Abstract
Objective We assessed the feasibility and acceptability to patients of a telephone-supported self-care intervention for depression among adults aged 40 years or over with one of six targeted chronic physical illnesses and comorbid depressive symptoms in family practice settings.
Methods An open, uncontrolled trial (feasibility study) was conducted among patients treated in Montreal family practices. Eligible patients were aged 40 years or over, had one or more of the targeted chronic physical illnesses for at least 6 months (arthritis, hypertension, diabetes, heart disease, asthma and chronic obstructive pulmonary disease) and were evaluated as having at least mild depressive symptoms (a score of ≥ 5 on the 9-item Patient Health Questionnaire, PHQ-9). Participants received a package of six self-care tools (information booklet, video, Internet programme, action plan, workbook and mood-monitoring tool) with telephone support by a lay coach for up to 6 months.
Results In total, 63 eligible patients provided written consent and completed the baseline interview; 57 (90%) and 55 (87%) patients completed 2-month and 6-month follow-up interviews, respectively. The mean number of telephone calls made by coaches to participants was 10.5 (SD 4.0), and the average length of these calls was 10.6 minutes. At the 6-month follow-up, 83.6% of the participants reported that one or more of the tools were helpful. Clinically significant improvements were seen in depressive symptoms (as assessed by the PHQ-9) at 6 months, with an effect size of 0.88 (95% CI, 0.55, 1.14).
Conclusion A telephone-supported self-care intervention for depression was feasible, was acceptable to patients, and was associated with a significant 6-month improvement in depressive symptoms. A randomised trial of this intervention is justified.
Keywords: comorbidity, depression, feasibility, primary care, self-management
Introduction
Depression is a frequent and serious problem in primary care settings; its course is often chronic and relapsing.1 People with chronic physical illnesses are at high risk for depression,2 and for experiencing poor outcomes (increased morbidity,3,4 mortality,5 functional decline,6–9 and high rates of use and costs of health services6,10,11). Depression increases non-adherence to medical treatment12 and unhealthy behaviours (e.g. physical inactivity).
Treatment guidelines for depression among adults with a chronic physical illness recommend low-intensity psychosocial interventions (including those based on principles of cognitive behaviour therapy, or CBT) rather than antidepressant medications.13 However, in many locations, publicly funded CBT is scarce.14 In this context, supported self-care interventions are attractive, because they offer a low-intensity alternative to the psychosocial/psychological/medical treatment and management of depression, and may reduce demands on mental health services.15,16 Self-care interventions based on CBT principles have shown promise in the management of many chronic illnesses, including depression.17,18 To date, however, there has been little research on the feasibility, acceptability to patients or effectiveness of self-care interventions for depression among adults with comorbid chronic physical illnesses.19
We aimed to assess the feasibility and acceptability of implementing a telephone-supported self-care intervention for depression in primary care patients aged 40 years or over with depressive symptoms and comorbid chronic physical illness. We conducted an open, uncontrolled trial of the intervention with the following objectives: (1) to explore barriers to identifying and recruiting eligible patients from family practices; (2) to describe patient use and perceptions of different types of self-care tools; (3) to describe changes in depressive symptoms and health behaviours in relation to use of tools; and (4) to compare the above as a function of age and baseline depression severity.
Methods
The study design was an open, uncontrolled trial. The study was conducted during 2010–2011.
The intervention
We conducted focus groups and consultations with family physicians (FPs), social workers, psychologists, and nurses with experience in depression management in primary care to develop the intervention and select the self-care tools. A ‘toolkit’ containing a variety of self-care approaches to manage depression (both informational and behavioural) was assembled, and included audio-visual, Internet and paper-based tools selected for their appeal to individuals with different learning styles. We used both existing materials and those adapted (with permission) for the study. Because of our bilingual population, tools were required in both English and French.
We then pre-tested the revised tools and study questionnaires among patients from family practice and psychiatric settings (n = 12), including older men and women with varying severity of depression. As a result of this preparatory phase, the language used in both the tools and the study questionnaires was simplified. We also adjusted some of the graphics and illustrations in the tools to make them more visually appealing.
The final toolkit consisted of three informational tools, three behavioural tools and two supplementary tools. The informational tools were (1) a video/DVD on depression,20 (2) an information leaflet that emphasised the link between depression and chronic disease, and (3) information on how to access two Internet programmes, one in English and the other in French.21,22 The behavioural tools incorporated principles of CBT, and consisted of (1) the Antidepressant Skills Workbook (paper and audio versions)23,24 used elsewhere in Canada in depression self-care interventions, (2) an Action Plan, adapted from the Workbook, that targeted five behaviours (taking prescribed medications, eating a healthy diet, being physically active, increasing social activity, and making time for rewarding activities), and (3) a Mood Monitoring Notebook, adapted from a similar tool25 that allowed individuals to rate their mood up to three times a day. The supplementary tools were an adapted Information Booklet for family members,26 and a Community Resources Manual that described support and self-help groups available in the community.
Two bilingual (English/French) coaches (non-therapists with some counselling experience) were trained to provide telephone-based support for up to 6 months. A schedule of short, weekly calls for the first 3 months was followed by monthly calls up to 6 months. The coaches were guided by scripts to provide information and encourage and guide the patient in the use of the tools, but not to provide therapy. The study psychiatrist (MC) and psychologist (KL) trained and supervised the coaches; each coach call was logged and audiotaped to aid supervision.
Recruitment of family practices
We sought to determine the feasibility of FP participation in an unselected sample of FPs using a list of FPs obtained from the provincial association of FPs. Thus we sent letters to a random sample of 375 FPs practising within approximately 30 minutes travelling time of the study site in metropolitan Montreal, inviting them to meet a research assistant (RA). Those who agreed to participate signed a consent form, and arranged to distribute (mostly via office staff) study screening forms to their patients during an office visit. A member of the research team met with office staff and helped them to select an appropriate method of distributing and collecting screening forms (e.g. via secretaries, nurses or FPs). This person then visited each practice regularly to troubleshoot the distribution of screening forms. A study newsletter to update FPs on progress with the study and to motivate continued participation was distributed periodically. Irrespective of this study, FPs were expected to continue their normal care for all patient problems as conditions dictated.
Recruitment and follow-up of patient sample
Participants were required to meet all of the following inclusion criteria: age 40 years or over, diagnosed with one or more of the targeted chronic physical illnesses (arthritis, hypertension, diabetes, heart disease, asthma, chronic obstructive pulmonary disease) at least 6 months previously, and evaluated as having at least mild depressive symptoms (a score of ≥ 5 on the 9-item Patient Health Questionnaire, PHQ-9).27,28 Exclusion criteria were residence in a nursing home, suicidal plans, inability to read in either English or French, and a cognitive or physical impairment that would prevent participation in the self-care intervention. Cognitive impairment was measured with the 6-item Blessed Orientation-Memory-Concentration (BOMC) test.29 Patients with a score of ≥ 10 were excluded; a score of 6–9 indicated mild cognitive impairment.30 Finally, patients who were receiving counselling or help at least once a month for a mental health problem from any health professional other than their family doctor were excluded. However, patients who began such treatment after enrolment were not withdrawn from the study.
Inclusion and exclusion criteria were assessed using a two-step process: (1) screening via self-completed questionnaire at an FP office visit; and (2) a telephone interview with a trained RA. During Step 1, patients completed a form enquiring about age, physician-diagnosed chronic physical illnesses, and a two-question depression screen.31,32 Patients who fulfilled the study criteria who were interested in participating in the study were asked to indicate this by signing the questionnaire and by providing a contact telephone number.
During Step 2, the RA administered a verbal consent. Among those who consented, the RA then verified the eligibility criteria and invited eligible patients to participate in the study. Those who provided subsequent verbal consent were sent the study consent form with a stamped pre-addressed return envelope. Those who returned the signed consent form were sent a package of self-care tools, and were contacted for a baseline telephone interview. Follow-up telephone interviews were conducted at 2 and 6 months after the baseline interview, to assess use and perceptions of the self-care tools, and outcomes.
Patients with severe depressive symptoms (a PHQ-9 score of ≥ 20) at screening were not excluded from the study, but were specifically referred to their FP. Those whose depression worsened during the course of the study were either referred to their FP or were closely observed by their coach and the study psychiatrist. Patients were not withdrawn from the study unless they had suicidal plans.
Outcome measures
The primary outcome measure was the change in the PHQ-9 score from baseline to 6 months. The PHQ-9 has been validated as a responsive outcome measure.27,28
The following secondary outcome measures were assessed at the baseline and 6-month follow-up interviews. The Short Form-12 (SF-12) physical and mental component summary scores measured physical and mental health status.33 The 13-item Patient Activation Measure (PAM)34,35 was used; the overall score ranges from 0 to 100, with higher scores indicating greater activation.34 Measures of daily activities during the previous week, adapted from prior instruments,36–39 included social activities (visits and telephone conversations with family members, friends and neighbours, attendance at religious services, social or recreational groups, and trips), solitary activities (spending time on hobbies, or on reading, writing, or listening to music, or attending concerts, plays or art exhibitions), and productive or physical activities (volunteer work, light housework and heavy housework). Questions about current smoking and alcohol use were adapted from the Health Practices Index.40 Adherence to prescribed medications was measured with the 4-item Morisky questionnaire.41 The Godin Leisure Time Exercise Questionnaire was used to assess physical activity during the previous week.42 At 6 months, participants were asked whether they had changed any health behaviours (adherence to daily medications, healthy eating, exercise, social activities, and making time for rewarding activities).
Antidepressant medication use at baseline was based on patient self-report. At the 6-month follow-up, patients were asked about any changes in these medications, and about any psychological or counselling therapies they had received since entering the study.
Measures of self-reported health services utilisation at baseline included hospitalisation during the previous 12 months, emergency department visits and doctor visits during the previous 3 months, and formal homecare services during the previous 4 weeks. These questions were repeated at the 6-month follow-up (the reporting period for hospitalisation was the 6 months since entry to the study).
Measures of patient adherence to and perceptions of the intervention
We assessed intervention adherence using measures of the extent to which patients reported that they used each tool at 2 months, and the total number of completed coach telephone calls made by 6 months. We assessed the acceptability of the intervention by asking patients at 6 months about the perceived helpfulness of each tool and the coach calls, and their overall satisfaction with the intervention.
At the 2-month interview, we asked patients which self-care tools they had tried, and how much of each tool they had completed on a 6-point Likert scale from 0 (not at all) to 5 (completed). The measure of use of the Mood Monitoring Notebook was frequency of use during the previous 2 months on a 6-point Likert scale from 0 (not at all) to 5 (every day). Mean tool use scores were computed across the informational and behavioural tools, respectively, and grouped as < 1 (minimal), 1–2 (moderate) and 3–5 (high). We also asked patients to comment on what they liked most and least about the tools that they had selected.
At the 6-month interview, patients were again asked which of the tools they had used (but not about the extent of use). We also asked how helpful each tool was in improving their mood (helpful, neutral or not helpful). Patients were asked to comment on how each tool was helpful, and what would have made each tool more helpful. They were also asked whether the phone calls from the coach were an important part of the intervention (yes, no or not sure), and whether they could have used the tools on their own (yes, no or not sure). General satisfaction with the study intervention was measured with the Client Satisfaction Questionnaire (CSQ-8).43,44
Other measures
Sociodemographic variables collected at screening or baseline interviews included age, gender, language of intervention (English or French), living arrangements, marital status, level of education, place of birth and family income.45,46 Comorbid mental disorders were also assessed at screening.47,48
Statistical methods
We compared characteristics of the sample, use and perceptions of the tools by age and depression severity using the chi-square test, Fisher's exact test and t-tests. The clinical significance of change in the PHQ-9 outcome at 6 months was assessed with two measures, namely the percentage of individuals whose symptoms declined by at least 50% from the initial level, and the effect size (the pre–post change divided by the SD of the 6-month score).49 Changes over time from screening or baseline to 6 months in the outcome variables were analysed using generalised estimating equation (GEE) methodology.50 Similar approaches were used to compare the change in the outcome variables for the two age groups (< 60 and ≥ 60 years) and baseline PHQ-9 group (< 15 and ≥ 15). The association between intervention adherence (use of tools at 2 months and number of coach contacts over 6 months) and changes in the PHQ-9 at 6 months was analysed using linear regression models.51 Level of depression (PHQ-9) at baseline was forced in all multivariable models. Additional baseline variables (age, gender, level of cognitive impairment (BOMC score) and SF-12 physical score) and depression treatment variables (antidepressant medication at baseline and/or follow-up and psychosocial treatment at follow-up) were also considered for the full multivariate model. Stepwise selection by the Bayesian information criterion (BIC)52 was used to assist with model reduction. All calculations were performed using SAS 9.1.
Results
Recruitment of family physicians
Of the 375 FPs who were invited to participate in the study, 119 (31.7%) could not be contacted by the RA. Of the remaining 256 FPs, 146 were ineligible (either because their practice location was outside our 30-minute travelling area, contrary to what was listed, or because the nature of their patients or type of practice did not meet the study objectives). Of the 110 potentially eligible FPs, consent to participate was received from 63 individuals (57.3%). One or more screening forms were returned by 41 out of 63 (65%) of these FPs' practices.
Recruitment of patients
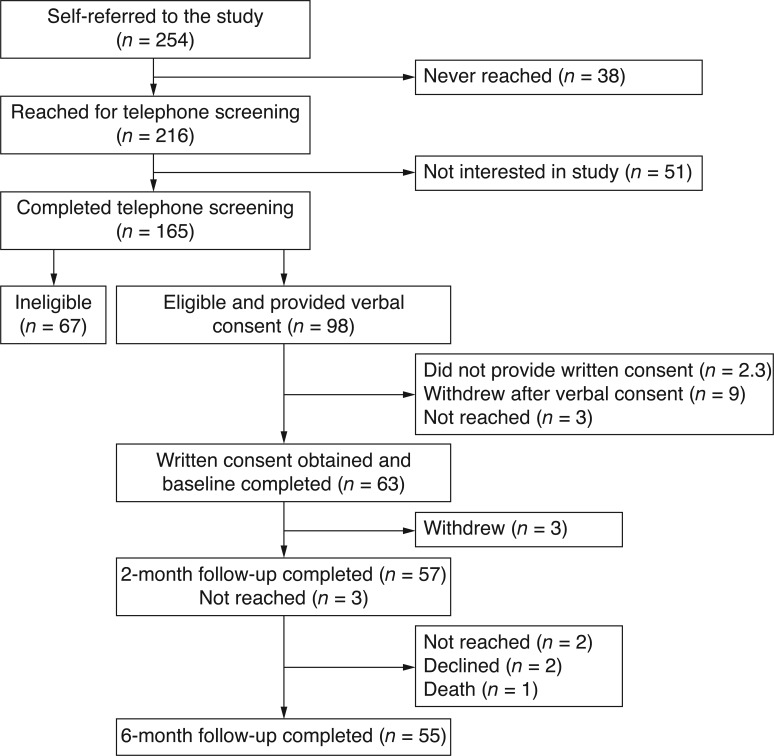
Of 254 patients whose completed screening forms were returned by the 41 practices, 98 (39%) were eligible for and interested in study participation (38 patients (15%) could not later be reached by telephone, 51 patients (20%) were no longer interested and 67 patients (26%) were not eligible) (see Figure 1). The reasons for ineligibility were no target chronic disease (9 patients), inability to read either English or French (5 patients), visual or physical impairment (3 patients), cognitive impairment (13 patients), a PHQ-9 score of < 5 (23 patients), currently receiving counselling (11 patients), and suicidal plans (3 patients). (The suicidal patients were referred to their FP and community suicide services.)
Figure 1.
Results of patient screening, recruitment and follow-up
Of the 98 patients who were interested in and eligible for participation in the study, 63 (64%) returned a signed consent form. The numbers of signed consent forms did not differ significantly by age, gender or PHQ-9 score. Of the 63 participants, 100% completed the baseline interview, 90% (57 patients) completed the 2-month follow-up, and 87% (55 patients) completed the 6-month follow-up interview. Reasons for non-completion were death (1 patient) and withdrawal or refusal (5 patients); the remainder could not be contacted within the time window for the follow-up. No patients became suicidal during the follow-up.
The characteristics of the participants are listed in Table 1. Older participants were more likely to have had a longer relationship with their FP. Although other differences by age were not statistically significant, older patients unexpectedly tended to have lower rates of mild cognitive impairment and lower rates of health services utilisation than middle-aged participants, and a similar level of physical health status (as assessed by the SF-12 PCS).
Table 1.
Characteristics of the study sample at baseline, by age group
| Characteristic | Overall (n = 63) | Age < 60 years (n = 30) | Age ≥ 60 years (n = 33) | P-value (χ2 test) |
|---|---|---|---|---|
| Sociodemographic | ||||
| Median age (range) | 61 (42) | |||
| Female (%) | 74.6 | 76.7 | 72.7 | 0.720 |
| Lives alone (%) | 30.2 | 20.0 | 39.4 | 0.094 |
| Married/common-law (%) | 44.4 | 46.7 | 42.4 | 0.735 |
| High-school education or more (%) | 82.5 | 86.7 | 78.8 | 0.411 |
| Born in Canada (%) | 76.2 | 76.7 | 75.8 | 0.933 |
| French-speaking (%) | 52.4 | 53.3 | 48.5 | 0.885 |
| Low income (%) | 27.5 | 30.8 | 24.0 | 0.588 |
| Health measures | ||||
| Chronic disease diagnoses | ||||
| Asthma (%) | 33.3 | 33.3 | 33.3 | 1.00 |
| Chronic obstructive lung disease (%) | 30.2 | 23.3 | 36.4 | 0.333 |
| Diabetes (%) | 30.2 | 26.7 | 33.3 | 0.565 |
| Hypertension (%) | 69.8 | 63.3 | 75.8 | 0.283 |
| Heart disease (%) | 20.6 | 10.0 | 30.3 | 0.138 |
| Arthritis (%) | 36.5 | 33.3 | 39.4 | 0.307 |
| Number of chronic diseases | 0.056 | |||
| 2 chronic diseases (%) | 33.3 | 33.3 | 33.3 | |
| ≥ 3 chronic diseases (%) | 22.2 | 10.0 | 33.3 | |
| Mean PHQ-9 score (SD) | 12.4 (5.0) | 13.1 (4.9) | 11.9 (5.1) | 0.350* |
| Mean SF-12 mental summary (MCS) (SD) | 39.4 (10.9) | 37.4 (10.7) | 41.3 (10.9) | 0.162* |
| Mean SF-12 physical summary (PCS) (SD) | 40.3 (11.1) | 40.6 (10.6) | 40.1 (11.7) | 0.877* |
| Depression diagnosis: | 0.780 | |||
| Major depression (%) | 31.8 | 33.3 | 30.3 | |
| Other depression (%) | 23.8 | 26.7 | 21.2 | |
| Panic disorder (%) | 20.6 | 23.3 | 18.2 | 0.614 |
| Other anxiety disorder (%) | 33.3 | 40.0 | 27.3 | 0.285 |
| Somatoform disorder (%) | 47.6 | 56.7 | 39.4 | 0.170 |
| Alcohol abuse (%) | 24.2 | 31.3 | 17.7 | 0.362 |
| Mild cognitive impairment (%) | 17.5 | 23.3 | 12.1 | 0.242 |
| Mean total number of medications (SD) | 5.5 (3.3) | 4.8 (3.6) | 6.2 (2.9) | 0.093* |
| Antidepressant medications | 0.325 | |||
| Current (%) | 33.3 | 28.6 | 37.9 | |
| Previous only (%) | 33.3 | 42.9 | 24.1 | |
| Previous psychological treatment (%) | 58.2 | 64.3 | 51.9 | 0.350 |
| Health services utilisation | ||||
| Hospitalisation in past 12 months (%) | 21.0 | 30.0 | 12.5 | 0.091 |
| Emergency department visits in past 3 months (%) | 21.0 | 26.7 | 15.6 | 0.286 |
| Homecare services in past 30 days (%) | 15.9 | 23.3 | 9.1 | 0.122 |
| Same family physician for ≥ 10 years (%) | 58.1 | 43.3 | 71.9 | 0.035 |
* t-test.
Patient adherence to and perceptions of the intervention
Table 2 shows the patients' use of the self-care tools and completed coach calls at the 2-month follow-up. Participants' use of the intervention was highest for the video/DVD and lowest for the Internet programmes. These rates did not differ with age group or PHQ-9 score.
Table 2.
Adherence to intervention at 2-month follow-up
| Measure | 2-month follow-up (n = 57) |
|---|---|
| Use of informational tools | |
| Information brochure | |
| Tried n (%) | 36 (63.1) |
| Tried and completed at least half n (%) | 23 (40.4) |
| Internet programmes | |
| Tried n (%) | 6 (10.6) |
| Tried and completed at least half n (%) | 4 (7.0) |
| Video/DVD | |
| Tried n (%) | 37 (64.9) |
| Tried and completed at least half n (%) | 35 (61.4) |
| Mean use of informational tools | |
| Minimal (< 1) | 14 (24.6) |
| Moderate (1–2) | 30 (52.6) |
| High (3–5) | 13 (22.8) |
| Use of behavioural tools | |
| Action plan | |
| Tried n (%) | 33 (57.9) |
| Tried and completed at least half n (%) | 21 (36.8) |
| Antidepressant Skills Workbook | |
| Tried n (%) | 32 (56.1) |
| Tried and completed at least half n (%) | 18 (31.6) |
| Mood Monitoring Notebook | |
| Tried n (%) | 37 (64.9) |
| Tried and completed at least half n (%) | 15 (26.3) |
| Mean use of behavioural tools | |
| Minimal (< 1) | 20 (35.1) |
| Moderate (1–2) | 22 (38.6) |
| High (3–5) | 15 (26.3) |
| Coaching | |
| Mean completed coach calls (SD) | 5.7 (2.4) |
| Mean duration of coach calls (minutes) (SD) | 11.7 (4.4) |
At the 6-month follow-up, about half of the participants reported that all of the tools had been helpful except for the Internet programmes, which were used much less (see Table 3). Overall, 84% of the participants reported that at least one tool had been helpful. There were significant differences by age group in both the use and perceptions of the Antidepressant Skills Workbook and the Mood Monitoring Notebook, indicating that whereas fewer of the older participants found the Workbook helpful, more of them found the Mood Monitoring Notebook helpful, compared with younger participants. Participants with a lower PHQ-9 at baseline (< 15) were more satisfied with the intervention, and more of them rated the coach calls as important, compared with the participants with higher scores.
Table 3.
Adherence to and acceptability of intervention at 6-month follow-up by age and initial PHQ-9 score
| Measure | Overall (n = 55) | Age < 60 years (n = 24) | Age ≥ 60 years (n = 31) | χ2 P-value | PHQ9 < 15 (n = 38) | PHQ9 ≥ 15 (n = 17) | χ2 P-value |
|---|---|---|---|---|---|---|---|
| Informational tools | |||||||
| Information brochurea | 0.397* | 0.259* | |||||
| Did not try n (%) | 2 (3.7) | 0 (0.0) | 2 (6.5) | 1 (2.7) | 1 (5.9) | ||
| Tried, did not find helpful n (%) | 22 (40.7) | 12 (50.0) | 11 (35.5) | 13 (35.1) | 9 (52.9) | ||
| Tried, found helpful n (%) | 30 (55.6) | 12 (50.0) | 18 (58.0) | 23 (62.2) | 7 (41.2) | ||
| Internet programmes | 1.000* | 0.304* | |||||
| Did not try n (%) | 41 (74.6) | 18 (75) | 23 (74.2) | 30 (79) | 11 (64.7) | ||
| Tried, did not find helpful n (%) | 5 (9.1) | 2 (8.3) | 3 (9.7) | 2 (5.3) | 3 (17.7) | ||
| Tried, found helpful n (%) | 9 (16.4) | 4 (16.7) | 5 (16.1) | 6 (15.8) | 3 (17.7) | ||
| Video/DVDa | 0.380 | 0.074* | |||||
| Did not try n (%) | 13 (24.1) | 7 (30.4) | 6 (19.4) | 10 (27.0) | 3 (17.7) | ||
| Tried, did not find helpful n (%) | 14 (25.9) | 7 (30.4) | 7 (22.6) | 6 (16.2) | 8 (47.1) | ||
| Tried, found helpful n (%) | 27 (50.0) | 9 (39.1) | 18 (58.1) | 21 (56.8) | 6 (35.3) | ||
| Any informational tool found helpful n (%) | 39 (70.9) | 15 (62.5) | 24 (77.4) | 0.227 | 30 (79) | 9 (52.9) | 0.062* |
| Behavioural tools | |||||||
| Action plana | 1.000* | 0.098* | |||||
| Did not try n (%) | 17 (31.5) | 8 (33.3) | 9 (30.0) | 10 (27.0) | 7 (41.2) | ||
| Tried, did not find helpful n (%) | 7 (13.0) | 3 (12.5) | 4 (13.3) | 3 (8.1) | 4 (23.5) | ||
| Tried, found helpful n (%) | 30 (55.5) | 13 (54.2) | 17 (56.7) | 24 (64.5) | 6 (35.3) | ||
| Antidepressant Skills Workbookb | 0.015* | 0.224* | |||||
| Did not try n (%) | 17 (32.1) | 3 (13.0) | 14 (46.7) | 11 (29.7) | 6 (37.5) | ||
| Tried, did not find helpful n (%) | 8 (15.1) | 6 (26.1) | 2 (6.6) | 4 (10.8) | 4(25.0) | ||
| Tried, found helpful n (%) | 28 (52.8) | 14 (60.9) | 14 (46.7) | 22 (59.5) | 6 (37.5) | ||
| Mood Monitoring Notebook | 0.025* | 0.615 | |||||
| Did not try n (%) | 18 (32.7) | 7 (29.2) | 11 (35.5) | 14 (36.8) | 4 (23.5) | ||
| Tried, did not find helpful n (%) | 8 (14.6) | 7 (29.2) | 1 (3.2) | 5 (13.2) | 3(17.7) | ||
| Tried, found helpful n (%) | 29 (52.7) | 10 (41.7) | 19 (61.3) | 19 (50) | 10 (58.8) | ||
| Any behavioural tool found helpful n (%) | 42 (76.4) | 18 (75) | 24 (77.4) | 0.834 | 31 (81.6) | 11 (64.7) | 0.190* |
| Any tool found helpful n (%) | 46 (83.6) | 19 (79.2) | 27 (87.1) | 0.482* | 34 (89.5) | 12 (70.6) | 0.116* |
| Coaching | |||||||
| Mean number of completed coach calls (SD) | 10.5 (4.0) | 9.9 (3.9) | 11.1 (4) | 0.272** | 10.9 (3.6) | 9.8 (4.6) | 0.332** |
| Mean duration of coach calls (minutes) (SD) | 10.6 (3.7) | 11.0 (4.2) | 10.4 (3.3) | 0.580 | 10.4 (4.1) | 11.2 (2.4) | 0.401 |
| Coach calls were important n (%) | 48 (90.6) | 21 (91.3) | 27 (90) | 0.358* | 35 (97.2) | 13 (76.5) | 0.032* |
| Could have used tools without coach n (%) | 24 (47.1) | 13 (56.5) | 11 (39.3) | 0.220 | 16 (44.4) | 8 (53.3) | 0.562 |
| Satisfaction (CSQ-8) mean (SD) | 25.1 (5.5) | 25.2 (4.5) | 25.1 (6.3) | 0.983** | 26.2 (4.9) | 22.8 (6.1) | 0.034** |
* Fisher's exact test.
** t-test.
a 1 missing.
b 2 missing.
Those who found the behavioural tools helpful indicated that seeing information in a written form provided them with both direction (e.g. ‘It gave me procedures to follow’, ‘It motivated me a lot to plan my day and arrange my life priorities’) and insight (e.g. ‘It helped me to pinpoint specific times in the day when specific things made me feel the way I was feeling’, ‘It let me detect when I was going to feel depressed and figure out ways to improve my mood’, ‘I learnt that things always look bigger than they are in reality’). Participants who did not find these tools helpful identified a conflict between their own preferences and the nature of these tools (e.g. ‘I am not good at writing things down’, ‘I find talking better than reading’). Positive comments on the information leaflet indicated that it clarified patients' understanding of depression, although some individuals commented that they already knew the information. Participants found the video/DVD helpful because the testimonials helped them to see that depression was a ‘normal thing in life.’ However, others said that they preferred reading. Although few participants found the Internet programmes helpful, one participant reported that this was the main tool that he used. Other participants found that these programmes were too complicated or stressful to use.
Clinical outcomes
There were statistically significant decreases from baseline to 6 months in the PHQ-9 score, the proportion of participants who were using antidepressant medications, and alcohol consumption by the participants (see Table 4). The Mental Component Summary score increased (indicating improvement), as did the frequency of social contacts. Notably, similar changes were seen among younger and older participants, and by initial PHQ-9 group. In response to direct questions about behaviour changes, 58% of the participants reported that they had made changes by eating a healthier diet, taking exercise, and making time for rewarding activities, 33% of the participants reported changes in social activities, and 23% reported making changes to improve their adherence to medication (data not shown).
Table 4.
Changes in clinical outcomes from baseline to 6-month follow-up (n = 55)
| Outcome variables | (Missing) | Baseline | Six-month follow-up | P-value* |
|---|---|---|---|---|
| Depression diagnosis | (2) | 0.001 | ||
| None (%) | 47.2 | 71.7 | ||
| Minor depression (%) | 18.9 | 7.6 | ||
| Major depression (%) | 34.0 | 20.8 | ||
| Mean depression severity (PHQ-9) (SD) | (2) | 12.4 (5.3) | 6.8 (6.3) | < 0.0001 |
| SF-12 | ||||
| Mean mental summary (MCS) (SD) | (3) | 39.0 (11.2) | 45.2 (12.9) | < 0.0001 |
| Mean physical summary (PCS) (SD) | (3) | 41.4 (11.0) | 41.9 (11.0) | 0.710 |
| Mean activation (SD) | (15) | 60.4 (13.6) | 62.2 (14.4) | 0.468 |
| Daily activities | ||||
| Mean social activities (SD) | (3) | 11.0 (7.0) | 13.3 (7.4) | 0.042 |
| Mean solitary activities (SD) | (3) | 6.1 (3.7) | 6.6 (3.9) | 0.487 |
| Mean productive activities (SD) | (3) | 4.6 (3.6) | 4.9 (3.6) | 0.563 |
| Mean exercise (SD) | (4) | 5.0 (4.7) | 4.4 (3.4) | 0.338 |
| Cigarette smoking | (1) | 0.320 | ||
| Does not smoke | 79.6 | 83.3 | ||
| Smokes < 10 cigarettes per week | 3.7 | 1.8 | ||
| Smokes ≥ 10 cigarettes per week | 16.7 | 14.8 | ||
| Alcohol consumption | (17) | 0.007 | ||
| Does not drink | 34.2 | 47.4 | ||
| 1–6 drinks per week | 44.7 | 39.5 | ||
| ≥ 7 drinks per week | 21.1 | 13.2 | ||
| Medication adherence | (3) | 0.075 | ||
| 0 (adherent) | 57.7 | 76.9 | ||
| 1 | 25.0 | 5.8 | ||
| ≥ 2 (non-adherent) | 17.3 | 17.3 | ||
| Antidepressant medication use | (2) | 32.1 | 20.8 | 0.006 |
| Emergency department visits in past 3 months | 17.7 | 19.6 | 0.739 | |
| Counselling or therapy | (2) | 20.7 | ||
* Generalised estimating equations (GEE) methodology was used to study the relationship of the change in time for each variable.
The measures of clinical significance on the PHQ-9 change (n = 53) indicated that 57% (95% CI: 43%, 70%) of the participants showed at least a 50% decline in their score; the overall effect size was 0.88 (95% CI: 0.55, 1.14). Of the patients whose initial PHQ-9 score was ≥ 10 (n = 35), 54% (95% CI: 38%, 71%) showed at least a 50% decline in their score; the effect size was 1.0 (95% CI: 0.60, 1.60).
Only three participants (5%) were observed either by interviewers or coaches to show a temporary worsening of depression symptoms during follow-up. Two of these individuals were brought to the attention of their FPs after their consent had been obtained; the third participant spoke to the study psychiatrist, who encouraged that patient to speak to their FP. None of the participants developed suicidal plans.
Predictors of clinical outcomes
The regression models found that a higher initial PHQ-9 score predicted a greater 6-month decline in the PHQ-9 score. After adjustment for PHQ-9 score, age, baseline SF-12 physical component summary score and gender were not associated with the change in PHQ-9 score (see Table 5). Cognitive impairment predicted less decline in the PHQ-9 score in the multivariate model.
Table 5.
Linear regression models of associations between baseline measures, adherence to interventions, depression treatment and change in PHQ-9 score at 6-month follow-up (n = 51)
| Univariate models | Multivariate models* | Multivariate model | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Beta | 95% CI | P-value | Beta | 95% CI | P-value | Beta | 95% CI | P-value | |
| Baseline measures*** | ||||||||||
| PHQ-9 (5-point increase) | 51 | −3.0 | −4.7, −1.4 | < 0.001 | −3.0 | −4.7, −1.4 | <0.001 | −3.6 | −5.1, −2.0 | < 0.001 |
| Cognitive impairment (1-point increase) | 51 | 0.5 | −0.2, 1.3 | 0.162 | 0.7 | 0.1, 1.4 | 0.031 | 0.7 | 0.1, 1.3 | 0.030 |
| SF-12 physical (1-point increase) | 51 | 0.0 | −0.2, 0.2 | 0.885 | −0.1 | −0.2, 0.1 | 0.351 | |||
| Age (years) | ||||||||||
| < 60 | 23 | 0.0 | 0.0 | |||||||
| ≥ 60 | 28 | −1.0 | −4.8, 2.9 | 0.620 | −1.6 | −5.1, 1.8 | 0.346 | |||
| Gender | ||||||||||
| Female | 36 | 3.2 | −0.9, 7.3 | 0.128 | 3.4 | −0.2, 7.1 | 0.064 | |||
| Male | 15 | 0.0 | 0.0 | |||||||
| Intervention adherence | ||||||||||
| Informational tool use (mean) | ||||||||||
| Minimal (< 1) | 11 | 0.0 | 0.0 | |||||||
| Moderate (1–2) | 28 | −1.2 | −6.1, 3.8 | 0.639 | −0.9 | −5.2, 3.4 | 0.671 | |||
| High (3–5) | 12 | −2.8 | −8.6, 3.0 | 0.335 | −3.5 | −8.5, 1.6 | 0.179 | |||
| Behavioural tool use (mean) | ||||||||||
| Minimal (< 1) | 15 | 0.0 | 0.0 | 0.0 | ||||||
| Moderate (1–2) | 21 | −5.5 | −9.9, −1.0 | 0.017 | −5.4 | −9.2, −1.6 | 0.006 | −5.4 | −9.0, −1.7 | 0.005 |
| High (3–5) | 15 | −3.5 | −8.3, 1.3 | 0.153 | −5.8 | −10.1, −1.6 | 0.008 | −5.4 | −9.5, −1.3 | 0.012 |
| Number of completed coach contacts | 51 | 0.0 | −0.5, 0.4 | 0.869 | −0.1 | −0.5, 0.3 | 0.608 | |||
| Depression treatment | ||||||||||
| Antidepressant medication | ||||||||||
| At both baseline and 6 months | 10 | 4.4 | −0.5, 9.2 | 0.075 | 4.0 | −0.2, 8.3 | 0.064 | |||
| Only at baseline | 6 | −0.3 | −6.2, 5.7 | 0.930 | −1.6 | −6.8, 3.7 | 0.556 | |||
| Neither | 35 | 0.0 | 0.0 | |||||||
| Psychosocial at 6 months | ||||||||||
| No | 40 | 0.0 | 0.0 | |||||||
| Yes | 11 | 3.5 | −1.1, 8.1 | 0.132 | 4.1 | 0.1, 8.1 | 0.045 | |||
95% CI, 95% confidence interval.
* Each model is adjusted for baseline PHQ-9 score.
At least moderate use of the behavioural tools at the 2-month follow-up was associated with a significantly greater decline in depressive symptoms compared with minimal adherence. Use of the informational tools and the number of coach contacts were not associated with decline in PHQ-9 score. Although both continued use of antidepressant medications from baseline to follow-up and initiation of psychological therapy were associated with an increase in the PHQ-9 score, after adjustment for baseline PHQ-9 score, these treatment measures did not contribute to the final model and were excluded (see Table 5).
Discussion
We have reported on a study of the feasibility and acceptability of implementing a telephone-supported self-care intervention for depression among depressed adults aged 40 years or over with comorbid chronic physical illnesses being treated in primary care. Overall we found that just over one-third of eligible FPs were able to implement the screening process in their practices. Among the participating patients, the intervention was feasible, acceptable, safe, and accompanied by a significant improvement in depressive symptoms across the different age groups and levels of depressive symptoms.
Feasibility
Physicians
The greatest barriers to feasibility of the intervention were identifying interested FPs and implementing the office-based screening procedures. Although the initial participation rate among eligible FPs was 57.3%, similar to that reported in other primary care studies,53 only two-thirds of the participating practices returned screening forms. The reasons for the low participation rate may include lack of interest in mental health or self-care, lack of interest in research, or lack of infrastructure to implement the screening.54 In future research on self-care, different strategies may be needed to recruit patients, such as better preparation of FPs before the study (e.g. by providing educational materials, and lectures on self-care as part of rounds), allowing FPs to refer patients directly to the study, direct mailing of self-screening forms to patients with chronic diseases, or placing research staff in FP offices to screen patients.
Patients
Recruitment of patients was generally feasible. The main barrier that we encountered in our telephone-based recruitment process was in obtaining written informed consent. In future, we recommend an initial face-to-face meeting with the patient to explain the study, request their informed consent and deliver the self-care tools. It was also feasible to complete most of the planned coaching telephone calls; an average of 10.5 calls per patient (out of a possible maximum of 15) were completed.
Acceptability of the intervention
Our findings on the use and perception of depression self-care tools are particularly rich, as patients were provided with a range of depression self-care tools, including those with informational and behavioural content, delivered using a range of educational technologies (paper-based, Internet and audio-visual). Overall, we found that all of the tools except the Internet programmes were perceived to be helpful by around 50% of the study participants; only 7% found the Internet tools to be acceptable. Almost all of the participants reported that the coaching was helpful.
Older participants were less likely to report that the Antidepressant Skills Workbook was helpful, but more likely to find the Mood Monitoring Notebook helpful. The Antidepressant Skills Workbook was the longest of the behavioural tools, requiring the most reading. The Mood Monitoring Notebook, in contrast, was relatively simple to complete. These findings should be interpreted cautiously because of the small sample size and the unexpected finding that older patients were no more ill and used (non-significantly) fewer health services than middle-aged patients. This suggests that older patients who were more ill and using more health services may have been less likely to participate in the study. Nevertheless, further research is needed on the differences between older and middle-aged patients in their self-care needs and preferences, and on how to engage more ill older adults in depression self-care interventions.55
Despite some concerns raised by health professional focus group members early in the study,56 our results also suggest that older adults and more severely depressed patients (including those with major depression and/or currently receiving antidepressant medication) can also benefit from this approach. The intervention did not appear to have any negative effects; the small number of cases of worsening depression improved quickly. Therefore we conclude that the intervention is safe as an adjunct to usual care, even among older or more severely depressed patients, if it is accompanied by frequent monitoring of patients as in our study.
Further development of depression self-care interventions will require the adaptation of tools and approaches to meet the needs of different populations. From patients' comments it appeared that individuals who did not use the behavioural tools preferred other means of receiving help. For example, some suggested that they were ‘not the writing type.’ Adding other tools (e.g. relaxation video, audio recordings) may provide these individuals with alternative means of participating in self-care.
Among the intervention components that we examined, only use of the behavioural tools was associated with a decline in depressive symptoms; neither use of informational tools nor number of coach contacts were associated with the depression outcome. In future, the number of coach calls might be tailored to individuals' preferences. These results suggest that efforts should be made to increase adherence to the behavioural tools.
Clinical outcomes
Although the primary focus of this study was on the feasibility and acceptability of the intervention, we found promising results in terms of the clinical outcomes. Among those with clinically significant symptoms, the overall effect size (regardless of adherence) is similar to those reported for other low-intensity psychological interventions,57–59 and for another telephone-supported self-care intervention for depression.60 Stronger effects might be expected from an intervention that encourages use of the behavioural tools.
Patients with higher initial PHQ-9 scores improved more than those with lower initial scores. Importantly, the improvement in PHQ-9 score was not affected by age, gender or physical health status. However, an increased level of cognitive impairment predicted a small increase in severity of depression over time. Self-care interventions may need to be adapted to the needs of patients with mild cognitive impairment.
Other depression-related measures were also found to have changed significantly at the 6-month follow-up (the SF-12 mental component summary score and use of antidepressant medications). Our findings with regard to the relationship between treatment for depression and change in PHQ-9 score (see Table 5) suggest that both continued antidepressant medication use and initiation of psychological/counselling therapy during the study were associated with worsening of depressive symptoms.
Although the majority of the participants reported that they had made changes in health behaviours (particularly eating a healthier diet, taking exercise and making time for rewarding activities) at the 6-month follow-up, these changes were not reflected in the pre–post behaviour change measures, perhaps due to lack of responsiveness of the behaviour measures, issues of social desirability, or a response shift bias.61 The level of patient activation also did not change over time, which is similar to previous research findings.62
Limitations of the study
Limitations of this study include potential selection bias in FP and patient participation, the use of self-reported outcomes that are subject to recall and social desirability biases, a possible non-specific ‘attention’ effect of the coach,63 and failure to use a period of ‘watchful waiting’, which may explain in part the improvement in depression outcomes.13,64 The better clinical outcomes found among patients who selected and adhered to the behavioural tools may be confounded by greater motivation or other unmeasured characteristics. The differences by age and depression severity should be interpreted with caution, as the sample was small and underpowered to detect clinically significant differences. Finally, because this study did not randomise the participants, and staff were not blinded to treatment allocation or to the use of specific self-care tools, the results should not be interpreted as evidence of effectiveness.
Conclusions
In an open uncontrolled trial, we found that a telephone-supported self-care intervention for depression was feasible and acceptable to patients with chronic physical illnesses, and possibly associated with improvements in clinical outcomes. Importantly, these findings were generally similar across age groups and among those with more severe depressive symptoms. A randomised trial to determine the effectiveness of the intervention is warranted.
FUNDING
This study was funded by a research grant from the Quebec Health Research Fund.
ETHICAL APPROVAL
The study protocol and consent procedures were approved by the St Mary's Hospital Research Ethics Committee.
CONFLICTS OF INTEREST
None.
Contributor Information
Jane McCusker, Department of Epidemiology, Biostatistics and Occupational Health, McGill University; St Mary's Research Centre, Montreal, Canada.
Martin Cole, Department of Psychiatry, McGill University; Psychiatry, St Mary's Hospital Centre, Montreal, Canada.
Mark Yaffe, Department of Family Medicine, McGill University; Family Medicine Centre, St Mary's Hospital Centre, Montreal, Canada.
Tamara Sussman, School of Social Work, McGill University, Montreal, Canada.
Kim L Lavoie, Montreal Behavioural Medicine Centre; Department of Psychology, University of Quebec at Montreal; Division of Chest Medicine, Research Center, Hôpital du Sacré-Cœur de Montréal; Research Centre, Montreal Heart Institute; Department of Psychology, Université du Québec à Montréal, Canada.
Erin Strumpf, Department of Epidemiology, Biostatistics and Occupational Health, McGill University; Department of Economics, McGill University, Montreal, Canada.
Maida Sewitch, Department of Medicine, McGill University; Divisions of Gastroenterology and Clinical Epidemiology, McGill University Health Centre; Royal Victoria Hospital, Montreal, Canada.
Deniz Sahin, Department of Family Medicine, McGill University; St Mary's Research Centre, Montreal, Quebec, Canada.
Manon de Raad, St Mary's Research Centre, Montreal, Quebec, Canada.
REFERENCES
- 1.Judd LL, Akiskal HS, Maser JD, et al. A prospective 12-year study of subsyndromal and syndromal depressive symptoms in unipolar major depressive disorders. Archives of General Psychiatry 1998;55:694–700 [DOI] [PubMed] [Google Scholar]
- 2.Patten SB. An analysis of data from two general health surveys found that increased incidence and duration contributed to elevated prevalence of major depression in persons with chronic medical conditions. Journal of Clinical Epidemiology 2005;58:184–9 [DOI] [PubMed] [Google Scholar]
- 3.Wells KB, Burman AM. Caring for depression in America: lessons learned from early findings of the Medical Outcomes Study. Psychiatric Medicine 1991;9:503–19 [PubMed] [Google Scholar]
- 4.Saz P, Dewey ME. Depression, depressive symptoms and mortality in persons aged 65 and over living in the community: a systematic review of the literature. International Journal of Geriatric Psychiatry 2001;16:622–30 [DOI] [PubMed] [Google Scholar]
- 5.Schulz R, Drayer RA, Rollman BL. Depression as a risk factor for non-suicide mortality in the elderly. Society of Biological Psychiatry 2002;52:205–25 [DOI] [PubMed] [Google Scholar]
- 6.Stein MB, Cox BJ, Afifi TO, et al. Does co-morbid depressive illness magnify the impact of chronic physical illness? A population-based perspective. Psychological Medicine 2006;36:587–96 [DOI] [PubMed] [Google Scholar]
- 7.Stuck AE, Walthert JM, Nikolaus T, et al. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Social Science and Medicine 1999;48:445–69 [DOI] [PubMed] [Google Scholar]
- 8.Schmitz N, Wang J, Malla A, et al. Joint effect of depression and chronic conditions on disability: results from a population-based study. Psychosomatic Medicine 2007;69:332–8 [DOI] [PubMed] [Google Scholar]
- 9.Tinetti ME, McAvay GJ, Chang SS, et al. Contribution of multiple chronic conditions to universal health outcomes. Journal of the American Geriatrics Society 2011;59:1686–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Himelhoch S, Weller WE, Wu AW, et al. Chronic medical illness, depression, and use of acute medical services among medicare beneficiaries. Medical Care 2004;42:512–21 [DOI] [PubMed] [Google Scholar]
- 11.Unützer J, Patrick DL, Simon G, et al. Depressive symptoms and the cost of health services in HMO patients aged 65 years and older: a 4-year prospective study. Journal of the American Medical Association 1997;277:1618–23 [DOI] [PubMed] [Google Scholar]
- 12.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effect of anxiety and depression on patient adherence. Archives of Internal Medicine 2000;160:2101–7 [DOI] [PubMed] [Google Scholar]
- 13.National Collaborating Centre for Mental Health Depression in Adults with a Chronic Physical Health Problem: Treatment and Management. NICE Clinical Guideline 91 National Institute for Health and Clinical Excellence: London, 2009 [Google Scholar]
- 14.Payne KA, Myhr G. Increasing access to cognitive-behavioural therapy (CBT) for the treatment of mental illness in Canada: a research framework and call for action. Healthcare Policy 2010;5:e173–85 [PMC free article] [PubMed] [Google Scholar]
- 15.Morgan AJ, Jorm AF. Self-help interventions for depressive disorders and depressive symptoms: a systematic review. Annals of General Psychiatry 2008;7:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hetrick SE, Parker AG, Hickie IB, et al. Early identification and intervention in depressive disorders: towards a clinical staging model. Psychotherapy and Psychosomatics 2008;77:263–70 [DOI] [PubMed] [Google Scholar]
- 17.de Silva D. Evidence: Helping People Help Themselves. The Evidence Centre: London, 2011 [Google Scholar]
- 18.Bodenheimer T, Lorig K, Holman H, et al. Patient self-management of chronic disease in primary care. Journal of the American Medical Association 2002;288:2469–75 [DOI] [PubMed] [Google Scholar]
- 19.Gellatly J, Bower P, Hennessy S, et al. What makes self-help interventions effective in the management of depressive symptoms? Meta-analysis and meta-regression. Psychological Medicine 2007;37:1217–28 [DOI] [PubMed] [Google Scholar]
- 20.Maher J-P., (director) Finding a Way Out of Depression (video recording) Sogestalt: 2001 [Google Scholar]
- 21.Christensen H, Griffiths K. E-Couch: a Self-Help Interactive Program for Depression. Centre for Mental Health Research, Australian National University: Canberra, Australia, 2010. Available from: http://ecouch.anu.edu.au/welcome [Google Scholar]
- 22.Briffault X, Caria A, Finkelstein C, et al. La Dépression: en Savoir plus pour en Sortir [Depression: Knowledge is a Way Out]. Institut National de Prévention et d'Education à la Santé: Saint-Denis Cedex, Paris, 2010. Available from: www.infodepression.fr [Google Scholar]
- 23.Bilsker D, Paterson R. Antidepressant Skills Workbook (2e) Centre for Applied Research in Mental Health and Addiction: Vancouver, Canada, 2010. www.comh.ca/antidepressant-skills/adult/resources/index-asw.cfm [Google Scholar]
- 24.Bilsker D, Anderson J, Samra J, et al. Behavioural interventions in primary care: an implementation trial. Canadian Journal of Community Mental Health 2008;27:179–89 [Google Scholar]
- 25.Beck AT. Cognitive Therapy of Depression. The Guilford Press: New York, 1979 [Google Scholar]
- 26.Totten J. Families for Depression Awareness: www.familyaware.org
- 27.Lowe B, Kroenke K, Herzog W, et al. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). Journal of Affective Disorders 2004;81:61–6 [DOI] [PubMed] [Google Scholar]
- 28.Lowe B, Unutzer J, Callahan CM, et al. Monitoring depression treatment outcomes with the Patient Health Questionnaire-9. Medical Care 2004;42:1194–201 [DOI] [PubMed] [Google Scholar]
- 29.Katzman R, Brown T, Fuld P, et al. Validation of a short Orientation-Memory-Concentration test of cognitive impairment. American Journal of Psychiatry 1983;140:734–9 [DOI] [PubMed] [Google Scholar]
- 30.Davous P, Lamour Y, Debrand E, et al. A comparative evaluation of the short orientation memory concentration test of cognitive impairment. Journal of Neurology, Neurosurgery, and Psychiatry 1987;50:1312–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arroll B, Khin N, Kerse N. Screening for depression in primary care with two verbally asked questions: cross sectional study. British Medical Journal 2003;327:1144–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Whooley MA, Avins AL, Miranda J, et al. Case-finding instruments for depression: two questions are as good as many. Journal of General Internal Medicine 1997;12:439–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ware JE, Kosinski M, Keller SD. A 12-item short form health survey: construction of scales and preliminary tests of reliability and validity. Medical Care 1996;34:220–33 [DOI] [PubMed] [Google Scholar]
- 34.Hibbard JH, Stockard J, Mahoney ER, et al. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Services Research 2004;39:1005–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hibbard JH, Mahoney ER, Stockard J, et al. Development and testing of a short form of the Patient Activation Measure. Health Services Research 2005;40:1918–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Menec V. The relation between everyday activities and successful aging: a 6-year longitudinal study. Journals of Gerontology Series B, Psychological Sciences and Social Sciences 2003;58:S74–82 [DOI] [PubMed] [Google Scholar]
- 37.Glass TA, De Leon CFM, Bassuk SS, et al. Social engagement and depressive symptoms in late life: longitudinal findings. Journal of Aging and Health 2006;18:604–28 [DOI] [PubMed] [Google Scholar]
- 38.Scarmeas N, Levy G, Tang MX, et al. Influence of leisure activity on the incidence of Alzheimer's disease. Journal of Neurology 2001;57:2236–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aartsen MJ, Smits CHM, van Tilburg T, et al. Activity in older adults: cause or consequence of cognitive functioning? A longitudinal study on everyday activities and cognitive performance in older adults. Journals of Gerontology Series B, Psychological Sciences and Social Sciences 2002;57:153–62 [DOI] [PubMed] [Google Scholar]
- 40.Berkman L, Breslow L, Wingard D. Health practices and mortality risk. Berkman L, Breslow L. Health and Ways of Living: The Alemeda County Study. Academic Press: New York, 1983 [Google Scholar]
- 41.Morisky D, Green L, Levine D. Concurrent and predictive validity of a self-reported measure of medication adherence. Medical Care 1986;24:67–74 [DOI] [PubMed] [Google Scholar]
- 42.Godin G, Shepard RJ. Godin Leisure-Time Exercise Questionnaire. Medicine and Science in Sports and Exercise 1997;29:36–8 [Google Scholar]
- 43.Sabourin S, Pérusse D, Gendreau P. Les qualités psychométriques de la version canadienne-française du questionnaire de satisfaction du consommateur de services psychothérapeutiques (QSC-8 et QSC-18B) [The Canadian-French version of the Client Satisfaction Questionnaire]. Canadian Journal of Behavioral Sciences 1989;21:147–59 [Google Scholar]
- 44.Attkisson CC. Client Satisfaction Questionnaire (CSQ-8) Corcoran K, Fischer J. Measures for Clinical Practice: A Sourcebook (3e) Free Press: New York, 1987 [Google Scholar]
- 45.Health Statistics Division, Statistics Canada, Data Liberation Initiative (Canada), McGill University, Electronic Data Resources Service et al. Canadian Community Health Survey – Cycle 1.2. Mental Health and Well-Being (2002). Health Statistics Division, Statistics Canada, Ottawa, distributed through Sherlock, Cooperative Data Access System for Quebec University Libraries; 2003. http://sherlock.crepuq.qc.ca/cgi-bin/sherlock.pl?langue=E;action=LAE;region=Canada;region=Autres [Google Scholar]
- 46.Health Statistics Division, Statistics Canada, Data Liberation Initiative (Canada), McGill University, Electronic Data Resources Service et al. Canadian Community Health Survey – Cycle 2.1– 2003. Health Statistics Division, Statistics Canada, Ottawa, distributed through Sherlock, Cooperative Data Access System for Quebec University Libraries; 2004. http://sherlock.crepuq.qc.ca/cgi-bin/sherlock.pl?langue=E;action=LAE;region=Canada;region=Autres [Google Scholar]
- 47.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. Journal of the American Medical Association 1999;282:1737–44 [DOI] [PubMed] [Google Scholar]
- 48.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. Journal of the American Medical Association 1994;272:1749–56 [PubMed] [Google Scholar]
- 49.Cohen J. Statistical Power Analysis for the Behavioral Sciences (2e) Lawrence Erlbaum Associates: Hillsdale, NJ, 1988 [Google Scholar]
- 50.Johnston G, Strokes M. Application of GEE Methodology Using the SAS System. SAS Institute Inc.: Cary, NY, 1997 [Google Scholar]
- 51.Neter J, Wasserman W, Kutner MH. Applied Linear Statistical Models. Irwin: Homewood, IL, 1985 [Google Scholar]
- 52.Raftery AE. Bayesian model selection in social research. Marsden P. Sociological Methodology. Blackwells: Cambridge, MA, 1995. pp. 111–96 [Google Scholar]
- 53.Johnston S, Liddy C, Hogg W, et al. Barriers and facilitators to recruitment of physicians and practices for primary care health services research at one centre. BMC Medical Research Methodology 2010;10:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yaffe M, McCusker J, Strumpf E. How do family physicians view the use of self-care tools by depressed adults? 12th Canadian Collaborative Mental Health Care Conference, 23–25 June 2011, Halifax, Nova Scotia [Google Scholar]
- 55.Robinson P, Katon W, Von Korff M, et al. The education of depressed primary care patients: what do patients think of interactive booklets and a video? Journal of Family Practice 1997;44:562–71 [PubMed] [Google Scholar]
- 56.Sussman T. Health professionals' views on self-care as a strategy for managing late-life depression. Annual Meeting of the Canadian Association of Gerontology, 1 December 2010, Montreal, Quebec [Google Scholar]
- 57.Richards DA, Borglin G. Implementation of psychological therapies for anxiety and depression in routine practice: two-year prospective cohort study. Journal of Affective Disorders 2011;133:51–60 [DOI] [PubMed] [Google Scholar]
- 58.Ekers D, Wilson R. Depression case management by practice nurses in primary care: an audit. Mental Health in Family Medicine 2008;5:111–19 [PMC free article] [PubMed] [Google Scholar]
- 59.Clark DM, Layard R, Smithies R, et al. Improving access to psychological therapy: initial evaluation of two UK demonstration sites. Behaviour Research and Therapy 2009;47:910–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Canadian Mental Health Association, British Columbia Division Bounce Back: Reclaim Your Health. Balma Creative: British Columbia, 2009. www.cmha.bc.ca/bounceback [Google Scholar]
- 61.Streiner DL, Norman GR. Health Measurement Scales: A Practical Guide to Their Development and Use (3e) Oxford University Press: New York, 2003 [Google Scholar]
- 62.Hibbard JH, Mahoney ER, Stock R, et al. Do increases in patient activation result in improved self-management behaviors? Health Services Research 2007;42:1443–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.McCusker J, Cole M, Keller E, et al. Effectiveness of treatments of depression in older ambulatory patients. Archives of Internal Medicine 1998;158:705–12 [DOI] [PubMed] [Google Scholar]
- 64.Dwight Johnson M, Meredith LS, Hickey SC, et al. Influence of patient preference and primary care clinician proclivity for watchful waiting on receipt of depression treatment. General Hospital Psychiatry 2006;28:379–86 [DOI] [PubMed] [Google Scholar]