LETTER
A recent paper by Kurtz et al. (1) describes a role for the cytokine interleukin-6 (IL-6) during infection by the bacterial pathogen Francisella tularensis. The paper discusses how IL-6 plays an important role in the progression of primary disease caused by a substantial dose of the live vaccine strain (LVS) in mice and explores how it contributes to the generation of protective immunity. Ablation of IL-6 in LVS-infected mice decreased the 50% lethal dose (LD50) for the pathogen. Mouse models of infection for the disease tularemia frequently use the LVS strain, as the progression of the disease is thought similar to that in humans while also offering the advantage of being handled at a lower biosafety level than highly virulent strains of F. tularensis, such as SCHU-S4 (2).
The host response during tularemia has been described as “too much, too late,” implying that the host is slow to respond to the infection and that, when it does, the response is uncontrolled, contributing directly to the severity of disease (3). There are two potential therapeutic strategies for addressing this issue. The first is stimulating an earlier immune response through the use of proinflammatory therapies. This approach has some therapeutic benefit when given as a prophylaxis (4, 5). The second is the mitigation of the damaging “too much” response (cytokine storm) using anti-inflammatory therapeutics in combination with antibiotics (6). This second strategy led us to evaluate IL-6 as a potential target by performing experiments similar to those described by Kurtz et al. except using a F. tularensis SCHU-S4 type A strain. Comparing the infections in wild-type and knockout (KO) mice, our findings, in contrast with those found using the LVS strain (1), suggest that IL-6 does not have any effect on the progression of this disease (Fig. 1).
Fig 1.
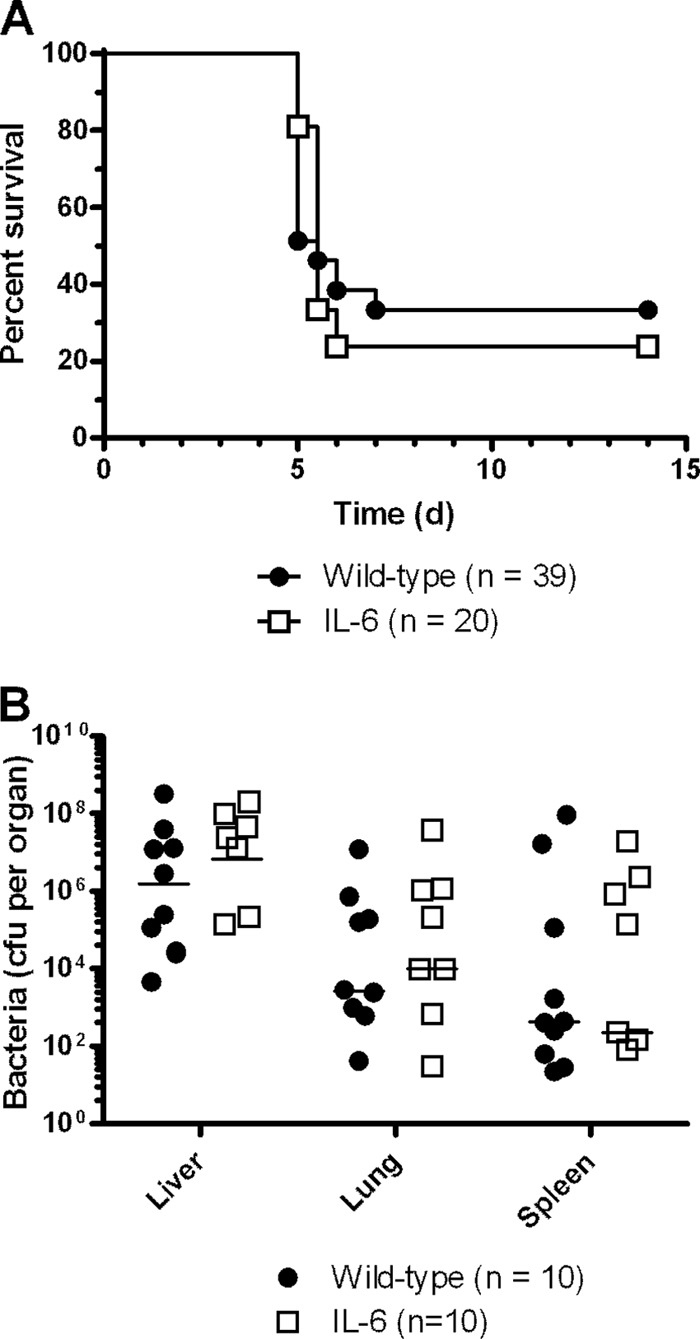
Progression of disease in wild-type and IL-6 knockout C57BL/6 mice following challenge with F. tularensis strain SCHU-S4. (A) Wild-type C57BL/6J mice (n = 39) (Charles River, United Kingdom) and IL-6, B6.129S2-Il6tm1Kopf/J, knockout mice (n = 20) (Jackson Laboratories) were infected intranasally with approximately 150 CFU of F. tularensis SCHU-S4 under light, halothane anesthesia and checked twice daily for signs. Survival was measured, and the plot contains data from two separate experiments. We found that the IL-6 knockout mice exhibited survival characteristics similar to those of their wild-type counterparts (P > 0.10, using a log rank test stratified by experimental run) and that this was consistent between experiments (P > 0.10, using a log rank test stratified by mouse strain). d, day. (B) At day 4 postinfection, 10 additional animals from each experiment (5 KO and 5 wild type) were culled. The bacterial burden was enumerated, and the cytokine release was determined (by cytometric bead array [CBA; BD Biosciences] read on a FACSCanto II flow cytometer [BD Biosciences]) from within the lung, liver, and spleen. No differences in bacterial load were observed (P < 0.10, using a Kruskal-Wallis test). The absence of IL-6 was confirmed within the knockout strains of mice (data not shown).
Collectively, the data suggest that there is a differential role for IL-6 during primary infection with LVS and SCHU-S4 in mice. A notable difference in the bacterial burdens in organs was observed between the IL-6 KO and wild-type mice late in LVS infection (day 6) (1). As SCHU-S4 causes a shorter and more acute infection (mice surviving 4 to 5 days), this divergence was absent in our model. An additional effect of IL-6 ablation in LVS infection, an increase in liver enzymes, was observed in the blood at day 6 (1). However, we found the levels of these enzymes to be similar using SCHU-S4 at day 4 (data not shown). Kurtz et al. also demonstrated that, after secondary challenge, IL-6-ablated mice had more IgM and less IgG than wild-type mice (1). This might suggest that the adaptive immune response matures more slowly in the absence of IL-6. If this were true, it could account for the difference between the LVS and SCHU-S4 models of infection where, after primary challenge and by virtue of the extended survival by 1 to 2 days, the LVS model has more time for an early adaptive response to contribute to survival (or not in the absence of IL-6). These data further contribute to the growing discussions as to what model is most suitable for developing/assessing treatments against tularemia.
Footnotes
Published ahead of print 28 May 2013
REFERENCES
- 1. Kurtz S, Foreman O, Bosio CM, Anver MR, Elkins KL. 2013. IL-6 is essential for primary resistance to Francisella tularensis LVS infection. Infect. Immun. 81:585–597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Conlan JW, Chen W, Bosio CM, Cowley SC, Elkins KL. 2011. Infection of mice with Francisella as an immunological model. Curr. Protoc. Immunol. 93:19.14.119.14.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cowley SC. 2009. Editorial: proinflammatory cytokines in pneumonic tularemia: too much too late? J. Leukoc. Biol. 86:469–470 [DOI] [PubMed] [Google Scholar]
- 4. Duckett NS, Olmos S, Durrant DM, Metzger DW. 2005. Intranasal interleukin-12 treatment for protection against respiratory infection with the Francisella tularensis live vaccine strain. Infect. Immun. 73:2306–2311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Elkins KL, Rhinehart-Jones TR, Stibitz S, Conover JS, Klinman DM. 1999. Bacterial DNA containing CpG motifs stimulates lymphocyte-dependent protection of mice against lethal infection with intracellular bacteria. J. Immunol. 162:2291–2298 [PubMed] [Google Scholar]
- 6. D'Elia RV, Harrison K, Oyston PC, Lukaszewski RA, Clark GC. 2013. Targeting the “cytokine storm” for therapeutic benefit. Clin. Vaccine Immunol. 20:319–327 [DOI] [PMC free article] [PubMed] [Google Scholar]


