Abstract
Background
Hospital readmission has attracted attention from policymakers as a measure of quality and a target for cost reduction. The aim of the study was to evaluate the frequency and patterns of rehospitalization after a pancreaticoduodenectomy (PD).
Methods
The records of all patients undergoing a PD at an academic medical centre for malignant or benign diagnoses between January 2006 and September 2011 were retrospectively reviewed. The incidence, aetiology and predictors of subsequent readmission(s) were analysed.
Results
Of 257 consecutive patients who underwent a PD, 50 (19.7%) were readmitted within 30 days from discharge. Both the presence of any post-operative complication (P = 0.049) and discharge to a nursing/rehabilitation facility or to home with health care services (P = 0.018) were associated with readmission. The most common reasons for readmission were diet intolerance (36.0%), pancreatic fistula/abscess (26.0%) and superficial wound infection (8.0%). Nine (18.0%) readmissions had lengths of stay of 2 days or less and in four of those (8.0%) diagnostic evaluation was eventually negative.
Conclusion
Approximately one-fifth of patients require hospital readmission within 30 days of discharge after a PD. A small fraction of these readmissions are short (2 days or less) and may be preventable or manageable in the outpatient setting.
Introduction
The Affordable Care Act (ACA) of 2010 set the foundation for a number of new quality measures for the health care system. Beginning as early as October of 2012, Medicare reimbursements will likely be decreased for 30-day hospital readmissions above a specified observed-to-expected ratio for acute myocardial infarction (AMI), heart failure and pneumonia.1 It is anticipated that the list of conditions to which these rules are applied will expand in the coming years. Complex abdominal surgery is of particular interest for cost savings given high rates of post-operative morbidity and readmission.
Pancreaticoduodenectomy (PD) has been the focus of readmission studies given post-operative morbidity rates of 40–60% and 30-day readmission rates ranging from 16–22% (Table 1).2–8 Readmission after a PD is commonly associated with a number of procedure-specific complications as well as with general post-operative complications and disease progression. While the debate continues regarding whether any of these readmissions are truly preventable, it is clear that there is an associated economic burden. A recent study by Kent et al. found an approximate increase in mean overall medical cost of $16 000 per patient readmitted after a PD ($41 000) relative to their non-readmitted counterparts ($25 000).2
Table 1.
Previous studies on incidence and predictors of readmission after a major pancreatic surgery
| Author | Year | Study period | Type | PD (n) | Readmission with 30 days from discharge | Predictors of readmission | Not predictors of readmission |
|---|---|---|---|---|---|---|---|
| Grewal et al.15 | 2011 | 2005–2010 | Single-institution | 124 | 18.5%a | LOS, chronic pancreatitis, transfusion | Commorbidities, complications, biliary stent, BMI, pylorus preservation, vascular reconstruction |
| Kent et al.2 | 2011 | 2001–2009 | Single-institution | 371 | 22% | Small duct (<3 mm), any/major complications, clinical or latent pancreatic fistula, DGE, SSI | Age, gender, BMI, ASA, POSSUM, malignancy, blood loss, transfusion |
| Reddy et al.8 | 2009 | 1992–2003 | SEER | 1309 | 16% | LOS > 10 days, distal pancreatectomy | Demographics, complications |
| Yermilov et al.4 | 2009 | 1994–2003 | OSHPD | 2023 | 19% | LOS, age >73 yrs, T-stage, comorbidity | Gender, race, nodal status |
Within 30–90 days after surgery.
ASA, American Society of Anesthesiologists Physical Status classification system; BMI, body mass index; DGE, delayed gastric emptying; EBL, estimated blood loss; LOS, length of stay; OSHPD, Office of Statewide Health Planning and Development database; PD, pancreaticoduodenectomy; POSSUM, Physiological and Operative Severity Score for the enumeration of Mortality and Morbidity predictor of risk; SEER, Surveillance Epidemiology and End Results database; SSI, surgical site infection.
With emerging political measures aimed at limiting the cost and improving the quality of the health care services provided in the United States, it will become increasingly important for practitioners to stay engaged, along with payers and hospital administrators, in defining expected disease- and procedure-specific outcomes. While decreasing readmission rates will benefit patients as well as the health care system, it is prudent to prevent the necessary readmission from being perceived as a ‘failed discharge’, but rather as a an ‘early rescue’.9 The current study aimed to further define the incidence, aetiology and characteristics of readmissions after a PD by evaluating a contemporary cohort of patients at a high-volume pancreatic surgery centre.
Methods
After obtaining institutional review board approval, the medical records of all patients undergoing a PD between January 2006 and September 2011 at our tertiary referral academic medical centre were retrospectively reviewed. Data were collected from the index hospitalization as well as all subsequent readmissions within 12 months of the index discharge. The time to readmission was defined using the day of index discharge as the day of reference. Readmissions to outside hospitals were not captured.
Individual patient data collection included basic demographics, pre-operative factors [diabetes mellitus (DM), coronary artery disease (CAD), hypertension (HTN), and tobacco use], intra-operative factors (estimated blood loss, major vascular reconstruction and pylorus preservation), postoperative outcomes and hospital length of stay (LOS).
Post-operative outcomes were identified by review of discharge International Classification of Diseases, 9th Revision (ICD-9) codes and by individual review of the medical record. Patients were considered to have a pancreatic fistula if they met a minimum of the criteria required for the diagnosis of a grade A fistula as defined by the International Study Group of Pancreatic Fistula (>3× normal serum amylase with no clinical manifestation).10 It should be noted, however, that drain fluid amylase was not routinely checked thus preventing the identification of some non-clinically relevant pancreatic fistulae. Similarly, the diagnosis of delayed gastric emptying (DGE) was applied to any patient who met at least the minimum criteria required for the diagnosis of grade A DGE as defined by the International Study Group of Pancreatic Surgery (one of the following: nasogastric tube required for more than 3 days, NGT reinserted after post-operative day three or inability to tolerate solid oral intake by post-operative day seven).11 A surgical site infection (SSI) was defined according to the commonly accepted Center of Disease Control (CDC) classification scheme.12
The post-operative care of the patients included in this study was left to the discretion of the attending surgeon in conjunction with the house staff. No fast-track programmes or post-operative pathways were instituted during the study period.
Readmission diagnoses were identified by ICD-9 codes and were confirmed by review of the associated admission note, daily progress notes and discharge summary. For the purpose of analysis, diagnoses were grouped into the following categories: procedure-related complications, general post-operative complications, readmission for diagnostic workup and others. The ‘procedure-related’ category included a pancreatic fistula, abdominal abscess/phlegmon, haemorrhage, cholangitis and per os (PO) intolerance. The ‘general post-operative’ category included SSI, urinary tract infection (UTI), deep venous thrombosis (DVT) and bacteraemia. The ‘negative diagnostic workup’ category included those patients readmitted with symptoms for whom no underlying diagnosis was identified after detailed evaluation. The ‘other’ category included admission for chest pain, ketoacidosis, dehydration, constipation and unrelated procedures.
Statistical analyses
Statistical analyses were performed using SAS statistical software (SAS Enterprise Guide 4.3; SAS Institute Inc., Cary, NC, USA). Demographic, pre-operative, intra-operative and post-operative factors were evaluated as predictors of readmission in univariate analyses. Student's t-test and chi-square were used to analyse continuous and categorical outcomes, respectively. A multivariate logistic regression was performed using factors of significance from the univariate analyses while controlling for patient age, gender, pre-operative comorbidities and disease pathology. Survival analysis was performed using non-parametric Kaplan–Meier methodology. All outcomes were considered statistically significant when P < 0.05.
Results
Two hundred fifty-seven (257) patients underwent a PD at our institution between January 2006 and September 2011. In-hospital mortality was 1.9% (n = 5, Fig. 1). Readmission rates were 19.7% (50/254) within 30 days, 24.0% (59/246) within 90 days, 27.4% (63/230) within 6 months and 37.4% (73/195) within 1 year from index discharge. The number of patients decreased as those who died were excluded and not all patients in the cohort had reached the indicated length of follow-up at the time of analysis. Twenty-three (8.9%) patients required multiple readmissions. There was no statistical difference in age, gender, pre- or intra-operative factors between patients requiring readmission within 30 days from index discharge and their non-readmitted counterparts (Table 2).
Figure 1.
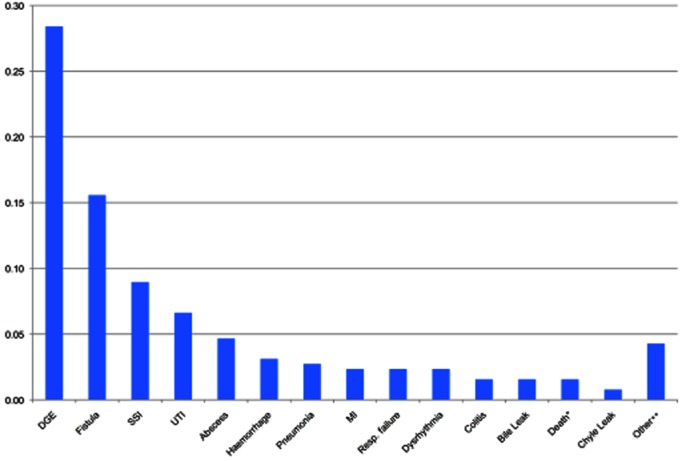
Post-operative complications during index hospitalization (% of all operations, n = 257). *Post-operative deaths: 3 deaths within 30 days of operation, 2 additional deaths during index hospitalization >30 days after operation (1.2% 30-day mortality, 1.9% in-hospital mortality). **Other (n = 1 for each complication noted): cerebral vascular accident, deep vein thrombosis, portal vein thrombus, pulmonary embolus, pseudoaneurysm without haemorrhage, biliary obstruction, bowel necrosis, decubitus ulcer, sepsis from indeterminate source and a complication from an unrelated procedure. DGE, delayed gastric emptying; SSI, surgical site infection; MI, myocardial infarction
Table 2.
Patient characteristics stratified by 30-day readmission
| Characteristic | No readmission (n = 207) | Readmission (n = 50) | P |
|---|---|---|---|
| Pre-operative factors | |||
| Age, years, mean (SD) | 64.4 (11.3) | 65.3 (13.7) | 0.633 |
| Female, n (%) | 83 (40.1) | 24 (48.0) | 0.309 |
| Hypertension, n (%) | 94 (45.4) | 21 (43.9) | 0.747 |
| Coronary artery disease, n (%) | 31 (14.9) | 3 (6.1) | 0.101 |
| Diabetes, n (%) | 50 (24.2) | 10 (20.4) | 0.578 |
| Current tobacco use, n (%) | 28 (13.5) | 4 (8.0) | 0.303 |
| Intra-operative factors | |||
| Estimated blood loss > 500 ml, n (%) | 112 (54.1) | 28 (56.0) | 0.830 |
| Vessel reconstruction, n (%) | 22 (10.6) | 2 (4.0) | 0.148 |
| Pylorus preservation, n (%) | 160 (77.3) | 36 (72.0) | 0.430 |
| Pathology | |||
| Malignant, n (%) | 157 (75.9) | 35 (70.0) | 0.393 |
The post-operative complications identified during index hospitalization included delayed gastric emptying (n = 73, 28.4%), pancreatic fistula (n = 40, 15.6%), surgical site infection (n = 23, 8.9%), urinary tract infection (n = 17, 6.6%), abdominal abscess (n = 12, 4.7%) and hemorrhage (n = 8, 3.1%) with 18 additional complications occurring in less than 3% of the study population (Fig. 1). One hundred fifty-nine patients (61.9%) experienced at least one post-operative complication.
Those not readmitted were less likely to have experienced a post-operative complication relative to their readmitted counterparts (58.9% versus 74%, P = 0.049). Readmitted patients experienced relatively higher rates of pancreatic fistulae, delayed gastric emptying and surgical site infections, but these trends failed to reach statistical significance (Table 3). In multivariate logistic regression controlling for patient age, gender, pre-operative comorbidities and disease pathology, the presence of any post-operative complication was associated with readmission with an odd ratio (OR) of 2.02 [95% confidence interval (CI) 1.02–4.21] (Table 4).
Table 3.
Factors associated with 30-day readmission
| No Readmission (n = 207) | Readmission (n = 50) | P | |
|---|---|---|---|
| Any complication, n (column %) | 122 (58.9) | 37 (74.0) | 0.049 |
| Pancreatic fistula, n (column %) | 30 (14.5) | 10 (20.0) | 0.335 |
| Delayed gastric emptying, n (column %) | 57 (27.5) | 17 (34.0) | 0.365 |
| Surgical site infection, n (column %) | 16 (7.7) | 7 (14.0) | 0.163 |
| Other complicationa, n (column %) | 55 (26.6) | 19 (38.0) | 0.119 |
| Disposition | |||
| Home, n (row %) | 175 (83.3) | 35 (16.7) | 0.018 |
| Home health care services, n (row %) | 15 (65.2) | 8 (34.8) | |
| Nursing/rehabilitation facilityx, n (row %) | 12 (63.2) | 7 (36.8) | |
| Index Hospitalization LOSa, mean (median, range) | 14.4 (11.0, 6–116) | 18.0 (11.0, 7–92) | 0.066 |
| Cumulative LOS, mean (median, range) | 15.9 (11.0, 6–122) | 30.3 (26.0, 8–153) | <0.001 |
Other: urinary tract infection (UTI), abscess, haemorrhage, pneumonia, myocardial infarction (MI), respiratory distress, dysrhythmia, death, colitis, bile leak, chyle leak, cerebral vascular accident, deep vein thrombosis, portal vein thrombus, pulmonary embolus, pseudoaneurysm without haemorrhage, biliary obstruction, bowel necrosis, decubitus ulcer, sepsis from indeterminate source and a complication from an unrelated procedure.
Table 4.
Multivariate logistic regression for predictors of 30-day readmissiona
| Odds ratio | 95% Confidence Interval | |
|---|---|---|
| Any post-operative complication | 2.02 | 1.02–4.21 |
| Non-routine discharge | 2.69 | 1.17–6.12 |
Controlled for age, gender, coronary artery disease (CAD), diabetes mellitus (DM), hypertension (HTN), tobacco use, malignant disease.
The level of care required at index discharge was associated with readmission. After routine discharge to home, patients had lower rates of 30-day readmission compared with patients discharged with home health services and as well as those discharged to nursing/rehabilitation facilities (16.7%, 34.8%, 36.8%, P = 0.018; Table 3). Multivariate logistic regression controlling for patient age, gender, pre-operative comorbidities and disease pathology, subsequently found non-routine discharge (discharge with home health services or discharge to nursing or rehab facility) to be associated with 30-day readmission with an OR of 2.69 (95% CI 1.17–6.12) (Table 4).
The median LOS for index admission was 11.0 days in both the readmitted and non-readmitted groups with the mean LOS 18.0 versus 14.4 days, respectively (P = 0.066; Table 3). The mean cumulative LOS (i.e. the summed LOS of index readmission and all subsequent readmissions within 1 year of index discharge) was, not surprisingly, significantly longer for patients requiring readmission within 30 days of index discharge (30.3 versus 15.9 days, P < 0.0001; Table 3).
Indications for readmission included procedure-related complications (n = 33, 66.0%), general post-operative complications (n = 7, 14.0%), negative fever workup (n = 4, 8.0%) and other (n = 6, 12.0%) (Table 5).
Table 5.
Primary diagnosis at 30-day readmission
| n (%) | |
|---|---|
| Procedure-cpecific complication | 33 (66.0) |
| PO intolerance | 18 (36.0) |
| Pancreatic fistula/abscess/phlegmon | 13 (26.0) |
| Haemorrhage | 1 (2.0) |
| Cholangitis | 1 (2.0) |
| General post-operative complications | 7 (14.0) |
| SSI | 4 (8.0) |
| UTI | 1 (2.0) |
| DVT | 1 (2.0) |
| Bacteraemia | 1 (2.0) |
| Negative fever workup | 4 (8.0) |
| Othera | 6 (12.0) |
Other: Negative workup for chest pain, ketoacidosis, dehydration, constipation, liver failure, unrelated procedure.
UTI, urinary tract infection; SSI, surgical site infection; DVT, deep vein thrombosis.
The median LOS for the readmissions was 6 days (range 1–32). Of 50 patients readmitted within 30 days, 9 (18.0%) had a readmission LOS of 1 to 2 days. Indications for these readmissions included fever with a negative workup (n = 3), an UTI (n = 1), cholangitis (n = 1), SSI (n = 1), PO intolerance (n = 1), chest pain with a negative workup (n = 1) and an unrelated procedure (n = 1) (Table 6). Therefore, 4 out of 9 patients readmitted for just 1 to 2 days were readmitted for diagnostic evaluation of symptoms (fever and chest pain) without identification of a specific diagnosis.
Table 6.
Characteristics of readmissions with length of stay (LOS) 1–2 days (n = 9)
| Patient | Readmission LOS (d) | Time from index discharge to readmission (days) | Readmission Dx |
|---|---|---|---|
| 1 | 1 | 8 | Fevera |
| 2 | 2 | 10 | Fevera |
| 3 | 2 | 23 | Fevera |
| 4 | 2 | 2 | UTI |
| 5 | 2 | 8 | SSI |
| 6 | 2 | 29 | Cholangitis |
| 7 | 1 | 8 | PO intolerance |
| 8 | 1 | 11 | Chest paina |
| 9 | 2 | 18 | Unrelated procedure |
Negative diagnostic workup.
UTI, urinary tract infection; SSI, surgical site infection; PO, per os.
Kaplan–Meier survival analysis revealed no discernible difference in survival for those readmitted relative to the non-readmitted cohort (Fig. 2, Table 7). This held true for patients with both benign and malignant disease.
Figure 2.
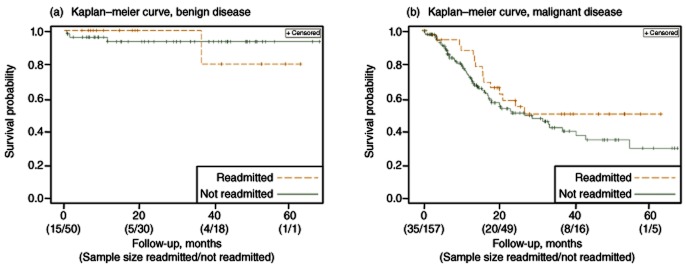
Kaplan–Meier survival curves: (a) Patients with benign disease, show no difference in survival when stratified by 30-day readmission (Log-Rank Chi-Square = 0.02, P = 0.88); (b) patients with malignant disease, show no difference in survival when stratified by 30-day readmission (Log-Rank chi-square = 1.51, P = 0.22)
Table 7.
Kaplan–Meier survival curves, number at risk
| Month 0 | Month 20 | Month 40 | Month 60 | |
|---|---|---|---|---|
| Benign, readmitted | 15 | 5 | 4 | 1 |
| Benign, not readmitted | 50 | 30 | 18 | 1 |
| Malignant, readmitted | 35 | 20 | 8 | 1 |
| Malignant, not readmitted | 157 | 49 | 16 | 5 |
Discussion
In the current study, 19.7% of all patients undergoing a PD were readmitted within 30 days of index discharge. Readmission was associated with the occurrence of any post-operative complication and with the level of care required at discharge. Readmitted patients had a longer mean index LOS relative to their non-readmitted counterparts, although this trend failed to reach statistical significance (18.0 versus 14.4 days, P = 0.066). Nine patients (18.0% of the readmitted patients) had readmission LOS of 1–2 days, four (8.0%) of whom were ultimately discharged after a negative diagnostic workup. There was no difference in survival between the readmitted and non-readmitted patients during the study period.
The findings of the present study are consistent with the reports by Emick et al. (2006) and Kent et al. (2011) both of whom found readmission after a PD to be associated with post-operative complications during the index hospitalization.2,13 In the current study, 80% of all readmissions were for indications related to the operation (66% procedure specific and 14% general post-operative) compared with 65% in the Kent et al. study (47% procedure specific and 18% general post-operative).2 Also congruent with the existing literature was the trend towards a longer index LOS for the patients requiring readmission. Emick et al. reported an increase in the mean index LOS for readmitted patients (13.8 versus 11.6 days, P = 0.02), an observation confirmed in two large administrative database reviews, suggesting that the shorter index hospitalization, or premature discharge, is not primarily responsible for readmission after a PD (Table 1).3,4,13
Our observation of a higher rate of readmission in patients discharged with home health services and those discharged to skilled nursing/rehab facilities is consistent with two previous reports.2,14 Specifically, in a prospective study of 266 patients undergoing major intra-abdominal procedures (including oesophageal, gastric, intestinal, liver and pancreatic resections), Martin et al. reported a 27% rate of readmission within 90 days from the index operation.14 Among the 72 patients who were readmitted, 62% were discharged with home health services and 19% to subacute rehabilitation as opposed to only 11% and 10% of their non-readmitted counterparts (P < 0.0001).14 In addition, only 25% of patients who got readmitted were seen by the treating physician before the readmission.14 These findings may certainly suggest that discharge resources are being appropriately allocated to sicker patients (i.e. those more likely to be readmitted). However, closer communication with the next level of caregivers and more intensified outpatient follow-up appear reasonable strategies for the timely identification and management of post-operative problems that may eventually lead to rehospitalization.
Of all 30-day readmissions in the present study, 18.0% (9/50) had a LOS of 2 days or less. Four of these patients (8.0% of all readmissions) underwent a negative diagnostic workup and were discharged without intervention. Kent et al. reported that of all patients readmitted after a major pancreatic resection, 14% presented with some element of clinical concern, but inpatient diagnostic evaluation failed to identify a specific diagnosis or complication.2 Perhaps this small fraction of readmitted patients could be evaluated in the outpatient setting or in a 23-h observational unit and then rehospitalized if diagnostic evaluation points to a specific diagnosis mandating inpatient care. This approach may prevent this small fraction (8–14%) of readmissions after a PD.
The present study has a number of limitations worthy of discussion. The single institution design may limit the generalizability of the results. Additionally, the present study did not capture readmissions to outside hospitals and may have underestimated the actual rate of rehospitalization after a PD. Interestingly, however, two recent administrative database analyses of patients undergoing a PD (capturing readmission data to any hospital) reported 30-day readmission rates of 16% and 19%.3,4 These data, when compared with both the present study (19.7% 30-day readmission rate) and the single-institution study performed by Kent et al. (22.1% 30-day readmission rate for PD patients) suggest that the majority of readmissions within 30 days of index discharge occur at the index hospital and that little 30-day readmission data are missed by single-institution studies.2 Finally, the low number (n = 9) of patients who were readmitted for only 1–2 days limit the ability to draw definitive conclusions regarding the preventability of such ‘short’ readmissions.
It is undeniable that hospital readmission is a burden on the health care system. A recent analysis of 11.8 million hospitalized Medicare beneficiaries found an overall 30-day readmission rate of roughly 20% (medical and surgical patients) at an annual cost of $17.4 billion.15 When the focus is major abdominal surgery, however, the issue of readmission as a quality metric is complex. In a recent editorial, Brown et al. put forth the notion that readmission of the post-surgical patient may lead to the early detection and ‘rescue’ of a peri-operative complication in the setting of good clinical judgment rather than represent a ‘failed discharge’.9
Moving forward, it is important for surgeons to stay engaged in policy discussions to ensure that novel quality metrics address the issues as they pertain to surgical patients. In the case of complex abdominal operations, such as a PD, the safest and most effective patient care may require a relatively low threshold for readmission. Clearly, coordination of care is imperative particularly with patients at a risk for re-admission. In patients with complications and the need for extended care post-discharge, a greater emphasis on post-discharge instruction and care could be brought forward. While it is probably true that a small fraction of readmissions after a PD may be preventable, we must approach this matter cautiously to avoid stigmatization of the necessary readmission. We as surgeons should at the very least participate in the discussion as public policy is developed in this area.
Conflicts of interest
None declared.
References
- 1.Affordable Care Act. Available at http://www.healthcare.gov/law/full/ (last accessed 2 February 2012)
- 2.Kent TS, Sachs TE, Callery MP, Vollmer CM. Readmission after major pancreatic resection: a necessary evil? J Am Coll Surg. 2011;213:515–523. doi: 10.1016/j.jamcollsurg.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 3.Yermilov I, Bentrem D, Sekeris E, Jain S, Maggard MA, Ko CY, et al. Readmissions following pancreaticoduodenectomy for pancreas cancer: a population-based appraisal. Ann Surg Oncol. 2009;16:554–561. doi: 10.1245/s10434-008-0178-6. [DOI] [PubMed] [Google Scholar]
- 4.Reddy DM, Townsend CM, Kou YF, Freeman JL, Goodwin JS, Riall TS. Readmission after pancreatectomy for pancreatic cancer in Medicare patients. J Gastrointest Surg. 2009;13:1963–1974. doi: 10.1007/s11605-009-1006-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grewal SS, McClaine RJ, Schmulewitz N, Alzahrani MA, Hanseman DJ, Sussman JJ, et al. Factors associated with recidivism following pancreaticoduodenectomy. HPB. 2011;13:869–875. doi: 10.1111/j.1477-2574.2011.00377.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yeo CJ, Cameron JL, Sohn TA, Lillimoe KD, Pitt HA, Talamini MA, et al. Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s: pathology, complications, and outcomes. Ann Surg. 1997;226:248–257. doi: 10.1097/00000658-199709000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pecorelli N, Balzano G, Capretti G, Zerbi A, Di Caprio V, Braga M. Effect of surgeon volume on outcome following pancreaticoduodenectomy in a high-volume hospital. J Gastrointest Surg. 2011;16:518–523. doi: 10.1007/s11605-011-1777-2. [DOI] [PubMed] [Google Scholar]
- 8.Riall TS, Cameron JL, Lillimoe KD, Campbell KA, Sauter PK, Coleman J, et al. Pancreaticoduodenectomy with or without distal gastrectomy and extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma – part 3: update on 5-year survival. J Gastrointest Surg. 2005;9:1191–1204. doi: 10.1016/j.gassur.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 9.Brown RE, Qadan M, Martin RC, Polk HC. The evolving importance of readmission data to the practicing surgeon. J Am Coll Surg. 2010;211:558–560. doi: 10.1016/j.jamcollsurg.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 10.Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8–13. doi: 10.1016/j.surg.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS) Surgery. 2007;142:761–768. doi: 10.1016/j.surg.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 12.Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol. 1992;13:606–608. [PubMed] [Google Scholar]
- 13.Emick DM, Riall TS, Cameron JL, Winter JM, Lillimoe KD, Coleman J, et al. Hospital readmission after pancreaticoduodenectomy. J Gastrointest Surg. 2006;10:1243–1252. doi: 10.1016/j.gassur.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 14.Martin RC, Brown R, Puffer L, Block S, Callender G, Quillo A, et al. Readmission rates after abdominal surgery: the role of surgeon, primary caregiver, home health, and subacute rehab. Ann Surg. 2011;254:591–597. doi: 10.1097/sla.0b013e3182300a38. [DOI] [PubMed] [Google Scholar]
- 15.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]


