Abstract
The step-up activity (stair-ascending) is an important daily function of the knee. This study aimed to investigate the articular cartilage contact kinematics on both tibial and femoral cartilage surfaces and describe the femoral condylar motion using the transepicondylar axis (TEA) and the geometric center axis (GCA) during a step-up activity. Twenty-one healthy subjects were included and their knee joint models were reconstructed using MR images. A single-stair step-up activity was imaged using a dual-fluoroscopic imaging system. Three-dimensional knee joint contact points were determined and projected onto the tibial plateau and femoral condyle surfaces. The contact points on the medial and lateral tibial plateau moved anteriorly (by 13.5 ± 3.2 and 10.7 ± 5.0 mm, respectively, p>0.05) with knee extension. The contact points on the medial and lateral femoral condyle moved from the posterior to the anterior portion (by 32.2 ± 4.9 mm and 25.5 ± 4.2 mm, respectively, p<0.05) and were located on the inner half of the femoral cartilage throughout the activity. The data on articular contact kinematics and the femoral condylar motion described using the TEA and GCA indicated that the medial and lateral compartments had similar motion patterns during the step-up activity. The knee does not demonstrate a medial-pivoting motion character during the step-up activity. The data may provide insight to contemporary TKA development.
Keywords: cartilage contact, condylar motion, in vivo knee kinematics, step-up activity
Introduction
Step–up (stair ascending) is one of the most important daily activities, and has been adopted as a closed-kinetic chain exercise in various lower extremity rehabilitation protocols.1, 2 During a step-up activity, a large knee joint moment could be generated together with a quadriceps-hamstring co-contraction to help stabilize the knee joint.3, 4 Therefore, a thorough understanding of the biomechanics of the knee during step-up activity is important for optimizing the rehabilitation protocol to enhance its efficacy in treatment of different pathologies of the knee such as osteoarthritis (OA), ACL reconstruction and total knee arthroplasty (TKA) 3, 5.
Few studies have quantitatively reported on the knee joint kinematics during the step-up motion.6–8 For example, Gao et al.9 used motion analysis method to measure the kinematics of ACL deficient and ACL reconstructed knees. Kozanek et al.7 compared the knee kinematics during the step-up exercise between ACL deficient and intact contralateral knees using a combined dual-fluoroscopic imaging system (DFIS) and MRI-based model. In a recent study by Moro-oka et al.10, the articular contact patterns of the knee were approximated using the distance mapping between the tibiofemoral articular cartilage surfaces. While these studies have greatly improved our knowledge on knee kinematics during the step-up activities, the different experimental designs and coordinate system selections made it difficult to obtain a systematic understanding of the knee joint kinematics behavior during the step-up activity.
Therefore, the purpose of this study was to measure the kinematic features of the tibiofemoral joint during the step-up activity using the combined DFIS and MRI technique. Specifically, we measured the tibiofemoral articular cartilage contact point locations during a dynamic step-up motion. Furthermore, we measured the femoral condylar motions using two well-known flexion axes, i.e., the transepicondylar axis (TEA) and the geometry center axis (GCA), and calculated the axial tibial rotation based on these two flexion axes.11
Methods
Twenty-one healthy knees without any history of surgery from 21 subjects were recruited in this study (age, 34.6 ± 10.4 years; gender, 14 males and 7 females; body height, 1.8 ± 0.1 m; body weight, 80.9 ± 18.1 kg) with informed consent. The testing protocol was approved by our institutional review board. A 3-Tesla magnetic resonance machine (MAGNETOM Trio, Siemens, Malvern, PA) was used to scan the knee joint in the sagittal plane with a double-echo water excitation sequence (thickness: 1mm, resolution: 512x512 pixels). The images were reviewed by an orthopaedic surgeon to ensure the intact structures of the knee joint and surrounding tissues. Three-dimensional (3D) models of the knee, including the femur, tibia, and their cartilage surfaces, were reconstructed using an established protocol with the MR images.12
Each subject then performed a dynamic step-up and the knee motion was captured by a validated dual-fluoroscopic imaging system at 30 Hz and with a 8 ms pulse-width.13, 14 The beginning (0%) of the step-up activity was defined as the initiation of the knee extension motion and the end point (100%) was defined when the subject’s knee fully extended (Fig. 1A). Fluoroscopic images at every 10% of the activity were selected and were imported into a virtual dual-fluoroscopic environment constructed in a solid modeling software (Rhinoceros, Seattle, WA).12 The 3D bony models were imported and manipulated until their projections matched the silhouettes of the corresponding bones on the fluoroscopic images.12 The cartilage models of the femur and tibia were mapped to the corresponding bone models at each knee position. The cartilage contact at a given knee position is represented by overlapping of the tibial and femoral cartilage surfaces. The centroid of the overlapping area was defined as the cartilage contact point.15
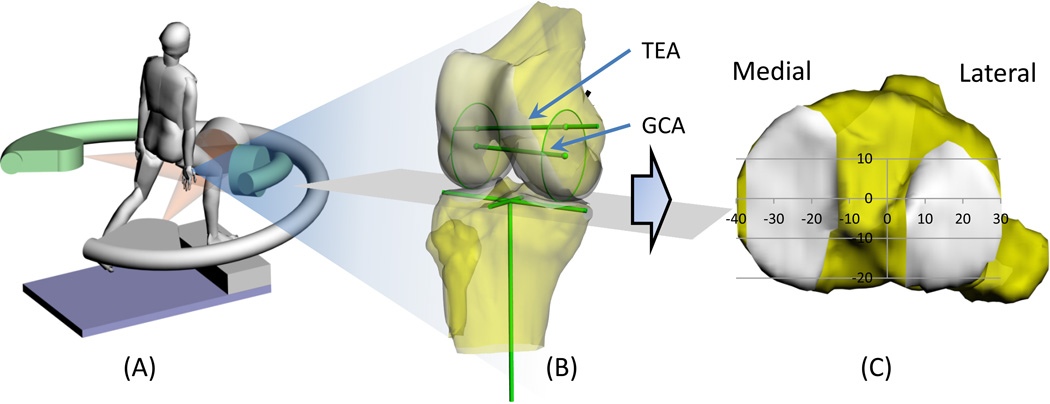
Figure 1.
Schematic drawing showing (A) the step-up activity captured using a dual-fluoroscopic imaging system; (B) coordinate systems of the knee; and (C) coordinate system on tibial plateau: mediolateral axis was defined by connecting the centers of the medial and lateral compartments; anteroposterior axis was perpendicular to the mediolateral axis.
To quantitatively describe the knee joint contact points, a coordinate system on the tibial plateau was established (Fig. 1B). The tibial long axis was parallel to the posterior wall of the tibial shaft. The medial-lateral axis was defined as a line connecting the centroids of the two circles fit to the medial and lateral tibial plateau surfaces.16 The anterior-posterior axis was perpendicular to the other two axes. The femoral long axis was defined along the femoral shaft. The knee flexion was measured between the long axes of the tibia and femur in the sagittal plane.
To quantify the cartilage contact on the femoral condyles, we measured the femoral contact angle in the sagittal plane and deviation angle in a plane perpendicular to the sagittal plane (Fig. 3).15 The contact line was defined as a line connecting the contact point to the corresponding centroid of the condyle. The femoral contact angle was defined as the angle between contact line and the femoral long axis (Fig. 3A). The deviation angle was measured along a plane perpendicular to the sagittal plane and the contact line (Fig. 3B).
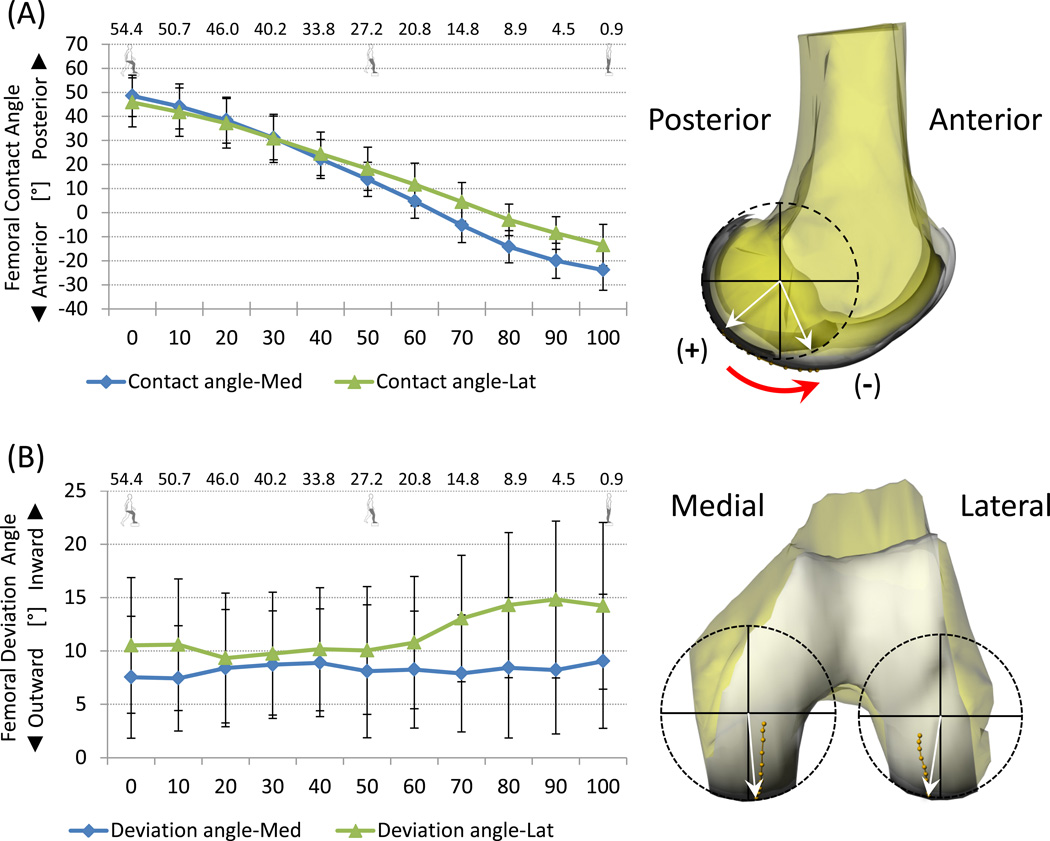
Figure 3.
Femoral contact angle (A) and deviation angle (B) during step-up activity.
To describe the condylar motions, both transepicondylar axis (TEA) and geometric center axis (GCA) were selected. The TEA was defined as a line connecting both medial and lateral epicondyles of the femur and the GCA was defined as a line connecting the centroids of two circles fit to the posterior portions of the medial and lateral condyles in the sagittal plane (Fig. 1B).11 Two reference points of each axis were selected to represent the centers of the medial and lateral condyles. Those reference points were projected on the tibial plateau surface to determine the condylar motions, similarly to the aforementioned cartilage contact motion (Fig. 1B).17 The rotation of the projections of the axes on the tibial plateau was used to determine the axial rotation of the femur during extension of the knee.11, 17
A one-way analysis of variance (ANOVA) was used to analyze the kinematic characteristics of the tibiofemoral joint during the step-up activity. The anteroposterior translation of articular cartilage contact points, femoral cartilage contact angle and deviation angle, and femoral condylar motion were considered as dependent variables. Condylar side (medial/ lateral) was defined as the independent variable to determine the differences at medial and lateral compartments. Turkey post-hoc analysis was used when a significance was found. A statistically significant difference was determined when p < 0.05.
Results
The flexion angles ranged from 54.4 ± 7.1° at initial contact to full extension at the end of the step-up activity. The average time for the activity was 0.8 ± 0.2 seconds.
Contact points on tibial plateau
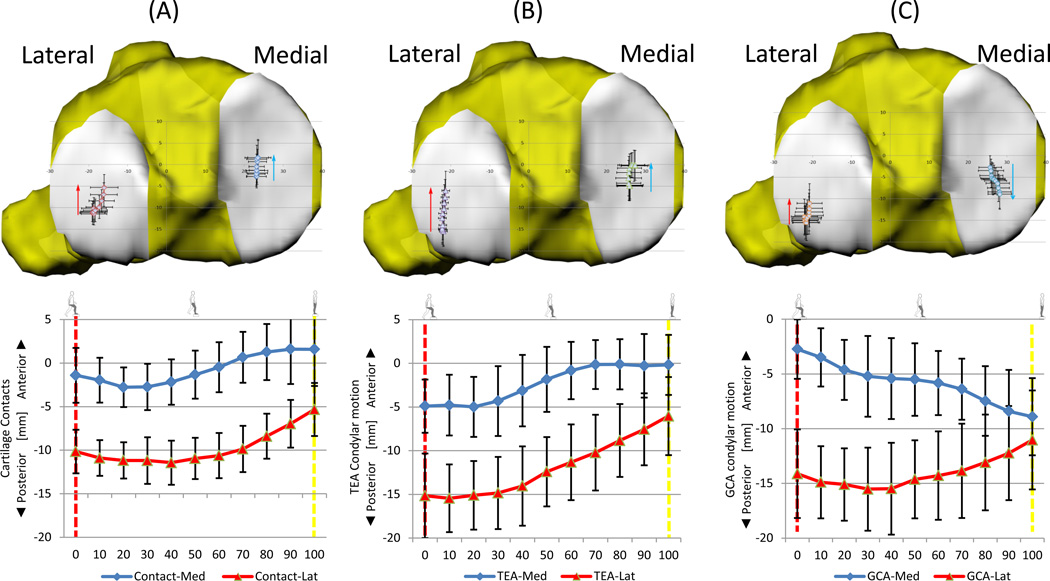
The contact points started at −1.4 ± 3.1 mm and −10.1 ± 2.5 mm to the center of the medial and lateral tibial plateaus, respectively (Fig. 2A). Both medial and lateral contact points slightly shifted posteriorly from initiation of movement until 30% of the step-up, and then gradually shifted anteriorly until 80% of the step-up motion. Thereafter, the medial contact points moved slightly anteriorly to 1.6 ± 4.2 mm, whereas the lateral contact points continued to shift anteriorly to −5.3 ± 3.0 mm at 100% of the step-up activity (Fig. 2A). In addition, the total excursions of the medial and lateral contacts were 13.5 ± 3.2 mm and 10.7 ± 5.0 mm, respectively. No significant difference was found in total excursion between the medial and lateral compartments.
Figure 2.
Anteroposterior translation of contact points and condylar motions during step-up activity. (A) articular cartilage contact points; (B) TEA condylar motion; (C) GCA condylar motion.
In the medial-lateral direction, the translation of the medial contact points during the stepup was within 0.4 mm. The lateral contact point started from −18.7 ± 3.1 mm and then slightly moved medially from −19.0 ± 2.8 mm to −16.0 ± 3.6 mm between 30 and 100% of the activity.
Contact points on femoral condyles
The sagittal contact angles at the beginning of the step-up activity were 48.6 ± 10.2° and 45.9 ± 8.6° on the medial and lateral femoral condyles, respectively (Fig. 3A). Both contact angles consecutively changed to 13.8 ± 9.0° and 18.3 ± 7.3° at the 50% of the activity. At the end of step-up activity, the contact angles rested at −24.3 ± 8.6° and −13.6 ± 8.6° on the medial and lateral femoral condyles, respectively. The range of contact angles were 73.0 ± 12.0° and 59.4 ± 9.4° for the medial and lateral femoral condyles, respectively, with the medial side significantly higher than the lateral side (p<0.05).
The deviation angle of the medial condyle started at 8.2 ± 5.0° and the change during the step-up activity was within 1.4° (Fig. 3B). The deviation angle of the lateral condyle started from 10.7 ± 6.5°. The mean angle then changed within 1.3° at the first 50% of the activity. Thereafter, the deviation angle changed from 10.4 ± 5.9° to 14.7 ± 7.7°.
The total translational excursions of the contact points were 32.2 ± 4.9 mm on the medial condylar surface and 25.5 ± 4.2 mm on the lateral condylar surface. The total excursion of the medial contact points were significantly longer than that of the lateral contact points (p < 0.05).
Condylar motion measured using TEA and GCA
The condylar motion measured using the TEA gradually shifted anteriorly (medial: −5.0 ± 3.5 to −0.1 ± 2.8 mm; lateral: −15.1 ± 3.9 to −10.2 ± 4.3 mm) from beginning to 70% of the activity. The position of the medial condyle remained constant throughout the activity thereafter; however, the lateral condyle continued to move anteriorly to −6.0 ± 4.5 mm (Fig. 2B). The total excursions of the medial and lateral femoral condyles measured using the TEA were 12.7 ± 2.9 mm and 14.5 ± 4.0 mm, respectively, and no significant difference was found between the two excursions. The tibia rotated internally 13.3 ± 5.6° at the beginning and externally rotated to 8.3 ± 5.4° at the end of the step-up activity.
The condylar motions measured using the GCA showed an opposite trend between the medial and lateral condyles (Fig. 2C); that is, the medial condyle moved posteriorly from −5.5 to −8.9 mm while the lateral condyle shifted from −14.7 to −11.0 mm. The total excursions measured using GCA were 11.9 ± 4.1 mm and 11.8 ± 4.1 mm for the medial and lateral femoral condyles, respectively, with no significant difference between them. The axial tibial rotation was measured to be 14.3 ± 5.7° internal rotation at the beginning and was 3.9 ± 5.5° at the end of the step-up activity.
Discussion
This study investigated the in-vivo articular cartilage contact kinematics on both tibial plateau and femoral condyle surfaces during a functional step-up (stair ascending) activity. The femoral condylar motions were also measured using the TEA and GCA. In general, both medial and lateral contact points moved anteriorly on the tibial articular surfaces along the step-up motion path. The total excursion of the articular contact points was similar on the medial and lateral tibial surfaces. However, the total excursion on the medial femoral condyle was significantly larger than that on the lateral condyle. Using the TEA, the femoral condylar motions presented a similar pattern as the contact points throughout the activity; nevertheless, when the GCA was used, the femoral condyle motion pattern was dramatically different. The medial condyle moved anteriorly, while the lateral condyle shifted posteriorly throughout the activity.
In current knowledge of knee joint kinematics, the medial condyle was thought to be less mobile in translation compared to the lateral side during flexion/extension of the knee. This kinematics feature, so-called medial-pivoting, has been reported in many studies that investigated either non-weight-bearing flexion18, 19 or weight-bearing flexion20–22, 23 of the knee. For example, the relative movements between the medial and lateral condyles has been investigated using an open MRI and at different non-weight-bearing flexion angles of the knee, where the lateral condyle was found to move posteriorly but the medial condyle move little during unloaded knee flexion.18, 24, 25 Johal et al. 25 reported the knee contact points under quasi-static weight-bearing and non-weight-bearing conditions by an open MRI and found the medial contact points moved minimally and lateral contact points translated posteriorly with the knee flexion up to 120°. DeFrate et al.20 reported the total excursion of the tibiofemoral contact points during a quasi-static lunge of the knee and found that the translation of the medial contact point was smaller than that of the lateral side. The minimal medial femoral condyle motion during flexion was also reported using sagittal plane fluoroscopy.26 The observation on lager lateral femoral condyle motions than medial side resulted in a tibial internal rotation with flexion around an axis located at the medial side of the knee that led to the concept of medial-pivoting of the knee during flexion.18, 24, 25
However, there are other studies that did not find medial-pivoting, but found that the medial condyle moves similarly to the lateral side or with a greater excursion than the lateral condyle.17, 27, 28 For example, Hoshino et al.27 investigated the contact path derived using bone-to-bone distance approximation using 3D CT bony models during the early stance of running and found no significant difference between the medial and lateral plateau in terms of tibial contact path, but significantly larger excursion was observed on the medial femoral condyle. Wretenberg et al.19 investigated the tibiofemoral contact points in vivo using a closed MRI to directly measure the tibiofemoral contact points from sixteen subjects. The knee joint was placed in different flexion angles by a customized orthosis without physiological loading. The contact points of the medial and lateral condyles moved posteriorly in the first 30° of flexion, and then slightly moved anteriorly between 30 to 60° of flexion. Both Koo et al.28 and Kozanek et al.17 found that the knee actually had a lateral-pivoting tendency during stance phases of gait.
In a recent study of step-up activity, Moro-Oka et al 10. used a dynamic sagittal X-ray and approximated the tibiofemoral joint contact kinematics by distance mapping and found that both medial and lateral condyles slid anteriorly during the step-up activity on the tibial plateau. This is similar to our observations in this study that the medial and lateral femoral condylar motion, measured using either contact point locations or TEA axis, slid anteriorly during the dynamic step-up activity. The total excursion of the contact points was similar on the medial and lateral plateau surfaces but was significantly larger on the medial femoral condyle surface than that on the lateral side of the knee. The knee joint kinematics during step-up activity did not show the phenomenon of medial-pivoting knee flexion as observed during passive, non-weight-bearing flexion or quasi-static knee joint flexion.18, 20, 24, 25 This data revealed that the knee joint flexion is loading-dependent and it is insufficient to describe the knee joint flexion using one characteristic pattern, such as medial-pivoting, which was not concluded from data reflecting functional daily activities.
It is interesting to note that the tibial contact points or the condylar motions represented using the TEA or GCA were located at the center portion of the medial tibial compartment in anterior-posterior direction, but at the posterior portion of the lateral tibial compartment. On the femoral condyle, the contact points were all located in the half towards the intercondylar notch in medial-lateral direction. Similar observations were reported by Li et al. in a single-legged lunge activity.15 Our data also indicated that the condylar motion could be different if a different flexion axis was selected. The medial condyle moved in opposite directions when using the TEA compared to the GCA to measure the knee joint motion. In addition, greater axial tibial rotation was measured using the GCA than that using the TEA. Similar observations were also reported by Most et al.11
This data might have implications for contemporary total knee replacement designs that are aimed to simulate more physiological articulations of the native knees. The kinematics feature of medial-pivoting has been implemented into several contemporary TKA designs.29, 30 However, clinical and biomechanical studies have not shown the superiority of these contemporary designs over the conventional TKA designs.10, 17, 28 As a matter of fact, the medial-pivoting was not observed in daily activities such as gait17, 28, stair ascending10 and this study. Medial-pivoting might over constrain the knee at low flexion angles such as experienced during gait or stair ascending activities. Therefore, it is still a challenge to distinguish whether the medial-pivoting or lateral-pivoting should be implemented into a TKA design to reproduce the kinematics of a normal knee.
It should be pointed out that the articular contact kinematics of this study was only measured using cartilage-to-cartilage contact. Menisci are important structures in the knee joint function as well. However, due to the limitations of the technique, the motion of the menisci could not be detected using the fluoroscopic images. The cartilage-to-meniscus contact was not included in this study. Therefore, a complete description of articular contact kinematics, including meniscus function, is yet to be explored and implemented in new technology.
In conclusion, this study quantitatively described the motion characteristics of the knee joint during a step-up activity. The contact points were measured on both tibial and femoral cartilage surfaces. On tibial cartilage surface, the contact points gradually moved anteriorly during the step-up activity on both the medial and lateral compartments. On the femoral cartilage surface, the contact points of the medial and lateral condyle monotonically moved from the posterior portions to the anterior portions during the step-up activity. Furthermore, selection of knee coordinate systems results in different kinematics description of the knee. This data may be instrumental in the development of total knee arthroplasty that is aimed to reproduce native knee function.
The tibial contact points moved anteriorly during the step-up, similar to TEA, but not GCA
Medial-pivoting was not observed during step-up activity
Selection of coordinate systems changed knee joint kinematics description dramatically
Acknowledgements
The authors would like to gratefully acknowledge the financial support of the National Institute of Health (R01 AR055612) and the Department of Orthopaedic Surgery at Massachusetts General Hospital.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bynum EB, Barrack RL, Alexander AH. Open versus closed chain kinetic exercises after anterior cruciate ligament reconstruction. A prospective randomized study. Am J Sports Med. 1995;23(4):401–406. doi: 10.1177/036354659502300405. [DOI] [PubMed] [Google Scholar]
- 2.McQuade KJ, de Oliveira AS. Effects of progressive resistance strength training on knee biomechanics during single leg step-up in persons with mild knee osteoarthritis. Clin Biomech (Bristol, Avon) 2011;26(7):741–748. doi: 10.1016/j.clinbiomech.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garling EH, Wolterbeek N, Velzeboer S, Nelissen RG, Valstar ER, Doorenbosch CA, Harlaar J. Co-contraction in RA patients with a mobile bearing total knee prosthesis during a step-up task. Knee Surg Sports Traumatol Arthrosc. 2008;16(8):734–740. doi: 10.1007/s00167-008-0537-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaufman KR, Hughes C, Morrey BF, Morrey M, An KN. Gait characteristics of patients with knee osteoarthritis. J Biomech. 2001;34(7):907–915. doi: 10.1016/s0021-9290(01)00036-7. [DOI] [PubMed] [Google Scholar]
- 5.Wilk KE, Macrina LC, Cain EL, Dugas JR, Andrews JR. Recent advances in the rehabilitation of anterior cruciate ligament injuries. J Orthop Sports Phys Ther. 2012;42(3):153–171. doi: 10.2519/jospt.2012.3741. [DOI] [PubMed] [Google Scholar]
- 6.Andriacchi TP, Andersson GB, Fermier RW, Stern D, Galante JO. A study of lower-limb mechanics during stair-climbing. J Bone Joint Surg Am. 1980;62(5):749–757. [PubMed] [Google Scholar]
- 7.Kozanek M, Hosseini A, de Velde SK, Moussa ME, Li JS, Gill TJ, Li G. Kinematic evaluation of the step-up exercise in anterior cruciate ligament deficiency. Clin Biomech (Bristol, Avon) 2011;26(9):950–954. doi: 10.1016/j.clinbiomech.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riener R, Rabuffetti M, Frigo C. Stair ascent and descent at different inclinations. Gait Posture. 2002;15(1):32–44. doi: 10.1016/s0966-6362(01)00162-x. [DOI] [PubMed] [Google Scholar]
- 9.Gao B, Cordova ML, Zheng NN. Three-dimensional joint kinematics of ACL-deficient and ACL-reconstructed knees during stair ascent and descent. Hum Mov Sci. 2012;31(1):222–235. doi: 10.1016/j.humov.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 10.Moro-oka TA, Hamai S, Miura H, Shimoto T, Higaki H, Fregly BJ, Iwamoto Y, Banks SA. Dynamic activity dependence of in vivo normal knee kinematics. J Orthop Res. 2008;26(4):428–434. doi: 10.1002/jor.20488. [DOI] [PubMed] [Google Scholar]
- 11.Most E, Axe J, Rubash H, Li G. Sensitivity of the knee joint kinematics calculation to selection of flexion axes. J Biomech. 2004;37(11):1743–1748. doi: 10.1016/j.jbiomech.2004.01.025. [DOI] [PubMed] [Google Scholar]
- 12.Li G, Wuerz TH, DeFrate LE. Feasibility of using orthogonal fluoroscopic images to measure in vivo joint kinematics. J Biomech Eng. 2004;126(2):314–318. doi: 10.1115/1.1691448. [DOI] [PubMed] [Google Scholar]
- 13.Li G, Van de Velde SK, Bingham JT. Validation of a non-invasive fluoroscopic imaging technique for the measurement of dynamic knee joint motion. J Biomech. 2008;41(7):1616–1622. doi: 10.1016/j.jbiomech.2008.01.034. [DOI] [PubMed] [Google Scholar]
- 14.Tashman S. Comments on "validation of a non-invasive fluoroscopic imaging technique for the measurement of dynamic knee joint motion". J Biomech. 2008;41(15):3290–3291. doi: 10.1016/j.jbiomech.2008.07.038. author reply 3292–3293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li G, DeFrate LE, Park SE, Gill TJ, Rubash HE. In vivo articular cartilage contact kinematics of the knee: an investigation using dual-orthogonal fluoroscopy and magnetic resonance image-based computer models. Am J Sports Med. 2005;33(1):102–107. doi: 10.1177/0363546504265577. [DOI] [PubMed] [Google Scholar]
- 16.Chen CH, Li JS, Hosseini A, Gadikota HR, Gill TJ, Li G. Anteroposterior stability of the knee during the stance phase of gait after anterior cruciate ligament deficiency. Gait Posture. 2012;35(3):467–471. doi: 10.1016/j.gaitpost.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kozanek M, Hosseini A, Liu F, Van de Velde SK, Gill TJ, Rubash HE, Li G. Tibiofemoral kinematics and condylar motion during the stance phase of gait. J Biomech. 2009;42(12):1877–1884. doi: 10.1016/j.jbiomech.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br. 2000;82(8):1189–1195. doi: 10.1302/0301-620x.82b8.10717. [DOI] [PubMed] [Google Scholar]
- 19.Wretenberg P, Ramsey DK, Nemeth G. Tibiofemoral contact points relative to flexion angle measured with MRI. Clin Biomech (Bristol, Avon) 2002;17(6):477–485. doi: 10.1016/s0268-0033(02)00036-0. [DOI] [PubMed] [Google Scholar]
- 20.DeFrate LE, Sun H, Gill TJ, Rubash HE, Li G. In vivo tibiofemoral contact analysis using 3D MRI-based knee models. J Biomech. 2004;37(10):1499–1504. doi: 10.1016/j.jbiomech.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 21.Dennis DA, Mahfouz MR, Komistek RD, Hoff W. In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech. 2005;38(2):241–253. doi: 10.1016/j.jbiomech.2004.02.042. [DOI] [PubMed] [Google Scholar]
- 22.Li G, Moses JM, Papannagari R, Pathare NP, DeFrate LE, Gill TJ. Anterior cruciate ligament deficiency alters the in vivo motion of the tibiofemoral cartilage contact points in both the anteroposterior and mediolateral directions. J Bone Joint Surg Am. 2006;88(8):1826–1834. doi: 10.2106/JBJS.E.00539. [DOI] [PubMed] [Google Scholar]
- 23.Logan M, Dunstan E, Robinson J, Williams A, Gedroyc W, Freeman M. Tibiofemoral kinematics of the anterior cruciate ligament (ACL)-deficient weightbearing, living knee employing vertical access open "interventional" multiple resonance imaging. Am J Sports Med. 2004;32(3):720–726. doi: 10.1177/0095399703258771. [DOI] [PubMed] [Google Scholar]
- 24.Hill PF, Vedi V, Williams A, Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 2: the loaded and unloaded living knee studied by MRI. J Bone Joint Surg Br. 2000;82(8):1196–1198. doi: 10.1302/0301-620x.82b8.10716. [DOI] [PubMed] [Google Scholar]
- 25.Johal P, Williams A, Wragg P, Hunt D, Gedroyc W. Tibio-femoral movement in the living knee. A study of weight bearing and non-weight bearing knee kinematics using 'interventional' MRI. J Biomech. 2005;38(2):269–276. doi: 10.1016/j.jbiomech.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 26.Mu S, Moro-Oka T, Johal P, Hamai S, Freeman MA, Banks SA. Comparison of static and dynamic knee kinematics during squatting. Clin Biomech (Bristol, Avon) 2011;26(1):106–108. doi: 10.1016/j.clinbiomech.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 27.Hoshino Y, Tashman S. Internal tibial rotation during in vivo, dynamic activity induces greater sliding of tibio-femoral joint contact on the medial compartment. Knee Surg Sports Traumatol Arthrosc. 2012;20(7):1268–1275. doi: 10.1007/s00167-011-1731-6. [DOI] [PubMed] [Google Scholar]
- 28.Koo S, Andriacchi TP. The knee joint center of rotation is predominantly on the lateral side during normal walking. J Biomech. 2008;41(6):1269–1273. doi: 10.1016/j.jbiomech.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amiri S, Cooke TDV, Wyss UP. Conceptual design for condylar guiding features of a total knee replacement. J. Med. Devices. 2011;5:025001–025001. [Google Scholar]
- 30.Walker PS, Sussman-Fort JM, Yildirim G, Boyer J. Design features of total knees for achieving normal knee motion characteristics. J Arthroplasty. 2009;24(3):475–483. doi: 10.1016/j.arth.2007.11.002. [DOI] [PubMed] [Google Scholar]