Abstract
Background
To investigate whether intakes of calcium and dairy-servings within-recommendations were associated with plaque score when allowing for vitamin D intakes.
Methods
In this cross-sectional study, including 606 older Danish adults, total dietary calcium intake (mg/day) was classified as below vs. within-recommendations and dairy intake as <3 vs. ≥3 servings/ d. Dental plaque, defined as the percentage of tooth surfaces exhibiting plaque, was classified as < median vs. ≥median value (9.5%). Analyses were stratified by lower and higher (≥6.8 μg/d) vitamin D intake.
Findings
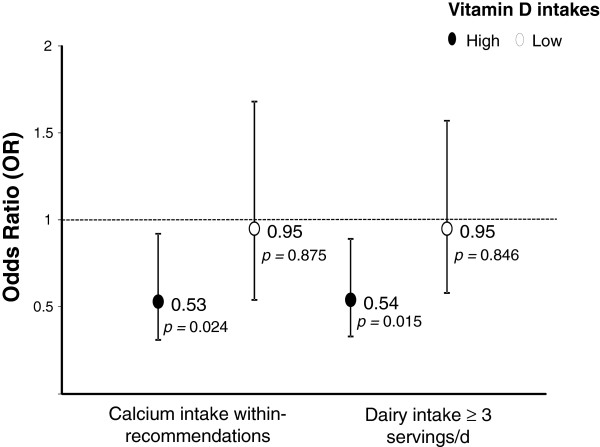
Intakes of calcium (OR = 0.53; 95% CI = 0.31–0.92) and dairy servings (OR = 0.54; 95% CI = 0.33–0.89) within-recommendations were significantly associated with lower plaque score after adjustments for age, gender, education, intakes of alcohol, sucrose and mineral supplements, smoking, diseases, number of teeth, visits to the dentist, use of dental floss/tooth pick and salivary flow, among those with higher, but not lower, vitamin D intake.
Conclusion
Intakes of calcium dairy-servings within-recommendations were inversely associated with plaque, among those with higher, but not lower, vitamin D intakes. Due to the cross-sectional nature of the study, it is not possible to infer that this association is causal.
Keywords: Calcium, Dairy-foods, Dental plaque, Older adults, Oral-health, Vitamin D
Background
Plaque, a deposit on tooth surfaces consisting of food debris and bacteria, is reduced by good oral hygiene, e.g. brushing and flossing [1]. Long-term plaque may lead to periodontitis and caries [2]. Prevention of these conditions is, therefore, primarily based on plaque control, though dietary factors may also be important [3].
Apart from studies investigating the association between the amount and frequency of free sugars intake and dental caries, little attention has been given to the importance of interactions between dietary nutrients or specific foods on oral health. So far, only few studies have investigated the associations between intake of dairy products (regardless of vitamin D consumption) and oral health [3].
High concentrations of calcium and phosphate in plaque or saliva may reduce bacterial adhesion to enamel and inhibit bacterial biofilm formation [4]. Higher calcium intake may also enhance enamel remineralisation, reduce demineralization [5] and prevent alveolar bone loss [6]. Additionally, casein may protect against caries by reducing bacterial adherence to teeth [7]. Dairy product intakes are particularly relevant as these foods are high in calcium, phosphate, and casein [8]. However, most populations consume substantially less dairy-foods than are recommended for provision of adequate intakes of calcium [9]. Furthermore, vitamin D is essential for calcium absorption [10], and promotes oral health through its effects on bone metabolism and innate immunity [11]. Our previous findings showed associations between tooth loss and calcium intake below recommendations [12] [data not examined for stratification with vitamin D status] and of periodontitis with low dairy calcium intakes with no variation with vitamin D intake [13].
The present study aimed to investigate whether within-recommendation intakes of calcium and dairy-servings are associated with dental plaque score among older adults with higher and lower vitamin D intakes.
Methods
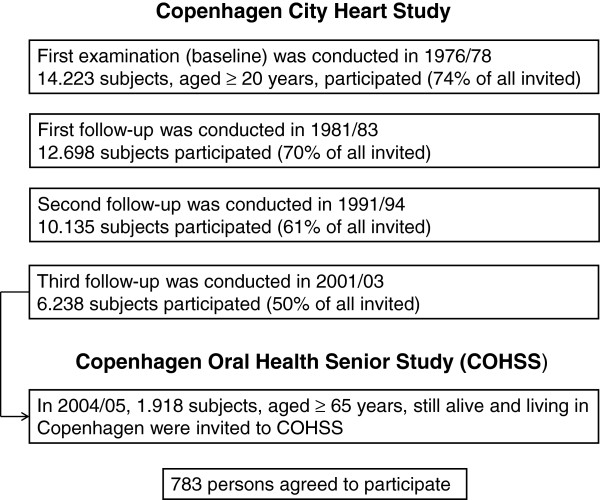
The Copenhagen Oral Health Senior Study (COHSS) 2004/05, addressed lifestyle factors and oral health in older adults. In total, 1918 of all 6238 subjects, who had participated in the third follow-up of the Copenhagen City Heart Study 2001/03 (detailed published elsewhere [14]), and were still alive, aged ≥65 years old, living in Copenhagen, able to communicate verbally and travel independently, were invited to participate in this oral health study (COHSS), and 783(40%) agreed to participate (Figure 1). Details of participants and non-participants are described elsewhere [15]. Briefly, a larger proportion of non-participants was older and of male gender vs. participants (P <0.001). COHSS was approved by local Ethical Committees (KF 01-144/01).
Figure 1.
Flow chart for participants in the Copenhagen Oral Health Senior Study.
Dietary assessment
Dietary data were collected using a ‘diet history interview’ based on information about diet in the past month, validated for use in older populations [16]. Participants reported on meal contents and patterns at interview through pre-coded questions. Quantitative information on meals, food intakes and portion sizes was collected using photo-series, cups and measures. All interviews were performed by a single dietician.
Total dietary and supplemental intakesb of vitamin D2 + D3 (μg/d) were estimated. Total vitamin D intakes were within-recommendations (15 μg/d for adults aged 51–70 y; 20 μg/d for ≥71 y) [17] in 4% of subjects and intake was, therefore, classified as < median vs. ≥median (6.8 μg/d).
Total dietary and supplemental calcium intakes were classified as: below vs. within recommendations (1000 and 1200 mg/day for men aged 51–70 and >70 y respectively; 1200 mg/d for women aged ≥ 51 y) [17]. Due to limited information on calcium contents of the supplements used, 800 mg was added to the total amount of calcium intake, but only for those who reported taking calcium supplements daily. Total dairy food intake: <3 vs. ≥3 servings/d, as recommended for elders, by the Food Guide Pyramid [18]. Dairy servings refer to one cup of milk, one slice of cheese or one medium yogurt pot.
Oral examination
One dentist (KH) trained by an experienced clinical examiner (PH-P), performed all oral examinations, including determination of un-stimulated salivary flow rates [19], number of teeth and visible plaque at six sites per tooth, modified from Silness & Löe [20].
Plaque score was determined as % of sites with plaque amongst total sites examined, classified as scoring < median vs. ≥median (9.5%).
Covariates
These included age, gender and primary education (≤7 vs. >7 y), current smoking (yes/no) and intakes of alcohol (above vs. within-recommendations from the Danish National Board of Healtha[21]), sucrose (≤10% vs. >10% of total energy intake, matching suggested thresholds for increased caries rates and lower vitamin and mineral intakes [22]), and daily mineral supplements (yes/no) over the previous year.
From a questionnaire covering 14 common diseases (e.g. cardiovascular, metabolic, respiratory, hepatic, urinary diseases), current ‘medical condition’ was classified as 0–4 vs. ≥5 diseases [15].
Most subjects (98%) reported daily tooth brushing; therefore regular use of dental floss or tooth pick was used for assessing oral hygiene. Elapsed time since last dental-care visit (≤12 vs. >12 months), number of teeth, and salivary flow were included in analyses.
Statistical analysis
Descriptive statistics were presented as ‘mean (±SD)’ or ‘percentage (n)’. Logistic regression was used to assess relationships between calcium and dairy intakes within-recommendations and plaque scores, stratified by vitamin D intakes. Data were analysed with STATA (StataCorp 9.2, TX-USA).
Results
Of the 783 participants, 96 were edentulous, 78 did not complete the questionnaires, leaving a study population of 606 partial or fully dentate participants with complete information on diet, plaque score and covariates for inclusion in our cross-sectional analyses. Participants did not differ for age, gender, smoking, alcohol, sucrose consumption or medical condition from non-participants. However, non-participants had lower education, used dental floss/tooth pick and visited a dentist less often than participants (data not shown, P <0.05).
Total dietary calcium intake ranged from 161 mg to 3439 mg. Dental plaque score ranged from 0% to 90%. Descriptive data are presented in Table 1. Individuals reporting calcium intake below recommendations were older, had higher alcohol consumption, lower vitamin D and dairy-servings intakes and fewer teeth compared to those with adequate calcium intake.
Table 1.
General characteristics of the study population
| |
Calcium intake according to recommendations |
|||
|---|---|---|---|---|
| Characteristics | Total % (n) | Below % (n) | Within % (n) | P |
| Age* |
75.5 (6.4) |
75.9 (6.3) |
74.4 (6.6) |
0.01 |
| ≤ 7 y of education |
30.7 (186) |
32.1 (144) |
26.6 (42) |
0.20 |
| Males |
39.4 (239) |
36.2 (162) |
48.7 (77) |
0.005 |
| Smoking |
22.4 (136) |
23.4 (106) |
19 (30) |
0.226 |
| Vitamin D intake < 6.8 μg/d |
50.7 (307) |
52.9 (237) |
44.3 (70) |
0.063 |
| Vitamin D intake (μg/d )* |
7.4 (4.9) |
7.1 (4.8) |
8.2 (5.1) |
0.02 |
| Calcium intake (mg/d)* |
989 (460) |
776 (211) |
1591 (439) |
< 0.0001 |
| Dairy intake < 3 servings/d |
62.4 (378) |
80.6 (361) |
10.8 (17) |
< 0.001 |
| > 10% energy from sucrose |
16.2 (98) |
15.4 (69) |
18.3 (29) |
0.386 |
| Alcohol > recommendations |
28.7 (174) |
31 (139) |
22.1 (35) |
0.048 |
| Current diseases ≥ 5 |
52 (315) |
51.6 (231) |
53.2 (84) |
0.729 |
| > 12 months since last dental care visit |
8.7 (53) |
9.1 (41) |
7.6 (12) |
0.551 |
| No regular use of dental floss/tooth pick |
59 (357) |
60.9 (273) |
53.2 (84) |
0.09 |
| Number of teeth* |
20.2 (7.8) |
19.8 (7.9) |
21.3 (7.4) |
0.03 |
| Plaque Score (%)* | 14.4 (20) | 14.9 (21) | 13.2 (19) | 0.370 |
Data presented as % (n) unless otherwise stated. * Data presented as mean (SD).
Table 2 shows the overall associations of calcium, dairy products and vitamin D intakes with plaque score. The results showed protective effects of calcium, dairy products and vitamin D intakes on plaque score, but none of the associations were statistically significant. When the analysis were stratified by vitamin D intake, it was observed that increased intakes of calcium and dairy-servings (within-recommendations) were significantly associated with lower plaque score, amongst those with higher vitamin D intakes, after adjustment for age, gender, education, intakes of alcohol, sucrose and mineral supplements, smoking, current diseases, number of teeth, visits to the dentist, use of dental floss/tooth pick and salivary flow. Associations were not significant amongst those with lower vitamin D intakes (Figure 2).
Table 2.
Overall associations of calcium, dairy products and vitamin D with plaque score
| Calcium | Within recommendations | Below recommendation | P | |
|---|---|---|---|---|
| |
n |
158 |
448 |
|
| |
OR (95% CI) |
0.72 (0.49-1.0) |
1.0 |
0.090 |
|
Dairy products |
|
≥ 3 servings/day |
< 3 servings/day |
P |
| |
n |
228 |
378 |
|
| |
OR (95% CI) |
0.72 (0.51-1.0) |
1.0 |
0.057 |
|
Vitamin D |
|
≥ median |
< median |
P |
| |
n |
299 |
307 |
|
| OR (95% CI) | 0.96 (0.68-1.35) | 1.0 | 0.083 |
Models adjusted for age, gender, education, intakes of alcohol, sucrose and mineral supplements, smoking, current diseases, number of teeth, visits to the dentist, use of dental floss/tooth pick and salivary flow.
Plaque score classified as < vs. ≥ 9.5%.
Figure 2.
Association between calcium and dairy servings intakes and plaque score, stratified by vitamin D intakes. Models adjusted for age, gender, education, intakes of alcohol, sucrose and mineral supplements, smoking, current diseases, number of teeth, visits to the dentist, use of dental floss/tooth pick and salivary flow. Plaque score classified as < vs. ≥ 9.5%. Analyses were stratified by lower and higher (≥6.8 μg/d) vitamin D intake.
Additional subgroup analyses by gender, age, alcohol consumption and number of teeth were performed, but no significant difference between groups were found.
Discussion
Our findings show that higher intakes of calcium and dairy-servings (within-recommendations) are associated with lower plaque scores, when vitamin D intakes are ≥6.8 μg/d, but not when intakes are <6.8 μg/d.
To our knowledge, this is the first observational study examining associations between calcium and dairy-servings intakes and plaque score. However, consistent evidence suggests that higher intakes of calcium, dairy-foods and vitamin D are inversely associated with caries and periodontitis [8,11,23], though earlier studies on dairy-foods and oral health have not stratified analyses by vitamin D intake.
Dietary calcium absorption is critical for calcium availability for bone mineralization [17] and vitamin D status is an important factor influencing intestinal calcium absorption [24]. Our data, therefore, suggests that better vitamin D intakes facilitate beneficial effects of higher calcium intakes, probably by enhancement of calcium absorption.
Weaknesses of this study include the high drop-out rate from the original cohort and exclusions due to insufficient data availability. However, participants and non-participants showed no significant differences in major socio-demographic and lifestyle characteristics. Lower risks in participants would have led to underestimations rather than overestimates of the reported associations. Another limitation was the lack of detailed data for supplemental calcium intakes. However, underestimates of total calcium intake would have attenuated the significance of our findings.
Silness & Löe’s method for plaque assessment [20] focusses on plaque quantity at time of inspection and does not reveal how long plaque has been present. In considering plaque as an etiological risk-factor for caries and periodontitis, time must be a most important factor [2]. Human responses and individual susceptibility to plaque vary with gender, ethnicity, medical status, genotype and manual dexterity for achieving a satisfactory level of oral cleanliness through self-care [1]. Therefore, individuals with similar hygiene practices may present different plaque scores. In this study, higher intakes of calcium and dairy-foods were associated with a lower plaque score, even after adjustment for many socio-demographic factors, health conditions, lifestyle and oral hygiene, influencing plaque formation.
Kappa for intra-examiner plaque assessment was not calculated in this study. However, for caries assessment the Kappa-value for the intra-observer reliability was 0.97, which may be considered as excellent agreement. Since visual inspection of detectable plaque is a much simpler procedure for an experienced dentist, it is reasonable to assume that the present study was unlikely to have been significantly affected by intra-observer variation.
Finally, most participants reported daily tooth brushing, but it was not possible to distinguish between tooth brushing once or twice a day.
Conclusion
Our cross-sectional data corroborate the hypothesis that calcium and dairy-foods intakes within-recommendations are associated with lower plaque scores [23] amongst those with higher, but not lower, vitamin D intakes. However, it is not possible to infer that these associations are causal. Given the high percentage of individuals with below-recommendation intakes of calcium and vitamin D, consumption of foods rich in calcium and providing vitamin D at 6.8 μg/day or more should be promoted, as it may contribute to reduction of plaque formation and protection of oral health, whilst awaiting data from further studies on the effects of intakes of vitamin D currently advised by the Institute of Medicine [17] or above, on dental health.
Endnotes
a The Danish National Board of Health recommends a maximum consumption of 168 g alcohol/wk for women and 252 g alcohol/wk for men.
b For daily supplemental vitamin D, multivitamins, or cod-liver oil, intakes of 10 μg, 5 μg or 6 μg of vitamin D were added, respectively.
Abbreviations
COHSS: Copenhagen Oral Health Senior Study; CI: Confidence interval; d: Day; OR: Odds ratio; SD: Standard deviation; vs: Versus; wk: Week; y: Years.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
ARA carried out the statistical analysis and did most of the writing. BJB contributed to plans for data analysis. PH-P and KA designed and supervised the study. All authors helped draft the manuscript and read and approved the final manuscript.
Contributor Information
Amanda RA Adegboye, Email: AAR@ipm.regionh.dk.
Lisa B Christensen, Email: lbch@sund.ku.dk.
Poul Holm-Pedersen, Email: holmp@sund.ku.dk.
Kirsten Avlund, Email: kiav@sund.ku.dk.
Barbara J Boucher, Email: bboucher@doctors.org.uk.
Berit L Heitmann, Email: blh@ipm.regionh.dk.
Acknowledgments
We thank Claus Holt for statistical advice and Karen Heegaard (KH) for data collection and database creation. This study was supported by the Zendium Household & Body Care Research Foundation, the Danish Dental Association Research Foundation (FUT⁄Calcin), the Tryg-Foundation, and the Danish Dairy Research Foundation.
References
- White DJ. Dental calculus: recent insights into occurrence, formation, prevention, removal and oral health effects of supragingival and subgingival deposits. Eur J Oral Sci. 1997;105:508–522. doi: 10.1111/j.1600-0722.1997.tb00238.x. [DOI] [PubMed] [Google Scholar]
- Broadbent JM, Thomson WM, Boyens JV, Poulton R. Dental plaque and oral health during the first 32 years of life. J Am Dent Assoc. 2011;142:415–426. doi: 10.14219/jada.archive.2011.0197. [DOI] [PubMed] [Google Scholar]
- Moynihan PJ. The relationship between nutrition and systemic and oral well-being in older people. J Am Dent Assoc. 2007;138:493–497. doi: 10.14219/jada.archive.2007.0201. [DOI] [PubMed] [Google Scholar]
- Danielsson NL, Hernell O, Johansson I. Human milk compounds inhibiting adhesion of mutans streptococci to host ligand-coated hydroxyapatite in vitro. Caries Res. 2009;43:171–178. doi: 10.1159/000213888. [DOI] [PubMed] [Google Scholar]
- Ferrazzano GF, Cantile T, Quarto M, Ingenito A, Chianese L, Addeo F. Protective effect of yogurt extract on dental enamel demineralization in vitro. Aust Dent J. 2008;53:314–319. doi: 10.1111/j.1834-7819.2008.00072.x. [DOI] [PubMed] [Google Scholar]
- Krall EA, Wehler C, Garcia RI, Harris SS. wson-Hughes B. Calcium and vitamin D supplements reduce tooth loss in the elderly. Am J Med. 2001;111:452–456. doi: 10.1016/S0002-9343(01)00899-3. [DOI] [PubMed] [Google Scholar]
- Llena C, Forner L, Baca P. Anticariogenicity of casein phosphopeptide-amorphous calcium phosphate: a review of the literature. J Contemp Dent Pract. 2009;10:1–9. [PubMed] [Google Scholar]
- Merritt J, Qi F, Shi W. Milk helps build strong teeth and promotes oral health. J Calif Dent Assoc. 2006;34:361–366. [PubMed] [Google Scholar]
- Fulgoni VL III, Huth PJ, DiRienzo DB, Miller GD. Determination of the optimal number of dairy servings to ensure a low prevalence of inadequate calcium intake in Americans. J Am Coll Nutr. 2004;23:651–659. doi: 10.1080/07315724.2004.10719407. [DOI] [PubMed] [Google Scholar]
- Christakos S, Dhawan P, Porta A, Mady LJ, Seth T. Vitamin D and intestinal calcium absorption. Mol Cell Endocrinol. 2011;347:25–29. doi: 10.1016/j.mce.2011.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon D, Hildebolt CF, Miley DD, Garcia MN, Pilgram TK, Couture R, Anderson SC, Civitelli R. Calcium and vitamin D use among adults in periodontal disease maintenance programmes. Br Dent J. 2009;206:627–631. doi: 10.1038/sj.bdj.2009.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adegboye AR, Fiehn NE, Twetman S, Christensen LB, Heitmann BL. Low Calcium Intake Is Related to Increased Risk of Tooth Loss in Men. J Nutr. 2010;140:1864–1868. doi: 10.3945/jn.109.117770. [DOI] [PubMed] [Google Scholar]
- Adegboye AR, Christensen LB, Holm-Pedersen P, Avlund K, Boucher BJ, Heitmann BL. Intake of dairy products in relation to periodontitis in older danish adults. Nutrients. 2012;4:1219–1229. doi: 10.3390/nu4091219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appleyard M, Hansen A, Schnohr P, Jensen G, Jensen G, Nyboe J. A book of tables with data from the first examination (1976–78) and a five-year follow-up (1981–83) Scand J Soc Med. 1989;170:1–160. [PubMed] [Google Scholar]
- Heegaard KM, Holm-Pedersen P, Bardow A, Hvidtfeldt UA, Gronbaek M, Avlund K. The Copenhagen Oral Health Senior Cohort: design, population and dental health. Gerodontology. 2011;28:165–176. doi: 10.1111/j.1741-2358.2010.00383.x. [DOI] [PubMed] [Google Scholar]
- Pedersen AN, Fagt S, Ovesen L, Schroll M. Quality control including validation in dietary surveys of elderly subjects. The validation of a dietary history method (the SENECA-method) used in the 1914-population study in Glostrup of Danish men and women aged 80 years. J Nutr Health Aging. 2001;5:208–216. [PubMed] [Google Scholar]
- Ross CA, Taylor CL, Yaktine AL, Del Vale HB. Dietary Reference Intakes for Calcium and Vitamin D. Washington D.C: Institute of Medicine; The National Academies Press; 2011. [PubMed] [Google Scholar]
- Shaw AM, Escobar AJ, Davis P. Reassessing the Food Guide Pyramid: Decision-Making Framework. J Nutr Educ. 2000;32:111–118. doi: 10.1016/S0022-3182(00)70528-0. [DOI] [Google Scholar]
- Smidt D, Torpet LA, Nauntofte B, Heegaard KM, Pedersen AM. Associations between oral and ocular dryness, labial and whole salivary flow rates, systemic diseases and medications in a sample of older people. Community Dent Oral Epidemiol. 2011;39:276–288. doi: 10.1111/j.1600-0528.2010.00588.x. [DOI] [PubMed] [Google Scholar]
- Silness J, Loe H. Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22:121–135. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- National Board of Health, DK [Internet]. [Cited 2010 Feb 3] http://www.sst.dk.
- Committee on Medical Aspects of Food Policy, Department of Health. Dietary Sugars and Human Disease. 1989.
- Grant WB, Boucher BJ. Are Hill’s criteria for causality satisfied for vitamin D and periodontal disease? Dermatoendocrinol. 2010;2:30–36. doi: 10.4161/derm.2.1.12488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gueguen L, Pointillart A. The bioavailability of dietary calcium. J Am Coll Nutr. 2000;19:119S–136S. doi: 10.1080/07315724.2000.10718083. [DOI] [PubMed] [Google Scholar]