Abstract
Objective
Health care workers are at high risk of developing musculoskeletal symptoms and pain. This study tested the hypothesis that sleep deficiency is associated with pain, functional limitations, and work-interfering physical limitations.
Methods
Hospital patient care workers completed a survey (79% response rate) including measures of health, sociodemographic, and workplace factors. Associations of sleep deficiency with pain, work interference due to this pain, and functional limitations were determined.
Results
Of 1572 respondents (90% women; mean age 41 years) fifty-seven percent reported sleep deficiency, 73% pain in last 3 months, 33% work interference, 18% functional limitation. Sleep deficiency was associated with higher rates of pain, work interference, and functional limitation controlling for socioeconomic, individual, and workplace characteristics.
Conclusions
Sleep Deficiency is significantly associated with pain, functional limitation and workplace interference, suggesting modifiable outcomes for workplace health and safety interventions.
Keywords: Occupational health practice, Sleep, Musculoskeletal, Epidemiology
Introduction
This study is part of the inaugural project for the Harvard School of Public Health Center for Work, Heath, and Wellbeing exploring how policies, programs and practices on the healthcare unit impact the work and health of these workers. Health care workers are at a high risk of developing musculoskeletal symptoms, pain, injuries and disorders. Health care is a rapidly growing industry(1) composed of an aging workforce,(2) such that the rates of these injuries and chronic conditions are expected to raise the level of disability in the workforce and force some employees from the field. Estimates of the annual incidence of back injury and pain in the nursing workforce range between 30% and 75% and of the lifetime incidence between 35% and 80%.(3-13) Nursing aides suffer from back pain involving days away from work at rate of 28 per 10,000 full-time workers compared to the national average of 4, the highest of any occupation. Those suffering from any pain involving days away from work had a rate of 68 per 10,000 full-time workers compared to the national average of 13, a rate second only to that observed in police officers.(14) The physical demands of nursing work, including patient handling, are suspected as the major factor associated with the high rates of musculoskeletal symptoms and disorders of the lower back and other body parts.(15) Various interventions have been implemented to reduce risk for chronic musculoskeletal disorders including education programs, programs to reduce physical load such as conditioning and exercise programs, or the use of mechanical lifts or other patient transfer equipment and organizational changes such as prompt disability management.(16-18) In addition, occupational factors such as the psychosocial environment and organizational support are associated with pain, though not in all studies,(9) and are thought to interfere with pain resolution and return to full functionality.(19, 20)
Less clear is the role of sleep in mediating the effects of work and workplace factors on pain. Habitual short sleep duration independently predicts the risk of a fall or other injury requiring an Emergency Room visit.(21) In healthcare workers, decreased sleep duration and extended shifts, as seen in shift work, have been related to workplace injuries (Hopcia K, Dennerlein JT, Hashimoto DM, Stoddard AM, Orechia T, Sorensen G. Hospital Registered Nurses and Patient Care Associate Injuries on Units With and Without Ceiling Lifts. (Under Review)). Mechanisms involved are thought to include the increased sleepiness associated with inadequate sleep.(22) Laboratory studies of sleep restriction have noted an increase in spontaneous pain reports (23, 24) and an increase in the response to a standard pain stimulus.(25, 26) Insomnia is also associated with an increased incidence of pain.(27-29)
Sleep deficiency, a new term (30), marks the presence of short sleep duration and/or sleep insufficiency (31), such as by a sleep disorder and reflects unmet sleep need that further results in suboptimal health, performance, or well-being (32, 33). Short sleep duration and/or sleep insufficiency has been linked to weight gain, obesity, type 2 diabetes, elevated blood pressure, cardiovascular disease, and premature mortality.(34-39) Together, these health outcomes represent a large portion of morbidity and mortality both in the United States(40) and the world.(41)
A number of studies have examined the role of sleep disturbance on work disability, and worker physical and psychological health.(42, 43) Conversely, both cross-sectional and longitudinal analyses of workplace stressors have been shown to contribute to sleep disturbances.(44)
The goal of this paper is to test the hypotheses that sleep deficiency is associated with self-reported pain, work interference due to this pain, and functional limitations. Change in functional limitations may impact productivity or the ability to perform demanding healthcare work. It was hypothesized that, in a socio-ecological framework that includes individual, occupational, and workplace characteristics, sleep deficiency (short sleep duration, insomnia symptoms, and/or sleep insufficiency) would be independently associated with outcomes of pain, work interference, and functional limitations while controlling for key covariate indicators of work organization and experiences. A sleep deficiency composite variable was defined and the contributions of the components to the associations with the outcomes were described to establish sleep deficiency as a useful concept for future research.
Methods
Study Design
This study focuses on cross-sectional survey data collected from patient care workers at two large academic hospitals in metropolitan Boston October 2009-January 2010. Research protocols approved by the applicable Institutional Review Board were conducted in accordance with the Declaration of Helsinki.
Study sample
A Human Resources database at each hospital was used to identify eligible employees. The sampling frame for the Patient Care Worker Survey included all current benefits-eligible workers employed in Patient Care Services who had direct patient care responsibilities during May 30, 2009 - August 22, 2009. Eligible employees worked on a unit defined primarily as a patient care unit. Staff assigned to the “float” unit were eligible but those assigned to environmental services and physical medicine units (Physical therapy, Occupational Therapy, Speech Therapy, etc.) were excluded. Workers on extended absence >12 weeks, per diem staff, traveling/contract nurses, administrative workers, and those working <20 hours/week on average or with jobs not exclusively related to a specific unit were ineligible. From 7019 eligible workers (3474 from one hospital, 3545 from the other), a random sample of 2000 was selected. Detailed shift information was extracted from a payroll database to create a nightshift variable (see below).
Data collection
Eligible employees and directors were sent an introductory email and a personalized link to the web-based survey. A second email was sent two weeks later to anyone who had not completed the survey. A paper survey was sent to the home of those who did not complete the online survey with a stamped return envelope followed by one more email and mailed survey at two-week intervals for a total of up to 5 contacts. A $20 gift card was given to participants. A total of 1572 workers initiated the survey online and 1399 (89%) completed at least 50% of the items, the eligibility requirement for this analysis; 173 workers completed a paper version. The total number of completed surveys was 1572 (response rate: 79%).
Measures
Outcomes
Pain was measured using an adaption of the Nordic question for musculoskeletal systems,(45) “During the past 3 months, have you had pain or aching in any of the areas shown on the diagram?” Using a diagram as a reference, respondents were asked to identify areas in which they experienced pain: lower back, shoulder, wrist or forearm, knee, neck, ankle or feet, or none of the above.
Work interference due to pain reported in the modified Nordic question for musculoskeletal systems: “In general how much did this pain interfere with your normal work?” Responses were on a five-point scale from “Not at all” to “Extremely.” Work interference was defined as a response of moderately or greater.
Functional limitation was assessed by a series of questions asking the participant about their ability to do a list of activities in the last week. For each activity they rated their ability on a five point scale from 1 = “No difficulty” to 5 = “Unable to do without help.” The activities included heavy household chores, carry a shopping bag or brief case, recreational activities in which there is impact in the arm, shoulder or hand, stand for an hour or more, reach for an object on a high shelf, put on shoes or socks, get in or out of a car, stoop or bend toward the floor, kneel or squat and use any hand held tool or equipment. The scores were summed resulting in a scale that ranged from 10 (no difficulty on any item) to 50 (unable to do any of the 10 items without help). Functional limitation was defined to be a score of ≥14, the 83rd percentile.(46)
Covariates
All covariates were determined a priori.
Respondents answered questions regarding their sleep habits in the preceding four weeks. Sleep duration was assessed by asking how many hours respondents slept each night. Sleep insufficiency was assessed by asking how often they got enough sleep to feel rested upon waking, with five response categories from never to always, similar to the previously used term sleep adequacy(30, 47). Insomnia symptoms were assessed by asking how often they woke in the middle of the night or early with four response categories from not at all in the last 4 weeks to 3 or more times a week. In an exploratory analysis, Sleep deficiency was defined as the presence of short sleep duration (<6h/day) or sleep insufficiency (never feeling rested on waking) or insomnia symptoms 3 or more times a week.
For sociodemographic factors, participants reported their occupation, race/ethnicity, education, gender, age, height and weight. BMI was computed as weight (kg) per meter squared (m2) of height.
Psychological distress was measured using the K-6 Non-specific Distress Scale,(48) a six item scale that asks how often the respondent has felt the following ways in the last 30 days: “So sad nothing could cheer you up,” “Nervous,” “Restless or fidgety,” “Hopeless,” “That everything was an effort,” “Worthless.” Responses were on a five point scale from 0= “None of the time” to 4= “All of the time.” Responses to the six items were summed resulting in a scale that ranged from 0 to 24.
Unit category
Participants worked in 128 patient care units. The patient care units were grouped into 12 categories reflecting similar workloads based on type of unit, acuity, staffing, physical location, and number of beds. The categories are: Emergency Department (ER), Operating Room (OR), Adult Medical/Surgical, Adult intensive care (ICU), step-down, Pediatric Medical/Surgical, Pediatric/Neonatal intensive care, Psychiatry, Obstetrics/Postpartum, Float Pool, Ambulatory units and Orthopedics.
Total work hours was assessed by self-report about a typical week (<20, 20-29, 30-34, 35-39, 40-44, 45-50, and >50 hours).
Job title was categorized as staff nurse (Assistant Nurse Manager, Clinical Nurse Specialist, Staff Nurse), Patient Care Associate, or other (Operations Coordinator and other).
Two measures of social support on the job were included. Coworker support was assessed using two items: (“If needed, I can get support and help with my work from my co-workers,” “The people I work with are helpful in getting the job done,”) with 5 response categories from 1 = “never” to 5 = “always.” The responses were summed resulting in a scale that ranged from 2 to 10.(49)Supervisor support was measured using three items (“If needed, I can get support and help with my work from my immediate supervisor,” “My supervisor is helpful in getting the job done,” “My work achievements are appreciated by my immediate supervisor,”) with response categories on the same five point scale. The responses were summed resulting in a scale (range: 3-15).(49)
Job demands were determined using an abbreviated version of the Job Content Questionnaire (JCQ),(49) with a focus on the psychological job demand sub-scales (5 items) with equally weighted responses summed and scaled (range: 12-48).
Nightwork shifts were quantified from administrative payroll data during the period October 2008-August 2009 compiled as the average number of hours between 10pm and 6am for those months worked, excluding shifts <4 hrs, and categorized as 0-6, 6-72, and >72 hrs/month.
Analysis
Associations between sleep variables and pain, work interference and functional limitations, controlling for other worker and work characteristics were examined using simple and multiple logistic regression analysis (SAS statistical software 9.2, SAS Institute, Inc. Cary, NC). Odds ratios are reported with 95% confidence intervals.
Results
Of the 1572 respondents, 90% were women, with a mean age of 41.4 years (s.d.=11.7), and a mean BMI of 26.3 kg/m2 (s.d.=5.3).
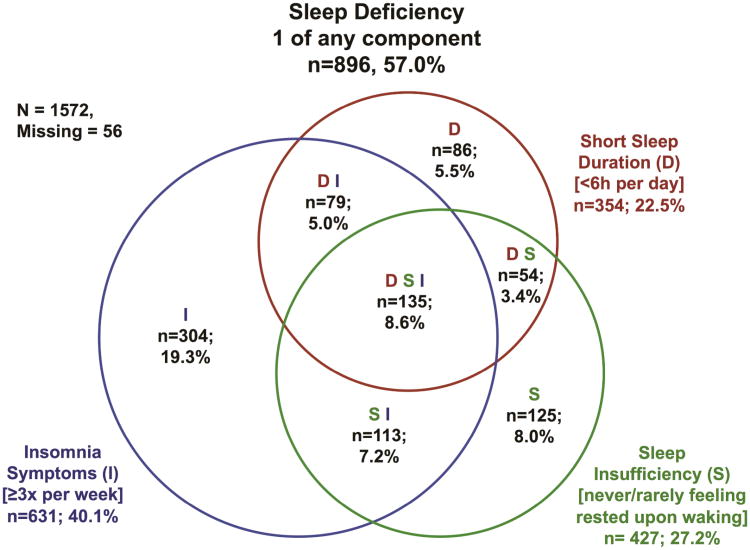
Table 1 presents the bivariate associations of the participant characteristics with each of the sleep variables. Short sleep duration was reported by 22.5% of total respondents, sleep insufficiency by 27.2%, and insomnia symptoms by 40.1%. Figure 1 depicts the frequencies of the sleep variables, numbers missing, and their overlap with one another. Pain was reported by 73.4%, functional limitation by 17.6%, and work interference by 32.8% of the entire sample.
Table 1.
Frequency (and percent) or mean (± standard deviation) of respondent characteristics by presence or absence of deficiency within each of the three sleep variables, duration, quality, and insomnia symptoms, with p-value for test of no association with the sleep variables. Significant p-values are bolded. Variables significant across all three sleep variables are also bolded and include any pain, work interference, functional limitation, and psychological distress.
| Sleep Duration | Sleep Sufficiency | Insomnia Symptoms | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| <6 hrs/night (N=354) |
≥ 6hrs/night(N=1115) | p | Never/Rarely (N=428) |
Sometimes/Often/ Always(N=1075) |
p | ≥ 3times/wk (N=631) |
<3 times/wk (N=872) |
p | |||
| Any Pain | No | 73 (20.6%) | 312 (28.0%) | 0.006 | 87 (20.3%) | 306 (28.5%) | 0.001 | 130 (20.6%) | 268 (30.7%) | < 0.0001 | |
| Yes | 281 (79.4%) | 803 (72.0%) | 341 (79.7%) | 769 (71.5%) | 501 (79.4%) | 604 (69.3%) | |||||
|
| |||||||||||
| Work Interference | No | 206 (58.7%) | 781 (70.3%) | < 0.0001 | 238 (55.9%) | 769 (71.9%) | < 0.0001 | 380 (60.2%) | 632 (73.1%) | < 0.0001 | |
| Yes | 145 (41.3%) | 330 (29.7%) | 188 (44.1%) | 301 (28.1%) | 251 (39.8%) | 233 (26.9%) | |||||
|
| |||||||||||
| Functional Limitation | No | 271 (76.6%) | 945 (84.8%) | < 0.001 | 334 (78.0%) | 904 (84.1%) | 0.005 | 482 (76.4%) | 762 (87.4%) | < 0.0001 | |
| Yes | 83 (23.4%) | 170 (15.2%) | 94 (22.0%) | 171 (15.9%) | 149 (23.6%) | 110 (12.6%) | |||||
|
| |||||||||||
| Race | Hispanic | 13 (3.7%) | 49 (4.5%) | 0.001 | 20 (4.8%) | 43 (4.1%) | 0.912 | 18 (2.9%) | 45 (5.3%) | 0.001 | |
| White | 261 (74.4%) | 905 (82.3%) | 330 (78.8%) | 845 (79.7%) | 528 (84.6%) | 650 (75.9%) | |||||
| Black | 50 (14.2%) | 92 (8.4%) | 45 (10.7%) | 108 (10.2%) | 48 (7.7%) | 103 (12.0%) | |||||
| Mixed Race/Other | 27 (7.7%) | 54 (4.9%) | 24 (5.7%) | 64 (6.0%) | 30 (4.8%) | 58 (6.8%) | |||||
|
| |||||||||||
| Sex | Male | 29 (8.2%) | 108 (9.8%) | 0.393 | 41 (9.8%) | 99 (9.3%) | 0.770 | 60 (9.6%) | 81 (9.4%) | 0.916 | |
| Female | 323 (91.8%) | 998 (90.2%) | 379 (90.2%) | 969 (90.7%) | 567 (90.4%) | 780 (90.6%) | |||||
|
| |||||||||||
| Age (years) | 42.3 (± 11.45) | 40.9 (± 11.77) | 0.056 | 39.6 (± 10.88) | 42.0 (± 11.93) | < 0.001 | 42.9 (± 11.56) | 40.1 (± 11.60) | < 0.0001 | ||
|
| |||||||||||
| BMI (kg/m2) | 27.3 (± 5.84) | 26.0 (± 5.04) | < 0.001 | 26.4 (± 5.45) | 26.3 (± 5.22) | 0.765 | 26.5 (± 5.37) | 26.1 (± 5.22) | 0.154 | ||
|
| |||||||||||
| Psychological Distress | 3.2 (± 3.68) | 2.3 (± 3.21) | < 0.001 | 3.7 (± 4.11) | 2.1 (± 2.83) | < 0.0001 | 3.1 (± 3.69) | 2.2 (± 3.02) | < 0.0001 | ||
|
| |||||||||||
| Unit Category | ER | 25 (7.1%) | 56 (5.0%) | 0.485 | 26 (6.1%) | 59 (5.5%) | 0.822 | 32 (5.1%) | 51 (5.8%) | 0.017 | |
| OR | 37 (10.5%) | 109 (9.8%) | 44 (10.3%) | 107 (10.0%) | 66 (10.5%) | 84 (9.6%) | |||||
| Adult Med/Surg | 122 (34.5%) | 378 (33.9%) | 142 (33.2%) | 373 (34.7%) | 201 (31.9%) | 315 (36.1%) | |||||
| Adult ICU | 48 (13.6%) | 136 (12.2%) | 52 (12.1%) | 138 (12.8%) | 87 (13.8%) | 101 (11.6%) | |||||
| Stepdown | 18 (5.1%) | 59 (5.3%) | 25 (5.8%) | 55 (5.1%) | 27 (4.3%) | 54 (6.2%) | |||||
| Ped Med/Surg | 4 (1.1%) | 16 (1.4%) | 7 (1.6%) | 13 (1.2%) | 6 (1.0%) | 14 (1.6%) | |||||
| Ped ICU/NICU | 17 (4.8%) | 45 (4.0%) | 21 (4.9%) | 40 (3.7%) | 33 (5.2%) | 30 (3.4%) | |||||
| Psychiatry | 0 (0.0%) | 19 (1.7%) | 3 (0.7%) | 17 (1.6%) | 7 (1.1%) | 13 (1.5%) | |||||
| OB-Postpartum | 28 (7.9%) | 98 (8.8%) | 39 (9.1%) | 86 (8.0%) | 55 (8.7%) | 71 (8.1%) | |||||
| Float Pool | 12 (3.4%) | 50 (4.5%) | 16 (3.7%) | 48 (4.5%) | 30 (4.8%) | 34 (3.9%) | |||||
| Amb only/Consult/Educ | 35 (9.9%) | 120 (10.8%) | 46 (10.7%) | 109 (10.1%) | 79 (12.5%) | 76 (8.7%) | |||||
| Orthopedics | 8 (2.3%) | 29 (2.6%) | 7 (1.6%) | 30 (2.8%) | 8 (1.3%) | 29 (3.3%) | |||||
|
| |||||||||||
| Hours Worked | 30 hours | 60 (17.0%) | 277 (24.9%) | 0.004 | 95 (22.4%) | 241 (22.5%) | 0.178 | 137 (21.8%) | 200 (23.0%) | 0.229 | |
| 30-34 hours | 41 (11.6%) | 138 (12.4%) | 60 (14.1%) | 120 (11.2%) | 84 (13.4%) | 97 (11.2%) | |||||
| 35-39 hours | 98 (27.8%) | 324 (29.2%) | 117 (27.5%) | 315 (29.4%) | 185 (29.4%) | 247 (28.5%) | |||||
| 40-44 hours | 137 (38.8%) | 328 (29.5%) | 128 (30.1%) | 355 (33.1%) | 190 (30.2%) | 293 (33.8%) | |||||
| >44 hours | 17 (4.8%) | 44 (4.0%) | 25 (5.9%) | 41 (3.8%) | 33 (5.2%) | 31 (3.6%) | |||||
|
| |||||||||||
| Occupation | Staff Nurse | 238 (67.4%) | 812 (73.2%) | 0.074 | 291 (68.5%) | 768 (71.6%) | 0.375 | 447 (71.1%) | 612 (70.5%) | 0.024 | |
| Patient Care Associate | 31 (8.8%) | 68 (6.1%) | 32 (7.5%) | 82 (7.6%) | 35 (5.6%) | 79 (9.1%) | |||||
| Other | 84 (23.8%) | 230 (20.7%) | 102 (24.0%) | 222 (20.7%) | 147 (23.4%) | 177 (20.4%) | |||||
|
| |||||||||||
| Nightwork | 0-6 hrs/month | 188 (53.1%) | 651 (58.4%) | 0.167 | 228 (53.3%) | 629 (58.5%) | 0.175 | 379 (60.1%) | 479 (54.9%) | 0.085 | |
| 6-72 hrs/month | 99 (28.0%) | 291 (26.1%) | 121 (28.3%) | 274 (25.5%) | 160 (25.4%) | 234 (26.8%) | |||||
| >72 hrs/month | 67 (18.9%) | 173 (15.5%) | 79 (18.5%) | 172 (16.0%) | 92 (14.6%) | 159 (18.2%) | |||||
|
| |||||||||||
| Coworker Support | 7.8 (± 1.51) | 8.1 (± 1.45) | 0.008 | 7.8 (± 1.59) | 8.1 (± 1.45) | 0.007 | 8.0 (± 1.45) | 8.0 (± 1.52) | 0.552 | ||
|
| |||||||||||
| Supervisor Support | 10.5 (± 2.96) | 10.7 (± 2.96) | 0.228 | 10.0 (± 3.17) | 10.9 (± 2.88) | < 0.0001 | 10.6 (± 2.93) | 10.7 (± 3.02) | 0.444 | ||
|
| |||||||||||
| Job Demands | 36.4 (± 5.12) | 35.8 (± 5.13) | 0.080 | 36.8 (± 5.24) | 35.6 (± 5.14) | < 0.0001 | 36.3 (± 5.29) | 35.6 (± 5.08) | 0.006 | ||
Figure 1. Frequencies of Sleep Deficiencies.
Subjects (n=1516 without missingness) with short sleep duration (<6h/day, red circle; D), sleep insufficiency (never/rarely feeling rested on waking; green; S), and/or insomnia symptoms (3 or more times a week, blue; I) are depicted.
Multivariable associations of sleep variables to outcomes
In multivariable models, short sleep duration was significantly associated with increased pain (OR=0.88, CI:0.79-0.98, p=0.020), and work interference (OR=0.86, CI:0.78-0.96, p=0.005), but not functional limitation (OR=0.90, CI:0.79-1.03, p=0.115). These effects remained despite controlling for covariates that remained significant in multivariable models (sex, age, BMI, psychological distress, occupation, job demands, coworker support, and supervisor support) and other non-significant covariates (race, unit category, hours worked, and nightwork). See table 2 for details.
Table 2.
Multivariable association of sleep duration and other respondent characteristics with pain, work interference and functional limitations: Odds ratios, 95% confidence intervals and p-values. Significant p-values and variables significant across all three outcomes are bolded.
| Sleep Duration Models | Any Pain | Work Interference | Functional Limitation | |||
|---|---|---|---|---|---|---|
| Effect | Odds Ratio(95% CI) | p | Odds Ratio(95% CI) | p | Odds Ratio(95% CI) | p |
| Hours Sleep | 0.88 (0.79-0.98) | 0.020 | 0.86 (0.78-0.96) | 0.005 | 0.90 (0.79-1.03) | 0.115 |
| Race (vs. Hispanic) | - | 0.083 | - | 0.438 | - | 0.893 |
| White | 0.94 (0.44-2.01) | - | 0.60 (0.30-1.20) | - | 1.30 (0.46-3.71) | - |
| Black | 0.49 (0.21-1.14) | - | 0.52 (0.23-1.18) | - | 1.35 (0.42-4.29) | - |
| Mixed Race/Other | 0.82 (0.32-2.09) | - | 0.66 (0.27-1.58) | - | 1.63 (0.46-5.70) | - |
| Sex (Female vs. Male) | 1.48 (0.94-2.31) | 0.089 | 1.77 (1.09-2.89) | 0.022 | 0.99 (0.56-1.75) | 0.974 |
| Age (years) | 1.00 (0.99-1.02) | 0.689 | 1.02 (1.00-1.03) | 0.016 | 1.05 (1.03-1.07) | <.0001 |
| BMI (kg/m2) | 1.03 (1.00-1.06) | 0.045 | 1.03 (1.01-1.06) | 0.009 | 1.08 (1.04-1.11) | <.0001 |
| Psychological Distress | 1.06 (1.01-1.12) | 0.012 | 1.10 (1.06-1.14) | <.0001 | 1.13 (1.08-1.18) | <.0001 |
| Occupation (vs. Staff Nurse) | - | 0.002 | - | 0.057 | - | 1.000 |
| Patient Care Associate | 0.75 (0.40-1.4) | - | 1.46 (0.78-2.75) | - | 1.00 (0.43-2.34) | - |
| Other | 0.51 (0.35-0.74) | - | 0.71 (0.48-1.04) | - | 0.99 (0.63-1.57) | - |
| Nightwork(vs. 0-6 hrs/month) | - | 0.611 | - | 0.327 | - | 0.669 |
| 6-72 hrs/month | 1.16 (0.80-1.68) | - | 1.29 (0.92-1.81) | - | 1.16 (0.74-1.81) | - |
| >72 hrs/month | 0.94 (0.63-1.43) | - | 1.05 (0.71-1.55) | - | 0.91 (0.55-1.51) | - |
| Job Demands | 1.05 (1.02-1.08) | <.001 | 1.06 (1.03-1.09) | <.0001 | 1.04 (1.01-1.08) | 0.017 |
| Coworker Support | 1.02 (0.91-1.14) | 0.692 | 0.96 (0.87-1.06) | 0.447 | 0.86 (0.76-0.98) | 0.024 |
| Supervisor Support | 0.96 (0.91-1.01) | 0.134 | 0.95 (0.91-1.00) | 0.043 | 0.97 (0.91-1.03) | 0.329 |
Sleep insufficiency was significantly associated with increased pain (“sometimes” vs. “never/rarely” OR=0.89, CI:0.62-1.27; “often/always” vs. “never/rarely” OR=0.57, CI:0.39-082; p=0.003), work interference (“sometimes” vs. “never/rarely” OR=0.66, CI:0.49-0.89; “often/always” vs. “never/rarely” OR=0.48, CI:0.34-0.67; p<0.0001), and functional limitation (“sometimes” vs. “never/rarely” OR=0.83, CI:0.57-1.21; “often/always” vs. “never/rarely” OR=0.56, CI:0.36-087; p=0.033). These effects remained despite controlling for covariates that remained significant in multivariable models (age, BMI, psychological distress, occupation, job demands, coworker support, and supervisor support) and other non-significant covariates (race, sex, unit category, hours worked, and nightwork). See table 3 for details.
Table 3.
Multivariable association of sleep sufficiency and other respondent characteristics with Pain, Work Interference and Functional Limitations: Odds ratios, 95% confidence intervals and p-values. Significant p-values and variables significant across all three outcomes are bolded.
| Sleep Sufficiency Models | Any Pain | Work Interference | Functional Limitation | |||
|---|---|---|---|---|---|---|
| Effect | Odds Ratio(95% CI) | p | Odds Ratio(95% CI) | p | Odds Ratio(95% CI) | p |
| Sleep Sufficiency (vs. Never/Rarely) | - | 0.003 | - | <.0001 | - | 0.033 |
| Sometimes | 0.89 (0.62-1.27) | - | 0.66 (0.49-0.89) | - | 0.83 (0.57-1.21) | - |
| Often/Always | 0.57 (0.39-0.82) | - | 0.48 (0.34-0.67) | - | 0.56 (0.36-0.87) | - |
| Race (vs. Hispanic) | - | 0.099 | - | 0.591 | - | 0.683 |
| White | 1.08 (0.52-2.26) | - | 0.63 (0.32-1.25) | - | 1.34 (0.48-3.79) | - |
| Black | 0.58 (0.25-1.31) | - | 0.60 (0.27-1.34) | - | 1.79 (0.58-5.52) | - |
| Mixed Race/Other | 0.98 (0.40-2.42) | - | 0.67 (0.28-1.59) | - | 1.66 (0.48-5.77) | - |
| Sex (Female vs. Male) | 1.47 (0.95-2.28) | 0.087 | 1.60 (1.00-2.56) | 0.050 | 0.92 (0.53-1.59) | 0.765 |
| Age (years) | 1.01 (0.99-1.02) | 0.273 | 1.02 (1.01-1.03) | 0.002 | 1.05 (1.04-1.07) | <.0001 |
| BMI (kg/m2) | 1.02 (1.00-1.05) | 0.098 | 1.03 (1.00-1.05) | 0.025 | 1.07 (1.04-1.10) | <.0001 |
| Psychological Distress | 1.06 (1.01-1.11) | 0.030 | 1.09 (1.05-1.13) | <.0001 | 1.12 (1.07-1.17) | <.0001 |
| Occupation (vs. Staff Nurse) | - | 0.003 | - | 0.121 | - | 0.977 |
| Patient Care Associate | 0.82 (0.45-1.51) | 1.29 (0.70-2.37) | - | 1.06 (0.48-2.34) | - | |
| Other | 0.51 (0.35-0.75) | 0.73 (0.50-1.06) | - | 0.97 (0.62-1.53) | - | |
| Nightwork (vs. 0-6 hrs/month) | - | 0.541 | - | 0.355 | - | 0.710 |
| 6-72 hrs/month | 1.14 (0.78-1.64) | - | 1.27 (0.91-1.78) | - | 1.15 (0.74-1.79) | |
| >72 hrs/month | 0.89 (0.59-1.34) | - | 1.04 (0.71-1.53) | - | 0.92 (0.56-1.52) | - |
| Job Demands | 1.05 (1.02-1.08) | <.001 | 1.06 (1.03-1.09) | <.0001 | 1.04 (1.01-1.08) | 0.014 |
| Coworker Support | 1.02 (0.91-1.14) | 0.789 | 0.96 (0.87-1.07) | 0.480 | 0.85 (0.75-0.96) | 0.010 |
| Supervisor Support | 0.96 (0.91-1.02) | 0.163 | 0.95 (0.91-1.00) | 0.044 | 0.98 (0.92-1.04) | 0.417 |
The presence of insomnia symptoms was significantly associated with increased pain (OR=1.45, CI:1.09-1.93, p=0.010), work interference (OR=1.64, CI:1.27-2.12, p<0.001), and functional limitation (OR=1.85, CI:1.33-2.57, p<0.001). These effects remained despite controlling for covariates that remained significant in multivariable models (sex, age, BMI, psychological distress, occupation, job demands, coworker support, and supervisor support) and other non-significant covariates (race, unit category, hours worked, and nightwork). See table 4 for details.
Table 4.
Multivariable association of insomnia symptoms and other respondent characteristics with Pain, Work Interference and Functional Limitations: Odds ratios, 95% confidence intervals and p-values. Significant p-values and variables significant across all three outcomes are bolded.
| Insomnia Symptoms Models | Any Pain | Work Interference | Functional Limitation | |||
|---|---|---|---|---|---|---|
| Effect | Odds Ratio(95% CI) | p | Odds Ratio(95% CI) | p | Odds Ratio(95% CI) | p |
| Insomnia (Yes vs. No) | 1.45 (1.09-1.93) | 0.010 | 1.64 (1.27-2.12) | <.001 | 1.85 (1.33-2.57) | <.001 |
| Race (vs. Hispanic) | - | 0.168 | - | 0.512 | - | 0.627 |
| White | 1.06 (0.51-2.20) | - | 0.60 (0.30-1.18) | - | 1.26 (0.45-3.57) | - |
| Black | 0.60 (0.26-1.36) | - | 0.60 (0.27-1.34) | - | 1.75 (0.57-5.42) | - |
| Mixed Race/Other | 0.96 (0.39-2.36) | - | 0.66 (0.28-1.56) | - | 1.66 (0.48-5.75) | - |
| Sex (Female vs. Male) | 1.48 (0.96-2.30) | 0.079 | 1.60 (1.00-2.56) | 0.050 | 0.92 (0.53-1.59) | 0.764 |
| Age (years) | 1.00 (0.99-1.02) | 0.661 | 1.02 (1.00-1.03) | 0.026 | 1.05 (1.03-1.06) | <.0001 |
| BMI (kg/m2) | 1.03 (1.00-1.05) | 0.076 | 1.03 (1.01-1.06) | 0.017 | 1.07 (1.04-1.11) | <.0001 |
| Psychological Distress | 1.06 (1.01-1.11) | 0.013 | 1.10 (1.06-1.14) | <.0001 | 1.12 (1.07-1.17) | <.0001 |
| Occupation | - | 0.004 | - | 0.166 | - | 0.991 |
| Patient Care Associate | 0.80 (0.44-1.47) | - | 1.23 (0.67-2.27) | - | 1.04 (0.47-2.29) | - |
| Other | - | - | - | - | - | - |
| Nightwork(vs. 0-6 hrs/month) | - | 0.561 | - | 0.300 | - | 0.748 |
| 6-72 hrs/month | 1.19 (0.82-1.71) | - | 1.31 (0.93-1.83) | - | 1.18 (0.75-1.85) | - |
| >72 hrs/month | 0.96 (0.64-1.44) | - | 1.11 (0.76-1.63) | - | 1.01 (0.61-1.65) | - |
| Job Demands | 1.06 (1.03-1.09) | <.001 | 1.06 (1.03-1.09) | <.0001 | 1.04 (1.01-1.08) | 0.014 |
| Coworker Support | 1.01 (0.90-1.13) | 0.911 | 0.95 (0.86-1.06) | 0.365 | 0.84 (0.74-0.95) | 0.006 |
| Supervisor Support | 0.96 (0.90-1.01) | 0.1115 | 0.95 (0.90-0.99) | 0.028 | 0.97 (0.91-1.03) | 0.311 |
Discussion
This study assesses sleep and work-related outcomes of bodily pain, work interference from this pain, and functional limitations of tasks of daily living. Strong and significant associations of sleep deficiency with pain, functional limitation and workplace interference persisted despite controlling for the effects of sociodemographic, psychological and workplace factors. Obtaining short sleep duration, reporting insomnia symptoms, and/or having sleep insufficiency may thus be related to workplace exposures, or may represent additional health-related sequellae of workplace exposures ramifying the consequences of prior workplace exposures. Alternatively, bodily pain, work interference from this pain, and functional limitations of daily living tasks may increase the likelihood of sleep deficiency.
An innovative aspect of this analysis is the use of the sleep deficiency construct. Prior work in sleep typically focused on presence or absence of a specific sleep disorder. This novel construct for sleep deficiency(30) posits that sleep may become “deficient” for a variety of or even a constellation of reasons. Components of sleep deficiency each demonstrated association with all three outcomes of bodily pain and work interference from that pain, and functional limitations (see supplementary materials), but the contributions of psychosocial factors significantly associated with each outcome varied slightly by outcome. As with other organic deficiencies, the exact source of deficiency may be less important for outcomes than the presence of the deficiency, though the components are critical for identifying modifiable sources. The strength of the sleep deficiency construct is in defining an important factor for positive change, irrespective of the source. The validity of this emerging construct is strengthened by its significant association with three conceptually-related but distinct outcomes.(23, 24, 50) Restricting time in bed to four hours/night over 12 days in a laboratory setting has been shown to increase self-reported levels of pain and of the inflammatory markers interleukin-6 and C-reactive protein.(23) Sleep-deprived health subject report significantly more pain than when rested.(24) Sleep sufficiency also matters for bodily pain; insomnia symptoms are associated with increased levels of pain(27-29) and conversely, pain, especially untreated, can lead to disrupted sleep.(33, 51) Restoration of sleep sufficiency is associated with the resolution of pain.(52) Sleep deficiency may be related to the concept of chronic “exhaustion” developed from the vitality scale of the SF-36, which is related to psychosocial factors at work, controlling for pain and other sociodemographic factors.(53)
Sleep, pain, and pain-related disability are important health indicators for health care workers. The health care sector ranks second in the largest share of work-related injuries behind manufacturing.(54) By far, nursing personnel bear the largest burden of injury in health care, and back injuries constitute the greatest source of their disability.(55) Current trends in hospitalized patient characteristics and in the health care work force are only likely to increase these risks to workers' health in coming years given the aging nursing workforce(56) and increased work demands.(57)
Work organizational factors included psychosocial job demands,(58, 59) which was significantly related to sleep deficiency in bivariate analyses, yet independently and significantly related to all three outcomes in this study. In contrast, perceived coworker support was only related to the outcome of functional limitation on tasks of daily living and supervisor social support was only related to work interference. A particular strength of the current analysis was the nightshift variable gleaned from administrative payroll records; a precise measure of actual night hours worked over the past year compared to self-reported nightshift status typically used. In contrast to work organization and social factors, nightshift was not significant in the current analyses. While the public health literature has focused on identifying specific risk factors, intervention research indicates that approaches addressing multiple factors are often the most effective, providing credence to the organizational and psychosocial environmental factors.(30, 60)
Limitations
This analysis has several important limitations, primarily that the cross-sectional approach does not allow for inferences on causal directions for the effects of workplace factors on sleep deficiency and pain/limitations, the effects of sleep deficiency on pain/limitations, or the effects of pain/limitations on sleep deficiency. Longitudinal and intervention studies will be needed to fully understand the causal mechanisms involved. Also, self-report was relied upon for sleep and other measures in this occupational cohort. Future studies using the sleep deficiency construct would benefit if components of sleep deficiency were measured (e.g., actigraphy or polysomnography). Sleep disordered breathing was not included in the construct but given its importance for health, should be included in future studies.
Although important to retain in the model, there was not a significant relationship of work hours or night shift for either sleep deficiency or any components of sleep deficiency (see Supplemental Tables). The associations of sleep deficiency with each of the pain, work interference, and functional limitation outcomes thus appear to be independent of the expected confounders work hours and night shift.
Conclusion
A reductionist approach to sleep(61) might characterize that separate ‘disorders’ account for sleep-related health and other problems, and focus clinical and other healthcare-related efforts on ameliorating specific individual level sleep maladies with targeted treatments. In population-level studies however, it can be useful to first identify whether sleep overall is deficient in a cohort, then to identify specific sources of disruption, e.g. to a workforce, that may impact workers in a heterogeneous manner despite potentially common root causes such as the workplace factors of low supervisor and coworker support. The role of the social environment may not be immediately apparent, as an understanding of causal relationships does not extend to a full understanding of what constitutes an effective intervention. Ultimately, both population and individual level interventions will be needed to reduce the public health burden of sleep deficiency by treating sleep disorders and improving conditions in the workplace. The current study suggests that comprehensive workplace interventions may usefully include sleep deficiency to address sleep duration-extending behaviors, sleep disorder mitigation, and other sleep promotion activities. At a minimum, future workplace interventions could include components on sleep deficiency in the assessment of modifiable outcomes closely related and potentially causally linked to musculoskeletal disorders, pain, and functional limitations that may increase the risk of disability.(62)
Multi-level interventions may be an effective way of supporting changes among individual workers within the context of the work environment. For example, policies that provide increased flexibility on shift length and timing may contribute to a supportive work environment that acknowledges the pivotal role of sleep in worker health outcomes. In tandem, educational programs to inform workers of the important associations between sleep, musculoskeletal disorders and pain may motivate workers to consider improved sleep hygiene practices.
Supplementary Material
Statement of Clinical Significance.
Comprehensive workplace interventions may usefully include sleep deficiency to address sleep duration-extending behaviors, sleep disorder mitigation, and other sleep promotion activities. Future workplace interventions could include components on sleep deficiency in the assessment of modifiable outcomes closely related and potentially causally linked to musculoskeletal disorders, pain, and functional limitations.
Acknowledgments
This work was supported by a grant from the National Institute for Occupational Safety and Health (U19 OH008861) for the Harvard School of Public Health Center for Work, Health and Well-being. OB was in part supported by the National Heart, Lung and Blood Institute (R01HL107240).This study would not have been accomplished without the participation of Partners HealthCare System and leadership from Dennis Colling and Kurt Westerman. The authors would like to thank Partners Occupational Health Services including Marlene Freeley for her guidance and Terry Orechia for programming support. We also thank individuals at each of the hospitals including Jeanette Ives Erickson, Mairead Hickey and Trish Gibbons in Patient Care Services leadership, and Jeff Davis and Lisa Pontin in Human Resources. We also thank Lorraine Wallace for her oversight within the Center.
Disclosure of funding: This work was supported by a grant from the National Institute for Occupational Safety and Health (U19 OH008861) for the Harvard School of Public Health Center for Work, Health and Well-being. NIOSH contributed to the development of the questionnaire, but otherwise had no role in the collection, analysis, and interpretation of data, and in the writing of this report.
Footnotes
Conflict of Interest Statement: There are no conflicts of interest to report, but in the interest of full disclosure, Dr. Buxton received investigator-initiated research grants from Cephalon and Sepracor, has received unrestricted educational grants from Minimitter and Takeda (more than 4 years ago), served on the speaker's bureau for Takeda (3 years ago), and previously served as a consultant for Sepracor. Dr. Buxton currently consults for Disnmore LLC (as an expert witness). All other authors have no conflicts of interest to report.
Contributor Information
Karen Hopcia N.P., Email: khopcia@hsph.harvard.edu.
Grace Sembajwe, Email: grace_sembajwe@dfci.harvard.edu.
James H. Porter, Email: jporter5@partners.org.
Jack T. Dennerlein, Email: jackdennerlein@gmail.com.
Christopher Kenwood, Email: ckenwood@neriscience.com.
Anne M.Stoddard, Email: astoddard@neriscience.com.
Dean Hashimoto, Email: dhashimoto@partners.org.
Glorian Sorensen, Email: glorian_sorensen@dfci.harvard.edu.
References
- 1.National Institute for Occupational Safety Health. [Accessed 11/2/2011];NIOSH Workplace Safety & Health Topics. 2011 http://www.cdc.gov/niosh/topics/healthcare/
- 2.Hader R. Engaging the new wave of second-career nurses. Nurs Manage. 2010;41:6. doi: 10.1097/01.NUMA.0000368558.07900.db. [DOI] [PubMed] [Google Scholar]
- 3.Smedley J, Egger P, Cooper C, Coggon D. Prospective cohort study of predictors of incident low back pain in nurses. BMJ. 1997;314:1225–1228. doi: 10.1136/bmj.314.7089.1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harber P, Billet E, Gutowski M, SooHoo K, Lew M, Roman A. Occupational low-back pain in hospital nurses. J OccupMed. 1985;27:518–524. [PubMed] [Google Scholar]
- 5.Hignett S. Work-related back pain in nurses. J Adv Nurs. 1996;23:1238–1246. doi: 10.1046/j.1365-2648.1996.13423.x. [DOI] [PubMed] [Google Scholar]
- 6.Retsas A, Pinikahana J. Manual handling activities and injuries among nurses: an Australian hospital study. J Adv Nurs. 2000;31:875–883. doi: 10.1046/j.1365-2648.2000.01362.x. [DOI] [PubMed] [Google Scholar]
- 7.Smedley J, Egger P, Cooper C, Coggon D. Manual handling activities and risk of low back pain in nurses. Occup Environ Med. 1995;52:160–163. doi: 10.1136/oem.52.3.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yip VY. New low back pain in nurses: work activities, work stress and sedentary lifestyle. J Adv Nurs. 2004;46:430–440. doi: 10.1111/j.1365-2648.2004.03009.x. [DOI] [PubMed] [Google Scholar]
- 9.Smedley J, Inskip H, Trevelyan F, Buckle P, Cooper C, Coggon D. Risk factors for incident neck and shoulder pain in hospital nurses. Occup Environ Med. 2003;60:864–869. doi: 10.1136/oem.60.11.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lagerstrom M, Hansson T, Hagberg M. Work-related low-back problems in nursing. Scand J Work Environ Health. 1998;24:449–464. doi: 10.5271/sjweh.369. [DOI] [PubMed] [Google Scholar]
- 11.Nelson A, Fragala G, Menzel N. Myths and facts about back injuries in nursing. Am J Nurs. 2003;103:32–40. doi: 10.1097/00000446-200302000-00021. [DOI] [PubMed] [Google Scholar]
- 12.National Research Council, Institute of Medicine. Musculoskeletal Disorders and the workplaces: Low Back and Upper Extremities. Washington, D.C.: National Academy Press; 2001. [Google Scholar]
- 13.Videman T, Ojajarvi A, Riihimaki H, Troup JD. Low back pain among nurses: a follow-up beginning at entry to the nursing school. Spine (Philadelphi, Pa 1976) 2005;30:2334–2341. doi: 10.1097/01.brs.0000182107.14355.ca. [DOI] [PubMed] [Google Scholar]
- 14.U.S. Bureau of Labor Statistics. Nonfatal Occupational Injuries and Illnesses Requiring Days Away from Work. 2010 [Google Scholar]
- 15.Tullar JM, Brewer S, Amick BC, III, et al. Occupational safety and health interventions to reduce musculoskeletal symptoms in the health care sector. J Occup Rehabil. 2010;20:199–219. doi: 10.1007/s10926-010-9231-y. [DOI] [PubMed] [Google Scholar]
- 16.Dawson AP, McLennan SN, Schiller SD, Jull GA, Hodges PW, Stewart S. Interventions to prevent back pain and back injury in nurses: a systematic review. Occup Environ Med. 2007;64:642–650. doi: 10.1136/oem.2006.030643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hignett S. Intervention strategies to reduce musculoskeletal injuries associated with handling patients: a systematic review. Occup Environ Med. 2003;60:E6. doi: 10.1136/oem.60.9.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martimo KP, Verbeek J, Karppinen J, et al. Manual material handling advice and assistive devices for preventing and treating back pain in workers. Cochrane Database Syst Rev. 2007:CD005958. doi: 10.1002/14651858.CD005958.pub2. [DOI] [PubMed] [Google Scholar]
- 19.Shaw WS, Main CJ, Johnston V. Addressing Occupational Factors in the Management of Low Back Pain: Implications for Physical Therapist Practice. Phys Ther. 2011 doi: 10.2522/ptj.20100263. [DOI] [PubMed] [Google Scholar]
- 20.Geuskens GA, Burdorf A, Barendregt PJ, Hazes JM. A high physical workload and high job demands hamper the good prognosis in physical functioning in persons with early inflammatory joint conditions. Rheumatology (Oxford) 2011;50:789–798. doi: 10.1093/rheumatology/keq359. [DOI] [PubMed] [Google Scholar]
- 21.Choi SW, Peek-Asa C, Sprince NL, et al. Sleep quantity and quality as a predictor of injuries in a rural population. Am J Emerg Med. 2006;24:189–196. doi: 10.1016/j.ajem.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 22.Czeisler CA, Buxton OM. The Human Circadian Timing System and Sleep-Wake Regulation. In: Kryger MH, Roth T, Dement MC, editors. Principles and Practices of Sleep Medicine. Elsevier; 2010. pp. 402–419. [Google Scholar]
- 23.Haack M, Sanchez E, Mullington JM. Elevated inflammatory markers in response to prolonged sleep restriction are associated with increased pain experience in healthy volunteers. Sleep. 2007;30:1145–1152. doi: 10.1093/sleep/30.9.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haack M, Lee E, Cohen DA, Mullington JM. Activation of the prostaglandin system in response to sleep loss in healthy humans: potential mediator of increased spontaneous pain. Pain. 2009;145:136–141. doi: 10.1016/j.pain.2009.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lautenbacher S, Kundermann B, Krieg JC. Sleep deprivation and pain perception. Sleep Med Rev. 2006;10:357–369. doi: 10.1016/j.smrv.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 26.Smith MT, Haythornthwaite JA. How do sleep disturbance and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature. Sleep Med Rev. 2004;8:119–132. doi: 10.1016/S1087-0792(03)00044-3. [DOI] [PubMed] [Google Scholar]
- 27.Leshner AI, Baghdoyan HA, Bennett SJ, et al. Manifestations and management of chronic insomnia in adults. Bethesda, Maryland: Journal of Clinical Sleep Medicine; pp. 412–421. [Google Scholar]
- 28.Sivertsen B, Overland S, Pallesen S, et al. Insomnia and long sleep duration are risk factors for later work disability. The Hordaland Health Study. J Sleep Res. 2009;18:122–128. doi: 10.1111/j.1365-2869.2008.00697.x. [DOI] [PubMed] [Google Scholar]
- 29.Sivertsen B, Overland S, Neckelmann D, et al. The long-term effect of insomnia on work disability: the HUNT-2 historical cohort study. Am J Epidemiol. 2006;163:1018–1024. doi: 10.1093/aje/kwj145. [DOI] [PubMed] [Google Scholar]
- 30.Sorensen G, Stoddard AM, Stoffel S, et al. The role of the work context in multiple wellness outcomes for hospital patient care workers. Journal of Occupational and Environmental Medicine/American College of Occupational and Environmental Medicine. 2011;53:899–910. doi: 10.1097/JOM.0b013e318226a74a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Center for Disease Control. [Accessed 11/3/2011];Sleep and Sleep Disorders. http://www.cdc.gov/sleep/data_statistics.htm.
- 32.Hoevenaar-Blom MP, Spijkerman AMW, Kromhout D, van den Berg JF, Verschuren WMM. Sleep duration and sleep quality in relation to 12-year cardiovascular disease incidence: the MORGEN Study. Sleep. 2011;34(11):1487–1492. doi: 10.5665/sleep.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Institue of Medicine Committee on Sleep Medicine Research, Board on Health Sciences Policy. Sleep Disorders and Sleep Deprivation An unmet Public Health Problem. Washington, D.C.: Institute of Medicine of the National Academies; The National Academies Press; 2006. [PubMed] [Google Scholar]
- 34.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 2008;16:643–653. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hale L. Who has time to sleep? J Public Health (Oxf) 2005;27:205–211. doi: 10.1093/pubmed/fdi004. [DOI] [PubMed] [Google Scholar]
- 36.Trinkoff AM, Le R, Geiger-Brown J, Lipscomb J. Work schedule, needle use, and needlestick injuries among registered nurses. Infect Control Hosp Epidemiol. 2007;28:156–164. doi: 10.1086/510785. [DOI] [PubMed] [Google Scholar]
- 37.Gottlieb DJ, Redline S, Nieto FJ, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29:1009–1014. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 38.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010 doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 39.Wingard DL, Berkman LF. Mortality risk associated with sleeping patterns among adults. Sleep. 1983;6:102–107. doi: 10.1093/sleep/6.2.102. [DOI] [PubMed] [Google Scholar]
- 40.U.S. Department of Health and Human Services. Tracking Healthy People 2010. Washington, D.C.: U.S. Government Printing Office; 2000. Nutrition and overweight; pp. B19-11–B19-42. [Google Scholar]
- 41.World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Geneva: World Health Organization; 2000. [PubMed] [Google Scholar]
- 42.Salo P, Oksanen T, Siversen B, et al. Sleep disturbances as a predictor of cause-specific work disability and delayed return to work. Sleep. 2010;33:1323–1332. doi: 10.1093/sleep/33.10.1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Akerstedt T, Kecklund G, Selen J. Disturbed sleep and fatigue as predictors of return from long-term sickness absence. Industrial Health. 2010;48:209–214. doi: 10.2486/indhealth.48.209. [DOI] [PubMed] [Google Scholar]
- 44.Rugulies R, Norborg M, Sorensen TS, Knudsen LE, Burr H. Effort-reward imbalance at work and risk of sleep disturbances. Cross-sectional and prospective results from the Danish Work Environment Cohort Study. J Psychosom Res. 2009;66:75–83. doi: 10.1016/j.jpsychores.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 45.Kuorinka I, Jonsson B, Kilbom A, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18:233–237. doi: 10.1016/0003-6870(87)90010-x. [DOI] [PubMed] [Google Scholar]
- 46.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 47.Buxton OM, Quintiliani LM, Yang MH, et al. Association of sleep adequacy with more healthful food choices and positive workplace experiences among motor freight workers. Am J Public Health. 2009;S 99:636–643. doi: 10.2105/AJPH.2008.158501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kessler RC, Barber C, Beck A, et al. The World Health Organization Health and Work Performance Questionnaire (HPQ) J Occup Environ Med. 2003;45:156–174. doi: 10.1097/01.jom.0000052967.43131.51. [DOI] [PubMed] [Google Scholar]
- 49.Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3:322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 50.Haack M, Mullington JM. Sustained sleep restriction reduces emotional and physical well-being. Pain. 2005;119:56–64. doi: 10.1016/j.pain.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 51.Menefee LA, Cohen MJ, Anderson WR, Doghramji K, Frank ED, Lee H. Sleep disturbance and nonmalignant chronic pain: a comprehensive review of the literature. Pain Med. 2000;1:156–172. doi: 10.1046/j.1526-4637.2000.00022.x. [DOI] [PubMed] [Google Scholar]
- 52.Davies KA, Macfarlane GJ, Nicholl BI, et al. Restorative sleep predicts the resolution of chronic widespread pain: results from the EPIFUND study. Rheumatology(Oxford) 2008;47:1809–1813. doi: 10.1093/rheumatology/ken389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lindeberg SI, Rosvall M, Choi B, et al. Psychosocial working conditions and exhaustion in a working population sample of Swedish middle-aged men and women. Eur J Public Health. 2011;21:190–196. doi: 10.1093/eurpub/ckq039. [DOI] [PubMed] [Google Scholar]
- 54.U.S. Bureau of Labor Statistics. Total recordable nonfatal occupational injury and illness incidence rates, by case type, private industry, 2003-06. 2007 [Google Scholar]
- 55.U.S. Bureau of Labor Statistics. Incidence rates of nonfatal occupational injuries and illnesses by industry and selected case types. 2000 [Google Scholar]
- 56.U.S. Department of Health and Human Services. Understanding and improving health. Washington, DC: U.S. Government Printing Office; 2000. Healthy people 2010. [Google Scholar]
- 57.Committee on the Adequacy of Nursing Staff in Hospitals and Nursing Homes, Institute of Medicine. Nursing staff in hospitals and nursing homes: Is it adequate? Washington, D.C.: National Academy Press; 1996. [PubMed] [Google Scholar]
- 58.Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. Job content questionnaire and user's guide. Los Angeles: University of Southern California, Department of Industrial and systems Engineering; 1998. [Google Scholar]
- 59.Dennerlein JT, Hopcia K, Sembajwe G, Kenwood C, Stoddard AM, Tveito T, Hashimoto DM, Sorensen G. Ergonomic practices within patient care units are associated with musculoskeletal pain and limitations. Am J Ind Med. 2012;55(2):107–16. doi: 10.1002/ajim.21036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kennedy CA, Amick BC, III, Dennerlein JT, et al. Systematic review of the role of occupational health and safety interventions in the prevention of upper extremity musculoskeletal symptoms, signs, disorders, injuries, claims and lost time. J Occup Rehabil. 2010;20:127–162. doi: 10.1007/s10926-009-9211-2. [DOI] [PubMed] [Google Scholar]
- 61.American Academy of Sleep Medicine. The International Classification of Sleep Disorders; Diagnostic and Coding Manual. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 62.Sorensen G, Stoddard A, Hammond SK, Hebert JR, Avrunin JS, Ockene JK. Double jeopardy: workplace hazards and behavioral risks for craftspersons and laborers. Am J Health Promot. 1996;10:355–363. doi: 10.4278/0890-1171-10.5.355. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.