Abstract
Transgender patients have particular needs with respect to demographic information and health records; specifically, transgender patients may have a chosen name and gender identity that differs from their current legally designated name and sex. Additionally, sex-specific health information, for example, a man with a cervix or a woman with a prostate, requires special attention in electronic health record (EHR) systems. The World Professional Association for Transgender Health (WPATH) is an international multidisciplinary professional association that publishes recognized standards for the care of transgender and gender variant persons. In September 2011, the WPATH Executive Committee convened an Electronic Medical Records Working Group comprised of both expert clinicians and medical information technology specialists, to make recommendations for developers, vendors, and users of EHR systems with respect to transgender patients. These recommendations and supporting rationale are presented here.
Keywords: Transgender, Electronic, Records, Recommendation, Transsexual
Introduction
The World Professional Association for Transgender Health (WPATH) is an international multidisciplinary professional association that publishes recognized standards for the care of transgender and gender variant persons. WPATH recommends1—in concert with policy statements from the American Medical Association,2 the American Psychiatric Association,3 the American Psychological Association,4 the American College of Obstetricians and Gynecologists,5 and the Center of Excellence for Transgender Health at the University of California, San Francisco6—that the healthcare needs of transgender people should be openly and properly addressed, at the same level of quality and thoroughness as is afforded to any other person. Failure to collect data on and provide systematic inclusion in health delivery systems of transgender persons has negative impacts on health; in order to receive appropriate and meaningful care, it is essential that individual populations be recognized and ‘counted.’7 A 2010 Institute of Medicine (IOM) report on the health of lesbian, gay, bisexual and transgender (LGBT) persons recommends that data on gender identity be collected in electronic health records (EHRs) and that this goal be incorporated into meaningful-use objectives.8
Data are severely lacking with respect to the use of EHR systems in transgender care. A PubMed search conducted on January 7, 2013 using a variety of combinations of the terms ‘transgender,’ ‘electronic,’ and ‘record’ as well as ‘(‘Electronic Health Records’[MeSH])’ AND ‘(‘Transgendered Persons’[MeSH])’ yielded no relevant results. Therefore, in September 2011, the WPATH Executive Committee convened an Electronic Medical Records Working Group, comprised of both expert clinicians and medical information technology specialists, to make recommendations for developers, vendors, and users of EHR systems with respect to transgender patients.
Background
Transgender people experience their gender identity as different from the sex which was assigned to them at birth.1 Transgender people may seek medical care such as hormone therapy or surgery to effect changes in their secondary sex characteristics toward those of the gender with which they identify, as part of a process referred to as gender transition.9 It should be noted that the terms ‘sex’ and ‘gender,’ while often used interchangeably, have specific medical and psychological meanings that may differ from general social—or even legal—usage. ‘Sex’ commonly refers to one's physical sex characteristics (eg, facial hair, body fat distribution, breasts), whereas ‘gender’ represents one's identity and self-image. ‘Gender transition’ may be thought of as the process through which one aligns one's physical sex (through hormones, surgery, etc) with one's gender identity, keeping in mind that not all transgender people will seek a medical transition but may simply focus on a social one; for any given individual, transition may or may not have a specific ‘end point’ and may represent a continued state of flux and exploration that varies by the individual.10
Transgender people may have preferred names and/or pronouns that differ from those listed on government-issued documents or health insurance policies. Furthermore, transgender people may obtain name and/or sex/gender designation changes on identity or other documents (eg, passport, birth certificate, driver's license, financial accounts, etc) at various stages of their transition. In the USA, specific guidelines exist for identity document changes both at the federal level as well as state by state. Failing to be identified by the preferred name and pronoun in a medical setting has been shown to impact patient satisfaction and quality of care for transgender people.11 For example, a patient with an outwardly female appearance may be called by a male name in a crowded medical office reception area, or a patient listed as female who has a male appearance and identity may be referred to with a feminine pronoun by a healthcare provider unfamiliar with the patient's history and preferences. This may negatively impact the patient–provider relationship, as well as put patients at risk for verbal or even physical abuse from other patients in the waiting area. A recent non-peer reviewed report on transgender discrimination showed some 28% of respondents had experienced harassment in a clinic setting and that 2% had been subject to physical abuse.12 It may also lead to the avoidance of care or loss of retention of the patient if they feel that their gender identity is not being acknowledged or respected. A qualitative study of HIV+ low income transgender women of color found that culturally sensitive practices influenced linkage to a variety of healthcare services.13
In addition to concerns about demographic information such as listed versus preferred name, gender, and pronouns, providers require a means to maintain an accurate record of what organs a patient may or may not have; this record cannot be limited or defined by the patient's assigned or apparent sex/gender as entered into the EHR. For example, a patient may have been assigned female at birth, and have transitioned to male through the use of testosterone and surgical removal of the breasts; they may also have obtained a court ordered name and sex or gender change and are registered in the EHR system under a male name and gender. However, since this patient still has a cervix, ovaries, and uterus, health care providers will require the ability to enter pelvic exam findings and gynecologic review of systems, and to order a cervical pap smear within the EHR system. EHR products that restrict or pre-populate an individual encounter with sex-specific history, exam, or ordering templates will prevent this patient's provider from accurately and efficiently documenting their care.
As another example, a patient may have been assigned male at birth and have transitioned to female through the use of estrogen; however, this patient has not yet changed her government-issued identity documents and is currently listed with a male name and sex or gender. The patient has an outwardly female appearance and wishes to be referred to using a feminine name and pronouns. The patient also has breasts as a result of their hormone treatment and will require a breast examination and ordering of a mammogram. An EHR system should guide the administrative and clinical staff to use the patient's chosen name and pronoun, which should serve to improve patient engagement and comfort while improving retention in care. An EHR system should also allow the provider to document a breast examination and order a mammogram—even though the patient remains registered as male.
Basis for recommendations
Given these concerns, the Working Group recommends an individualized approach in the care of each transgender patient, based on a current inventory of organs as well as the patient's own transgender status and sex- or gender-specific history. Drawing on methods first developed by the Center of Excellence for Transgender Health at the University of California, San Francisco, the Working Group adopted a two-step question technique (table 1) to allow the collection and documentation of gender identity information.14 This technique involves first querying the patient's gender identity, followed by a query of the sex assigned at birth; by querying gender identity first, the importance of this parameter from the perspective of a transgender person is emphasized over that of the assigned birth sex. Furthermore, this technique provides more detailed and accurate demographic and historical information, and also increases overall rates of identification of transgender patients as compared to older one-step methods (ie, choices of ‘male,’ ‘female,’ or ‘transgender’). This information could be collected via a face-to-face interaction with clinic staff or a provider; some evidence suggests such information would be more accurately collected via self-registration kiosks or patient portals.15
Table 1.
Two-step method for the collection of sex and gender identity information
| Current gender identity | Sex assigned at birth |
|---|---|
| Male | Male |
| Female | Female |
| Transmale/transman/FTM | Other |
| Transfemale/transwoman/MTF | |
| Genderqueer/gender-non-conforming | |
| Different identity: please state_________________ |
FTM, female to male (ie, female assigned at birth, male-spectrum identity); MTF, male to female (ie, male assigned at birth, female-spectrum identity).
Using a two-step method has been shown to increase the identification of transgender patients in demographics studies as compared to a one-step method. The two-step method was adopted in 2011 by the US Centers for Disease Control and Prevention for use in their Adult Case Report Form as well as their electronic surveillance system, the Enhanced HIV/AIDS Reporting System (EHARS).16 This method has been found to be superior at identifying transgender individuals in comparison to other methods, according to a recently published study.17
Consensus process
The Working Group was composed of WPATH members from a range of disciplines with a variety of backgrounds, including medicine, nursing, pharmacy, social work, policy, law, and public health; all members had experience in EHR use. Members were selected for participation via a written application process overseen by the WPATH Board of Directors. Initial draft recommendations were developed via an informal consensus process among several clinician Working Group members; this consensus process was directed by a physician experienced in EHR use in transgender care as well as in directing informal consensus guideline development, who also holds a degree in computer information systems. All clinicians who contributed to the initial draft guidelines were experienced in both transgender clinical care and EHR use and implementation. These initial draft recommendations were then circulated among the entire Working Group membership for further comment; an updated draft was then sent to the WPATH Board of Directors for final approval.
Recommendations
It is recognized that the overwhelming majority of patients are not transgender, which has led to implementation of a binary male/female oriented system across multiple platforms such as EHR systems, billing and coding systems, and laboratory systems; however, this structure inhibits the collection of accurate medical information, and therefore such systems should be modified.
Preferred name, gender identity, and pronoun preference, as identified by patients, should be included as demographic variables (such as with ethnicity). These would be captured in readily amendable, optional fields that are separate from the patient's state-listed name and sex or gender designation, which may continue to be used for billing purposes in circumstances when the patient has not yet obtained legal change of name and/or sex or gender designation. Note that some patients may identify as ‘genderqueer’ and prefer the use of neither pronoun. While lists of current common gender identities, sex options (table 2), and pronoun options (box 1) are provided, ideally field parameters would be easily amended to reflect changing paradigms and social trends within transgender communities.
Provide a means to maintain an inventory of a patient's medical transition history and current anatomy. An anatomical inventory would allow providers to record into the chart (and/or update as needed) the organs each individual patient has at any given point in time; this inventory would then drive any individualized auto-population of history and physical exam templates. This inventory should be uncoupled from the patient's recorded gender identity, assigned sex, or preferred pronouns. A list of recommended organs for inventory in transgender patients appears in box 2, and commonly sought treatments and procedures which may not be listed in current systems but should be included as selectable items in the medical or surgical history, appear in box 3. The following non-exhaustive list of procedures are not transgender-specific procedures and are omitted from box 3 as they are already listed in existing systems: hysterectomy, oophorectomy, vaginectomy, orchiectomy, breast augmentation. These procedures, however, also should also be un-coupled from any gender-coded template so that an individual coded as male who has had a hysterectomy, for example, could have that history documented. In addition, sex-specific organ procedures and diagnoses relating to these organs should be un-coupled, so that (as an example) a prostatic ultrasound may be ordered on a patient registered as female, or a cervical pap smear ordered on a patient registered as male. Such practices would allow enhanced decision support for transgender-specific care, such as medication interactions, organ- and sex-specific preventive health alerts, or accommodations for sex-specific laboratory normal value ranges. For example, a patient with a female birth sex and male gender identity, currently registered as a female, who is taking testosterone, may have a hemoglobin of 17 g/dl flagged as ‘high’ by the interfacing laboratory system. A local flag driven by the patient's birth sex, gender identity, and current testosterone prescription could alert clinicians to reconsider this ‘high’ flag and review laboratory male reference ranges.
The system should allow a smooth transition from one listed name, anatomical inventory, and/or sex to another, without affecting the integrity of the remainder of the patient's record. It should be noted that, in some cases, changes in name and sex or gender designation of record will come at different times, and that in some jurisdictions official recognition of a change of sex or gender designation is not possible.
A system should exist to notify providers and clinic staff of a patient's preferred name and/or pronoun (if either or both of these differ from the current legal documented name/sex). Systems should include an easily recognized notification or alert flag which appears at a time most consistent with the end-user's workflow (figure 1).
Table 2.
Suggested optional* gender identity and sex data collection fields
| Gender identity options | Sex assigned at birth options |
|---|---|
| Male | Male |
| Female | Female |
| Transmale/transman/FTM | Other |
| Transfemale/transwoman/MTF | |
| Genderqueer/gender-non-conforming | |
| Different identity: please state_________________ |
*Data should be able to be collected for any patient (ie, transgender/gender-non-conforming persons) but would not be required fields for the majority of (non-transgender) patients whose birth and current listed sex as well as gender identity are identical. These data could be housed in a special supplemental demographics section or in the medical or social history sections of the chart. Additionally, the patient's ‘current listed sex’ (ie, the sex/gender as they are listed on their insurance documents, current state-issued identity documentation, etc) would be collected and stored in the primary sex/gender demographics field for billing purposes.
FTM, female to male (ie, female assigned at birth, male-spectrum identity); MTF, male to female (ie, male assigned at birth, female-spectrum identity).
Box 1. Suggested optional pronoun data collection fields.
▸ Masculine pronouns
▸ Feminine pronouns
▸ Neutral pronouns
▸ No pronouns
▸ Something else (please specify):
Box 2. Organs for inventory.
▸ Penis
▸ Testes
▸ Prostate
▸ Breasts
▸ Vagina
▸ Cervix
▸ Uterus
▸ Ovaries
Box 3. Common treatments and procedures.
▸ Cross-sex hormone therapy, current user
▸ Cross-sex hormone therapy, past user
▸ Vaginoplasty, penile inversion
▸ Vaginoplasty, colon graft
▸ Phalloplasty, abdominal flap
▸ Phalloplasty, free flap
▸ Metoidioplasty
▸ Scrotoplasty
▸ Urethroplasty
▸ Scalp advancement
▸ Forehead reconstruction
▸ Reduction thyrochondroplasty
▸ Laryngeal feminization surgery
▸ Soft tissue filler injections
▸ Bilateral total reduction mammoplasty
▸ Voice surgery
▸ Other unlisted surgical procedure
Figure 1.
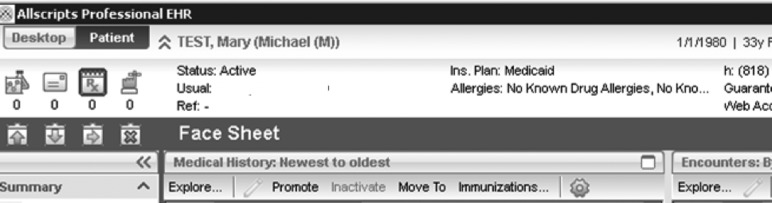
Implementation in Allscripts Professional EHR using the ‘Nickname’ field and a coding system. The preferred name (Michael) is seen in parentheses after the patient's legal name (Mary) in the heading of every screen by every viewer. The preferred pronoun (‘M’ for male) is indicated by a second-order parenthesized letter after the preferred name. Clinic staff are trained in this coding mechanism. EHR, electronic health record.
Conclusion
As the care of transgender patients moves into the mainstream, the medical informatics field will be asked to respond to the unique needs of this demographic through the implementation of more accurate and appropriate data collection methods in a range of products and systems. It is hoped that these user-driven recommendations will better inform health information technology research and EHR vendors on the specific needs of transgender patients in this context. Future research should aim to explore current practices among both clinicians and vendors; ultimately this information would be used to drive developer implementation of feasible models which satisfy the recommendations presented here.
These recommendations of the Working Group have been reviewed and endorsed by the WPATH Board of Directors.
Footnotes
Correction notice: This article has been corrected since it was first published online first. The article is now open access.
Acknowledgements: The authors wish to thank Shane Snowdon, MA for her assistance with and contributions to this project.
Collaborators: Members of the WPATH EMR Working Group: Madeline B Deutsch, MD (Co-Chair); JoAnne Keatley, MSW (Co-Chair); Jamison Green, PhD (WPATH Board Liaison); Rebecca Allison, MD; Oliver Blumer, DC; Stephen Brown, MD; Mary Kay Cody, MSN, RN-BC; Kristopher Fennie, PhD, MPH; Alexandra M Hall, MD; Jennifer Hastings, MD; Gal S Mayer, MD; Gwen Moscoe, Pharm D; Rachael St Claire, Psy D; Moonhawk River Stone, MS, LMHC; André Wilson, MS; Carolyn Wolf-Gould, MD.
Contributors: MBD, GM, JH, and AMH wrote the Recommendations section based on Working Group recommendations. MBD, JG, and JK then edited this section and wrote the rest of the article. MBD takes responsibility for the manuscript as a whole. All six authors participated in the original consensus process (facilitated by MBD) and have reviewed and approve the final version of the manuscript.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Contributor Information
Collaborators: Madeline B Deutsch, JoAnne Keatley, Jamison Green, Rebecca Allison, Oliver Blumer, Stephen Brown, Mary Kay Cody, Kristopher Fennie, Alexandra M Hall, Jennifer Hastings, Gal S Mayer, Gwen Moscoe, Rachael St Claire, Moonhawk River Stone, André Wilson, and Carolyn Wolf-Gould
References
- 1.Coleman E, Bockting W, Botzer M, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgenderism 2012;13:165–232 [Google Scholar]
- 2.American Medical Association, GLBT Advisory Committee H-185.950 Removing Barriers to Care for Transgender Patients. 2008. http://www.ama-assn.org/ama/pub/about-ama/our-people/member-groups-sections/glbt-advisory-committee/ama-policy-regarding-sexual-orientation.shtml (accessed 22 Apr 2013).
- 3.American Psychiatric Association Position Statement on Access to Care for Transgender and Gender Variant Individuals. 2012. http://www.psychiatry.org/File_Library/Advocacy_and_Newsroom/Position_Statements/ps2012_TransgenderCare.pdf (accessed 22 Apr 2013).
- 4.American Psychological Association APA Policy Statement: Transgender, Gender Identity & Expression Non-Discrimination. 2008. http://www.apa.org/about/governance/council/policy/transgender.aspx (accessed 22 Apr 2013).
- 5.Committee on Health Care for Underserved Women. Committee opinion no. 512: health care for transgender individuals. Obstet Gynecol 2011;118:1454–8 [DOI] [PubMed] [Google Scholar]
- 6.University of California, San Francisco, Center of Excellence for Transgender Health Primary Care Protocols for Transgender Patient Care. 2011. http://www.transhealth.ucsf.edu/trans?page=protocol-patients (accessed 22 Apr 2013).
- 7.Bauer GR, Hammond R, Travers R, et al. “I don't think this is theoretical; this is our lives”: how erasure impacts health care for transgender people. J Assoc Nurses AIDS Care 2009;20:348–61 [DOI] [PubMed] [Google Scholar]
- 8.Institate of Medicine of the National Academies. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding 2011. http://www.iom.edu/Reports/2011/The-Health-of-Lesbian-Gay-Bisexual-and-Transgender-People.aspx (accessed 13 Jan 2013). [PubMed]
- 9.Williamson C. Providing care to transgender persons: a clinical approach to primary care, hormones, and HIV management J Assoc Nurses AIDS Care 2010;21:221–9 [DOI] [PubMed] [Google Scholar]
- 10.Gagné P, Tewksbury R, McGaughey D. Coming out and crossing over identity formation and proclamation in a transgender community. Gend Soc 1997;11:478–508 [Google Scholar]
- 11.Mizock L, Lewis TK. Trauma in transgender populations: risk, resilience, and clinical care. J Emotional Abuse 2008;8:335–54 [Google Scholar]
- 12.National Gay and Lesbian Task Force Injustice; at Every Turn: A Report of the National Transgender Discrimination Survey. 2011. http://www.thetaskforce.org/reports_and_research/ntds8b (accessed 13 Jan 2013).
- 13.Melendez RM, Pinto RM. HIV prevention and primary care for transgender women in a community-based clinic. J Assoc Nurses AIDS Care 2009;20:387–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Center of Excellence for Transgender Health. How to Accurately Capture Data on Trans Clients. 2007. http://www.transhealth.ucsf.edu/trans?page=lib-trans-count (accessed Oct 2012).
- 15.Mackenzie SLC, Kurth AE, Spielberg F, et al. Patient and staff perspectives on the use of a computer counseling tool for HIV and sexually transmitted infection risk reduction. J Adolesc Health 2007;40:572–e9–16. [DOI] [PubMed] [Google Scholar]
- 16.CDC National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Division of HIV/AIDS Prevention HIV Infection among Transgender People. 2011. http://www.cdc.gov/hiv/transgender/pdf/transgender.pdf (accessed Oct 2012).
- 17.Tate CC, Ledbetter JN, Youssef CP. A Two-question method for assessing gender categories in the social and medical sciences. J Sex Res 2012;18:1–10 [DOI] [PubMed] [Google Scholar]


