Abstract
Objective
Applying the science of networks to quantify the discriminatory impact of the ICD-9-CM to ICD-10-CM transition between clinical specialties.
Materials and Methods
Datasets were the Center for Medicaid and Medicare Services ICD-9-CM to ICD-10-CM mapping files, general equivalence mappings, and statewide Medicaid emergency department billing. Diagnoses were represented as nodes and their mappings as directional relationships. The complex network was synthesized as an aggregate of simpler motifs and tabulation per clinical specialty.
Results
We identified five mapping motif categories: identity, class-to-subclass, subclass-to-class, convoluted, and no mapping. Convoluted mappings indicate that multiple ICD-9-CM and ICD-10-CM codes share complex, entangled, and non-reciprocal mappings. The proportions of convoluted diagnoses mappings (36% overall) range from 5% (hematology) to 60% (obstetrics and injuries). In a case study of 24 008 patient visits in 217 emergency departments, 27% of the costs are associated with convoluted diagnoses, with ‘abdominal pain’ and ‘gastroenteritis’ accounting for approximately 3.5%.
Discussion
Previous qualitative studies report that administrators and clinicians are likely to be challenged in understanding and managing their practice because of the ICD-10-CM transition. We substantiate the complexity of this transition with a thorough quantitative summary per clinical specialty, a case study, and the tools to apply this methodology easily to any clinical practice in the form of a web portal and analytic tables.
Conclusions
Post-transition, successful management of frequent diseases with convoluted mapping network patterns is critical. The http://lussierlab.org/transition-to-ICD10CM web portal provides insight in linking onerous diseases to the ICD-10 transition.
Keywords: ICD-9-CM, ICD-10-CM, billing complexity, transition to ICD-10-CM, networks, motifs
Introduction
The World Health Organization (WHO) released the International Classification of Diseases V.10 (ICD-10) in 1990. While the rest of the world transitioned to ICD-10 (∼14 000 codes) in the late 1990s, the USA will be transitioning from International Classification of Disease 9th Revision Clinical Modification (ICD-9-CM; 14 567 codes) to ICD-10-CM (∼68 000 codes) as of 1 October 2014. Using the Center for Medicare and Medicaid Services (CMS) mapping tables, the American Medical Association (AMA) predicts implementation costs of US$83 000 to US$2.7 million per practice.1
Fundamentally, changing the controlled billing terminology impacts our capacity to compare, contrast, manage, and plan future needs during the transition to the new coding set, ICD-10-CM. These concerns were also voiced when the US government transitioned from ICD-8, ICDA-8, and H-ICDA-2 in 1979.2
As encoding into these terminologies is usually performed manually or semi-automatically, there is a potential impact on the overall accuracy. The ICD-10-CM coding system contains three times the number of codes, which requires using an entirely new coding organization, or significantly restructuring the relationships between codes. In other words, memorized codes, training, and coding-support software need to start afresh. Some commercial software have been proposed to bridge this transition, but there are limited details on their capabilities.3 Training materials have been provided by a number of organizations. However, the material is either at the planning stage or more qualitative. Few provide specific analytic tools to identify high value challenges.3–5
We hypothesized that network models6 can without bias identify problematic ICD-9-CM to ICD-10-CM mapping patterns (mapping motifs) and quantify their proportions per clinical specialty. We further hypothesized that these mapping motifs can clarify and quantify the administrative and financial impact arising from the ICD-10-CM implementation in clinical datasets. In this report, we quantify unaddressed ambiguities and redundancies arising from mappings between ICD-9-CM and ICD-10-CM codes. We establish that the meanings of a high proportion of the ICD-9-CM to ICD-10-CM mappings are entangled in complex mapping motifs that have the potential to induce inaccuracies and reporting errors. Using a case study of emergency departments’ Medicaid data, we demonstrate how a substantial proportion of non-reciprocal or abstruse mappings have the potential to disrupt billing and clinical practice.
Methods
An overview of the methodology appears in supplementary figure S1 (available online only). Data integration and analyses are detailed in sections A–E and table 1. The research project was approved by the University of Illinois Institutional Review Board (id#2012-0150).
Table 1.
Datasets
| Descriptions | Abbreviations |
|---|---|
| ICD-10-CM release (2012) release7 | ICD-10-CM |
| Center for Medicaid and Medicare Services mapping files for General equivalence mappings8 (Accessed 02/29/2012): ICD-9-CM to ICD-10-CM maps (2012_I9gem.txt); ∼100 000 relationships ICD-10-CM to ICD-9-CM maps (2012_I10gem.txt) |
CMS–GEM (2 files) |
| 2010 Emergency departments statewide Medicaid billing data for all patients with University of Illinois as primary home; 24 008 patient visits in 217 emergency departments | (IHC–ED) |
Three datasets were used. Twenty-two per cent of the Illinois Health Connect, Emergency Department (IHC–ED) care was delivered at University of Illinois Hospital, and the remainder of the data were generated from 217 other facilities. An expert curator reviewed 100 randomly selected Center for Medicaid and Medicare Services (CMS)–general equivalence mappings (GEM) maps and observed one error (95% CI 0.2% to 5.0% precision).
Construction of bidirectional mapping network from unidirectional maps of CMS–GEM
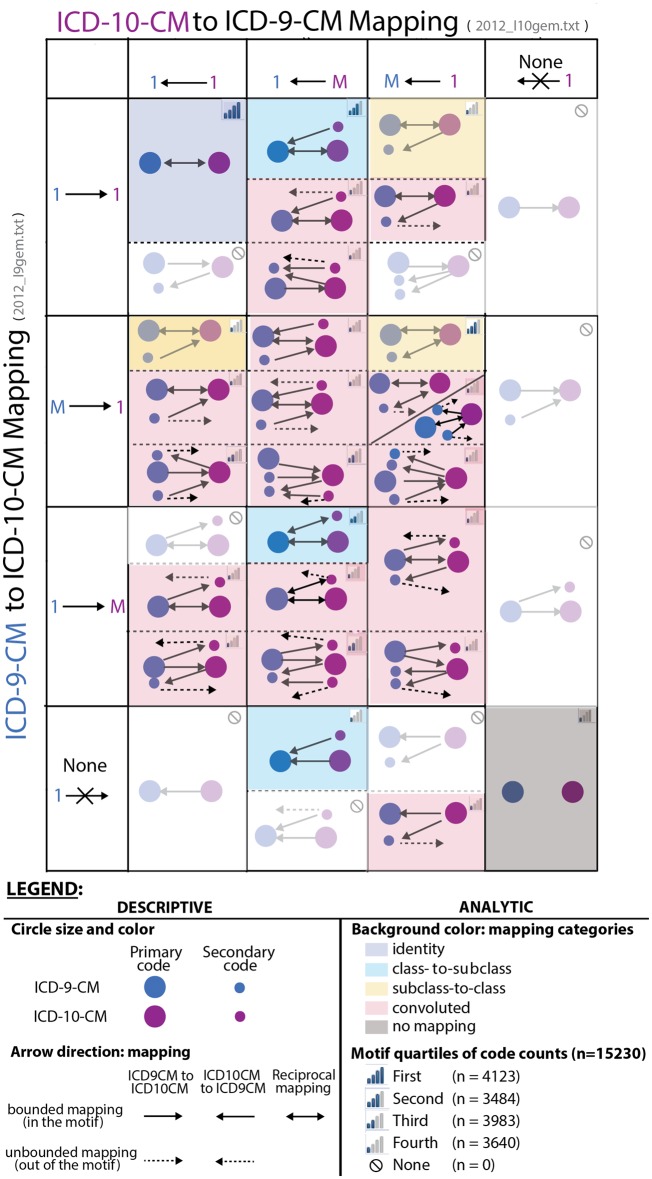
CMS–general equivalence mappings (GEM) files provide distinct directional mapping tables from ICD-9-CM to ICD-10-CM and from ICD-10-CM to ICD-9-CM because the mappings are not necessarily reciprocal.8 From the CMS mapping tables described in table 1, we created a bipartite network consisting of two types of nodes (ICD-9-CM and ICD-10-CM codes) and their directed relationships (arrow pointing in the direction of the mapping) (figures 1 and 2A; tables 2 and 3). This was loaded as a large table in MySQL V.5.0.18 (table 4). Of note, approximately 14 000 ICD-9-CM codes directionally map to only approximately 18 000 of the approximately 68 000 ICD-10-CM codes, while nearly all 68 000 ICD-10-CM codes map to ICD-9-CM codes. Therefore, the two mapping tables are required in order to query patient data coded in ICD-10-CM, and to compare these to ICD-9-CM coded data (table 1, 2012_I9gem.txt and 2012_I10gem.txt). In each CMS table, mapping is unidirectional, either ICD-9-CM to ICD-10-CM (table 1, 2012_I9gem.txt) or the reverse (table 1, 2012_I10gem.txt). In the CMS map of ICD-9-CM to ICD-10-CM maps (2012_I9gem.txt file), each row represents a single ICD-9-CM to ICD-10-CM mapping. We then calculate the number of distinct ICD-10-CM codes associated with each ICD-9-CM code and vice versa. This leads to a model of the cardinality of these relationships represented on the vertical axis in figure 1: as one-to-one (1→1), many-to-one (M→1), one-to-many (1→M), and none. We similarly modeled the CMS map of ICD-10-CM to ICD-9-CM (2012_I10gem.txt file) to produce the columns of figure 1. As the bidirectional mappings are not necessarily reciprocal, their complex combinations have been systematically detailed in figure 1, where each axis describes the type of unidirectional mapping (vertical axis: ICD-9-CM to ICD-10-CM; horizontal axis: ICD-10-CM to ICD-9-CM) and where each of their combinations generate a bidirectional mapping motif (cells of the matrix).
Figure 1.
ICD-9-CM to ICD-10-CM conversion: from bipartite mapping maps to insightful network motifs (see Methods section). The mapping of ICD-9-CM to ICD-10-CM and back yields complex networks that we simplified into elementary motifs represented in this figure. Seventy-five per cent of the ICD-9-CM codes are represented by the top seven mapping motifs. Importantly, 63% of ICD-9-CM codes occur in simple mapping motifs (motifs with no dashed arrows). Interestingly, 1% of ICD-9-CM codes have no corresponding ICD-10-CM codes. However, the remaining 36% of convoluted motifs (pink background, dashed arrows) are likely to be harder to understand for coders, clinicians, and managers. An ICD-9-CM mapping that proceeds via a convoluted motif leads to a complex interpretation of its corresponding ICD-10-CM code(s). Indeed, there is no straightforward way to query patient data across the ICD-9-CM and ICD-10-CM divide of convoluted motifs. Due to the non-reciprocal mappings, the majority of convoluted motifs are unbounded (dashed arrows). Blurred matrix cells contain no ICD-9-CM codes (legend; empty set). Each of the matrix cells comprises one or more mapping motifs that are further synthesized into five mapping categories utilized in figures 2–4 (background color, legend). Of note, the illustrated motifs represent 98.9% of the discovered ones.
Figure 2.
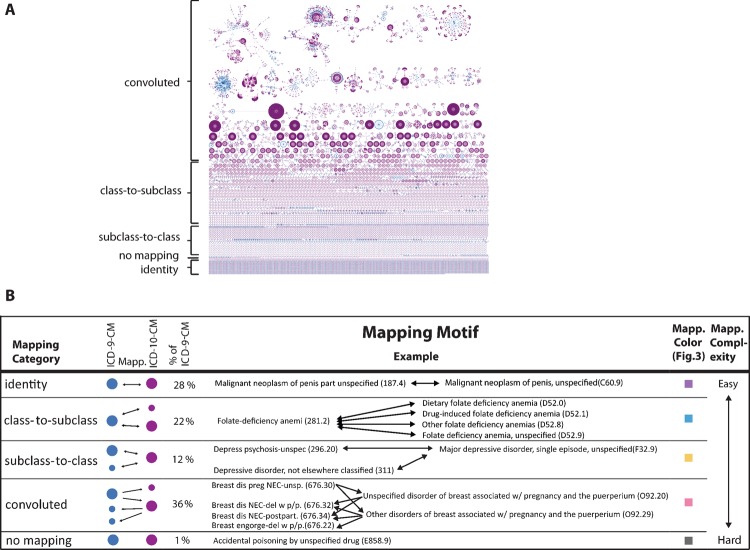
From ICD-9-CM to ICD-10-CM mapping network to actionable categories of motifs. Using Center for Medicare and Medicaid Services ICD-9-CM to ICD-10-CM mapping tables, the full network of (A) illustrates the complexity of mappings attributable to mappings (lines) between ICD-9-CM (blue circles) and ICD-10-CM (purple circles). In (A), large purple networks correspond to thousands of ICD-10-CM codes associated with a single ICD-9-CM code, while large blue networks are the converse. In addition, the mappings are not reciprocal leading to entanglements between the meanings of different codes (figure 1). Twenty-seven distinct patterns of mapping motifs (figure 1, background color) were observed and classified into five mapping categories organized by increasing complexity (B, first column) each category has a specific color scheme (B, fifth column) utilized in the background of figure 1 and the bar graph of figures 3 and 4. The abbreviation, Mapp., refers to mapping. Each mapping category is illustrated with an example (A, B, columns 3 and 4). The examples of the two last categories demonstrate the difficulties that may arise from interpreting data collected in ICD-9-CM or in ICD-10-CM, which may affect a clinical practice beyond billing practices. For example, the concept of ‘Accidental poisoning by unspecified drug’ does not exist anymore in ICD-10-CM, where emergency department physicians will be required to specify the drug category, which requires a certainty not reflecting clinical practice.
Table 4.
Resource sharing of ICD-9-CM and ICD-10-CM mapping motifs and categories
| Resource sharing work product | Use case or targeted audience | Description or content |
|---|---|---|
| Comprehensive network in high resolution | Within the complex entire network, identify specific ICD-9-CM and ICD-10-CM codes searchable in PDF format. Audience: clinical informaticians and analysts. | http://lussierlab.org/transition-to-ICD10CM/Scalablenetwork-small.pdf |
| Tables of mapping motifs and categories (.xls format) | Rapid reuse in software developed by health information technologists and informaticians. | http://lussierlab.org/transition-to-ICD10CM/ICD-9–10-Transl-Cat.xlsx, 326643 rows, eight columns headers |
| SQL database of mapping motifs and categories | Lookup of SQL queries and specific results by health system analysts strategically to improve health system operations and plan transition to ICD-10-CM. |
http://lussierlab.org/publication/Motif_table_SQLcode/ DB name, 38 distinct queries, one table, 324913 rows, five columns |
| Web portal | Administrator, clinicians, and other users studying a practice pattern in ICD-9-CM and ICD-10-CM. They copy and paste the patient encounter statistics of their clinical practice or health system coded in ICD-9-CM, and organized in a table. |
http://lussierlab.org/transition-to-ICD10CM Input: Insert multiple ICD-9-CM codes of interest with patient encounters’ statistics (counts or frequency or claims). Output: Visualization of ICD-9-CM, ICD-10-CM, relationships and associated mapping categories in two formats: dynamic network figure or tabular. |
Available at http://lussierlab.org/transition-to-ICD10CM.
We further combined unidirectional mappings from ICD-9-CM to ICD-10-CM to those of ICD-10-CM to ICD-9-CM, thus creating a complex bidirectional network. The complex network of bidirectional mapping is illustrated in figure 2A using Cytoscape V.2.8,9 where the blue nodes are ICD-9-CM codes, the purple nodes are ICD-10-CM codes, and the arrows represent mapping between two codes.
Decomposition of the bidirectional mapping network in bidirectional mapping motifs and defining bounded versus unbounded mapping motifs
The combination of these two directions of mapping (ICD-9-CM to ICD-10-CM and vice versa) can be synthetized as bidirectional mapping motifs. For example, the simplest mapping motif corresponds to one ICD-9-CM mapped to one ICD-10-CM (figure 1 mauve background). On the other hand, some of the most complex mapping motifs arise as illustrated in the other combinations of rows and columns. We systematically indexed each type of mapping motif via specialized SQL queries for each matrix cell (provided with the database, table 4). Of note, a single ICD-9-CM code mapped to a single ICD-10-CM code from file 2012_I9gem.txt (table 1) is used as a computational seed (seed) for each mapping motif calculation with the exception of J-IV, for which there are no mappings to an ICD-10-CM code. This seed is presented in figure 1 as: (1) a single large blue circle (primary ICD-9-CM code); (2 a single large purple circle (primary ICD-10-CM code); and (3) the corresponding relationship (arrow) between the two. For each seed, the first step of the mapping motif construction consists in finding the additional non-primary ICD-9-CM codes that map to the primary ICD-10-CM codes using the 2012_I9gem.txt file, as well as in finding if they map to other non-primary ICD-10-CM codes (defined here as secondary ICD-9-CM codes and represented by small purple circles in figure 1). In addition, non-primary ICD-10-CM codes targeted by the primary ICD-9-CM code of the seed are discovered at this step (these are defined as secondary ICD-10-CM codes). Of note, there may be no mapping to an ICD-10-CM code for a primary ICD-9-CM code. The second step consists in mapping the primary ICD-10-CM code of the seed, as well as the secondary ICD-10-CM codes (discovered in the first step) back to the ICD-9-CM code using the 2012_I10gem.txt file. Within this step, we also identify all non-primary ICD-10-CM codes mapping to the primary ICD-9-CM code (these are also defined as secondary ICD-10-CM codes). These ICD-10-CM to ICD-9-CM maps can point to the primary ICD-9-CM code of the seed and/or additional non-primary ICD-9-CM codes (also defined as secondary ICD-9-CM codes represented by small blue circles in figure 1). The third and fourth steps consist in repeating steps one and two to determine whether or not the mapping motif identified in the first two steps is limited to these relationships (bounded mapping motifs) or the motif keeps propagating in the network (unbounded mapping motifs represented by dashed lines pointing out of the mapping motif in figure 1). Of note, many ICD-10-CM codes are not targeted by the computational seeds that originate from the 2012_I9gem.txt maps. An additional step consists in identifying ICD-10-CM codes with no mapping to ICD-9-CM codes in the 2012_I10gem.txt file. Each cell in the figure 1 matrix corresponds to one mapping motif. Our analysis identified 37 distinct mapping motifs. We then quantified the number of distinct seed ICD-9-CM codes in each of the remaining mapping motifs, and organized the results as quartiles (figure 1 bar graphs).
An alternative approach, addressed briefly in the Results and Discussion sections, consists in seeding the relationship using the ICD-10-CM to ICD-9-CM mapping rather than the ICD-9-CM to ICD-10-CM mapping.
Organization of mapping motifs into mapping categories and complexity
In order to provide reports to a non-informatician audience (eg, clinicians and administrators) (figures 1 and 2B, table 4), we aggregate the mapping motifs further into five bidirectional mapping categories: identity (mauve background; figure 1); class-to-subclass (blue background; figure 1); subclass-to-class (yellow background; figure 1); convoluted (pink background, figure 1; majority of matrix cells); no mapping in either direction (gray background; figure 1; figure 2B, examples of motifs). In figure 2B, the percentage of distinct primary ICD-9-CM (seed of each distinct motif) is reported for each mapping category (when an ICD-9-CM code is primary in multiple motifs, it is counted in the most complex motif, thus each ICD-9-CM code is counted only once). By definition, the identity, class-to-subclass, subclass-to-class, and no mapping categories are composed exclusively of bounded motifs and are thus bounded mapping categories (table 2). The convoluted category is defined by exclusion as motifs that are more complex than the four other categories. Furthermore, the convoluted category is the only one comprising unbounded mapping motifs (represented with dashed lines in figure 1). However, some bounded mapping motifs may be the recipient of mappings (see Methods section: Calculation of mapping motifs’ entanglement).
Table 2.
Key concepts
| Type | Term | Definition |
|---|---|---|
| Network construction | Bipartite graph | A graph whose nodes are clustered in two disjoint sets (in this manuscript the sets are ICD-9-CM and ICD-10-CM nodes). Every relationship connects one node of a set with one of the other set. |
| Computational seed | In this manuscript, a computational seed corresponds to a single ICD-9-CM code mapped to a single ICD-10-CM code in the 2012_I9gem.txt file. It is used as an input for each calculation of the motifs. | |
| Crosswalk | A term that the American Medical Association uses to describe directional mappings between ICD-9-CM and ICD-10-CM. http://www.ama-assn.org/resources/doc/washington/crosswalking-between-icd-9-and-icd-10.pdf. | |
| Directional relationship | Relationship between two nodes that is explicitly directed from an originated node to a destination node. Here used to represent mappings between ICD-9-CM and ICD-10-CM. | |
| Graph | Mathematical representation of a set of objects (called nodes) connected in pairs by one or many links (called edges or relationships). | |
| Node | In this manuscript, nodes are ICD-9-CM or ICD-10-CM codes. | |
| Reciprocal relationship | Relationship between two nodes that has both directions. In this manuscript, mappings between ICD-9-CM and ICD-10-CM found in both the 2012_I9gem.txt and the 2012_I910gem.txt files. | |
| Relationship | A relationship is a mapping between two nodes (ie, two ICD codes). | |
| Network analysis | Bounded/unbounded mapping motif | A bounded mapping motif is a motif from which all the relationships originating from it are constrained to the motif. Conversely, in an unbounded mapping motif, the relationships propagate in the network, out of the motif. |
| Class-to-subclass (mapping motif category) | Motif category representing the mapping of an ICD-9-CM code to several ICD-10-CM codes, each being a more precise definition of the first. | |
| Complexity, mapping complexity | In the context of the clinic–administrative transition to ICD-CM-10, we arbitrarily defined an ordinal scale of complexity for mapping motif categories; from less to more complex: identity, one-to-many, many-to-one, convoluted, or no mapping. | |
| Convoluted (mapping motif category) | Motif category defined by exclusion as motifs that are more complex than the four other motif categories. | |
| Entanglement | Entanglement between mapping motifs occurs when either mapping motifs are unbounded and point into other mapping motifs or when other mapping motifs point into a bounded motif (see example in supplementary methods, available online only).. | |
| Identity (mapping motif category) | Motif category defined as a single reciprocal mapping between an ICD-9-CM code and an ICD-10-CM code. Those codes are left unchanged. | |
| Mapping motif category | Five different motif categories were identified that classify the motifs: (1) identity, (2) convoluted, (3) class-to-subclass, (4) subclass-to-class, (5) no mapping. | |
| Mapping motif | Identified mapping pattern in the bipartite network. | |
| No mapping (mapping motif category) | Motif category representing all codes that are not mapped from ICD-9-CM to ICD-10-CM and vice versa. | |
| Subclass-to-class (mapping motif category) | Motif category representing the mapping of several ICD-9-CM codes to one ICD-10-CM code, thus aggregating and generalizing the initial definition. |
In the tables and figures, each ICD-9-CM code is counted only once according to the highest complexity of its associated mapping motif category (table 2, definition of complexity). Indeed, an ICD-9-CM code may be considered primary in multiple seeds, each of which has an associated mapping motif classified in one of five mapping motif categories.
Calculation of mapping motifs’ entanglement—a higher level of complexity
Entanglement between mapping motifs occurs when either mapping motifs are unbounded and point into other motifs or when other mapping motifs point into a bounded mapping motif (not represented in figure 1 for simplicity) (table 3). An example of entanglement between a bounded mapping motif and an unbounded one is provided in the supplementary methods (available online only). Therefore, unentangled mapping motifs provide straightforward transitions from ICD-9-CM to ICD-10-CM because they are bounded (do not point to other motifs), and no other mapping motifs point to them.
Table 3.
Entanglement of diagnosis coding alternatives: complexity of ICD mappings pointing into translational motifs of each category
| Mapping category (total number of motifs) | Entanglement: additional ICD-10-CM codes (ICD-10-CM→ICD-9-CM) pointing to the motifs of the mapping category (% & count of affected motifs) | Entanglement: additional ICD-9-CM codes (ICD-9-CM→ICD-10-CM) pointing to motifs of the mapping category (% & count of affected motifs) | Entanglement total |
|---|---|---|---|
| Identity (4123) | 0 | 0 | |
| Class-to-subclass (3260) | N/A | 6% (184) | |
| Subclass-to-class (1757) | 39% (694) | N/A | |
| Convoluted (5280) | 100% (5280) | Not calculated | |
| No mapping (147) | N/A | N/A | |
| Motifs TOTALS (14567) | 42% (6158) |
Each mapping motif was constructed from a seed mapping of one ICD-9-CM code mapped into one ICD-10-CM code with two additional lookups of mappings: all mappings back to ICD-9-CM from the seed ICD-10-CM potentially generating secondary ICD-9-CM codes, and all mapping of the latter secondary ICD-9-CM thus generating secondary ICD-10-CM codes. Here, we show a summary of the motifs connected by higher order mappings (third and higher), which we term entanglement because of the added complexity this introduces.
Summarization of ICD-9-CM codes in clinical classes
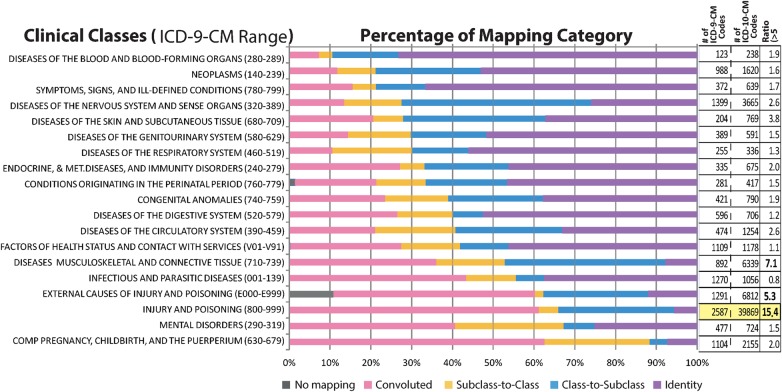
Clinical classes were constructed from the topmost ICD-9-CM hierarchies, which served as a basis to calculate the impact of the mapping to ICD-10-CM codes across clinical specialties (figure 3). The range of ICD-9-CM codes is reported beside each clinical class (figure 3). Each ICD-9-CM code was previously assigned a corresponding mapping category (see Methods section: Organization of mapping motifs into mapping categories and complexity), as well as a clinical class, from which the proportions were calculated and shown as horizontal bars (figure 3; color coding legend). In addition, the total count of ICD-9-CM codes and of ICD-10-CM codes are reported, as well as the ratio of the count of ICD-10-CM to ICD-9-CM to determine the importance of the change between versions of ICD. All novel ICD-10-CM clinical classes were manually mapped to their equivalent ICD-9-CM clinical classes for comparative purposes.
Figure 3.
Discrimination by clinical specialty. Furthermore, clinical specialty is unequally impacted as shown with the percentage of ICD-9-CM codes per mapping category (color coding of the bars from figure 2B, column 5). Clinical classes with a larger proportion of convoluted network motifs and higher ICD-10-CM to ICD-9-CM codes ratios are most likely to be affected by the transition. Mapping categories range from simple (identity) to convoluted, and are used as a proxy to estimate the impact of ICD-10-CM transition to clinical practice. Convoluted and no mapping will incur disproportionally more costs than simple motifs of mappings due to the inability to compare clinical practice before and after transition using ICD codes. In addition, a ratio was calculated comparing the number of total codes per clinical class (figure 3, rightmost column [#ICD-10-CM]/[#ICD-9-CM]). ‘Injury and poisoning's’ outstandingly high ratio is highlighted in yellow).
Case study calculations
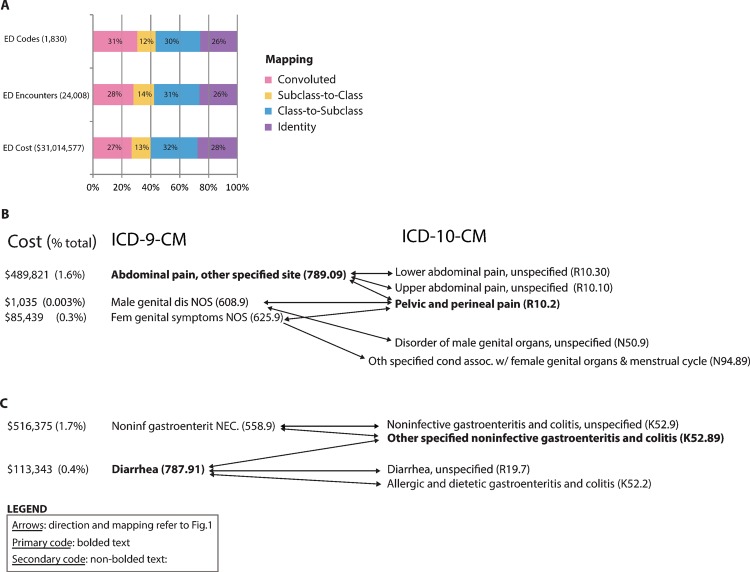
All primary ICD-9-CM codes of emergency department encounters (Illinois Health Connect, emergency department dataset, table 1) were tallied and assigned to a mapping category of identity, class-to-subclass, subclass-to-class, convoluted, or no mapping (Methods section: Organization of mapping motifs into mapping categories and complexity) (figure 4). By design, for simplicity of the network and interpretation, no secondary ICD-9-CM codes associated with encounters were included. The number of encounters for each ICD-9-CM code was counted, as well as the total cost of each ICD-9-CM code for the year, and summarized for each mapping category (figure 4A). Analysis was performed on the high cost ICD-9-CM codes to evaluate the impact of convoluted mappings and the two highest ICD-9-CM codes associated with the highest costs were shown with their mapping motifs (figure 4B,C).
Figure 4.
Case study: identifying ICD-10-CM conversion challenges in 24 000 clinical encounters in 217 emergency departments. (A) The convoluted mapping categories correspond to approximately 27% of the emergency department (ED) costs, encounters and codes, increasing the risk of inaccuracies and errors and has significant implications on the data reliability pre and post-ICD-10-CM transition; 31% of the billed ED codes were convoluted and corresponded to 28% of visits and 27% of costs, while 56% of codes were the less complex mapping motifs (blue and purple) which correspond to 57% of encounters and 60% of costs. Interestingly, there was a 3.6% decrease of ED payments for encounters coding to convoluted mapping category and an increase of 5.2% for those associated witho less complex mapping categories. There is no inherent inconsistency of the payment variations because complexity of mapping from ICD-9-CM to ICD-10-CM is not associated with the amounts of diagnoses payments. (B) Example of convoluted mapping in the ED: ‘Abdominal pain’ with associated cost data. Of note, Center for Medicare and Medicaid Services mapping confounds mappings of male and female genital symptoms (ICD-9-CM) with abdominal pain location (ICD-10-CM). Post-transition, gender-specific information will be required in addition to the ICD codes for inventory management of speculum. (C) Example of convoluted mapping in the ED: ‘diarrhea’ and ‘non-infection gastroenteritis’ are confounded in ICD-10-CM with implication for infectious disease protocols and inventories (eg, culture sampling, disposable isolation supplies).
Results
Descriptive statistics of the ICD-9-CM to ICD-10-CM mapping network
In summary, we simplified a complex mapping network of approximately 80 000 ICD codes and approximately 100 000 mappings to a network of five types of mapping categories of approximately 14 000 motifs and approximately 6000 relationships. Only approximately 60% of the motifs are easily understood (unentangled; tables 3 and 4).
The entire bidirectional mapping network is composed of 23 912 mappings of 14 567 ICD-9-CM to 16 604 ICD-10-CM codes and 78 840 converse mappings from 69 833 ICD-10-CM to 11 603 ICD-9-CM codes, of which only 4123 are reciprocal (figure 2A; also available as a scalable version, table 4). Thirty-seven distinct mapping motifs were predicted from the systematic combination of unidirectional mappings from ICD-9-CM to ICD-10-CM and the converse maps, but only 28 mapping motifs contained actual mappings (figure 1; database and SQL queries provided—see middle line of table 4). Furthermore, these mapping motifs could be synthetized as five mapping categories for which the proportion of associated distinct motifs are described in figure 2B (the number of primary ICD-9-CM codes represents each motif, figure 1, Methods). We first report that convoluted motifs account for 36% of the network, with a potential impact on transitioning well-defined clinical conditions and their management (figure 2B). Forty-two per cent (6158) of all ICD-9-CM codes are entangled in more than one mapping motif (table 3).
Of note, an alternative method to calculate the motifs could proceed using a seed relationship starting from ICD-10-CM and mapped to ICD-9-CM. The network of figure 2B remains the same. Only the proportion of motifs would differ in figure 1, but the matrix remains with the same axes and cells (not shown). The corresponding proportions of mapping categories are: 0.3% identity, 1% class-to-subclass, 10% subclass-to-class, 87% convoluted, and 1% no mapping (reported from the count of ICD-10-CM codes).
Impact of mapping motifs on clinical specialties
By distributing these mapping motifs into clinical classes, we have estimated the proportion of increasingly more complex mapping (figure 3). From the proportion of convoluted mapping motifs (figure 3, pink bars), we determined that hematology and oncology are poised for easy transition, while obstetrics, psychiatry, and emergency medicine (poisoning) will be among the most challenged. Furthermore, 42% of infectious disease code mappings remain convoluted, which will impact most specialties. In addition, harder to transition ICD-10-CM to ICD-9-CM code ratios greater than five are found in musculoskeletal, injury, and poisoning clinical classes (figure 3, right columns).
Shared resources
We computed ICD-9-CM codes, their mapping category, their corresponding ICD-10-CM codes, and their unique subnetwork identifier (table 4, second line). We also created a web portal to help mitigate the mapping challenges for IT personnel, clinicians, and administrators (table 4, last line). On the web portal, the mapping from ICD-9-CM to ICD-10-CM codes and inversely is provided for user-defined lists of ICD-9-CM codes with options for a tabular output (text files) and a dynamic network visualization as a web portal.
Case study
In a case study of 24 008 encounters from 14 472 patients of 217 emergency departments in Illinois for calendar year 2010 (table 1, Illinois Health Connect, emergency department), we calculated the impact of conversion to ICD-10-CM codes on the visits and costs (figure 4A). A total of 59 846 ICD-9-CM codes was affiliated with these encounters. On average, 27% of the costs are attributed to ICD-9-CM codes for which the associated mapping motifs to ICD-10-CM are convoluted. As illustrated in figure 4B, abdominal pain displays a cost of over US$500 000/year (1.8% of emergency department billing in Illinois) mapping to many ICD-10-CM codes and back to other ICD-9-CM codes. Gastroenteritis is similarly convoluted (1.7% of emergency department billing, figure 4C).
Discussion
By using exclusively CMS data for determining the complexity of mappings, this study was designed with simplification and clarification of this complexity using network topology transformation from ICD-level relationship to motif level relationships, and reports straightforward metrics to facilitate the interpretation of results by a broader community of administrators and clinicians.
Contribution of network metrics to ‘change management’ of terminologies
Full network analyses have yielded valuable insight into the pleiotropy of genes between different diseases9 and have been applied to clinical claims coded in ICD codes for discovery of patterns.10 11 In addition, a number of simplified networks such as directed acyclic graph (DAG) theory-based approaches have been applied to the hierarchical system of a controlled terminology12 (eg, segmentation service, partition tools, etc). However, these systems were not designed for full graph analyses or bipartite graphs. Furthermore, change management approaches to controlled terminologies, developed by clinical informaticians and ontologists, have been focused on semantics and DAG or tree-like hierarchies within a version of a terminology.6 13–15 The bipartite network revealed by the transition from ICD-9-CM codes to ICD-10-CM codes requires a different paradigm, as it cannot be simplified to a DAG16 nor defined exclusively with the desiderata of controlled terminology.17 Furthermore, the well-established formalisms of ambiguity and redundancy14 of terms within a terminology are insufficient to describe unbounded and convoluted motifs. Indeed, the class-to-subclass mapping category (23% of ICD-9-CM codes, figure 2B) can be viewed as both a mapping to potentially redundant ICD-10-CM codes for an ICD-9-CM code, as well as an ambiguous ICD-9-CM code disambiguated in multiple coding to ICD-10-CM. The converse applies to the subclass-to-class mapping category (12% of ICD-9-CM codes, figure 2B). While a focus in semantics is sufficient to address a small number of changes between two updates of a terminology, we show here how the significant changes imparted by the ICD-9-CM to ICD-10-CM transition require additional structural metrics that characterize the complexity of bipartite networks of mappings. In our framework, the cardinality of relationships is initially described according to the direction of mapping (see Methods section: Construction of bidirectional mapping network from unidirectional maps of CMS–GEM): ICD-9-CM→ICD-10-CM and then ICD-10-CM→ICD-9-CM. Reciprocal cardinalities are 1→M and 1←M of which a subset is bounded and labeled as the ‘class-to-subclass’ category. Similar reciprocal cardinalities are observed for the bounded mapping categories labeled as ‘identity’ and ‘subclass-to-class’. The combination of two non-reciprocal cardinalities produces exclusively unbounded motifs: M→1 and 1←M, as well as 1→M and M←1. This principle has a practical application: one can determine a priori that some pairing of cardinalities for an ICD-9-CM code will obligate unbounded motifs. As cardinalities can be calculated in simple tables, there is no need to construct or analyze a network to determine that a subset of unbounded motifs would arise from combinations of mappings forward and back for each ICD-9-CM code. It follows that unbounded motifs correspond to unconstrained definitions or undetermined meanings in semantics. This network composition principle is also scalable to the translation of terms between any two terminologies (eg, applicable to the unified medical language system).15
Lessons learned from other ICD transitions and our study
The WHO ICD-9 (7000 terms) transition to ICD-10 (14 400 terms) met with the following challenges. In a Swiss analysis, co-morbidity coded in the simpler ICD-10 that required 5 years of coding sensitivity (recall), improved from 37% to 43% using detailed chart abstraction, which was attributable to the coders’ ‘learning curve.’18 Of note, the authors do not mention pre-ICD-10 coding accuracies. Thirty-two diagnoses assessed from billing data in another study comprising 4008 randomly selected charts were re-coded in ICD-9-CM and compared to the billed ICD-10-CA (Canadian enhancement to ICD-10). The authors report a low sensitivity for all conditions in both coding systems (9–72%), worsening in seven diagnoses in ICD-10-CA.19 Within the field of the Centers for Disease Control and Prevention (CDC) public health in the USA, over two million decedents were coded in both the WHO of ICD-9 and ICD-10 (6969 and 14 199 codes, respectively).20 The authors observe inconsistencies in outcomes when coded as ICD-9 versus ICD-10, with sensitivity as low as 26% for some categories of death. They conclude that there is a substantial impact of this transition on relative risk estimates.20 They recommend recoding cause of death in ICD-9 to avoid bias during the transition to ICD-10. Based on 1 852 671 individuals recoded from ICD-9 to ICD-10 from the 1996 national vital statistics reports of the CDC, substantial discrepancies in death were attributed to the differences in coding scheme.21 For example, septicemia was 20% more likely to be selected in ICD-10 than in ICD-9, adding over 3000 additional cases. Conversely, bronchitis was 60% less likely to be selected in ICD-10. From the study, the following diseases demonstrated discontinuity: septicemia, influenza, pneumonia, Alzheimer’s disease, nephritis, nephrotic syndrome, and nephrosis.
Unsurprisingly, our results corroborate these previous reports of considerable disruption in reporting clinical data post-ICD transition. Indeed, the transition to ICD-10-CM is far more challenging than those reported for ICD-10. Here, we substantiate that 36% of ICD-9-CM code mappings are convoluted and have no straightforward correspondence in ICD-10-CM (figures 1 and 2). Indeed, the convoluted motifs are so complex that substantial discontinuities in reporting patient diseases are expected. Furthermore, clinical specialties will be affected unequally, some with a proportion of convoluted motifs as high as 62% (figure 3). It is unlikely that reports containing convoluted motifs could be interpreted accurately within the frameworks developed using ICD-9-CM without significant modifications.
Minimizing disruption in reporting diagnoses post-transition
To create longitudinal reports from data coded in ICD-9-CM and then ICD-10-CM, mapping maps will be required (a ‘crosswalk’). The AMA recommends ‘the direction that you crosswalk the data will depend on how much of the data is in one code set or the other.’22 However, others and our team have shown such unsophisticated mapping is likely to contribute to significant discontinuities in convoluted motifs. For 2014, as 9 months will have been coded in ICD-9-CM before the transition, the AMA states: ‘it will be easier to crosswalk the ICD-10 codes back to ICD-9 in order to compare all of the data together’.22 However, we have shown that the number of convoluted mappings when seeding the mapping from ICD-10-CM increases to 87% (see Results, after table 3). With a quarter of the calendar year 2014 coded in ICD-10-CM, this disruption is likely to be substantial, not to mention that the coding from ICD-10-CM to ICD-9-CM has less than 1% identity motifs and is missing 2964 ICD-9-CM codes as target. With the AMA strategy, 21% of ICD-9-CM codes would contain not a single patient in the last quarter of 2014 (a trend to zero). Of note, Nadkrni and Darer23 have also identified limitations with concept matching software to translate ICD-9 to SNOMED. They recommend the use of ‘query expansion strategies’. Here, we follow such advice and propose a more comprehensive crosswalk involving an educated use of bidirectional mappings and entanglement annotations. For example, reports could be stratified into two parts until the meaning of the new trends is understood: the 60% ICD-9-CM codes associated with non-entangled motifs would map without discontinuity and should be immediately interpretable, the remaining 40% of ICD-9-CM codes require additional work in future studies. For example, it would be useful to provide coding policies that would allow including the parts of ICD-10-CM codes involved in entangled patterns in a step-wise incremental fashion in order to control the discontinuity in disease groups. However, this may go against government or AMA policies. An alternative straightforward approach could be to conduct double coding (ICD-9-CM and ICD-10-CM) for the entangled ICD-9-CM codes and compare motifs in ICD-9-CM and ICD-10-CM in the final reports of the medical system or clinics, such as graph-pruning strategies to subsets offering reasonable coverage.24 However, dual coding is cost-prohibitive as coding to ICD-10-CM codes may require additional patient information that is available in patient charts but unobtainable from the historical ICD-9-CM claims. To mitigate the costs of double billing, we provide web portal tools, files, and charts to assess the risk profile per clinical condition, and to identify minimally affected ICD-9-CM codes (eg, transition motifs of identity or class-to-subclass; tables 2 and 3 and figure 3).
Future studies and limitations
In future work, we plan to report the metrics of particularly intricate ICD-9-CM and ICD-10-CM mapping motifs using additional properties such as centrality. The motifs could have been generated differently. For example, we could have reported the hubs and the bottlenecks of the networks;11 25 however, we believe the insight gathered would not necessarily have translated into action plans for the non-informaticians. We have provided tools to identify the problems; however, identifying strategies to mitigate the complexity of the mapping with practical solutions is likely to be more useful and is one of our next planned steps. This issue is particularly important because studies report that some ICD-10 codes are complex and difficult and frustrating to use.26
Additional analyses are warranted to understand the combination of primary and secondary ICD-9-CM codes to create a patient centered transition to ICD-10-CM coding; for simplicity, this additional analysis was omitted. We plan to provide guidelines to compare the data reported in ICD-10-CM with historical data reported in ICD-9-CM. In future studies, sophisticated semantics leveraging the unified medical language system could provide deeper insight into the transition to ICD-10-CM.15 27
Conclusion
The case study informs us that converting primary encounters with ICD-9-CM to ICD-10-CM codes will be convoluted for 28% of emergency room encounters (0–100% depending on the clinical class), potentially impacting staff (utilization, workflow, division of labor, etc), supply management, and clinical revenue. The top two ICD-9-CM codes with convoluted mapping account for approximately 3.5% of Illinois emergency room visits (figure 4B). Comparable observations can be derived for all clinical departments, and are likely to vary considerably across clinical specialties and individual practices, justifying the requirement for customized mitigating tools. Furthermore, training of personnel and management resources of clinical specialties should focus on the frequently used and complex mapping motifs to ensure a successful transition to ICD-10-CM, which can readily be assessed via web portal tools.
Supplementary Material
Supplementary Material
Footnotes
Contributors: YAL, ADB, JJL, MJ, and IZ vonceived and designed the experiments. ADB, JJL, MDB, and RQL performed the experiments. ADB, JJL, MDB, MJ, VJ, IA, RQL, IL, NB, SBB, TVH, and YAL analyzed and evaluated the data. ADB, JJL, YAL, ADB, NB, and MJ designed and evaluated the web portal. YAL, JJL, MB, NB, SBB, and TVH contributed reagents/materials/analysis tools. YAL, ADB, JJL, MJ, IZ, and VG wrote the paper. YAL conceived and directed the project. YAL had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. ADB, JJL, MDB, and MJ contributed equally
Funding: ADB and YAL are supported in part by the Center for Clinical and Translational Sciences of the University of Illinois (NIH 1UL1RR029879-01, NIH/NCATS UL1TR000050), the Institute for Translational Health Informatics of the University of Illinois at Chicago and the Office of the Vice-President for Health Affairs of the University of Illinois Hospital and Health Science System.
Competing interests: None.
Ethics approval: The case study was approved as a de-identified study exempt of consent by the Institutional Review Board of the University of Illinois at Chicago (IRB protocol #2012-0150).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Comprehensive computed motifs and data are available from the web portal: http://lussierlab.org/transition-to-ICD10CM.
References
- 1.Letter of the American Medical Association (AMA) ICD-10 comment Letter to the Secretary of the US Department of Health and Human Services, dated 2/2/2012. 2012; https://www.ama.assn.org/resources/doc/washington/icd-10-comment-letter-02feb2012.pdf (accessed 29 Apr 2013).
- 2.Farseth PH. Changing diagnosis codes. N Engl J Med 1978;299:1187–90 [DOI] [PubMed] [Google Scholar]
- 3.Wollman J. ICD -10: a master data challenge. Health Manag Technol 2011;32:16, 20–1 [PubMed] [Google Scholar]
- 4.Bhuttar VK. Crosswalk options for legacy systems. Implementing near-term tactical solutions for ICD-10. J AHIMA 2011;82:34–7 [PubMed] [Google Scholar]
- 5.HIMSS ICD-10 Play Book. 2012; https://www.himss.org/asp/topics_icd10playbook.asp (accessed 3 Dec 2012). [Google Scholar]
- 6.Bales ME, Lussier YA, Johnson SB. Topological analysis of large-scale biomedical terminology structures. J Am Med Inform Assoc 2007;14:788–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention ICD-10 Update. 2012; http://www.cdc.gov/nchs/icd/icd10cm.htm#10update (accessed Jan 2012). [PubMed] [Google Scholar]
- 8.CMS Overview ICD-10. 2011; https://www.cms.gov/ICD10/ (accessed 29 Feb 2012). [Google Scholar]
- 9.Li H, Lee Y, Chen JL, et al. Complex-disease networks of trait-associated single-nucleotide polymorphisms (SNPs) unveiled by information theory. J Am Med Inform Assoc 2012;19:295–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hidalgo CA, Blumm N, Barabasi AL, et al. A dynamic network approach for the study of human phenotypes. PLoS Comput Biol 2009;5:e1000353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loscalzo J, Kohane I, Barabasi AL. Human disease classification in the postgenomic era: a complex systems approach to human pathobiology. Mol Syst Biol 2007;3:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pathak J, Johnson TM, Chute CG. Survey of modular ontology techniques and their applications in the biomedical domain. Integr Comput Aided Eng 2009;16:225–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oliver DE, Shahar Y, Shortliffe EH, et al. Representation of change in controlled medical terminologies. Artif Intell Med 1999;15:53–76 [DOI] [PubMed] [Google Scholar]
- 14.Cimino JJ. Desiderata for controlled medical vocabularies in the twenty-first century. Methods Inf Med 1998;37:394–403 [PMC free article] [PubMed] [Google Scholar]
- 15.Wu ST, Liu H, Li D, et al. Unified Medical Language System term occurrences in clinical notes: a large-scale corpus analysis. J Am Med Inform Assoc 2012;19:e149–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cimino JJ, Clayton PD, Hripcsak G, et al. Knowledge-based approaches to the maintenance of a large controlled medical terminology. J Am Med Inform Assoc 1994;1:35–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cimino JJ. In defense of the Desiderata. J Biomed Inform 2006;39:299–306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Januel JM, Luthi JC, Quan H, et al. Improved accuracy of co-morbidity coding over time after the introduction of ICD-10 administrative data. BMC Health Serv Res 2011;11:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Quan H, Li B, Saunders LD, et al. Assessing validity of ICD-9-CM and ICD-10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res 2008;43:1424–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richardson DB. The impact on relative risk estimates of inconsistencies between ICD-9 and ICD-10. Occup Environ Med 2006;63:734–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anderson RN, Minino AM, Hoyert DL, et al. Comparability of cause of death between ICD-9 and ICD-10: preliminary estimates. Natl Vital Stat Rep 2001;49:1–32 [PubMed] [Google Scholar]
- 22.AMA Crosswalking Between ICD-9 and ICD-10. Preparing for the ICD-10 Code Set: October 1, 2014 Compliance Date. Fact Sheet 7. 2012; http://www.ama-assn.org/resources/doc/washington/crosswalking-between-icd-9-and-icd-10.pdf (accessed 5 Apr 2013). [Google Scholar]
- 23.Nadkarni PM, Darer JA. Migrating existing clinical content from ICD-9 to SNOMED. J Am Med Inform Assoc 2010;17:602–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lopez-Garcia P, Boeker M, Illarramendi A, et al. Usability-driven pruning of large ontologies: the case of SNOMED CT. J Am Med Inform Assoc 2012;19:e102–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yu H, Kim PM, Sprecher E, et al. The importance of bottlenecks in protein networks: correlation with gene essentiality and expression dynamics. PLoS Comput Biol 2007;3:e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hernandez-Avila JE, Palacio-Mejia LS, Lara-Esqueda A, et al. Assessing the process of designing and implementing electronic health records in a statewide public health system: the case of Colima, Mexico. J Am Med Inform Assoc 2013;20:238–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Halper M, Morrey CP, Chen Y, et al. Auditing hierarchical cycles to locate other inconsistencies in the UMLS. AMIA Annu Symp Proc 2011;2011:529–36 [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.