Abstract
Objectives
Many youth develop complex trauma, which includes regulation problems in the domains of affect, attachment, behavior, biology, cognition, and perception. Therapists often request strategies for using evidence-based treatments (EBTs) for this population. This article describes practical strategies for applying Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) for youth with complex trauma.
Methods
TF-CBT treatment phases are described and modifications of timing, proportionality and application are described for youth with complex trauma. Practical applications include a) dedicating proportionally more of the model to the TF-CBT coping skills phase; b) implementing the TF-CBT Safety component early and often as needed throughout treatment; c) titrating gradual exposure more slowly as needed by individual youth; d) incorporating unifying trauma themes throughout treatment; and e) when indicated, extending the TF-CBT treatment consolidation and closure phase to include traumatic grief components and to generalize ongoing safety and trust.
Results
Recent data from youth with complex trauma support the use of the above TF-CBT strategies to successfully treat these youth.
Conclusions
The above practical strategies can be incorporated into TF-CBT to effectively treat youth with complex trauma.
Practice implications
Practical strategies include providing a longer coping skills phase which incorporates safety and appropriate gradual exposure; including relevant unifying themes; and allowing for an adequate treatment closure phase to enhance ongoing trust and safety. Through these strategies therapists can successfully apply TF-CBT for youth with complex trauma.
Introduction
Many youth experience multiple and chronic traumas (Copeland et al., 2007; Finkelhor, Ormrod, & Turner, 2007). Child maltreatment, domestic violence, and other forms of early interpersonal trauma that disrupt primary attachments increase the risk for developing a constellation of difficulties referred to as “complex trauma”(Herman, 1992; Cook et al., 2005; Ford & Cloitre, 2009). Complex trauma is characterized by significant problems with attachment security, affect regulation, biological regulation, dissociation, behavioral regulation, cognition and self-concept (Cook et al., 2005).
Evidence-based treatments (EBTs) are those that have produced positive outcomes in randomized controlled treatment trials (RCTs). Typically RCTs include youth exposed to a specified trauma type (e.g., sexual abuse or domestic violence). As a result, even though most participants in such RCTs have experienced multiple traumas and have problems in complex trauma domains (e.g., Cohen, Deblinger, Mannarino, & Steer, 2004; Deblinger, Mannarino, Cohen, Runyon, & Steer, 2011; Lieberman, Van Horn, & Ippen, 2005; Stein et al., 2003), a common misconception is that EBTs are not suitable for youth with complex trauma. Therapists often ask how to implement trauma-focused EBT for youth with complex trauma. This paper describes practical strategies for applying Trauma-Focused Cognitive Behavioral Therapy (TF-CBT, Cohen, Mannarino, & Deblinger, 2006; www.musc.edu/tfcbt) for these youth. Two composite case descriptions are used to illustrate these strategies throughout the paper.
Assessing youth with complex trauma
Assessing youth with complex trauma can be challenging for a number of reasons and a detailed description is beyond the scope of this paper. Briefly, the therapist attempts to gather not only basic information about the youth's trauma experiences but also about secondary adversities that often occur related to traumas. These include removal or rejection from family, placement in foster care or a residential treatment facility (RTF), legal, medical or other procedures that in themselves may also be traumatic. Youth who have complex trauma often under-report traumatic experiences and trauma-related problems. This may be because they avoid overwhelming trauma material; attachment-related injuries cause youth to not trust the therapist; and/or because they view chronic trauma and regulation problems as the normal fabric of life. Assessment is therefore usually an ongoing process which requires obtaining information from parents or caregivers (hereafter referred to as “caregivers”), if available, and other adults who know about the youth's history and functioning.
By definition complex trauma impacts multiple domains including affect, attachment, behavior, biology, cognition and perception, self-image, and academic functioning in addition to standard Posttraumatic Stress Disorder (PTSD) symptoms. Therapists must conduct ongoing assessment of all of these domains. Therapists gather information from the youth, caregiver(s), school and other resources while also understanding the critical importance of establishing a trusting relationship with the youth who may view such information gathering with suspicion. Standardized instruments can be used to assess trauma exposure (e.g., the Traumatic Events Screening Inventory for Children, TESI-C, National Center for PTSD, 2011), PTSD (e.g., the UCLA PTSD Reaction Index, Steinberg, Brymer, Decker, & Pynoos, 2004) and complex trauma outcomes (e.g., Trauma Symptom Checklist for Children, TSCC, Briere, 1996). More information about assessment is available elsewhere (e.g., Briere & Spinazzola, 2005).
Applying TF-CBT for complex trauma: Phase-based treatment
Several authors recommend that youth with complex trauma respond best to phase-based treatment with an initial stabilization phase to provide coping skills, a trauma processing phase to understand personal trauma experiences, and a final integration phase to consolidate and generalize safety and trust (e.g., Ford et al., 2005; Ford & Cloitre, 2009). TF-CBT consists of several progressive components summarized by the acronym PRACTICE. As Figure 1 illustrates, these components are divided into three distinct phases that parallel the recommended phases for youth with complex trauma: an initial coping skills-building phase (stabilization phase); a second trauma narrative and processing phase (trauma processing phase) and a final treatment consolidation and closure phase (integration phase) (Murray, Cohen, Ellis, & Mannarino, 2008).
Figure 1. TF-CBT PRACTICE Components for Complex Trauma.
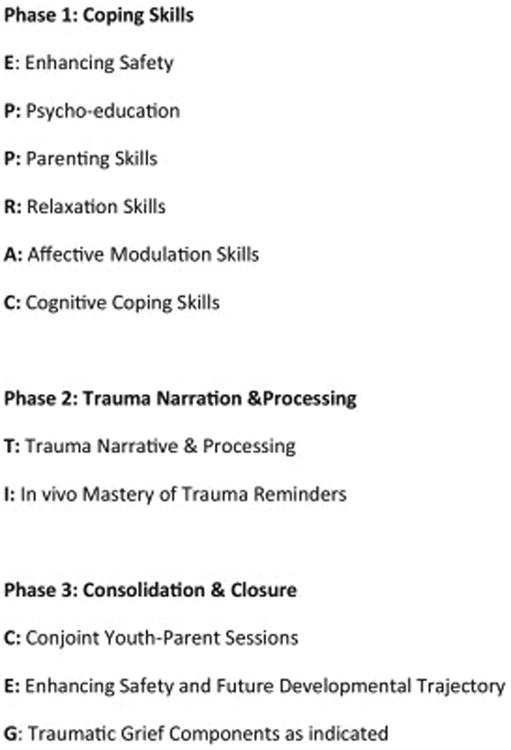
Proportion and balance are important concepts in providing TF-CBT. Typically therapists dedicate approximately the same number of treatment sessions to each of the 3 TF-CBT treatment phases (i.e., 1/3 of sessions for coping skills; 1/3 for trauma narrative and processing; 1/3 for treatment consolidation and closure). However, youth with complex trauma have significant regulation problems in multiple domains and these are frequently compounded by challenges in establishing a consistent, trusting therapeutic relationship. Therefore the proportionality of treatment is modified to dedicate about half of the total TF-CBT treatment sessions to the coping skill building phase. The duration of TF-CBT treatment also often needs to be extended, from the typical 8-16 sessions to 25 sessions and occasionally up to 28-30 sessions assuming sessions of 50 minute duration.
Developing and sustaining the therapeutic relationship is always central in TF-CBT treatment (Cohen et al., 2006, pp 46-53) but is especially critical for youth with complex trauma and their caregivers. Due to repeated interpersonal trauma experiences youth with complex trauma view most relationships as potentially threatening. Every TF-CBT component typically includes gradual exposure to help youth gain mastery over trauma reminders. The therapeutic relationship itself often serves as a trauma reminder for youth with complex trauma. During early TF-CBT sessions the therapist gradually exposes the youth to the idea of a safe and predictable relationship. This work can also be considered part of the in vivo mastery component as described later. Often caregivers have personal chronic trauma histories as well. The therapist must carefully calibrate both the youth's and the caregiver's abilities to tolerate distress related to the relationship and decrease the intensity of the interaction when needed. Distress tolerance is defined here as the youth's ability to self-regulate when experiencing negative affective states, including those triggered by trauma reminders. Practical strategies to target affective distress are described below. Gradual exposure to traditional trauma reminders may need to be modified as described later.
Phase 1: TF-CBT coping skills for complex trauma
Overview
During the initial coping skills phase youth begin to establish a trusting relationship with the therapist and develop safer and more effective self-regulation skills. Under optimal circumstances, participating caregivers also gain understanding of and attunement to youths' complex trauma responses and needs. However, since these changes require youth to shift their longstanding responses for adapting to severe stress, they rarely occur in a linear fashion. Even if the youth's trauma responses are maladaptive or dangerous, they seem to have helped the youth to survive, so giving them up may be terrifying. As a result, youth usually need many attempts of practicing using new self-regulation skills in diverse situations before they begin to use them effectively. Youth may respond very poorly to disappointing early attempts and “give up,” requiring the therapist to repeatedly reengage the youth in attempts to try new self-regulation skills. The youth may repeatedly “test” the therapist for trustworthiness during this process (e.g., a youth may not mention self-injury until the end of a session to see whether the therapist “cares” enough to extend the session). The therapist may be challenged to maintain personal regulation in these situations but doing so is critical to modeling coping skills as well as a fair, predictable, consistent relationship whose rules and boundaries the youth can come to understand and rely upon. Thus, the youth gradually gains increasing self-regulation while learning to tolerate reasonable levels of frustration within the context of an ongoing supportive relationship.
Enhancing safety
As Figure 1 illustrates, Enhancing Safety is usually the final TF-CBT treatment component. However, for youth living with ongoing threats to safety or stability, addressing safety concerns becomes the first treatment priority and often is an ongoing process throughout TF-CBT (Cohen, Mannarino, & Murray, 2011; Ford & Cloitre, 2009). Indeed, enhancing the youth's sense of safety is the core therapeutic goal for many youth with complex trauma. Ongoing danger may include the youth's suicidality, self-injury or risk-taking behaviors including serious substance abuse; ongoing abuse or violence toward the youth; or other immediate threats such as a new HIV diagnosis or imminent placement disruption. Youth with complex trauma have a great need, yet often few skills, for developing consistent, safe, nurturing relationships. Since secure attachments are essential for youth to develop a “felt sense of security” (Siegel, 1999; Cassidy & Shaver, 2008), establishing a trusting therapeutic relationship is essential for enhancing the youth's sense of safety. Developing other safe relationships in the youth's immediate and extended environment will further enhance the youth's sense of safety. Especially at the start of TF-CBT treatment, the therapist advocates for the youth with the caregiver, educators, direct care staff and others to increase safety, build positive relationships, and thus to promote resiliency. The therapist encourages the development of safety by including the caregiver in TF-CBT; identifying safe adults in the community in order to enhance safety; providing psychoeducation to caregivers, educators and RTF direct care staff to ensure a consistent understanding of the youth's trauma-related impairments where there may be a consistent trauma theme; and nurturing the youth to express his own views and choices both in and outside of therapy. Examples of these advocacy roles are described in case examples below, and are consistent with the CDC violence prevention strategy of increasing safe, nurturing social networks for victimized youth (www.CDC.gov) Safety strategies include building the youth's and caregiver's personal safety skills, as well as helping them to access available external resources. The strategy of working with the youth and caregiver to develop a specific safety plan conveys to the youth that he has the ability to make positive choices and to obtain appropriate support, rather than continuing to view himself as helplessly at the mercy of malevolent others. Often youth have lived in crisis for years and have no experience in perceiving caregivers, police, teachers or other authority figures as helpful. Systematic work is often necessary to change this state of affairs. This includes helping the youth to identify adults he is willing to turn to for help. It also involves helping the caregiver and other significant adults to learn specific behavioral responses that reliably provide the youth with optimal safety and a sense of security. The therapist also engages other services to increase safety and protectiveness in the broader environment (e.g., encouraging enrollment in after-school, spiritual, or other safe activities). An additional practical strategy therapists must address is assuring safe learning and therapeutic environments as described in the following example.
Case example
Kayla witnessed early domestic violence of her mother until mother threatened to call the police. Father absconded with Kayla when she was 6 years old and they lived “on the run” until she was 10 years old. At that time father was arrested and sent to prison for dealing drugs. Kayla's identity was discovered and she was found to have several sexually transmitted diseases. She disclosed that several of father's associates had sexually abused her. Kayla was returned to live with mother where she had severe behavior problems. Mother became physically abusive and Kayla was removed from her care. Mother's parental rights were later terminated. Kayla was placed in a series of foster homes where she experienced additional episodes of sexual abuse by males in the community. She was sent to a residential treatment facility (RTF) at 13 years old after she stabbed a male teacher. Upon admission, Kayla required therapeutic holds several times a day due to aggression towards male staff and peers. Every night she barricaded herself in her room by moving all of the furniture in the room against the door. Several staff members had to break into the room each morning to wake her up resulting in her losing points on the level system. Her therapist began the TF-CBT safety component by observing that Kayla seemed to be trying very hard to keep herself safe at nighttime. Kayla asked why the staff kept taking away levels for this. The therapist validated Kayla's need for nighttime precautions since she had not been safe at night in the past, but that the choices she was making were not safe (e.g., if there was a fire she could be trapped). She and Kayla brainstormed about alternative strategies that would make Kayla feel safe and agreed on 1) having a staff member check the room each night and sit directly outside her door all night; 2) giving Kayla a shriek alarm to hold all night; 3) leaving a night light on all night in Kayla's room; and 4) allowing Kayla to come out of her room twice each night if she was scared. The therapist encouraged direct care staff members to respond more positively and compassionately to Kayla's needs as described later and she subsequently felt more understood and supported. The therapist also suggested some relaxation strategies that Kayla could use at night when she was scared (she chose listening to favorite music). At subsequent sessions they established a fear hierarchy and made a schedule for Kayla to gradually work up to sleeping through the night in the RTF without needing a staff member outside her room (in vivo mastery plan). They agreed to start working on this plan with the understanding that it might take several weeks for Kayla to be able to sleep through the night.
Psychoeducation
This component provides the youth and caregiver with information about trauma impact, trauma reminders and hope for recovery (Cohen et al., 2006). Therapists often ask, “Which traumas should I focus on for youth with complex trauma?” Assessment instruments often ask youth to identify a single “worst” trauma experience. Doing so rarely captures the essence of the youth's complex traumatic experiences or outcomes. It is usually more helpful to conceptualize one or more underlying trauma “theme(s)” that cut across and provide an integrative meaning to the youth's trauma experiences. Thus the theme/themes rather than a specific trauma type, become the focus of TF-CBT treatment. Throughout TF-CBT, gradual exposure focuses on trauma reminders to the youth's theme. The therapist weaves specific traumas the youth experienced into this theme throughout treatment.
The therapist and youth work together to co-identify the youth's theme early in TF-CBT treatment. Often the theme emerges naturally during psychoeducation, and the therapist assists the youth in identifying it through Socratic dialogue (described in detail at www.musc.edu/tfcbt and www.musc.edu/cpt). During the assessment and early psychoeducation sessions, the therapist elucidates the youth's history and trauma experiences (understanding that more details will likely be revealed as the youth's trust in the therapist increases). The therapist may use information from an assessment instrument; statements that the youth makes during therapy; or observations from interactions with the youth to initiate an interaction about the youth's trauma theme. The therapist uses clinical judgment to determine whether to directly introduce this topic (e.g., “I would like us to talk about identifying your trauma theme”) or to explore this topic more indirectly as in the case example that follows. These trauma themes are usually relational (e.g., feeling unsafe or afraid in relationships) but they may occasionally focus on self-concept (e.g., “I am worthless,” etc). Initially identifying the trauma theme generally requires relatively few sessions through the process described in the following example. Addressing this central theme is the core task of the rest of the TF-CBT treatment. As in most effective therapies, the theme may evolve or shift focus somewhat as new mastery is gained and new issues emerge (for example, from basic safety to establishing an intimate relationship).
Case example
Daniel, aged 14 years, was severely neglected by his substance-addicted mother and witnessed domestic violence of mother by several drug dealers from early childhood. At 6 years old he had still never attended school; he was found by police naked, covered with feces, and severely dehydrated; mother's whereabouts were unknown and she has never been located. Daniel was placed in a series of temporary foster homes, eventually living with maternal great-grandmother (“grandma”) at 7 years old. Daniel lived with grandma until 9 years of age when he witnessed grandma's sudden death from a stroke. Daniel was placed in several foster homes but each placement was terminated due to Daniel's aggressive behaviors. At 12 years old Daniel was placed in an adoptive home. Parents had decided to adopt after 18 years of unsuccessful attempts to conceive. Soon after the adoption was finalized adoptive mother unexpectedly became pregnant. When the adoptive parents told Daniel about the pregnancy he became increasingly aggressive and began abusing a variety of drugs. When the therapist approached the topic of Daniel's recent drug use, Daniel said to his therapist “They just want to get rid of me. What difference does it make if I do drugs?” The therapist asked a clarifying question, “I can hear that you feel hopeless about things. Help me understand why you think they want to get rid of you?” Daniel said, “Because they don't care about me now that they're having a baby. They're just gonna get rid of me once the baby comes.” The therapist said, “It sounds like you're having a really hard time believing that your parents care about you now that they are having a baby.” Daniel said, “Why should they care about me? No one else does and now they won't either. I might as well get high.” The therapist said, “It's hard to believe that your parents care about you because no one else does? Help me understand what you mean about no one else caring about you?” Daniel said, “I'm sick of this.” The therapist responded, “Do you mean you're sick of people not caring about you?” Daniel said, “I'm sick of thinking people will be here for me and then they aren't.” The therapist said, “It's hard for you to believe that anyone will be here for you when people haven't been here for you before.” Daniel said, “Why should they? They have their own kid now.” The therapist said, “It's really scary to put your trust in them since you've been let down so many times before.” Daniel said, “I've been through this before. It sucks. I don't want to go through it again.” Through this process of Socratic dialogue the therapist was able to help Daniel identify his own trauma theme of “It's hard to believe anyone cares about me when no one's been here for me before” This became Daniel's theme during TF-CBT. The therapist worked closely with adoptive parents throughout TF-CBT treatment as described below to enhance their sensitivity, understanding and support of Daniel.
Trauma reminders for youth with complex trauma may be idiosyncratic (e.g., a color or internal feeling) or very general (e.g., adults correcting them using loud voices; hearing peers arguing). In either case they may not be easily recognized early in treatment. Identifying the youth's theme often facilitates the identification of trauma reminders since the reminders are often associated with the theme. As trauma reminders are identified, the therapist helps the youth and caregivers understand connections between these and the youth's regulation problems. Then they begin to develop stabilization skills to address them.
Case example
Daniel's therapist described typical trauma reminders for youth who have experienced traumatic loss (e.g., that they may get very upset when other people act indifferently, do not say hello, or leave without warning. Daniel said that he hated when people “disrespect me.” For example, when a girl in school whom Daniel wanted to ask out did not talk to him, Daniel cut school to use drugs. Daniel did not initially connect this to his mother's neglect or grandma's death, but he agreed when the therapist said, “Some kids have been hurt in big ways. When someone hurts them now it reminds them of the big ways they were hurt before.” The therapist helped Daniel's adoptive mother understand this trauma reminder. Over time, and through ongoing parenting skills used in conjunction with coping skills for Daniel, adoptive mother became much better attuned to Daniel's sensitivity to rejection and how to successfully respond to this.
Parenting skills
Ultimately, the goal of including caregivers in TF-CBT is to build (or rebuild) a relationship between the youth and caregiver based on understanding, trust and mutual respect. Therapists provide every TF-CBT component to caregivers in parallel parenting sessions. Optimizing caregivers' parenting skills is particularly important. In order to support youth with complex trauma, caregivers must understand the youth's trauma-related problems as such (“bad things happened to him”), rather than viewing these as the youth “being bad.” Due to the complexity, severity and duration of these youths' problems, caregivers often have difficulties believing or accepting this explanation. This is particularly difficult in relation to persistent externalizing behavior problems that seem remote from the trauma. Negative caregiver cognitions and attitudes towards the youth (e.g., “he's just using trauma as an excuse,” “I was abused as a child and I didn't act like this”) are likely to be reflected in negative behaviors towards the youth, and contribute to further deterioration of the youth's trust and safety. Helping the caregiver understand the impact of trauma (psychoeducation) and adopt positive, safe interactions with the youth (positive parenting skills) are thus critical initial priorities in the parenting component of TF-CBT treatment. Daniel was fortunate to live with committed, supportive adoptive parents who recognized the challenge that having a new sibling would present in light of his trauma theme. They were dedicated to helping him through this difficult transition period. Youth with complex trauma are frequently living in chaotic or unstable situations (e.g., homeless; with a perpetrator) in which no caregiver is identified to participate in TF-CBT. In these situations the therapist adopts a multi-pronged approach to the parenting component. If at all feasible the therapist locates a stable adult in the youth's life (e.g., a grandparent; adult sibling, other relative or previous foster parent) that the youth is willing to include in TF-CBT to whatever extent is feasible and possible.
Youth who live in foster homes often hesitate to include their foster parent in therapy because they do not trust this caregiver and do not want to share details of their past life with them. These youth may also struggle with conflicting loyalties to biological parents and not want to form attachments to foster parents through engaging in therapy with them. Recent research documents that specific therapeutic efforts to include foster parents in TF-CBT often improve the foster parents' understanding of complex trauma, enhance their supportive attitudes and behaviors towards foster youth, and improve outcomes for youth with complex trauma (Dorsey, 2012).
Whether or not an appropriate adult can be identified to participate in TF-CBT with the youth, the therapist should attempt to locate and engage other adults to participate in providing a supportive, safe, predictable “extended parenting” environment. These adults may include extended family, faith community, educators, other health or mental health professionals, or others. The therapist educates these adults about ways to enhance positive interactions while not encouraging trauma reenactment.
Case example
Criticism was difficult for Daniel, especially when it occurred publicly. Daniel's schoolwork had initially improved upon placement with his adoptive family, but after his mother became pregnant his school attitude, performance and attendance deteriorated. On one occasion his math teacher openly criticized Daniel in class for coming late. Daniel immediately stormed out of the school. After speaking with mother and obtaining Daniel's permission, the therapist called the math teacher. The teacher was initially negative about Daniel. However, once the therapist validated the teacher's right to expect regular attendance and appropriate behavior, the teacher was willing to listen. The therapist explained that due to Daniel's previous trauma history, public criticism served as a trauma reminder and interfered with his tenuous self-regulation abilities. After that call the math teacher started to “look out” for Daniel in school. He refrained from critical comments to Daniel, privately offered to help him with math homework during study hall, said hello to him when he saw him in the hallways, and generally served as a positive presence for Daniel at school. With this supportive presence and ongoing positive parenting interventions (e.g., help with homework, validation of negative feelings about the pregnancy; support about the female peer ignoring him), Daniel's feelings about school changed and he began to attend regularly.
Youth in RTF often experience more frequent disruptions of caregiver relationships. The caregiver may not visit, be uninvolved in the youth's treatment, or placement/custody may be terminated during the youth's RTF stay. RTF direct care staff members then become the youth's de facto caregivers for the duration of the RTF placement. Involving these staff members in the youth's treatment is often critical. Direct care staff members are ideally incorporated into the process from the time TF-CBT is first introduced into an RTF setting. This occurs by educating direct care staff members about trauma impact and about how to support TF-CBT coping skills. As individual youth begin TF-CBT treatment, the therapist asks the youth about sharing information about these coping skills with direct care staff members, so that the direct care staff can help the youth to use these skills successfully. Many youth will initially object, since trust is so tenuous at this stage and the youth expects betrayal. The therapist may brainstorm with the youth about how to safely provide this information. For example, the youth may choose to personally demonstrate the skill to a single chosen staff member during a treatment session with the therapist, enabling the youth to retain control of the information shared and how it is provided. This may reassure the youth that “secret” communications between the therapist and the staff member about the youth's therapy sessions will not occur without the youth's knowledge and agreement. Once youth trust the communication process, they become more willing to share coping skills with additional direct care staff members. In some instances, youth will become willing to include a chosen direct care staff member in the TF-CBT treatment itself.
Case example
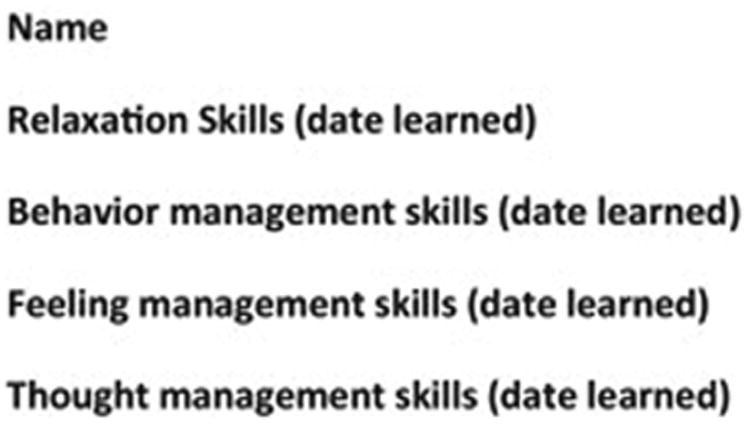
Soon after starting TF-CBT, Kayla's therapist suggested that a direct care staff member participate in TF-CBT treatment. Kayla refused. Her therapist said, “It's hard to feel safe when you were unprotected for so long” (Kayla's theme). As the therapist continued to address the safety component, Kayla said, “I just need to get away from everyone. If everyone would just leave me alone I wouldn't need any more (therapeutic) holds.” The therapist suggested discussing this plan with a chosen staff member. Kayla could ask this staff member to help her find a quiet place whenever she needed time alone. Kayla said, “It won't work—no one listens to me.” The therapist said, “I think you've got a good idea. Let's pick one staff member, and try it out.” The therapist assumed Kayla would select one several female staff members who had been remaining outside Kayla's room at nighttime Instead, Kayla chose to discuss her plan with Chuck, a very popular staff member who was admired by other residents and staff. Chuck readily agreed to the plan. During the following weeks, Kayla tested Chuck repeatedly (e.g., constantly interrupting him to ask to go to a quiet place). Chuck responded fairly, predictably, and according to the agreed plan. After several weeks Kayla was no longer receiving therapeutic holds during Chuck's shifts. In a subsequent session when Kayla learned affective modulation skills, the therapist was ending the session when Kayla asked, “Isn't Chuck coming in to hear how to do this with me on the unit?” The therapist agreed and suggested that she complete a TF-CBT Coping Card to share with Chuck (Figure 2). Kayla demonstrated the affective modulation strategies for Chuck and showed Chuck her Coping Card. Chuck thanked Kayla and praised her for her recent improvements in the milieu. Over time, Kayla showed the Coping Card to other direct care staff as well. As she continued to share coping skills with Chuck, the therapist suggested that she could include a staff member in her TF-CBT treatment. Kayla asked Chuck and he agreed to participate in TF-CBT with her.
Figure 2. TF-CBT Coping Card.
Relaxation, affective and cognitive coping skills
Youth with complex trauma have documented dysregulation of neurobiological stress systems (e.g., DeBellis et al., 1999; Ford, 2005). These youth have often used maladaptive strategies (e.g., drugs or alcohol; unprotected sex; skipping school) to cope with elevated levels of stress and have likely been criticized or punished for these behaviors. The therapist validates for the youth that these strategies were the youth's best attempts at the time to cope with the neurobiological impact of trauma, although they were often problematic (e.g., they got the youth in trouble). The therapist then helps the youth to develop more effective coping strategies, understanding that he will likely need more time than other youth to consistently and effectively use these strategies to reverse longstanding hyperarousal. Early in the coping skills phase, physically-based relaxation strategies (e.g., yoga, progressive muscle relaxation, dance, etc) may be more useful than cognitive-based ones (e.g., visualization or mindfulness) (Kliethermes & Wamser, in press).
Some youth become highly dysregulated if the initial coping skills sessions contain even minimal trauma information. For these youth, the therapist often starts TF-CBT using relaxation skills without gradual exposure as Kayla's therapist did initially. That is, these strategies are initially not paired with the youth's trauma reminders. Once the youth gains some ability to use one or more relaxation strategy, the therapist carefully begins to introduce gradual exposure through the safety and psychoeducation components, encouraging the youth to use the previously mastered relaxation skills as trauma information is introduced. As the youth gains increased mastery using relaxation skills, the therapist then pairs these with specific trauma reminders (further titrating the gradual exposure).
Case example
Once Kayla was successfully using music, yoga, deep breathing and visualization strategies at bedtime, her therapist worked with her to identify other situations that made her anxious (e.g., being around groups of males in the RTF; hearing laughing or loud talking) when she could also use these skills. Kayla gradually became more able to use these strategies when she became anxious or irritable. Over time she became more aware of internal responses to these reminders (“cues,” e.g., fisting her hands; clenching her teeth) and used these cues as signals that she should use relaxation coping strategies.
Youth with complex trauma often have blunted affect and lack a full range of affective vocabulary. Most commonly they have learned not to express feelings because doing so was previously punished, ridiculed and/or dangerous. The therapist does not make assumptions about expressing feelings in the current home or community environment being safe since this may not be the case. The therapist personally models a range of appropriate affective expression and validates a broad range of feelings as acceptable, but youth may be understandably reluctant to accept such statements at face value. Youth will often initially “test the waters” through expressing negative emotions that leave the youth less vulnerable (e.g., anger; disdain). Therapists work with parents or caregivers to validate and support appropriate emotional expression as described below. Feeling identification work may need to start on a very basic level. For example, the therapist (and ideally the caregiver) may need to mirror the youth's facial expressions (e.g., smiling when the youth smiles) and labeling the emotion the youth appears to be experiencing in the moment (e.g., “You feel happy!”). This process is similar to interactions that occur between adults and very young children in secure attachment relationships and serves as the foundation for developing more advanced affective regulation skills.
TF-CBT includes a wide range of practical strategies for decreasing affective distress (Cohen et al., 2006).Some specific strategies used for youth with complex trauma include distraction; mindfulness; perceptual bias modification; self-awareness skills; and cognitive coping skills. Each is described briefly here.
Distraction activities are helpful when initially starting to manage affective distress since most youth with complex trauma already use some of these activities (e.g., talking to or texting peers; watching TV; playing video games).These can be used as examples of how the youth has already learned to “turn down the volume” of difficult emotional states. The therapist encourages the youth to identify and practice a variety of distraction techniques and experience how different types of distraction activities feel very different. For example, listening to music, doing a crossword puzzle, watching a comedy show, taking a walk or knitting are likely to elicit different responses. As the youth adds different distraction techniques to his “toolkit,” he then uses different activities in different distressing situations to see which works best in which situations. Youth may overuse distraction strategies to their detriment (e.g., watching TV all night instead of doing homework) because they do not have an adequate range of alternative strategies for distress tolerance. Situations in which youth find they are overusing distraction can thus serve as learning opportunities for youth to apply new skills.
Mindfulness refers to the ability to be fully aware of and in touch with the present moment without taking a judgmental or evaluative approach to one's inner experiences. The therapist may use a variety of sensory activities to introduce mindfulness to the youth. For example, instructing the youth to focus on the sensation of taste as he allows different foods to melt in his mouth one by one (e.g., chocolate; ice; mint); focusing on touch as he reaches into a bag and explores different pieces of fabrics (silk; corduroy, denim). The therapist encourages the youth to fully experience the sensations associated with each and to fully describe what each was like. Through these exercises, the youth becomes increasingly aware of the present moment. The therapist instructs youth to spend specified periods of time dedicated to mindfulness each day. As the youth gains mindfulness he is increasingly able to observe his feelings without having to react to them. For youth who prefer physically-based activities, yoga can provide an entrée to developing mindfulness.
Perceptual bias modification strategies aim to correct youths' bias towards perceiving negative affective states in others (Pollack & Tolley-Schell, 2003). The therapist first asks the youth to identify a variety of feelings expressed in magazine pictures or photos of youth and adults. If the youth displays bias towards negative emotions (e.g., labels neutral faces “mad” or is unable to distinguish between different negative emotions), the therapist provides practice in accurate emotion identification. This includes in vitro (e.g., using pictures) as well as in vivo experiences (asking individuals how they are feeling), using gradual exposure to assure that safe individuals are selected for the initial in vivo activities. Through these activities youth gain a more accurate perspective on others' emotions, which are often a source of the youth's own affective distress. Self-awareness skill-building: Many youth with complex trauma lack self-awareness about how others perceive them in social interactions. The therapist encourages the youth to describe a recent negative social interaction and to tape record the youth's description of this interaction. After the youth describes the interaction (preferably including verbal exchanges between the youth and the other person), the therapist asks the youth to describe the feeling the youth was trying to convey to the other person. The therapist then replays the tape recording as the youth and therapist to explore whether the youth accurately conveyed the desired emotion during the youth's description of the interaction. For example, a youth who intended to express hurt feelings to a friend for not calling, instead realized upon listening to herself that she had expressed a great deal of anger and rejection towards her friend. This led to her expressing remorse because she “didn't mean to sound like that” and problem solving about how to correct mistakes that are later regretted. Through similar self-reflective activities, youth gain greater ability to modulate social interactions and thus to effectively access social support.
Cognitive coping strategies help youth and caregivers to identify alternative thoughts that may be more accurate or helpful than their current beliefs. Youth with complex trauma struggle to implement these strategies more than other youth because their maladaptive cognitions are often more deeply ingrained than those of other youth. Indeed, a thought the therapist is questioning (e.g., Daniel said, “You can't trust anyone”) may be the one the youth believes is responsible for his survival. In this instance the therapist validated and acknowledged the importance of this belief in the Daniel's past (e.g., “There was a time when no one in your life was trustworthy so it was very important for you to remind yourself of this to keep yourself safe from harm.”) The therapist then inquired about Daniel's current circumstances and whether there was any room to revise the belief, even slightly (e.g., “Since being adopted, has there ever been a time or a person that you thought you could trust at all, even a little?”). Daniel acknowledged that he sometimes trusted his adoptive mother, and revised his thought to “I don't trust most people but sometimes I trust my mom.” He was able to recognize that this helped him feel safer and more cared about at home than thinking that he couldn't trust anyone, and that these feelings in turn helped him get along better with his parents.
Involving caregivers in skills components
As the above process occurs to develop the youth's coping skills, the therapist meets regularly in parallel sessions with the caregiver to help the caregiver learn these skills. This enables the caregiver to support skills implementation at home or in the youth's current setting, both when the youth is exposed to trauma reminders and when the youth otherwise experiences dysregulation. The caregiver must recognize the connection between trauma reminders and regulation problems (psychoeducation and parenting skills); understand how the youth is supposed to implement the above coping skills (learn relaxation, affect modulation and cognitive coping skills as they have been individualized for the youth), and effectively intervene with the youth when regulation difficulties begin. This usually requires significant caregiver commitment as well as repetition, practice, in-session role play and, often, tweaking of unsuccessful strategies. For example, in the above affective modulation description, if the caregiver responds negatively to the youth's expression of anger, the youth is likely to dismiss affective expression as a “waste of time. If this occurs, the caregiver and therapist will need to spend extra time convincing the youth that it is indeed worthwhile expressing feelings to the caregiver (and having the caregiver practice a different response if and when they youth does so in the future). However, if the caregiver praises or validates the youth for expressing anger in a relatively appropriate manner (e.g., using angry words—even swear words—instead of aggressive behavior), the youth is more likely to begin believing that affective expression is a viable strategy and continue to express other feelings.
Case example
Daniel had a pattern of responding to perceived rejection by “shutting off” emotionally, leaving the situation and using drugs. The therapist addressed this by observing when Daniel distanced himself emotionally in therapy. Over time she and Daniel were able to talk about Daniel's feelings when these situations occurred. Daniel acknowledged his belief that no one really cared about him and that talking about feelings was “useless.” The therapist's validation of this within the context of Daniel's experiences helped him to feel understood and to start to trust his therapist more. Over several weeks Daniel expressed more feelings with the therapist. Concurrently the therapist was meeting weekly with adoptive parents to encourage their positive response whenever Daniel expressed any feelings. The adoptive father was especially annoyed when Daniel “shut down” and was likely to take a “to hell with him” attitude when this occurred. Daniel in turn was extremely sensitive to this rejection. He would respond to this by going to his room and using marijuana, which father was then sure to smell and punish Daniel for using. The therapist pointed out that father was “playing into Daniel's expectations” by doing this. Mother and father agreed to experiment with only positive responses to any affective expression that Daniel made during a 3-week period. Parents would not respond negatively to any episodes of Daniel shutting down. Each parent was given a “homework” assignment to observe and comment positively on Daniel's affective expression at least 3 times each day, and to record this along with Daniel's responses at the end of each day. Both parents found the idea of tracking their behaviors and Daniel's response to be helpful in “keeping us on track” and observing Daniel's improvements. Father successfully attended to Daniel when he expressed anger and annoyance. For example, when Daniel said, “This sucks so much” father responded, “Daniel, I really appreciate you sharing your disgust and annoyance with me.” Daniel actually smiled and said, “Anytime, dad” and did not lose his temper as he usually would in this circumstance. Using this strategy Daniel gradually began expressing more feelings with adoptive parents. Over the next several weeks, he also began to express feelings his math teacher when he felt upset at school. He found that these adults were increasingly supportive and understanding of his feelings. Parents reported that Daniel experienced growing self-regulation abilities and he used drugs less frequently. With similar parental support he showed significant improvement in cognitions, problem-solving and reading of social cues related to peers. Rather than thinking “No one respects me” and using drugs when the chosen girl continued to not talk to him, Daniel began to date another girl.
Phase 2: Trauma narration and processing of complicated trauma
Overview
Asking youth to talk and think about their complex trauma experiences introduces new challenges to recently gained regulation abilities. However, to the extent that trauma narration and processing allows youth to understand themselves, their relationships and their past experiences in new and more positive ways, it also offers the opportunity for enhancing self-regulation mastery. For many youth, particularly those who have higher levels of anxiety or fear, trauma processing may be necessary to obtain an optimal level of self-regulation (Deblinger et al., 2011). Through the trauma narration and processing phase, youth gradually understand and integrate their traumatic experiences in greater depth.
Therapists are often uncertain about the optimal level of self-regulation needed before beginning the trauma narration and processing phase of TF-CBT for youth with complex trauma. Youth gain increasing ability to use self-regulation skills during the coping skills phase, but often regulation continues to vary in some domains. Since self-regulation is relative, and often fluctuates for these youth, the concept of “stably unstable” is useful. Youth that have gained at least some ability to use coping skills and have “leveled off” in terms of improvement, can be considered stably instable. These youth can usually begin trauma narrative and processing. In other words, it is often unrealistic to expect mastery of these skills before moving onto trauma narrative and processing.
Case example
Daniel had gained substantial self-regulation skills during 14 TF-CBT sessions. However, as mother's pregnancy progressed, he experienced renewed difficulty in expressing feelings and began using drugs with increasing frequency related to his fears of being displaced by the coming baby. For example, when parents invited Daniel to choose the baby's middle name, he believed this was “to remember me after they kick me out” and went on a drug binge. This angered father and he punished Daniel. Daniel pointed to father's anger as proof that parents were about to send him away. Daniel said, “Why shouldn't I get high? Everyone loves that baby and no one ever gave a damn about me.” The therapist agreed that what had happened to Daniel when he was young was very unfair, but suggested that telling his life story would clarify whether anything had changed for him since then. Daniel said that was a stupid idea. The therapist reflected Daniel's irritation by saying that anything she suggested then would probably seem stupid. Having accurately validated his mood Daniel said, “Okay, let's do the stupid f---king story,” and gradually became engaged in trauma processing.
Trauma narrative and processing
Narrative development and processing for youth with complex trauma revolves around the trauma theme rather than a specific trauma type. Specific traumatic experiences, cognitions, feelings, behaviors and other trauma-related experiences are woven into the core theme as appropriate. Many youth cannot create a fully integrated trauma narrative due to the fragmented and non-linear nature of complex trauma memories. The therapist may encourage the development of a “life narrative” which typically begins at the youth's birth or earliest remembered point of reference (e.g., “whom do you first remember living with?”) and then proceeds sequentially, woven around the trauma theme while including specific events, experiences, sensations, thoughts, feelings, and other trauma material that the youth remembers. Using rap or other music the youth likes as a metaphor for story telling may help some youth to engage in trauma processing. Importantly, the therapist meets with the caregiver alone as the youth is creating the narrative to share the developing narrative with the caregiver and prepare the caregiver to support the youth during the upcoming conjoint sessions. Often the caregiver has not previously understood the youth's trauma experiences and/or does not know the impact these experiences have had on the youth. Hearing the youth's trauma narrative enhances the caregiver's ability to more fully understand and support the youth. It is critical to carefully assess the caregiver's ability and motivation to engage in this process. Youth with complex trauma have often experienced relationships with caregivers characterized by inconsistency, neglect, and abuse. They thus may be easily triggered by perceived negative caregiver behavior during conjoint sessions. Therefore, a motivated, well-regulated caregiver is a high priority. If the therapist is not confident the available caregiver is can provide this presence it may be wise to postpone or eliminate conjoint trauma narrative sessions.
Finally, it should be noted that for many youth with complex trauma, the idea of sharing their trauma narrative with a caregiver may be a point of contention. This may be particularly true when the youth has been removed from the custody of their biological parents and placed with an alternative caregiver (e.g., foster parent) who is participating in TF-CBT. Subsequently, the youth may be reluctant for their current caregiver to know their life history. This reluctance often seems to be related to embarrassment/shame, distrust of “the system,” a sense of loyalty to their biological family, or a combination of the three. It is critical to validate the youth's concerns about sharing the trauma narrative, to provide a clear rationale for why it would be specifically beneficial for the youth, and to be open to negotiation (i.e., giving the youth some appropriate choices with regard to when, where, and how the conjoint work occurs). Ultimately, should the youth decide that they do not want to share their trauma narrative with the caregiver this decision should be respected. The youth may perceive failure to respect this decision as a serious violation of the therapeutic relationship, which would be a significant impediment to further treatment progress.
Case example
Kayla said her “whole life was trauma.” She continued to use music as a relaxation strategy and agreed when her therapist pointed out that some of her favorite singers “told a story” in their music. The therapist suggested that Kayla write a song about her own life story, focusing on her theme of not feeling safe because no one protected her. Kayla's memories of these events were recalled in bits and pieces over the course of nine sessions. Her song included the following:
From when I was only three, Dad was always hurting me.
There was never safety for me, only danger waiting for me.
He traded me for drugs and cash like I was just part of his stash.
He said I was just like crack when they had me on my back.
My mom knew all along. I don't know who did more wrong.
Why can't they see there is a me?
Will anyone ever care?
As Kayla created and discussed her narrative with the therapist, the therapist also shared the narrative with Chuck in separate sessions in preparation for upcoming conjoint sessions. It was often very difficult for Chuck to hear about Kayla's previous life (for example, the therapist noted that Chuck was often tearful and angry when hearing the narrative). He was grateful for being included in the treatment since it allowed him to better understand and support Kayla.
Alternatively the therapist may encourage youth to select several seminal “anchors” (e.g., foster homes; schools; significant life events) around which they mentally think about their life and organize the narrative accordingly. For example, TF-CBT often utilizes a timeline to mark down important and traumatic events, which can then be used to organize the narrative.
Case example
Daniel thought of his life as “before grandma,” “with grandma” and “after grandma.” The therapist suggested that they organize this story into these chapters. As Daniel created the following narrative the therapist shared it with the adoptive parents and prepared them for the coming conjoint sessions. Daniel developed the following information over several weeks, in a non-linear fashion. BEFORE GRANDMA: I don't remember. I was alone for a long time, like maybe a month. I drink out of the toilet and there was no water and I had to go to the bathroom. Annabelle (biological mother) always had needles in her arms. All the men beat her up. She beat me up. There was no food and it was cold. It was dark and that's it. The cops come. At foster homes there was food and I went to school. GRANDMA'S: When I went to grandma's I was happy because I had a home and grandma would keep me. I liked living with grandma because she always cooked dinner for me. She put my schoolwork on her refrigerator and said “I love you” every night before I went to sleep. I thought everything was okay, safe and happy in life until I was 9 years old. One day I came home and grandma wasn't cooking dinner. Right then I got the feeling things weren't okay. An hour later grandma fell over and I couldn't wake her up. I called 911 and the ambulance came, but grandma was dead. They called the police and I went back to foster care. I didn't even get to go to grandma's funeral. No one will ever love me like grandma. AFTER GRANDMA'S: In foster care I was mad, kids stole my nice clothes that grandma got me and they didn't even know that those things meant something to me. I was always getting punished and that made me even madder. At first when I got adopted I thought it would be okay even though it wasn't grandma's house. They were nice and got me new clothes. But then they're having a new baby. They only adopted me because they couldn't have their own. Soon it will be here and they won't want me anymore because they'll have their own. It's just like with grandma. I thought everything would be okay and then everything gets taken away again. Maybe it will be okay. I don't know. I'm tired of having to leave. For once I just want a place that lasts.
Developing the trauma narrative is an iterative process that occurs between the youth and the therapist; whatever is created on the written page (or in whatever format is selected) is less important than the actual process that occurs during the therapy sessions between the youth and the therapist. In most cases the final narrative “product” reflects only a very small portion of this process. As the term implies, trauma processing implies that the youth both describes past complex trauma experiences and comes to new understandings about the meaning of these life experiences. In order to successfully process these experiences, the youth must identify and thoughtfully examine the impact of core beliefs related to the underlying theme. Since complex trauma impacts core beliefs in multiple arenas, creating a life or trauma narrative provides many opportunities for identifying and processing deeply internalized maladaptive core beliefs.
Although these beliefs may have served a survival purpose and been functional in the youth's previous living situations, they are now preventing positive adaptations. Although the youth usually understands that their current way of thinking is hurting them and preventing positive changes, changing this requires considerable time during which the youth repeatedly tests an alternative belief to see if it can be trusted. Even after a new belief has been successfully adopted, under stressful circumstances youth are prone to returning to previous maladaptive cognitions. The therapist prepares the youth and caregiver for this occurrence and encourages the youth to re-test the new cognition, usually repeatedly. TF-CBT is believed to be effective for these youth in part because a primary goal is to provide youth and caregivers skills for thinking about things in alternative ways.
Case example
The therapist explored Kayla's beliefs about why no one protected her from the experiences she described in her narrative (sexual abuse by father; father trading her for drugs or money; mother knowing about father sexually abusing her prior to leaving and not protecting her). Kayla initially defended her parents' behaviors by attributing this to “something wrong with me.” The therapist used Socratic dialogue (Cohen et al., 2006; www.musc.edu/cpt) to help Kayla explore this belief. Kayla first said that her parents' maltreatment was because she was probably a “really bad child.” Specifically, she said she cried, broke things and didn't listen. The therapist asked what kind of punishment parents usually use for those kinds of behaviors. Kayla thought and said, “Time out or taking away TV….or maybe being spanked.” The therapist asked,” So those behaviors are not usually punished with sexual abuse. Help me understand what types of behaviors children have that parents should punish with sexual abuse or allowing the child to be sexually abused by someone else for drugs?” Through this strategy, Kayla herself came to see that her parents' behaviors were not typical punishments for children behaving badly.
Through this process, she came to realize that what her parents did was not in response to her behavior or her fault. Kayla was then able to talk about how hard it was to be angry at her parents because she still wished that her parents would care about her and come back for her. The therapist validated this wish and said, “It's really hard to think that you can't control how your parents feel about you or what they do. Part of thinking that what happened was your fault is wishing that you could control what happened. It's hard to accept that you didn't have any control over what your parents did then, or what they do now.” This led Kayla to explore alternative explanations for her parents' abuse and neglect. She came up with several possible explanations (drugs, mental problems, bad childhood, etc.) and said, “It's hard to not know why. And not know if—if they'll ever feel sorry, if they'll ever want to see me again or if they'll ever care about me.” The therapist validated how hard it was to have these unanswered questions. She also acknowledged the difficulty of knowing that she could not change her parents. Having her therapist understand and acknowledge this uncertainty and pain allowed Kayla to more clearly consider how her parents' behaviors had impacted her. Kayla's cognitions shifted over time from internalized responsibility for not being protected (“what was wrong with me?”), to holding her parents responsible. As she confronted the reality that her parents would likely never provide the care she needed, Kayla experienced intense sadness and loss. The therapist provided TF-CBT grief-focused components to address these issues (described below). Kayla developed greater self-acceptance and hope that she would receive what she needed from future relationships. This was facilitated by the safety and nurturance she felt in relationships with the therapist, Chuck, and RTF peers and staff. In this regard she added the following lines to complete her narrative:
“I was filled with despair, thought no one would care But I've found a new way to start every day I'm open to feeling, I know I am healing Thank you for being here.”
In vivo mastery of trauma reminders
For youth who experience generalized avoidance of a specific trauma reminders, developing a hierarchy of feared stimuli and a schedule for gradual exposure to these situations is generally done in a similar manner for youth with complex trauma, with the caveat that these youth may require a longer period of time to achieve mastery of these situations, as in Kayla's example described earlier. However many trauma reminders for these youth will not be specific stimuli related to a traumatic event (e.g., the bedroom in which an episode of sexual abuse occurred). Instead, their trauma reminders are often more general situations and experiences associated with the underlying themes that developed due to trauma exposure. Relatively innocuous relationships may serve as trauma triggers for youth who expect betrayal (Saxe, Ellis, & Kaplow, 2007) as in the case of Daniel's teacher described above. In vivo exposure can be used for these more general situations and experiences also. In Daniel's case, his therapist worked with the teacher to gradually change the relationship to one in which Daniel could experience trust and support. In the RTF setting, youth are naturally exposed to ongoing relationships with the therapist and direct care staff as described earlier, as well as to other residents. Therapists should be mindful of how such exposure can serve as trauma triggers. However, these exposures also provide many opportunities for in vivo mastery as youth gain skills and trust.
Phase 3: Treatment consolidation and closure
Overview
Once the youth completes trauma processing the final phase of TF-CBT encourages the gradual transfer of communicating about trauma and a primary trust relationship from the therapist to the caregiver (if one is participating in TF-CBT treatment); generalizes the ability to establish positive, trusting relationships from the therapist to other important people in the youth's environment; and generalizes the youth's ability to maintain safety in daily life. This phase is often prolonged for youth with complex trauma as they repeatedly apply and “test out” what they have learned earlier in TF-CBT treatment while attempting to establish safety and develop appropriate relationships in real life situations. Including TF-CBT grief-focused components is also relevant for the many youth with complex trauma who have experienced traumatic grief.
Conjoint youth-parent sessions
If a caregiver has participated in TF-CBT several conjoint sessions occur during which the youth typically shares their narrative directly with the caregiver, the youth and caregiver communicate directly about the youth's trauma experiences, and the youth gains confidence that the caregiver will respond supportively to such communications in the future. This is another step in the process of the youth and caregiver building a relationship based on understanding and trust.
Case example
Daniel shared his narrative with parents and they continued to assure him that he was a permanent part of their family. Father said that hearing Daniel's narrative helped him to better understand why Daniel used drugs and “shut down” when father became angry or frustrated with him. During these sessions father also talked about his own father (now deceased), who had been a stern man who demanded obedience and with whom father had had difficulty sharing feelings. Father wanted to be a different kind of father, but said that he knew he sometimes acted the same way his father had. He asked Daniel to be patient with him while they learned together. Daniel was surprised that father did not blame him for everything that went wrong in their relationship but agreed to keep trying.
Enhancing safety and trust
Youth with complex trauma often require additional time to apply what they have learned in TF-CBT to their current (or new) environments. Transitioning from trusting the therapist and a caregiver to trusting new people requires trial and error; as the youth engages in this process the therapist supports the youth to use skills through expected setbacks. As the youth gradually learns to tolerate these disappointments they are offset by successes and growing mastery in multiple domains
Case example
Kayla completed conjoint sessions with Chuck and was doing well in RTF after 20 TF-CBT sessions. However several attempts to transition to foster homes were unsuccessful due to problematic interactions between Kayla and prospective foster parents (e.g., Kayla reported that 1 foster parent threatened her; she ran away from another home during a weekend visit, and got into a physical altercation with a male foster son at a third prospective foster home). Chuck suggested that Kayla was undermining these placements in order to remain in the RTF setting where she felt safe. The therapist explored this with Kayla during two additional sessions focused on enhancing safety. Kayla was able to acknowledge her desire to continue treatment with the current therapist and contact with Chuck whom she viewed as a protective adult presence and to openly say that she was afraid of going to an uncertain future since her past foster care experiences had been unsafe. The therapist explored the possibility of Kayla going to a group home which she was more comfortable with; during the next 2 months Kayla gradually transitioned to a nearby group home. The therapist continued to focus on safety, and how Kayla could use what she had learned during TF-CBT treatment to ease the transition to the new setting. Kayla met the group home therapist and had 3 joint sessions with this therapist and her RTF therapist; during the 4th joint session Kayla volunteered that she had created a trauma narrative in the RTF and that she would share this with the new therapist. Chuck took her to visit the group home, she met several residents whom she liked and after another month Kayla successfully transitioned to the group home. Since Kayla had no community supports, Chuck offered that Kayla could call him at the RTF if she needed support. Kayla called Chuck appropriately and successfully transitioned to the group home.
TF-CBT grief-focused components for youth with complex trauma
The TF-CBT model includes several grief-focused components for youth who have experienced traumatic grief (Cohen et al., 2006; www.musc.edu/ctg). These components are provided after the trauma components described above. Many but not all youth with complex trauma have experienced inappropriate parenting (e.g., Kayla). Although Daniel had also experienced neglect by his biological mother, his most salient traumatic grief issues were related to the death of “grandma” as described below.
Case example
After the birth of Daniel's sister, mother developed significant medical complications requiring a 6 week hospitalization. This triggered past traumatic loss reminders for Daniel, specifically, he “went back in my head to when grandma died.” Daniel was terrified that mother would die like his grandma had. He initially blamed his new sister for causing mother's illness and he refused to go to the hospital to see sister. He initially had several problematic behaviors (aggression in school; drug use; tantrums at home). The supportive network in place was helpful in containing some of these behaviors. Daniel's math teacher met with the school counselor and developed a plan to help Daniel in school; father became Daniel's primary caregiver during this period and worked with the therapist to continue being supportive to Daniel. The therapist initially focused on safety, psychoeducation, and skills components that Daniel had previously mastered, helping him to apply these to the current situation. Once mother's safety was certain, the therapist introduced the TF-CBT grief-focused components. Daniel was initially very hesitant to enter into this work, but reluctantly agreed to, telling the therapist that “I guess I don't have much to lose.” After grief psychoeducation the therapist helped Daniel to talk about what he missed about his grandma and what he would miss in the future. Daniel talked about currently missing grandma's cooking most; he said in the future he would most miss his grandma seeing him graduate from high school since she always told him to get an education. Preserving positive memories about grandma was somewhat challenging because Daniel had no concrete keepsakes… However he described many positive memories which the therapist made into a “memory book.” Daniel also used each letter of grandma's name to write one happy memory of their time together (e.g., “M: made dinner for me every night.”) The therapist then helped Daniel to draw one balloon that he was holding onto, to represent things about grandma that he still had (“memories; what she taught me; and the love we shared.”) Daniel then drew a second “helium balloon” floating into the sky, to represent things about grandma that he had to let go of (“the house we lived in, the time we shared together; being able to hear her voice; and seeing her when I came home from school every day.”) The therapist then talked with Daniel about committing to present relationships. Daniel said that no one could “take grandma's place” but he acknowledged that he was relieved and happy that his parents had stuck by him despite the birth of his sister. After refusing to do so for several weeks, Daniel agreed to visit his baby sister in the hospital. To his surprise he enjoyed holding her and spending time with her. His behavior problems gradually stabilized over the next several weeks and when mother and sister came home he was doing somewhat better. The therapist continued to work with the family to incorporate the skills they had learned for several more sessions until Daniel fully adjusted to sister being part of the family. Treatment closure included addressing the likelihood that Daniel would experience future trauma and loss reminders and planning for how he and his family could cope with these going forward.
Data supporting TF-CBT for youth with complex trauma
TF-CBT studies have typically included youth with complex trauma; the following studies specifically focused on these youth. 1) Three evidence-based treatments were compared to Systems of Care treatment as usual (SOC) for youth in foster care at high risk of placement disruption due to externalizing behavior problems. In this project TF-CBT was modified as described in this paper. Outcomes were assessed using the Child and Adolescent Needs and Strengths (CANS) and the UCLA PTSD Reaction Index. Compared to SOC, TF-CBT led to significantly greater improvement in emotional and behavioral problems and PTSD symptoms and was significantly superior in preventing placement disruption and running away (Weiner, Schneider, & Lyons, 2009). 2) Using the modifications described above, TF-CBT was provided to 30 youth with complex trauma who were adjudicated to RTF. These youth experienced significant improvement in PTSD symptoms from pre- to post-treatment with mean scores on the UCLA PTSD Reaction Index decreasing from 52 to 21 (p<.01) (Cohen & Mannarino, 2011). 3) Two studies of youth with complex trauma from sex trafficking or having been former child soldiers or in the Democratic Republic of Congo received group TF-CBT modified as described above. These youth experienced positive improvements in multiple trauma domains (Paul O'Callaghan, personal communication, December 20, 2011).
Summary
TF-CBT implementation can be conceptualized in a phase-based fashion that is attentive to the needs of youth with complex trauma. This approach maintains the components and flow of TF-CBT, yet allows for additional time and focus on the multiple domains that are problematic in complex trauma cases. TF-CBT should be considered for these youth with the modifications that are described in detail in this paper. Practical strategies include extending the TF-CBT coping skills phase to address the needs of complex trauma; including overarching trauma themes throughout TF-CBT treatment; progressing to the trauma narrative and processing phase even when absolute stability has not yet been attained; and as indicated, allowing for a somewhat longer treatment consolidation and closure phase that includes TF-CBT traumatic grief components. Extensive clinical experience and growing empirical evidence suggests that with some modifications TF-CBT can lead to significant improvement across multiple domains that impact youth with complex trauma. Continued research is warranted in applying TF-CBT for youth with complex trauma.
Acknowledgments
Support for this manuscript was provided in part from funding from Grants No. SM54319, Substance Abuse and Mental Health Services Administration; and R01MH 095208, National Institute of Mental Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Briere J. Professional manual. FL: Psychological Assessment Resources, Inc; 1996. Trauma Symptom Checklist for Children. [Google Scholar]
- Briere J, Spinazzola J. Phenomenology and psycholigcal assessment of complex posttraumatic states. Journal of Traumatic Stress. 2005;18:401–412. doi: 10.1002/jts.20048. [DOI] [PubMed] [Google Scholar]
- Cassidy J, Shaver PR. Handbook of attachment: Theory, research & clinical applications. New York: Guilford Press; 2008. [Google Scholar]
- Cohen JA, Deblinger E, Mannarino AP, Steer R. A multi-site randomized controlled trial for children with sexual abuse-related PTSD. Journal of the American Academy Child Adolescent Psychiatry. 2004;43:393–402. doi: 10.1097/00004583-200404000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. TF-CBT for youth in residential treatment facilities: Preliminary treatment outcome findings. Data reported in NIMH grant application Number R01MH95208 funded to Allegheny Singer Research Institute July 2011 2011 [Google Scholar]
- Cohen JA, Mannarino AP, Deblinger E. Treating trauma and traumatic grief in children and adolescents. New York: Guilford Press; 2006. [Google Scholar]
- Cohen JA, Mannarino AP, Murray LA. Trauma-focused CBT for youth who experience ongoing trauma. Child Abuse & Neglect. 2011;35:637–646. doi: 10.1016/j.chiabu.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook A, Spinazzola J, Ford J, Lanktree C, Blaustein M, Cloitre M, DeRosa R, Hubbard R, Kagan R, Liautard J, Mallah K, Olafson E, van der Kolk B. Complex trauma in children and adolescents. Psychiatric Annals. 2005;35:390–398. [Google Scholar]
- Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry. 2007;64:577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- DeBellis MD, Keshevan MS, Clark DB, Casey BJ, Giedd JN, Frustaci K, Ryan ND. Developmental traumatology, Part II: Brain development. Biological Psychiatry. 1999;45:1271–1284. doi: 10.1016/s0006-3223(99)00045-1. [DOI] [PubMed] [Google Scholar]
- Deblinger E, Mannarino AP, Cohen JA, Runyon M, Steer R. Trauma-focused cognitive behavioral therapy for children: Impact of the trauma narrative and treatment length. Depression & Anxiety. 2011;28:67–75. doi: 10.1002/da.20744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorsey S. Trauma-focused CBT for youth in foster care: preliminary findings from a randomized controlled trial. Presented at the San Diego Conference on Child and Family Maltreatment; San Diego. January 2012.2012. [Google Scholar]
- Finkelhor D, Ormrod RK, Turner HA. Poly-victimization: A neglected component in child victimization. Child Abuse & Neglect. 2007;31:7–26. doi: 10.1016/j.chiabu.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Ford JD, Cloitre M. Best practices in psychotherapy for children and adolescents. In: Cortois CA, Ford JA, editors. Treating complex traumatic stress disorders: An evidence-based guide. New York: Guilford Press; 2009. pp. 59–81. [Google Scholar]
- Ford JD, Cortois CA, Steele K, van der Hart O, Mijenhuis ERS. Treatment of complex posttraumatic self-dysregulation. Journal of Traumatic Stress. 2005;18:437–447. doi: 10.1002/jts.20051. [DOI] [PubMed] [Google Scholar]
- Herman JL. Trauma and recovery. New York: Basic Books; 1992. [Google Scholar]
- Kliethermes M, Wamser R. Trauma-focused CBT for adolescents with complex trauma. In: Cohen J, Mannarino A, Deblinger E, editors. Trauma-focused CBT for children and adolescents: Treatment applications. New York: Guilford Press; [Google Scholar]
- Lieberman AF, van Horn P, Ippen CG. Toward evidence-based treatment: Child – parent psychotherapy for young children exposed to marital violence. Journal of the American Academy of Child Adolescent Psychiatry. 2005;44:1241–1248. doi: 10.1097/01.chi.0000181047.59702.58. [DOI] [PubMed] [Google Scholar]
- Murray LK, Cohen JA, Ellis BH, Mannarino AP. Cognitive behavioral therapy for symptoms of trauma and traumatic grief in refugee youth. Child & Adolescents Psychiatric Clinics of North America. 2008;17:585–604. doi: 10.1016/j.chc.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for PTSD. Traumatic Events Screening Inventory for Children. [Accessed December 4, 2011];2011 Available at http://www.ptsd.va.gov/professional/pages/assessments/assessment-pdf/TESI-C.pdf.
- Pollack SD, Tolley-Schell SA. Selective attention to facial emotion in physically abused children. Journal of Abnormal Psychology. 2003;112:323–338. doi: 10.1037/0021-843x.112.3.323. [DOI] [PubMed] [Google Scholar]
- Saxe GN, Ellis BH, Kaplow JB. Collaborative treatment of traumatized children and teens: The trauma systems therapy approach. New York: Guilford Press; 2007. [Google Scholar]
- Siegel DJ. The developing mind: How relationships and the brain interact to shape who we are. New York: Guilford Press; 1999. [Google Scholar]
- Stein BD, Jaycox LH, Kataoka SH, Wong M, Tu W, Elliott MN, Fink A. A mental health intervention for school children exposed to violence: A randomized controlled trial. Journal of the American Medical Association. 2003;290:603–611. doi: 10.1001/jama.290.5.603. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MB, Decker K, Pynoos RS. The University of California Los Angeles Posttraumatic Stress Disorder Reaction Index for DSM-IV. Psychiatric Assessment. 2004;6:96–100. doi: 10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]
- Weiner D, Schneider A, Lyons JA. Evidence-based treatments for trauma among culturally diverse foster care youth: Treatment retention and outcomes. Child and Youth Services Review. 2009;31:1199–1205. [Google Scholar]


