Abstract
Two models of vulnerability to socioenvironmental risk were examined in 337 African American children (M = 7.8 years) recruited to over-represent prenatal alcohol or cocaine exposure: the cumulative risk model predicted synergistic effects from exposure to multiple risk factors, and the fetal patterning of disease model predicted that prenatal insult will increase vulnerability to environmental risk. Four or more risks emerged as a threshold for poorer cognitive and behavioral outcome among the non-substance exposed children, whereas substance-exposed children showed greater vulnerability to lower levels of environmental risk. Cumulative risk was associated with increased delinquent and internalizing behaviors only for the substance-exposed group. Results support the cumulative risk model for non-substance exposed children and increased vulnerability to environmental risk among the substance-exposed group.
A wide range of factors in the social environment has been shown to put the child at risk for poorer cognitive and emotional development. One approach to understanding the effects of multiple-risk exposure on children’s outcomes has focused on the examination of cumulative risk. The cumulative risk model hypothesizes that the total number of risk factors to which the child is exposed is critically important in predicting child maladjustment (Garmezy, 1985; Rutter, 1979; Sameroff, Seifer, Baldwin, & Baldwin, 1993). This model suggests that, regardless of the specific risk factor, as the number of risk factors increases, child psychosocial adjustment becomes increasingly compromised. An alternative model for examining the impact of socioenvironmental risk focuses on the moderating impact of fetal patterning of adult disease. This approach is based on evidence from developmental biology and animal studies suggesting that environmental influences operating in utero can affect the propensity for a disease that may not become manifest until later in development (Gluckman & Hanson, 2004; Wadhwa, 2005). It is hypothesized that an intrauterine event may alter neural development so as to render certain individuals at risk for pathology later in life, increasing vulnerability to chronic illness, including depression, anxiety disorders, schizophrenia, and drug abuse (McDonald, Devan, & Hong, 2004). One implication of this model is that an intrauterine insult, such as fetal alcohol or drug exposure, might increase vulnerability to socioenvironmental risk factors encountered by a child who is reared in a less-than-optimal environment. The study reported here examined the impact of socioenvironmental risk on cognitive and behavioral outcomes from the perspectives of both models—cumulative risk and fetal patterning of disease—using data from a prospective, longitudinal study of inner-city African American children.
Cumulative Risk
A cumulative risk model provides information regarding the number of risk factors the child can “tolerate” before his or her psychosocial adjustment deteriorates markedly (Jones, Forehand, Brody, & Armistead, 2002). For example, in the Isle of Wight study, when using a risk score based on the presence or absence of up to six risk factors (e.g., low socioeconomic status, overcrowding, maternal psychiatric disorder), the incidence of child psychiatric diagnosis increased sevenfold when the total risk score was four or more (Rutter, 1979). Werner and Smith (1982) used a set of twelve risk variables, including poverty, parental psychopathology, and disruption of family unit, and found that children with risk scores of four or more at age 2 years had significantly poorer quality of adaptation at ages 10 and 18 than children with fewer than four factors. Applying this model to cognitive outcomes, Sameroff et al. (1993) used a cumulative risk index in their longitudinal study of IQ scores in 4- and 13-year-old children whose mothers were recruited to overrepresent maternal mental illness. The authors examined 10 risk factors (minority group status, occupation of head of household, maternal education, family size, father absence, stressful life events, parenting perspectives, maternal anxiety and mental health, and mother-child interaction—each of which was dichotomized as high or low risk), and a risk index score was calculated based on the number of risk factors in the child’s family. They found that IQ scores decreased at both ages as the number of risks increased, with the risk index accounting for 34% of the variance in IQ at 4 years and 37% at 13. This effect persisted even after socioeconomic status (SES) was controlled statistically and was still substantial after adjustment for the effects of maternal IQ.
Burchinal, Roberts, Hooper, and Zeisel (2000) compared the predictive power of the cumulative risk approach, in which each risk factor is dichotomized to permit tabulation of the number of high risks to which the child is exposed, with a multiple regression approach, in which child outcomes are predicted from individual risk variables examined simultaneously. The authors note that the multiple regression approach retains the full predictive power of the original continuous risk measures and permits evaluation of the relative importance of each predictor. An important advantage of the cumulative risk approach is that it permits examination of the hypothesis that the impact of multiple risks becomes exacerbated after the number of risks to which the child is exposed exceeds a given threshold.
African Americans have been underrepresented in studies examining cumulative risk, and some studies that have examined cumulative risk in African American children have yielded different findings from those studying Caucasian children. Deater-Deckard, Dodge, Bates and Pettit (1998) found that individual differences in the increase in externalizing behaviors between 5 and 10 years of age were related to both individual risk factors and cumulative risk. However, their results suggested that most of the prediction of externalizing behavior from cumulative risk was found among Caucasian rather than African American children. Similarly, Gerard and Buehler (2004) found that the association of their cumulative risk measure with conduct problems in 7th to 11th grade children was stronger for Caucasian than for African American youth. In the Sameroff et al. study (1993), the effect of the cumulative risk at age 4 years was also found only among the Caucasian families, although it was evident within both the Caucasian and African American families at 13 years.
An improved understanding of vulnerability to socioenvironmental risk in the African American population is particularly important given that this population is disproportionately exposed to environments with high levels of psychosocial risk (McLoyd, 1990). In a study of 277 African American children living in single-mother households, Jones et al. (2002) found that cumulative risk was not related to externalizing problems but was predictive of internalizing problems. Among the individual risk factors that these authors examined, only inadequate parenting was significantly related to externalizing problems, whereas maternal depressive mood and inadequate parenting were related to internalizing problems. Kim and Brody (2005) examined risk factors longitudinally using the same data set. They found that an accumulation of family risk factors at age 11 years was linked with maternal psychological functioning at age 12 years, which forecast competence-promoting parenting practices at age 13 years. These parenting practices indirectly predicted externalizing and internalizing behaviors 2 years later, a process that was mediated by youth self-regulation at age 14 years. Thus, cumulative risk impacted the child’s later behavior by influencing the child’s psychosocial experiences, including interaction with his/her parents.
Fetal Origins of Vulnerability to Socioenvironmental Risk
Numerous studies have examined the relation of prenatal exposure to alcohol and illicit drugs to cognitive and emotional development. Fetal alcohol spectrum disorder (FASD) ranges from the most severe form—fetal alcohol syndrome (FAS), which is characterized by a distinctive craniofacial dysmorphology, small head circumference, and pre- and/or postnatal growth retardation (Hoyme et al., 2005)—to alcohol-related neurodevelopmental disorder (ARND), a term applied to children exposed prenatally to alcohol who lack the characteristic FAS dysmorphology but exhibit measurable, albeit generally subtler neurobehavioral deficits (Stratton, Howe & Battaglia, 1996; Hoyme et al., 2005). Although many children with FAS are mentally retarded (IQ < 70), most children with ARND perform in the normal range (Streissguth, Barr & Sampson, 1990; Streissguth, Aase, Clarren, Randels, LaDue & Smith, 1991; Mattson, Riley, Gramling, Delis & Jones, 1997; Goldschmidt, Richardson, Stoffer, Geva & Day. 1996). These effects are generally more severe in children whose mothers were older at time of delivery and/or had a history of alcohol abuse problems and less severe in those who received more optimal parental intellectual stimulation and emotional support (Jacobson, Jacobson, Sokol, Chiodo & Corobana, 2004). In addition to its effects on cognitive development, prenatal alcohol exposure has been linked to depression in children (O’Connor et al., 2002) and adults (Famy, Streissguth & Unis, 1998; Carmichael Olson, Feldman, Streissguth, Sampson, & Bookstein, 1998; Spohr & Willms, 1993; Steinhausen, Willms, & Spohr, 1993)
Because the biological insult associated with prenatal substance exposure is likely to be confounded with environmental influences associated with maternal drinking during childhood, it is important to try to distinguish these influences. O’Connor and Paley (2006) found that, whereas prenatal alcohol exposure was associated with increased depressive symptoms in the child, these symptoms were not related to current maternal drinking patterns or depression, supporting the hypothesis that fetal exposure plays a critical role in increasing vulnerability to child depression. Similarly, Jacobson et al. (2006) found that prenatal alcohol exposure was predictive of teacher reports of externalizing problems in the classroom but that these problems were unrelated to current maternal drinking, again suggesting a particular role for fetal exposure in increasing the risk of developing emotional problems in childhood.
Prenatal exposure to cocaine has also been studied in relation to childhood cognitive and emotional development. Coles and Black (2006) point out that, by contrast to fetal alcohol exposure, findings on the effects of prenatal cocaine exposure have been mixed, with the clearest effects seen in cases of heavy cocaine exposure (Alessandri & Bendersky, 1998; Frank & McCarten, 1999; Jacobson, Jacobson, Sokol, Martier & Chiodo, 1996; Singer et al., 2001; Singer et al., 2002). There have been relatively few reports of adverse effects on cognitive performance, play behavior, academic achievement, and classroom behavior (Frank et al. 2002; Mayes, 2002; Mayes, Molfese, Key & Hunter, 2005). The effects have been found primarily on behavioral problems, task persistence and attention, and language performance. Bendersky, Bennett, and Lewis (2006) examined childhood aggression at age 5 years in a multiple risk model that included cocaine exposure, environmental risk, and gender as predictors and found that all three of these factors were related to a composite aggression score based on reports from multiple informants. Carta et al. (2001) examined the effects of cumulative prenatal substance exposure and cumulative environmental risk on the developmental trajectories of 278 infants, toddlers, and preschool children. Both prenatal exposure and environmental risk added unique variance to the prediction of rate of growth and developmental level and after controlling for birth weight and gender.
The studies to date have focused primarily on detecting main effects of prenatal substance exposure on long-term outcome after controlling for the influences of the social environment. However, studies of preterm infants have demonstrated that fetal and neonatal insult can also increase vulnerability to environmental risk. For example, Levy-Shiff, Einat, Mogilner, Lerman, and Krikler (1994) examined the role of biological and psychosocial factors in predicting long-term outcome in adolescents who were born prematurely at very low birth weight compared with those who were born full-term at normal birth weight. They found that SES predicted visual-motor coordination and hyperactive behavior in the very low birth weight group but not in the normal birth weight group, indicating an interaction between biological vulnerability and environmental risk. Landry, Smith, Swank, Assel and Vellet (2001) studied the role of early vs. ongoing maternal responsiveness in predicting cognitive development in full-term and preterm children at five ages ranging from 6 months to 4 years. They found that both preterm and full-term children’s developmental rates in cognitive skills were close to the expected gains of 12 months per year with consistently high levels of responsive parenting. On the other hand, preterm children’s gains were only 9 months per year, compared to 11 months per year gained by full-term children, when parented by consistently low-responsive mothers. Thus, their data demonstrate the greater vulnerability of children who have experienced an early biological insult to less than optimal parental responsiveness (see also Parker, Greer, and Zuckerman, 1988). Whereas most of these studies have focused on specific environmental risks, the few that have examined the impact of neonatal insult on increased vulnerability to cumulative risk lacked an appropriate control group (e.g, Escalona, 1982). Based on these studies from the preterm literature, we hypothesize that children who are biologically vulnerable due to prenatal alcohol or drug exposure and are also exposed to cumulative environmental risks may also be at “double jeopardy” for poor outcomes (Carta et al., 2001).
Aims of the Study
The principal aim of this study was to examine the degree to which cumulative risk and fetal substance exposure modify vulnerability to socioenvironmental risk in a sample of economically-disadvantaged, African American inner city children. We looked at socioenvironmental risks associated with poor outcome and compared their cumulative effects on the child’s cognitive and emotional development in prenatally exposed and non-exposed groups. The goal was to examine whether cumulative risk operates differently in these two groups, as well as the degree to which the impact of cumulative risk in the non-exposed African American children resembles that reported in studies of Caucasian children. In addition, it was hypothesized that children who were prenatally exposed would be more vulnerable to cumulative risk factors. Specifically, we predicted that the magnitude of association between risk factors and negative outcome would be stronger in exposed children and that the threshold for a poorer outcome would be lower among children who were exposed to substances prenatally than those who were not.
METHOD
Participants
Mothers were recruited during pregnancy for a longitudinal study on the effects of prenatal exposure to alcohol and cocaine on child development (Jacobson et al., 2004; Jacobson et al., 2006). All African American women were screened for alcohol consumption during their first visit to a prenatal clinic in a large urban maternity hospital (M = 23.4 weeks of gestation, SD= 7.9) from 1986–1989 using a timeline follow-back interview (Jacobson, Chiodo, Jacobson & Sokol, 2002). Those averaging seven drinks per week or more at the time of conception (≥0.5 oz absolute alcohol [AA] per day), the lowest level at which adverse effects have been observed (Jacobson & Jacobson, 1994; Jacobson, Jacobson, Sokol & Ager, 1998), were invited to participate in the study in order to overrepresent women who were drinking at moderate-to-heavy levels during pregnancy. A random sample of 5% of the abstainers and lighter drinkers (< 0.5 oz AA/day) from the clinic population were also invited to participate. In addition, the sample includes 78 women who reported heavy cocaine (≥= 2 days per week), light alcohol (< 7 drinks per week) use at the time of recruitment. The inclusion of this subgroup substantially reduced the confounding of prenatal alcohol and cocaine exposure (Jacobson et al., 1996); only eight moderate-to-heavy drinkers reported heavy use of cocaine at recruitment. Mean maternal age at recruitment was 26.4 years (SD = 6.0), with 6.3 % between 14 and 18 years. Infant exclusionary criteria included birth weight < 1500 gram, gestational age < 32 weeks, major chromosomal anomalies or neural tube defects, or multiple births. A total of 480 children and their mothers were recruited and assessed in the laboratory during infancy.
The sample evaluated in this study was comprised of the 337 children and their mothers or current primary caregivers who were assessed at 7.5 years of age (M = 7.8, SD = 0.3). A comparison of the 7.5-year study participants (70.0%) with those lost to follow-up (30.0%) indicated no differences in SES, maternal educational level, alcohol consumption at conception, drug use during pregnancy, or psychopathology (all p’s > .20). Retention rates were similar in the exposed (72.1%) and non-exposed (66.3%) groups, χ2(1) = 1.60, n.s.. The only significant difference was that the mothers who participated in the follow-up were slightly older, M = 26.7 compared with 25.5 years for non-participants, t (478) = −2.07, p < .05.
To examine the degree to which the impact of socioenvironmental risk may differ depending on prenatal exposure history, two groups were created based on prenatal alcohol and cocaine exposure. The “exposed” group consisted of 227 children whose mothers reported consuming ≥ 0.5 oz AA/day (the equivalent of ≥ 1 standard drink/day) at time of conception or using cocaine at least once per week during pregnancy. The “non-exposed” group consisted of 110 children whose mothers drank < 0.5 oz AA/day with no or, at most, rare, minimal cocaine use during pregnancy. Most of the prenatal alcohol exposure in the exposed group was in the moderate range (M = 1.3 oz AA/day, SD = 2.3), and only three children met criteria for a diagnosis of FAS. When averaged across pregnancy, cocaine was used regularly (≥ 1 day/week) by 7.4% of the mothers.
At the 7.5-year visit, the biological mother was the primary caregiver for a large majority of the children (see Table 1). The primary caregivers for the remaining children were the father (1.3%) or a family relative, usually a grandmother (8.5%) or aunt (1.3%); one child (0.3%) had been adopted by foster parents. Median SES for both the exposed and non-exposed groups fell in the fourth level on the Hollingshead Scale (1975), the second lowest of five levels on the scale. Differences between the non-exposed and exposed groups were observed on four demographic measures. The mothers of the exposed children were older, higher in parity and less likely to be married, and the exposed children were more likely to be male. Because the difference in parity was a consequence of the difference in primary caregiver age, parity was not considered further. Caregiver age and marital status and child gender were included in the regression analyses described below, where appropriate, to control for their potential confounding effects.
Table 1.
Sample Characteristics
| Non-exposed (n = 110)
|
Exposed (n = 227)
|
t or χ2 | |||
|---|---|---|---|---|---|
| M or % | SD | M or % | SD | ||
| Maternal/primary caregiver | |||||
| Socioeconomic statusa,b | 26.5 | 9.7 | 25.4 | 11.7 | 0.9 |
| Group 1 (%) | 0.0 | 1.3 | |||
| Group 2 (%) | 13.6 | 15.0 | |||
| Group 3 (%) | 21.8 | 14.5 | |||
| Group 4 (%) | 38.2 | 30.0 | |||
| Group 5 (%) | 26.4 | 39.2 | |||
| Ageb | 33.3 | 9.4 | 37.8 | 9.6 | −4.1** |
| Parityc | 1.0 | 1.2 | 1.5 | 1.6 | −3.7** |
| Verbal competencec,d | 74.1 | 12.7 | 73.4 | 14.0 | 0.4 |
| Marital status (% married)b | 25.5 | 15.9 | 3.8* | ||
| Welfare (% receiving)b | 63.6 | 72.2 | 2.6 | ||
| Child | |||||
| Primary caregiver (% biological mother) | 90.0 | 83.3 | 2.7 | ||
| Gender (% male) | 49.1 | 62.6 | 5.5* | ||
Primary caregiver.
Biological mother.
Peabody Picture Vocabulary Test-Revised (Dunn & Dunn, 1981).
p < .05.
p < .01.
Procedures
All child assessments were conducted by examiners who were blind with respect to the child’s prenatal exposure and risk status. Procedures were approved by the Wayne State University Human Investigation Committee. Written informed consent was obtained from the mother/primary caregiver at recruitment and at the 7.5-year assessment, and oral assent from the child at 7.5 years. Child cognitive performance was assessed in the laboratory, and behavior problems were rated by the child’s classroom teacher. The primary caregiver was interviewed in detail about her current alcohol and drug consumption and other socioenvironmental factors and was administered a test of verbal competence and a test assessing severity of alcohol-related problems. The primary caregiver received monetary compensation and a photo of the child, and the children received a small gift for their participation.
Assessment Battery
Eight risk variables in the child’s social and family environment were included in the analyses reported here. Six of these constructs were adapted from Sameroff et al. (1993), which is a landmark study in examining the effects of cumulative risk on child development. Given the focus of this study on prenatal substance abuse exposure, current substance abuse and parental violence, which often accompanies substance abuse, were also included in the analyses. In order to calculate the cumulative risk index, each of these variables was dichotomized using the criteria listed below. Missing data were estimated by using the group median of the exposure group that the participant belonged to. Table 2 summarizes the risk cut-off criteria and presents the percentage of each group that was categorized as high risk.
Table 2.
Risk Factors and Cut-Off Scores
| Measure | Risk cut-off | % in risk group
|
Coefficient of variation
|
||||
|---|---|---|---|---|---|---|---|
| Non- exposed | Exposed | χ2 | Non-exposed | Exposed | |||
| Socioeconomic status | Hollingshead scalea | < 20 | 25.5 | 39.2 | 6.18* | .36 | .46 |
| Number of children | --- | ≥ 4 | 13.6 | 11.9 | .21 | .93 | .89 |
| Presence of father | Lives with biological father | Father absent | 82.7 | 80.2 | .31 | ||
| Stressful life events | Life Events Scaleb | Highest quartile | 22.7 | 28.2 | 1.14 | .78 | .77 |
| Depression | Beck Depression Inventoryc | ≥ 16 | 11.8 | 18.5 | 2.42 | 1.00 | .83 |
| Parent-child interaction | HOMEd | Lowest quartile | 26.4 | 26.0 | .01 | ||
| Parental violence | Conflict Tactics Scalee | 95 %ile U.S. norm | 39.1 | 43.6 | .62 | 1.88 | 1.63 |
| Current substance abuse | MASTf | ≥ 5 | 20.9 | 50.7 | 27.12** | ||
| or cocaine use | ≥ 1 day/week | ||||||
| or alcohol use | ≥ 4 drinks/day | ||||||
Adapted from Holmes & Rahe (1967).
Home Observation for Measurement of the Environment (Caldwell & Bradley, 1984).
Conflict Tactics Scale (Straus, 1979).
Michigan Alcoholism Screening Test (Selzer, 1971).
p < .05.
p < .01.
Socioeconomic status (SES)
Numerous studies have demonstrated that lower SES is associated with a wide range of poorer outcomes in children, including cognitive and socioemotional functioning (e.g., Bradley & Corwyn, 2002) and neurocognitive abilities (e.g., Noble, McCandliss, & Farah, 2007). In this study, SES was computed on the Hollingshead (1975) scale separately for the primary caregiver and partner based on their educational attainment and occupational status, which was averaged together if both were employed; if not, SES was based on the educational attainment and occupational status of the head of household. The continuous Hollingshead SES measure ranges from 8 to 66, which is then grouped into five SES levels; when SES was dichotomized for risk categorization, a score < 20—the lowest of the five Hollingshead SES levels—was classified as high risk.
Number of children at home
It has been shown that having a larger number of children in the home is associated with poorer child cognitive outcome (Luster & McAdoo, 1994). In our study, data on number of children under age 18 years living in the household were obtained. Following Sameroff et al. (1993), four or more children was considered as high risk.
Presence of father at home
The primary caregiver was asked whether the child lives with his/her father. Although we obtained information regarding the presence of biological fathers, stepfathers, and any father figures (e.g., grandfathers, uncles), the absence of the biological father was used as the high risk category criterion in this study based on our finding that only the presence of the biological father protected against psychosocial risk in this population (Yumoto et al., 2002). In this sample, it was common for children to have second households where they spend weekends or holidays. However, the biological father was considered to be “present” only when the child lived with him in the primary household.
Stressful life events
Negative life events experienced by primary caregivers (e.g., job loss, divorce, or illness) have been found to be related to children’s depression (Compas, Howell, Phares, Williams & Giunta, 1989), delinquency (Tolan, 1988), aggression (Attar, Guerra & Tolan, 1994), and cognitive performance (Krishnakumar & Black, 2002). Information was obtained using an adaptive version of the Schedule of Recent Events (Holmes & Rahe, 1967), on which primary caregivers rated any of 43 events they experienced during the preceding year in terms of how stressful they found each event. The continuous measure of life stress consisted of the sum of these ratings; a score in the highest quartile, was used as the risk cut-off. One case was missing data on the Schedule of Recent Events and was estimated by using a group median.
Depression
Maternal depression has been shown to be related to children’s behavior problems, including aggression, anxiety, and social incompetence (Dodge, 1990) and externalizing problem behaviors (Krishnakumar & Black, 2002). To assess maternal/primary caregiver depression, the present study used the Beck Depression Inventory (BDI; Beck & Steer, 1987), which was also highly correlated with the Global Severity Index on the Symptoms Checklist 90-Revised (SCL-90-R; Derogatis, 1992) in this sample (r = .73, p < .001). We used the BDI score of 16 or above, which is considered indicative of moderate to severe depression, as the high risk cut-off.
Parent-child interaction
Quality of the home environment, as measured by the elementary age version of the Home Observation for Measurement of the Environment (HOME; Caldwell & Bradley, 1984), has been found to be related to child cognitive functioning among 6-to 9-year-old African American children (Luster & McAdoo, 1994). In addition, emotional quality of the parent-child relationship on the elementary age HOME was significantly related to both internalizing and externalizing behaviors in children aged 6 to 10 years (Wasserman, Miller, Pinner, & Jaramillo, 1996). In our study, scores on two subscales from the HOME —Verbal Responsivity and Emotional Climate—were used to assess quality of primary caregiver-child interaction. The parent-child interaction variable was constructed by combining the standardized scores on these two subscales. Both subscales are comprised largely of examiner ratings based on the observation of the emotional quality of interaction between the primary caregiver and the child. Although mean interobserver reliability was not available for these specific items at this age, previous interobserver reliability on the HOME for this cohort averaged 95% (range = 88–100%) (Jacobson, Jacobson, Sokol, Martier, & Ager, 1993) and the HOME data obtained at this age were predictive of child IQ (Jacobson et al., 2004), as reported in other studies. A score in the lowest quartile of the sample distribution, indicating low sensitivity and cold emotional climate at home, was used to define the risk category. For two missing cases, the group median was used to estimate missing values.
Parental violence
Exposure to domestic violence, as measured by the Conflict Tactics Scale (CTS; Straus, 1979), has been linked to increased internalizing and aggressive behavior problems (Holden & Ritchie, 1991) and increased general psychopathology among 6- to 12-year-olds (McCloskey, Figueredo, & Koss, 1995). The CTS assesses the incidence and severity of verbal and physical conflict between the primary caregiver and his or her partner. Scores on the CTS Violence scale falling in the top 5% of the national norms for this scale were considered high risk.
Primary caregiver’s current substance abuse
Parental substance abuse has been considered a significant risk factor that negatively impacts on children’s cognitive functioning and is related to increased externalizing and internalizing behaviors (Wilens et al., 2002; Nunes et al., 1998; Puttler, Zucker, Fitzgerald & Bingham, 1998; Weinberg, 1997; Moss, Vanyukov, Majumder, Kirisci, & Tarter, 1995). We assessed current substance abuse by the primary caregiver based on the following three measures: (1) frequency of alcohol use, (2) frequency of opiate and cocaine use, and (3) Michigan Alcoholism Screening Test (MAST; Selzer, 1971) score. The MAST is a 25-item self-report measure widely used to identify problems related to alcohol consumption, such as alcohol-related loss of job or friendship or arrest for driving while intoxicated. A positive MAST score (≥ 5) indicates that the respondent has experienced psychosocial and/or physiological problems related to alcohol abuse and is alcoholic or at risk for alcoholism. The continuous variable used to measure current substance abuse was created by averaging standardized scores for oz AA/day, days per month of opiate and cocaine use, and the MAST score obtained at the 7.5-year follow-up assessment. For six cases that were missing one or two of the variables mentioned above, the median of the standardized scores for each exposure group were used to estimate missing values. The high risk group for current substance abuse was comprised of primary caregivers who currently drank at least 2 oz AA (four or more standard drinks)/day, currently used cocaine ≥ once/week, or scored 5 or more on the MAST.
Table 2 presents the coefficients of variation (CV; standard deviation/mean) for the eight risk factors in the non-exposed and exposed groups to assess potential restriction of range. Of the five non-standardized continuous socio-environmental risk variables, CV for the exposed group was slightly larger on SES (0.5, compared with 0.4); slightly smaller on maternal depression (0.8, compared with 1.0) and parental violence (1.6, compared with 1.9); and very similar on the remaining measures. With regard to the outcome measures, CV for the exposed group was very similar for the three IQ measures, slightly lower for Externalizing behavior (1.1, compared with 1.2) and slightly higher for Internalizing behavior (1.1, compared with 1.0).
In addition to the eight socioenvironmental risk factors, verbal competence of the child’s biological mother was assessed on the Peabody Picture Vocabulary Test-Revised (PPVT-R; Dunn & Dunn, 1981), which is strongly correlated with WAIS Full Scale IQ (r = .72) and has been validated for use with this cohort (Jacobson, Jacobson, & Frye, 1991). PPVT-R score was used as a covariate to test the degree to which the socioenvironmental risk factors impact on cognitive development over and above the contribution of maternal verbal intellectual competence.
Outcome Variables
The Wechsler Intelligence Scale for Children: Third Edition (WISC-III; Wechsler, 1991) was used to assess the child’s cognitive functioning. The WISC-III yields Full Scale IQ (FSIQ), Verbal IQ (VIQ), and Performance IQ (PIQ) scores. The child’s classroom teacher was sent the Teacher Report Form (TRF; Achenbach, 1991) to complete and received a small gift when the questionnaire was returned. Four summary measures derived from the TRF were used in the analyses: Aggressive behavior problems; Delinquent behavior problems; Externalizing total score, which is comprised of the Aggressive and Delinquent behavior problem scales; and Internalizing total score, which consists of the Withdrawn, Somatic Complaints, and Anxious Depressed scales.
Data Analyses
Dichotomous risk variables were constructed from the social and family variables using the criteria described above. A cumulative risk index was then computed by assigning a score of 1 for the presence of each risk factor. Cumulative risk was defined as the total number of risk factors out of the eight examined in this study.
All analyses were conducted separately for the substance-exposed and non-exposed groups. Multiple regression analyses were conducted using the eight risk variables as continuous measures to examine the associations of social and family variables with the child outcome variables. Hierarchical regression analyses were then conducted to control for three additional sociodemographic potential confounding variables—primary caregiver’s age and marital status and child gender—by including all of the risk variables in the first step and the additional potential confounders in the second step.
Following these analyses, a correlational analysis was conducted to examine the relation of cumulative risk to the outcome variables. VIQ and PIQ scores were then examined in relation to the cumulative risk score in analyses of covariance (ANCOVAs) to detect whether there were thresholds above which performance is affected particularly strongly, after controlling for the biological mother’s verbal competence. The cumulative risk index was recoded into four groups (0–1, 2, 3, 4 or more) to ensure a sufficient number of cases in each group. Analyses of variance (ANOVAs) were conducted to assess whether there were threshold effects in the relation of cumulative risk to the behavior problem outcomes assessed. Post hoc comparisons were based on least-square difference (LSD) analyses.
RESULTS
Table 3 presents correlations among eight risk factors for each group. The highest correlation among the risk factors in both the non-exposed and exposed groups was between the primary caregiver’s depression and stressful life events in the past year. In the non-exposed group, the next highest correlations were between stressful life events and parental violence and between current substance abuse problems and parental violence. In the exposed group, the next highest correlation was between current substance abuse problems and stressful life events. In the exposed group, SES, primary caregiver’s depression, and primary caregiver’s current substance abuse problem were all significantly correlated with the responsiveness and emotional climate at home, whereas none of these risk factors were associated with quality of home environment in the non-exposed group. Another difference observed between two groups was in the relation between the primary caregiver’s depression and substance abuse, which was significant only in the exposed group.
Table 3.
Correlations among Risk Factors
| SES | Number of children | Presence of father | Stressful life events | Depression | Parent-child interaction | Parental violence | Current substance use | |
|---|---|---|---|---|---|---|---|---|
| Socioeconomic status (SES) | --- | −.23* | .12 | .14 | −.02 | .10 | .02 | .02 |
| Number of children | −.05 | --- | .18† | .10 | .05 | −.18† | −.05 | −.02 |
| Presence of father | .17* | .06 | --- | .09 | −.08 | .10 | −.02 | .01 |
| Stressful life events | .02 | .14* | .09 | --- | .48*** | −.08 | .30** | .21* |
| Depression | −.09 | .06 | .06 | .54*** | --- | −.06 | .29** | .11 |
| Parent-child interaction | .25*** | −.07 | .03 | −.05 | −.20** | --- | .02 | −.04 |
| Parental violence | −.12† | .11† | .09 | .31*** | .31*** | −.11† | --- | .30** |
| Current substance abuse | −.08 | −.03 | .13† | .33*** | .32*** | −.22** | .31*** | --- |
Note. Values are Pearson r’s. Values below the diagonal are from the exposed group and above the diagonal are from the non-exposed group.
p < .10.
p < .05.
p < .01.
p < .001.
When the risk factors were examined as continuous measures, the non-exposed and exposed groups differed on only three. Mothers of the substance-exposed children were more likely to have current substance abuse problems, t (335) = −7.72, p < .001, be depressed, (t (335) = −2.68, p < .01), and report more stressful life events in the previous year, t (335) = −2.14, p < .05. Although we have previously reported effects of prenatal alcohol exposure on IQ (Jacobson et al., 2004) and TRF behavior problems (Jacobson et al., 2006), in these analyses, no differences in mean IQ, Delinquency, Aggression, or Internalizing or Externalizing behavior problem scores were found between the non-exposed and exposed groups because effects of prenatal alcohol and cocaine exposure were combined in this study of environmental risk, thereby presumably masking their specific teratological impact (see Table 4).
Table 4.
Mean IQ and TRF Scores (SDs) by Exposure Group
| Non-exposed | Exposed | t value | |
|---|---|---|---|
| WISC-IIIa | |||
| Full Scale IQ | 85.6 (13.1) | 83.6 (11.9) | 1.4 |
| Verbal IQ | 89.0 (12.9) | 86.6 (12.1) | 1.6 |
| Performance IQ | 84.5(13.6) | 83.2 (12.7) | 0.9 |
| TRFb | |||
| Delinquency | 1.9 (2.4) | 2.4 (2.8) | −1.6 |
| Aggression | 8.0 (10.2) | 10.3 (11.8) | −1.5 |
| Externalizing | 9.9 (12.0) | 12.7 (14.1) | −1.6 |
| Internalizing | 7.1 (6.8) | 6.1 (6.4) | 1.3 |
n = 110 for Non-exposed and 227 for Exposed.
n = 80 for Non-exposed and 171 for Exposed.
Multiple Regression Analyses
Table 5 summarizes the results from the multiple regression analyses. The simple correlations relating the cumulative risk index score with the outcome variables are shown in the bottom row. The principal predictors of FSIQ for the non-exposed group were number of children living at home and parental violence, with an effect of SES falling short of significance. For the children in the exposed group, SES and parental current substance abuse were the principal predictors of FSIQ. Similar patterns were observed with VIQ and PIQ, except that having a biological father living at home was negatively related to PIQ in the exposed group, β = −.14, p = .04, and, for the non-exposed group, parental violence was related to VIQ, β = −.25, p = .01, but not to PIQ. The Multiple R based on the eight discrete risk factors measured as continuous variables was markedly stronger than the r for cumulative risk index for both groups. Moreover, in each regression, the Multiple R was markedly stronger than the individual standardized regression coefficients, indicating that the combined effect of those risk factors measured as continuous variables exceeds that associated with any of the individual risk factors.
Table 5.
Full Scale IQ and TRF Scores in Non-exposed vs. Exposed Groups
| Groups | Full Scale IQ
|
Externalizing Total Score
|
Delinquent Behavior
|
Aggressive Behavior
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-Exposed (n = 110)
|
Exposed (n = 227)
|
Non-exposed (n = 80)
|
Exposed (n = 171)
|
Non-Exposed (n = 80)
|
Exposed (n = 171)
|
Non-Exposed (n = 80)
|
Exposed (n = 171)
|
|||||||||
| r | β | r | β | r | β | r | β | r | β | r | β | r | β | r | β | |
| SES | .25** | .18† | .23** | .22** | .05 | .09 | .02 | .06 | −.06 | .01 | −.09 | −.03 | .07 | .10 | .05 | .08 |
| Number of children | −.28** | −.24** | −.10† | −.10 | .03 | .03 | .05 | .05 | .13 | .14 | .10† | .09 | .00 | −.00 | .03 | .03 |
| Presence of father | −.11 | −.11 | −.10† | −.12† | −.12 | −.16 | −.11† | −.12 | −.15† | −.20† | −.12† | −.13† | −.11 | −.15 | −.11† | −.12 |
| Stressful life events | .11 | .16 | .02 | .04 | −.03 | .06 | .00 | .04 | −.09 | −.03 | .06 | .03 | −.01 | .07 | −.01 | .04 |
| Depression | .06 | .06 | .02 | .10 | −.18† | −.27* | −.06 | −.10 | −.16† | −.23† | .02 | −.08 | −.17† | −.26* | −.08 | −.10 |
| Parent-child interaction | .11 | .08 | .19** | .12† | −.22* | −.26* | −.15* | −.16* | −.24* | −.24* | −.25** | −.20* | −.20* | −.24* | −.12† | −.15† |
| Parental violence | −.13 † | −.21* | −.05 | .02 | .03 | .10 | −.08 | −.11 | .01 | .10 | .04 | −.07 | .04 | .10 | −.11† | −.12 |
| Current substance abuse | −.04 | −.02 | −.16** | −.15* | −.04 | −.05 | .07 | .10 | −.09 | −.09 | .24** | .23* | −.02 | −.04 | .03 | .06 |
| Multiple R | .42** | .35** | .36** | .25* | .39** | .36** | .34** | .24* | ||||||||
| Cumulative risk index | −.19** | −.15* | .06 | .06 | .12 | .20** | .04 | .03 | ||||||||
p < .10.
p < .05.
p < .01.
Differential patterns of risk for the TRF scores were also observed for the non-exposed and exposed groups, with one notable exception. The primary caregiver’s responsivity and emotional climate at home predicted Externalizing behavior problems (i.e., Delinquent and Aggressive behaviors, and the Externalizing total score) for both groups. Whereas the primary caregiver’s depression was related to the Externalizing behaviors in the non-exposed group, the primary caregiver’s substance use problems were related to Delinquent behavior problems only for the children in the exposed group. Internalizing behavior problems were not related to any of the individual risk factors, and the Multiple R for the regression relating the eight risk factors to Internalizing total score was not significant for either group.
The regression analyses shown in Table 5 were rerun to control for primary caregiver’s age, marital status, and the gender of the child, in order to examine whether those demographic variables alter the effects observed in the regression. The results were essentially unchanged, except that the effects of the primary caregiver’s responsivity and emotional climate at home on Delinquent and Aggressive behaviors were reduced somewhat in the non-exposed group when the gender of the child was included in the analyses (Externalizing total score was reduced from β = −.26 to −.18; Delinquent behavior score, from β = −.24 to −.20; Aggressive behavior score, from β = −.24 to −.17), suggesting that the effect of quality of parenting on Externalizing was possibly due, in part, to the fact that girls, who are less prone to exhibit Externalizing behavior, were provided with more optimal interaction and warmer emotional climate at home in the non-exposed group.
Cumulative Risk Index
The cumulative risk index was calculated by counting number of risk factors the child experienced out of eight risk factors examined. Children in the exposed group experienced somewhat more risk factors (M = 3.0, Range = 0–7) than those in the non-exposed group (M = 2.4, Range = 0–6; t = 14.6, p < .05). The correlations of the cumulative risk index with FSIQ and the behavioral outcomes are shown in the bottom row of Table 5. As expected, a higher cumulative risk index was associated with lower FSIQ in both groups. Although the Multiple R from the eight-variable regression was significantly related to all child outcome measures except the Internalizing total score, the cumulative risk index was not related to the Externalizing total score or the Aggressive behavior score in either group. The cumulative risk index was related to the Delinquent behavior score only in the exposed group. The Internalizing total score was also related to the cumulative risk index score only in the exposed group (r = .20, p < .01, compared with r = −.02, n.s., in the non-exposed group).
Threshold Effects
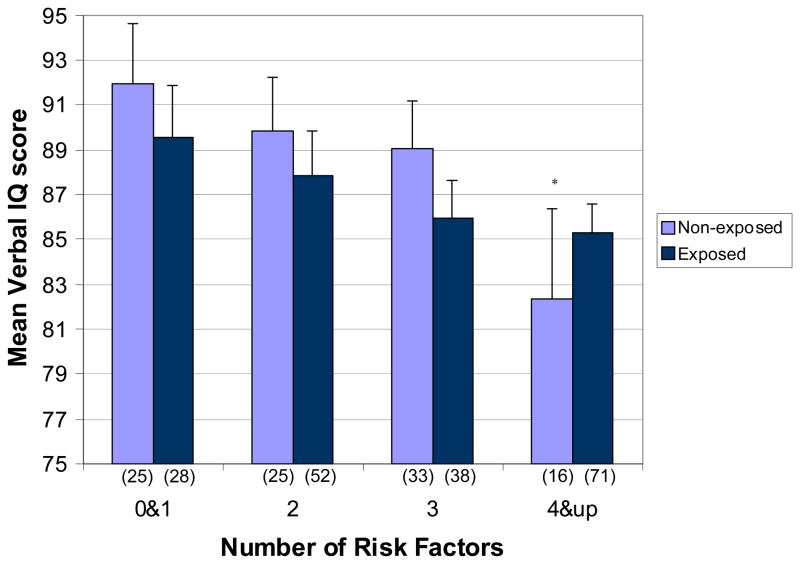
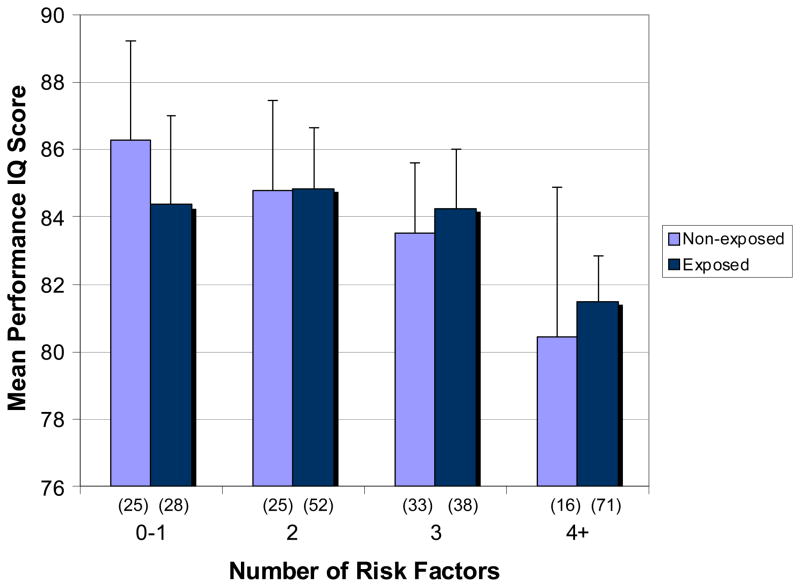
The ANCOVAs revealed different patterns for the exposed and non-exposed groups on VIQ (see Figure 1). The VIQ scores among the children who were not exposed to alcohol or drugs during pregnancy dropped dramatically in the presence of four or more risk socioenvironmental risk factors (LSD p = .05, for 3 vs. 4 or more risk factors), whereas the VIQ in the exposed group decreased gradually as the number of risk factors they had experienced increased (r =−.13, p = .06). By contrast, with the PIQ, both groups showed a gradual linear decrease as the number of risk factors increased (see Figure 2; r’s = −.15, p = .10, and −.14, p = .04, for the non-exposed and exposed groups, respectively).
Figure 1.
Mean Verbal IQ score as a function of a number of risk factors in non-exposed and exposed groups. Numbers in parentheses are sample sizes for each subgroup. Vertical lines depict standard errors of the means. *p < .05 based on LSD post hoc test for 3 vs. 4 or more risk factors in non-exposed group.
Figure 2.
Mean Performance IQ score as a function of a number of risk factors in non-exposed and exposed groups. Numbers in parentheses are sample sizes for each subgroup. Vertical lines depict standard errors of the means.
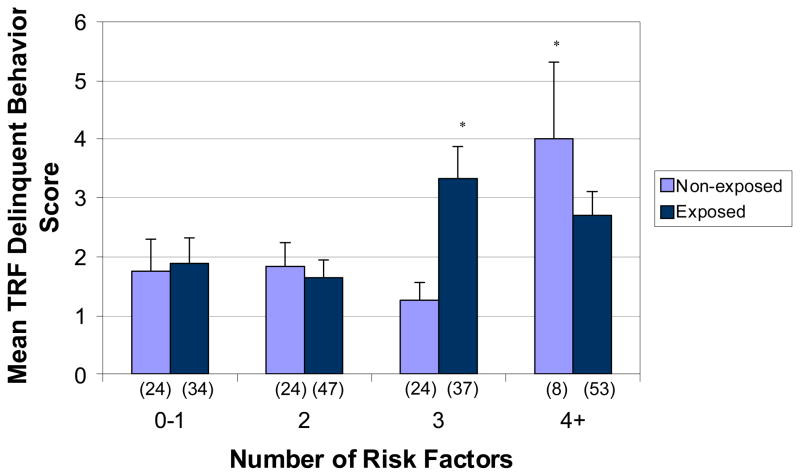
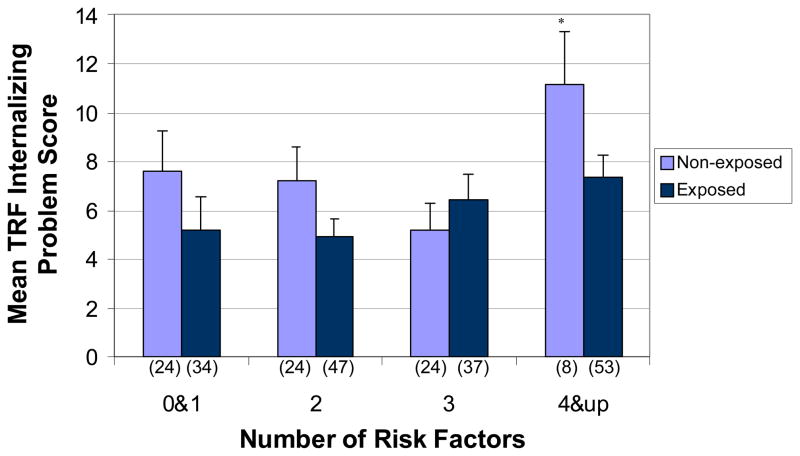
Differential patterns were also observed for the TRF scores. Figure 3 shows that Delinquent behavior observed by the child’s teacher significantly increased with four or more risk factors in the non-exposed group (LSD p < .01, for 3 vs. 4 or more risk factors). By contrast, Delinquent behavior significantly increased after three risk factors in the exposed group (LSD p < .01, for 2 vs. 3 risk factors). No threshold effects were observed for Aggressive behavior assessed by teachers in either group. As shown in Figure 4, the number of internalizing problems reported by teachers increased significantly with four or more risk factors in the non-exposed group. (LSD p = .03, for 3 vs. 4 or more risk factors) In the exposed group, increasing risk was associated with a gradual increase in Internalizing total score (r = .20, p < .01).
Figure 3.
Mean TRF Delinquent Behavior score as a function of a number of risk factors in non-exposed and exposed groups. Numbers in parentheses are sample sizes for each subgroup. Vertical lines depict standard errors of the means. *p < .01 based on LSD post hoc test for 3 vs. 4 or more risk factors in non-exposed group and for 2 vs. 3 risk factors in exposed group.
Figure 4.
Mean TRF Internalizing Problem score as a function of a number of risk factors in non-exposed and exposed groups. Numbers in parentheses are sample sizes for each subgroup. Vertical lines depict standard errors of the means. *p < .05 based on LSD post hoc test for 3 vs. 4 or more risk factors in non-exposed group.
DISCUSSION
A major aim of this study was to examine the impact of prenatal exposure to alcohol and/or cocaine on vulnerability to risks encountered in the child-rearing environment. When we previously examined the data looking specifically at moderate to heavy exposure to alcohol during pregnancy on IQ and Externalizing behaviors, we reported significant effects of fetal alcohol exposure on IQ, working memory, number processing and a range of behavioral endpoints on the TRF, using continuous measures of alcohol exposure (Jacobson et al., 2004; Jacobson et al., 2006; Burden, Jacobson, & Jacobson, 2005; Burden, Jacobson, Sokol, & Jacobson, 2005; Jacobson et al., 2003). These and other infant effects were specific to prenatal alcohol exposure (Jacobson, 1998) and different from those found for heavy cocaine or other teratogenic exposures (Jacobson et al., 1998) for this cohort. The lack of group differences reported here on these outcomes reflects the inclusion of cocaine exposed children with little or no alcohol exposure in the high exposure group in this study that was designed to focus on the moderating effects of prenatal substance exposure, thereby obscuring the prenatal alcohol effects. Thus, as expected, the prenatally exposed children as a group did not differ from the non-exposed group on the developmental outcomes examined—IQ and Internalizing and Externalizing behavior problems. Despite the similar mean IQ and behavior problem scores, however, the data revealed differences in vulnerability to environmental risk operates in these two groups, thereby supporting the fetal patterning of later development hypothesis. Not surprisingly, current maternal substance abuse impacted more strongly on the IQ scores of the prenatally-exposed children, presumably due to its more limited range in the non-exposed group. By contrast, number of children in the household was related to FSIQ only in the non-exposed group. Being raised in a smaller family had a beneficial effect on cognitive performance only for the children not exposed prenatally to alcohol or cocaine.
The findings from previous studies regarding the applicability of cumulative risk models of the impact of socioenvironmental factors on development in African American children have been inconsistent due, in part, to limited sample sizes. Our multiple regression data (Table 5) make clear, however, that the joint effect of multiple environmental risks markedly exceeds that of any of the individual risk factors. On the other hand, the cumulative risk index, which is based on dichotomizing each of the risk factors and is, therefore, generally less sensitive (Burchinal et al., 2000), was significant for the cognitive outcomes for both the substance-exposed and non-exposed children. For the exposed children, the cumulative risk was also related to Delinquent and Internalizing behaviors. We note that the term “delinquent” is not usually used with early elementary school-age children and that the children’s scores on the TRF delinquency scale were low. The principal TRF delinquent behaviors endorsed by the teachers were breaking school rules and lying or cheating. The data show that the cumulative risk was related to increased incidence of these behaviors at 7.5 years of age among the children exposed to substances prenatally.
It is of interest that the cognitive and behavioral endpoints examined in this study were influenced by different sets of risk factors. Whereas SES, family size, parental substance abuse, and parental violence were the principal risk factors for FSIQ, having an emotionally responsive primary caregiver and a warm emotional climate at home was the most consistent predictor of lower levels of delinquent and aggressive behaviors at school across groups. The presence of the biological father in the home also appears to be associated with reduced delinquent behavior. The inverse relation between maternal depression and externalizing behaviors in the non-exposed group, which was not predicted, suggests that family temperament or modeling parental behaviors may influence whether the child’s psychosocial problems will be expressed in the form of delinquent or aggressive behaviors. The identification of the parent-child interaction as the most important socioenvironmental predictor of externalizing behavior problems is consistent with data from another African American sample (Jones et al., 2002). Just as much emphasis has been placed on the importance of intellectual stimulation and emotional support for cognitive development in middle class Caucasian samples, quality of parenting also appears to be most important for socioemotional development and behavioral outcomes for inner city, African American children.
In the Isle of Wight study, Rutter (1979) found that the relation of the number of risk factors to which the child was exposed to developmental outcome was nonlinear, with a threshold of four or more. Whereas most children are relatively unaffected by three or fewer socioenvironmental risk factors, Rutter’s data indicate that exposure to multiple risks interacts so that their effect on development becomes synergistic. It is of particular interest that, similar to Caucasian, middle class cohorts, four or more risks emerged as a threshold in our dose-response analyses of the African American children in our cohort who were not exposed prenatally to alcohol or cocaine for three important outcomes—verbal IQ, Delinquent behaviors, and Internalizing behaviors.
The multiple regression and correlational data in Table 5 did not indicate increased vulnerability to socioenvironmental risk in the prenatally exposed group; the Multiple R’s for the regressions and correlation coefficients for the cumulative risk index were generally slightly higher in the non-exposed group. Since the coefficients of variation for the risk factors were similar for the two groups (Table 2), this difference in effect size cannot be attributed to restriction of range in the exposed group. By contrast, the data from the dose-response analyses indicate that the dampening of the effect of exposure to three or fewer risk factors in the non-exposed group was not found in the prenatally-exposed group. For most endpoints, each additional risk factor was associated with poorer cognitive performance and increased behavior problems in a linear fashion among the substance-exposed children. Moreover, for the one endpoint where a threshold was observed—Delinquent behavior—behavior problems increased at a lower threshold (≥3 risk factors) than among the non-exposed children. Another indication of increased vulnerability is the finding that cumulative risk was associated with increased Internalizing behavior problems only for the prenatally-exposed children. In addition, the data in Table 3 suggests that multiple risk factors are more likely to occur together in the families of the substance-exposed children. Although parental substance abuse, life stress, and maternal depression are moderately intercorrelated in both groups, for the prenatally-exposed children quality of parenting, the principal protective factor for Externalizing behavior problems, was also more correlated with SES, caregiver depression, and substance abuse, increasing the likelihood of the co-occurrence of multiple risks for the children in that group.
In interpreting the findings, certain limitations of the study should be noted. Because the focus of the study was on economically disadvantaged, inner-city, African American families, one must be cautious about generalizing from these findings to other populations, who may have greater access to community or other forms of social support. Since prenatal substance exposure is associated with prematurity and reduced birth weight, the exclusion of very low birth weight and severe preterm deliveries may have reduced the number of more severely affected children in the cohort. In addition, although moderating effects of gender on externalizing behaviors have been reported in children prenatally exposed to alcohol and cocaine (Nordstrom Bailey et al., 2005), we did not examine the interaction between gender and prenatal substance exposure in this study, because the cell sizes in such analyses would have been unduly small. Nordstorm Bailey et al.’s data also suggest that prenatal alcohol exposure may moderate prenatal cocaine effects on teacher-reported child externalizing behavior. We did not examine the effects of prenatal alcohol and cocaine exposure separately, however, in order to optimize cell sample sizes and because our hypothesis regarding fetal patterning focused on the impact of substance exposure generally on vulnerability to socioenvironmental risk.
Despite these limitations, these data lend support to findings of synergistic effects among multiple socioenvironmental risk factors reported in previous studies and provide evidence that four or more risks may be an important threshold for non-substance-exposed, inner city African American children as well as the Caucasian children examined in previous studies. These data also provide support for the prediction from the fetal patterning of disease model that prenatal exposure to alcohol and/or cocaine can increase vulnerability to socioenvironmental risk. Based on the cumulative risk index and dose-response data, vulnerability to the adverse effects of socioenvironmental risk appears to be enhanced particularly on two endpoints—delinquent and internalizing behaviors.
Acknowledgments
This research was funded by grants R01-AA06966, R01-AA09524, and P50-AA07606 from the National Institute on Alcohol Abuse and Alcoholism, with supplemental support from a Minority Biomedical Research Support grant S06-RR08167 from the National Institutes of Health, and a grant from the Joseph Young, Sr., Fund from the State of Michigan. We thank Robert J. Sokol, Susan Martier, Joel Ager, and Erawati Bawle, our collaborators on this research; Douglas Barnett, for his suggestions; Neil Dodge, Lisa Chiodo, Renee Sun, Jeannine Tell, Brenda Tuttle, Jennifer Jester, and Raluca Corobana, who helped collect and analyze the data; and the mothers/caregivers and children who participated in the study. This study is based on a master’s thesis completed by Chie Yumoto at Wayne State University.
Contributor Information
Chie Yumoto, Department of Psychology, Wayne State University.
Sandra W. Jacobson, Department of Psychiatry and Behavioral Neurosciences, Wayne State University
Joseph L. Jacobson, Department of Psychiatry and Behavioral Neurosciences, Wayne State University
References
- Achenbach TM. Integrative guide for the 1991 CBCL/4–18, YSR and TRF profiles. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Alessandri SM, Bendersky ML. Cognitive functioning in 8 to 18 month old drug-exposed infants. Developmental Psychology. 1998;34:565–573. doi: 10.1037//0012-1649.34.3.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attar BK, Guerra NG, Tolan PH. Neighborhood disadvantage, stressful life events, and adjustment in urban elementary-school children. Journal of Clinical Child Psychology. 1994;23:391–400. [Google Scholar]
- Beck AT, Steer RA. BDI, Beck Depression Inventory: Manual. SanAntonio, TX: Psychological Corporation; 1987. [Google Scholar]
- Bendersky M, Bennett D, Lewis M. Aggression at age 5 as a function of prenatal exposure to cocaine, gender, and environmental risk. Journal of Pediatric Psychology. 2006;31:71–84. doi: 10.1093/jpepsy/jsj025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley RH, Corwyn RF. Socioeconomic status and child development. Annual Review of Psychology. 2002;53:371–399. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- Burden MJ, Jacobson SW, Jacobson JL. The relation of prenatal alcohol exposure to cognitive processing speed and efficiency in childhood. Alcoholism: Clinical and Experimental Research. 2005;29:1473–1483. doi: 10.1097/01.alc.0000175036.34076.a0. [DOI] [PubMed] [Google Scholar]
- Burden MJ, Jacobson SW, Sokol RJ, Jacobson JL. Effects of prenatal alcohol exposure on attention and working memory at 7.5 years of age. Alcoholism: Clinical and Experimental Research. 2005;29:443–452. doi: 10.1097/01.alc.0000156125.50577.ec. [DOI] [PubMed] [Google Scholar]
- Burchinal MR, Roberts JE, Hooper S, Zeisel SA. Cumulative risk and early cognitive development: A comparison of statistical risk models. Developmental Psychology. 2000;36:793–807. doi: 10.1037//0012-1649.36.6.793. [DOI] [PubMed] [Google Scholar]
- Caldwell B, Bradley R. Home Observation for Measurement of the Environment. Little Rock, AR: University of Arkansas at Little Rock; 1984. [Google Scholar]
- Carmichael Olson H, Feldman JJ, Streissguth AP, Sampson PD, Bookstein FL. Neuropsychological deficits in adolescents with fetal alcohol syndrome: Clinical findings. Alcoholism: Clinical and Experimental Research. 1998;22:1998–2012. [PubMed] [Google Scholar]
- Carta JJ, Atwater JB, Greenwood CR, McConnell SR, McEvoy MA, Williams R. Effects of cumulative prenatal substance exposure and environmental risks on children’s developmental trajectories. Journal of Clinical Child Psychology. 2001;30:327–337. doi: 10.1207/S15374424JCCP3003_5. [DOI] [PubMed] [Google Scholar]
- Coles CD, Black MM. Introduction to the special issue: Impact of prenatal substance exposure on children’s health, development, school performance, and risk behavior. Journal of Pediatric Psychology. 2006;31:1–4. doi: 10.1093/jpepsy/jsj036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Howell DC, Phares V, Williams RA, Giunta CT. Risk factors for emotional/behavioral problems in young adolescents: A prospective analysis of adolescent and parental stress and symptoms. Journal of Consulting and Clinical Psychology. 1989;53:732–740. doi: 10.1037//0022-006x.57.6.732. [DOI] [PubMed] [Google Scholar]
- Deater-Deckard K, Dodge KA, Bates JE, Pettit GS. Multiple risk factors in the development of externalizing behavior problems: Group and individual differences. Development and Psychopathology. 1998;10:469–493. doi: 10.1017/s0954579498001709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR. SCL-90-R: Administration, scoring & procedures manual-II. Baltimore, MD: Clinical Psychometric Research; 1992. [Google Scholar]
- Dodge KA. Developmental psychopathology in children of depressed mothers. Developmental Psychology. 1990;26:3–6. [Google Scholar]
- Dunn LM, Dunn LM. PPVT Manual for Forms L and M. Circle Pines, MN: American Guidance Service; 1981. [Google Scholar]
- Escalona SK. Babies at double hazard: early development of infants at biologic and social risk. Pediatrics. 1982;70:670–676. [PubMed] [Google Scholar]
- Famy C, Streissguth AP, Unis AS. Mental illness in adults with fetal alcohol syndrome or fetal alcohol effects. American Journal of Psychiatry. 1998;155:552–554. doi: 10.1176/ajp.155.4.552. [DOI] [PubMed] [Google Scholar]
- Frank DA, Jacobs RR, Beeghly M, Augustyn M, Bellinger D, Cabral H, et al. Level of prenatal cocaine exposure and scores on the Bayley Scales of Infant Development: Modifying effects of caregiver, early intervention, and birth weight. Pediatrics. 2002;110:1143–1152. doi: 10.1542/peds.110.6.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank DA, McCarten KM. Level of in utero cocaine exposure and neonatal ultrasound findings. Pediatrics. 1999;104:1101–1105. doi: 10.1542/peds.104.5.1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garmezy N. Stress-resistant children: The church for protective factors. In: Stevenson J, editor. Recent research in developmental psychopathology. Oxford, UK: Pergamon Press; 1985. pp. 213–233. [Google Scholar]
- Gerard JM, Buehler C. Cumulative environmental risk and youth maladjustment: The role of youth attributes. Child Development. 2004;75:1832–1849. doi: 10.1111/j.1467-8624.2004.00820.x. [DOI] [PubMed] [Google Scholar]
- Gluckman PD, Hanson MA. Living with the past: Evolution, development and patterns of disease. Science. 2004;305:1733–1736. doi: 10.1126/science.1095292. [DOI] [PubMed] [Google Scholar]
- Goldschmidt L, Richardson GA, Stoffer DS, Geva D, Day NL. Prenatal alcohol exposure and academic achievement at age six: A nonlinear fit. Alcoholism: Clinical and Experimental Research. 1996;20:763–770. doi: 10.1111/j.1530-0277.1996.tb01684.x. [DOI] [PubMed] [Google Scholar]
- Holden GW, Ritchie KL. Linking extreme marital discord, child rearing, and child behavior problems: Evidence from battered women. Child Development. 1991;62:311–327. doi: 10.1111/j.1467-8624.1991.tb01533.x. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Unpublished manuscript. Yale University; 1975. Four factor index of social status. [Google Scholar]
- Holmes TH, Rahe RH. The Social Readjustment Rating Scale. Journal of Psychosomatic Research. 1967;11:213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- Hoyme HE, May PA, Kalberg WO, Kodituwakku P, Gossage JP, Trujillo PM, et al. A practical clinical approach to diagnosis of fetal alcohol spectrum disorders: Clarification of the 1996 Institute of Medicine criteria. Pediatrics. 2005;115:39–47. doi: 10.1542/peds.2004-0259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson JL, Jacobson SW. Prenatal alcohol exposure and neurobehavioral development: Where is the threshold? Alcohol Health and Research World. 1994;18:30–36. [PMC free article] [PubMed] [Google Scholar]
- Jacobson JL, Jacobson SW, Sokol RJ, Ager JW. Relation of maternal age and pattern of pregnancy drinking to functionally significant cognitive deficit in infancy. Alcoholism: Clinical and Experimental Research. 1998;22:345–351. doi: 10.1111/j.1530-0277.1998.tb03659.x. [DOI] [PubMed] [Google Scholar]
- Jacobson SW. Specificity of neurobehavioral outcomes associated with prenatal alcohol exposure. Alcoholism: Clinical and Experimental Research. 1998;22:313–320. doi: 10.1111/j.1530-0277.1998.tb03654.x. [DOI] [PubMed] [Google Scholar]
- Jacobson SW, Carr LG, Croxford J, Sokol RJ, Li TK, Jacobson JL. Protective effects of the alcohol dehydrogenase-ADH1B allele in African American children exposed to alcohol during pregnancy. Journal of Pediatrics. 2006;148:30–37. doi: 10.1016/j.jpeds.2005.08.023. [DOI] [PubMed] [Google Scholar]
- Jacobson SW, Chiodo LM, Jacobson JL, Sokol RJ. Validity of maternal report of alcohol, cocaine, and smoking during pregnancy in relation to infant neurobehavioral outcome. Pediatrics. 2002;109:815–825. doi: 10.1542/peds.109.5.815. [DOI] [PubMed] [Google Scholar]
- Jacobson SW, Dodge N, Chiodo LM, Sokol RJ, Dehaene S, Jacobson JL. Evidence for a specific effect of prenatal alcohol exposure on “number sense”. Alcoholism: Clinical and Experimental Research. 2003;27:121A. [Google Scholar]
- Jacobson SW, Jacobson JL, Frye KF. Incidence and correlates of breast-feeding in socioeconomically disadvantaged women. Pediatrics. 1991;88:728–736. [PubMed] [Google Scholar]
- Jacobson SW, Jacobson JL, Sokol RJ, Chiodo LM, Corobana R. Maternal age, alcohol abuse history, and quality of parenting as moderators of the effects of prenatal alcohol exposure on 7.5-year intellectual function. Alcoholism: Clinical and Experimental Research. 2004;28:1732–1745. doi: 10.1097/01.alc.0000145691.81233.fa. [DOI] [PubMed] [Google Scholar]
- Jacobson SW, Jacobson JL, Sokol RJ, Martier SS, Ager JW. Prenatal alcohol exposure and infant information processing ability. Child Development. 1993;64:1706–1721. [PubMed] [Google Scholar]
- Jacobson SW, Jacobson JL, Sokol RJ, Martier SS, Chiodo LM. New evidence for neurobehavioral effects of in utero cocaine exposure. Journal of Pediatrics. 1996;129:581–590. doi: 10.1016/s0022-3476(96)70124-5. [DOI] [PubMed] [Google Scholar]
- Jones DJ, Forehand R, Brody G, Armistead L. Psychosocial adjustment of African American children in single-mother families: A test of three risk models. Journal of Marriage and Family. 2002;64:105–115. [Google Scholar]
- Kim S, Brody GH. Longitudinal pathways to psychological adjustment among black youth living in single-parent households. Journal of Family Psychology. 2005;19:305–313. doi: 10.1037/0893-3200.19.2.305. [DOI] [PubMed] [Google Scholar]
- Krishnakumar A, Black MM. Longitudinal predictors of competence among African American children: The role of distal and proximal risk factors. Applied Developmental Psychology. 2002;23:237–266. [Google Scholar]
- Landry SH, Smith KE, Swank PR, Assel MA, Vellet S. Does early responsive parenting have a special importance for children’s development or is consistency across early childhood necessary? Developmental Psychology. 2001;37:387–403. doi: 10.1037//0012-1649.37.3.387. [DOI] [PubMed] [Google Scholar]
- Levy-Shiff R, Einat G, Mogliner MB, Lerman M, Krikler R. Biological and environmental correlates of developmental outcome of prematurely born infants in early adolescence. Journal of Pediatric Psychology. 1994;19:63–78. doi: 10.1093/jpepsy/19.1.63. [DOI] [PubMed] [Google Scholar]
- Luster T, McAdoo HP. Factors related to the achievement and adjustment of young African American children. Child Development. 1994;65:1080–1094. doi: 10.1111/j.1467-8624.1994.tb00804.x. [DOI] [PubMed] [Google Scholar]
- Mattson SN, Riley EP, Gramling L, Delis DC, Jones KL. Heavy prenatal alcohol exposure with or without physical features of fetal alcohol syndrome leads to IQ deficits. Journal of Pediatrics. 1997;131:718–721. doi: 10.1016/s0022-3476(97)70099-4. [DOI] [PubMed] [Google Scholar]
- Mayes LC. A behavioral teratogenic model of the impact of prenatal cocaine exposure on arousal regulatory systems. Neurotoxicology and Teratology. 2002;24:385–395. doi: 10.1016/s0892-0362(02)00200-3. [DOI] [PubMed] [Google Scholar]
- Mayes LC, Molfese DL, Key APF, Hunter NC. Event-related potentials in cocaine-exposed children during a Stroop task. Neurotoxicology and Teratology. 2005;27:797–813. doi: 10.1016/j.ntt.2005.05.011. [DOI] [PubMed] [Google Scholar]
- McCloskey LA, Figueredo AJ, Koss MP. The effects of systemic family violence on children’s mental health. Child Development. 1995;66:1239–1261. [PubMed] [Google Scholar]
- McDonald RJ, Devan BD, Hong NS. Multiple memory systems: The power of interactions. Neurobiology of Learning and Memory. 2004;82:333–346. doi: 10.1016/j.nlm.2004.05.009. [DOI] [PubMed] [Google Scholar]
- McLoyd VC. The impact of economic hardship on Black families and children: Psychological distress, parenting, and socioemotional development. Child Development. 1990;61:311–346. doi: 10.1111/j.1467-8624.1990.tb02781.x. [DOI] [PubMed] [Google Scholar]
- Moss H, Vanyukov M, Majumder P, Kirisci L, Tarter RE. Prepubertal sons of substance abusers: Influences of parental and familial substance abuse on behavioral disposition, IQ, and school achievement. Addictive Behaviors. 1995;20:345–358. doi: 10.1016/0306-4603(94)00077-c. [DOI] [PubMed] [Google Scholar]
- Noble KG, McCandliss BD, Farah MJ. Socioeconomic gradients predict individual differences in neurocognitive abilities. Developmental Science. 2007;10:464–480. doi: 10.1111/j.1467-7687.2007.00600.x. [DOI] [PubMed] [Google Scholar]
- Nordstrom-Bailey B, Sood BG, Sokol RJ, Ager J, Janisse J, Hannigan JH, et al. Gender and alcohol moderate prenatal cocaine effects on teacher-report of child behavior. Neurotoxicology and Teratology. 2005;27:181–189. doi: 10.1016/j.ntt.2004.10.004. [DOI] [PubMed] [Google Scholar]
- Nunes E, Weissman M, Goldstein R, McAvay G, Seracini AM, Verdeli H, et al. Psychopathology in children of parents with opiate dependence and/or major depression. Journal of American Academy of Child and Adolescent Psychiatry. 1998;37:1142–1151. doi: 10.1097/00004583-199811000-00013. [DOI] [PubMed] [Google Scholar]
- O’Conner MJ, Paley B. The relationship of prenatal alcohol exposure and the postnatal environment to child depressive symptoms. Journal of Pediatric Psychology. 2006;31:50–64. doi: 10.1093/jpepsy/jsj021. [DOI] [PubMed] [Google Scholar]
- O’Connor MJ, Shah B, Whaley S, Cronin P, Gunderson B, Graham J. Psychiatric illness in a clinical sample of children with prenatal alcohol exposure. American Journal of Drug and Alcohol Abuse. 2002;28:743–754. doi: 10.1081/ada-120015880. [DOI] [PubMed] [Google Scholar]
- Parker S, Greer S, Zuckerman B. Double jeopardy: The impact of poverty on early child development. The Pediatric Clinics of North America. 1988;35:1227–1240. doi: 10.1016/s0031-3955(16)36580-4. [DOI] [PubMed] [Google Scholar]
- Puttler LI, Zucker RA, Fitzgerald HE, Bingham CR. Behavioral outcomes among children of alcoholics during the early and middle childhood years: Familial subtype variations. Alcoholism: Clinical and Experimental Research. 1998;22:1972. [PubMed] [Google Scholar]
- Rutter M. Protective factors in children’s responses to stress and disadvantage. In: Kent MW, Rolf JE, editors. Primary prevention of psychopathology: Social competence in children. Hanover, NH: University Press of New England; 1979. pp. 49–74. [Google Scholar]
- Sameroff A, Seifer R, Baldwin A, Baldwin C. Stability of intelligence from preschool to adolescence: The influence of social and family risk factors. Child Development. 1993;64:80–97. doi: 10.1111/j.1467-8624.1993.tb02896.x. [DOI] [PubMed] [Google Scholar]
- Selzer ML. The Michigan Alcoholism Screening Test: The quest for a new diagnostic instrument. American Journal of Psychiatry. 1971;127:1653–1658. doi: 10.1176/ajp.127.12.1653. [DOI] [PubMed] [Google Scholar]
- Singer LT, Arendt R, Minnes S, Farkas K, Salvator A, Kirchner HL, et al. Cognitive and motor outcomes of cocaine-exposed infants. Journal of American Medical Association. 2002;287:1952–1960. doi: 10.1001/jama.287.15.1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, Arendt R, Minnes S, Salvator A, Siegel AC, Lewis BA. Developing language skills of cocaine-exposed infants. Pediatrics. 2001;107:1057–1064. doi: 10.1542/peds.107.5.1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spohr HL, Willms J. Prenatal alcohol exposure and long-term developmental consequences. Lancet. 1993;341:907–910. doi: 10.1016/0140-6736(93)91207-3. [DOI] [PubMed] [Google Scholar]
- Steinhausen HC, Willms J, Spohr HL. Long-term psychopathological and cognitive outcome of children with fetal alcohol syndrome. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:990–994. doi: 10.1097/00004583-199309000-00016. [DOI] [PubMed] [Google Scholar]
- Stratton K, Howe C, Battaglia F. Fetal alcohol syndrome: Diagnosis, epidemiology, prevention, and treatment. Washington, DC: National Academy Press; 1996. [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: The Conflict Tactics (CT) Scales. Journal of Marriage and the Family. 1979;41:75–88. [Google Scholar]
- Streissguth AP, Aase JM, Clarren SK, Randels SP, LaDue RA, Smith DF. Fetal Alcohol Syndrome in adolescents and adults. Journal of the American Medical Association. 1991;265:1961–1967. [PubMed] [Google Scholar]
- Streissguth AP, Barr HM, Sampson PD. Moderate prenatal alcohol exposure: Effects on child IQ and learning problems at age 7 1/2 years. Alcoholism: Clinical and Experimental Research. 1990;14:662–669. doi: 10.1111/j.1530-0277.1990.tb01224.x. [DOI] [PubMed] [Google Scholar]
- Tolan PH. Socioeconomic, family, and social stress correlates of adolescent antisocial and delinquent behavior. Journal of Abnormal Child Psychology. 1988;16:317–331. doi: 10.1007/BF00913803. [DOI] [PubMed] [Google Scholar]
- Wadhwa PD. Psychoneuroendocrine processes in human pregnancy influence fetal development and health. Psychoneuroendocrinology. 2005;30:724–743. doi: 10.1016/j.psyneuen.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Wasserman GA, Miller LS, Pinner E, Jaramillo B. Parenting predictors of early conduct problems in urban, high-risk boys. Journal of American Academy of Child and Adolescent Psychiatry. 1996;35:1227–1236. doi: 10.1097/00004583-199609000-00020. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Intelligence Scale for Children. 3. San Antonio, TX: Psychological Corporation; 1991. [Google Scholar]
- Weinberg NZ. Cognitive and behavioral deficits associated with parental alcohol use. Journal of American Academy of Child and Adolescent Psychiatry. 1997;34:779–785. doi: 10.1097/00004583-199709000-00009. [DOI] [PubMed] [Google Scholar]
- Werner EE, Smith RS. Vulnerable but invincible: A longitudinal study of resilient children and youth. New York: McGraw Hill; 1982. [Google Scholar]
- Wilens TE, Biederman J, Bredin E, Hahesy AL, Abrantes A, Neft D, et al. A family study of the high-risk children of opioid- and alcohol-dependent parents. The American Journal on Addictions. 2002;11:41–51. doi: 10.1080/10550490252801620. [DOI] [PubMed] [Google Scholar]
- Yumoto C, Corobana R, Jacobson SW, Chiodo L, Sokol RJ, Jacobson JL. The influence of father’s presence in the home on alcohol-related aggression and delinquency in childhood. Alcoholism: Clinical and Experimental Research. 2002;26:92A. [Google Scholar]