Abstract
The integration of electronic health records (EHRs) across care settings including residential care facilities (RCFs) promises to reduce medical errors and improve coordination of services. Using data from the 2010 National Survey of Residential Care Facilities (n=2302), this study examines the association between facility structural characteristics and the use of EHRs in RCFs. Findings indicate that in 2010, only 3% of RCFs nationwide were using an EHR. However, 55% of RCFs reported using a computerized system for one or more (but not all) of the functionalities defined by a basic EHR. Ownership, chain membership, staffing levels, and facility size were significantly associated with the use of one or more core EHR functionalities. These findings suggest that facility characteristics may play an important role in the adoption of EHRs in RCFs.
Keywords: electronic health record, residential care facilities, health information technology, long term care
Introduction
With the passage of the 2009 Federal Health Information Technology for Economic and Clinical Health Act, there have been unprecedented efforts by private and public sector leaders to improve the safety and delivery of healthcare through the adoption of electronic health records (EHRs).1 While a growing body of literature provides detailed accounts on how EHRs impact quality of care in clinical settings,2–5 EHR adoption remains largely inattentive to the needs of long-term services and support (LTSS) providers.6 Given the vulnerability of older adults who utilize LTSS to adverse health outcomes during care transitions7 and new Medicare penalties for high rehospitalization rates within 30-days of discharge,8 the opportunities for promoting EHR utilization across the LTSS system should be greater than ever.6
Across the LTSS system, EHRs have the potential to improve administrative and operations productivity9 and improve the quality of care by allowing for interoperability among providers during periods of care transitions. However, LTSS providers lag in EHR adoption compared to other sectors of healthcare.10 While several studies have examined the factors affecting EHR implementation in LTSS settings including nursing home (NH), home health, and hospice agencies,11–14 there has been no widespread evaluation of this technology among community, residential care facilities (RCFs). Thus, the ability to provide a comprehensive understanding of EHR utilization across the LTSS system has been hampered by limited information about EHR adoption within RCFs.
In the past two decades, RCFs—such as assisted living communities—have emerged as an important alternative to NHs for frail older Americans.15 Driven largely by consumer preference and without the influence of government financing or regulation, RCFs have developed to meet the needs of approximately one million elders.16 Nationally, these community-based living environments provide housing and tailor personal care services to individuals who cannot live independently but do not require the skilled care provided by NHs. Although there is heterogeneity in the services provided, amount of care offered, and regulatory standards governing RCFs, these facilities serve an increasingly disabled resident population.17 18 Moreover, as Medicaid expenditures for home- and community-based services increase, RCFs are frequently used as an alternative to NH placement.19 However, since RCFs are not licensed healthcare facilities, residents are vulnerable to potentially avoidable hospitalizations20 and errors with medication mismanagement.21 22
Consequently, EHR integration into RCFs has the potential to improve residents’ health outcomes and reduce unnecessary expenditures. However, data on EHR use in RCFs is limited. A recent pilot study examining EHR utilization in RCFs found that EHR use was correlated with larger, for-profit facilities that employed a higher number of direct care staff,23 but these findings were based on a small unrepresentative sample. Other than descriptive results, EHR use in RCFs at the national level has yet to be examined. Responding to the current knowledge gap, this study examines the association between facility characteristics and the use of EHRs in RCFs.
Methods
Source of the data
Facility level data were drawn from the 2010 National Survey of Residential Care Facilities (NSRCF), a nationally-representative, probability sample survey of US RCFs.24 To be eligible for the NSRCF, RCFs must be licensed, registered, or otherwise regulated by the state; have four or more licensed beds with at least one resident living in their facility; and provide 24-h supervision and personal care with at least two meals a day to the residents.25 Facilities licensed to serve the mentally ill or developmentally disabled populations exclusively were excluded from the NSRCF.
The 2010 NSRCF used a stratified two-stage probability design and was conducted between March and November 2010 by the National Center for Health Statistics.25 The first stage was the selection of RCFs from a sampling frame of 39 635 facilities representing a total of 1 073 043 beds.25 The second stage was the selection of residents.25 For the 2010 NSRCF, 3605 RCFs were sampled with probability proportional to facility size. On-site interviews were completed on 2302 facilities for a weighted response rate of 81%.25
Measures
Outcome variable
Although the Institute of Medicine has identified core functions of an EHR,26 there is no consensus on what functionalities constitute the essential elements of an EHR for LTSS providers. Recognizing that LTSS providers lag in EHR adoption compared to other sectors of healthcare and that relatively few RCFs might have a fully functional EHR, we adopted the basic definition of an EHR.2 27 This definition recognizes a basic EHR as having the capabilities to record resident demographics, resident problem lists, and medications taken by the residents; to order prescriptions and laboratory tests; and to view laboratory and imaging results.2 27
Predictor variables
The Donabedian Structure Process Outcome (SPO) Model28 posits that quality is composed of three interacting elements: structure (characteristics of the physical and organizational environment), process (the technical process of care), and outcomes. Using the SPO model, we hypothesized that RCF structural characteristics will influence the decision to adopt an EHR.
Guided by other analyses using the SPO model,29–32 we included size, chain membership, ownership, Medicaid participation, occupancy, facility location, and staffing levels as structural characteristics. Facility size corresponds to the number of beds in the facility and was categorized as small (4–10 beds), medium (11–24 beds), large (24–100 beds), or extra-large (100 or more beds). Chain membership was defined as whether the facility was owned by a chain, group, or multi-facility system. Facility ownership was dichotomized as for-profit and non-profit/government owned. Medicaid participation was affirmed based on whether the facility was certified to participate in Medicaid. In RCFs, Medicaid participation is of growing importance to researchers since the degree to which RCFs substitute for NHs is largely dependent on the extent to which Medicaid will pay for RCFs and the extent that research demonstrates differences in care practices and quality outcomes between the two settings.33 Moreover, it is well documented that NHs which have a higher percentage of Medicaid funded residents are less likely to have processes of care that result in better outcomes of care.32 34 Occupancy rate was defined as the total number of residents divided by the total number of beds in the facility and converted to a percentage. The NSRCF defined response categories for occupancy rate as 0–6.5%, 6.51–80%, 80.1–95.0%, or 95.1–100%. Staffing measures included direct care hours per patient day (HPPD) of registered nurses (RN), licensed practical nurses (LPN), and personal care aides (PCA) and were categorized based on the NSRCF response categories. Facility location was based on the metropolitan statistical area (MSA) and dichotomized into MSA and non-MSA facilities. MSAs are used by the US Census Bureau to represent geographical regions with a high population density. Resident demographics were described by the percentage of female and Caucasian residents residing in the facility.
Statistical analysis
Descriptive statistics were calculated separately for EHR users and non-users.
Logistic regression (n=2,302) was used to model the factors associated with the use of a basic EHR (model 1) and the use of one or more core EHR functionalities (model 2). The regression models were weighted to account for the complex, sampling design of the NSRCF. Statistical significance was assessed with a two-tailed α of 0.05. All analyses were performed using SAS V.9.2.
Results
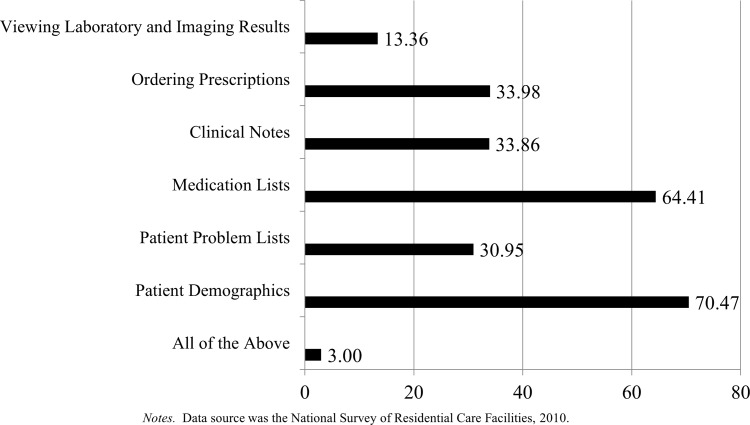
In 2010, approximately 3% of RCFs reported using an EHR. More than 55% of RCFs reported using a computerized system for one or more (but not all) of the functionalities defined by a basic EHR (figure 1).
Figure 1.
Core functionalities in facilities using EHR components.
A bivariate comparison between EHR users (n=69) and non-users (n=2233) suggested that facilities using the technology were larger, non-profit facilities that participated in Medicaid and provided more than 0.5 HPPD of direct care from RNs and LPNs and three or more HPPD of care via PCAs than non-users (table 1). EHR users also differed from non-users based on occupancy rate, with occupancy rates in facilities using EHRs varying between 65.01–80% and 95.1–100% occupancy.
Table 1.
Residential care facilities characteristics by electronic health record (EHR) strata
| Descriptive results | ||||
|---|---|---|---|---|
| Total sample (N=2302) | Comparison by strata | |||
| EHR users (n=69) | EHR non-users (n=2233) | χ2 or t | ||
| Organizational size | 31.4*** | |||
| Small (4–10 beds) | 49.6 | 48.8 | 49.6 | |
| Medium (11–24 beds) | 15.9 | 21.6 | 15.7 | |
| Large (24–100 beds) | 27.8 | 22.7 | 27.9 | |
| Extra-large (100+ beds) | 6.7 | 6.9 | 6.7 | |
| Chain: chain member | 37.7 | 40.0 | 37.6 | 2.4 |
| Ownership: non-profit | 17.6 | 20.3 | 17.5 | 4.9* |
| Medicaid participation | 49.7 | 63.1 | 49.3 | 75.7*** |
| Facility location: urban | 75.1 | 75.4 | 75.1 | 0.14 |
| Occupancy rate | 114.9*** | |||
| 1.0–65% occupancy | 21.6 | 10.3 | 21.9 | |
| 65.01–80% occupancy | 25.5 | 36.6 | 25.2 | |
| 80.1–95% occupancy | 27.7 | 25.6 | 27.8 | |
| 95.1–100% occupancy | 25.2 | 27.5 | 25.1 | |
| Staffing measures | ||||
| HPPD RN | 84.96*** | |||
| 0 HPPD | 61.3 | 48.8 | 61.7 | |
| <0.125 | 20.9 | 25.0 | 20.7 | |
| 0.125–0.249 HPPD | 8.5 | 14.1 | 8.3 | |
| >0.5 | 9.1 | 12.1 | 8.9 | |
| HPPD LPN | 21.51** | |||
| 0 HPPD | 66.5 | 67.5 | 66.5 | |
| <0.125 | 10.6 | 9.7 | 10.7 | |
| 0.125–0.249 HPPD | 8.8 | 5.8 | 8.9 | |
| >0.5 | 13.9 | 17.1 | 13.8 | |
| HPPD PCA | 49.9*** | |||
| 0 HPPD | 5.2 | 2.5 | 5.3 | |
| <1 | 16 | 12.6 | 15.9 | |
| 1–1.999 HPPD | 26.4 | 25.2 | 26.5 | |
| 2–2.999 HPPD | 18.5 | 13.8 | 18.6 | |
| 3 or more HPPD | 33.6 | 41.0 | 33.3 | |
| Resident demographics | ||||
| Percent female (mean, SD) | (68.2, 92.1) | (69.4, 67.8) | (66.9, 110.6) | 0.41 |
| Percent Caucasian (mean, SD) | (88.5, 79.6) | (87.7, 96.2) | (86.4, 91.2) | 0.33 |
Data source was the National Survey of Residential Care Facilities, 2010.
*p<0.05, **p<0.01, ***p<0.001.
HPPD, hours per patient day; LPN, licensed practical nurse; PCA, personal care aide; RN, registered nurse.
Logistic regression results (table 2) indicated that facilities using a basic EHR were likely to be non-profit facilities (OR 1.10, 95% CI 1.58 to 2.11) and participate in Medicaid (OR 1.78, 95% CI 1.03 to 3.07). Facilities using one or more of the core EHR functionalities were likely to be larger (OR 2.14, 95% CI 1.58 to 2.88), non-profit facilities (OR 2.4, 95% CI 1.56 to 3.07) that were members of a chain (OR 1.53, 95% CI 1.26 to 1.87). Facilities not providing care via LPNs (OR 0.62, 95% CI 0.46 to 0.81) were 40% less likely to use this technology. Similarly, those facilities not providing care via PCAs (OR 0.35, 95% CI 0.20 to 0.61) were 65% less likely to use one or more of the core EHR functionalities compared to those facilities with higher staffing levels. Other structural characteristics were not associated with the use this technology.
Table 2.
Logistic regression results predicting the use of electronic health records (EHRs)
| Predictors | OR (95% CI) | |
|---|---|---|
| Full EHR | Any EHR component | |
| Organizational size | ||
| Small (4–10 beds) | Reference | Reference |
| Medium (11–24 beds) | 1.34 (0.65 to 2.75) | 1.41 (1.09 to 1.83) |
| Large (24–100 beds) | 1.02 (0.42 to 2.49) | 2.14 (1.59 to 2.89) |
| Extra-large (100+ beds) | 1.45 (1.04 to 5.34) | 4.36 (2.72 to 6.99) |
| Chain: chain member | 0.98 (0.57 to 1.68) | 1.53 (1.26 to 1.87) |
| Ownership: non-profit | 1.10 (1.58 to 2.11) | 2.41 (1.89 to 3.07) |
| Medicaid participation | 1.78 (1.03 to 3.07) | 1.02 (0.84 to 1.24) |
| Facility location: urban | 1.04 (0.57 to 1.91) | 0.9 (0.73 to 1.12) |
| Occupancy rate | ||
| 1.0–65% occupancy | 0.67 (0.28 to 1.58) | 0.90 (0.67 to 1.21) |
| 65.01–80% occupancy | 1.43 (0.73 to 2.83) | 0.94 (0.71 to 1.24) |
| 80.1–95% occupancy | 0.93 (0.43 to 1.99) | 0.96 (0.74 to 1.25) |
| 95.1–100% occupancy | Reference | Reference |
| Staffing measures | ||
| HPPD RN | ||
| 0 HPPD | 1.11 (0.45 to 2.72) | 0.84 (0.61 to 1.16) |
| <0.125 | 1.55 (0.59 to 4.02) | 1.22 (0.84 to 1.76) |
| 0.125–0.249 HPPD | 1.91 (0.63 to 5.81) | 1.13 (0.73 to 1.73) |
| >0.5 | Reference | Reference |
| HPPD LPN | ||
| 0 HPPD | 0.64 (0.32 to 1.29) | 0.62 (0.46 to 0.82) |
| <0.125 | 0.50 (0.18 to 1.43) | 0.76 (0.51 to 1.06) |
| 0.125–0.249 HPPD | 0.46 (1.03 to 3.07) | 0.76 (0.52 to 1.13) |
| >0.5 | Reference | Reference |
| HPPD PCA | ||
| 0 HPPD | 0.3 (0.04 to 2.29) | 0.35 (0.20 to 0.61) |
| <1 | 0.51 (0.19 to 1.31) | 0.74 (0.54 to 1.00) |
| 1–1.999 HPPD | 0.53 (0.26 to 1.08) | 0.9 (0.89 to 1.18) |
| 2–2.999 HPPD | 0.56 (0.25 to 1.21) | 0.89 (0.67 to 1.18) |
| 3 or more HPPD | Reference | Reference |
| Resident demographics | ||
| Per cent female | 1.01 (0.99 to 1.01) | 1.00 (0.99 to 1.01) |
| Per cent Caucasian | 1.00 (0.98 to 1.01) | 1.00 (0.99 to 1.01) |
Data source was the National Survey of Residential Care Facilities, 2010.
HPPD, hours per patient day; LPN, licensed practical nurse; PCA, personal care aide; RN, registered nurse.
Discussion
With 3% of RCFs nationwide using EHRs, these findings provide evidence that the majority of RCFs are not using the technology. However, many functionalities that underlie electronic systems were widely implemented and it appears that the use of EHRs in RCFs is influenced by facility characteristics including size, profit status, chain membership, staffing, and Medicaid participation. Findings suggest that facilities using a basic EHR were non-profit facilities that also participated in Medicaid; whereas those facilities using one or more of the core functional components were more likely to be larger, non-profit facilities that were members of a chain. These associations are largely consistent with trends in other care settings11 13 14 and indicate that RCFs, like their NH and acute care counterparts, may require centralized data management.
Although RCFs lag behind other LTSS providers in the adoption of health information technology, it is possible that since 55% of RCFs used at least one of the core EHR functionalities, this setting may be in the early stages of transitioning from paper communications to EHRs. Additionally, considering the initial financial investment required in adopting an EHR, many facilities might implement the technology in stages with its use best modeled by a continuum of applicability instead of the current dichotomy. Moreover, questions remains as to whether the adoption of an EHR or specific functional components would result in measurable improvements in efficiency.
Because RCFs are considered a cost-effective alternative to NHs for some older adults, it is critical to understand how EHRs affect healthcare utilization. At a minimum, RCFs are expected to provide safe living accommodations, with provisions for assistance with activities of daily living and coordination of health-related services to its residents.35 Since RCFs were designed as social environments and not medical institutions, it appears that EHR implementation within this setting is determined based on resident care needs. For example, with 94% of RCF residents taking at least one medication and the high prevalence of cardiovascular and psychotropic drugs,36 medication safety is of considerable importance within RCFs. This concern is reflected in the high implementation rates of EHRs for medication management compared to other core functionalities. Additionally, since RCFs are not medical facilities, common clinical tasks such as viewing or recording laboratory and imaging results are used to a lesser extent within this setting.
The study design, including its large sample and generalizability, are strengths of the study. However, limitations must be considered. First, the NSRCF is cross-sectional and provides no information about the duration of EHR use. Second, several variables used in this study including facility size, occupancy rate, and staffing are constrained by the NSRCF categorical definitions and cannot be examined as continuous variables. However, the NSRCF provides nationally representative data on EHR use in RCFs, making this data source extremely valuable for studying the current utilization of EHRs in this setting. Third, this study only examined the broad use of EHRs in RCFs and is unable to report the impact EHRs have on resident outcomes.
Considering the growing number of elders who require care coordination across multiple settings, EHRs have the potential to improve the delivery and quality of care when fully integrated across acute and LTSS settings. Although EHR adoption may serve as a valuable tool as the industry moves towards more patient-centered care, the benefits of such a system cannot come to fruition without first implementing a fully functional EHR across the LTSS spectrum.
Acknowledgments
The authors would like to thank the reviewers for their comments on earlier versions of this manuscript.
Footnotes
Contributors: All authors contributed to the design and conduct of the study, as well as the preparation of the manuscript.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Individuals interested in the sample and associated analyses may contact the corresponding author to obtain such information.
References
- 1.Buntin MB, Burke MF, Hoaglin MC, et al. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff (Millwood) 2011;30:464–71 [DOI] [PubMed] [Google Scholar]
- 2.Jha AK, DesRoches CM, Campbell EG, et al. Use of electronic health records in U.S. hospitals. N Engl J Med 2009;360:1628–38 [DOI] [PubMed] [Google Scholar]
- 3.Shekelle P, Morton SC, Keeler EB. Costs and benefits of health information technology. Rockville, MD: Agency for Healthcare Research and Quality, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu S, Chaudhry B, Wang J, et al. Systematic review: Impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006;144:742–52 [DOI] [PubMed] [Google Scholar]
- 5.Linder JA, Ma J, Bates DW, et al. Electronic health records use and the quality of ambulatory care in the United States. Arch Intern Med 2007;167:1400–5 [DOI] [PubMed] [Google Scholar]
- 6.LTC HIT Summit A road map for health IT in long term care, 2008. http://library.ahima.org/xpedio/groups/public/documents/ahima/bok1_047484.pdf [Google Scholar]
- 7.Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc 2003;51:549–55 [DOI] [PubMed] [Google Scholar]
- 8.Medpac Reducing the hospitalization rate for Medicare beneficiaries receiving home health care, 2012. http://www.medpac.gov/transcripts/HomehealthhospitalizationNov2012.pdf [Google Scholar]
- 9.Hedstrom K. The values of IT in elderly care. Information Technology & People. 2007;20:72–84 [Google Scholar]
- 10.Kaushal R, Bates DW, Poon EG, et al. Functional gaps in attaining a national health information network. Health Aff (Millwood) 2005;24:1281–9 [DOI] [PubMed] [Google Scholar]
- 11.Chan S. Factors associated with the use of electronic information systems for drug dispensing and medication administration records in nursing homes. J Am Med Directors Assoc 2008;9:414–21 [DOI] [PubMed] [Google Scholar]
- 12.Davis JA, Brannon D, Whitman MV. Organizational factors association with the use of information systems in nursing homes. Health Care Manage Rev 2009;34:141–51 [DOI] [PubMed] [Google Scholar]
- 13.Resnick HE, Alwan M. Use of health information technology in home health and hospice agencies: United States, 2007. J Am Med Inform Assoc 2010;17:389–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Resnick HE, Manard BB, Stone RI, et al. Use of electronic information systems in nursing homes: United States, 2004. J Am Med Inform Assoc 2009;16:179–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Golant SM. The future of assisted living residences. A response to its uncertainty. In: Golant SM, Hyde J. The assisted living residences. A vision for the future. Baltimore, MD: John Hopkins Press, 2008:3–45 [Google Scholar]
- 16.Mollica R, Sims-Kastelein K, O'Keefe J. Residential care and assisted living compendium: 2007. In: Services USDoHaH, ed. Washington, DC: National Academy for State Health Policy, 2008. http://aspe.hhs.gov/daltcp/reports/2007/07alcom.htm [Google Scholar]
- 17.Spillman BC, Liu K, McGillard C. Trends in residential long-term care: use of nursing homes and assisted living and characteristics of facilities and residents. In: Services USDoHaH, ed. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, 2002 [Google Scholar]
- 18.Stevenson DG, Grabowski DC. Sizing up the market for assisted living. Health Aff (Millwood) 2010;29:35–43 [DOI] [PubMed] [Google Scholar]
- 19.U.S. Government Accountability Office Medicaid: States’ plans to pursue new and revised options for home- and community-based services. 2012. http://www.gao.gov/assets/600/591560.pdf [Google Scholar]
- 20.Becker M, Boaz T, Andel R, et al. Predictors of avoidable hospitalizations among assisted living residents. J Am Med Directors Assoc 2011 [DOI] [PubMed] [Google Scholar]
- 21.Briesacher B, Limcangco R, Simoni-Wastila L, et al. Evaluation of nationally mandated drug use reviews to improve patient safety in nursing homes: a natural experiment. J Am Geriatr Soc 2005;53:991–6 [DOI] [PubMed] [Google Scholar]
- 22.Sloane PD, Gruber-Baldini AL, Zimmerman S, et al. Medication undertreatment in assisted living settings. Arch Intern Med 2004;164:2031–7 [DOI] [PubMed] [Google Scholar]
- 23.Holup AA, Dobbs D, Temple A, et al. Going digital: the adoption of electronic health records in assisted living facilities. J Appl Gerontol 2012. Published Online First 1 Aug 2012. doi:10.1177/0733464812454009 [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention National survey of residential care facilities. Washington DC: CDC/National Center for Health Statistics, 2010 [Google Scholar]
- 25.Moss AJ, Harris-Kojetin LD, Sengupta M. Design and operations of the 2010 National Survey of Residential Care Facilities. In: Statistics NCfH, ed 2011 [PubMed] [Google Scholar]
- 26.Institute of Medicine Key capabilities of an electronic health record system: Letter report, Washington DC: The National Academies Press, 2003. http://www.iom.edu/Reports/2003/Key-Capabilities-of-an-Electronic-Health-Record-System.aspx [PubMed] [Google Scholar]
- 27.DesRoches CM, Campbell EG, Rao SR, et al. Electronic health records in ambulatory care—a national survey of physicians. N Engl J Med 2008;359:50–60 [DOI] [PubMed] [Google Scholar]
- 28.Donabedian A. Evaluating the quality of medical care. Milbank Q 1996;44:166–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Castle NG. Deficiency citations for physical restraint use in nursing homes. J Gerontol Ser B: Psychol Sci Social Sci 2000;55B:S33–40 [DOI] [PubMed] [Google Scholar]
- 30.Krok J, Dobbs D, Hyer K, et al. Nurse managers’ perspectives of structural and process characteristics related to residents’ advance directives in nursing homes. Appl Nurs Res 2011;24:e45–50 [DOI] [PubMed] [Google Scholar]
- 31.Luo H, Fang X, Liao Y, et al. Associations of special care units and outcomes of residents with dementia: 2004 national nursing home survey. The Gerontologist 2010;50:509–18 [DOI] [PubMed] [Google Scholar]
- 32.Castle NG, Ferguson JC. What is nursing home quality and how is it measured? The Gerontologist 2010;50:426–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zimmerman D, Sloane PD, Eckert JK. Assisted living: needs, policies, and practices in residential care for the elderly. Baltimore, MD: The John Hopkins University Press, 2001 [Google Scholar]
- 34.Kang-Yi CD, Mandell DS, Mui CA, et al. Interaction effect of Medicaid census and nursing home characteristics on quality of psychosocial care for residents. Health Care Manage Rev 2001;36:47–57 [DOI] [PubMed] [Google Scholar]
- 35.The Scan Foundation Residential care facilities for the elderly, Technical Brief, March 2001, No. 7, Long Beach, CA, 2011. http://www.thescanfoundation.org/residential-care-facilities-elderly [Google Scholar]
- 36.Williams BR, Nichol MB, Lowe B, et al. Medication use in residential care facilities for the elderly. Ann Pharmacother 1999;33:149–55 [DOI] [PubMed] [Google Scholar]