Abstract
Objective
Bereavement-related depression is excluded from a diagnosis of major depressive episode (MDE) in DSM-IV unless the syndrome is prolonged or complicated. The objective of this study is to assess the validity of the bereavement exclusion by comparing characteristics of bereavement-related episodes that are excluded from a diagnosis, and bereavement-related episodes that qualify for a diagnosis (complicated bereavement), to MDE.
Methods
We used data from two waves of the National Epidemiologic Survey on Alcohol and Related Conditions to compare bereavement-excluded depression and complicated bereavement to MDE with respect to indicators of pre-existing risk for psychopathology (antecedent indicators) and indicators of disorder severity (consequent indicators).
Results
Compared to individuals with MDE, individuals with bereavement-excluded depression had lower risks of pre-existing psychiatric disorders (e.g., 0.44 lower odds of social phobia, P=0.006), fewer depressive episodes (recurrence rate 0.37 times lower, P<0.001), less impairment, an 0.18 times lower odds of seeking treatment (P<0.001), and a lower risk of psychiatric disorders during a 3-year follow-up period. Unexpectedly, this same pattern of differences was observed between individuals with complicated bereavement and MDE.
Conclusion
Despite the presence of a clinically significant depressive episode, bereavement-excluded depression is in many ways less indicative of psychopathology than MDE. However, complicated bereavement was more similar to bereavement-excluded depression than to MDE. We therefore question whether the DSM-IV criteria validly distinguish between non-disordered loss reactions (bereavement-excluded depression), pathological loss reactions (complicated bereavement), and non-loss related MDE.
Keywords: Depression, bereavement, validity
INTRODUCTION
DSM-IV excludes individuals experiencing “an expectable and culturally sanctioned response to a particular event, for example, the death of a loved one” (DSM-IV-TR, p.xxxi) from receiving a psychiatric diagnosis. This rule is incorporated into the diagnostic criteria for major depressive episode (MDE) by excluding syndromes of short duration that occur in the context of bereavement.1–3 DSM-IV also recognizes that some depressive episodes following a loss are sufficiently extreme that they are pathological, and therefore provides for an exception to this exclusion.
There is emerging evidence that depression following bereavement does not differ from depression that is unrelated to bereavement (or other types of stressors).4–7 There is also evidence that bereavement-related depression improves following antidepressant and psychotherapeutic treatments,8–11 suggesting a clinical benefit to assigning a diagnosis of MDE even if it occurs in the context of bereavement. It is therefore important to clarify the ambiguous status of bereavement vis-à-vis the diagnosis of depression.
Accordingly, this study investigates the diagnostic exclusion for bereavement-related depression, as well as the exception to this exclusion. We compare individuals with depression who are excluded from a diagnosis of MDE because of bereavement (“bereavement-excluded depression”) to individuals who qualify for a diagnosis of MDE despite their depression occurring in the context of bereavement (“complicated bereavement”), and to individuals with MDE that is unrelated to bereavement. We use as comparators 2 types of indicators of psychopathology: 1) antecedent indicators12 of pre-existing vulnerability to psychopathology (e.g., family history, prior psychiatric disorders); and 2) consequent indicators of clinical course (e.g., recurrence risk).13 The expectation, based on the DSM-IV criteria, is that individuals with bereavement-excluded depression would score lower on each of the antecedent and consequent indicators because their depression would be more indicative of non-disordered sadness than of major depressive episode. In contrast, individuals with complicated bereavement are expected to score similarly on the disorder indicators as those with MDE.
METHODS
Study sample
Data come from the National Epidemiology Survey on Alcohol and Related Conditions (NESARC), a two-wave, nationally representative household survey conducted by the National Institute on Alcohol Abuse and Alcoholism.14,15 The Wave 1 sample included 43,093 adult participants. The Wave 2 survey, conducted approximately 3 years later, included 39,959 of the Wave 1 participants. The combined response rate for both waves was 70.2%.16
Measures
Lifetime MDE was assessed using the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS).17 The AUDADIS is a fully structured diagnostic interview administered by trained non-clinician interviewers.18–20 The AUDADIS algorithm for MDE requires ≥5 clinically significant symptoms of depression occurring during a 2-week period of sadness or anhedonia.21 If participants reported symptoms of a major depressive episode that began to happen just after someone close to them died, a diagnosis of MDE is excluded; we classified these participants in the “bereavement-excluded depression” group (unless they had the “complicated” features described below).
Depression occurring in association with the loss of a loved one qualifies for a DSM-IV diagnosis if it persisted for 2 months or more or exhibited marked functional impairment, morbid preoccupation with worthlessness, suicidal ideation, psychomotor retardation, or psychotic symptoms, which we term “complicated bereavement.” This is not “complicated grief” or “prolonged grief,” which is a separate condition that is phenomenologically distinct from depression.22–24
Except for the duration requirement, there is no guidance in DSM-IV for operationalizing the criteria for “complicated bereavement.” For example, it is unclear how “marked functional impairment” differs from the generic requirement of “clinically significant distress or impairment in social or occupational functioning.”25,26 We defined complicated bereavement as a depressive episode following the loss of a loved one that either persisted for at least 2 months, or that was accompanied by one of the following symptoms: marked functional impairment, suicidal ideation, or psychomotor retardation. We considered marked functional impairment to be present if respondents endorsed all three of the NESARC’s impairment items that reference functional impairment (“arguments or friction with friends, family, people at work;” “trouble doing things you were supposed to do;” and “couldn’t do the things you usually did or wanted to do”). Suicidal ideation was based on endorsement of suicide attempt, thoughts of suicide, desire to die, or frequent thoughts of one’s own death. Psychomotor retardation was based on the item, “move or talk MUCH more slowly than usual, most days for at least 2 weeks.” We did not operationalize two of the criteria for complicated bereavement: psychotic symptoms, which were not assessed in the NESARC; and morbid preoccupation with worthlessness, which we interpret to imply a higher degree of severity than the general MDE criterion of “feelings of worthlessness.” The NESARC assessed symptoms of depression that were present during participants’ worst period of depression. Accordingly, the diagnoses that were compared in the current study refer to participants’ worst or (for single-episode cases) only lifetime episode.
Antecedent indicators of psychopathology
A high family history loading of depression and alcoholism was defined as being in the top decile of a measure indexing the proportion of first and second-degree relatives with each disorder, weighted by their degree of genetic relatedness to the respondent.19,27 History of panic disorder, generalized anxiety disorder, social phobia, and alcohol dependence prior to the first onset of depression was determined by comparing the lifetime histories and ages at onset for each of these disorders to the age at first depression onset. DSM-IV personality disorders were assessed on a lifetime basis as described previously.28
Consequent indicators of psychopathology
The number of lifetime depressive episodes was assessed by a single item asking about the number of episodes lasting at least 2 weeks that were separated by a 2-month period of improvement in mood. Psychosocial impairment was defined as the number of difficulties that respondents associated with their depression, not counting those items that were used in the definition of “marked functional impairment” described above. Treatment seeking was based on participants’ reports of seeking professional help to improve one’s mood, being hospitalized, seeking emergency room care, or being prescribed medications for mood. Finally, we investigated the risk of MDE, panic disorder, generalized anxiety disorder, social phobia, and alcohol dependence in interval between the Wave 1 and Wave 2 interviews.
Statistical analysis
The analyses of antecedent indicators involved comparisons of individuals with complicated bereavement and with bereavement-excluded depression to individuals with MDE. Comparisons were made using multinomial logistic regression models in which the dependent variable was the type of diagnosis, and antecedent indicators were entered as predictors.
In contrast, regression models for consequent indicators treat the consequent indicators as dependent variables, and the diagnosis as predictor. Analyses of consequent indicators were conducted by fitting regression models for the number of lifetime depressive episodes (using Poisson regression), mean impairment scores (using linear regression), the likelihood of treatment seeking (using logistic regression), and the risk of psychiatric disorders at Wave 2 (logistic regression). Poisson regression coefficients, when exponentiated, indicate differences in the recurrence rate of depressive episodes between individuals with MDE and those with either complicated bereavement or bereavement-excluded depression. Linear regression coefficients indicate mean differences in psychosocial impairment scores across groups. Finally, odds ratios obtained from the logistic regression models indicate differences in the odds of treatment seeking and odds of Wave 2 disorders across groups.
The analysis sample comprised participants with a lifetime history of depressive symptoms that are required for a DSM-IV diagnosis of MDE. We made comparisons in this sample between individuals with MDE, complicated bereavement, and bereavement-excluded depression. However, we included all NESARC participants in the analyses of Wave 2 disorders, wherein we added a fourth comparison group: individuals with no lifetime history of depression.
We conducted the analyses in SUDAAN,29 which adjusts variances and point estimates for the multi-stage sampling design and differential selection probabilities used to ascertain the NESARC sample. Missing data on Wave 1 covariates (approximately 1% of the sample), and on psychiatric disorders among Wave 2 non-participants (approximately 20% of the sample), were imputed using the method of multiple imputation as implemented in IVEware,30 with adjustments made for the complex sampling design of the NESARC.31
RESULTS
Prevalence of MDE, complicated bereavement, and bereavement-excluded depression
The lifetime prevalence of MDE was 20.0% (95% confidence interval (CI), 19.2–20.8; n=8,626). The majority of cases were unrelated to bereavement (91.5%, n=7,864) and thus classified as MDE; 6.2% of cases (n=566) were bereavement-related but qualified for a diagnosis of MDE because of being “complicated bereavement;” and 2.3% of cases (n=196) were excluded from a diagnosis because of bereavement. Prevalences of MDE, complicated bereavement, and bereavement-excluded depression are shown according to participant demographic in Table 1.
Table 1.
Demographic characteristics of the National Epidemiologic Survey on Alcohol and Related Conditions sample (n=43,093), and characteristics of participants with lifetime major depressive episode, complicated bereavement, and bereavement-excluded depression.
| Sample distribution % (n) | Major depressive episode % (n) | Complicated bereavement % (n) | Bereavement- excluded depression % (n) | |
|---|---|---|---|---|
| Total | 100 (43,093) | 18.3 (7,864) | 1.2 (566) | 0.5 (196) |
| Sex | ||||
| Male | 47.9 (18,518) | 13.2 (2,437) | 0.9 (179) | 0.3 (57) |
| Female | 52.1 (24,575) | 23.0 (5,426) | 1.5 (387) | 0.6 (139) |
| Race/ethnicity | ||||
| White | 70.9 (24,507) | 20.0 (5,072) | 1.2 (304) | 0.5 (128) |
| Black | 11.1 (8,245) | 13.5 (1,152) | 1.6 (137) | 0.6 (39) |
| Other | 18.0 (10,341) | 14.5 (1,640) | 1.2 (126) | 0.3 (30) |
| Age | ||||
| 18–29 | 21.8 (8,666) | 18.5 (1,636) | 1.2 (116) | 0.4 (40) |
| 30–44 | 30.9 (13,382) | 19.4 (2,620) | 1.5 (189) | 0.5 (57) |
| 45–64 | 31.1 (12,840) | 21.1 (2,727) | 1.2 (172) | 0.5 (58) |
| ≥65 | 16.2 (8,205) | 10.5 (881) | 0.9 (89) | 0.6 (43) |
| Marital status | ||||
| Married | 61.6 (22,081) | 16.4 (3,452) | 1.2 (259) | 0.4 (93) |
| Separated, widowed, or divorced | 17.5 (11,117) | 25.0 (2,554) | 1.6 (178) | 0.6 (57) |
| Never marred | 20.9 (9,895) | 18.2 (1,857) | 1.2 (129) | 0.5 (46) |
| Education | ||||
| Less than high school | 15.7 (7,849) | 17.1 (1,269) | 1.4 (122) | 0.2 (26) |
| High school or GED | 29.3 (12,547) | 17.4 (2,184) | 1.4 (189) | 0.4 (50) |
| Some college or higher | 55.0 (22,697) | 19.1 (4,411) | 1.1 (255) | 0.6 (121) |
Differences in antecedent indicators of psychopathology between MDE, complicated bereavement, and bereavement-excluded depression
Results of multinomial logistic regression models predicting either MDE (reference category), complicated bereavement, or bereavement-excluded depression are presented in Table 2. Virtually all of the odds ratios were less than 1, indicating that the antecedent indicators of psychopathology are less likely to precede complicated bereavement and bereavement-excluded depression than they are to precede MDE. For example, a high family history loading of depression (first row of Table 2) was associated with a 0.85 lower odds of complicated bereavement (CI: 0.65, 1.13), and a 0.81 lower odds of bereavement-excluded depression (CI: 0.54, 1.21), relative to MDE. Statistically significant associations in Table 2 were observed for a diagnosis of social phobia prior to depression onset, and for lifetime diagnoses of avoidant, obsessive-compulsive, paranoid, and schizoid personality disorders.
Table 2.
Associations between antecedent indictors of psychopathology and Major Depressive Episode (MDE), complicated bereavement, and bereavement-excluded depression in the National Epidemiologic Survey on Alcohol and Related Conditions (n=8,626).a
| Complicated bereavement (vs. MDE) | Bereavement- excluded depression (vs. MDE) | χ2 (df=2), P | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | ||
| High family history loading of psychiatric disorders | |||
| Depression | 0.85 (0.65, 1.13) | 0.81 (0.54, 1.21) | 2.7, 0.265 |
| Alcoholism | 0.83 (0.62, 1.11) | 0.58 (0.32, 1.07) | 4.3, 0.117 |
| Disorders prior to depression onset | |||
| Panic | 0.83 (0.47, 1.49) | 1.43 (0.50, 4.05) | 0.9, 0.627 |
| Generalized Anxiety Disorder | 0.72 (0.33, 1.57) | 0.48 (0.19, 1.21) | 2.9, 0.230 |
| Social Phobia | 0.53 (0.34, 0.84) | 0.44 (0.20, 0.97) | 10.1, 0.006 |
| Alcohol dependence | 1.08 (0.76, 1.53) | 1.07 (0.55, 2.06) | 0.3, 0.883 |
| Personality disorders | |||
| Avoidant | 0.48 (0.28, 0.82) | 0.24 (0.08, 0.70) | 13.4, 0.001 |
| Obsessive-Compulsive | 0.62 (0.46, 0.84) | 0.54 (0.33, 0.88) | 15.8, <0.001 |
| Paranoid | 0.59 (0.42, 0.82) | 0.53 (0.25, 1.13) | 12.3, 0.002 |
| Schizoid | 0.55 (0.36, 0.83) | 0.20 (0.07, 0.54) | 18.6, <0.001 |
| Histrionic | 0.57 (0.33, 1.00) | 0.76 (0.26, 2.18) | 4.2, 0.123 |
| Antisocial | 0.90 (0.59, 1.39) | 0.50 (0.14, 1.81) | 1.3, 0.525 |
Results from multinomial logistic regression analyses of depression category, with MDE as the reference, adjusting for age, sex, marital status, race/ethnicity, and educational attainment. Odds ratios (OR) indicate the likelihood of either complicated bereavement or bereavement-excluded depression, relative to MDE, associated with each antecedent indicator. Each row presents the results from a separate model.
Differences in consequent indicators of psychopathology between MDE, complicated bereavement, and bereavement-excluded depression
Relative to individuals with MDE, those with complicated bereavement (Rate Ratio: 0.52; CI: 0.38, 0.70) and bereavement-excluded depression (RR: 0.37; CI: 0.30, 0.46) reported fewer depressive episodes over their lifetimes (Table 3). Complicated bereavement and bereavement-related depression were also associated with significantly less psychosocial impairment, and a lower likelihood of seeking treatment, than MDE. Further, individuals with complicated bereavement and bereavement-related depression had a 0.32 (CI: 0.25, 0.42) and 0.23 (0.14, 0.39) lower odds of being prescribed medication for their depression, respectively, than individuals with MDE.
Table 3.
Associations between consequent indicators of psychopathology and Major Depressive Episode, complicated bereavement, and bereavement-excluded depression in the National Epidemiologic Survey on Alcohol and Related Conditions (n=8,626).a
| Complicated bereavement (vs. MDE) | Bereavement-excluded depression (vs. MDE) | ||
|---|---|---|---|
| RR (95% CI) | RR (95% CI) | χ2 (df=2), P | |
| Number of lifetime depressive episodesb | 0.52 (0.38, 0.70) | 0.37 (0.30, 0.46) | 103.9, <0.001 |
| Mean difference (CI) | Mean difference (CI) | F (df), P | |
| Psychosocial impairmentc | −0.29 (−0.43, −0.15) | −0.77 (−0.98, −0.57) | 36.9, <0.001 |
| Treatment seeking for depressiond | OR (95% CI) | OR (95% CI) | χ2 (df), P |
| Any treatment | 0.32 (0.26, 0.41) | 0.18 (0.12, 0.30) | 144.5, <0.001 |
| Sought treatment from mental health professional | 0.29 (0.23, 0.38) | 0.15 (0.09, 0.24) | 136.2, <0.001 |
| Hospitalized for depression | 0.58 (0.36, 0.95) | 0.09 (0.02, 0.42) | 13.8, 0.001 |
| Visited emergency room for depression | 0.56 (0.35, 0.90) | 0.10 (0.02, 0.58) | 13.2, 0.001 |
| Prescribed medication for depression | 0.32 (0.25, 0.42) | 0.23 (0.14, 0.39) | 103.0, <0.001 |
Models predicting consequent indicators adjusting for age, sex, marital status, race/ethnicity, and educational attainment.
Poisson regression model of the number of lifetime depressive episodes. Rate ratios (RR) indicate the ratio of number of depressive episodes between individuals with complicated bereavement or bereavement-excluded depression, and individuals with MDE.
Linear regression model of psychosocial impairment scores across groups. Regression coefficients indicate mean differences in psychosocial impairment scores between individuals with complicated bereavement or bereavement-excluded depression, and individuals with MDE.
Logistic regression models of indicators of treatment seeking. Odds ratios (OR) indicate the difference in the odds of seeking treatment for depression between individuals with complicated bereavement or bereavement-excluded depression, and individuals with MDE.
Risks for Wave 2 Psychiatric Disorders
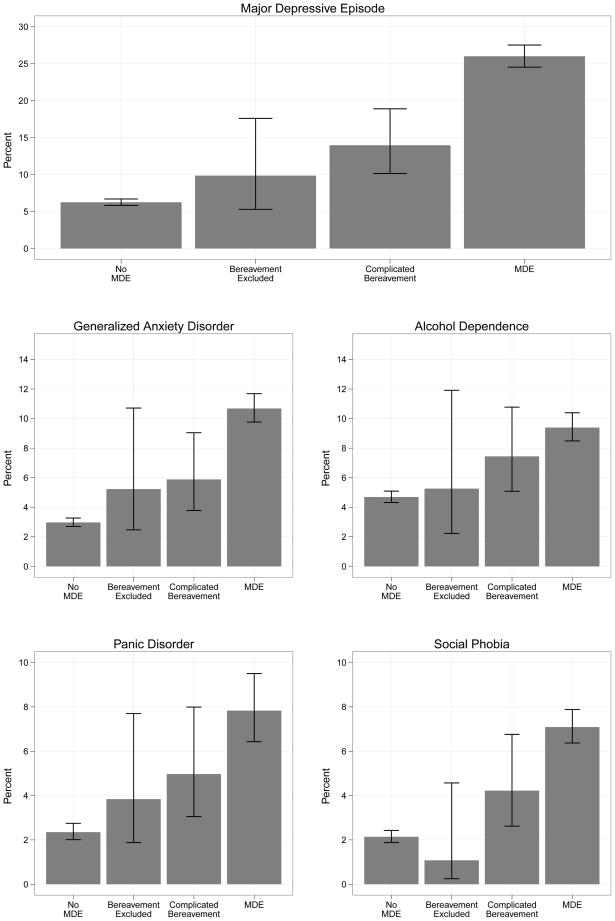
The prevalences of depression, panic disorder, social phobia, and generalized anxiety disorder during the 3-year interval between the Wave 1 and Wave 2 interviews are shown in Figure 1, with the vertical bars representing disorder status at Wave 1. The general pattern that emerges is an increasing risk of disorders, ranging from lowest to highest, among individuals with no lifetime depression at Wave 1, bereavement-related depression, complicated bereavement, and MDE.
Figure 1. Prevalence of psychiatric disorders during the 3-year follow-up period among participants in the National Epidemiologic Survey on Alcohol and Related Conditions (n=43,093) according to diagnosis category at the baseline assessment.a.
aBaseline diagnosis categories on the X-axis are: No Major Depressive Episode (No MDE), Bereavement Excluded depression, Complicated Bereavement, and MDE. The Y-axis indicates the percent of individuals with each disorder during the NESARC follow-up period, assessed at the Wave 2 interview.
Logistic regression analyses were then conducted for each disorder (Table 4). As would be expected, individuals without a lifetime history of depression at Wave 1 had a substantially lower risk of future disorders compared to individuals with MDE (column 1, OR’s ranging from 0.21–0.46). Similarly, bereavement-excluded depression was also associated with a lower risk of subsequent depression (OR: 0.33; CI: 0.16 0.65) and other disorders (OR’s for bereavement-excluded depression were statistically significant for depression and social phobia). However, contrary to what would be predicted by the DSM-IV diagnostic criteria, individuals with complicated bereavement (column 2) also had lower risks for subsequent disorders than individuals with MDE (OR’s were statistically significant for 3 out of 5 disorders: depression, social phobia, and generalized anxiety disorder). None of the tests comparing the odds ratios for bereavement-excluded depression to the odds ratios for no lifetime depression (fourth column) and for complicated bereavement (fifth column) were statistically significant. Thus, while MDE at Wave 1 was associated with an increased risk for psychiatric disorders over a 3-year follow-up interval, this was not true for bereavement-excluded depression at Wave 1 nor complicated bereavement at Wave 1.
Table 4.
Odds ratiosa for psychiatric disorders during the 3-year follow-up period among participants in the National Epidemiologic Survey on Alcohol and Related Conditions (n=43,093) according to diagnosis category at the baseline assessment.
| Diagnosis category at Baseline
|
Significance tests (test statistics and P- values) for the contrast between Bereavement- excluded depression and no MDE (column 3 vs. column 1) | Significance tests (test statistics and P- values) for the contrast between Bereavement- excluded depression and complicated bereavement (column 3 vs. column 2) | |||
|---|---|---|---|---|---|
| 1. No lifetime depression (vs. MDE) | 2. Complicated bereavement (vs. MDE) | 3. Bereavement- excluded depression (vs. MDE) | |||
| Risks for Disorders During the Follow-up Period | OR (95% CI) | OR (95% CI) | OR (95% CI) | χ2 (df=1), P | χ2 (df=1), P |
| Depression | 0.21 (0.19, 0.23) | 0.46 (0.32, 0.66) | 0.33 (0.16, 0.65) | 1.7, 0.199 | 0.3, 0.373 |
| Panic | 0.32 (0.23, 0.46) | 0.63 (0.36, 1.08) | 0.52 (0.24, 1.13) | 1.6, 0.211 | 0.2, 0.686 |
| Social Phobia | 0.31 (0.26, 0.37) | 0.59 (0.36, 0.97) | 0.15 (0.04, 0.68) | 0.9, 0.348 | 2.9, 0.087 |
| Generalized Anxiety Disorder | 0.29 (0.25, 0.33) | 0.53 (0.33, 0.86) | 0.48 (0.22, 1.04) | 1.7, 0.191 | 0.1, 0.819 |
| Alcohol Dependence | 0.46 (0.40, 0.52) | 0.78 (0.51, 1.21) | 0.60 (0.25, 1.43) | 0.4, 0.526 | 0.3, 0.575 |
Odds ratios obtained from separate logistic regression models predicting each disorder, adjusting for age, sex, marital status, race/ethnicity, and educational attainment.
DISCUSSION
We sought to assess the validity of the bereavement exclusion in MDE, and theorized that if bereavement-excluded depression represents a loss reaction distinct from other cases of MDE, it would be associated with a lower level of the psychopathology indicators than both complicated bereavement and MDE.
Bereavement-excluded depression was less indicative of underlying psychopathology than MDE on the basis of psychiatric history, lower number of lifetime depressive episodes, lower levels of psychosocial impairment, lower likelihood of treatment seeking, and a reduced risk of subsequent disorders. These results might argue in favor of maintaining the distinction between MDE and bereavement-excluded depression in the diagnostic criteria. However, a problem with this argument is that individuals with bereavement-excluded depression still had a clinically significant depressive episode, which based on accumulating evidence may benefit from psychiatric treatment.8–11 We therefore do not interpret the results of this study to argue against providing professional treatment (either with psychotherapy, medication, or both) to individuals with clinically significant depressive symptoms that occur after a loss.
Despite the presence of symptoms that invoke the DSM-IV exception to the bereavement exclusion, complicated bereavement was rated similarly lower on the antecedent and consequent disorder indicators as was bereavement-excluded depression. Under the current diagnostic framework, the validity of the bereavement exclusion rests in part on the validity of its exception—allowing for a diagnosis to be made for bereavement-related depressions that are extreme. Therefore, if the bereavement exclusion were to be maintained, the exception for complicated bereavement should be strengthened so that cases of complicated bereavement more closely resemble MDE than bereavement-excluded depression.
Finally, the prevalence of bereavement-excluded depression in the NESARC was low in the overall sample (0.5%), and comprised a small proportion of individuals meeting symptom and impairment criteria for depression (2.3%). Though this finding is based on participants’ reports of their symptoms during their worst lifetime episode, which are subject to measurement error, it does not support the concern that has been expressed regarding a “massive pathologization of normal sadness”32,p.103 in epidemiologic studies applying DSM-IV criteria.
There are several recent studies on the role of bereavement and other stressors in the diagnosis of MDE. Karam et al. observed minimal differences between individuals with bereavement-related versus non-bereavement episodes of depression.4 Kessing et al. and Bock et al. also found no differences in pre-existing psychiatric vulnerability and in the long-term course of first-onset depression between patients whose depression was either preceded by the loss of a loved one, other stressful life events, or no events.33,34 In population-based samples, Wakefield et al. and Kendler et al. found substantially more similarities than differences between individuals with bereavement-related depression and individuals whose depression was related to other types of stressful life events.5,6 Corruble et al. investigated the severity of depression in a large case control study of patients who sought treatment for depression.35 In contrast to the other studies mentioned, Corruble et al. found that bereavement-excluded subjects had more severe depression than MDE controls without bereavement.
There are important differences in the designs used and specific questions posed between our study and those just cited. Karam et al.’s study is most similar to ours, comparing bereavement-related depression to non-bereavement depression in an epidemiologic sample unselected for seeking depression treatment.4 Kendler et al. and Wakefield et al. questioned whether or not the bereavement exclusion should be extended to cover other types of events or losses, and therefore compared bereavement-related depression to other event-related depression.5,6 The studies by Bock et al., Kessing et al., and Corruble et al. were based on treatment-seeking samples, and may over-represent severe cases; however, they benefitted from standardized interviews using validated scales of depressive symptoms and from diagnoses of depression made by clinicians.33–35 In contrast, our study compares the groups specifically referenced in DSM-IV (bereavement-related depression that is excluded from a diagnosis, bereavement-related depression that qualifies for a diagnosis—complicated bereavement, and MDE).
Limitations
Our study is based on the framework proposed by Robins and Guze,13,36–38 which posits that the validity of the diagnostic criteria can be established on the basis of phenomenological coherence and correlations with external indicators of psychiatric illness. Although we included a wider range of diagnostic indicators than Robins and Guze originally proposed, their approach to validation remains an indirect one. There are also alternative explanations for differences between groups on some of the diagnostic indicators used. For example, differences in rates of treatment seeking may be more reflective of cultural biases towards ignoring or normalizing one’s own depressive symptoms in the context of a recent loss than they are of differences in the pathological nature of depression.
There are limitations in our assessment of complicated bereavement. We were unable to implement the exceptions for morbid preoccupation with worthlessness and psychotic symptoms, and as a consequence, some cases of complicated bereavement were incorrectly classified as bereavement-excluded depression. Therefore, our analyses could underestimate the true differences between groups (because presumably more “severe” cases of depression were categorized along with the “less severe” group). Due to the skip patterns used in the NESARC interview, we could not determine the presence of the “complicated” symptoms for all cases of bereavement-related depression. Further research is needed using prospective follow-up and standardized clinical interviews to capture the extent of phenomenological variation in depressive episodes associated with the loss of a loved one, other stressful life events, or no identifiable stressors.
Finally, our comparisons were between different types of depressive episodes that were regarded as the participant’s worst episode (or, for single-episode cases, the participant’s only episode). The validity of these comparisons rests on the accuracy of participants’ recall of the timing of their depressive episodes relative to the experience of a loss, which may weaken over time.39,40 We also could not investigate the patterns of diagnostic indicators for different episodes in multi-episode cases, nor establish the temporality of all diagnostic validators with respect to the participant’s worst episode.
Conclusions
Bereavement-excluded depression is in many ways less indicative of psychopathology than MDE, but so is complicated bereavement. Our results showed marked differences in the magnitude of disorder indicators between individuals with MDE, and those with bereavement-excluded depression and complicated bereavement. However, the same pattern of differences that we observed between bereavement-excluded depression and MDE existed between complicated bereavement and MDE, and there were no detectable differences in disorder indicators between bereavement-excluded depression and complicated bereavement.
One interpretation of these findings, as explained above, is that bereavement-excluded depression should continue to be distinguished from MDE. This interpretation assumes maintaining the current diagnostic framework that has a bereavement exclusion and a complicated bereavement exception. However, our results suggest that the DSM-IV criteria cannot differentiate between non-disordered bereavement reactions and bereavement reactions that evolve into a psychiatric disorder. This is not surprising, given that psychiatric nosology since DSM-III has been designed to be “theory neutral,”41 and rejects classifying disorders based on their supposed causes.
Therefore, an alternative conclusion is that the exclusion-exception framework should be abandoned, and the diagnosis of MDE made solely based on symptoms, duration, and impairment, without regard to environmental precipitants. Doing so avoids the need to distinguish between episodes that are “understandable reactions to stressors”42, p.1847 and episodes that are pathological because they are disproportionate reactions, which requires making causal attributions for an individual’s symptoms—i.e., determining that the content of the symptoms is directly connected to a loss.43–45
For example, it is not simply the presence of suicidal ideation that currently separates MDE from bereavement; rather, the suicidal ideation must consist of “thoughts of death other than the survivor feeling that he or she would be better off dead or should have died with the deceased person;” similarly, the psychotic symptoms that separate MDE from bereavement include “experiences other than thinking that he or she hears the voices of, or transiently sees the image of, the deceased person.”46, p.741 Therefore, the bereavement exclusion in MDE is contradictory with our phenomenologically based nosology that purports not to incorporate assumptions about causal mechanisms into the diagnostic criteria.46,p.xxvi
Emerging evidence on the role of stressful life events in MDE, as well as supporting evidence for the role of stressors in neurobiological models of depression,47 suggest the possibility of advancing towards an etiologically based psychiatric nosology. Until then, however, incorporating hypothesized causes of disorders into the diagnostic criteria risks imposing theoretical and methodological challenges on research that aims to investigate those hypothesized causes.
Acknowledgments
Sources of support: This work was supported in part by National Institutes of Health grants MH087544, DA080887, and MH66057.
Footnotes
Prior presentation: A prior version of this work was presented at the Society for Epidemiologic Research, Anaheim, CA, June 2009.
Disclosures
Dr. Smoller. In the past 3 years, Dr. Smoller has consulted to Eli Lilly, the Herman Dana Trust, and RTI International, Inc.
Dr. Fava. Research Support: Abbott Laboratories, Alkermes, Aspect Medical Systems, Astra-Zeneca, Bio Research, BrainCells, Inc., Bristol-Myers Squibb Company, Cephalon, Clinical Trial Solutions, Eli Lilly & Company, Forest Pharmaceuticals Inc., Ganeden, GlaxoSmithKline, J & J Pharmaceuticals, Lichtwer Pharma GmbH, Lorex Pharmaceuticals, NARSAD, NCCAM, NIDA, NIMH, Novartis, Organon Inc., PamLab, LLC, Pfizer Inc, Pharmavite, Roche, Sanofi-Aventis, Shire, Solvay Pharmaceuticals, Inc., Synthelabo, Wyeth-Ayerst Laboratories
Advisory/Consulting: Abbott Laboratories, Amarin, Aspect Medical Systems, Astra-Zeneca, Auspex Pharmaceuticals, Bayer AG, Best Practice Project Management, Inc, BioMarin Pharmaceuticals, Inc., Biovail Pharmaceuticals, Inc., BrainCells, Inc, Bristol-Myers Squibb Company, Cephalon, Clinical Trials Solutions, CNS Response, Compellis, Cypress Pharmaceuticals, Dov Pharmaceuticals, Eli Lilly & Company, EPIX Pharmaceuticals, Euthymics Bioscience, Inc., Fabre-Kramer, Pharmaceuticals, Inc., Forest Pharmaceuticals Inc., GlaxoSmithKline, Grunenthal GmBH Janssen Pharmaceutica, Jazz Pharmaceuticals, J & J Pharmaceuticals, Knoll Pharmaceutical Company, Labopharm, Lorex Pharmaceuticals, Lundbeck, MedAvante Inc. Merck, Methylation Sciences, Neuronetics, Novartis, Nutrition 21, Organon Inc., PamLab, LLC, Pfizer Inc, PharmaStar, Pharmavite, Precision Human Biolaboratory, PsychoGenics, Roche, Sanofi-Aventis, Sepracor, Schering-Plough, Solvay Pharmaceuticals, Inc., Somaxon, Somerset Pharmaceuticals, Synthelabo, Takeda, Tetragenex, TransForm Pharmaceuticals, Inc., Transcept Pharmaceuticals, Vanda Pharmaceuticals Inc, Wyeth-Ayerst Laboratories
Speaking/Publishing: Advanced Meeting Partners, American Psychiatric Association, Astra-Zeneca, Belvoir, Boehringer-Ingelheim, Bristol-Myers Squibb Company, Cephalon, Eli Lilly & Company, Forest Pharmaceuticals Inc., GlaxoSmithKline, Imedex, Novartis, Organon Inc., Pfizer Inc, PharmaStar, MGH Psychiatry Academy/Primedia, MGH Psychiatry Academy/Reed-Elsevier, UBC, Wyeth-Ayerst Laboratories
Equity Holdings: Compellis
Royalty/patent, other income: patent applications for SPCD and for a combination of azapirones and bupropion in MDD, copyright royalties for the MGH CPFQ, SFI, ATRQ, DESS, and SAFER
References
- 1.Clayton PJ, Halikes JA, Maurice WL. The bereavement of the widowed. Dis Nerv Syst. 1971 Sep;32(9):597–604. [PubMed] [Google Scholar]
- 2.Clayton PJ, Halikas JA, Maurice WL. The depression of widowhood. Br J Psychiatry. 1972 Jan;120(554):71–77. doi: 10.1192/bjp.120.554.71. [DOI] [PubMed] [Google Scholar]
- 3.Clayton PJ, Herjanic M, Murphy GE, Woodruff R., Jr Mourning and depression: their similarities and differences. Can Psychiatr Assoc J. 1974 Jun;19(3):309–312. doi: 10.1177/070674377401900312. [DOI] [PubMed] [Google Scholar]
- 4.Karam EG, Tabet CC, Alam D, et al. Bereavement related and non-bereavement related depressions: a comparative field study. J Affect Disord. 2009 Jan;112(1–3):102–110. doi: 10.1016/j.jad.2008.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kendler KS, Myers J, Zisook S. Does bereavement-related major depression differ from major depression associated with other stressful life events? Am J Psychiatry. 2008 Nov;165(11):1449–1455. doi: 10.1176/appi.ajp.2008.07111757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wakefield JC, Schmitz MF, First MB, Horwitz AV. Extending the bereavement exclusion for major depression to other losses: evidence from the National Comorbidity Survey. Arch Gen Psychiatry. 2007 Apr;64(4):433–440. doi: 10.1001/archpsyc.64.4.433. [DOI] [PubMed] [Google Scholar]
- 7.Karam EG. The nosological status of bereavement-related depressions. Br J Psychiatry. 1994 Jul;165(2):48–52. doi: 10.1192/bjp.165.1.48. [DOI] [PubMed] [Google Scholar]
- 8.Zisook S, Shuchter SR, Pedrelli P, Sable J, Deaciuc SC. Bupropion sustained release for bereavement: results of an open trial. J Clin Psychiatry. 2001 Apr;62(4):227–230. doi: 10.4088/jcp.v62n0403. [DOI] [PubMed] [Google Scholar]
- 9.Reynolds CF, 3rd, Miller MD, Pasternak RE, et al. Treatment of bereavement-related major depressive episodes in later life: a controlled study of acute and continuation treatment with nortriptyline and interpersonal psychotherapy. Am J Psychiatry. 1999 Feb;156(2):202–208. doi: 10.1176/ajp.156.2.202. [DOI] [PubMed] [Google Scholar]
- 10.Hensley PL, Slonimski CK, Uhlenhuth EH, Clayton PJ. Escitalopram: an open-label study of bereavement-related depression and grief. J Affect Disord. 2009 Feb;113(1–2):142–149. doi: 10.1016/j.jad.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 11.Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. Lancet. 2007 Dec 8;370(9603):1960–1973. doi: 10.1016/S0140-6736(07)61816-9. [DOI] [PubMed] [Google Scholar]
- 12.Zisook S, Kendler KS. Is bereavement-related depression different than non-bereavement-related depression? Psychol Med. 2007 Jun;37(6):779–794. doi: 10.1017/S0033291707009865. [DOI] [PubMed] [Google Scholar]
- 13.Robins E, Guze SB. Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. Am J Psychiatry. 1970 Jan;126(7):983–987. doi: 10.1176/ajp.126.7.983. [DOI] [PubMed] [Google Scholar]
- 14.Grant BF, Kaplan K, Shepard J, Moore T. Source and accuracy statement for Wave 1 of the 2001–2002 National Epidemiology Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- 15.Grant BF, Kaplan K, Moore T, Kimball J. Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions: Source and Accuracy Statement. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2007. [Google Scholar]
- 16.Dawson DA, Goldstein RB, Grant BF. Rates and correlates of relapse among individuals in remission from DSM-IV alcohol dependence: a 3-year follow-up. Alcohol Clin Exp Res. 2007 Dec;31(12):2036–2045. doi: 10.1111/j.1530-0277.2007.00536.x. [DOI] [PubMed] [Google Scholar]
- 17.Grant BF, Dawson D. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. [Google Scholar]
- 18.Grant BG, Towle LH. Standardized diagnostic interviews for alcohol research. Alcohol Health & Research World. 1990;14(4):340–348. [Google Scholar]
- 19.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003 Jul 20;71(1):7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 20.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004 Aug;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 21.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005 Oct;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 22.Prigerson HG, Frank E, Kasl SV, et al. Complicated grief and bereavement-related depression as distinct disorders: preliminary empirical validation in elderly bereaved spouses. Am J Psychiatry. 1995 Jan;152(1):22–30. doi: 10.1176/ajp.152.1.22. [DOI] [PubMed] [Google Scholar]
- 23.Shear K, Frank E, Houck PR, Reynolds CF., 3rd Treatment of complicated grief: a randomized controlled trial. JAMA. 2005 Jun 1;293(21):2601–2608. doi: 10.1001/jama.293.21.2601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prigerson HG, Horowitz MJ, Jacobs SC, et al. Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS medicine. 2009 Aug;6(8):e1000121. doi: 10.1371/journal.pmed.1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Narrow WE, Rae DS, Robins LN, Regier DA. Revised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys’ estimates. Arch Gen Psychiatry. 2002 Feb;59(2):115–123. doi: 10.1001/archpsyc.59.2.115. [DOI] [PubMed] [Google Scholar]
- 26.Spitzer RL, Wakefield JC. DSM-IV diagnostic criterion for clinical significance: does it help solve the false positives problem? Am J Psychiatry. 1999 Dec;156(12):1856–1864. doi: 10.1176/ajp.156.12.1856. [DOI] [PubMed] [Google Scholar]
- 27.Thomas DC. Statistical methods in genetic epidemiology. Oxford; New York: Oxford University Press; 2004. [Google Scholar]
- 28.Grant BF, Hasin DS, Stinson FS, et al. Prevalence, correlates, and disability of personality disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2004 Jul;65(7):948–958. doi: 10.4088/jcp.v65n0711. [DOI] [PubMed] [Google Scholar]
- 29.Research Triangle Institute. SUDAAN Language Manual, Release 9.0. Research Triangle Park, NC: Research Triangle Institute; 2004. [Google Scholar]
- 30.Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology. 2001;27(1):85–95. [Google Scholar]
- 31.Reiter JP, Raghunathan TE, Kinney SK. The importance of modeling the sampling design in multiple imputation for missing data. Survey Methodology. 2006;32(2):143–149. [Google Scholar]
- 32.Horwitz AV, Wakefield JC. The loss of sadness: how psychiatry transformed normal sorrow into depressive disorder. New York: Oxford University Press; 2007. [DOI] [PubMed] [Google Scholar]
- 33.Bock C, Bukh JD, Vinberg M, Gether U, Kessing LV. Do stressful life events predict medical treatment outcome in first episode of depression? Soc Psychiatry Psychiatr Epidemiol. 2009 Sep;44(9):752–760. doi: 10.1007/s00127-008-0491-1. [DOI] [PubMed] [Google Scholar]
- 34.Kessing LV, Bukh JD, Bock C, Vinberg M, Gether U. Does bereavement-related first episode depression differ from other kinds of first depressions? Soc Psychiatry Psychiatr Epidemiol. 2009 Aug 20; doi: 10.1007/s00127-009-0121-6. [DOI] [PubMed] [Google Scholar]
- 35.Corruble E, Chouinard VA, Letierce A, Gorwood PA, Chouinard G. Is DSM-IV bereavement exclusion for major depressive episode relevant to severity and pattern of symptoms? A case-control, cross-sectional study. J Clin Psychiatry. 2009 Aug;70(8):1091–1097. doi: 10.4088/JCP.08m04475. [DOI] [PubMed] [Google Scholar]
- 36.Kendell RE. Clinical validity. Psychol Med. 1989 Feb;19(1):45–55. doi: 10.1017/s0033291700011016. [DOI] [PubMed] [Google Scholar]
- 37.Kendler KS. The nosologic validity of paranoia (simple delusional disorder). A review. Arch Gen Psychiatry. 1980 Jun;37(6):699–706. doi: 10.1001/archpsyc.1980.01780190097012. [DOI] [PubMed] [Google Scholar]
- 38.Kendler KS. Toward a scientific psychiatric nosology. Strengths and limitations. Arch Gen Psychiatry. 1990;47(10):969–973. doi: 10.1001/archpsyc.1990.01810220085011. [DOI] [PubMed] [Google Scholar]
- 39.Farrer LA, Florio LP, Bruce ML, Leaf PJ, Weissman MM. Reliability of self-reported age at onset of major depression. J Psychiatr Res. 1989;23(1):35–47. doi: 10.1016/0022-3956(89)90015-0. [DOI] [PubMed] [Google Scholar]
- 40.Wittchen HU, Burke JD, Semler G, Pfister H, Von Cranach M, Zaudig M. Recall and dating of psychiatric symptoms. Test-retest reliability of time-related symptom questions in a standardized psychiatric interview. Arch Gen Psychiatry. 1989;46(5):437–443. doi: 10.1001/archpsyc.1989.01810050051009. [DOI] [PubMed] [Google Scholar]
- 41.Wakefield JC. The DSM’s theory-neutral nosology is scientifically progressive: response to Follette and Houts (1996) Journal of Consulting & Clinical Psychology. 1998;66(5):846–852. doi: 10.1037//0022-006x.66.5.846. [DOI] [PubMed] [Google Scholar]
- 42.Kendler KS. Setting boundaries for psychiatric disorders. Am J Psychiatry. 1999 Dec;156(12):1845–1848. doi: 10.1176/ajp.156.12.1845. [DOI] [PubMed] [Google Scholar]
- 43.Kessing LV. Endogenous, reactive and neurotic depression -- diagnostic stability and long-term outcome. Psychopathology. 2004 May-Jun;37(3):124–130. doi: 10.1159/000078611. [DOI] [PubMed] [Google Scholar]
- 44.Pies RW. Depression and the pitfalls of causality: implications for DSM-V. J Affect Disord. 2009 Jul;116(1–2):1–3. doi: 10.1016/j.jad.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 45.Ghaemi SN. Pluralism in psychiatry: Karl Jaspers on science. Philosophy, Psychiatry, & Psychology. 2007;14(1):57–66. [Google Scholar]
- 46.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 47.Schiepers OJ, Wichers MC, Maes M. Cytokines and major depression. Prog Neuropsychopharmacol. Biol Psychiatry. 2005 Feb;29(2):201–217. doi: 10.1016/j.pnpbp.2004.11.003. [DOI] [PubMed] [Google Scholar]