Abstract
T-20EK is a novel fusion inhibitor designed to have enhanced α-helicity over T-20 (enfuvirtide) through engineered electrostatic interactions between glutamic acid (E) and lysine (K) substitutions. T-20EK efficiently suppresses wild-type and T-20-resistant variants. Here, we selected T-20EK-resistant variants. A combination of L33S and N43K substitutions in gp41 were required for high resistance to T-20EK. While these substitutions also caused resistance to T-20, they did not cause cross-resistance to other known fusion inhibitors.
TEXT
Enfuvirtide (T-20), a 36-amino-acid peptide derived from the C-terminal heptad repeat (C-HR) of HIV-1 gp41, has been approved as the first fusion inhibitor of HIV-1 entry. T-20 inhibits HIV-1 replication by interfering with the formation of the fusion intermediate six-helix bundle, which is composed of three N-terminal heptad repeats (N-HRs) and three C-HRs arranged in an antiparallel orientation (1). Because of its unique mechanism of action, T-20 effectively suppresses replication of HIV-1 resistant to inhibitors targeting the reverse transcriptase and protease (2, 3). However, long-term therapy with a T-20-containing regimen can result in the emergence of T-20-resistant strains (4, 5). These strains contain substitutions at the N-HR region of gp41, including G36D, V38A, and N43K/D, both in vitro and in vivo, and exhibit reduced susceptibility to T-20 through decreased binding of T-20 to the mutated N-HR (6–14). To suppress replication of such variants and obtain durable efficacy in HIV-1-infected patients, new fusion inhibitors are needed.
To date, several novel fusion inhibitors have been developed, including tifuvirtide (T-1249) (15), sifuvirtide (SFT) (16), and T-2635 (TRI-1144) (17), that potently suppress replication of T-20-resistant variants (Fig. 1A), as well as d-peptide-based (18) or small-molecule inhibitors (19). We recently developed the electrostatically constrained fusion inhibitors SC35EK and its 29-residue shorter form, SC29EK, which also inhibit replication of T-20-resistant HIV-1 (20, 21). These are peptides with electrostatic interactions between glutamic acid (E) and lysine (K) substitutions placed at the i and i + 4 positions in the solvent-interacting site (EK motif) and are designed to enhance the α-helicity of the peptides (22). The enhancement in α-helicity correlates well with an enhancement in binding affinity for the targeted region and appears to be a key determinant for inhibition of T-20-resistant HIV-1. In addition to C34 (Fig. 1A), we have also applied the EK modification to T-20, termed T-20EK, that shows sustained activity to T-20-resistant variants and HIV-2 strains (23). Moreover, T-20EK showed activity in an animal model (24). To address the mechanism of HIV-1 resistance to T-20EK in vitro, we selected T-20EK-resistant HIV-1 strains by using a dose escalation method, identified the primary substitutions that caused resistance to this inhibitor, and evaluated susceptibility of the T-20EK-resistant strains to other fusion inhibitors.
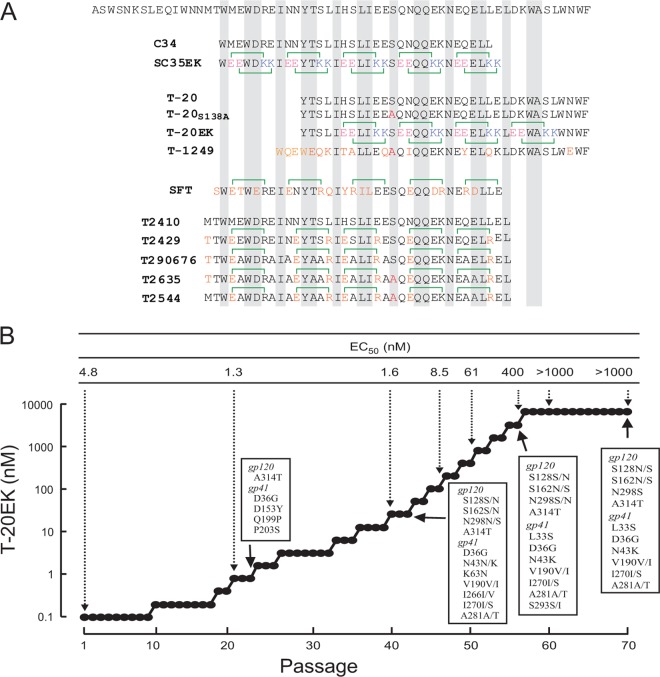
Fig 1.
(A) Amino acid sequences of fusion-inhibitory peptides used in this study. The HIV-1 C-HR amino acid sequence is shown in the first row. Electrostatic interactions are indicated in pink and light blue for acidic (glutamic acid [E]) and basic (lysine [K]) residues, respectively. Modified amino acids are indicated in orange. A resistance-associated substitution, S138A, is indicated in red. Amino acids for the interactive site are shaded gray. (B) The dose escalation method for selection of T-20EK resistance through passage in MT-2 cells. Induction of resistant HIV-1 was performed over a total of 70 passages from 0.1 nM T-20EK. At the indicated passage, proviral DNAs were sequenced, and the 50% effective concentrations (EC50s) of the HIV-1 variants were determined in a MAGI assay. All substitutions shown in boxes were observed in combination.
Selection passages were carried out in MT-2 cells using HIV-1NL4-3 as the starting wild-type virus (25, 26). The first HIV-1 mutants with enhanced susceptibility to T-20EK emerged at passage 22 (P-22) and were A314T in gp120 and D36G in gp41 (Fig. 1B). The D36G substitution has been widely observed in HIV-1 strains and is thought to contribute to efficient replication rather than causing resistance by decreasing binding to the inhibitor (10, 27, 28). At P-44, we observed the K63N change and a mixture of asparagine and lysine at residue 43 (N43N/K) in gp41. Substitutions in gp120 (see Fig. S1 in the supplemental material) appear to be polymorphisms, because these substitutions were not directly involved in resistance (see Table S1 in the supplemental material). Moreover, S128N and S162N are reported as polymorphisms in the Los Alamos Database (Los Alamos National Library, HIV Sequence Database; http://www.hiv.lanl.gov) and are observed as mixed viruses over a relatively long period of time. We (21, 25, 26) and others (29) have previously reported that substitutions in gp120 can enhance fusion kinetics (30, 31) but do not significantly affect susceptibility to fusion inhibitors. Finally, HIV-1 acquired L33S, N43K, and cytoplasmic tail (CT) substitutions, resulting in viruses that replicated efficiently even in the presence of 1,000 nM T-20EK.
We prepared HIV-1 recombinant clones with the substitutions discovered during our passages and determined the antiviral activities of T-20EK and other peptides against the T-20EK-resistant variants (Fig. 1B) and clones by using a MAGI (multinuclear activation of a β-galactosidase indicator) assay (10, 25, 26). Our data revealed that L33S and N43K are major primary substitutions for T-20EK resistance (Table 1). Substitutions in the CT domain weakly enhanced the resistance induced by L33S/N43K. We previously showed that the S138A substitution in T-20 (T-20S138A) leads to substantial inhibition of the T-20-resistant variant HIV-1L33S/N43K (10, 14, 23). Interestingly, T-20EKS138A, a variant of T-20EK that is expected to exert strong activity to resistant variants, did not inhibit efficiently HIV-1L33S/N43K (Table 1). We found cross-resistance between T-20EK and other T-20-based fusion inhibitors, except for T1249, which has an amino acid sequence that overlaps with T-20 (Fig. 1A). In contrast, C34 and its derivatives maintained their activity to T-20EK-resistant variants. These results indicated that T-20EK may show cross-resistance only with T-20-derived peptides and that the mechanisms of resistance to T-20 and C34 derivatives are different.
Table 1.
Susceptibilities of HIV-1 recombinant clones with substitutions in gp41 to peptide fusion inhibitorsa
| Peptide | EC50 (nM) of HIV-1 clone |
||||
|---|---|---|---|---|---|
| HIV-1WTb | HIV-1L33S | HIV-1N43K | HIV-1L33S/N43K | HIV-1L33S/N43K/T-CTc | |
| Dideoxycytosine | 356 ± 89 | 347 ± 129 (1.0) | 489 ± 37 (1.4) | 431 ± 75 (1.2) | 474 ± 273 (1.3) |
| T-20-based peptides | |||||
| T-20 | 2.5 ± 0.2 | 66 ± 9 (26) | 31 ± 4 (12) | >1,000 (>400) | >1,000 (>400) |
| T-20S138A | 0.55 ± 0.14 | 3.2 ± 0.7 (5.8) | 0.45 ± 0.07 (0.8) | 30 ± 10 (55) | 73.3 ± 23 (133) |
| T-20EK | 1.2 ± 0.3 | 12 ± 2 (10) | 12 ± 1 (10) | >1,000 (>833) | >1,000 (>833) |
| T-20EKS138A | 0.43 ± 0.06 | 2.2 ± 0.4 (5.1) | 2.3 ± 0.7 (5.4) | 112 ± 20 (260) | 301 ± 110 (700) |
| T1249 | 0.29 ± 0.07 | 0.31 ± 0.10 (1.1) | 0.35 ± 0.10 (1.2) | 0.60 ± 0.16 (2.2) | ND |
| C34-based peptides | |||||
| C34 | 1.1 ± 0.2 | 2.9 ± 0.4 (2.6) | 2.6 ± 0.7 (2.4) | 4.1 ± 1.6 (3.7) | 9 ± 5.2 (8) |
| SC35EK | 1.7 ± 0.4 | 1.8 ± 0.3 (1.1) | 2.4 ± 0.5 (1.4) | 2.5 ± 0.6 (1.5) | 3.4 ± 1.9 (2) |
| Sifvirtide | 2.1 ± 0.4 | 2.5 ± 0.2 (1.2) | 1.5 ± 0.3 (0.7) | 2.2 ± 0.5 (1.0) | ND |
| T2410 | 1.1 ± 0.3 | 0.64 ± 0.23 (0.6) | 1.8 ± 0.5 (1.6) | 1.4 ± 0.5 (1.3) | ND |
| T2429 | 1.9 ± 0.3 | 1.9 ± 0.5 (1.0) | 2.5 ± 0.8 (1.3) | 1.8 ± 0.1 (0.9) | ND |
| T290676 | 0.46 ± 0.14 | 0.54 ± 0.12 (1.2) | 0.46 ± 0.10 (1.0) | 1.1 ± 0.5 (2.4) | ND |
| T2635 | 0.43 ± 0.02 | 0.55 ± 0.22 (1.3) | 1.4 ± 0.6 (3.3) | 0.57 ± 0.22 (1.3) | 1.7 ± 0.4 (4) |
| T2544 | 0.46 ± 0.08 | 1.3 ± 0.3 (2.8) | 2.4 ± 0.4 (5.2) | 1.1 ± 0.4 (2.4) | ND |
Drug susceptibilities were determined in a MAGI assay and are reported here as means ± standard deviations from at least three independent assays. Values in parentheses are the fold change in resistance compared with HIV-1WT. Peptide fusion inhibitors that caused more than 10-fold resistance are indicated in bold. ND, not determined.
NL4.3D36G was defined as wild-type HIV-1 (HIV-1WT).
T-CT (transmembrane and cytoplasmic tail domains) indicates the substitutions V190I, I270S, and A281T, which were only observed in a mixture.
During the selection, we observed one substitution in the gp41 transmembrane domain, V190I, and two in the cytoplasmic domain (intravirion), I270S and A281T (Fig. 1B). These three substitutions are also observed in T-20-naive isolates (Los Alamos National Library, HIV Sequence Database; http://www.hiv.lanl.gov). Although these substitutions contributed little to the resistance (Table 1), I270S/A281T substitutions in gp41 cytoplasmic tail restored significantly reduced replication kinetics by substitutions in the ectodomain and transmembrane domain (see Fig. S2 in the supplemental material). Other substitutions, K63N, D153Y, Q199P, P203S, I266V, and S293I, were transiently observed but later disappeared during the selection (see Fig. S1 in the supplemental material). K63N is located adjacent to Q64, which was previously shown to be a resistance-associated substitution (32). The synonymous change in V72 (GTG to GTA) may influence the RRE structural stability, as we have previously described (28). With the exception of D153Y, Q199P, and P203S in gp41, all substitutions were observed in the vast majority of T-20-naive patients, indicating that they are natural polymorphisms. P203S was also selected as a low-level SC34EK resistance-associated substitution (26). This is consistent with our data showing that combinations of CT substitutions only enhance resistance by 2- to 3-fold (Table 1). Moreover, most substitutions coexisted with variants containing the wild-type sequence, strongly indicating that they, as well as those in gp120, exerted only a modest effect on resistance.
We previously demonstrated that T-20EK inhibited T-20-resistant variants harboring G36D, V38A, or N43D/K substitutions (28) and that it maintains its strong antiviral effect against HIV-2 (23). T-20EK-resistant variants showed very limited cross-resistance to other novel fusion inhibitors, with the exception of T-20-based peptides, indicating that the combination of T-20EK with other new fusion inhibitors may be suitable for therapy. The enhanced hydrophilicity of T-20EK by the engineered hydrophilic amino acids (Glu and Lys) is a favorable property for solubility, which is expected to reduce some of the adverse effects of T-20, such as skin reactions at the injection site (33). Interestingly, our experiments did not result in the selection of any secondary substitutions in the C-HR, such as N126K and S138A, that are frequently observed in variants that are resistant to novel fusion inhibitors (26, 34, 35). In contrast, one of the primary substitutions was L33S, a substitution at a site outside the N-HR. Notably, the replication kinetics of L33S are comparable to those of wild-type HIV-1 (unpublished data). Therefore, L33S seems to be a T-20-specific substitution that does not require the presence of secondary substitutions. Importantly, use of T-20EK does not lead to the appearance of substitutions that confer cross-resistance to other novel fusion inhibitors. Thus, our study establishes that T-20EK can become an efficient new fusion inhibitor.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported in part by a grant for the Promotion of AIDS Research from the Ministry of Health, Labor and Welfare of Japan (E.N.K.) and a grant from the Ministry of Education, Culture, Sports, Science and Technology of Japan (E.N.K.). S.G.S. was supported in part by National Institutes of Health grants AI076119, AI074389, and AI079801.
We are grateful to the Biomedical Research Core, Tohoku University School of Medicine, for technical support. We thank Megumi Ono for editorial assistance.
Footnotes
Published ahead of print 20 May 2013
Supplemental material for this article may be found at http://dx.doi.org/10.1128/AAC.00237-13.
REFERENCES
- 1. Wild C, Oas T, McDanal C, Bolognesi D, Matthews T. 1992. A synthetic peptide inhibitor of human immunodeficiency virus replication: correlation between solution structure and viral inhibition. Proc. Natl. Acad. Sci. U. S. A. 89:10537–10541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lalezari JP, Henry K, O'Hearn M, Montaner JS, Piliero PJ, Trottier B, Walmsley S, Cohen C, Kuritzkes DR, Eron JJ, Jr, Chung J, DeMasi R, Donatacci L, Drobnes C, Delehanty J, Salgo M. 2003. Enfuvirtide, an HIV-1 fusion inhibitor, for drug-resistant HIV infection in North and South America. N. Engl. J. Med. 348:2175–2185 [DOI] [PubMed] [Google Scholar]
- 3. Lazzarin A, Clotet B, Cooper D, Reynes J, Arasteh K, Nelson M, Katlama C, Stellbrink HJ, Delfraissy JF, Lange J, Huson L, DeMasi R, Wat C, Delehanty J, Drobnes C, Salgo M. 2003. Efficacy of enfuvirtide in patients infected with drug-resistant HIV-1 in Europe and Australia. N. Engl. J. Med. 348:2186–2195 [DOI] [PubMed] [Google Scholar]
- 4. Mink M, Mosier SM, Janumpalli S, Davison D, Jin L, Melby T, Sista P, Erickson J, Lambert D, Stanfield-Oakley SA, Salgo M, Cammack N, Matthews T, Greenberg ML. 2005. Impact of human immunodeficiency virus type 1 gp41 amino acid substitutions selected during enfuvirtide treatment on gp41 binding and antiviral potency of enfuvirtide in vitro. J. Virol. 79:12447–12454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Xu L, Pozniak A, Wildfire A, Stanfield-Oakley SA, Mosier SM, Ratcliffe D, Workman J, Joall A, Myers R, Smit E, Cane PA, Greenberg ML, Pillay D. 2005. Emergence and evolution of enfuvirtide resistance following long-term therapy involves heptad repeat 2 mutations within gp41. Antimicrob. Agents Chemother. 49:1113–1119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bai X, Wilson KL, Seedorff JE, Ahrens D, Green J, Davison DK, Jin L, Stanfield-Oakley SA, Mosier SM, Melby TE, Cammack N, Wang Z, Greenberg ML, Dwyer JJ. 2008. Impact of the enfuvirtide resistance mutation N43D and the associated baseline polymorphism E137K on peptide sensitivity and six-helix bundle structure. Biochemistry 47:6662–6670 [DOI] [PubMed] [Google Scholar]
- 7. Baldwin CE, Sanders RW, Deng Y, Jurriaans S, Lange JM, Lu M, Berkhout B. 2004. Emergence of a drug-dependent human immunodeficiency virus type 1 variant during therapy with the T20 fusion inhibitor. J. Virol. 78:12428–12437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cabrera C, Marfil S, Garcia E, Martinez-Picado J, Bonjoch A, Bofill M, Moreno S, Ribera E, Domingo P, Clotet B, Ruiz L. 2006. Genetic evolution of gp41 reveals a highly exclusive relationship between codons 36, 38 and 43 in gp41 under long-term enfuvirtide-containing salvage regimen. AIDS 20:2075–2080 [DOI] [PubMed] [Google Scholar]
- 9. Champagne K, Shishido A, Root MJ. 2009. Interactions of HIV-1 inhibitory peptide T20 with the gp41 N-HR coiled coil. J. Biol. Chem. 284:3619–3627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Izumi K, Kodama E, Shimura K, Sakagami Y, Watanabe K, Ito S, Watabe T, Terakawa Y, Nishikawa H, Sarafianos SG, Kitaura K, Oishi S, Fujii N, Matsuoka M. 2009. Design of Peptide-based inhibitors for human immunodeficiency virus type 1 strains resistant to T-20. J. Biol. Chem. 284:4914–4920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lu J, Deeks SG, Hoh R, Beatty G, Kuritzkes BA, Martin JN, Kuritzkes DR. 2006. Rapid emergence of enfuvirtide resistance in HIV-1-infected patients: results of a clonal analysis. J. Acquir. Immune Defic. Syndr. 43:60–64 [DOI] [PubMed] [Google Scholar]
- 12. Oliveira AC, Martins AN, Pires AF, Arruda MB, Tanuri A, Pereira HS, Brindeiro RM. 2009. Enfuvirtide (T-20) resistance-related mutations in HIV type 1 subtypes B, C, and F isolates from Brazilian patients failing HAART. AIDS Res. Hum. Retroviruses 25:193–198 [DOI] [PubMed] [Google Scholar]
- 13. Reeves JD, Lee FH, Miamidian JL, Jabara CB, Juntilla MM, Doms RW. 2005. Enfuvirtide resistance mutations: impact on human immunodeficiency virus envelope function, entry inhibitor sensitivity, and virus neutralization. J. Virol. 79:4991–4999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Watabe T, Terakawa Y, Watanabe K, Ohno H, Nakano H, Nakatsu T, Kato H, Izumi K, Kodama E, Matsuoka M, Kitaura K, Oishi S, Fujii N. 2009. X-ray crystallographic study of an HIV-1 fusion inhibitor with the gp41 S138A substitution. J. Mol. Biol. 392:657–665 [DOI] [PubMed] [Google Scholar]
- 15. Lalezari JP, Bellos NC, Sathasivam K, Richmond GJ, Cohen CJ, Myers RA, Jr, Henry DH, Raskino C, Melby T, Murchison H, Zhang Y, Spence R, Greenberg ML, Demasi RA, Miralles GD. 2005. T-1249 retains potent antiretroviral activity in patients who had experienced virological failure while on an enfuvirtide-containing treatment regimen. J. Infect. Dis. 191:1155–1163 [DOI] [PubMed] [Google Scholar]
- 16. He Y, Xiao Y, Song H, Liang Q, Ju D, Chen X, Lu H, Jing W, Jiang S, Zhang L. 2008. Design and evaluation of sifuvirtide, a novel HIV-1 fusion inhibitor. J. Biol. Chem. 283:11126–11134 [DOI] [PubMed] [Google Scholar]
- 17. Dwyer JJ, Wilson KL, Davison DK, Freel SA, Seedorff JE, Wring SA, Tvermoes NA, Matthews TJ, Greenberg ML, Delmedico MK. 2007. Design of helical, oligomeric HIV-1 fusion inhibitor peptides with potent activity against enfuvirtide-resistant virus. Proc. Natl. Acad. Sci. U. S. A. 104:12772–12777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Welch BD, VanDemark AP, Heroux A, Hill CP, Kay MS. 2007. Potent D-peptide inhibitors of HIV-1 entry. Proc. Natl. Acad. Sci. U. S. A. 104:16828–16833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wang H, Qi Z, Guo A, Mao Q, Lu H, An X, Xia C, Li X, Debnath AK, Wu S, Liu S, Jiang S. 2009. ADS-J1 inhibits human immunodeficiency virus type 1 entry by interacting with the gp41 pocket region and blocking fusion-active gp41 core formation. Antimicrob. Agents Chemother. 53:4987–4998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Naito T, Izumi K, Kodama E, Sakagami Y, Kajiwara K, Nishikawa H, Watanabe K, Sarafianos SG, Oishi S, Fujii N, Matsuoka M. 2009. SC29EK, a peptide fusion inhibitor with enhanced alpha-helicity, inhibits replication of human immunodeficiency virus type 1 mutants resistant to enfuvirtide. Antimicrob. Agents Chemother. 53:1013–1018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nishikawa H, Nakamura S, Kodama E, Ito S, Kajiwara K, Izumi K, Sakagami Y, Oishi S, Ohkubo T, Kobayashi Y, Otaka A, Fujii N, Matsuoka M. 2009. Electrostatically constrained alpha-helical peptide inhibits replication of HIV-1 resistant to enfuvirtide. Int. J. Biochem. Cell Biol. 41:891–899 [DOI] [PubMed] [Google Scholar]
- 22. Marqusee S, Baldwin RL. 1987. Helix stabilization by Glu-Lys+ salt bridges in short peptides of de novo design. Proc. Natl. Acad. Sci. U. S. A. 84:8898–8902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Oishi S, Ito S, Nishikawa H, Watanabe K, Tanaka M, Ohno H, Izumi K, Sakagami Y, Kodama E, Matsuoka M, Fujii N. 2008. Design of a novel HIV-1 fusion inhibitor that displays a minimal interface for binding affinity. J. Med. Chem. 51:388–391 [DOI] [PubMed] [Google Scholar]
- 24. Li X, Qian H, Miyamoto F, Naito T, Kawaji K, Kajiwara K, Hattori T, Matsuoka M, Watanabe K, Oishi S, Fujii N, Kodama EN. 2012. A simple, rapid, and sensitive system for the evaluation of anti-viral drugs in rats. Biochem. Biophys. Res. Commun. 424:257–261 [DOI] [PubMed] [Google Scholar]
- 25. Nameki D, Kodama E, Ikeuchi M, Mabuchi N, Otaka A, Tamamura H, Ohno M, Fujii N, Matsuoka M. 2005. Mutations conferring resistance to human immunodeficiency virus type 1 fusion inhibitors are restricted by gp41 and Rev-responsive element functions. J. Virol. 79:764–770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shimura K, Nameki D, Kajiwara K, Watanabe K, Sakagami Y, Oishi S, Fujii N, Matsuoka M, Sarafianos SG, Kodama EN. 2010. Resistance profiles of novel electrostatically constrained HIV-1 fusion inhibitors. J. Biol. Chem. 285:39471–39480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Izumi K, Nakamura S, Nakano H, Shimura K, Sakagami Y, Oishi S, Uchiyama S, Ohkubo T, Kobayashi Y, Fujii N, Matsuoka M, Kodama EN. 2010. Characterization of HIV-1 resistance to a fusion inhibitor, N36, derived from the gp41 amino-terminal heptad repeat. Antiviral Res. 87:179–186 [DOI] [PubMed] [Google Scholar]
- 28. Ueno M, Kodama EN, Shimura K, Sakurai Y, Kajiwara K, Sakagami Y, Oishi S, Fujii N, Matsuoka M. 2009. Synonymous mutations in stem-loop III of Rev-responsive elements enhance HIV-1 replication impaired by primary mutations for resistance to enfuvirtide. Antiviral Res. 82:67–72 [DOI] [PubMed] [Google Scholar]
- 29. Eggink D, Bontjer I, Langedijk JP, Berkhout B, Sanders RW. 2011. Resistance of human immunodeficiency virus type 1 to a third-generation fusion inhibitor requires multiple mutations in gp41 and is accompanied by a dramatic loss of gp41 function. J. Virol. 85:10785–10797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Reeves JD, Gallo SA, Ahmad N, Miamidian JL, Harvey PE, Sharron M, Pohlmann S, Sfakianos JN, Derdeyn CA, Blumenthal R, Hunter E, Doms RW. 2002. Sensitivity of HIV-1 to entry inhibitors correlates with envelope/coreceptor affinity, receptor density, and fusion kinetics. Proc. Natl. Acad. Sci. U. S. A. 99:16249–16254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Reeves JD, Miamidian JL, Biscone MJ, Lee FH, Ahmad N, Pierson TC, Doms RW. 2004. Impact of mutations in the coreceptor binding site on human immunodeficiency virus type 1 fusion, infection, and entry inhibitor sensitivity. J. Virol. 78:5476–5485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yu X, Lu L, Cai L, Tong P, Tan S, Zou P, Meng F, Chen YH, Jiang S. 2012. Mutations of Gln64 in the HIV-1 gp41 N-terminal heptad repeat render viruses resistant to peptide HIV fusion inhibitors targeting the gp41 pocket. J. Virol. 86:589–593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Borras-Blasco J, Navarro-Ruiz A, Borras C, Castera E. 2008. Adverse cutaneous reactions associated with the newest antiretroviral drugs in patients with human immunodeficiency virus infection. J. Antimicrob. Chemother. 62:879–888 [DOI] [PubMed] [Google Scholar]
- 34. Liu Z, Shan M, Li L, Lu L, Meng S, Chen C, He Y, Jiang S, Zhang L. 2011. In vitro selection and characterization of HIV-1 variants with increased resistance to sifuvirtide, a novel HIV-1 fusion inhibitor. J. Biol. Chem. 286:3277–3287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Melby T, Demasi R, Cammack N, Miralles GD, Greenberg ML. 2007. Evolution of genotypic and phenotypic resistance during chronic treatment with the fusion inhibitor T-1249. AIDS Res. Hum. Retroviruses 23:1366–1373 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.