI] [PubMed] [Google Scholar]
- 541. Deeb BJ, DiGiacomo RF, Bernard BL, Silbernagel SM, Chengappa MM. 1989. Field trial of a live streptomycin dependent Pasteurella multocida serotype A:12 vaccine in rabbits. Lab. Anim. Sci. 39:229–233 [PubMed] [Google Scholar]
- 542. Haesebrouck F, Pasmans F, Chiers K, Maes D, Ducatelle R, Decostere A. 2004. Efficacy of vaccines against bacterial diseases in swine: what can we expect? Vet. Microbiol. 100:255–268 [DOI] [PubMed] [Google Scholar]
- 543. Lee J, Kang HE, Woo HJ. 2012. Protective immunity conferred by the C-terminal fragment of recombinant Pasteurella multocida toxin. Clin. Vaccine Immunol. 19:1526–1531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 544. Liao CM, Huang C, Hsuan SL, Chen ZW, Lee WC, Liu CI, Winton JR, Chien MS. 2006. Immunogenicity and efficacy of three recombinant subunit Pasteurella multocida toxin vaccines against progressive atrophic rhinitis in pigs. Vaccine 24:27–35 [DOI] [PubMed] [Google Scholar]
- 545. Lu YS, Pakes SP, Massey L. 1987. Hyperimmune serum from rabbits immunized with potassium thiocyanate extract of Pasteurella multocida protects against homologous challenge. J. Clin. Microbiol. 25:2173–2180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 546. Lu YS, Pakes SP, Massey L, Stefanu C. 1987. A potassium thiocyanate extract vaccine prepared from Pasteurella multocida 3:A protects rabbits against homologous challenge. Infect. Immun. 55:2967–2976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 547. Magyar T, Donko T, Kovacs F. 2008. Atrophic rhinitis vaccine composition triggers different serological profiles that do not correlate with protection. Acta Vet. Hung. 56:27–40 [DOI] [PubMed] [Google Scholar]
- 548. Magyar T, King VL, Kovacs F. 2002. Evaluation of vaccines for atrophic rhinitis—a comparison of three challenge models. Vaccine 20:1797–1802 [DOI] [PubMed] [Google Scholar]
- 549. Petersen SK, Foged NT, Bording A, Nielsen JP, Riemann HK, Frandsen PL. 1991. Recombinant derivatives of Pasteurella multocida toxin: candidates for a vaccine against progressive atrophic rhinitis. Infect. Immun. 59:1387–1393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 550. Seo J, Lee S, Pyo H, Lee J, Kim T. 2010. Protective potential of an attenuated Pasteurella multocida, which expresses only the N-terminal truncated fragment of P. multocida toxin. Can. J. Vet. Res. 74:25–29 [PMC free article] [PubMed] [Google Scholar]
- 551. Seo J, Pyo H, Lee S, Lee J, Kim T. 2009. Expression of 4 truncated fragments of Pasteurella multocida toxin and their immunogenicity. Can. J. Vet. Res. 73:184–189 [PMC free article] [PubMed] [Google Scholar]
- 552. To H, Someno S, Nagai S. 2005. Development of a genetically modified nontoxigenic Pasteurella multocida toxin as a candidate for use in vaccines against progressive atrophic rhinitis in pigs. Am. J. Vet. Res. 66:113–118 [DOI] [PubMed] [Google Scholar]
- 553. Suckow MA. 2000. Immunization of rabbits against Pasteurella multocida using a commercial swine vaccine. Lab. Anim. 34:403–408 [DOI] [PubMed] [Google Scholar]
- 554. Barfod K, Pedersen KB. 1984. Influence of vaccination of sows with Bordetella-Pasteurella vaccines on the occurrence of atrophic rhinitis among their offspring after experimental infection with Bordetella bronchiseptica and toxigenic Pasteurella multocida. Nord. Vet. Med. 36:337–345 [PubMed] [Google Scholar]
- 555. Hsuan SL, Liao CM, Huang C, Winton JR, Chen ZW, Lee WC, Liao JW, Chen TH, Chiou CJ, Yeh KS, Chien MS. 2009. Efficacy of a novel Pasteurella multocida vaccine against progressive atrophic rhinitis of swine. Vaccine 27:2923–2929 [DOI] [PubMed] [Google Scholar]
- 556. Pedersen KB, Barfod K. 1982. Effect on the incidence of atrophic rhinitis of vaccination of sows with a vaccine containing Pasteurella multocida toxin. Nord. Vet. Med. 34:293–302 [PubMed] [Google Scholar]
- 557. Riising HJ, van Empel P, Witvliet M. 2002. Protection of piglets against atrophic rhinitis by vaccinating the sow with a vaccine against Pasteurella multocida and Bordetella bronchiseptica. Vet. Rec. 150:569–571 [DOI] [PubMed] [Google Scholar]
- 558. Jarvinen LZ, Hogenesch H, Suckow MA, Bowersock TL. 1998. Induction of protective immunity in rabbits by coadministration of inactivated Pasteurella multocida toxin and potassium thiocyanate extract. Infect. Immun. 66:3788–3795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 559. Suckow MA, Bowersock TL, Nielsen K, Chrisp CE, Frandsen PL, Janovitz EB. 1995. Protective immunity to Pasteurella multocida heat-labile toxin by intranasal immunization in rabbits. Lab. Anim. Sci. 45:526–532 [PubMed] [Google Scholar]
- 560. Nielsen JP, Foged NT, Sorensen V, Barfod K, Bording A, Petersen SK. 1991. Vaccination against progressive atrophic rhinitis with a recombinant Pasteurella multocida toxin derivative. Can. J. Vet. Res. 55:128–138 [PMC free article] [PubMed] [Google Scholar]
- 561. Register KB, Sacco RE, Brockmeier SL. 2007. Immune response in mice and swine to DNA vaccines derived from the Pasteurella multocida toxin gene. Vaccine 25:6118–6128 [DOI] [PubMed] [Google Scholar]
- 562. Vasfi Marandi M, Mittal KR. 1997. Role of outer membrane protein H (OmpH)- and OmpA-specific monoclonal antibodies from hybridoma tumors in protection of mice against Pasteurella multocida. Infect. Immun. 65:4502–4508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 563. Lee J, Kim YB, Kwon M. 2007. Outer membrane protein H for protective immunity against Pasteurella multocida. J. Microbiol. 45:179–184 [PubMed] [Google Scholar]
- 564. Mohd Yasin IS, Mohd Yusoff S, Mohd ZS, Abd Wahid Mohd E. 2011. Efficacy of an inactivated recombinant vaccine encoding a fimbrial protein of Pasteurella multocida B:2 against hemorrhagic septicemia in goats. Trop. Anim. Health Prod. 43:179–187 [DOI] [PubMed] [Google Scholar]
- 565. Okay S, Ozcengiz E, Gursel I, Ozcengiz G. 2012. Immunogenicity and protective efficacy of the recombinant Pasteurella lipoprotein E and outer membrane protein H from Pasteurella multocida A:3 in mice. Res. Vet. Sci. 93:1261–1265 [DOI] [PubMed] [Google Scholar]
- 566. Tatum FM, Tabatabai LB, Briggs RE. 2009. Protection against fowl cholera conferred by vaccination with recombinant Pasteurella multocida filamentous hemagglutinin peptides. Avian Dis. 53:169–174 [DOI] [PubMed] [Google Scholar]
- 567. Confer AW, Suckow MA, Montelongo M, Dabo SM, Miloscio LJ, Gillespie AJ, Meredith GL. 2001. Intranasal vaccination of rabbits with Pasteurella multocida A:3 outer membranes that express iron-regulated proteins. Am. J. Vet. Res. 62:697–703 [DOI] [PubMed] [Google Scholar]
- 568. Prado ME, Dabo SM, Confer AW. 2005. Immunogenicity of iron-regulated outer membrane proteins of Pasteurella multocida A:3 in cattle: molecular characterization of the immunodominant heme acquisition system receptor (HasR) protein. Vet. Microbiol. 105:269–280 [DOI] [PubMed] [Google Scholar]
- 569. Zhao G, Pijoan C, Choi K, Maheswaran SK, Trigo E. 1995. Expression of iron-regulated outer membrane proteins by porcine strains of Pasteurella multocida. Can. J. Vet. Res. 59:46–50 [PMC free article] [PubMed] [Google Scholar]
- 570. Ruffolo CG, Jost BH, Adler B. 1998. Iron-regulated outer membrane proteins of Pasteurella multocida and their role in immunity. Vet. Microbiol. 59:123–137 [DOI] [PubMed] [Google Scholar]
- 571. Adler B, Chancellor R, Homchampa P, Hunt M, Ruffolo C, Strugnell R, Wapling D. 1996. Immunity and vaccine development in Pasteurella multocida infections. J. Biotechnol. 44:139–144 [DOI] [PubMed] [Google Scholar]
- 572. Choi-Kim K, Maheswaran SK, Felice LJ, Molitor TW. 1991. Relationship between the iron regulated outer membrane proteins and the outer membrane proteins of in vivo grown Pasteurella multocida. Vet. Microbiol. 28:75–92 [DOI] [PubMed] [Google Scholar]
- 573. Glisson JR, Contreras MD, Cheng IH, Wang C. 1993. Cross-protection studies with Pasteurella multocida bacterins prepared from bacteria propagated in iron-depleted medium. Avian Dis. 37:1074–1079 [PubMed] [Google Scholar]
- 574. Herath C, Kumar P, Singh M, Kumar D, Ramakrishnan S, Goswami TK, Singh A, Ram GC. 2010. Experimental iron-inactivated Pasteurella multocida A: 1 vaccine adjuvanted with bacterial DNA is safe and protects chickens from fowl cholera. Vaccine 28:2284–2289 [DOI] [PubMed] [Google Scholar]
- 575. Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. 2011. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol. Biol. Evol. 28:2731–2739 [DOI] [PMC free article] [PubMed] [Google Scholar]