Abstract
Background
Axis IV is for reporting “psychosocial and environmental problems that may affect the diagnosis, treatment, and prognosis of mental disorders.” No studies have examined the prognostic value of Axis IV in DSM-IV.
Method
We analyzed data from 2,497 participants in the National Epidemiologic Survey on Alcohol and Related Conditions with major depressive episode (MDE). We hypothesized that psychosocial stressors predict a poor prognosis of MDE. Secondarily, we hypothesized that psychosocial stressors predict a poor prognosis of anxiety and substance use disorders. Stressors were defined according to DSM-IV’s taxonomy, and empirically using latent class analysis.
Results
Primary support group problems, occupational problems, and childhood adversity increased the risks of depressive episodes and suicidal ideation by 20–30%. Associations of the empirically derived classes of stressors with depression were larger in magnitude. Economic stressors conferred a 1.5-fold increase in risk for a depressive episode (CI=1.2–1.9); financial and interpersonal instability conferred a 1.3-fold increased risk of recurrent depression (CI=1.1–1.6). These two classes of stressors also predicted the recurrence of anxiety and substance use disorders. Stressors were not related to suicidal ideation independent from depression severity.
Conclusions
Psychosocial and environmental problems are associated with the prognosis of MDE and other Axis I disorders. Though DSM-IV’s taxonomy of stressors stands to be improved, these results provide empirical support for the prognostic value of Axis IV. Future work is needed to determine the reliability of Axis IV assessments in clinical practice, and the usefulness of this information to improving the clinical course of mental disorders.
INTRODUCTION
The presence of environmental stressors has since DSM-III factored into an individual’s psychiatric evaluation via Axis IV of DSM’s multi-axial system (Williams, 1985a). According to DSM-IV (see Text Box), “Axis IV is for reporting psychosocial and environmental problems that may affect the diagnosis, treatment, and prognosis of mental disorders” (DSM-IV, p.31). The problems that are relevant for reporting on Axis IV include those problems that might be etiologically relevant to the disorder (e.g., as precipitants of the current episode), as well as those that are relevant to the future course of the disorder. Though DSM-IV limits the problems that should be reported on Axis IV to those that have occurred within the past year, problems prior to the past year may also be reported if they are clearly relevant to the current disorder.
TEXT BOX. Axis IV: Psychosocial and Environmental Problems (DSM-IV-TR, p. 31).
“Axis IV is for reporting psychosocial and environmental problems that may affect the diagnosis, treatment, and prognosis of mental disorders (Axes I and II). A psychosocial or environmental problem may be a negative life event, and environmental difficulty or deficiency, a familial or other interpersonal stress, and inadequacy of social support or personal resources, or other problem relating to the context in which a person’s difficulties have developed. So-called positive stressors, such as job promotion, should be listed only if they constitute or lead to a problem, as when a person has difficulty adapting to the new situation. In addition to playing a role in the initiation or exacerbation of a mental disorder, psychosocial problems may also develop as a consequence of a person’s psychopathology or may constitute problems that should be considered in the overall management plan.
“When an individual has multiple psychosocial or environmental problems, the clinician may note as many as are judged to be relevant. In general, the clinician should note only those psychosocial and environmental problems that have been present during the year preceding the current evaluation. However, the clinician may choose to note psychosocial and environmental problems occurring prior to the previous year if these clearly contribute to the mental disorder or have become a focus of treatment—for example, previous combat experiences leading to Posttraumatic Stress Disorder.”
It is unclear what role Axis IV currently plays in clinical practice (Skodol, 1997), and the evidence for maintaining Axis IV is scant. We have been unable to identify any empirical investigations of the validity or clinical utility of the DSM-IV version of Axis IV. In DSM-III and DSM-III-R, Axis IV was formulated as a rating scale of the severity of psychosocial stressors (Moncur and Luthra, 2009). The reliability and validity of that rating scale were evaluated, with mixed results (Plapp et al., 1987, Rey et al., 1987a, Rey et al., 1987b, 1988, Skodol and Shrout, 1988, 1989a, b, Zimmerman et al., 1985). For example, with respect to its predictive validity, Zimmerman et al. found that among patients hospitalized for depression, higher scores on the Axis IV rating scale were associated with higher levels of depressive symptoms at hospital discharge, but were unrelated to their depression outcomes after six months of follow-up (Zimmerman et al., 1987).
Axis IV in its current formulation delineates nine categories of “psychosocial and environmental” problems that should be documented as part of a patient’s diagnostic evaluation: problems with primary support group, problems related to the social environment, educational problems, occupational problems, housing problems, economic problems, problems with access to health care services, problems related to interactions with the legal system/crime, and other psychosocial and environmental problems. In theory, information regarding these problems should aid in the development of treatment plans and in the identification of potential barriers to treatment adherence (Moncur and Luthra, 2009). The clinical utility of Axis IV, as Zimmerman et al. noted, ultimately “rests with its relation to prognosis” (Zimmerman et al., 1985, p.1140).
Evidence from clinical samples suggests that environmental stressors such as those indicated on Axis IV are predictive of depression relapse. For example, social support problems were predictive of poor treatment outcomes—i.e., lack of full remission—in an outpatient sample being treated for depression (Ezquiaga et al., 1999). Brown et al. reported that exposure to serious life events was associated with worse depression outcomes (Brown et al., 2010), and Monroe et al. and Lenze et al. reported worse depression outcomes in the context of non-severe life events (Lenze et al., 2008, Monroe et al., 2006). It is unclear whether these findings extend to non-clinical samples.
We address two issues of concern regarding Axis IV, which have specific relevance to depression. First, does the presence of psychosocial problems predict the prognosis of depression? Second, is there evidence for the validity of the taxonomy of psychosocial and environmental problems outlined in DSM-IV? This study is based on a population-based sample of individuals with depression, and followed prospectively for 3 years. We investigate whether and which types of psychosocial problems at baseline predict depression prognosis during the follow-up period. In addition to examining DSM-IV’s taxonomy of psychosocial stressors listed above, we apply latent class analysis to an inventory of life stressors in the past year in order to evaluate the predictive validity of an empirically derived taxonomy of stressors. Finally, we conduct comparative analyses of a broader range of anxiety and substance use disorders to evaluate the utility of Axis IV beyond the diagnosis of major depression.
METHOD
Sample
Data come from the National Epidemiology Survey on Alcohol and Related Conditions (NESARC), a two-wave, nationally representative household survey (Hasin et al., 2005). The Wave 1 sample included 43,093 adult participants. The Wave 2 survey, conducted approximately 3 years later, included 34,653 of the 39,959 Wave 1 participants eligible for follow-up. The combined response rate for both waves was 70.2% (Dawson et al., 2007). The primary analytic sample for the current study included participants with a diagnosis of major depressive episode (MDE) in the 12 months preceding the Wave 1 interview who were followed up at Wave 2, and who provided complete data on all study covariates. Secondary analyses were conducted among participants with any mood, anxiety, or substance use disorder in the 12 months preceding the Wave 1 interview who were followed up at Wave 2.
Measures
Past-year MDE was assessed using the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS) (Grant and Dawson, 2001, Grant et al., 2003). The AUDADIS algorithm for MDE requires ≥5 clinically significant symptoms of depression occurring during a 2-week period of sadness or anhedonia (Hasin et al., 2005). The test-retest reliability of depression diagnoses over a period of 2–3 months was good (kappa=0.65 for a lifetime diagnosis of major depression, and 0.59 for a past-year diagnosis) (Grant et al., 2003). The following features of depression assessed at Wave 1 were also included in the analyses: number of DSM-IV criterion ‘A’ symptoms of MDE; level of impairment, defined as the number of the NESARC’s 8 impairment items related to depression that were endorsed; and the number of lifetime depressive episodes.
We investigated two outcomes of depression assessed at the Wave 2 follow-up interview. The first was the presence of any depressive episode during the follow-up period. The second was any suicidal thoughts or attempts during the follow-up period. Suicidal thoughts were assessed at Wave 2 from participants who reported either two weeks of depressed mood or loss of interest since the Wave 1 interview, whereas suicidal attempts were assessed from all Wave 2 participants. We also investigated the role of psychosocial stressors in predicting episodes of the following disorders during the NESARC’s follow-up period: social phobia, panic disorder, generalized anxiety disorder, alcohol dependence and substance dependence.
The presence or absence of the following psychosocial and environmental problems in the 12 months prior to the Wave 1 interview were assessed: 1) death of a close friend or family member; 2) serious illness or injury of a close friend or family member; 3) separation, divorce, or end of a serious relationship; 4) serious problems with a neighbor, friend, or relative; 5) being fired or laid off; 6) currently unemployed or unemployed for >1 month during the past year; 7) trouble with boss or coworker; 8) change of jobs, responsibilities, or work hours; 9) experienced a major financial crisis, declared bankruptcy, or more than once been unable to pay bills on time; 10) household income less than 150% of the federal poverty threshold; 11) received public assistance (e.g., welfare, food stamps); 12) lack of health insurance; 13) trouble with the police, arrested, or sent to jail; and 14) victim of a crime. The test-retest reliability of the NESARC’s assessment of stressful life events over a 6-week period was excellent (intra-class correlation=0.94) (Ruan et al., 2008).
We analyzed these 14 indicators of psychosocial and environmental problems in the following two ways. First, we grouped them into the categories of stressors outlined in the description of Axis IV in DSM-IV. The categories were: problems with primary support group (problems 1, 2, and 3), problems related to the social environment (problem 4), occupational problems (problems 5 through 8), economic problems (problems 9, 10, and 11), problems with access to health care services (item 12), problems related to interaction with the legal system/crime (problems 13 and 14). There were three categories of problems outlined in DSM-IV that we could not assess: educational problems, housing problems, and a generic category of “other” psychosocial problems.
Second, we used latent class analysis (LCA) to derive empirically based groupings of individuals based on their experiences of the above 14 stressors (McCutcheon, 1987). In LCA, correlations among the observed dependent variables (the 14 stressors) are related to a categorical latent variable through a set of logistic regression equations. The number of categories is determined by fitting multiple LCA models and then selecting the best-fitting model using summary statistics of model fit. The results of the LCA were used to assign each individual to a specific class, which was used as a predictor of depression course. The LCA was implemented in Mplus, with adjustments made for the complex sampling design of the NESARC (Muthen and Muthen, 1998–2010).
We also analyzed childhood adversities in order to evaluate the relevance to Axis IV of stressors that occurred prior to the current depression. These were assessed retrospectively at the Wave 2 interview (Benjet et al., 2010, Clark et al., 2010, Salum et al., 2010). The childhood adversities included standardized indices of childhood abuse (including neglect, verbal abuse, and physical abuse) and sexual maltreatment, and a dichotomous indicator of childhood economic deprivation. Abuse and maltreatment during childhood were assessed via a series of items asking participants about their frequency of exposure to different types of adversities, which they rated on a 5-point scale anchored by ‘Never’ and ‘Very Often.’ The test-retest reliabilities of these childhood adversities in the NESARC are excellent, with intra-class correlations ranging from 0.80 to 0.94 (Ruan et al., 2008). Childhood economic deprivation was defined as receiving government financial assistance before age 18.
Additional adjustment factors that we included in the analyses were co-occurring anxiety (generalized anxiety disorder, panic disorder, or social phobia) and substance (alcohol or substance dependence) disorders, and participant demographic factors (age, sex, educational attainment, and race/ethnicity). These factors were included in the analyses because they are known to be associated with both stressful life events and psychopathology, and could therefore be potential confounding variables.
Analysis of depression outcomes and other psychiatric disorders during the follow-up period
The study design involved fitting Poisson regression models for a depressive episode and for suicidal thoughts or attempts occurring between the Wave 1 and Wave 2 interviews. This model yields regression coefficients that, when exponentiated, can be interpreted as prevalence ratios (Zou, 2004). For each outcome, we fitted models that included the DSM-IV categories of the psychosocial and environmental problems (with and without adjusting for past-year comorbid disorders, indicators of depression severity, and childhood adversities), and models that included the stress exposure groupings from the LCA. The descriptive analyses and the Poisson regression analyses were conducted in SUDAAN (Research Triangle Institute, 2004), which adjusts variances and point estimates for the multi-stage sampling design and differential selection probabilities used to ascertain the NESARC sample. Percentages are weighted using the study’s Wave 2 sampling weights; actual sample sizes are reported.
RESULTS
The prevalence of past-year depression in the NESARC sample at baseline is 7.9% (n=3,485). Among these individuals, 2,497 (73.4%) participated in the follow-up interview and had complete data on all variables included in the present study, and therefore constitute the primary analytic sample. The analysis sample is predominantly female (66.6%) and White (74.4%). One-third of the sample was enrolled between ages 18–29 (30.3%), and approximately half of the sample (54.7%) had at least some college education. Two-fifths of the sample had a depressive episode during the follow-up period (39.5%, n=1,002). Most of these individuals (93.2%, n=944) had at least one recurrent episode, meaning that they experienced the onset of a new depressive episode following >2 months of improved mood and resolution of accompanying symptoms. Almost one-fifth of the sample reported suicidal thoughts or attempts during the follow-up period (16.4%, n=419).
The distribution of psychosocial and environmental stressors at baseline is presented in table 1. The first column presents the distribution of each stressor in the analysis sample. Support group problems were quite common, with half the sample reporting a serious illness or injury of a close friend or family member. Economic problems were somewhat less common, with approximately one-third of the sample reporting a major financial problem or a household income less than 150% of the poverty threshold. The second and third columns indicate the associations of each stressor with the likelihood of a depressive episode (second column) and suicidal thoughts or attempts (third column) during the three-year follow-up period of the NESARC. Compared to the risks of depression (39.5%) and suicidal thoughts or attempts (16.4%) in the sample overall, risks of depression were elevated among those reporting economic and legal problems (ranging from 44–49%), and risks of suicidal thoughts or attempts were elevated among individuals reporting social, economic, and legal problems (ranging from 20–24%).
Table 1.
Distribution of psychosocial and environmental problems among participants with a diagnosis of major depressive episode at the baseline interview of the National Epidemiologic Survey on Alcohol and Related Conditions, and who participated in the three-year follow-up interview.
| Distribution in the analysis samplea % (se) | Percentage with a depressive episode at follow-up % (se) | Percentage with suicidal ideation at follow-up % (se) | |
|---|---|---|---|
| Problems with primary support group | |||
| 1. Death of a close friend or family member | 37.8 (1.3) | 42.2 (2.0) | 16.8 (1.4) |
| 2. Serious illness or injury of a close friend or family member | 50.0 (1.3) | 43.5 (1.7) | 17.3 (1.3) |
| 3. Separated, divorced, or break off a serious relationship | 16.9 (0.9) | 41.8 (2.9) | 22.0 (2.3) |
| Any of the above | 67.6 (1.3) | 42.3 (1.4) | 17.8 (1.2) |
| Problems related to the social environment | |||
| 4. Serious problems with a neighbor, friend, or relative | 19.1 (1.1) | 46.4 (3.1) | 23.8 (2.5) |
| Occupational problems | |||
| 5. Fired or laid off | 12.8 (0.9) | 39.1 (3.5) | 21.0 (3.0) |
| 6. Currently unemployed or unemployed for >1 month during the past year | 29.1 (1.2) | 44.7 (2.3) | 23.3 (1.9) |
| 7. Trouble with boss or coworker | 19.5 (1.0) | 41.1 (2.7) | 18.8 (2.2) |
| 8. Changed jobs, responsibilities, or work hours | 39.1 (1.2) | 38.9 (2.0) | 16.8 (1.4) |
| Any of the above | 59.4 (1.2) | 42.3 (1.7) | 19.4 (1.3) |
| Economic problems | |||
| 9. Experienced a major financial crisis, declared bankruptcy, or more than once been unable to pay bills on time | 31.2 (1.2) | 45.7 (2.3) | 23.1 (1.8) |
| 10. Household income less than 150% of the federal poverty threshold | 30.4 (1.2) | 45.2 (2.3) | 21.4 (1.8) |
| 11. Received public assistance | 13.2 (0.9) | 48.7 (3.3) | 24.0 (2.6) |
| Any of the above | 49.0 (1.3) | 44.0 (1.9) | 20.8 (1.4) |
| Problems with access to health care services | |||
| 12. Lack of health insurance | 21.8 (1.1) | 36.6 (2.5) | 16.4 (1.9) |
| Problems related to interaction with the legal system/crime | |||
| 13. Trouble with the police, arrested, or sent to jail | 14.0 (0.9) | 47.5 (3.3) | 24.1 (3.0) |
| 14. Victim of a crime | 13.7 (0.9) | 43.9 (3.4) | 22.4 (2.8) |
| Any of the above | 23.2 (1.1) | 44.5 (2.7) | 21.9 (2.1) |
Analysis sample includes n=2,497 participants with major depression who were reinterviewed at follow-up, and with complete data.
Proportion with major depression during the follow-up period, 39.5% (n=1,002).
Proportion with suicidal thoughts or attempts during the follow-up period, 16.4% (n=419).
Risks for a depressive episode during the NESARC’s follow-up period are presented in table 2. Three models were fitted: model 1 for each category of stressor, model 2 adding in childhood adversities, and model 3 adding comorbid anxiety and substance disorders, and indicators of depression severity (e.g., number of symptoms, level of impairment, number of lifetime episodes). The categories of stressors that were significantly (P<0.05) associated with a depressive episode in the first model were problems with social support group (prevalence ratio (PR)=1.18; 95% confidence interval (CI)=1.04–1.34), occupational problems (PR=1.15; CI=1.00–1.32), and economic problems (PR=1.15; CI=1.00–1.33). The association between social support group problems and recurrent depression remained in the second and third models that controlled for childhood adversities and clinical control variables (PR=1.17; CI=1.04–1.32). In the final model adjusting for all covariates (model 3), higher scores on the childhood adversity index (PR=1.07; CI=1.03–1.11) were also associated with recurrent depressive episodes during the follow-up period.
Table 2.
Psychosocial and environmental predictors of a Wave 2 depressive episode during the 3-year follow-up period of the National Epidemiologic Survey on Alcohol and Related Conditions.
| Model 1a PR (95% CI) |
Model 2a PR (95% CI) |
Model 3a,b PR (95% CI) |
|
|---|---|---|---|
| Problems with social support group | 1.18 (1.04, 1.34) | 1.18 (1.04, 1.34) | 1.17 (1.04, 1.32) |
| Social or environmental problems | 1.08 (0.93, 1.25) | 1.06 (0.92, 1.21) | 0.97 (0.85, 1.11) |
| Occupational problems | 1.15 (1.00, 1.32) | 1.13 (0.99, 1.30) | 1.10 (0.97, 1.26) |
| Economic problems | 1.15 (1.00, 1.33) | 1.14 (0.99, 1.32) | 1.10 (0.97, 1.26) |
| Lack of health insurance | 0.86 (0.74, 1.00) | 0.86 (0.74, 1.00) | 0.85 (0.74, 0.98) |
| Legal problems | 1.10 (0.96, 1.26) | 1.07 (0.94, 1.22) | 1.03 (0.91, 1.17) |
| Childhood adversity index | 1.10 (1.05, 1.14) | 1.07 (1.03, 1.11) | |
| Childhood sexual maltreatment index | 1.00 (0.99, 1.02) | 0.99 (0.98, 1.01) | |
| Family on welfare during childhood | 0.94 (0.80, 1.10) | 0.91 (0.77, 1.06) |
Additional control variables not shown: age at enrollment, sex, educational attainment, and race/ethnicity.
Additionally controlling for prior anxiety and substance disorders, the number of criterion ‘A’ depressive symptoms, level of impairment, and number of lifetime depressive episodes.
PR indicates prevalence ratio.
A similar set of models was fitted for suicidal thoughts or attempts during the follow-up period (table 3). Three categories of stressors were initially predictive of suicidal thoughts or attempts: social or environmental problems (PR=1.30; CI=1.01–1.67); occupational problems (PR=1.34; CI=1.04–1.72); and economic problems (PR=1.39; CI=1.09–1.79). These associations were attenuated slightly when childhood adversities were added in model 2, and were more substantially reduced when comorbid anxiety and substance disorders and indicators of depression severity were added in model 3. In the final analysis, the only psychosocial predictor of suicidal ideation during the follow-up period was the childhood adversity index (PR=1.10; CI=1.02–1.18).
Table 3.
Psychosocial and environmental predictors of suicidal ideation assessed at the three-year follow-up interview of the National Epidemiologic Survey on Alcohol and Related Conditions.a
| Model 1a PR (95% CI) |
Model 2a PR (95% CI) |
Model 3a,b PR (95% CI) |
|
|---|---|---|---|
| Problems with social support group | 1.15 (0.88, 1.50) | 1.13 (0.86, 1.48) | 1.12 (0.85, 1.46) |
| Social or environmental problems | 1.30 (1.01, 1.67) | 1.26 (0.99, 1.60) | 1.13 (0.90, 1.43) |
| Occupational problems | 1.34 (1.04, 1.72) | 1.29 (1.01, 1.65) | 1.23 (0.97, 1.57) |
| Economic problems | 1.39 (1.09, 1.79) | 1.33 (1.04, 1.70) | 1.22 (0.96, 1.55) |
| Lack of health insurance | 0.84 (0.64, 1.10) | 0.85 (0.65, 1.11) | 0.85 (0.66, 1.09) |
| Legal problems | 1.20 (0.94, 1.54) | 1.13 (0.88, 1.44) | 1.08 (0.85, 1.36) |
| Childhood adversity index | 1.13 (1.05, 1.21) | 1.10 (1.02, 1.18) | |
| Childhood sexual maltreatment index | 1.03 (0.99, 1.06) | 1.01 (0.98, 1.04) | |
| Family on welfare during childhood | 1.26 (0.99, 1.60) | 1.19 (0.95, 1.49) |
Additional control variables not shown: age at enrollment, sex, educational attainment, and race/ethnicity.
Additionally controlling for prior anxiety and substance disorders, the number of criterion ‘A’ depressive symptoms, level of impairment, and number of lifetime depressive episodes.
PR indicates prevalence ratio.
The results presented thus far are based on DSM-IV’s “taxonomy” of psychosocial and environmental problems. Using an empirically based approach to classifying stressors revealed stronger risks for poor prognosis in this sample. There were two parts to this analysis: first a LCA of the 14 stressors to extract latent classes of stress exposure (which demarcate groups of individuals with distinct patterns of stress exposure), and second, using group membership to predict psychiatric outcomes.
The best-fitting LCA model of the 14 stressors had 5 latent classes. This is based on the entropy statistic (0.71), a measure of overall classification; the sample-size adjusted BIC statistic, which had trivial reductions after adding 6 or more classes; and the VLMR likelihood ratio test statistics, which rejected a 4-class model in favor of a model with 5 classes, but failed to reject a model with 5 classes relative to a model with 6 classes (Muthen and Muthen, 1998–2010).
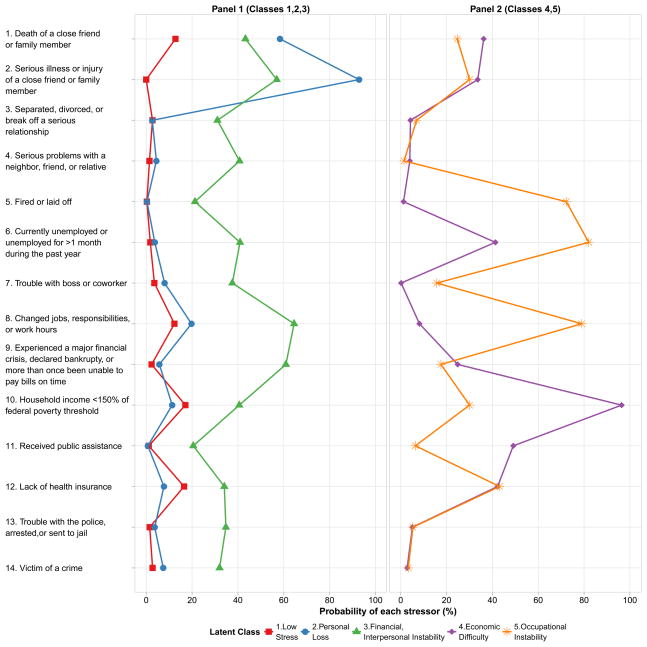
The results of the LCA are shown in figure 1, displayed across two panels for ease of interpretation. Each line represents a distinct class, and each point along the graph indicates the probability of stressors in each class. The interpretation of the LCA solution is as follows. In Panel 1, Class 1 is characterized by a low probability of exposure to all 14 stressors (“low stress exposure”). Class 2 differs from class 1 only with respect to stressors 1 and 2—death or serious illness of a close friend or family member (“personal loss”). Class 3 is characterized by a high probability of exposure to stressors 8 (job change) and 9 (major financial crisis), and is the class with the highest probabilities of exposure to stressors 13 and 14 (trouble with police, arrested or jailed, victim of a crime). We therefore label class 3 as “financial and interpersonal instability.” In Panel 2, classes 4 and 5 are shown; these two classes represent two distinct patterns of exposure to economic and occupational stressors. Class 4 is characterized by high probabilities of stressors 10 and 11 (poverty and receipt of public assistance); in contrast, class 5 is characterized by a high probability of stressors 5, 6, and 8 (fired/laid off, unemployed, and changed jobs). We therefore label class 4 as “economic difficulty,” and class 5 as “occupational instability.”
Figure 1.
Results of the latent class analysis (LCA) of 14 psychosocial and environmental problems.a
aEach line represents 1 of 5 latent classes of stress exposures. The figure shows the average probability of endorsing each stressors among participants in each latent class. The proportion of participants in each class is: 19.3% in class 1 (n=488); 25.2% in class 2 (n=636); 43.1% in class 3 (n=1,199); 8.8% in class 4 (n=304); and 3.7% in class 5 (n=99).
It is notable that some of the stressors had a high frequency in more than one class. What differentiates the classes from one another is the broader pattern of concomitant stressors. For example, changing jobs was common in class 3 and class 5. Individuals in class 3 also had a high likelihood of problems with the police and of being the victim of a crime whereas those in class 5 had a very low frequency of these stressors. In contrast, individuals in class 5 had a much higher likelihood of having been fired and of experiencing an extended period of unemployment.
The LCA generates a set of predicted probabilities of class membership; we used these predicted probabilities to assign each individual to their most likely class, and then used class membership to predict suicidal thoughts or attempts and depressive episodes during the follow-up period (table 4), and other mood, anxiety, and substance disorders (table 5). The unadjusted proportions of depressive episodes and suicidal ideation across latent classes are shown in the first column of table 4, followed by prevalence ratios comparing the risk of suicidal ideation and depression between individuals in classes 2–5 relative to class 1. In models predicting depressive episodes during the follow-up period, individuals in the classes characterized by personal loss, financial/interpersonal instability, and economic difficulty were all at significantly greater risk than individuals in the low stress exposure class (PR=1.27, 1.33, and 1.52, respectively). A history of childhood adversity was also associated with the prognosis of major depression (PR=1.07; CI=1.03, 1.11).
Table 4.
Psychosocial and environmental predictors, based on latent class analysis, of suicidal ideation and depressive episodes during the three-year follow-up period of the National Epidemiologic Survey on Alcohol and Related Conditions.a
| Depressive Episode
|
Suicidal Ideation
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Risk of a recurrent depressive episode in each class % (SE) | Model 1a PR (95% CI) |
Model 2a | Model 3b PR (95% CI) |
Risk of suicidal ideation in each class % (SE) | Model 1a PR (95% CI) |
Model 2a | Model 3b PR (95% CI) |
|
| Class 1, “low stress exposure” | 28.1 (2.3) | 1 | 1 | 1 | 9.6 (1.7) | 1 | 1 | 1 |
| Class 2, “personal loss” | 37.4 (2.4) | 1.29 (1.06, 1.58) | 1.28 (1.04, 1.56) | 1.27 (1.05, 1.55) | 12.2 (1.6) | 1.29 (0.82, 2.03) | 1.21 (0.77, 1.90) | 1.19 (0.75, 1.87) |
| Class 3, “financial, interpersonal instability” | 44.9 (2.0) | 1.55 (1.28, 1.88) | 1.48 (1.22, 1.80) | 1.33 (1.11, 1.61) | 21.5 (1.6) | 2.01 (1.36, 2.98) | 1.78 (1.20, 2.63) | 1.46 (0.97, 2.19) |
| Class 4, “economic difficulty” | 47.9 (3.7) | 1.60 (1.27, 2.01) | 1.58 (1.25, 1.98) | 1.52 (1.21, 1.90) | 18.2 (2.9) | 1.75 (1.09, 2.80) | 1.59 (0.99, 2.55) | 1.49 (0.92, 2.41) |
| Class 5, “occupational instability” | 30.6 (6.6) | 1.12 (0.69, 1.80) | 1.13 (0.70, 1.82) | 1.06 (0.68, 1.64) | 16.8 (5.1) | 1.65 (0.86, 3.17) | 1.60 (0.84, 3.03) | 1.39 (0.76, 2.56) |
| Childhood adversity index | 1.10 (1.05, 1.14) | 1.07 (1.03, 1.11) | 1.13 (1.05, 1.22) | 1.09 (1.02, 1.18) | ||||
| Childhood sexual maltreatment index | 1.01 (0.99, 1.02) | 0.99 (0.98, 1.01) | 1.03 (1.00, 1.06) | 1.01 (0.98, 1.04) | ||||
| Family on welfare during childhood | 0.94 (0.80, 1.10) | 0.92 (0.78, 1.08) | 1.27 (1.00, 1.61) | 1.20 (0.95, 1.51) | ||||
| Model AUC statistic | 0.63 | 0.65 | 0.70 | 0.63 | 0.67 | 0.72 | ||
Additional control variables not shown: age at enrollment, sex, educational attainment, and race/ethnicity.
Additionally adjusted for anxiety and substance disorders, the number of criterion ‘A’ depressive symptoms, level of impairment, and number of lifetime depressive episodes.
Table 5.
Psychosocial and environmental predictors, based on latent class analysis, of anxiety and substance use disorders during the three-year follow-up period of the National Epidemiologic Survey on Alcohol and Related Conditions.a
| Social Phobia (N=582) | Panic (n=619) | GAD (n=751) | Alcohol Dependence (n=953) | Substance Dependence (n=2,904) | |
|---|---|---|---|---|---|
|
| |||||
| Proportion of participants with the outcome disorder in each class during the 3-year follow-up period
|
|||||
| % (SE) | % (SE) | % (SE) | % (SE) | % (SE) | |
| Class 1, “low stress exposure” | 6.5 (0.7) | 5.4 (0.6) | 6.6 (0.7) | 12.0 (0.9) | 40.1 (1.2) |
| Class 2, “personal loss” | 5.8 (0.7) | 6.9 (0.7) | 8.6 (0.8) | 10.4 (0.8) | 37.8 (1.4) |
| Class 3, “financial, interpersonal instability” | 10.4 (0.9) | 12.6 (1.0) | 16.0 (1.1) | 19.4 (1.2) | 43.1 (1.6) |
| Class 4, “economic difficulty” | 10.1 (1.3) | 11.2 (1.4) | 10.3 (1.3) | 10.2 (1.6) | 48.5 (2.4) |
| Class 5, “occupational instability” | 8.5 (1.5) | 5.4 (1.2) | 8.5 (1.6) | 21.2 (2.7) | 46.0 (2.6) |
|
Regression analysis of the outcome disorder during the 3-year follow-up period
|
|||||
| PR (95% CI) | PR (95% CI) | PR (95% CI) | PR (95% CI) | PR (95% CI) | |
| Class 1, “low stress exposure” | 1 | 1 | 1 | 1 | 1 |
| Class 2, “personal loss” | 0.80 (0.60, 1.06) | 1.15 (0.85, 1.57) | 1.15 (0.88, 1.51) | 0.98 (0.80, 1.21) | 0.98 (0.90, 1.06) |
| Class 3, “financial, interpersonal instability” | 0.91 (0.69, 1.20) | 1.34 (0.98, 1.83) | 1.45 (1.09, 1.94) | 1.31 (1.06, 1.61) | 1.11 (1.02, 1.22) |
| Class 4, “economic difficulty” | 1.25 (0.89, 1.76) | 1.55 (1.09, 2.22) | 1.22 (0.91, 1.65) | 0.94 (0.66, 1.33) | 1.19 (1.07, 1.32) |
| Class 5, “occupational instability” | 1.36 (0.92, 2.03) | 1.04 (0.65, 1.67) | 1.41 (0.90, 2.21) | 1.27 (0.94, 1.73) | 1.03 (0.91, 1.16) |
| Model AUC statistic | 0.75 | 0.75 | 0.73 | 0.75 | 0.81 |
| AUC statistic from reduced modelb | 0.64 | 0.70 | 0.69 | 0.70 | 0.64 |
Analyses in this table included data from participants in NESARC with any of the disorders listed at Wave 1 (n=7,364). Unadjusted proportions shown in the top panel; results of regression analyses shown in the bottom panel, adjusted for: age at enrollment, sex, educational attainment, race/ethnicity, childhood adversities, and the presence of mood, anxiety, and substance use disorders at Wave 1.
Reduced model omits controls for prior psychiatric history at Wave 1, indicating the predictive value of the model containing only latent classes of past-year stressors, childhood adversities, and demographic factors.
Consistent with the analyses reported in Table 3, associations between past-year stressors and suicidal ideation in model 1 were attenuated after controlling for childhood adversities (in model 2) and clinical control variables (in model 3). Higher levels of childhood adversity were independently associated with the risk of suicidal ideation during the follow-up period (PR=1.09; CI=1.02, 1.18).
The ability of the latent class categories to predict 3-year risks of suicidal ideation and depression can be quantified by the AUC statistic—that is, the area under the receiver operating characteristics curve. An AUC value of 0.5 indicates prediction no better than chance, and a value of 1.0 indicates perfect prediction. The AUC statistics for suicidal ideation and recurrent depressive episodes ranged between 0.63 and 0.72, respectively (last row of table 4). This degree of prediction could be characterized as modest, but falls in the same range as validated prediction models for physical health outcomes (e.g., 0.70 for the Framingham coronary heart disease prediction score (D’Agostino et al., 2001, Wilson, 2009)).
Finally we conducted comparative analyses of the association between latent class membership and episodes of anxiety and substance use disorders during the NESARC’s follow-up period (Table 5). The sample for these analysis comprised individuals of any of the following disorders without complete data on Wave 1 covariates that also participated at Wave 2 (n=7,364). The most consistent finding across disorders involved financial and interpersonal instability. Individuals in this latent class had elevated risks of generalized anxiety disorder, alcohol dependence, and substance dependence during the follow-up period (PR’s ranging from 1.11 to 1.45). Participants in the economic difficulty class had significantly higher risks of panic disorder (PR=1.55) and substance dependence (PR=1.19) during the follow-up period. Psychosocial and environmental problems were unrelated to social phobia during the follow-up period. The AUC statistics for these disorders are presented in the last two rows of Table 5. In the fully adjusted model for each (i.e., the model from which the PR’s were obtained), AUC’s ranged from 0.73 to 0.81. We present AUC statistics from a reduced model in the final row; the reduced model removed the clinical control variables, with the resulting AUC statistics providing an indication of the prognostic value of the psychosocial stressors and demographic factors alone (i.e, before accounting for prior psychiatric history). These AUC statistics ranged from 0.64 to 0.70, indicating that past-year and lifetime stressors have significant prognostic value for ongoing psychopathology.
DISCUSSION
One of the purposes of introducing a multi-axial system of classification into DSM-III was to incorporate into the diagnostic evaluation information on clinical features of a disorder beyond the diagnosis that are important for treatment planning (Rutter et al., 1969, Strauss, 1975, Williams, 1985a). Even at the time that DSM-IV was published, Skodol commented, “It seems reasonable to conclude that a thorough evaluation of Axis IV has yet to be done” (Skodol, 1997). In the years since, we have found no studies that have conducted such an evaluation.
We therefore sought to determine the usefulness of Axis IV in the diagnostic evaluation of major depression. We investigated whether or not psychosocial and environmental stressors were predictive of depression prognosis, indicated by recurrent depressive episodes and suicidal ideation in a nationally representative follow-up study of individuals with depression. Our results support the prognostic value of past-year and childhood psychosocial and environmental stressors in the longitudinal course of major depression. Childhood stressors were also associated with the risk of suicidal ideation among individuals with depression; however, past year-stressors did not predict suicidal ideation independently from other indicators of depression severity. We conclude from these results that the presence of psychosocial and environmental stressors should be maintained as part of the diagnostic evaluation in a multi-axial diagnostic classification.
Limitations
The NESARC’s assessment of psychosocial stressors is subject to the limitations that adhere generally to checklist-type measures of stressful life events. This includes the problem of intracategory variability; as Dohrenwend defines it, the problem is that “the actual experiences that lead a respondent to make a positive response to a given checklist category vary greatly” (Dohrenwend, 2006, p. 479). Relatedly, the NESARC’s assessment of stressors does not provide information on the meaning of the individual stressors to the participants. In prior research the relation between stressors and depressive episodes has been found to be contingent on the stressor’s psychological impact. For example, Kendler et al. demonstrated that stressors most strongly related to depressive episodes were those that evoked feelings of loss and humiliation (Kendler et al., 2003). The NESARC’s assessment of stressors did not make these distinctions, and also did not determine whether some items on the checklist—job change, for example—might have had both positive and negative mental health effects depending on the individual circumstances.
Axis IV does not posit specific dimensions of stressors that are important for the clinical course of disorders. In part, then, these limitations of the NESARC’s assessment of stressors are also limitations of Axis IV. There exists a substantial evidence base to support the development of a more sophisticated Axis IV, one which would go beyond the simple presence or absence of events and incorporate both the nature of the stressors and context in which they occur. This might include distinguishing chronic from acute stressors, and identifying stressors that impact an individual’s core identity or that individuals appraise as highly disruptive (Hammen et al., 2009, Hettema et al., 2006, Kendler et al., 2003, Kendler et al., 1999, Shrout et al., 1989). A related issue that is anticipated by Axis IV is the role of psychiatric disorders in generating stressors. In these instances, the stressors would not have been a contributing cause of the disorder but may still be associated with the risk of recurrent episodes.
An additional limitation is that we could not conduct analyses to distinguish the separate associations of stressors with episode duration, remission, and recurrence. Data from population-based studies indicate that the majority of depressive episodes remit within a period of months, and virtually all within 2 years (Eaton et al., 2008, Furukawa et al., 2008, Spijker et al., 2002). This time frame exceeds the duration of the NESARC’s follow-up period. Consistent with this evidence, 93.2% of depressive episodes reported during the follow-up period were recurrences. Our results therefore pertain directly to the role of stressors in depression recurrence and not the role of stressors in prolonging the time to recovery. Future work in samples with more fine-grained temporal resolution is needed to assess differences in risks for episode persistence and remission. Finally, while suicide attempts were assessed from all NESARC participants at the follow-up assessment, suicidal thoughts were assessed only from participants who also reported either depressed mood or loss of interest. Therefore our measure of suicidal ideation may have missed suicidal thoughts that occurred outside of the context of depression.
Conclusions
The presence of environmental stressors may play a role in worsening the prognosis of depression and other types of psychopathology. Plausible explanations for this are that, 1) stressors themselves endure over time, generate future stressors, and heighten one’s vulnerability to the effects of stress on psychopathology (McLaughlin et al., 2010, Post et al., 1986, Safford et al., 2007); and 2) psychosocial stressors reduce the effectiveness of psychiatric treatments (Cohen et al., 2009, Cohen et al., 2006). Treatment plans that address the presence of social adversity may therefore be more effective at improving the long-term course of the disorder (Brown et al., 2010).
Further work is needed to evaluate the validity of DSM-IV’s taxonomy of psychosocial and environmental problems. Stressors categorized according to the DSM-IV had statistically significant associations with depression prognosis and with suicidal thoughts or attempts, but these associations were modest in magnitude (i.e., prevalence ratios indicating 20% elevations in future risk). However, our empirically based taxonomy of stressors identified subgroups of individuals who had much more pronounced elevations in future risk—e.g., approximately 50% higher risks of a recurrent depressive episode. The results of the ROC analyses conducted suggest that the psychosocial and environmental stressors identified have prognostic value in terms of predicting recurrent episodes. These results also suggest that the presence of individual types of stressors may be of less prognostic value than the overall constellation of stressors experienced by an individual. This is because the latent classes, which summarize broad patterns of stressors to which an individual is exposed, were more strongly predictive of depression recurrence that individual stressors. We note that Chapter XXI of the International Classification of Diseases, 10th edition, describes a much broader range of psychosocial stressors than DSM-IV (World Health Organization, 2007), and that the ICD-10 taxonomy is being considered for adoption by DSM-V (American Psychiatric Association, 2010). We are not aware of evidence to support the validity of the ICD-10 taxonomy, however.
An additional finding of our study is that childhood stressors were predictive of the course of adult depression. This finding is consistent with studies demonstrating an association between childhood adversity and adult psychopathology (McLaughlin et al., 2010, Slopen et al., 2010). Fewer studies have examined associations between childhood adversity and the course of adult depression. This issue warrants much further attention as it relates to Axis IV, because DSM-IV currently limits reporting stressors that occurred prior to the past year to situations in which the stressors “clearly contribute” to the current disorder (DSM-IV, p.31).
There is minimal evidence that clinicians can reliably establish whether or not environmental stressors “clearly contribute” to an individual’s psychiatric disorder. For example, Skodol and Shrout highlighted the existence of substantial variation across clinicians in ratings of “etiologically significant stressors” (Skodol and Shrout, 1989a). Schrader et al. also reported on the difficulty that clinicians experience in judging the etiological significance of a stressor, pointing out the problem of determining the meaning of the stressor to the patient, as well as the meaning of the stressor to the clinician (Schrader et al., 1986).
When the analyses were extended to other mood, anxiety, and substance use disorders, there was a similar pattern of results. The latent classes that were most strongly predictive of recurrent depression, those characterized by financial and interpersonal instability as economic difficulty, were also predictive of these other disorders (except social phobia).
We conclude that psychosocial and environmental stressors have prognostic value for depression, as well as other mood, anxiety, and substance disorders, and therefore should be retained in the diagnostic evaluation on an axis separate from the diagnostic criteria. Unfortunately, advancing the theoretical and empirical basis for Axis IV has not played a major role in the activities surrounding the development of DSM-5 (Kupfer et al., 2002, Regier, 2011). Setting aside the broader question regarding the usefulness of a multiaxial system of classification (Gruenberg and Goldstein, 2003, Williams, 1985a, b), we would articulate the following research agenda for strengthening Axis IV. First, research is needed to enhance our understanding of the psychosocial and environmental problems that are most important for the prognosis of psychiatric disorders. This work should incorporate detailed assessments of stressors that cover the entire lifespan, that include information on the psychological impact of stressors, and that overcome the limitations of stressful event checklists (Dohrenwend, 2006). Second, research is needed to develop standardized measures of psychosocial and environmental problems that could be administered in clinical settings. These will by necessity be shorter and less extensive than research assessments, but should cover all of the relevant domains of stressors found to predict the prognosis of disorders, and be subjected to reliability testing. Third, research is needed to determine whether information on psychosocial and environmental problems can be used to enhance psychiatric treatment and thereby improve prognosis. For example, this could include incorporating into treatment plans steps to overcome barriers to treatment effectiveness that exist in the context of social and environmental stressors (Cohen et al., 2006). The third step in this research agenda is most critical for establishing the clinical utility of Axis IV.
Acknowledgments
Grant support: This research was supported in part by grants MH085050 and MH087544 from the National Institutes of Health.
The authors sincerely appreciate the contributions of Ms. Kathleen McGaffigan for data management and statistical programming, and Ms. Rebecca Hawrusik for research assistance.
Footnotes
DECLARATION OF INTEREST
Disclosures: Dr. Fava has received research support from Abbott Laboratories; Alkermes, Inc.; Aspect Medical Systems; AstraZeneca; BioResearch; BrainCells Inc.; Bristol-Myers Squibb; Cephalon, Inc.; CeNeRx BioPharma; Clinical Trials Solutions, LLC; Clintara, LLC; Covidien; Eli Lilly and Company; EnVivo Pharmaceuticals, Inc.; Euthymics Bioscience, Inc.; Forest Pharmaceuticals, Inc.; Ganeden Biotech, Inc.; GlaxoSmithKline; Icon Clinical Research; i3 Innovus/Ingenix; Johnson & Johnson Pharmaceutical Research & Development; Lichtwer Pharma GmbH; Lorex Pharmaceuticals; National Alliance for Research on Schizophrenia & Depression (NARSAD); National Center for Complementary and Alternative Medicine (NCCAM); National Institute of Drug Abuse (NIDA); National Institute of Mental Health (NIMH); Novartis AG; Organon Pharmaceuticals; PamLab, LLC.; Pfizer Inc.; Pharmavite® LLC; Photothera; Roche; RCT Logic, LLC; Sanofi-Aventis US LLC; Shire; Solvay Pharmaceuticals, Inc.; Synthelabo; Wyeth-Ayerst Laboratories. He has served as advisor or consultant to Abbott Laboratories; Affectis Pharmaceuticals AG; Alkermes, Inc.; Amarin Pharma Inc.; Aspect Medical Systems; AstraZeneca; Auspex Pharmaceuticals; Bayer AG; Best Practice Project Management, Inc.; BioMarin Pharmaceuticals, Inc.; Biovail Corporation; BrainCells Inc; Bristol-Myers Squibb; CeNeRx BioPharma; Cephalon, Inc.; Clinical Trials Solutions, LLC; CNS Response, Inc.; Compellis Pharmaceuticals; Cypress Pharmaceutical, Inc.; DiagnoSearch Life Sciences (P) Ltd.; Dinippon Sumitomo Pharma Co. Inc.; Dov Pharmaceuticals, Inc.; Edgemont Pharmaceuticals, Inc.; Eisai Inc.; Eli Lilly and Company; ePharmaSolutions; EPIX Pharmaceuticals, Inc.; Euthymics Bioscience, Inc.; Fabre-Kramer Pharmaceuticals, Inc.; Forest Pharmaceuticals, Inc.; GenOmind, LLC; GlaxoSmithKline; Grunenthal GmbH; i3 Innovus/Ingenis; Janssen Pharmaceutica; Jazz Pharmaceuticals, Inc.; Johnson & Johnson Pharmaceutical Research & Development, LLC; Knoll Pharmaceuticals Corp.; Labopharm Inc.; Lorex Pharmaceuticals; Lundbeck Inc.; MedAvante, Inc.; Merck & Co., Inc.; MSI Methylation Sciences, Inc.; Naurex, Inc.; Neuronetics, Inc.; NextWave Pharmaceuticals; Novartis AG; Nutrition 21; Orexigen Therapeutics, Inc.; Organon Pharmaceuticals; Otsuka Pharmaceuticals; PamLab, LLC.; Pfizer Inc.; PharmaStar; Pharmavite® LLC.; PharmoRx Therapeutics; Precision Human Biolaboratory; Prexa Pharmaceuticals, Inc.; Puretech Ventures; PsychoGenics; Psylin Neurosciences, Inc.; Rexahn Pharmaceuticals, Inc.; Ridge Diagnostics, Inc.; Roche; RCT Logic, LLC; Sanofi-Aventis US LLC.; Sepracor Inc.; Servier Laboratories; Schering-Plough Corporation; Solvay Pharmaceuticals, Inc.; Somaxon Pharmaceuticals, Inc.; Somerset Pharmaceuticals, Inc.; Sunovion Pharmaceuticals; Supernus Pharmaceuticals, Inc.; Synthelabo; Takeda Pharmaceutical Company Limited; Tal Medical, Inc.; Tetragenex Pharmaceuticals, Inc.; TransForm Pharmaceuticals, Inc.; Transcept Pharmaceuticals, Inc.; Vanda Pharmaceuticals, Inc. He has received speaking or publishing fees from Adamed, Co; Advanced Meeting Partners; American Psychiatric Association; American Society of Clinical Psychopharmacology; AstraZeneca; Belvoir Media Group; Boehringer Ingelheim GmbH; Bristol-Myers Squibb; Cephalon, Inc.; CME Institute/Physicians Postgraduate Press, Inc.; Eli Lilly and Company; Forest Pharmaceuticals, Inc.; GlaxoSmithKline; Imedex, LLC; MGH Psychiatry Academy/Primedia; MGH Psychiatry Academy/Reed Elsevier; Novartis AG; Organon Pharmaceuticals; Pfizer Inc.; PharmaStar; United BioSource,Corp.; Wyeth-Ayerst Laboratories. He owns stock in Compellis. He has a received royalty, patent, or other income from Patent for Sequential Parallel Comparison Design (SPCD) and patent application for a combination of azapirones and bupropion in Major Depressive Disorder (MDD), copyright royalties for the MGH Cognitive & Physical Functioning Questionnaire (CPFQ), Sexual Functioning Inventory (SFI), Antidepressant Treatment Response Questionnaire (ATRQ), Discontinuation-Emergent Signs & Symptoms (DESS), and SAFER. Patent for research and licensing of SPCD with RCT Logic; Lippincott, Williams & Wilkins; World Scientific Publishing Co. Pte.Ltd. The other authors report no financial relationships with commercial interests.
References
- American Psychiatric Association. [Accessed January 6, 2011];Classification issues under discussion. ( http://www.dsm5.org/ProposedRevisions/Pages/ClassificationIssuesUnderDiscussion.aspx)
- Benjet C, Borges G, Medina-Mora ME. Chronic childhood adversity and onset of psychopathology during three life stages: Childhood, adolescence and adulthood. J Psychiatr Res. 2010;44:732–740. doi: 10.1016/j.jpsychires.2010.01.004. [DOI] [PubMed] [Google Scholar]
- Brown GW, Harris TO, Kendrick T, Chatwin J, Craig TK, Kelly V, Mander H, Ring A, Wallace V, Uher R. Antidepressants, social adversity and outcome of depression in general practice. J Affect Disord. 2010;121:239–46. doi: 10.1016/j.jad.2009.06.004. [DOI] [PubMed] [Google Scholar]
- Clark C, Caldwell T, Power C, Stansfeld SA. Does the influence of childhood adversity on psychopathology persist across the lifecourse? A 45-year prospective epidemiologic study. Ann Epidemiol. 2010;20:385–94. doi: 10.1016/j.annepidem.2010.02.008. [DOI] [PubMed] [Google Scholar]
- Cohen A, Gilman SE, Houck PR, Szanto K, Reynolds CF., 3rd Socioeconomic status and anxiety as predictors of antidepressant treatment response and suicidal ideation in older adults. Social Psychiatry and Psychiatric Epidemiology. 2009;44:272–7. doi: 10.1007/s00127-008-0436-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen A, Houck PR, Szanto K, Dew MA, Gilman SE, Reynolds CF., 3rd Social inequalities in response to antidepressant treatment in older adults. Arch Gen Psychiatry. 2006;63:50–6. doi: 10.1001/archpsyc.63.1.50. [DOI] [PubMed] [Google Scholar]
- D’Agostino RB, Sr, Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA : the journal of the American Medical Association. 2001;286:180–7. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Grant BF. Rates and correlates of relapse among individuals in remission from DSM-IV alcohol dependence: a 3-year follow-up. Alcoholism, Clinical and Experimental Research. 2007;31:2036–45. doi: 10.1111/j.1530-0277.2007.00536.x. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP. Inventorying stressful life events as risk factors for psychopathology: Toward resolution of the problem of intracategory variability. Psychol Bull. 2006;132:477–95. doi: 10.1037/0033-2909.132.3.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton WW, Shao H, Nestadt G, Lee HB, Bienvenu OJ, Zandi P. Population-based study of first onset and chronicity in major depressive disorder. Archives of General Psychiatry. 2008;65:513–20. doi: 10.1001/archpsyc.65.5.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezquiaga E, Garcia A, Pallares T, Bravo MF. Psychosocial predictors of outcome in major depression: a prospective 12-month study. Journal of Affective Disorders. 1999;52:209–16. doi: 10.1016/s0165-0327(98)00057-3. [DOI] [PubMed] [Google Scholar]
- Furukawa TA, Fujita A, Harai H, Yoshimura R, Kitamura T, Takahashi K. Definitions of recovery and outcomes of major depression: results from a 10-year follow-up. Acta Psychiatr Scand. 2008;117:35–40. doi: 10.1111/j.1600-0447.2007.01119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson D. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV) National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 2001. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Gruenberg AM, Goldstein RD. Multiaxial assessment in the twenty-first century. In: Phillips KA, First MB, Pincus HA, editors. Advancing DSM: dilemmas in psychiatric diagnosis. American Psychiatric Association; Washington, D.C: 2003. pp. 145–152. [Google Scholar]
- Hammen C, Kim EY, Eberhart NK, Brennan PA. Chronic and acute stress and the prediction of major depression in women. Depress Anxiety. 2009;26:718–23. doi: 10.1002/da.20571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62:1097–106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Kuhn JW, Prescott CA, Kendler KS. The impact of generalized anxiety disorder and stressful life events on risk for major depressive episodes. Psychol Med. 2006;36:789–95. doi: 10.1017/S0033291706007367. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Hettema JM, Butera F, Gardner CO, Prescott CA. Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Arch Gen Psychiatry. 2003;60:789–96. doi: 10.1001/archpsyc.60.8.789. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry. 1999;156:837–41. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, First MB, Regier DA. A research agenda for DSM-V. American Psychiatric Association; Washington, D.C: 2002. [Google Scholar]
- Lenze SN, Cyranowski JM, Thompson WK, Anderson B, Frank E. The cumulative impact of nonsevere life events predicts depression recurrence during maintenance treatment with interpersonal psychotherapy. Journal of Consulting and Clinical Psychology. 2008;76:979–87. doi: 10.1037/a0012862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCutcheon AL. Latent class analysis. Sage Publications; Newbury Park: 1987. [Google Scholar]
- McLaughlin KA, Conron KJ, Koenen KC, Gilman SE. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychological Medicine. 2010;40:1647–58. doi: 10.1017/S0033291709992121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moncur RA, Luthra AS. Axis IV of the DSM: origins, evolution, and utility. McMaster University Medical Journal. 2009;6:11–15. [Google Scholar]
- Monroe SM, Torres LD, Guillaumot J, Harkness KL, Roberts JE, Frank E, Kupfer D. Life stress and the long-term treatment course of recurrent depression: III. Nonsevere life events predict recurrence for medicated patients over 3 years. Journal of Consulting and Clinical Psychology. 2006;74:112–20. doi: 10.1037/0022-006X.74.1.112. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide. Muthen & Muthen; Los Angeles: 1998–2010. [Google Scholar]
- Plapp JM, Rey JM, Stewart GM, Bashir MR, Richards IN. Ratings of psychosocial stressors in adolescence using DSM-III Axis IV criteria. Journal of the American Academy of Child and Adolescent Psychiatry. 1987;26:80–6. doi: 10.1097/00004583-198701000-00016. [DOI] [PubMed] [Google Scholar]
- Post RM, Rubinow DR, Ballenger JC. Conditioning and sensitisation in the longitudinal course of affective illness. British Journal of Psychiatry. 1986;149:191–201. doi: 10.1192/bjp.149.2.191. [DOI] [PubMed] [Google Scholar]
- Regier DA. The conceptual evolution of DSM-5. American Psychiatric Pub; Washington, DC: 2011. [Google Scholar]
- Research Triangle Institute. SUDAAN Language Manual, Release 9.0. Research Triangle Institute; Research Triangle Park, NC: 2004. [Google Scholar]
- Rey JM, Plapp JM, Stewart GW, Richards I, Bashir M. Reliability of DSM-III Axis IV. Archives of General Psychiatry. 1987a;44:96–7. doi: 10.1001/archpsyc.1987.01800130108019. [DOI] [PubMed] [Google Scholar]
- Rey JM, Stewart GW, Plapp JM, Bashir MR, Richards IN. Sources of unreliability of DSM-III Axis IV. Australian and New Zealand Journal of Psychiatry. 1987b;21:75–80. doi: 10.3109/00048678709160902. [DOI] [PubMed] [Google Scholar]
- Rey JM, Stewart GW, Plapp JM, Bashir MR, Richards IN. DSM-III axis IV revisited. American Journal of Psychiatry. 1988;145:286–92. doi: 10.1176/ajp.145.3.286. [DOI] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Lebovici S, Eisenberg L, Sneznevskij AV, Sadoun R, Brooke E, Lin TY. A tri-axial classification of mental disorders in childhood. An international study. Journal of child psychology and psychiatry, and allied disciplines. 1969;10:41–61. doi: 10.1111/j.1469-7610.1969.tb02067.x. [DOI] [PubMed] [Google Scholar]
- Safford SM, Alloy LB, Abramson LY, Crossfield AG. Negative cognitive style as a predictor of negative life events in depression-prone individuals: a test of the stress generation hypothesis. J Affect Disord. 2007;99:147–54. doi: 10.1016/j.jad.2006.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salum GA, Polanczyk GV, Miguel EC, Rohde LA. Effects of childhood development on late-life mental disorders. Curr Opin Psychiatry. 2010;23:498–503. doi: 10.1097/YCO.0b013e32833ead33. [DOI] [PubMed] [Google Scholar]
- Schrader G, Gordon M, Harcourt R. The usefulness of DSM-III axis IV and axis V assessments. American Journal of Psychiatry. 1986;143:904–7. doi: 10.1176/ajp.143.7.904. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Link BG, Dohrenwend BP, Skodol AE, Stueve A, Mirotznik J. Characterizing life events as risk factors for depression: the role of fateful loss events. Journal of Abnormal Psychology. 1989;98:460–7. doi: 10.1037//0021-843x.98.4.460. [DOI] [PubMed] [Google Scholar]
- Skodol AE. DSM-IV sourcebook. 1997. Axis IV; pp. 409–422. [Google Scholar]
- Skodol AE, Shrout PE. Axis IV of DSM-III. American Journal of Psychiatry. 1988;145:1046–7. doi: 10.1176/ajp.145.8.aj14581046. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Shrout PE. Use of DSM-III axis IV in clinical practice: rating etiologically significant stressors. American Journal of Psychiatry. 1989a;146:61–6. doi: 10.1176/ajp.146.1.61. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Shrout PE. Use of DSM-III Axis IV in clinical practice: rating the severity of psychosocial stressors. Psychiatry Research. 1989b;30:201–11. doi: 10.1016/0165-1781(89)90161-3. [DOI] [PubMed] [Google Scholar]
- Slopen N, Fitzmaurice G, Williams DR, Gilman SE. Poverty, food insecurity, and the behavior for childhood internalizing and externalizing disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:444–52. doi: 10.1097/00004583-201005000-00005. [DOI] [PubMed] [Google Scholar]
- Spijker J, de Graaf R, Bijl RV, Beekman AT, Ormel J, Nolen WA. Duration of major depressive episodes in the general population: results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS) British Journal of Psychiatry. 2002;181:208–13. doi: 10.1192/bjp.181.3.208. [DOI] [PubMed] [Google Scholar]
- Strauss JS. A comprehensive approach to psychiatric diagnosis. The American journal of psychiatry. 1975;132:1193–7. doi: 10.1176/ajp.132.11.1193. [DOI] [PubMed] [Google Scholar]
- Williams JB. The multiaxial system of DSM-III: where did it come from and where should it go? I. Its origins and critiques. Archives of General Psychiatry. 1985a;42:175–80. doi: 10.1001/archpsyc.1985.01790250069009. [DOI] [PubMed] [Google Scholar]
- Williams JB. The multiaxial system of DSM-III: where did it come from and where should it go? II. Empirical studies, innovations, and recommendations. Archives of General Psychiatry. 1985b;42:181–6. doi: 10.1001/archpsyc.1985.01790250075010. [DOI] [PubMed] [Google Scholar]
- Wilson PW. Risk scores for prediction of coronary heart disease: an update. Endocrinology and Metabolism Clinics of North America. 2009;38:33–44. doi: 10.1016/j.ecl.2008.11.001. [DOI] [PubMed] [Google Scholar]
- World Health Organization. [Accessed January 25, 2011];Persons with potential health hazards related to socionomic and psychosocial circumstances (Z55–Z65) ( http://apps.who.int/classifications/apps/icd/icd10online/gz55.htm)
- Zimmerman M, Pfohl B, Coryell W, Stangl D. The prognostic validity of DSM-III axis IV in depressed inpatients. American Journal of Psychiatry. 1987;144:102–6. doi: 10.1176/ajp.144.1.102. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Pfohl B, Stangl D, Coryell W. The validity of DSM-III axis IV (severity of psychosocial stressors) American Journal of Psychiatry. 1985;142:1437–41. doi: 10.1176/ajp.142.12.1437. [DOI] [PubMed] [Google Scholar]
- Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]