Abstract
Objective
To examine the prevalence, correlates, persistence, and treatment-seeking related to symptoms of eating disorders (EDs) in a random sample of college students.
Participants
A random sample of students at a large university were recruited for an Internet survey in Fall 2005 and a follow-up survey in Fall 2007.
Methods
ED symptoms were measured using the SCOFF screen and adjusted for nonresponse using administrative data and a nonresponse survey.
Results
2,822 (56%) students completed the baseline survey. Among undergraduates the prevalence of positive screens was 13.5% for women and 3.6% for men. Among students with positive screens, 20% had received past-year mental health treatment. In the follow-up sample (N = 753), ED symptoms at baseline significantly predicted symptoms 2 years later.
Conclusions
Symptoms of EDs were prevalent and persistent among college students in this study. These findings suggest that brief screens can identify a large number of students with untreated EDs.
Keywords: correlates, eating disorders, prevalence, survey
Evidence from a variety of sources indicates that symptoms of eating disorders (EDs) are pervasive in college populations. Prevalence estimates of current EDs among college students range from 8% to 17%.1–4 In a recent national survey of college students, 20% of respondents said they suspected that they had suffered from an ED at some point in their lives.5 In the American College Health Association’s National College Health Assessment (ACHA-NCHA), 3% of females and 0.4% of males reported ever receiving a diagnosis of anorexia; 2% of females and 0.2% of males reported a previous diagnosis of bulimia; and 4% of females and 1% of males reported vomiting or taking laxatives to lose weight in the previous 30 days.6
These studies highlight the significance of addressing eating pathology in college populations, particularly considering the many channels—residential life, academics, extracurricular activities, social networks, and health services—by which students can be reached. With the exception of a small number of studies such as the ACHA-NCHA, however, most studies with information related to EDs among college students have examined convenience samples (eg, from psychology classes or certain residence halls) or specific groups (eg, athletes).1,2,4 To complement these studies, it is also important to examine the distribution and characteristics of eating pathology throughout entire student populations. This information can assist the development and implementation of effective campus-level prevention, detection, and intervention strategies. Understanding populations who are not receiving clinical care is particularly important, as early detection and treatment of EDs greatly increases the chances of full recovery.7,8 In particular, longitudinal data are needed in order to understand the persistence and predictors of EDs, which can aid in identification and prevention efforts.
In addition, it is important to understand how ED risk varies across student characteristics, such as sex, race/ethnicity, academic level, and socioeconomic status. A more detailed picture of how these variables relate to ED risk can help inform efforts to target or tailor intervention strategies on campuses. It is also important to understand the extent to which students with elevated ED risk are receiving mental health care, in order to illuminate the likely value of increased efforts to identify and refer such students.
In this study, we addressed these knowledge gaps using a randomly selected sample of students at a large, public university in the midwestern United States. Specifically, we addressed 4 issues. First, we estimated the prevalence of ED symptoms across subgroups defined by sex, academic level (undergraduate or graduate student), and race/ethnicity, using a standardized instrument (the SCOFF) (see Methods section for explanation of acronym). We hypothesized that the prevalence of ED symptoms would be higher among women, as in previous studies,6 whereas we did not have a clear expectation regarding differences by academic level or race/ethnicity (given the sparse previous literature on EDs across these groups in college populations). Second, we estimated the extent to which ED symptoms co-occurred with depressive and anxiety symptoms and health-related behaviors. We hypothesized that ED symptoms would be positively correlated with other mental health problems such as depression and anxiety and also positively correlated with health behaviors that may be coping mechanisms for psychological distress, such as binge drinking, cigarette smoking, and frequent exercise. This hypothesis was based on prior findings of substantial psychiatric comorbidities among people with eating disorders in the general adult population.9 Third, we estimated the extent to which various forms of mental health treatment were received by students with ED symptoms. We hypothesized that the majority of students with positive ED screens did not receive treatment, given the well-known delays in treatment-seeking for these conditions.9 Fourth, we examined the persistence over time of symptoms and apparent unmet need for services, using a follow-up survey 2 years after the baseline survey. We hypothesized that ED symptoms and lack of treatment would be persistent over time for the majority of students with ED risk at baseline, again based on previous literature documenting reluctance and delays in seeking appropriate care.
METHODS
Sample
Our initial sample was selected randomly from the registrar’s list of enrolled students at a large, midwestern, public university during the Fall 2005 semester. In terms of race, ethnicity, and sex, this university’s population approximates the demographic characteristics of the national population of college students.10
For the baseline survey, we randomly selected 5,021 students (2,495 undergraduates and 2,526 graduate students) who were at least 18 years old. The sample size was chosen in order to yield 95% confidence intervals spanning approximately 3% (±1.5%) for prevalence estimates of key mental health and treatment utilization measures, which we anticipated to be close to 10%. The randomly selected students were sent e-mails inviting them to complete the survey on a secure Web site. After reading an online consent form, participants could indicate consent by clicking to begin the survey, which was administered using Illume software. The respondents to this survey constituted our Fall 2005 baseline sample. Two years later, in Fall 2007, we recruited for a follow-up survey the baseline respondents who were still enrolled at the university. The study was approved by the university’s institutional review board.
Measures
We measured symptoms of EDs using the written US version of the SCOFF screening instrument, a 5-item questionnaire designed to identify subjects likely to have an ED.11 A previous study of university students used 2 or more symptoms as the threshold for a positive SCOFF screen and found a sensitivity of 53%, specificity of 93%, positive predictive value of 67%, and negative predictive value of 89%.12 Another study with a university student population found a positive likelihood ratio of 11, when using 3 symptoms as the threshold for a positive SCOFF screen, as compared to a positive likelihood ratio of 6 when using 2 symptoms at the threshold.13 Both of these studies validated the instrument using samples including both females and males. In this study we adopted the more conservative threshold (which yields fewer false positives) of 3 or more symptoms. Using this threshold, we would expect a higher positive predictive value (but lower negative predictive value), as compared to the study by Parker and colleagues.12
We collected information about a variety of potential correlates of eating disorders: sociodemographic characteristics including race/ethnicity, sex, and academic level; health behaviors (self-injury, substance use, and exercise); and several measures of mental health. Specifically, symptoms of depression in the past 2 weeks were measured using the Patient Health Questionnaire-9 (PHQ-9), a screening instrument based on the 9 Diagnostic and Statistical Manual for Mental Disorders (DSM)-IV criteria for a major depressive episode.14 We used the PHQ-9’s standard algorithm to categorize people as screening positive for major depression, “other” depression (which includes dysthymia or depression not otherwise specified), any depression (either major or “other”), or neither. The PHQ-9 has been validated as internally consistent and highly correlated with diagnoses by clinicians in a wide variety of age groups and racial/ethnic groups.15 In our sample, the internal consistency was also high (Cronbach’s alpha equal to .84). Symptoms of panic disorder and generalized anxiety disorder over the past 4 weeks were measured using screens from the PHQ anxiety module, which has also been validated in diverse populations.14 Suicidal ideation was measured using 1 item asking whether the participant had seriously thought about committing suicide during the past 4 weeks. Participants were also shown a list of the most common types of mental health conditions (including EDs) and asked to note any of them for which they had ever been diagnosed by a health professional.
Regarding help-seeking, we asked all participants about their perceived need for and utilization of mental health services, using items that were developed and validated in the national Healthcare for Communities study.16 In previous work using the baseline sample in the present study, we found strong associations between these measures of perceived need and service utilization and mental health status.17 In the baseline survey we asked about help-seeking in the previous year, whereas in the follow-up survey we asked about the time period since baseline (the previous 2 years). Perceived need for help was ascertained by the question, “Did you think you needed help for emotional or mental health problems such as feeling sad, blue, anxious or nervous?” Service utilization was indicated if participants reported receiving counseling or therapy for their mental or emotional health from a health professional (psychiatrist, psychologist, social worker, or physician), or if they had taken any psychotropic medications. Finally, participants were asked if they had visited any health provider for any reason.
Adjusting for Survey Nonresponse
All students in the random sample had regular access to the Internet and to their university e-mail account in particular, because official university e-mail addresses are used frequently in courses and other communications to students. Nevertheless, as in any survey, those who choose to participate may be different in various dimensions from those who do not. We therefore incorporated sample probability weights to adjust for survey nonresponse. For the baseline sample, we constructed these weights using methods analogous to those used by Kessler and colleagues.18 To do this we used administrative data obtained from the university on several characteristics of all students randomly selected for the study (sex, race/ethnicity, year in school, nationality [US or international], and grade point average) and data on depressive symptoms and mental health care utilization from an abbreviated follow-up survey of nonrespondents to the main survey. A poststratification weight was also used to reflect the mix of undergraduates and graduate students (approximately 2:1) of the student population. More details on the weighting are available in the appendix to a previous report.17 For the follow-up sample (students who responded both at baseline and at follow-up), we constructed response propensity weights using mental health and other variables collected at baseline.
Statistical Analysis
We estimated the proportion of positive screens by subgroups defined by sex and academic level (undergraduate or graduate student), and also by sex and race/ethnicity for the 3 groups with sufficient sample sizes: white, non-Hispanic; black, non-Hispanic; and Asian/Asian American. We evaluated the significance of differences in measures across subgroups using 2-tailed chi-square tests. To investigate the co-occurrence of ED symptoms and other health measures, we estimated means of health indicators by whether individuals had positive or negative SCOFF screens. Similarly, we estimated means of measures of mental health care utilization by whether individuals had positive SCOFF screens. All analyses were performed using Stata 9.2.
RESULTS
The baseline survey was completed by 2,822 students, representing a 56.2% response rate. Of these 2,822 students, 1,272 were still enrolled as of Fall 2007 and were recruited for the follow-up survey. Among these students, 753 completed the follow-up survey, representing a 59% response rate. Response rates were higher among women compared to men and among graduate students compared to undergraduates. As noted earlier, sample probability weights were used to account for these differences. Table 1 shows the demographic characteristics of the weighted sample.
TABLE 1.
Demographic Characteristics of Sample
| Undergraduates
|
Graduates
|
|||||
|---|---|---|---|---|---|---|
| Female | Male | All | Female | Male | All | |
| N | 677 | 604 | 1,181 | 819 | 843 | 1,662 |
| Age | ||||||
| 18–22 | 95.1 | 93.0 | 94.0 | 10.0 | 7.1 | 8.4 |
| 23–25 | 3.1 | 5.8 | 4.5 | 34.9 | 29.0 | 31.7 |
| 26–30 | 1.0 | 0.5 | 0.8 | 36.7 | 40.4 | 38.7 |
| 31+ | 0.8 | 0.6 | 0.7 | 18.4 | 23.5 | 21.2 |
| Race/Ethnicity | ||||||
| White or Caucasian, non-Hispanic, non-Arab | 68.6 | 68.1 | 68.4 | 56.5 | 53.9 | 55.1 |
| African American/Black, non-Hispanic | 7.7 | 6.3 | 7.0 | 7.4 | 5.0 | 6.1 |
| Hispanic/Latino | 3.1 | 3.8 | 3.4 | 3.9 | 4.5 | 4.2 |
| Asian or Pacific Islander | 15.0 | 15.9 | 15.5 | 24.4 | 30.8 | 27.9 |
| Arab/Middle Eastern or Arab American | 0.2 | 1.9 | 1.1 | 1.6 | 1.7 | 1.7 |
| More than 1 of the above | 5.3 | 3.8 | 4.5 | 5.5 | 3.6 | 4.5 |
| Other | 0.3 | 0.2 | 0.2 | 0.7 | 0.8 | 0.7 |
Note. All values are percentages calculated using response propensity survey weights.
Table 2 shows the estimated prevalence of ED symptoms at baseline, based on the SCOFF, by sex and academic level and by sex and race/ethnicity. Using the threshold of 3+ symptoms on the SCOFF, we found positive screens for 13.5% of undergraduate females, 9.3% of graduate females, 3.6% of undergraduate males, and 3.1% of graduate males. Comparing across race/ethnicity, the prevalence of positive screens was nearly identical for Asian and white, non-Hispanic students, and lower for black students, although this difference was not statistically significant (χ2[1, N = 2822] = 2.39, p = .21).
TABLE 2.
Prevalence of Eating Disorder Symptoms
| Undergraduates
|
Graduates
|
White, non-Hispanic
|
Black, non-Hispanic
|
Asian/Asian American
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | M | All | F | M | All | F | M | All | F | M | All | F | M | All | |
| N | 674 | 494 | 1,168 | 815 | 839 | 1,654 | 910 | 780 | 1,690 | 79 | 42 | 121 | 291 | 339 | 630 |
| Positive screen (3+ on SCOFF) | 13.5 | 3.6 | 9.4 | 9.3 | 3.1 | 5.8 | 11.9 | 3.2 | 7.3 | 9.0 | 0.0 | 4.9 | 11.3 | 3.0 | 6.5 |
| Individual SCOFF items | |||||||||||||||
| Do you make yourself sick because you feel uncomfortably full? | 13.7 | 4.3 | 9.0 | 11.9 | 7.3 | 9.4 | 14.0 | 5.2 | 9.4 | 7.3 | 3.4 | 5.5 | 14.1 | 8.0 | 10.0 |
| Do you worry you have lost control over how much you eat? | 26.4 | 8.4 | 17.3 | 24.0 | 10.0 | 16.3 | 27.3 | 8.9 | 7.7 | 16.7 | 2.5 | 10.3 | 21.9 | 9.2 | 4.5 |
| Have you recently lost more than 14 pounds in a 3 month period? | 4.9 | 5.2 | 5.0 | 4.1 | 3.7 | 4.9 | 4.7 | 4.7 | 4.7 | 7.2 | 6.7 | 7.0 | 3.2 | 3.0 | 3.1 |
| Do you believe yourself to be fat when others say you are thin? | 33.8 | 9.2 | 21.5 | 24.2 | 11.6 | 17.2 | 31.1 | 10.3 | 20.2 | 17.9 | 12.8 | 15.6 | 28.4 | 8.2 | 16.7 |
| Would you say that food dominates your life? | 16.8 | 7.1 | 11.9 | 14.1 | 5.0 | 9.0 | 16.0 | 5.2 | 10.3 | 9.9 | 3.6 | 7.0 | 15.5 | 7.2 | 10.7 |
| Previous ED diagnosis (any) | 3.2 | 0.1 | 1.7 | 4.6 | 0.5 | 2.3 | 5.1 | 0.4 | 2.7 | 2.0 | 0.0 | 1.1 | 1.2 | 0.5 | 0.8 |
| Anorexia nervosa | 2.2 | 0.1 | 1.2 | 2.7 | 0.3 | 1.4 | 3.4 | 0.3 | 1.8 | 0.0 | 0.0 | 0.0 | 0.6 | 0.2 | 0.4 |
| Bulimia nervosa | 1.7 | 0.0 | 0.9 | 2.1 | 0.0 | 0.9 | 2.5 | 0.0 | 1.2 | 2.0 | 0.0 | 1.2 | 0.0 | 0.0 | 0.0 |
| Previous ED diagnosis, among positive screens | 5.4 | 0.0 | 4.3 | 14.0 | 6.2 | 11.7 | 9.4 | 5.6 | 8.5 | 22.4 | n/a | 22.4 | 4.7 | 0.0 | 3.5 |
Note. All results are expressed in % points and adjusted by response propensity weights.
Among the individual items on the SCOFF, by far the 2 most commonly endorsed were “Do you believe yourself to be fat when others say you are thin?” and “Do you worry you have lost control over how much you eat?” The item least frequently endorsed was “Have you recently lost more than 14 pounds in a 3-month period?” At least 1 item was endorsed by 50.9% of undergraduate females, 21.8% of undergraduate males, 44.6% of graduate females, and 24.6% of graduate males. These female-male differences were statistically significant (χ2[1, N = 2822] = 152, p < .001). As shown in Table 2, the item that appears to be driving the higher prevalence of positive screens among undergraduate females, as compared to graduate females, is “Do you believe yourself to be fat when others say you are thin?”
About 4% of females and 0.2% of males reported having ever received an ED diagnosis (difference by sex: χ2[1, N = 2822] = 52.4, p < .001). Despite the similar prevalence of current symptoms among Asian and white, non-Hispanic females, the latter group was over 4 times more likely to have a previous diagnosis (5.1% vs 1.2%, χ2[1, N = 1177] = 6.24, p = 0.012). Among students with positive SCOFF screens, previous diagnoses were reported by only 5.4% of undergraduate females, 0% of undergraduate males, 14% of graduate females, and 6.2% of graduate males. These differences by sex were marginally significant (χ2[1, N = 223] = 3.38, p < .068).
The results shown in Table 3 indicate that a positive screen for an ED was associated with several measures of mental health and health-related behaviors. A positive ED screen was most significantly associated with a higher likelihood of a positive screen for major depression (both sexes, χ2[1, N = 2822] = 21.6, p < .001), panic disorder (males only, χ2[1, N = 1332] = 11.4, p < .001), generalized anxiety disorder (both sexes, (χ2[1, N = 2822] = 5.84, p = .012), and suicidal thoughts (both sexes, χ2[1, N = 2812] = 9.16, p = .011). Health-related behaviors positively and significantly associated with ED symptoms were self-injury (both sexes, χ2[1, N = 2781] = 19.0, p < .001), binge drinking (females only, χ2[1, N = 1480] = 8.54, p = .010), cigarette smoking (both sexes, χ2[1, N = 2798] = 14.4, p < .001), and marijuana use (females only, χ2[1, N = 1479] = 5.67, p = .034). Frequent exercise was positively associated with ED symptoms among females (χ2[1, N = 1484] = 4.47, p = .061) and negatively associated among males (χ2[1, N = 1328] = 5.24, p = .035). Gambling was negatively associated with ED symptoms for both sexes (χ2[1, N = 2780] = 13.1, p = .001).
TABLE 3.
Mental Health Problems and Health Behaviors, Co-occurring With Eating Disorders
| Eating disorder screen
|
||||||
|---|---|---|---|---|---|---|
| Positive
|
Negative
|
|||||
| Female | Male | All | Female | Male | All | |
| N | 181 | 47 | 228 | 1,312 | 1,287 | 2,599 |
| Percentage who screened positive for: | ||||||
| Major depression | 13.3 | 5.4 | 11.4 | 4.8 | 3.7 | 4.2 |
| Other depression | 10.6 | 13.9 | 11.4 | 7.3 | 8.4 | 7.9 |
| Panic disorder | 1.4 | 5.7 | 2.4 | 2.5 | 0.7 | 1.5 |
| Generalized anxiety disorder | 6.3 | 2.7 | 5.4 | 4.0 | 1.7 | 2.7 |
| Suicidal thoughts | 4.0 | 9.9 | 5.4 | 1.5 | 2.4 | 2.0 |
| Percentage who engaged in: | ||||||
| Nonsuicidal self-injury behavior, past 4 weeks | 13.1 | 28.4 | 16.8 | 7.5 | 8.2 | 7.9 |
| Binge drinking, past 30 days | 54.1 | 32.1 | 48.9 | 42.2 | 47.3 | 45.0 |
| Cigarette smoking (at least 1–5 cigs/day, past 30 days) | 11.3 | 13.5 | 11.8 | 3.2 | 7.1 | 5.3 |
| Marijuana use, past 30 days | 18.1 | 14.1 | 17.1 | 11.1 | 13.7 | 12.5 |
| Gambling, past year | 14.4 | 30.8 | 18.3 | 17.8 | 39.9 | 29.8 |
| Exercise (moderate intensity or higher, 1+ hours/week past 30 days) | 74.4 | 61.2 | 71.2 | 71.2 | 76.7 | 74.2 |
| Exercise (moderate intensity or higher, 5+ hours/week past 30 days) | 30.8 | 14.7 | 26.9 | 23.3 | 30.3 | 27.1 |
Note. All results are expressed in % points and adjusted by response propensity weights.
As shown in Table 4, students with positive screens for EDs were more likely than those with negative screens to have perceived a need for help with mental or emotional health (χ2[1, N = 2807] = 34.3, p < .001) and to have used services (psychotropic medication or counseling/therapy) in the previous year (χ2[1, N = 2782] = 7.89, p = .004). Still, only 48% of students with positive screens perceived a need for help, and only 15% had any counseling or therapy visits for their mental health. The vast majority (83%) of those with positive screens had at least some contact with the health care system during the previous year, with 1 or more visits to any type of health professional.
TABLE 4.
Mental Health Service Use in Past Year, by Eating Disorder Status
| Eating disorder screen
|
||||||
|---|---|---|---|---|---|---|
| Positive
|
Negative
|
|||||
| Female | Male | All | Female | Male | All | |
| N | 181 | 47 | 228 | 1,312 | 1,287 | 2,599 |
| Think you needed help for mental or emotional difficulties, past year | 52.8 | 31.7 | 47.8 | 38.2 | 21.3 | 29.1 |
| Psychotropic medication use | ||||||
| Any in list below | 16.4 | 13.9 | 15.8 | 10.6 | 6.7 | 8.5 |
| Psychostimulants | 2.9 | 4.3 | 3.2 | 0.9 | 1.9 | 1.4 |
| Antidepressants | 11.5 | 4.5 | 9.9 | 7.5 | 3.9 | 5.5 |
| Antipsychotics | 2.1 | 0.0 | 1.6 | 0.1 | 0.0 | 0.0 |
| Antianxiety | 2.1 | 0.0 | 1.6 | 2.1 | 0.9 | 1.5 |
| Mood stabilizers | 2.2 | 2.3 | 2.3 | 0.5 | 0.2 | 0.3 |
| Sleep medications | 3.7 | 8.7 | 4.9 | 3.0 | 1.5 | 2.2 |
| Counseling/Therapy visits | ||||||
| Any | 15.6 | 11.3 | 14.6 | 14.1 | 6.6 | 10.0 |
| 1 or 2 | 1.5 | 2.3 | 1.7 | 3.7 | 1.3 | 2.4 |
| 3–5 | 1.6 | 2.3 | 1.7 | 3.9 | 1.8 | 2.7 |
| 6–12 | 5.7 | 4.2 | 5.3 | 3.4 | 2.2 | 2.7 |
| 12+ | 6.9 | 2.5 | 5.8 | 3.2 | 1.3 | 2.1 |
| Any medication or therapy/counseling | 21.7 | 16.0 | 20.4 | 19.1 | 10.0 | 14.2 |
| Any visit to health professional at all | 86.6 | 71.7 | 83.1 | 88.0 | 70.3 | 78.4 |
Note. All results are expressed in % points and adjusted by response propensity weights.
Examining the follow-up sample, we found that a positive screen for EDs at baseline was modestly correlated with a positive screen 2 years later (correlation coefficient = .55 for females, .47 for males). Figure 1 shows the proportion of students with positive screens at follow-up, as a function of the number of SCOFF symptoms at baseline. These results indicate that the risk of a positive screen at follow-up increases sharply with each additional symptom at baseline, for both males and females (differences across groups de-fined by number of baseline symptom were significant at p < .001). We also used the follow-up sample to examine variables related to help-seeking and service utilization, among students who had persistent symptoms of EDs (a positive SCOFF screen both at baseline and 2 years later). In the follow-up survey, 80% of these students reported that they thought they needed help for their mental or emotional health since the baseline survey (previous 2 years), but only 19% had ever been diagnosed with an ED and only 37% had received any mental health treatment in the previous 2 years.
FIGURE 1.
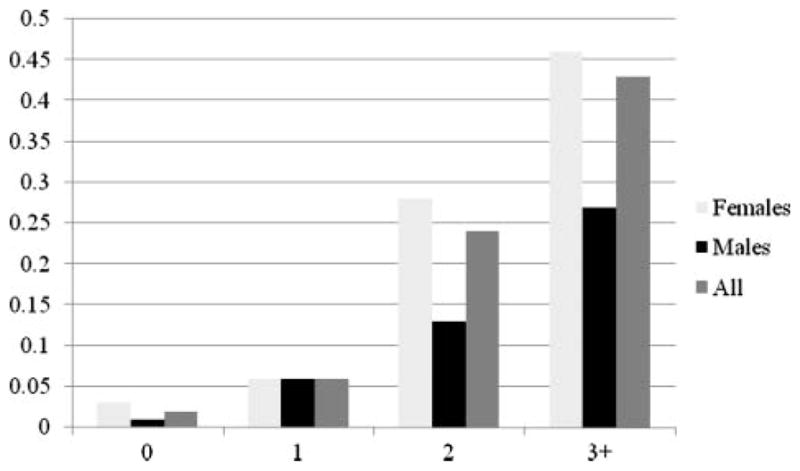
Probability of a positive screen at 2-year follow-up, by number of symptoms at baseline (0, 1, 2, 3+).
COMMENT
In a random sample of college students, the prevalence of positive SCOFF screens was 9% to 13% among females and 3% to 4% among males. Positive screens were significantly more likely among white, non-Hispanic, and Asian/Asian American students, as compared to black, non-Hispanic students. Positive screens were also correlated with measures of depression, anxiety, self-injury, and substance use. Among students with positive screens, fewer than 10% had ever received an ED diagnosis and about 20% had received any mental health treatment in the previous year. Symptoms of EDs were persistent for a large proportion of students—nearly half of students with positive screens at baseline also had positive screens 2 years later. In addition, even students with positive screens at both time points were unlikely to have received a diagnosis or any form of mental health treatment.
The female–male ratio of positive screens in our study was about 3 to 1, much lower than the female-male ratio of lifetime diagnoses (about 20 to 1). This 3-to-1 ratio also stands in contrast to the estimation that men experience eating pathology at one tenth the rate of women19 and highlights the importance of EDs among both females and males in adolescent and young adult populations. We also found that the correlates of ED symptoms were similar but not identical for females as compared to males, which is generally consistent with other recent studies of college students.20 For example, positive ED screens were associated with higher risks of psychiatric comorbidities for both sexes. On the other hand, males with positive ED screens were less likely to exercise intensively or binge drink than other males, whereas the opposite was true among females. Further understanding of these differences in profiles may be useful for tailoring campus efforts by sex to detect, prevent, and treat EDs.
The prevalence of positive screens was nearly identical for white, non-Hispanics compared to Asians and Asian Americans, and lower for black students. This finding is consistent with other studies that reported lower rates of eating pathology among black participants.21 The lifetime prevalence of diagnoses, however, was significantly lower among Asians compared to white students. This may be related to a relatively low likelihood of seeking help, which has been found in previous studies of both student and general populations of Asians in the United States.17,22–24 Special efforts to reduce stigma and promote help-seeking in culturally sensitive ways may be appropriate for this population.
Our results also indicate that students with symptoms of EDs are far more likely to experience co-occurring symptoms of psychopathology. For both male and female students, a positive ED screen was associated with depression, anxiety, suicidal ideation, and nonsuicidal self-injury. We also found that ED symptoms at baseline were significant predictors of panic disorder 2 years later. These associations further highlight the importance of early detection and intervention, as the mental health problems are likely to become more serious and complex over time.
This study supports the idea that a large proportion of college students with significant ED-related pathology are not identified or treated. This is consistent with several studies that have found widespread eating pathology among non-clinical female college students.1,2,4 One of the few studies using samples representative of campus populations, the ACHA-NCHA, found that among females, 3% had ever been diagnosed with anorexia and 2% with bulimia,25 similar to our estimates that 2.2% of undergraduate females had been diagnosed with anorexia and 1.7% with bulimia.
Using a conservative assumption about the positive predictive value for the SCOFF in our study—67% for the SCOFF, as in Parker et al12 (who used a threshold of 2+ symptoms, which should have a lower positive predictive value than the 3+ threshold in our study)—our findings imply that the prevalence of clinically diagnosable cases among the positive screens would be more than 3 times higher than the prevalence of treatment-seeking (67% as compared to 20%), and this differential would be even greater with respect to lifetime diagnoses. Although most of the clinically diagnosable cases are likely to be ED–Not Otherwise Specified (ED-NOS),12 these cases are still likely to benefit substantially from counseling.26,27 In addition, our findings indicate that a substantial proportion of students have symptoms of eating disorders that are persistent or recurrent.
The current study also provides new evidence about the prevalence of subclinical concerns about body image and eating behavior, which are important to identify because they may benefit from preventive interventions in the college setting.28 Approximately 20% of students (including 34% of undergraduate females) reported that they believed themselves to be fat even though others say they are thin, and approximately 17% of students (including 26% of undergraduate females) reported worrying that they have lost control over how much they eat. Also, even having only 1 SCOFF symptom at baseline corresponded to a significantly elevated risk of a positive screen (3 or more symptoms) 2 years later.
Our survey also asked why students did not receive mental health services. The most commonly endorsed answer choices among those with a positive ED screen and no service use were “I have not had any need,” “stress is normal in college,” “the problem will get better by itself,” and “I don’t have time.” These answers all indicate that students often do not view symptoms of EDs as important or urgent. On the one hand, this finding presents a sobering challenge to campus practitioners, highlighting that students with EDs are not predisposed to seek help. On the other hand, the finding can be viewed in an encouraging light, in that the primary barriers to help-seeking do not necessarily represent fierce resistance but rather passive lack of initiative and urgency. Many of the students who simply do not see an urgent need may be very open to counseling once the initial link is established.
Collectively, these findings highlight the potential effectiveness of a broad, preventive approach to EDs in college settings. Beyond preventing more serious cases, such an approach also has the potential to reduce the substantial psychological toll associated with subclinical body image and eating concerns. One possible strategy for implementing this approach would be to incorporate a brief screen into routine primary care visits or other settings where a large number of students could be reached. The National Eating Disorders Screening Program is an example of a successful program, having organized screening events through which students experiencing or at risk for EDs have been identified at over 400 colleges and universities.7 The present study suggests that online screens also hold promise, as our online survey identified a large number of students with positive ED screens who were not receiving treatment. Online screening programs might also be linked to online prevention programs, which have been shown in randomized studies to reduce concerns about eating and body image.28
Limitations
This study has a few important limitations that should be considered when interpreting the results. First, the measure of ED symptoms, the SCOFF, is a screening tool, not a clinical diagnosis; many students with positive screens would not necessarily qualify for a clinical diagnosis. However, this brief instrument has demonstrated acceptable sensitivity and specificity for detecting probable cases of EDs in university student populations, even when using a more inclusive threshold of 2+ symptoms: 78% sensitivity and 88% specificity when compared to the more extensive Questionnaire for ED Diagnoses (Q-EDD),13 and 53% sensitivity and 93% specificity when compared to DSM-IV criteria applied to the EDE-Q instrument.12 Another limitation is the possibility of survey nonresponse bias. Our sample probability weights adjusted for differences between responders and nonresponders along several dimensions, but not ED symptoms per se. If ED symptoms vary significantly across responders and nonresponders in ways not captured by our response weights, this would introduce inaccuracy in our estimates. This represents an important issue for future survey research on EDs among college students. It is also possible that the online format of the survey skewed the sample towards other characteristics that we did not account for, although it is not clear whether such characteristics would be related to ED risk. In addition, we measured utilization of mental health services in general, without asking respondents to specify whether the treatment was for eating pathology. If we had focused on treatment-seeking for eating pathology per se, the estimates may have been different. Finally, this was a single site study; multisite studies are needed to investigate these issues on a broader scale and analyze the potential roles of setting-level factors, such as academic competitiveness and availability of health services.
Conclusion
Our findings highlight the importance of understanding the full extent of EDs in college populations and the factors that influence students’ decisions to seek help for eating concerns. In understanding the lack of treatment-seeking, it would be useful to further disentangle the roles of potential explanations, such as lack of perceived need and urgency, perceived stigma surrounding diagnosis and treatment, limited availability of services, denial of illness, and lack of motivation for recovery inherent in EDs. In any of these cases, primary care physicians in student health centers and therapists in psychological counseling centers are ideally placed to identify eating pathology, as well as co-occurring psychiatric conditions and suicidal ideation, and provide or refer students to appropriate treatment. A brief screen could be a useful screening tool in primary care visits or online; it will be important to investigate the extent to which such screens increase utilization of ED treatment and preventive services on campuses. The high prevalence and persistence of eating pathology reported by this college sample, combined with low rates of treatment-seeking, also indicate that future work is needed to examine how identification, referral, and treatment protocols are organized at campuses nationwide, in order to ascertain which systems are associated with higher levels of appropriate service utilization.
Contributor Information
Dr. Daniel Eisenberg, Department of Health Management and Policy at the University of Michigan in Ann Arbor, Michigan.
Dr. Emily J. Nicklett, School of Social Work at the University of Michigan in Ann Arbor, Michigan.
Ms Kathryn Roeder, Department of Psychology at Vanderbilt University in Nashville, Tennessee.
Dr. Nina E. Kirz, Department of Psychiatry and Behavioral Sciences at Stanford University in Palo Alto, California.
References
- 1.Hoerr SL, Bokram R, Lugo B, Bivins T, Keast DR. Risk for disordered eating relates to both gender and ethnicity for college students. J Am Coll Nutr. 2002;21:307–314. doi: 10.1080/07315724.2002.10719228. [DOI] [PubMed] [Google Scholar]
- 2.Kirk G, Singh K, Getz H. Risk of eating disorders among female college athletes and nonathletes. J Coll Counsel. 2001;4:122–132. [Google Scholar]
- 3.Prouty AM, Protinsky HO, Canady D. College women: eating behaviors and help-seeking preferences. Adolescence. 2002;37:353–363. [PubMed] [Google Scholar]
- 4.Reinking MF, Alexander LE. Prevalence of disordered-eating behaviors in undergraduate female collegiate athletes and nonathletes. J Athl Train. 2005;40:47–51. [PMC free article] [PubMed] [Google Scholar]
- 5.National Eating Disorders Association. National Eating Disorders Association announces results of eating disorders poll on college campuses across the nation. [Accessed August 15, 2010];Market Wire. 2006 Sep; Available at: http://findarticles.com/p/articles_/mi_pwwi/is_/ai_n16742451.
- 6.American College Health Association. American College Health Association-National College Health Assessment reference group data report spring 2007. J Am Coll Health. 2008;56:469–479. doi: 10.3200/JACH.56.5.469-480. [DOI] [PubMed] [Google Scholar]
- 7.Becker AE, Franko DL, Nussbaum K, Herzog DB. Secondary prevention for eating disorders: the impact of education, screening, and referral in a college-based screening program. Int J Eat Disord. 2004;36:157–162. doi: 10.1002/eat.20023. [DOI] [PubMed] [Google Scholar]
- 8.Fichter M, Quadflieg N, Hedlund S. Twelve-year course and outcome predictors of anorexia nervosa. Int J Eat Disord. 2006;39:87–100. doi: 10.1002/eat.20215. [DOI] [PubMed] [Google Scholar]
- 9.Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey replication. Biol Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Center for Education Statistics. Digest of Education Statistics. Washington, DC: National Center for Education Statistics; 2005. Integrated postsec-ondary education data system (IPEDS), fall enrollment survey. Tables 205–206. [Google Scholar]
- 11.Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ. 1999;319:1467–1468. doi: 10.1136/bmj.319.7223.1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parker SC, Lyons J, Bonner J. Eating disorders in graduate students: exploring the SCOFF questionnaire as a simple screening tool. J Am Coll Health. 2005;54:103–107. doi: 10.3200/JACH.54.2.103-107. [DOI] [PubMed] [Google Scholar]
- 13.Cotton MA, Ball C, Robinson P. Four simple questions can help screen for eating disorders. J Gen Intern Med. 2003;18:53–56. doi: 10.1046/j.1525-1497.2003.20374.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 15.Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the Patient Health Questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med. 2006;21:547–552. doi: 10.1111/j.1525-1497.2006.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wells K, Sturm R, Burnam MA. Healthcare for Communities Household Survey Public Use Files: Revised Codebook. Ann Arbor, MI: ICPSR; 2003. [Google Scholar]
- 17.Eisenberg D, Golberstein E, Gollust SE. Help-seeking and access to mental health care in a university student population. Med Care. 2007;45:594–601. doi: 10.1097/MLR.0b013e31803bb4c1. [DOI] [PubMed] [Google Scholar]
- 18.Kessler RC, Berglund P, Chiu WT, et al. The US National Comorbidity Survey replication (NCS-R): design and field procedures. Int J Methods Psychiatr Res. 2004;13:69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Psychiatric Association, editor. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 20.Ousley L, Cordero ED, White S. Eating disorders and body image of undergraduate men [report] J Am Coll Health. 2008;56:617–622. doi: 10.3200/JACH.56.6.617-622. [DOI] [PubMed] [Google Scholar]
- 21.Striegel-Moore RH, Dohm FA, Draemer HC, et al. Eating disorders in white and black women. Am J Psychiatry. 2003;160:1326–1331. doi: 10.1176/appi.ajp.160.7.1326. [DOI] [PubMed] [Google Scholar]
- 22.Hickie AM, Davenport TA, Luscombe GM, Rong Y, Hickie ML, Bell M. The assessment of depression awareness and help-seeking behaviour: experiences with the international depression literacy survey. BMC Psychiatry. 2007;7:48. doi: 10.1186/1471-244X-7-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parker G, Chan B, Tully L. Depression and help-seeking in a western sample of ‘highly acculturated’ Chinese and controls. J Affect Disord. 2006;3:239–242. doi: 10.1016/j.jad.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 24.Abe-Kim J, Takeuchi DT, Hong S, et al. Use of mental health-related services among immigrant and US-born Asian Amer-icans: results from the National Latino and Asian American Study. Am J Public Health. 2007;97:91–98. doi: 10.2105/AJPH.2006.098541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American College Health Association. National College Health Assessment Spring 2006 Reference Group data report (abridged) J Am Coll Health. 2007;55:195–206. doi: 10.3200/JACH.55.4.195-206. [DOI] [PubMed] [Google Scholar]
- 26.Button EJ, Benson E, Nollett C, Palmer RL. Don’t forget ED-NOS (eating disorder not otherwise specified): patterns of service use in an eating disorders service. Psychiatr Bull. 2005;29:134–136. [Google Scholar]
- 27.Schwitzer A, Hatfield T, Jones AR, Duggan MH, Jurgens J, Winninger A. Confirmation among college women: the eating disorders not otherwise specified diagnostic profile [report] J Am Coll Health. 2008;56:607–609. doi: 10.3200/JACH.56.6.607-616. [DOI] [PubMed] [Google Scholar]
- 28.Taylor CB, Bryson S, Luce KH, et al. Prevention of eating disorders in at-risk college-age women. Arch Gen Psychiatry. 2006;63:881–888. doi: 10.1001/archpsyc.63.8.881. [DOI] [PMC free article] [PubMed] [Google Scholar]


