Abstract
Objectives This study examines associations between maternal depressive symptoms and macro- and micro-level aspects of mothers’ communication about their children’s cancer. Methods Mothers reported depressive symptoms after diagnosis or relapse (child mean age = 10.4 years; 53% male). Mother–child dyads (N = 94) were subsequently observed discussing the child’s cancer and maternal communication was coded. Results Macro-level indicators (positive and negative communication) were associated with certain micro-level indicators of communication (topic maintenance, reflections, reframes, and imperatives). Higher depressive symptoms predicted lower positive communication and higher negative communication. Maternal reflections and imperatives predicted positive communication, and topic maintenance and reframes predicted negative communication, beyond child age, family income, and depressive symptoms. Conclusions Findings suggest concrete targets for improving communication in families after diagnosis or relapse.
Keywords: cancer and oncology, mother–child communication
More than 12,000 children are diagnosed with cancer each year in the United States, and it is the second leading cause of death in children (Jemal, Siegel, Xu, & Ward, 2010). Although survival rates for these children continue to increase, children with cancer and their parents are faced with numerous challenges at diagnosis and throughout treatment (Rodriguez et al., 2012; Wijnberg-Williams, Kamps, Klip, & Hoekstra-Weebers, 2006). One of the greatest challenges facing parents is how to talk with their child about the disease, treatments, side effects, and prognosis. Research on other illnesses, such as type 1 diabetes (Jaser & Grey, 2010), asthma (Lim, Wood, Miller, & Simmens, 2011), and cystic fibrosis (DeLambo, Ievers-Landis, Drotar, & Quittner, 2004), indicates that positive parental communication is linked to children’s positive psychosocial adjustment and disease management, including lower rates of emotional and behavioral problems and higher adherence. Informational resources for parents of children with cancer also highlight the importance of positive communication (http://www.cancer.gov/cancertopics/coping/youngpeople/page4; http://www.cancer.net/patient/Coping/Relationships+and+Cancer/How+A+Child+Understands+Cancer). However, some parents of children with cancer may have difficulty putting these recommendations into practice without guidance, especially if they are distressed, and empirical research is lacking on how to help parents communicate effectively.
Despite its potential importance, previous research on parent–child communication about cancer is limited. First, most studies have only examined communication during medical procedures (Cline et al., 2006; Dahlquist, Power & Carlson; 1995). Second, studies that have examined parent–child communication about cancer more broadly have been limited by small samples and qualitative analyses, and none have used observational methods (Clarke, Davies, Jenney, Glaser, & Eiser, 2005; Young, Dixon-Woods, Windridge, & Heney, 2003). Quantitative analyses are a necessary next step in providing empirically supported recommendations for intervention, and observational methods reduce the likelihood of methodological confounds with self-reported adjustment. Therefore, quantitative analyses and the use of direct observations of parent–child communication can provide more rigorous tests of the hypothesized relations between communication and adjustment.
In addition to the limitations noted previously, studies with pediatric populations have typically emphasized broad macro-level indicators of communication (see Alderfer et al., 2008, for a review). At a macro level, measuring parent–child communication involves rating the overall quality of parental characteristics or behaviors (e.g., warmth, responsiveness, intrusiveness, permissiveness). Macro-level observational analyses code the overall frequency and intensity of the behaviors throughout an interaction (Melby & Conger, 2001) but do not quantify the frequency of specific behaviors or the sequence of behaviors between parents and children.
In contrast, micro-level analyses require observational data that are coded to evaluate whether a specific response or aspect of communication has occurred and to count how many times it occurs over the course of an interaction. Micro-level analyses have been used extensively to study discourse pragmatics (i.e., how parents direct or manage conversations with their children; Lasky & Klopp, 1982) and parental responsiveness (e.g., studies of “dyadic synchrony”; see Harrist & Waugh, 2002, for a review).
Research on parent–child communication in pediatric psychology overwhelmingly has used macro-level analyses (Dunn et al., 2011; Lim et al., 2011), whereas research in developmental psychology often relies on micro-level analyses (Hart & Risley, 1992; Raikes & Thompson, 2008). However, research that integrates macro and micro levels of analysis can strengthen findings, illuminate mechanisms of effect, and provide specific targets for intervention. For example, Holmbeck et al. (2003) found that children with spina bifida used more validations and recanting, which was consistent with macro-level findings that indicated these children were less controlling and more dependent. Integrative analyses such as these may identify micro-level aspects of parent–child discourse that are associated with global measures of parental behaviors (e.g., warmth), which may be teachable communication skills for parents of children with cancer. As such, the first aim of this study was to examine associations between micro- and macro-level communication coding systems. A major goal of these analyses was to identify aspects of maternal communication that are associated with positive or negative global communication styles, so that future research may specifically examine these micro-level behaviors in relation to child psychosocial outcomes and target these behaviors during interventions.
Parents’ communication with their children about cancer may be affected by parents’ distress after diagnosis. Mothers of children with cancer often experience elevated levels of depressive symptoms after their children are diagnosed (Bruce, 2006; Dunn et al., 2012). Research with other pediatric populations suggests that mothers’ depressive symptoms may negatively impact parent–child communication, and that poorer maternal communication impacts child adjustment (Jaser & Grey, 2010; Lim et al., 2011). However, no study has examined the relations between depressive symptoms and observed mother–child communication about cancer. Given the increased risk for depressive symptoms in these mothers and the impact that maternal depression and communication may have on child adjustment and family functioning, research is needed to understand the relationships between depressive symptoms and communication about cancer. Therefore, the second aim of this study was to test if higher maternal depressive symptoms were associated with poorer maternal communication about cancer with their children.
The current study examined associations between macro- and micro-level aspects of mothers’ communication and maternal depressive symptoms in a sample of children with cancer and their mothers. The scope of the current study was limited to maternal depressive symptoms and communication rather than child behaviors and outcomes to provide a more in-depth examination of multiple levels of maternal communication. The macro-level indicators were positive and negative communication, which were coded using a well-established, well-validated macro-coding system. The micro-level indicators were developed for the current study and included topic maintenance (i.e., whether the mother maintained the topic of conversation of the child’s preceding utterance) as well as the type of maternal response (i.e., whether it was a reflection, reframe, expansion, disclosure, solicit, provision of information, imperative, or validation; see Table I for definitions). Based on previous studies showing that maternal contingency is associated with positive parenting behaviors (Harrist & Waugh, 2002) and that imperatives are associated with negative parenting behaviors (Aragona & Eyberg, 1981), we hypothesized that more topic maintenance, reflections, expansions, and validations, and fewer imperatives, would be associated with higher levels of positive communication and lower levels of negative communication. In accordance with the second aim of testing whether maternal depressive symptoms predicted communication, we hypothesized that higher levels of maternal depressive symptoms would be positively associated with higher levels of maternal negative communication and lower levels of maternal positive communication. Finally, in accordance with the goal of identifying discrete targets for psychosocial intervention, we conducted regression analyses to examine if depressive symptoms and select micro-level codes contributed unique variance in predicting mothers’ macro-level positive and negative communication. If we found that the association between macro- and micro-level aspects of communication was not solely accounted for by the relationship with depressive symptoms, this finding would suggest that micro-level communication skills (e.g., reflections) could be taught to modify macro-level patterns of communication (e.g., positive communication) independent of depressive symptoms.
Table I.
Definitions, Examples, Descriptive Statistics, and Psychometric Properties of CCS and IFIRS Codes
| Code | Definition | Examples | Mean (SD) | Range | % Agreement/ Alpha/ICC |
|---|---|---|---|---|---|
| CCS: topic maintenance | Parent continues the topic of the preceding utterance and/or develops the general topic of the conversation. | Child: “I get lots of shots.” | 93.2 (4.8)a | 79.2–100.0a | 0.96c |
| Mother: “You got one today.” | |||||
| CCS: reflection | Parent repeats some or all of the child’s utterance with no additional content. | Child: “I like the nurses.” | 9.8 (8.2)a | 0.0–35.7a | 0.91c |
| Mother: “You like them.” | |||||
| CCS: reframe | Parent corrects or disagrees with the child, or states an alternate viewpoint. | Child: “None of my friends want to spend time with me anymore.” | 5.8 (4.9)a | 0.0–33.3a | 0.67c |
| Mother: “They can’t visit because you could get sick from them.” | |||||
| CCS: expansion | Parent repeats some or all of the child’s utterance but also adds additional content. | Child: “I like the nurses.” | 5.5 (3.7)a | 0.0–21.4a | 0.72c |
| Mother: “You like the people who work here.” | |||||
| CCS: disclosure | Parent expresses something about his/her own emotional experience. | Child: “I was scared before the surgery.” | 4.0 (4.2)a | 0.0–22.2a | 0.81c |
| Mother: “I was scared too.” | |||||
| CCS: solicit | Parent asks a question to elicit a response from the child. | Child: “I can’t wait until I’m off treatment.” | 23.7 (12.6)a | 0.0–61.9a | 0.94c |
| Mother: “What are you looking forward to doing?” | |||||
| CCS: POI | Parent conveys a fact or opinion to the child. | Child: “What’s it called again?” | 28.4 (12.4)a | 6.1–61.9a | 0.88c |
| Mother: “The cancer you have is called leukemia.” | |||||
| CCS: imperative | Parent directs the child to do something or stop doing something. | Child: “What’s the next question?” | 2.0 (3.3)a | 0.0–26.3a | 0.95c |
| Mother: “Read it.” | |||||
| CCS: validation | Parent confirms, empathizes, or praises the child’s utterance without adding new content. | Child: I don’t like the shots.” | 3.3 (3.1)a | 0.0–13.0a | 0.83c |
| Mother: “I know.” | |||||
| IFIRS: positive communication | Warm, prosocial, responsive, communicative, and child-centered verbal or non-verbal behavior toward the child. | Nodding or facial expression in response to the child’s statements; hugging the child. | 6.5 (1.0)b | 2.8–8.8b | 0.91d 0.74e |
| “I’m so proud of you for being brave.” | |||||
| IFIRS: negative communication | Negative, hostile, antisocial, intrusive, and neglectful verbal or non-verbal behavior toward the child. | Frowning or scowling at the child; looking away or not responding to the child’s statements. | 3.0 (1.1)b | 1.4–6.0b | 0.73d 0.65e |
| “You always do it wrong.” |
Note. ICC = intraclass correlation; CCS = Contingency Coding System; IFIRS = Iowa Family Interaction Rating Scale; POI = Provision of Information.
aPercent of total coded utterances.
bScore on the IFIRS 1–9 scale.
cPercent agreement.
dCronbach alpha.
eMean ICC.
Method
Participants
Participants were 94 children with cancer and their mothers. Although fathers were also eligible to participate, they were excluded from the present analyses owing to the small sample size (N = 23) and the larger variability in time since diagnosis for participating father–child dyads, compared with mother–child dyads. Children ranged from 5 to 18 years old and were on average 10.4 years old (SD = 3.8); 53% percent of the child sample was male, and 83% were white/Caucasian, 12% black/African American, and 5% other, whereas 3% were Hispanic/Latino. Children had received diagnoses of leukemia (46%), lymphoma (15%), brain tumor (7%), and other solid tumor (32%). Seven percent (n = 7) were recruited into the study after a relapse of their original cancer. Mothers were on average 38.5 years old (SD = 7.8). The families represented a variety of annual income levels: 23% earned $25,000 or less, 27% earned between $25,001 and $50,000, 15% earned between $50,001 and $75,000, 13% earned between $75,001 and $100,000, and 22% earned more than $100,000.
Measures
Demographic and Medical Data
Mothers provided demographic information, including age, race, ethnicity, and family income. The children’s medical chart was also reviewed to obtain information about their diagnosis and relapse status.
Mothers’ Depression Symptoms
Mothers completed the Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) as a measure of current depressive symptoms. The BDI-II has 21 items on which participants rate their symptoms on a 4-point scale from 0 (no change/not at all) to 3 (substantial change/severely). Internal consistency reliability in the current sample was α = .94.
Observed Macro-Level Mother–Child Communication: Iowa Family Interaction Rating Scales
The Iowa Family Interaction Rating Scales (IFIRS) is a macro-level coding system to code mothers’ and children’s verbal and non-verbal communication, behaviors, and emotions in a videotaped interaction (Melby & Conger, 2001). Codes were assigned a value from 1 to 9, with 1 reflecting the absence of the behavior or emotion, and 9 indicating a behavior or emotion that is “mainly characteristic” of the parent or child during the interaction (Melby & Conger, 2001). Twenty-four codes were scored for mothers, and 15 codes were scored for children. In the current study, a positive communication composite score was derived by summing the five positive maternal codes (warmth, prosocial, listener responsiveness, communication, and child-centeredness), and a negative communication composite score was derived by summing the five negative maternal codes (externalized negative, hostility, antisocial, neglect/distancing, and intrusiveness). Similar positive and negative composites have been used in previous research using the IFIRS with other pediatric populations (DeLambo et al., 2004; Lim et al., 2011). Table I presents code definitions and examples.
All observations were coded by a trained team of graduate and undergraduate students at one of the study sites. All coders passed a written test of code definitions and examples. All observations were coded independently by two coders, who then met to discuss ratings and reach consensus for codes on which there was initially disagreement. When coders’ ratings differed by one point, the higher rating was used. When ratings differed by two or more points, coders discussed the examples that they had observed related to that code, and reached a consensus score through discussion of correct examples. For situations in which coders could not agree after this discussion, coders or the whole coding team viewed the interaction again to determine the final score. Mean reliability between coders was calculated as intraclass correlations. For mothers’ individual IFIRS codes, the intraclass correlation was .74 for positive communication and .65 for negative communication. The internal consistency was .91 for the positive communication composite and .73 for the negative communication composite.
Observed Micro-Level Mother–Child Communication: Contingency Coding System
The Contingency Coding System (CCS) is a micro-level coding system that was developed for this study. Mother and child talk was orthographically transcribed and divided into utterances, defined as “unit[s] of speech with complete semantic and syntactic content” (McLaughlin, Schutz, & White, 1980). The two maternal utterances immediately after a child utterance were coded and percentages of each code were calculated out of the total number of coded utterances. Each utterance received a topic maintenance code (i.e., whether the mother “maintained” or “changed” the topic of conversation) and then received a single code for the category of utterance (e.g., reflection). Utterances did not receive multiple category codes (i.e., utterances could not be coded both as a reflection and solicit). The different categories of utterances were reflections, reframes, expansions, disclosures, solicits, provisions of information, imperatives, and validations (see Table I for code definitions and examples). Mother utterances after child utterances that were non-verbal (e.g., nods) or lacked sufficient content were coded as uncodeable and not included in the present analyses. Code names and definitions were based on previous research in language development (Fey, Krulik, Loeb, & Proctor-Williams, 1999; Lasky & Klopp, 1982). The coding system was further refined by coding pilot data on a similar cancer conversation task. Pilot coding indicated that independent coders could achieve reliability (i.e., once all code definitions were finalized, percent agreement exceeded 80% on pilot transcripts).
Similar to the IFIRS coding, all observations were contingency coded by a trained team of graduate and undergraduate students at one of the study sites. Coders had to achieve a score of at least 80% correct on a written test of code definitions and examples. All observations were coded independently by two coders, who then met to discuss ratings and reach consensus on utterances for which there was initially disagreement. For situations in which coders could not agree after this discussion, the whole coding team reviewed the transcript to determine the final code. Before consensus, mean percent agreement between coders across all codes was 84% (see Table I for percent agreement for each code). Kappa coefficients for CCS codes could not be calculated because data from individual coders about how many times they scored an utterance as a certain code were not recorded; only the total number of disagreements and agreements between raters for each code was recorded during consensus. The recorded data allowed us to calculate observed percent agreement but not expected agreement (i.e., accounting for agreement due to chance), and therefore, we could not calculate Kappa coefficients.
Procedure
The Institutional Review Boards at both sites approved the study protocol and consent procedures. Mothers and children gave informed consent or assent. Families were compensated for their participation. Families were recruited from registries at two pediatric oncology centers in the Southern and Midwestern United States. They were eligible to participate if their child met the following criteria: (a) had a new or relapsed cancer diagnosis; (b) was between 5 and 17 years of age at the time of the child’s diagnosis or relapse; (c) was receiving treatment through the oncology division; and (d) had no preexisting developmental disability.
Mothers and children were initially recruited to participate in a preliminary questionnaire study of family adjustment to pediatric cancer. Families of children who were at least 1 week post-diagnosis or post-relapse were approached for recruitment. At this time, mothers completed the BDI-II. Of the families recruited to participate in the preliminary questionnaire study, 226 (85%) consented and completed the questionnaires. Reasons for not participating or completing the questionnaires included not being interested, lack of time, or not being able to complete and return questionnaires within the initial months after diagnosis or relapse. All families who completed the questionnaire study were approached by phone or in person at the hospital approximately 3 months later to participate in the observation. On average, mothers returned questionnaires 2.4 months (74.3 days, SD = 63.0) after the child’s diagnosis or relapse, and mother–child dyads participated in the observation 5.9 months (176.5 days, SD = 89.7) after the child’s diagnosis or relapse. Of the 226 mothers who completed questionnaires, 94 mothers (42%) and their children completed the observation study. Families who did not participate gave reasons such as not having enough time, not wanting to be videotaped, and not being interested. Families who completed the observation did not differ from those who did not complete the observation on child age [t (227) = 0.17, n.s.], race (χ2 = 1.5, n.s.), ethnicity (χ2 = 3.2, n.s.), family income [t (219) = 1.7, n.s.], relapse status (χ2 = .05, n.s.), or maternal BDI-II scores [t (224) = 1.4, n.s.].
Each mother–child dyad completed an observation session that consisted of being videotaped while the mother and child had a conversation about the child’s cancer. Mothers were given several suggested prompts to facilitate the discussion: (1) what have we each learned about cancer and how it is treated? (2) What parts of your cancer and its treatment have been the hardest for each of us? (3) What kinds of feelings or emotions have we each had since we found out you have cancer? (4) What are the ways we each try to deal with these feelings and emotions? (5) What is it about cancer that has most affected each of our lives? (6) How do we each feel about what might happen in the next year? And after that? (7) If we were writing a book about cancer for other children and parents, what would we each include? What would we want to be sure to tell other children and parents? All observations lasted for 15 min and took place in the hospital in an outpatient room or in the child’s inpatient room.
Interactions were coded using the IFIRS and the CCS, and analysis of the CCS was conducted on transcribed interactions using Systematic Analysis of Language Transcripts software (SALT; Miller, 2004). All interactions were transcribed by a trained research assistant. Transcription training included reviewing SALT guidelines (e.g., SALT tutorial and manual), practicing transcription, and meeting with experienced transcribers to review questions. Research assistants were required to reach 80% agreement (on utterance boundaries, punctuation, etc.) with the transcript of a trained and reliable transcriber before transcribing independently.
Statistical Power and Data Analyses
First, we reported descriptive statistics of maternal depressive symptoms and positive and negative communication. Next, we conducted preliminary bivariate analyses to examine relationships between study variables (maternal depressive symptoms and communication) and demographic and medical variables, to examine what demographic or medical variables, if any, should be used as control variables in the main analyses. Next, we used partial correlations (controlling for demographic variables) to examine associations among study variables; the correlational results guided our choices of which independent variables we included as predictors in the subsequent regression analyses. In addition, given the wide child age range, interaction effects were tested between age (grouped into younger and older using a median split; West & Aiken, 1991) and contingency codes in predicting positive and negative communication. Finally, we conducted hierarchical multiple regression analyses using forward selection to test the relative contributions of demographic variables, maternal depressive symptoms, and micro-level maternal communication in accounting for mothers’ positive and negative communication. Hierarchical multiple regression enters variables in different steps based on theory. We entered control variables in the first step, followed by maternal depressive symptoms in step 2, followed by CCS codes in step 3, to test the weight of CCS codes in predicting macro-level communication, above and beyond control variables and maternal depressive symptoms. Forward selection enters variables into the model in the order of the strongest predictive weight onto the dependent variable. Only variables that meet certain criteria for significance (in this case, p ≤ .05) are included in the regression equation at each step. With the sample of 94 families, power was .91 to detect statistical significance for one-tailed correlations of .3 or greater, and .84 to detect significance for two-tailed correlations of .3 or greater with .05 probability. We chose to include the full sample of participants rather than limit our sample to only children with new diagnoses. Using the full sample helped maintain our power to detect smaller effects and increased generalizability of the results to the full population of children with cancer. However, results were generally consistent when analyses were conducted with the subsample of newly diagnosed children.1
Results
Descriptive Analyses
Mothers’ mean score on the BDI-II (M = 13.7, SD = 10.7) approached the cutoff score of 14 for the “mildly depressed” category (Beck et al., 1996), and 45% of mothers scored at or above this cutoff. Means scores and standard deviations of the IFIRS composites and CCS codes are reported in Table I. For mothers’ IFIRS codes, the mean score on a 9-point scale was 6.5 (SD = 1.0) for positive communication and 3.0 (SD = 1.1) for negative communication. Means for all CCS codes are presented as the percentage of total coded mother utterances. Mothers maintained the topic on average 93.2% of the time, and category codes ranged from 2.0% (imperatives) to 28.4% (provisions of information).
Preliminary Analyses of Associations Between Medical and Demographic Variables and Maternal Communication and Depressive Symptoms
No significant differences were found on any maternal communication variables or maternal depressive symptoms when comparing mothers of children with different diagnosis types (i.e., leukemia, lymphoma, brain tumor, and other solid tumor). Additionally, mothers of children with relapsed disease did not differ on any communication variables or depressive symptoms, with the exception that they used fewer disclosures [t (19) = 3.3, p < .01]; however, the sample was underpowered to examine differences between new diagnosis and relapse groups owing to the small number (n = 7) of children with relapsed disease.
Correlational analyses of maternal communication and depressive symptoms variables with demographic variables indicated that older child age was significantly negatively associated with levels of maternal positive communication (r = −.25, p < .05) but not significantly associated with maternal negative communication. Older child age was also significantly associated with fewer maternal reflections (r = −.48, p < .001), fewer solicits (r = −.51, p < .001), fewer imperatives (r = −.26, p < .05), more disclosures (r = .34, p < .01), and more provisions of information (r = .40, p < .001). Child age was not associated with maternal depressive symptoms. Family income was significantly positively associated with maternal positive communication (r = .29, p < .01) and negatively associated with maternal negative communication (r = −.29, p < .01), as well as more maternal validations (r = .25, p < .05) and fewer imperatives (r = −.29, p < .01). Family income was also significantly negatively associated with maternal depressive symptoms (r = −.25, p < .01). In families of sons compared with daughters, mothers did not differ on positive or negative communication or depressive symptoms. However, results indicated that mothers used more expansions, t (91) = −2.1, p < .05, and fewer disclosures, t (91) = 2.4, p < .05, with their sons.
Correlations Between Mothers’ Positive and Negative Communication and Mothers’ Contingency Codes and Depressive Symptoms
Table II presents partial correlations among mothers’ positive and negative communication, contingency codes, and depressive symptoms. Partial correlations were used to control for child age and family income owing to the associations between these variables and maternal communication. Higher levels of positive communication were significantly associated with use of more topic maintenance and reflections, fewer reframes and imperatives, and lower levels of maternal depressive symptoms (rs ranged from −.31 to .30). Higher rates of negative communication were associated with less topic maintenance, more reframes and imperatives, and more depressive symptoms (rs ranged from −.35 to .34). Mothers’ expansions, disclosures, solicits, provisions of information, and validations were not significantly correlated with their positive and negative communication. Table II also presents partial correlations between contingency codes and maternal depressive symptoms. Analyses indicated that higher levels of depressive symptoms were significantly correlated with fewer validations (r = −.22, p < .05).
Table II.
Correlations Between Mothers’ IFIRS Positive and Negative Communication and Mothers’ CCS Codes and Depressive Symptoms, Controlling for Child Age and Family Income
| IFIRS positive communication | IFIRS negative communication | BDI | |
|---|---|---|---|
| Topic maintenance | .30** | −.35** | −.05 |
| Reflections | .24* | −.20 | .05 |
| Reframes | −.22* | .34** | .17 |
| Expansions | .13 | −.07 | −.01 |
| Disclosures | .05 | −.06 | −.05 |
| Solicits | .01 | −.01 | −.01 |
| POIs | −.14 | −.02 | .00 |
| Imperatives | −.31** | .33** | .06 |
| Validations | .05 | −.03 | −.22* |
| BDI | −.21* | .30** | — |
Note. POIs = Provisions of Information; BDI = Beck Depression Inventory-II; CCS = Contingency Coding System; IFIRS = Iowa Family Interaction Rating Scale.
*p < .05; **p < .01.
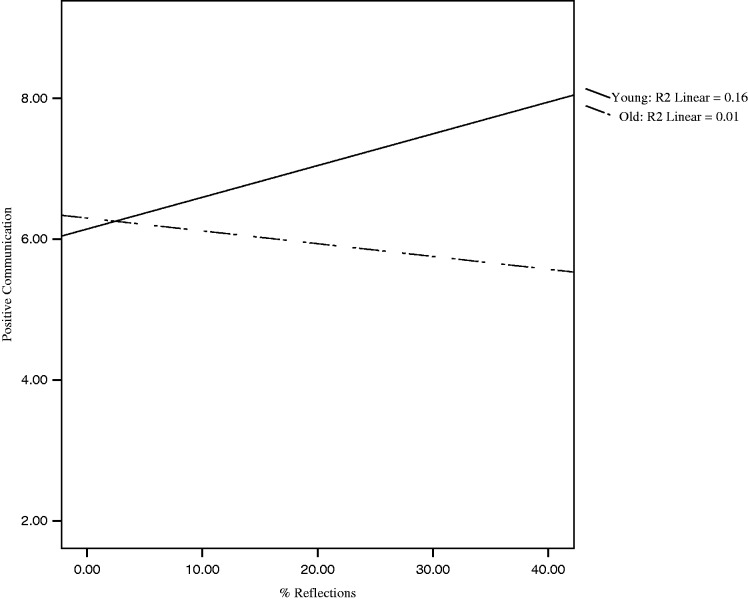
Analyses examining CCS codes × age interaction effects yielded a significant age × reflections interaction (β = −.18, p < .05) in predicting positive communication (see Figure 1). Results indicated that reflections were associated with positive communication for younger children (R2 = .16) but not older children (R2 = .01).
Figure 1.
Interaction of child age and maternal reflections predicting mothers’ positive communication. Note. young = child age < 10 years; old = child age ≥ 10 years.
Linear Multiple Regression Analyses
A series of hierarchical multiple regression analyses using the forward-entry method was conducted with mothers’ positive and negative communication scores as the dependent variables (see Table III). In each regression equation, child age and family income were entered in block 1, followed by mothers’ depressive symptoms on the BDI-II in block 2, followed by topic maintenance, reflections, reframes, and imperatives (for positive communication) and topic maintenance, reframes, and imperatives (for negative communication) in block 3. In the model predicting mothers’ positive communication, the change in R2 was significant after including depressive symptoms (R2 Δ = .04, p < .05), after including imperatives (R2 Δ = .07, p < .01), and after including reflections (R2 Δ = .03, p < .05). The overall final equation was significant (adjusted R2 = .30), and family income, child age, BDI-II scores, imperatives, and reflections were significant independent predictors of positive communication in the final equation; topic maintenance and reframes were not significant predictors. For the model predicting mothers’ negative communication, the change in R2 was significant after including BDI-II scores (R2 Δ = .08, p < .01), after including topic maintenance (R2 Δ = .10, p < .01), and after including reframes (R2 Δ = .07, p < .01). The overall final equation was significant (adjusted R2 = .30), and BDI-II scores, topic maintenance, and reframes were significant independent predictors of negative communication; income, child age, imperatives, and reflections were not significant predictors.2
Table III.
Final Regression Equations Predicting Mothers’ IFIRS Positive and Negative Communication Using Child Age, Family Income, Mothers’ Depression Symptoms, and Mothers’ CCS Codes
| IFIRS positive communication | IFIRS negative communication | |
|---|---|---|
| Predictor | β | β |
| Income | .27** | −.15 |
| Child age | −.29** | n.s. |
| BDI | −.19* | .23* |
| CCS reflections | .21* | n.s. |
| CCS reframes | n.s. | .26** |
| CCS imperatives | −.25* | n.s. |
| CCS topic maintenance | n.s. | −.29** |
| Total adjusted R2 | .30 | .30 |
Note. CCS = Contingency Coding System; IFIRS = Iowa Family Interaction Rating Scale; BDI = Beck Depression Inventory-II total score; β = standardized beta; n.s. = indicates that the variable did not meet criteria (p ≤ .05) to be entered by forward selection into the equation.
*p < .05; **p < .01.
Discussion
This study presents novel findings on the associations between micro- and macro-level aspects of maternal communication in mothers of children with cancer. We found that mothers who more frequently maintained the topic of the child’s preceding utterance, and responded with more reflections (for younger children) and fewer reframes and imperatives, were independently rated as high on a positive communication style, characterized by warmth, child-centeredness, and responsiveness. These associations held true for reflections and imperatives even after controlling for income, child age, and maternal depressive symptoms. Mothers who maintained the child’s topic less frequently, and used reframes and imperatives more often, demonstrated a negative communication style, characterized by hostility, neglect, and intrusiveness. This pattern held true for topic maintenance and reframes even when controlling for income, child age, and maternal depressive symptoms.
The current findings suggest directions for intervention with mothers of children with newly diagnosed or relapsed disease. Psychosocial interventions for parents of children with cancer have reduced parental distress by enhancing cognitive restructuring and family strengths (Kazak et al., 2005) and by improving problems-solving skills (Sahler et al., 2005). However, there is less evidence that psychosocial interventions can improve child outcomes (Pai, Drotar, Zebracki, Moore, & Youngstrom, 2006). The current study indicates that mother–child communication may be related to, but also somewhat independent of, maternal depressive symptoms, suggesting that interventions could target maternal communication as an additional pathway to improving child adjustment outcomes and family functioning beyond such factors as maternal distress, cognitive restructuring, and problem-solving. Thus, it will be crucial for future studies to assess child outcomes in relation to maternal communication, including whether positive or negative maternal communication is more predictive of child outcomes. The results regarding reflections suggest that reflecting the child’s talk is a key component of a positive maternal communication style with younger children, likely because reflections convey warmth and emotional support to the child. The opposing findings regarding imperatives suggest that mothers who use more commands are viewed as more hostile, intrusive, and insensitive, especially in the context of a conversation about cancer. Maternal imperatives may also be a response to children’s behavior, such that mothers of children who show more behavior problems are more likely to use imperatives during conversation as well as to interact with their child in a more hostile, intrusive manner (Aragona & Eyberg, 1981).
Interestingly, the results regarding reframes may appear counterintuitive at first glance, but ultimately may relate to how we chose to examine conversational responses (i.e., examining mothers’ first two utterances after the child speaks) and the context of the conversation (i.e., that mothers were reframing during a conversation about the child’s cancer). Although reframing or reappraising a problem may be an adaptive skill when used individually to cope with illness (Compas, Jaser, Dunn, & Rodriguez, 2012), maternal reframing of children’s talk may not be effective during communication about a highly emotional topic such as cancer. Rather, our results suggest that reframing may be perceived as hostile or insensitive when mothers respond this way immediately (i.e., in their first two utterances) after the child expresses a negative thought or emotion. Overall, our findings imply that for mother–child communication about specific, emotionally distressing, and uncontrollable situations (such as the experience of having cancer), it may be helpful to teach mothers certain conversation skills (e.g., topic maintenance, reflections), while discouraging other types of responses (e.g., reframes, imperatives) as part of an adaptive mother–child communication style.
As expected, maternal emotional depressive symptoms predicted mothers’ global positive and negative communication styles, such that mothers who reported more depression symptoms were less warm, supportive, and responsive and more hostile, intrusive, and neglectful in the interaction with their child. These results suggest that a key component of intervening to help these families communicate about cancer may be to reduce maternal depressive symptoms. Further, regression analyses suggested that when demographic factors (child age, family income), maternal depressive symptoms, and mothers’ micro-level aspects of communication are all taken into account to predict mothers’ global communication style, maternal depressive symptoms and micro-level aspects of communication each uniquely predicted mothers’ negative communication above and beyond child age and family income. These results strengthen the argument that interventions should concurrently attempt to reduce maternal depressive symptoms and promote certain micro-level communication skills (e.g., reflections) when intervening with these families.
This study has several strengths. First, the sample was relatively large and was recruited close in time to cancer diagnosis or relapse. A second strength is its methodological rigor, which included multi-method assessments (self-report, observational coding) and the double-coding of all observational data. Third, this study presents some of the first quantitative findings on mother–child communication about a child’s cancer, including associations between macro- and micro-level aspects of communication and associations between previous self-reported depressive symptoms and observed communication. Further, the results suggest concrete components of interventions for these families, such as teachable communication skills.
However, several limitations also exist and provide direction for future research. First, there were several limitations related to the observational coding process. We were only able to calculate percent agreement and not Kappa coefficients for CCS codes; therefore, we could not account for chance agreement, and our agreement is likely overestimated for these codes. Additionally, the reliability for the macro-level negative communication code was lower than desirable, which may have limited our ability to detect associations with other variables. It is possible that other micro-level codes would be significantly associated with negative communication with improved reliability. However, all observational data were double-coded, and the data used in our analyses represented both coders’ consensus agreement, which strengthens the findings despite these limitations in reliability. Second, this study involved clinic-based data collection. This approach may have influenced mother–child interactions and likely reduced father participation. Research suggests that distressed fathers may communicate with their children differently than distressed mothers (Jacob & Johnson, 2001). The inclusion of only mothers in the current analyses limits generalizability to whole families; to design interventions for the whole family, it is imperative to compare and contrast maternal and paternal communication with children about cancer as well as to include other family members (e.g., siblings, grandparents, or other caregivers) in studies of communication and family adjustment. Future studies should consider home-based data collection to increase father participation. Third, other characteristics of the sample may limit the generalizability of our results, such as the inclusion of relapse participants without controlling for disease prognosis, the wide age range of the children without assessing developmental level beyond age, and the lower retention rates for the families participating in the observation task, which may indicate that results do not generalize to lower functioning families who chose not to participate in the observation. Additional limitations include the wide range in socioeconomic status (SES) of the sample (although we controlled for income, there may be other aspects of SES that impact maternal depressive symptoms and communication) and the low percentage of racial and ethnic minority participants. Future studies should seek to replicate findings with a more diverse sample. Additionally, future studies should examine child developmental level to understand how children may benefit from different aspects of maternal communication at different points in development, which may aid in tailoring interventions for younger children or adolescents.
Finally, we did not analyze child communication or distress, which prevented us from examining bidirectional effects between mother and child. As it is likely that maternal communication is influenced by how and what children communicate during the conversation, future studies should assess child communication. Additionally, it will be important to incorporate child outcome variables such as distress and quality of life in future studies to understand how parental communication affects children’s adjustment after diagnosis. It will also be important to examine the content of the mother–child discussions, which may be associated with maternal depressive symptoms (e.g., more distressed mothers may avoid topics such as prognosis or the child’s negative emotions). Content may also predict child adjustment, because mothers who discuss difficult topics openly may, in the process, model positive adaptation and coping. Future studies should code content and examine associations with maternal and child distress.
The current findings also suggest directions for research in different contexts and with different populations. Although findings may be relevant to mother–child conversations about a child’s cancer, the implications are unknown for other conversational topics and other populations. Therefore, future studies should examine micro-level codes (specifically reflections, reframes, and imperatives) during non-cancer-related conversations, as well as for different populations, such as children with other chronic illnesses, children with mental health problems, and children with positive adjustment outcomes. For example, it is possible that mother–child discussions about other chronic illnesses are less emotionally charged, and therefore, the current findings regarding reframes and imperatives may not apply. Research on the development of coping also would benefit from examining the relation of certain conversational responses (e.g., reframes, disclosures) to parent and child coping strategies (e.g., cognitive restructuring, emotional expression). This research would provide much needed information about the role of parent–child communication in the development of coping and children’s positive adjustment.
Funding
This work was supported by the National Cancer Institute at the National Institutes of Health (grant numbers R01CA118332 and Ruth L. Kirschstein National Research Service Award F31CA136284); the Vanderbilt Clinical and Translational Science Award (CTSA) grant from the National Institutes of Health (grant number 1 UL1 RR024975); a gift from Patricia and Rodes Hart; and intramural funding from The Research Institute at Nationwide Children’s Hospital.
Conflicts of interest: None declared.
Footnotes
1 All analyses were also conducted with a reduced sample that excluded children with relapsed disease (n = 7). The results were consistent with results from the full sample, with the exception that the partial correlation between the BDI-II and positive communication became a trend (r = −.20, p = .07) and the partial correlation between reflections and negative communication became significant (r = −.27, p = .02). Regression analyses yielded consistent results with the reduced sample.
2 Because several of the CCS codes (reframes, disclosures, and imperatives) had skewed distributions, analyses were also conducted after these variables were transformed using a log 10 transformation of the data. The results of the correlational analyses were consistent with non-transformed data; however, regression analyses with transformed data indicated that topic maintenance became a significant predictor of both positive communication (β = 0.26, p < .01) and negative communication (β = −0.32, p < .01), reflections, reframes, and imperatives were not significant in the regression equations.
References
- Alderfer M A, Fiese B H, Gold J I, Cutuli J J, Holmbeck G N, Goldbeck L, Chambers C, Abad M, Spetter D, Patterson J. Evidence-based assessment in pediatric psychology: family measures. Journal of Pediatric Psychology. 2008;33:1046–1061. doi: 10.1093/jpepsy/jsm083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aragona J A, Eyberg S M. Neglected children: Mothers' report of child behavior problems and observed verbal behavior. Child Development. 1981;52:596–602. [PubMed] [Google Scholar]
- Beck A T, Steer R A, Brown G K. Beck depression inventory manual. 2nd ed. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Bruce M. A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clinical Psychology Review. 2006;26:233–256. doi: 10.1016/j.cpr.2005.10.002. [DOI] [PubMed] [Google Scholar]
- Clarke S, Davies H, Jenney M, Glaser A, Eiser C. Parental communication and children’s behaviour following diagnosis of childhood leukaemia. Psycho-Oncology. 2005;14:274–281. doi: 10.1002/pon.843. [DOI] [PubMed] [Google Scholar]
- Cline R J, Harper F W, Penner L A, Peterson A M, Taub J W, Albrecht T L. Parent communication and child pain and distress during painful pediatric cancer treatments. Social Science & Medicine. 2006;63:883–898. doi: 10.1016/j.socscimed.2006.03.007. [DOI] [PubMed] [Google Scholar]
- Compas B E, Jaser S S, Dunn M J, Rodriguez E M. Coping with chronic illness in childhood and adolescence. Annual Review of Clinical Psychology. 2012;8:455–480. doi: 10.1146/annurev-clinpsy-032511-143108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlquist L M, Power T G, Carlson L. Physician and parent behavior during invasive pediatric cancer procedures: relationships to child behavioral distress. Journal of Pediatric Psychology. 1995;20:477–490. doi: 10.1093/jpepsy/20.4.477. [DOI] [PubMed] [Google Scholar]
- DeLambo KE, Ievers-Landis CE, Drotar D, Quittner A L. Association of observed family relationship quality and problem-solving skills with treatment adherence in older children and adolescents with cystic fibrosis. Journal of Pediatric Psychology. 2004;29:343–353. doi: 10.1093/jpepsy/jsh038. [DOI] [PubMed] [Google Scholar]
- Dunn M J, Rodriguez E M, Barnwell A S, Grossenbacher J, Vannatta K, Gerhardt C A, Compas B E. Posttraumatic stress symptoms in parents of children with cancer within six months of diagnosis. Health Psychology. 2012;31:176–185. doi: 10.1037/a0025545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn M J, Rodriguez E M, Miller K S, Gerhardt C A, Vannatta K, Saylor M M, Schuele C M, Compas B E. Direct observation of mother-child communication in pediatric cancer: assessment of verbal and non-verbal behavior and emotion. Journal of Pediatric Psychology. 2011;36:565–575. doi: 10.1093/jpepsy/jsq062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fey M E, Krulik T E, Loeb D F, Proctor-Williams K. Sentence recast use by parents of children with typical language and children with specific language impairment. American Journal of Speech-Language Pathology. 1999;8:273–286. [Google Scholar]
- Harrist A W, Waugh R M. Dyadic synchrony: its structure and function in children's development. Developmental Review. 2002;22:555–592. [Google Scholar]
- Hart B, Risley T R. American communication of language-learning children: persistent differences in family-child interactions observed in natural home environments. Developmental Psychology. 1992;28:1096–1105. [Google Scholar]
- Holmbeck G N, Westhoven V, Phillips W S, Bowers R, Gruse C, Nikolopoulos T, Totura C W, Davison K. A multimethod, multi-informant, and multidimensional perspective on psychosocial adjustment in preadolescents with spina bifida. Journal of Consulting and Clinical Psychology. 2003;71:782–796. doi: 10.1037/0022-006x.71.4.782. [DOI] [PubMed] [Google Scholar]
- Jacob T, Johnson S L. Sequential interactions in the parent-child communications of depressed fathers and depressed mothers. Journal of Family Psychology. 2001;15:38–52. [PubMed] [Google Scholar]
- Jaser S S, Grey M. A pilot study of observed parenting and adjustment in adolescents with type 1 diabetes and their mothers. Journal of Pediatric Psychology. 2010;35:738–747. doi: 10.1093/jpepsy/jsp098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA: Cancer Journal for Clinicians. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- Kazak A E, Simms S, Alderfer M A, Rourke M T, Crump T, McClure K, Jones P, Rodriguez A, Boeving A, Hwang W -T, Reilly A. Feasibility and preliminary outcomes from a pilot study of a brief psychological intervention for families of children newly diagnosed with cancer. Journal of Pediatric Psychology. 2005;30:644–655. doi: 10.1093/jpepsy/jsi051. [DOI] [PubMed] [Google Scholar]
- Lasky E Z, Klopp K. Parent-child interactions in normal and language-disordered children. Journal of Speech and Hearing Disorders. 1982;47:7–18. doi: 10.1044/jshd.4701.07. [DOI] [PubMed] [Google Scholar]
- Lim J, Wood B L, Miller B D, Simmens S J. Effects of paternal and maternal depressive symptoms on child internalizing symptoms and asthma disease activity: mediation by interparental negativity and communication. Journal of Family Psychology. 2011;25:137–146. doi: 10.1037/a0022452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin B, Schutz C, White D. Parental speech to five-year-old children in a game-playing situation. Child Development. 1980;51:580–582. [Google Scholar]
- Melby J N, Conger R D. The Iowa family interaction rating scales: instrument summary. In: Kerig P K, Lindahl K M, editors. Family observational coding systems. Mahwah, NJ: Erlbaum; 2001. pp. 1–22. [Google Scholar]
- Miller J. Systematic analysis of language transcripts. 2004. (Research Version 8.0) [Computer software]. Madison: University of Wisconsin. Retrieved from http://www.saltsoftware.com/ [DOI] [PubMed] [Google Scholar]
- Pai A L, Drotar D, Zebracki K, Moore M, Youngstrom E. A meta-analysis of the effects of psychological interventions in pediatric oncology on outcomes of psychological distress and adjustment. Journal of Pediatric Psychology. 2006;31:978–988. doi: 10.1093/jpepsy/jsj109. [DOI] [PubMed] [Google Scholar]
- Raikes H A, Thompson R A. Attachment security and parenting quality predict children's problem-solving, attributions, and loneliness with peers. Attachment and Human Development. 2008;10:319–44. doi: 10.1080/14616730802113620. [DOI] [PubMed] [Google Scholar]
- Rodriguez E M, Dunn M J, Zuckerman T, Vannatta K, Gerhardt C A, Compas BE. Cancer-related sources of stress for children with cancer and their parents. Journal of Pediatric Psychology. 2012;37:185–197. doi: 10.1093/jpepsy/jsr054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahler O J, Fairclough D L, Phipps S, Mulhern R K, Dolgin M J, Noll R B, Katz E R, Varni J W, Copeland D R, Butler R W. Using problem-solving skills training to reduce negative affectivity in mothers of children with newly diagnosed cancer: report of a multisite randomized trial. Journal of Consulting and Clinical Psychology. 2005;73:272–283. doi: 10.1037/0022-006X.73.2.272. [DOI] [PubMed] [Google Scholar]
- West S G, Aiken L S. Multiple regression: testing and interpreting interactions. Thousand Oaks, CA: Sage Publications; 1991. [Google Scholar]
- Wijnberg-Williams B J, Kamps W A, Klip E C, Hoekstra-Weebers J E. Psychological adjustment of parents of pediatric cancer patients revisited: five years later. Psycho-Oncology. 2006;15:1–8. doi: 10.1002/pon.927. [DOI] [PubMed] [Google Scholar]
- Young B, Dixon-Woods M, Windridge KC, Heney D. Managing communication with young people who have a potentially life threatening chronic illness: qualitative study of patients and parents. British Medical Journal. 2003;326:1–5. doi: 10.1136/bmj.326.7384.305. [DOI] [PMC free article] [PubMed] [Google Scholar]