Abstract
This study investigated the prospective association between prenatal methamphetamine (MA) exposure and child behavioral problems at 5 years while also examining the home environment at 30 months and several primary caregiver (PC) risk factors. Participants were 97 MA-exposed and 117 comparison children and their PCs enrolled in the Infant Development, Environment and Lifestyle Study. Hypotheses were that child behaviors would be adversely impacted by (a) prenatal MA exposure, (b) home environments that provided less developmental stimulation and emotional responsiveness to the child, and (c) the presence of PC psychological symptoms and other risk factors. Prenatal MA exposure was associated with child externalizing behavioral problems at 5 years. Home environments that were more conducive to meeting children’s developmental and emotional needs were associated with fewer internalizing and externalizing behavioral problems. Independent of prenatal MA exposure, PC parenting stress and psychological symptoms were associated with increased child behavioral problems. Findings suggest prenatal MA exposure may contribute to externalizing behavioral problems in early childhood and the importance of considering possible vulnerabilities related to prenatal MA exposure in the context of the child’s caregiving environment.
Keywords: infants, children, pregnant women, methamphetamine use, prenatal substance exposure, primary caregiver, caregiving environment, parenting stress
Recent evidence suggests that methamphetamine (MA) use is increasing in the United States after a short period of decline (Carnevale, 2011). In 2009, 12.8 million individuals aged 12 and older reported using MA at least once in their lifetime, and past-year prevalence increased 37% from 2008 to 2009 (Substance Abuse & Mental Health Services Administration, 2010a). Drug treatment admissions related to MA rose from 1998 to 2005 and then declined slightly through 2008 (Substance Abuse & Mental Health Services Administration, 2010b). Among pregnant women admitted to a drug treatment facility in the United States, the proportion with a MA problem increased dramatically from 8% in 1994 to 24% in 2006 (Terplan, Smith, & Kozloski, 2009).
Several studies have clearly documented that prenatal exposure to illicit drugs, including MA, places children at risk for developmental, medical, psychological, and behavioral problems (Huestis & Choo, 2002; Keegan, Parva, Finnegan, Gerson, & Belden, 2010; Lester & Lagasse, 2010). One of the earliest studies of children prenatally exposed to amphetamine was conducted in Sweden by Billing, Eriksson, Steneroth, and Zetterstrom (1988), who assessed children longitudinally from birth to 14 years of age. Only 22% of the sample consistently remained with their biological mothers (Cernerud, Eriksson, Jonsson, Steneroth, & Zetterstrom, 1996). At age 8, children exposed to amphetamines throughout the pregnancy exhibited more aggressive behaviors and had poorer peer relationships than the children whose prenatal exposure was limited to the early pregnancy (Billing, Eriksson, Jonsson, Steneroth, & Zetterstrom, 1994). This study, however, had no formal control group and did not account for exposures to other drugs of abuse.
There is a growing body of evidence from the ongoing Infant Development, Environment, and Lifestyle (IDEAL) Study that children who have been prenatally exposed to MA exhibit restricted fetal growth (Nguyen et al., 2010; Smith et al., 2006), as well as poor quality of movement, low arousal, and increased stress signs in the newborn period (LaGasse et al., 2011; Smith et al., 2008). MA-exposed children also were more likely to have a decreased length trajectory from birth to 3 years (Zabaneh et al., 2011) and poor grasping ability at ages 1 and 3 years (Smith et al., 2011). Related to this study, MA-exposed children showed significantly higher scores on syndrome scales on the Child Behavior Checklist (CBCL) at 3 and 5 years, including emotional reactivity, anxiety and depression, and withdrawal, with more attention-deficit hyperactivity disorder issues and externalizing behaviors at 5, but not at 3 (LaGasse et al., 2012). Important to note is that two key covariates, primary caregiver (PC) psychological symptoms and poorer quality home, reliably predicted all or most of the syndrome scales in this study. Maternal perceptions of child behavioral problems did not differ between mothers with continuous custody of their children from birth to 3 years who had used MA during pregnancy and mothers in the comparison group (Liles et al., 2012). Mothers who had used MA during pregnancy, however, reported more parenting stress and depressive symptoms.
Prenatal Substance Exposure and Associated Risk Factors
The adverse childhood outcomes seen in children prenatally exposed to alcohol, tobacco, and illicit drugs may be a function of both drug exposure and environmental circumstances (Wouldes, LaGasse, Sheridan, & Lester, 2004). The caregiving environment and the quality of the early parent–child relationship are extremely important influences on developmental outcomes. A follow-up study of maternal mental health, substance use, and exposure to emotional abuse at 12 months predicted adverse child behavioral outcomes at 36 months (Whitaker, Orzol, & Kahn, 2006).
Coexisting substance abuse and psychiatric disorders, such as major depression, can interfere with competent parenting capacities (Hans, 1999), which can in turn adversely impact child behavior. Psychiatric disorders are prevalent among MA-using pregnant women and have been reported to be even more common than among women who use other drugs such as cocaine, marijuana, opiates, tobacco, or alcohol (Oei, Abdel- Latif, Clark, Craig, & Lui, 2010). The multiple risk factors associated with prenatal substance exposure have the potential to compromise child and caregiver well-being through both direct and indirect experiences. Parents play a pivotal role in organizing the child’s experiences, regulating affect and behavior and serving as models for behavior (Davies, 2011). Between the ages of 2 and 3, the child’s developing sense of self more fully emerges along with rapid advancements in cognitive and social development. The foundations for learning, social, and behavioral trajectories are laid. The primary caregivers’ functions expand as they need to understand and adjust to their children’s shifting developmental and emotional needs during this time of dramatic change.
Concerns about the parenting abilities of perinatal substance users and the safety and well-being of their infants contribute to substance-exposed newborns being removed from maternal care either immediately after birth or during their early years (Hans, 2002). The disruptions in relationships, home environments that lack developmental stimulation, and ongoing use of drugs of abuse that can co-occur with perinatal MA use could have an adverse impact on the child independent of prenatal exposure. An examination of the contexts in which a child is being raised, including the quality of parental care, is an important component of understanding the effects of prenatal substance exposure on child behavioral outcomes (Hans, 2002).
In addition to concerns about the caregiving environment and parenting practices, maternal drug use is in general associated with a number of adverse environmental risk factors, including domestic violence (Najavits, Sonn, Walsh, & Weiss, 2004; Sullivan & Holt, 2008) and other forms of abuse and violence (Cohen et al., 2003), maternal childhood trauma (Medrano, Zule, Hatch, & Desmond, 1999), psychiatric disorders, and limited social support (Carta et al., 2001; Suchman, McMahon, Slade, & Luthar, 2005). Psychosocial adversities identified among MA-using pregnant women include homelessness (Oei et al., 2010), substance-using family and friends, and involvement in the legal system (Derauf et al., 2007; Oei et al., 2010).
Given the multiple spheres of influence on child development outcomes, this study investigated several potential psychosocial predictors of increased behavioral problems at age 5. To distinguish deviant and nondeviant scores, we used the borderline clinical range as the cut point for externalizing, internalizing, and total behavioral problems. We hypothesized that child behaviors at age 5 would be adversely impacted by (a) prenatal MA exposure, (b) home environments that provided less developmental stimulation and emotional responsiveness to the child, and (c) the presence of PC psychological symptoms and other risk factors. As many MA-exposed children were not living with their biological mothers, unlike nearly all comparison children, we report PC and environmental characteristics and behavioral problems related to living situation.
Method
The Infant Development, Environment, and Lifestyle Study
The IDEAL Study is a multisite, longitudinal study investigating the effects of prenatal MA exposure on child developmental outcomes. Detailed recruitment methods have been reported previously (Arria et al., 2006). In brief, between September 2002 and November 2004, women who delivered at seven hospitals in four geographically diverse locations, Honolulu, Hawaii, Los Angeles, California, Tulsa, Oklahoma, and Des Moines, Iowa, were approached and screened for eligibility.
The Institutional Review Board at each site gave approval for the study. A federal Certificate of Confidentiality that superseded mandatory reporting for illicit substances was obtained for the project and ensured that information pertaining to maternal drug use could be kept confidential. The certificate was explained to the mother during recruitment and the informed consent process, including the condition that it did not exclude reporting of evidence of child abuse or neglect. Informed consent was obtained from all study participants who were fully informed of their rights and what participation in the study would entail. Maternal exclusion criteria were as follows: non-English speaking, younger than 18, use of opiates, lysergic acid diethylamide, phencyclidine, or cocaine only during the pregnancy, institutionalized for emotional disorders, low cognitive functioning, or current or history of psychosis. Infant exclusion criteria were as follows: critical illness and unlikely to survive, multiple gestation, life-threatening congenital anomaly, chromosomal abnormality associated with mental or neurological deficiency, overt clinical evidence of an intrauterine infection, or a sibling previously enrolled in the study. Epidemiology at the time of recruitment indicated that many users of MA also used cocaine. Thus, we allowed cocaine in the exposed group but not in the comparison group. All consented mothers were interviewed after delivery to obtain information about their pregnancy, demographics, and prenatal drug use. Meconium was collected from each infant and analyzed for drug metabolites.
Infants were included in the exposed group based on either maternal self-report of MA use during pregnancy or a positive meconium screen, or both, and gas chromatography or mass spectroscopy confirmation. Infants were included in the comparison or non-MA-exposed group if there was maternal denial confirmed by a negative meconium screen for MA. MA-exposed infants and mothers (n = 204) were matched to comparison infant–mother pairs (n = 208) based on maternal race, birth-weight category (<1500 g, 1500–2500 g, >2500 g), insurance (private vs. public), and education (high school education completed vs. not completed). Maternal use of alcohol, tobacco, and marijuana during pregnancy was considered as background variables in both the MA-exposed and comparison groups.
Study assessments were conducted when infants were 1, 12, 24, 30, and 36 months and 5 years. Interviewers were trained and certified in the administration of standardized and semistructured questionnaires, which were conducted in face-to-face interviews with the child’s PC.
Participants
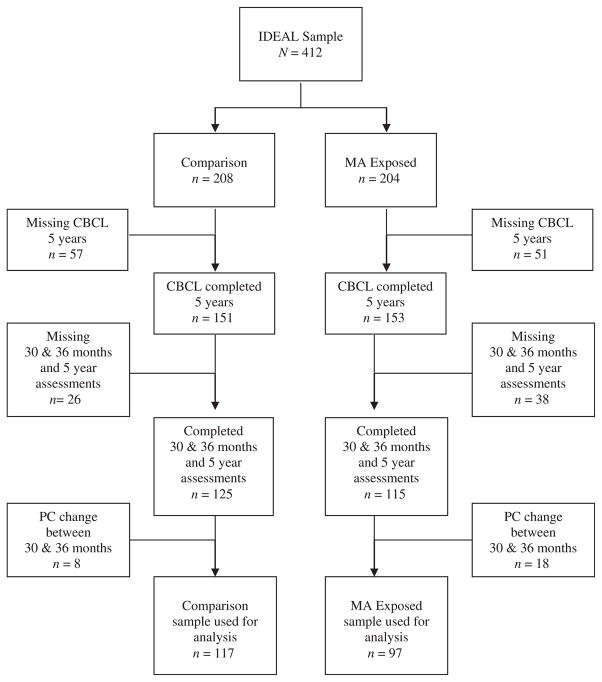
For this study, participants were selected from the larger IDEAL sample based on the criteria of a completed CBCL (Achenbach & Rescorla, 2000) at 5 years, a completed Infant– Toddler Home Observation for Measurement of the Environment (HOME; Caldwell & Bradley, 2001) at 30 months, a completed set of questionnaires at 36 months, and the same PC at the 30- and 36-month assessments (N = 214). A PC was defined as the person living with the child who assumed major parenting responsibilities such as feeding, bathing, dressing, soothing, and disciplining the child. Figure 1 is a flowchart of the number of study participants from the overall IDEAL sample excluded from this study.
Figure 1.
Flowchart of cohort (N = 412).
Maternal and neonatal characteristics were examined for significant differences between included (n = 214) and excluded (n = 198) participants (Table 1). The only group difference was that excluded dyads had more prenatal tobacco use (p = .026). There were no other differences in the baseline and demographic characteristics between these two groups.
Table 1.
Comparison of Included and Excluded Dyads
| N (%) or Mean (SD) | Included (n = 214) | Excluded (n = 198) | p |
|---|---|---|---|
| Neonatal characteristics | |||
| Gender | .653 | ||
| Male | 112 (52.3%) | 108 (54.5%) | |
| Race | .580 | ||
| White | 73 (34.6) | 69 (35.6) | |
| Hispanic | 47 (22.3) | 41 (21.1) | |
| Hawaiian/Pacific Islander | 41 (19.4) | 30 (15.5) | |
| Asian | 30 (14.2) | 32 (16.5) | |
| Black | 9 (4.3) | 11 (5.7) | |
| American Indian | 4 (1.9) | 8 (4.1) | |
| Other | 7 (3.3) | 3 (1.5) | |
| Small for gestational age | 28 (13.1) | 27 (13.6) | .869 |
| Birth weight, g | 3283 (617.3) | 3210 (577.8) | .217 |
| Low birth weight, <2500 g | 24 (11.2) | 23 (11.6) | .898 |
| Maternal characteristics at birth | |||
| Age | 24.9 (5.5) | 25.5 (5.8) | .294 |
| No partner | 98 (45.8) | 87 (43.9) | .705 |
| Low SES | 43 (20.1) | 50 (25.5) | .191 |
| Education, <HS | 87 (40.7) | 85 (43.4) | .578 |
| Public insurance | 206 (96.7) | 195 (98.5) | .244 |
| Prenatal drug use | |||
| Methamphetamine | 97 (45.3) | 107 (54.0) | .077 |
| Cocaine | 8 (3.7) | 10 (5.1) | .515 |
| Tobacco | 102 (47.7) | 116 (58.6) | .026 |
| Alcohol | 47 (22.0) | 59 (29.8) | .069 |
| Marijuana | 37 (17.3) | 39 (19.7) | .529 |
Measurements
Child behavior
At 5 years, the CBCL for ages 1½ to 5 (Achenbach & Rescorla, 2000) was administered to the child’s PC. This is a 113-item rating scale that measures child social, emotional, and behavioral problems. The summary scores include three broad-band scales: internalizing, externalizing, and total behavioral problems. Higher scores are indicative of more behavioral problems. For our analysis, we applied the clinical cut points described by Achenbach and Rescorla (2000). T scores of 60 or higher on the internalizing, externalizing, and total problem scales combine the borderline and clinically significant ranges.
Home environment
At 30 months, the Infant–Toddler HOME (Caldwell & Bradley, 2001) was conducted in the child’s home. The Infant–Toddler HOME measures the emotional and developmental support provided to the child, parent–child interactions, and events that typically occur in the family. The HOME is administered through a combination of observation and semistructured interview. The 45 items that comprise the Infant–Toddler HOME are scored using a binary system that indicates whether specific attributes of the home environment are present and, if so, how often. The overall summary score for the total quality of home is used in this study. Higher scores are indicative of home environments that provide the child with experiences that promote positive developmental outcomes. The HOME has strong validity and reliability and is widely used in assessing the environment parents create for their infants. At 36 months, the following four questionnaires were administered to primary caregivers.
Demographic measures
The Lifestyle Interview (LI) is a semistructured questionnaire developed for use in longitudinal studies on prenatal substance exposure and child developmental outcomes (Arria et al., 2006). It assesses household composition, socioeconomic status (SES), services received, and child protective service (CPS) involvement over the calendar year preceding the interview. SES was calculated using the four-factor Hollingshead Index adapted for single parent and nonnuclear families with Hollingshead V indicating low SES (LaGasse et al., 1999).
Psychological symptoms
The Brief Symptom Index (BSI; Derogatis, 1993) is a 53-item instrument with good internal consistency and established reliability and validity that identifies psychological symptom patterns. Response options for each item range from not at all to extremely. There are nine primary symptom dimensions: somatization, obsessive– compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, psychoticism, and three global indices: Global Severity Index (GSI), Positive Symptom Total, and Positive Symptom Distress Index. Standardized scales were developed with the T score having a mean of 50 and a standard deviation of 10. The GSI is based on number and severity of symptoms. GSI scores greater than or equal to a T score of 63 or any two symptom dimension scores greater than or equal to a T score of 63 are an effective screening measure for psychiatric disorders. In this study, we use this cutoff to indicate clinically significant psychological symptoms.
Parenting stress
The Parenting Stress Index (PSI; Abidin, 1990) is a 36-item scale that measures parenting stress using a 5-point Likert scale on which items are rated from strongly agree to strongly disagree. A total stress score of 90 or higher indicates a clinically significant level of stress. This cut point is used in this study. The PSI has been validated among racially and ethnically diverse groups of parents.
Substance use and exposure to abuse
The Substance Use Inventory (SUI) was used to determine frequency and quantity of MA and other illicit drugs, alcohol, and tobacco used by the child’s PC over the past year (DellaGrotta et al., 2009). A section of the SUI examines personal safety and was used to determine the primary caregiver’s exposure to physical or sexual abuse over the past year (yes or no).
Covariates
Potential covariates included study site; primary caregiver’s age; partner status (partnered vs. not); medical insurance status (public vs. other); education (<high school vs. other); prenatal exposure of the following drugs (yes vs. no): tobacco, alcohol, marijuana, cocaine, or MA; low child birthweight (<2500 g); and child gender; and at 36 months, PC experience of physical abuse; CPS involvement; and use of tobacco, alcohol, or illicit drugs. In addition, quality of the child’s home environment, parenting stress, and psychological symptom assessments were included.
Data Analysis
Sample characteristics (pre- and postnatal) and behavioral problems were examined by MA-exposed versus comparison groups (Table 2) and MA-exposed not with biological mother, MA-exposed with biological mother, and comparison groups (Table 3). Means and standard deviations were used for continuous measures. Categorical variables are expressed as observed counts and percentages. Significance levels for differences in MA exposure and MA exposure and placement status were derived from unpaired t tests and chi-square tests, as determined by variable type.
Table 2.
Sample Characteristics at Birth by MA Exposure
| N (%) or Mean (SD) | MA-Exposed (n = 97) | Comparison (n = 117) | p |
|---|---|---|---|
| Neonatal characteristics | |||
| Gender | .539 | ||
| Male | 53 (54.6%) | 59 (50.4%) | |
| Race | .662 | ||
| White | 33 (34.4) | 40 (34.8) | |
| Hispanic | 22 (22.9) | 25 (21.7) | |
| Hawaiian/Pacific Islander | 19 (19.8) | 22 (19.1) | |
| Asian | 16 (16.7) | 14 (12.2) | |
| Black | 3 (3.1) | 6 (5.2) | |
| American Indian | 2 (2.1) | 2 (1.7) | |
| Other | 1 (1.0) | 6 (5.2) | |
| Small for gestational age | 15 (15.5) | 13 (11.1) | .347 |
| Birth weight, g | 3239 (641.1) | 3319 (597.1) | .347 |
| Low birth weight, <2500 g | 10 (10.3) | 14 (12.0) | .702 |
| Maternal characteristics at birth | |||
| Age | 25.2 (5.5) | 24.6 (5.47) | .448 |
| No partner | 59 (60.8) | 39 (33.3) | <.001 |
| Low SES | 34 (35.1) | 9 (7.7) | <.001 |
| Education, <HS | 45 (46.4) | 42 (35.9) | .120 |
| Public insurance | 91 (94.) | 115 (98.3) | .154 |
| Prenatal drug use | |||
| Heavy MA use (≥3 days/week) | 21 | — | — |
| Cocaine | 8 (8.2%) | — | — |
| Tobacco | 77 (79.4) | 25 (21.4) | <.001 |
| Heavy tobacco use (≥10 cig/day) | 27 (28.1) | 4 (3.4) | <.001 |
| Alcohol | 33 (34.0) | 14 (12.0) | <.001 |
| Heavy alcohol use (≥5 oz/day) | 4 (4.1) | 0 (0.0) | <.001 |
| Marijuana | 32 (33.0) | 5 (4.3) | <.001 |
| Heavy marijuana use (≥1.5 joint/day) | 4 (4.2) | 2 (1.7) | <.001 |
Table 3.
Prenatal MA Exposure: Children Not Living With Biological Mother Versus Living With Biological Mother
| N (%) or Mean (SD) | MA-Exposed
|
Comparison
|
p
|
|||
|---|---|---|---|---|---|---|
| Not Living w/Bio Mom (1) (n = 41) | Living w/Bio Mom (2) (n = 56) | Living w/Bio Mom (3) (n = 116)a | (1) versus (2) | (2) versus (3) | (1) versus (3) | |
| PC characteristics—36 months | ||||||
| Age | 45.2 (9.8) | 29.1 (6.7) | 27.8 (5.5) | <.001 | .200 | <.001 |
| No partner | 13 (31.7) | 25 (44.6) | 33 (28.4) | .197 | .035 | .693 |
| Low SES | 2 (5.0) | 9 (16.1) | 6 (5.2) | .114 | .019 | .957 |
| Education, < HS | 5 (12.2) | 19 (33.9) | 27 (23.5) | .014 | .148 | .140 |
| Public insurance | 4 (9.8) | 35 (62.5) | 47 (40.5) | <.001 | .007 | <.001 |
| Parenting stress | 5 (12.2) | 13 (23.2) | 16 (13.8) | .168 | .122 | .796 |
| Psychological symptoms | 4 (9.8) | 19 (33.9) | 21 (18.1) | .006 | .021 | .209 |
| Tobacco use | 7 (17.1) | 38 (67.9) | 31 (26.7) | <.001 | <.001 | .215 |
| Alcohol use | 12 (29.3) | 30 (53.6) | 55 (47.4) | .017 | .449 | .043 |
| Illegal drug use | 1 (2.4) | 14 (25.0) | 12 (10.3) | .002 | .012 | .114 |
| Report of physical abuse | 1 (2.4) | 6 (10.7) | 4 (3.5) | .233 | .083 | .740 |
| Postnatal environment—30 months | ||||||
| HOME total score | 35.22 (3.03) | 33.70 (3.91) | 34.31 (3.97) | .040 | .341 | .184 |
| Child behavioral problems—5 years | ||||||
| Internalizing behaviors (T score >60) | 8 (19.5) | 21 (37.5) | 35 (30.2) | .056 | .337 | .188 |
| Externalizing behaviors (T score >60) | 10 (24.4) | 21 (37.5) | 26 (22.4) | .171 | .037 | .796 |
| Total behavioral problems (T score >60) | 5 (12.2) | 20 (35.7) | 33 (28.4) | .009 | .333 | .037 |
| CPS involvement—5 years | ||||||
| 4 (9.8) | 11 (19.6) | 6 (5.2) | .183 | .003 | .292 | |
One child in comparison group excluded from analysis for this table because child was not living with biological mother.
Multivariable logistic regression models were constructed with demographic characteristics, home environment assessment, PC parenting stress, and psychological symptom assessments, in addition to a dichotomous MA exposure variable and other prenatal drug exposures. Potential predictors were eliminated through backward selection using a p value ≤.20 including partner status, medical insurance status, education, low child birthweight, child gender, and prenatal exposure to tobacco, alcohol, or marijuana, as well as PC experience of physical abuse at 36 months, CPS involvement, use of tobacco, alcohol, or illicit drugs at 36 months. Variables that qualified for inclusion in any model were included in all three. In addition to exposure to MA and other drugs, the quality of home, parenting stress, and psychological symptom scores were retained in the models.
All analyses were performed using SPSS, version 17 (Chicago, IL). Two-sided p values <.05 were significant in the analysis.
Results
Participant Characteristics
Methamphetamine-exposed children comprised 45% of the sample. As shown in Table 2, there were no differences in neonatal characteristics in gender, race, incidence of small for gestational age, or low birthweight by MA exposure status. At birth, maternal age, education, and type of health insurance did not differ. Mothers in the MA-exposed group were more likely to be without a partner at delivery, to have lower SES, and use more tobacco, alcohol, and marijuana, including heavy use of these substances.
Overall, at the 30- and 36-month assessments, primary caregivers were as follows: biological mothers (80%), adoptive parents (9%), relatives (7%), fathers (2%), and nonrelatives (1%). The majority (98%; n = 42) of children not living with their biological mothers were in the MA-exposed cohort. Within the MA-exposed group, 58% of children were living with their biological mothers at the 30- and 36-month assessments. Although having the same PC at the 5-year visit was not a requirement for inclusion in this study, 94% (201 of 214) of children remained with the same PC for all three visits.
Table 3 shows three comparisons of PC characteristics at 36 months and behavioral problems at 5 years.
MA-exposed group living with PC who is not the biological mother versus MA-exposed group living with the biological mother (1 vs. 2)
Compared to other primary caregivers, biological mothers were more likely to be younger, have less than a high school education, and have public insurance. Biological mothers were more likely than other primary caregivers to have psychological symptoms and use tobacco, alcohol, and illegal drugs at 36 months. The quality of the home environments was lower for MA-exposed children who lived with their biological mothers. A greater percentage of MA-exposed children who lived with their biological mothers at 36 months had total behavioral problems at 5 years.
Child living with biological mother, MA-exposed group versus comparison group (2 vs. 3)
Compared to mothers in the comparison group, mothers in the MA-exposed group were less likely to have a partner and more likely to be low SES and have public insurance. Mothers in the MA-exposed group were more likely to have psychological symptoms and use tobacco and illegal drugs. A greater percentage of MA-exposed children had externalizing behavioral problems at 5 years than children in the comparison group. Child protective services were more likely to be involved with children in the MA-exposed group.
MA-exposed group not living with biological mother versus comparison group living with the biological mother (1 vs. 3)
Compared to primary caregivers who were not biological mothers for the MA-exposed group, biological mothers in the comparison group were more likely to be younger, have public insurance, and use alcohol. A greater percentage of comparison children who lived with their biological mothers had total behavioral problems at 5 years than MA-exposed children not living with a biological mother.
Child Behavioral Outcomes at 5 years
Table 4 shows the odds of a child having behavioral problems at 5 years. Children with prenatal MA exposure were more than twice as likely to exceed the clinical cutoff for externalizing behavioral problems relative to comparison children. Prenatal MA exposure was not associated with clinically significant internalizing or total behavioral problems at 5 years. Home environments that provided the child with more developmental stimulation and emotional responsiveness were associated with decreased risk of internalizing and externalizing behavioral problems. Parenting stress was associated with an almost threefold increase in child internalizing behavioral problems. Psychological symptoms of the PC were associated with an almost threefold increase in the likelihood of a child having externalizing problems and a more than threefold increase in the likelihood of total behavioral problems. Older primary caregivers were associated with decreased risk of internalizing, externalizing, and total behavioral problems.
Table 4.
Odds of Child Having Behavior Problems at 5 Years
| Odds Ratio | 95% Confidence Interval
|
p | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Internalizing behaviors | ||||
| Prenatal MA exposure | 1.258 | 0.642 | 2.462 | .504 |
| Quality of home | 0.907 | 0.834 | 0.986 | .022 |
| Parenting stress | 2.615 | 1.195 | 5.720 | .016 |
| PC’s age —36 months | 0.955 | 0.917 | 0.994 | .024 |
| Externalizing behaviors | ||||
| Prenatal MA exposure | 2.390 | 1.161 | 4.918 | .018 |
| Quality of home | 0.903 | 0.821 | 0.993 | .036 |
| Psychological symptoms | 2.794 | 1.310 | 5.957 | .008 |
| PC’s age —36 months | 0.948 | 0.907 | 0.990 | .017 |
| Total behavioral problems | ||||
| Prenatal MA exposure | 1.116 | 0.551 | 2.260 | .761 |
| Home total | 0.931 | 0.853 | 1.015 | .105 |
| Psychological symptoms | 3.239 | 1.558 | 6.734 | .002 |
| PC’s age —36 months | 0.952 | 0.911 | 0.996 | .031 |
Discussion
To our knowledge, this is the first report of clinically significant behavioral problems of children with prenatal MA exposure at 5 years of age that includes an examination of the predictive value of their home environments and PC risk factors. The main findings of this study are (a) prenatal MA exposure was associated with child externalizing behavioral problems at 5 years, (b) home environments that were more responsive to children’s developmental and emotional needs were associated with a decreased risk of internalizing and externalizing behavioral problems, and (c) parenting stress and psychological symptoms experienced by primary caregivers were associated with increased child behavioral problems. The quality of the child’s home environment and PC risk factors such as parenting stress and psychological symptoms were associated with child behavioral problems independent of prenatal MA exposure.
A closer examination of the primary caregivers of MA-exposed children found that MA-exposed children living with their biological mothers had more total behavioral problems at 5 years than MA-exposed children whose primary caregivers were not their biological mothers and more externalizing behavioral problems at 5 years than comparison children living with biological mothers. However, MA-exposed children who were not living with a biological mother had less total behavioral problems than comparison children who lived with their biological mothers. Biological mothers who were the PC of MA-exposed children were more likely to experience psychological symptoms and use tobacco, alcohol, and illegal drugs. These findings suggest that vulnerabilities associated with prenatal MA exposure, combined with risk factors associated with maternal substance use, may contribute to greater stressors on the child and mother, manifesting in child behavioral problems.
Parenting behaviors can be affected by child behaviors that have been compromised by prenatal drug exposure, and poor quality parenting can contribute to poorer child developmental outcomes (Hans, 2002). Findings from this study suggest the bidirectional influences of child and parent or PC characteristics on child behavioral outcomes. The association between prenatal MA exposure and child behavioral problems in early childhood may adversely affect primary caregivers’ mental health because of stress related to raising a child with challenging behaviors. Mothers who used MA during pregnancy may be more susceptible to experiencing psychological symptoms as they assume parenting responsibilities in the context of addressing substance dependence and multiple psychosocial risk factors. A child with a history of prenatal substance exposure may be more vulnerable or reactive to the adverse impact of a caregiver’s psychological distress. Lester et al. (2009) identify direct and indirect pathways in which prenatal cocaine exposure impacts child behavioral outcomes. Direct pathways signify the teratogenic effect of prenatal substance exposure, and indirect pathways indicate the “cascading effects” of prenatal substance exposure that contribute to behavioral dysregulation in infancy with implications for negative behavioral outcomes at later ages.
At age 5, behavioral problems may not be as evident, particularly if children are not in structured situations such as a classroom, when behavioral issues either may become more noticeable or brought to the attention of primary caregivers by teachers or other professionals. Children identified with behavioral problems at 5 years of age may have more difficulties negotiating the increasingly complex academic and social demands of the school-aged child. The externalizing behavioral problems identified in children with prenatal MA exposure could indicate deficits in inhibitory control, which suggest executive function domains may be affected by MA exposure. Further, externalizing problems are indicative of difficulties with self-regulation, impulsivity, and social relationships. The preschool child learns to regulate affect and develop adaptive coping and social skills within the context of the caregiving relationship. Disruptions in primary caregiving relationships, parenting stress, and parental psychological symptoms can compromise the primary caregiver’s ability to be responsive to the child’s emotional needs and adversely affect the quality of the parent–child relationship. These factors may interfere with the child’s being able to predictably rely on the PC for the support and modeling needed to develop self-regulatory capacities.
Substance-exposed infants often are placed, either informally or through formal channels such as CPS, with caregivers who are not their biological mothers. Between 30 and 36 months, 20% of children were not living with their biological mothers. At 5 years, no children had been reunified with their biological mothers, and an additional 5% had been removed from their biological mothers’ care. A strength of this study is that it examined characteristics of children’s primary caregivers to reflect that, for many substance-exposed infants, uninterrupted parenting from biological mothers is not the norm.
Limitations
Several limitations of the study must be noted. There may have been differences between the families included in this study who completed three consecutive visits over the course of 2½ years and families who did not attend all three visits. The majority of children in this study (91%) were living with a biological or adoptive parent, which may be indicative of permanency and stability in their lives. Child placements prior to 30 months were not examined. There could be reporting bias, as CBCL findings are based on PC report. PC characteristics, such as experiencing psychological symptoms, may have influenced their perceptions of the child’s behavior. This study examined important influences on a young child’s life including the home environment and risk factors associated with the person assuming primary caregiving responsibilities for the child. Understanding determinants of early childhood behavioral outcomes is complicated by many factors that can be difficult to control for, such as genetic vulnerabilities, child temperament, life experiences, quality of relationships, social support, and availability of community resources to support families with young children. Finally, because of the increased use of tobacco, alcohol, and marijuana in mothers who used MA during pregnancy, the contribution of these other drugs may be masked. Despite these limitations, the IDEAL Study provides a first look at the emergence of clinically significant behavioral problems in children with prenatal MA exposure in the context of their caregiving environments.
Implications
Study findings have implications for treatment and prevention. Identification of behavioral problems in the preschool years can contribute to understanding developmental trajectories and identifying approaches to prevention (Shonkoff & Phillips, 2000). Early identification of emergent behavioral problems can lead to interventions to support more adaptive functioning. Study results highlight the importance of considering potential vulnerabilities related to prenatal MA exposure within the context of the child’s caregiving environment. It is important to consider not only the characteristics of biological mothers, but also of the individuals who assume the primary parenting responsibility for a child, to understand more fully the context in which the child’s development occurs. Recognition of the importance of primary caregivers’ mental health needs places the child’s behavioral problems in the context of the larger family system. This is particularly important in working with vulnerable, high-risk populations such as perinatal substance users. There is increased recognition that a family-oriented approach is needed to promote more adaptive parenting in substance-using mothers and to reduce risk for adverse child outcomes (Whitaker et al., 2006). Interventions that address both child and parental or PC needs can create opportunities for more favorable child outcomes. Longitudinal follow-up can further determine the behavioral trajectories of children with prenatal MA exposure, as they move into school settings where they face increased academic, social, and behavioral demands.
Contributor Information
Jean Twomey, Warren Alpert Medical School at Brown University and Women and Infants Hospital.
Linda LaGasse, Warren Alpert Medical School at Brown University and Women and Infants Hospital.
Chris Derauf, Mayo Clinc.
Elana Newman, University of Tulsa.
Rizwan Shah, Blank Hospital Regional Child Protection Center.
Lynne Smith, LABioMed Institute at Harbor-UCLA Medical Center.
Amelia Arria, University of Maryland.
Marilyn Huestis, National Institute on Drug Abuse.
Sheri DellaGrotta, Warren Alpert Medical School at Brown University and Women and Infants Hospital.
Mary Roberts, Warren Alpert Medical School at Brown University and Women and Infants Hospital.
Lynne Dansereau, Warren Alpert Medical School at Brown University and Women and Infants Hospital.
Charles Neal, University of Hawaii.
Barry Lester, Warren Alpert Medical School at Brown University and Women and Infants Hospital.
References
- Abidin RR. Parenting Stress Index manual. Lutz, FL: Psychological Assessment Resources; 1990. [Google Scholar]
- Achenbach TM, Rescorla L. Manual for the ASEBA preschool forms and profiles. Burlington: University of Vermont, Research Center for Children, Youth, & Families; 2000. [Google Scholar]
- Arria AM, Derauf C, LaGasse LL, Grant P, Shah R, Smith L, Lester B. Methamphetamine and other substance use during pregnancy: Preliminary estimates from the Infant Development, Environment, and Lifestyle (IDEAL) Study. Maternal and Child Health Journal. 2006;10:293–302. doi: 10.1007/s10995-005-0052-0. [DOI] [PubMed] [Google Scholar]
- Billing L, Eriksson M, Jonsson B, Steneroth G, Zetterstrom R. The influence of environmental factors on behavioural problems in 8-year-old children exposed to amphetamine during fetal life. Child Abuse and Neglect. 1994;18:3–9. doi: 10.1016/0145-2134(94)90091-4. [DOI] [PubMed] [Google Scholar]
- Billing L, Eriksson M, Steneroth G, Zetterstrom R. Predictive indicators for adjustment in 4-year-old children whose mothers used amphetamine during pregnancy. Child Abuse and Neglect. 1988;12:503–507. doi: 10.1016/0145-2134(88)90067-1. [DOI] [PubMed] [Google Scholar]
- Caldwell BM, Bradley RH. HOME Inventory administration manual. 3. Little Rock: University of Arkansas; 2001. [Google Scholar]
- Carnevale J. The current status of the methamphetamine epidemic. Gaithersburg, MD: Carnevale Associates; 2011. (Policy Brief) [Google Scholar]
- Carta JJ, Atwater JB, Greenwood CR, McConnell SR, McEvoy MA, Williams R. Effects of cumulative prenatal substance exposure and environmental risks on children’s developmental trajectories. Journal of Clinical Child Psychology. 2001;30:327–337. doi: 10.1207/S15374424JCCP3003_5. [DOI] [PubMed] [Google Scholar]
- Cernerud L, Eriksson M, Jonsson B, Steneroth G, Zetterstrom R. Amphetamine addiction during pregnancy: 14-year followup of growth and school performance. Acta Paediatrica. 1996;85:204–208. doi: 10.1111/j.1651-2227.1996.tb13993.x. [DOI] [PubMed] [Google Scholar]
- Cohen JB, Dickow A, Horner K, Zweben JE, Balabis J, Vandersloot D, Reiber C. Abuse and violence history of men and women in treatment for methamphetamine dependence. American Journal on Addictions. 2003;12:377–385. [PubMed] [Google Scholar]
- Davies D. Child development: A practitioner’s guide. 3. New York, NY: The Guilford Press; 2011. [Google Scholar]
- DellaGrotta S, LaGasse LL, Arria AM, Derauf C, Grant P, Smith LM, Lester BM. Patterns of methamphetamine use during pregnancy: Results from the Infant Development, Environment, and Lifestyle (IDEAL) Study. Maternal and Child Health Journal. 2009;14:519–527. doi: 10.1007/s10995-009-0491-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derauf C, LaGasse LL, Smith LM, Grant P, Shah R, Arria A, Lester BM. Demographic and psychosocial characteristics of mothers using methamphetamine during pregnancy: Preliminary results from the Infant Development, Environment, and Lifestyle Study (IDEAL) American Journal of Drug and Alcohol Abuse. 2007;33:281–289. doi: 10.1080/00952990601175029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR. Brief Symptom Inventory: Administration, scoring, and procedures manual. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- Hans SL. Demographic and psychosocial characteristics of substance-abusing pregnant women. Clinical Perinatology. 1999;26:55–74. [PubMed] [Google Scholar]
- Hans SL. Studies of prenatal exposure to drugs focusing on parental care of children. Neurotoxicology and Teratology. 2002;24:329–337. doi: 10.1016/s0892-0362(02)00195-2. [DOI] [PubMed] [Google Scholar]
- Huestis MA, Choo RE. Drug abuse’s smallest victims: In utero drug exposure. Forensic Science International. 2002;128:20–30. doi: 10.1016/s0379-0738(02)00160-3. [DOI] [PubMed] [Google Scholar]
- Keegan J, Parva M, Finnegan M, Gerson A, Belden M. Addiction in pregnancy. Journal of Addictive Diseases. 2010;29:175–191. doi: 10.1080/10550881003684723. [DOI] [PubMed] [Google Scholar]
- LaGasse L, Derauf C, Smith LM, Newman E, Shah R, Neal C, Lester BM. Prenatal methamphetamine exposure and childhood behavior problems at 3 and 5 years of age. Pediatrics. 2012;129:681–688. doi: 10.1542/peds.2011-2209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaGasse LL, Seifer R, Wright LL, Lester BM, Tronick EZ, Bauer CR, Smeriglid V. The Maternal Lifestyle Study (MLS): The caretaking environment of infants exposed to cocaine/opiates. Pediatric Research. 1999;45(No 4 Part 2) [Google Scholar]
- LaGasse LL, Wouldes T, Newman E, Smith LM, Shah RZ, Derauf C, Lester BM. Prenatal methamphetamine exposure and neonatal neurobehavioral outcome in the USA and New Zealand. Neurotoxicology and Teratology. 2011;33:166–175. doi: 10.1016/j.ntt.2010.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester BM, Bagner DM, Liu J, LaGasse LL, Seifer R, Bauer CR, Abhik D. Infant neurobehavioral dysregulation: Behavior problems in children with prenatal substance exposure. Pediatrics. 2009;124:1354–1361. doi: 10.1542/peds.2008-2898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester BM, Lagasse LL. Children of addicted women. Journal of Addictive Diseases. 2010;29:259–276. doi: 10.1080/10550881003684921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liles BD, Newman E, LaGasse LL, Derauf C, Shah R, Smith LM, Lester BM. Perceived child behavior problems, parenting stress, and maternal depressive symptoms among prenatal methamphetamine users. Child Psychiatry and Human Development. 2012;43:943–957. doi: 10.1007/s10578-012-0305-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medrano MA, Zule WA, Hatch J, Desmond DP. Prevalence of childhood trauma in a community sample of substance- abusing women. American Journal of Drug and Alcohol Abuse. 1999;25:449–462. doi: 10.1081/ada-100101872. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Sonn J, Walsh M, Weiss RD. Domestic violence in women with PTSD and substance abuse. Addictive Behaviors. 2004;29:707–715. doi: 10.1016/j.addbeh.2004.01.003. [DOI] [PubMed] [Google Scholar]
- Nguyen D, Smith LM, LaGasse LL, Derauf C, Grant P, Shah R, Lester BM. Intrauterine growth of infants exposed to prenatal methamphetamine: Results from the Infant Development, Environment, and Lifestyle Study. Journal of Pediatrics. 2010;157:337–339. doi: 10.1016/j.jpeds.2010.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oei J, Abdel-Latif ME, Clark R, Craig F, Lui K. Short-term outcomes of mothers and infants exposed to antenatal amphetamines. Archives of Diseases in Childhood Fetal Neonatal Edition. 2010;95:F36–F41. doi: 10.1136/adc.2008.157305. [DOI] [PubMed] [Google Scholar]
- Shonkoff J, Phillips D, editors. From neurons to neighborhoods: The science of early childhood development. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- Smith LM, LaGasse LL, Derauf C, Grant P, Shah R, Arria A, Lester BM. The Infant Development, Environment, and Lifestyle Study: Effects of prenatal methamphetamine exposure, polydrug exposure, and poverty on intrauterine growth. Pediatrics. 2006;118:1149–1156. doi: 10.1542/peds.2005-2564. [DOI] [PubMed] [Google Scholar]
- Smith LM, LaGasse LL, Derauf C, Grant P, Shah R, Arria A, Lester BM. Prenatal methamphetamine use and neonatal neurobehavioral outcome. Neurotoxicology and Teratology. 2008;30:20–28. doi: 10.1016/j.ntt.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LM, LaGasse LL, Derauf C, Newman E, Shah R, Haning W, Lester BM. Motor and cognitive outcomes through three years of age in children exposed to prenatal methamphetamine. Neurotoxicology and Teratology. 2011;33:176–184. doi: 10.1016/j.ntt.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. NSDUH Series H-38A (HHS Publication No SMA 10-4586 Findings) Rockville, MD: Author; 2010a. Results from the 2009 national survey on drug use and health: Volume I. Summary of national findings. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. DASIS Series: S-55 (HHS Publication No SMA 10-4613) Rockville, MD: Author; 2010b. Treatment episode data set (TEDS): 1998–2008. State admissions to substance abuse treatment services. [Google Scholar]
- Suchman NE, McMahon TJ, Slade A, Luthar SS. How early bonding, depression, illicit drug use, and perceived support work together to influence drug-dependent mothers’ caregiving. American Journal of Orthopsychiatry. 2005;75:431–445. doi: 10.1037/0002-9432.75.3.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan TP, Holt LJ. PTSD symptom clusters are differentially related to substance use among community women exposed to intimate partner violence. Journal of Traumatic Stress. 2008;21:173–180. doi: 10.1002/jts.20318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terplan M, Smith EJ, Kozloski MJ. Methamphetamine use among pregnant women. Obstetrics and Gynecology. 2009;113:1285–1291. doi: 10.1097/AOG.0b013e3181a5ec6f. [DOI] [PubMed] [Google Scholar]
- Whitaker RC, Orzol SM, Kahn RS. Maternal mental health, substance use, and domestic violence in the year after delivery and subsequent behavior problems in children at age 3 years. Archives of General Psychiatry. 2006;63:551–560. doi: 10.1001/archpsyc.63.5.551. [DOI] [PubMed] [Google Scholar]
- Wouldes T, LaGasse L, Sheridan J, Lester B. Maternal methamphetamine use during pregnancy and child outcome: What do we know? New Zealand Medical Journal. 2004;117:1–10. [PubMed] [Google Scholar]
- Zabaneh R, Smith LM, LaGasse LL, Derauf C, Newman E, Shah R, Lester BM. The effects of prenatal methamphetamine exposure on childhood growth patterns from birth to 3 years of age. American Journal of Perinatology. 2011;29:203–210. doi: 10.1055/s-0031-1285094. [DOI] [PMC free article] [PubMed] [Google Scholar]