Abstract
The test and retest opportunity afforded by reviewing a patient over time substantially increases the total gain in certainty when making a diagnosis in low-prevalence settings (the time-efficiency principle). This approach safely and efficiently reduces the number of patients who need to be formally tested in order to make a correct diagnosis for a person. Time, in terms of observed disease trajectory, provides a vital mechanism for achieving this task. It remains the best strategy for delivering near-optimal diagnoses in low-prevalence settings and should be used to its full advantage.
Keywords: Continuity of care, diagnostic tests, patient safety, primary care, quality of care.
Introduction
Advances in medical technology have expanded the range of diagnostic tests that can be offered to patients in primary care. Indeed, the usual solutions proposed for real or perceived delayed or missed diagnoses in primary care often involve greater access to imaging, increased near-patient testing or greater access to secondary care.1 If establishing a diagnosis is viewed merely as a technical task, it might be assumed that performing more imaging and laboratory tests would help solve this problem.2 However, when used indiscriminately, such diagnostic technology may paradoxically make the process of diagnosis more costly, invasive and time consuming compared with more traditional diagnostic approaches. We, therefore, argue that the test of time offers an effective tool that should continue to be valued in 21st-century medicine.
The continued active use of the test of time in consultations needs a firm scientific basis, as emphasized by the Royal College of General Practitioners in their 2012 Commission on Medical Generalism, which called for evidence-based tools that could enhance diagnostics in low-prevalence settings.3 We therefore describe the scientific basis for purposefully using time as a diagnostic strategy. Many tests have high levels of sensitivity and specificity, yet in primary care, they are often found to be poor at helping to diagnose diseases with low prevalence.4,5 What may be less widely appreciated is how the test of time, the strategy of testing and retesting a patient over time, can substantially increase the total gain in certainty that a patient has a particular disease. By stating this explicitly, as a principle, its status as a key diagnostic strategy in primary care can be researched, discussed and taught.
Diagnosis in low-prevalence settings
Diagnostic ‘tests’ can be considered to include symptoms elicited from the patient’s history and signs obtained by physical examination, in addition to laboratory tests and imaging. The low prevalence of many diseases in primary care means that even tests with an exceptionally high sensitivity and specificity have relatively high negative predictive values (NPVs) and low positive predictive values (PPVs).2 The high NPV of most tests helps clinicians working in low-prevalence settings, such as GPs, to correctly identify patients without disease. This is an important role because missing any major pathology can have disastrous consequences.2 Conversely, the low PPV of most tests, rather than any lack of knowledge or skill, means that GPs are less able to unequivocally diagnose disease.2 In clinical decision-making, when disease prevalence is low, although it could appear that we learn more from a negative test result than from a positive test, this is not the case; we gain little new information from a negative test result when we already know that that disease is highly unlikely.6–9
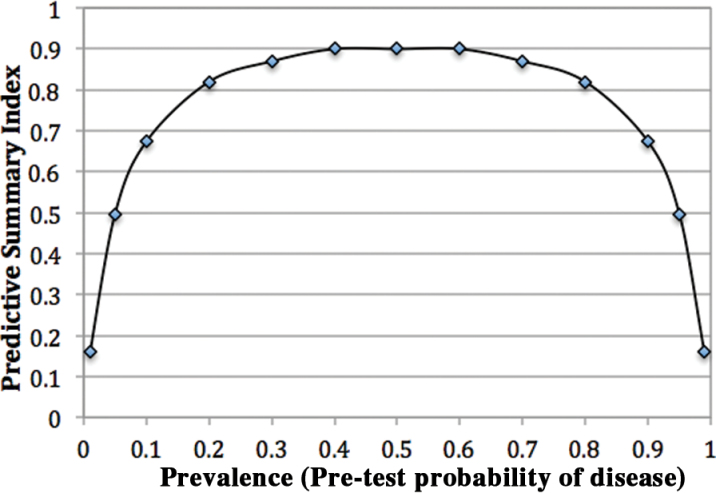
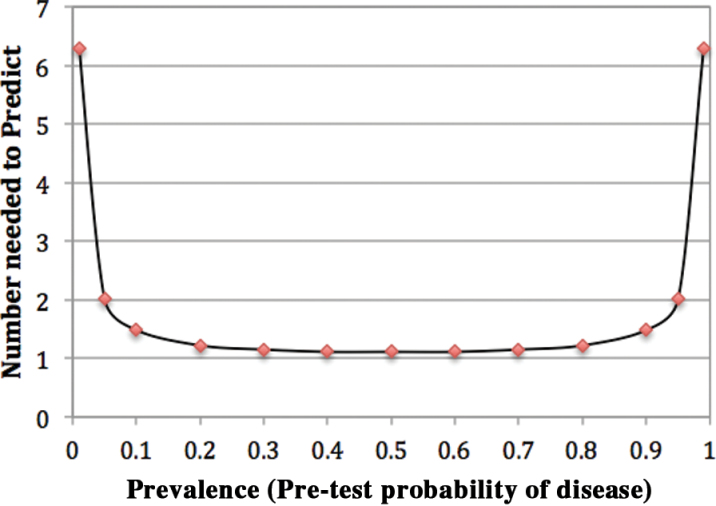
The principal justification for performing a diagnostic test is to gain new information. Test results can have little impact on clinical decision-making when the prevalence of disease is at extremes because there is little difference between the pre- and post-test probabilities.6 For any test, the relationship between prevalence and predictive values is dynamic.10 The total gain in certainty, as indicated by the predictive summary index (PSI, ψ = NPV + PPV − 1) is greatest when the pre-test probability of the disease (prevalence) is around 50% (Table 1, Fig. 1).6,7 Similarly, the number of persons needed to be examined in order to correctly predict a diagnosis of the disease (number needed to predict, NNP = 1/ψ) is also at its lowest around this midpoint (Table 1, Fig. 2). Here, a positive result from a sensitive and specific test almost guarantees the diagnosis and a negative result effectively eliminates the target disorder(s) from the differential diagnosis. All tests are of their greatest diagnostic use in the 50:50 dilemma when the pre-test probability of the target disease is equally likely to be present or absent. However, in practice, the time-efficiency principle will operate most effectively at low prevalences, typically between 0% and 10% (Fig. 2). Here, each small increase in prevalence results in the greatest fall in NNP, i.e. tests at follow-up rapidly become more useful. This is helpful as the probable prevalence of most major pathologies presenting in primary care is <10%. The diagnostic task is to then apply more refined tests, such as imaging or specialist opinion, for patients who have reached the point of flattening on the parabola, around the 10% prevalence point. It is the particular skill of a GP working in a low-prevalence setting to safely reach this 10% zone, where definitive testing or referral becomes much more useful, by using the time-efficiency principle.
Table 1.
The effect of prevalence on predictive summary index and number needed to predict when using an excellent sign, symptom or laboratory test*
| Prevalence (Pre-test probability) | 1% | 10% | 50% | 90% | 99% |
|---|---|---|---|---|---|
| Positive predictive value (PPV) | 16% | 68% | 95% | 99.4% | 99.9% |
| Negative predictive value (NPV) | 99.9% | 99.4% | 95% | 68% | 16% |
| Predictive summary index (PSI) (NPV + PPV − 1) | 15.9% | 67.4% | 90% | 67.4% | 15.9% |
| Number needed to predict (NNP) (1/PSI) | 6.3 | 1.4 | 1.1 | 1.4 | 6.3 |
Sensitivity and specificity equal 95% in every case.
Table constructed using data presented by Sackett et al.6
Figure 1.
The effect of prevalence on predictive summary index for an excellent sign, symptom or laboratory test. Figure constructed using data presented by Sackett et al. 6
Figure 2.
The effect of prevalence on number needed to predict for an excellent sign, symptom or laboratory test. Figure constructed using data presented by Sackett et al. 6
Using time in primary care
The ‘test of time’ involves careful initial assessment of the presenting problem(s), followed by one or more reassessment(s), ideally after a predefined period of time, although the same principles apply if the patients return entirely of their own volition.11 On reassessment(s), the symptoms or signs may become more clearly defined and may resolve or worsen, or new ones may appear. Diagnosis by test of time requires a sufficient understanding of the natural course of common or major conditions to enable appropriate reassessments, and this is where the GP’s knowledge and experience are most clearly displayed.11 These conditions may have a provisional diagnosis or informal diagnostic label, e.g. ‘it’s probably a virus’.12 This enables the clinician to view the disease as an evolving process.13
Explaining the time-efficiency principle
One of the most important diagnostic tasks performed by the GP is discriminating between the majority of patients with minor, usually self-limiting, illness and the minority with serious disease. For example, a cohort study of 2690 adults presenting with lower respiratory tract infections found that 92% had recovered within 3 weeks and only 1.1% were hospitalized, none of whom died.14 Because most patients improve within a relatively short time, this creates a dynamic process that efficiently increases the prevalence of serious disease in those patients who fail to recover in the anticipated time. The test of time thus serves as a silent adjudicator—discriminating between those with self-limiting illness and those with serious disease. It is driven by the self-limiting nature of most diseases in primary care, but it is necessary because self-limiting and progressive diseases can often not be distinguished early in their evolution. The prevalence of serious diseases increases over time to nearer the point of equipoise, where any subsequent tests will have their greatest impact on clinical decision-making.
The time-efficiency principle probably has important implications for how clinicians handle uncertainty. Schneider et al. demonstrated that the properties of the test of time were remarkable.15 They demonstrated that using the test of time when faced with uncertainty positively correlated with items relating to ‘intuition’, where a decision is reached even though the processes cannot be easily described. They suggested that the test of time contributes to a simple heuristic in keeping with Bayes theorem.16 Here, the clinician elicits specific points in the history and examination and then delays further testing to identify patients with a pre-test probability of the target disorders closer to the point of equipoise, e.g. in the 10% prevalence range, where any subsequent tests will be of great clinical value. Reaching this point is the reward for those clinicians willing to tolerate uncertainty and provide continuity of personal care.
When is the time-efficiency principle used?
It is important for clinicians to distinguish between patients who require rapid investigation, treatment or referral and those who would benefit from serial testing over time. The test of time should only be used in those situations where the benefit of applying time outweighs the risk of harm from a delayed or missed diagnosis, e.g. diarrhoea, where the initial assessment has not identified any substantial concerns and the usual course of presumed infectious causes is well established.17 By contrast, the occasional patients with red flag symptoms and signs, or who present late, warrant immediate referral.11
The main diagnostic challenge in primary care is low prevalence, not opportunities to use time, which are abundant.18 Patients are typically seen early in the course of an illness and care should be considered continuous. By contrast, in secondary care, many patients have been through the filter of primary care, where time may have already been used. As a consequence, patients are often seen later in the course of their illness when more urgent, definitive treatment is required.6
Minimizing the cascade effect
A major benefit of the test of time is that it serves to protect patients with non-serious disease from unnecessary additional testing. It is a brake upon cascade effects that occur when an initiating factor, such as an inappropriate test, is followed by a series of tests with increasing momentum, so that stopping becomes progressively harder, possibly moving to sophisticated tests and procedures where risk exceeds benefits.19 Cascade effects can be triggered by inappropriate data gathering such as the erroneous interpretation of a laboratory result outside normal ranges, underestimating the risks of test of treatment, underestimating the possibility of a false-positive result and the intolerance of uncertainty by the doctor. Because the chief source of error in medicine is not the quality of performance of processes but the quality of decisions to initiate those processes, it may be that the test of time serves as a relative brake against iatrogenesis.15 It may also be one of the key reasons why strong primary care is associated with lower health service costs.13,20
Continuity of care
The effectiveness of the time-efficiency principle is associated with the continuity of personal care provided by the clinician. It is here that we see the value of interpersonal warmth, trust and informality, which characterize most general practice consultations, together with the careful but economical exclusion of serious illness.21 For patients to tolerate the inevitable uncertainty of waiting for symptoms to resolve or develop, it is vital that they are able to trust their GP. Meanwhile, great care must be taken to ensure that the social rhythms of primary care, such as appointment systems, relate to the natural course of disease. General practice should be seen as an average of 38 minutes clinician–patient contact spread over the course of a year, not just discrete, typically 10- to 15-minute isolated consultations.22 At any time, a GP usually has several patients due to have further tests conducted at a specified time point when the diagnosis may become more clear.23 For example, a borderline thyroid function test may be repeated after 3–6 months to determine whether it has become abnormal or reverted to normal. A failure to provide such continuity of care weakens the opportunity to use time as a diagnostic strategy.
Circumventing the test of time
Primary care operates in a relatively technologically unsophisticated environment remarkably well suited for the populations it serves. In many ways, the time-efficiency principle typifies this approach by using the trust that comes from strong clinician–patient relationships to allow time to be actively used for self-limiting conditions to resolve or pathology to emerge. In recent years, this has been challenged by a growing interest in near-patient diagnostic testing, particularly in the USA, where 20% of laboratory results are performed and analysed solely in primary care.24 In doing this, the doctor lessens the use of the time in an attempt to diagnose disease earlier in the course of an illness. Such innovations can be quickly established in practice, especially when promoted by commercial interests, so that within a short space of time, the onus is on the doubter to show that they do not work rather than on proponents to show that they do.25 The test of time can also be circumvented by requesting wide batches of ‘routine tests’ early in the diagnostic process. This can come from patient pressure or defensive practice, an attempt to minimize all uncertainty as an assumed safeguard against litigation. Perhaps the greatest irony is that this approach may not only be counterproductive, it may actually increase malpractice risk.26 Studdert et al. argued that the more that refined diagnostic tests with low predictive values are performed for a given condition, the more likely is this to become a legal standard of care.27
Conclusion
The challenge for primary care and other low-prevalence settings is to only make diagnoses that are actually useful to patients, at the optimum time, while living with the uncertainty of informed doubt. The trust patients have for their doctor should be matched by a willingness to tolerate such uncertainty and not rush for technologically appealing investigation before time can be used appropriately to identify more clearly the possibility of serious pathology. If we cease to provide patient-centred diagnostics as reflected by the time-efficiency principle, it is primarily because we have lost our sense of respect towards the natural history and prevalence of disease that we see every day. If we allow a false reliance on inappropriate near-patient diagnostic testing, and residual alarm from rare late diagnoses where harm has ensued, to push us towards making over-refined diagnoses unnecessarily early, the costs for patients and for professional morale will be considerable.
Declaration
Funding: none.
Ethical approval: none.
Conflict of interest: none.
References
- 1. Department of Health. Over £330 Million to Give More Than Two and a Half Million Patients Better Care and Services. London, UK: Central Office of Information, 2012. [Google Scholar]
- 2. Mathers N, Hodgkin P. The gatekeeper and the wizard: a fairy tale. BMJ 1989; 298: 172–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Royal College of General Practitioners. Medical Generalism: Why Expertise in Whole Person Medicine Matters. London, UK: RCGP, 2012. [Google Scholar]
- 4. Aronoff SC. How useful are laboratory tests in diagnosing serious infections in febrile children? BMJ 2011; 342: d2782. [DOI] [PubMed] [Google Scholar]
- 5. Lindbaek M, Hjortdahl P, Johnsen UL. Use of symptoms, signs, and blood tests to diagnose acute sinus infections in primary care: comparison with computed tomography. Fam Med 1996; 28: 183–8. [PubMed] [Google Scholar]
- 6. Sackett D, Haynes R, Tugwell P. Clinical Epidemiology: A Basic Science for Clinical Medicine. Boston, MA: Little, Brown and Co., 1985. [Google Scholar]
- 7. Linn S, Grunau PD. New patient-oriented summary measure of net total gain in certainty for dichotomous diagnostic tests. Epidemiol Perspect Innov 2006; 3: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Connell FA, Koepsell TD. Measures of gain in certainty from a diagnostic test. Am J Epidemiol 1985; 121: 744–53. [DOI] [PubMed] [Google Scholar]
- 9. Salmim L. Re: Measures of gain in certainty from a diagnostic test. Am J Epidemiol 1986; 123: 1121–2. [DOI] [PubMed] [Google Scholar]
- 10. Sox HC, Jr, Hickam DH, Marton KI, et al. Using the patient’s history to estimate the probability of coronary artery disease: a comparison of primary care and referral practices. Am J Med 1990; 89: 7–14. [DOI] [PubMed] [Google Scholar]
- 11. Almond SC, Summerton N. Diagnosis in general practice. Test of time. BMJ 2009; 338: b1878. [DOI] [PubMed] [Google Scholar]
- 12. Crossley T. I Don’t Know What It Is But I Don’t Think It’s Serious: Confidence and Decisiveness in Primary Care. London, UK: RCGP, 2008. [Google Scholar]
- 13. Tudor-Hart J. The Political Economy of Health Care. 2nd edn. Bristol, UK: Policy Press, 2006. [Google Scholar]
- 14. van Vugt SF, Butler CC, Hood K, et al. Predicting benign course and prolonged illness in lower respiratory tract infections: a 13 European country study. Fam Pract 2012; 29: 131–8. [DOI] [PubMed] [Google Scholar]
- 15. Schneider A, Löwe B, Barie S, et al. How do primary care doctors deal with uncertainty in making diagnostic decisions? The development of the ‘Dealing with Uncertainty Questionnaire’ (DUQ). J Eval Clin Pract 2010; 16: 431–7. [DOI] [PubMed] [Google Scholar]
- 16. André M, Borgquist L, Foldevi M, Mölstad S. Asking for ‘rules of thumb’: a way to discover tacit knowledge in general practice. Fam Pract 2002; 19: 617–22. [DOI] [PubMed] [Google Scholar]
- 17. Hamilton W, Sharp D. Diagnosis of colorectal cancer in primary care: the evidence base for guidelines. Fam Pract 2004; 21: 99–106. [DOI] [PubMed] [Google Scholar]
- 18. Howie JG. Diagnosis–the Achilles heel? J R Coll Gen Pract 1972; 22: 310–5. [PMC free article] [PubMed] [Google Scholar]
- 19. Mold JW, Stein HF. The cascade effect in the clinical care of patients. N Engl J Med 1986; 314: 512–4. [DOI] [PubMed] [Google Scholar]
- 20. Starfield B. William Pickles Lecture. Primary and specialty care interfaces: the imperative of disease continuity. Br J Gen Pract 2003; 53: 723–9. [PMC free article] [PubMed] [Google Scholar]
- 21. Metcalfe D. Competence, Administration and Learning. London, UK: MSD Foundation, 1989. [Google Scholar]
- 22. Irving G, Reeve J. Do GPs really provide 47 minutes a year for the patient? Br J Gen Pract 2012; 62: 404–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hill A, Freeman G. Promoting Continuity of Care in General Practice. London, UK: RCGP, 2011. [Google Scholar]
- 24. Hobbs FD, Delaney BC, Fitzmaurice DA, et al. A review of near patient testing in primary care. Health Technol Assess 1997; 1: i–iv, 1–229. [PubMed] [Google Scholar]
- 25. Rogers E. Diffusion of Innovations. 5th edn. New York, NY: Free Press, 2003. [Google Scholar]
- 26. Budetti PP. Tort reform and the patient safety movement: seeking common ground. JAMA 2005; 293: 2660–2. [DOI] [PubMed] [Google Scholar]
- 27. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA 2005; 293: 2609–17. [DOI] [PubMed] [Google Scholar]