Abstract
Despite the availability of innovative health care research, a gap exists between research-generated knowledge and the utilization of that knowledge in real-world practice settings. This article examines the transition from research to implementation in the context of the dissemination of A. Jean Ayres’ sensory integration procedures and of the challenges currently facing the University of Southern California Well Elderly Studies research team. Drawing from the emerging field of implementation science, this article discusses how researchers can develop an implementation plan to more easily translate evidence into practice. Such plans should address the intervention’s reach (i.e., its capacity to penetrate into the intended target population), the settings for which it is applicable, the leaders who will encourage practitioner uptake, stakeholder groups, and challenges to dissemination. By taking action to ensure the more effective dissemination of research-generated knowledge, researchers can increase the likelihood that their interventions will lead to improvements in practice and more effective care for consumers.
MeSH TERMS: diffusion of innovation, evidence-based practice, information dissemination, translational medical research
Efficacious occupational therapy interventions exist across a broad spectrum of practice areas, and innovations in cutting-edge treatment approaches are continually being generated through research endeavors. However, too few of these interventions are actually implemented in the real world (Katz, 2010; Kitson et al., 2008). Occupational therapy researchers take for granted that implementation naturally flows from effective intervention trials, but this is not the case. Research suggests that less than half of evidence-based health care practices are ever implemented and that a 20-yr gap exists between research-generated knowledge and the utilization of that knowledge in health or mental health service delivery (Brekke, Ell, & Palinkas, 2007; Glasgow & Emmons, 2007). This gap between the demonstration of efficacious interventions and their implementation in practice manifests itself in patient care. Indeed, 30%–45% of patients receiving a wide range of professional programs and services currently do not receive care that is based on scientific evidence, and 20%–25% receive care that is not needed or is potentially harmful (Grol, 2008; Grol & Grimshaw, 2003).
In this article, we discuss the contributions of a newly emerging science—implementation science—and its implications for occupational therapy. Dedicated to uncovering systematic methods through which efficacious interventions can be validly and efficiently infused into practice, implementation science has challenged the assumption that this process happens automatically. We describe the actions occupational scientists and occupational therapy practitioners can take to maximize the likelihood of real-world implementation of evidence-based occupational therapy and of dissemination to consumers, policymakers, and the media. We start by presenting two contrasting case studies drawn from the profession’s history to illustrate the successes and challenges that occupational therapists have faced in implementing efficacious interventions in the real world.
Case Studies Illustrating Challenges to Research Translation
A. Jean Ayres and Sensory Integration Procedures
Today, we know A. Jean Ayres as a towering pioneer in the development of the sensory integration approach to treatment and as one of the first occupational therapists to conduct a systematic research program that resulted in the provision of preliminary intervention efficacy data. Looking back on the record of her achievements, we marvel at her vision, tenacity, scientific mind, and overall productivity. Clearly, occupational therapy owes her an enormous debt. But what is not well known is the strong resistance that her work initially encountered within the occupational therapy profession and the many barriers that she overcame in her efforts to ensure that sensory integration procedures would be widely adopted (Arluke, 1991). Today, not only are these procedures frequently incorporated as a component of occupational therapy service provision, but they are also firmly planted in many state-of-the-art comprehensive educational programs for children with neurodevelopmental disorders (Greenspan & Wieder, 2009; Mesibov, Shea, & Schopler, 2004; Prizant, Wetherby, Rubin, & Laurent, 2003; Rogers & Dawson, 2009; Schopler, 1997).
The first author (Florence Clark) met Ayres in 1974 while still a novice practitioner. Ayres had agreed to consult with Clark and her colleagues on a research project they were implementing on the effects of sensory integration procedures compared with operant methods in producing developmental gains in adults with intellectual disabilities (Clark, Miller, Thomas, Kucherawy, & Azen, 1978). Unaware at the time that Ayres’ work was controversial within the occupational therapy community, Clark completed this early study without worries of disapprobation.
In the late 1960s, Ayres had encountered fierce resistance from occupational therapy practitioners and was “excluded from, rather than embraced by, the community of therapists” (Peters, 2011, p. 256). In discussing the work of her colleague, Lela Llorens recalled that when Ayres
was at what I would call the height of her game in terms of sensory integration, teaching, and trying to teach the rest of the profession, she was greeted with real hostility. . . . She met with a lot of hostility from people who didn’t want to believe what she was saying. (as quoted in Peters, 2011, p. 256)
Why did this happen? Was the resistance Ayres experienced typical of what occurs during the gap between research generation and real-world implementation? Was the field unable and unprepared to incorporate new ideas and new evidence? Were therapists resistant to shifting their thinking about their practice, about nervous system plasticity, and about the potential of children with neurodevelopmental disorders to benefit from therapist-led interactions in sensory-rich environments? Did Ayres’ research and the therapeutic approach that flowed from it present a threat to the status quo?
Ayres persisted in her efforts to ensure that this scientifically grounded intervention would be implemented in educational curricula and practice. Seeking academic legitimization, in 1976 she accepted an adjunct appointment as a faculty member in the occupational therapy department at the University of Southern California (USC) and gained approval to teach a course, Advanced Sensory Integration Practice, using a combination of seminars and intense practice mentoring in a privately owned clinic (the Ayres Clinic). Coincidentally, Clark had just accepted a full-time faculty position at USC responsible for teaching sensory integration content and was one of four students enrolled in the first session of the Advanced Sensory Integration Practice course.
Thirty-six years later, reflecting on that time, Clark now realizes that the most important takeaway was not improving clinical skills, as she had anticipated, but rather witnessing firsthand how science-driven practice is created and successfully implemented in the real world. She came to fully appreciate the ways in which the basic animal studies on neuroplasticity and environmental enrichment to which Ayres had previously been exposed during her postdoctoral studies at the University of California, Los Angeles Brain Research Institute informed sensory integration theory. Ayres posited that, much in the same way that increases in dendritic arborization in rats had been shown to result from interaction in enriched environment studies, similar changes in neural architectures could be achieved in children if they were presented with appropriate sensory input and challenges. Implementation of this idea required Ayres to invent much of the equipment that is now in widespread use in settings providing sensory integration therapy, including customized platform and bolster swings, ramps, and scooter boards. Today, one is struck by the resemblance of the typical sensory integration clinic to the enriched environments used in the animal model studies that informed Ayres’ research (Figure 1).
Figure 1.

Examples of (A) an enriched environment animal study and (B) a modern-day sensory integration clinic.
Note. Photographs courtesy of Wendy Sternberg. Photo credits: (A) Matthew Stein, 2009. (B) Erna Blanche, n.d.
Before joining the USC faculty, Ayres had already embarked on a multifaceted implementation strategy. She had lectured on her work throughout the nation and had trained a cadre of therapists, who were providing continuing education programs on the therapeutic approach and would later offer a certification process to ensure valid use of the related battery of standardized tests Ayres had developed. This critical mass of transformational leaders, in combination with the strengths Ayres herself brought to the implementation process, was vital for gaining traction for the widespread incorporation of the sensory integration approach into pediatric occupational therapy. In part because of its adoption and the demonstration that it appeared efficacious for a subset of children with learning disabilities, the practice of pediatric occupational therapy surged. In the 1970s, 11% of all occupational therapists were working in pediatric practice; this percentage is now 32.2%, and 85% of practitioners working in a school setting report use of sensory integration as a component of their practice (American Occupational Therapy Association, 2010).
This case study is a shining example of how, despite significant headwinds and barriers to research translation, evidence-based interventions can successfully be adopted in practice and, concomitantly, can increase the demand for services. At the conclusion of her illustrious career, Ayres had published more than 50 articles and books, developed more than 10 standardized tests for differentiating types of sensory integration difficulties, specified a wide range of therapeutic procedures specifically tailored to be responsive to particular kinds of problems with sensory integration, and invented a wide range of therapeutic equipment, much of which is now commercially available.
USC Well Elderly Studies
A second, but contrasting, illustration of the challenges faced in translating evidence-based interventions into practice involves the USC Well Elderly Studies, two large-scale randomized controlled trials funded by the National Institutes of Health (R01 AG11810; 1 R01 AG021108–01A2) on which Clark served as principal investigator. These studies, involving a combined total of 800 participants, demonstrated the efficacy and cost-effectiveness of a preventive occupational therapy intervention (now called Lifestyle Redesign®) for improving the health and quality of life of independently living older adults. The overarching aim of the intervention is to enable older adults living independently to develop and implement sustainable, health-promoting routines in their everyday lives (Clark et al., 1997). In the first Well Elderly Study, the results showed that the Lifestyle Redesign intervention produced significant benefits across health, function, and quality of life domains, including vitality, general health, physical functioning, social functioning, and general mental health, and that 90% of gains were retained after 6 mo. The second Well Elderly Study replicated the previous results in a larger, more ethnically diverse population (Clark et al., 2012) and investigated the mechanisms that account for the intervention’s positive effects. Both studies demonstrated the intervention to be cost-effective.
Interestingly, the Well Elderly Studies have had a greater impact internationally on policy and practice than in the United States. For instance, a modified version of the Lifestyle Redesign intervention customized for older people in the United Kingdom was recommended for promotion of mental well-being by the U.K. National Health Service’s National Institute for Health and Clinical Excellence (2008). The intervention has also been adapted for use by Norwegian researchers to develop a manualized Lifestyle Redesign program for stroke survivors (Lund, Michelet, Kjeken, Wyller, & Sveen, 2012).
Fifteen years have passed since publication of the findings of the first Well Elderly Study, and more than 15 related publications have described aspects or findings of the combined Well Elderly Studies, but the intervention approach has not been widely adopted in practice in the United States. Why? Several key explanations are plausible. First, and perhaps most significant, prevention services of this kind for independently living adults are not funded by the Centers for Medicare and Medicaid Services. Second, relatively few occupational therapists are employed in community-based settings where older adults reside. Third, the investigators, unlike Ayres, have not carried out a well-thought-out dissemination and implementation plan involving certification and continuing education. Despite the mismatch between the focus of the intervention, on one hand, and the contexts in which therapists are typically employed and the reimbursement coverage appropriated in public policy, on the other, a carefully conceived implementation plan for clinical adoption could potentially lead to overcoming such barriers.
Implementation Science
The experience just described with respect to the USC Well Elderly Studies is not unique. The set of challenges that various professions have encountered in addressing this very problem has resulted in the emergence of a new field—implementation science. Broadly defined, implementation science “is the scientific study of methods to promote the systematic uptake of research findings and other evidence-based practices into routine practice, and, hence, to improve the quality and effectiveness of health services and care” (Eccles & Mittman, 2006, Implementation Science section, para. 2). Disciplines such as nursing, medicine, and social work have generated knowledge and developed implementation models that can help bridge the gap between science and practice.
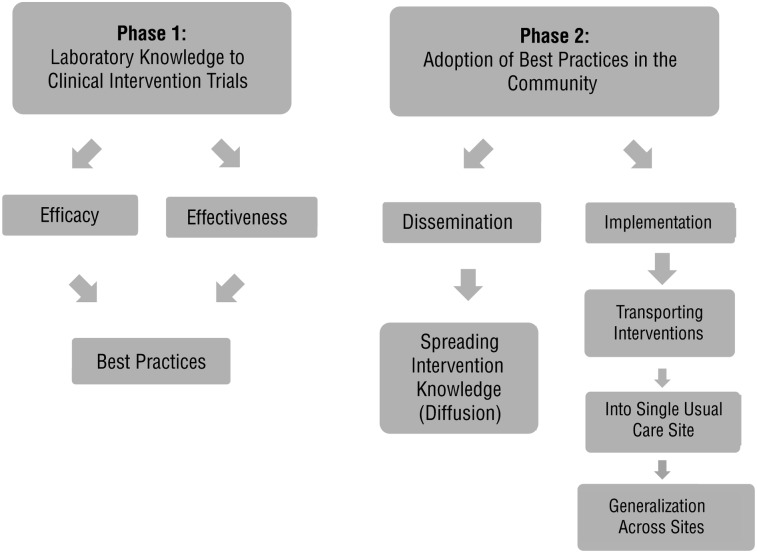
Figure 2 presents a two-phase research translation model developed by Brekke et al. (2007) after the implementation of social work mental health interventions. Phase 1 covers the progression from laboratory knowledge to clinical intervention trials through efficacy and effectiveness research, ideally resulting in strong research support for an intervention constituting best practice. Efficacy trials investigate whether an intervention produces a positive effect under ideal test conditions, whereas effectiveness trials investigate whether it produces similar results under real-world conditions among a more diverse population (Flay, 1986; Glasgow, Lichtenstein, & Marcus, 2003).
Figure 2.
Brekke, Ell, and Palinkas’ (2007) research translation model.
Note. From “Translational Science at the National Institute of Mental Health: Can Social Work Take Its Rightful Place?” by J. Brekke, K. Ell, & L. Palinkas, 2007, Research on Social Work Practice, 17, 123–133. http://dx.doi.org/10.1177/1049731506293693. Copyright © 2007 by SAGE Publications. Used with permission.
Phase 1 is similar to that completed by the USC Well Elderly Studies investigative team. Going beyond this, Figure 2 depicts Phase 2 as entailing a two-prong progression. One pathway corresponds to dissemination of research findings through strategies such as journal publications and outreach to media sources. The Well Elderly Studies investigative team completed these steps. However, the second pathway concerns implementation and transportation of interventions from the clinical trial sites into single usual-care sites and eventually into a larger, more diverse pool of population groups. In contrast to the course followed by Ayres, to date the Well Elderly Studies investigative team has not yet traversed this pathway.
Implementation Science at the Research Design Level: RE–AIMing Translational Research
As implementation science has developed and matured, there is widespread recognition that implementation of evidence-based practices is even more complicated than as depicted in Figure 2, requiring whole-system change at the research design, practitioner, and institution levels (Burke & Gitlin, 2012). Because of the multiple considerations that influence this change process, efficacy and effectiveness researchers need to take this complexity into account as they conceptualize and develop interventions and systematically study their outcomes. To that end, implementation science has brought to the forefront the understanding that it is not enough for an intervention to work: to have an impact, it must also have reach (Glasgow et al., 2003), defined as the capacity to be broadly applicable. Applicability, in turn, is maximized when interventions have the following characteristics:
They are seen by practitioners as having the potential to apply to large numbers of people.
They are not overly rigid but rather are easily customizable to the specific needs of local settings.
They can be replicated at a reasonable cost.
They do not require highly specialized training to consistently administer. (Glasgow et al., 2003)
In contrast, interventions that are viewed as too intensive, demanding too much time or effort, and not adequately packaged or manualized have been found to be less likely to be implemented (Glasgow & Emmons, 2007). To expedite the implementation process, interventions should be designed to possess real-world practicality and to be readily transferable to a wide range of practice settings. Taking these considerations into account, Russell Glasgow, a renowned behavioral scientist, developed the reach–effectiveness–adoption–implementation–maintenance (RE–AIM) framework as a heuristic for guiding researchers at the outset of their research programs in thinking through the entire progression of translational intervention trials so that implementation is more likely (Figure 3).
Figure 3.
Recommendations for RE–AIMing translational research.
Note. From “Translating Research to Practice: Lessons Learned, Areas for Improvement, and Future Directions,” by R. E. Glasgow, 2003, Diabetes Care, 26, p. 2452. Copyright © 2003 by the American Diabetes Association. Adapted with permission.
The first element of RE–AIM, reach, refers to the penetration of an intervention into its targeted audience (Glasgow, 2003). To maximize reach, researchers are encouraged to design interventions to be as broadly applicable as possible. Interventions that on the surface appear to be applicable to a narrow group of people are less likely to be implemented. In the case of Lifestyle Redesign, the intervention, although broadly applicable to independently living older adults, was not readily so for the rehabilitation population with whom occupational therapists typically work, making implementation complicated.
The second element of RE–AIM, effectiveness, refers to measurable change in important health outcomes, which optimally include an intervention’s impact on quality of life. Research that demonstrates that an intervention influences such factors as disability, function, and health care costs and other economic measures maximizes the likelihood of its being perceived as relevant to real-world concerns. For example, the adoption of sensory integration procedures as a component of pediatric occupational therapy was, in part, contingent on demonstrating that the intervention went beyond minimizing “symptoms” and improved academic abilities in children with learning disabilities (Ayres, 1972).
The RE–AIM framework’s third element, adoption, refers to the participation rate among clinical settings (e.g., clinics, organizations). To promote adoption, interventions should be developed that are feasible, replicable, and easily tailored to the particular needs of different settings, as previously discussed.
The fourth element, implementation, is defined narrowly in the RE–AIM model as the ability of the intervention to be delivered with consistency and fidelity. In designing intervention research, researchers need to specify methods for evaluating and ensuring intervention fidelity, such as manualizing the intervention and creating tools for assessing fidelity. Unfortunately, in the early implementation of sensory integration procedures, tools were not available to assess the degree to which practice implementation across settings was consistent and in keeping with the intervention’s theoretically driven guidelines (i.e., fidelity). As a result, approaches have varied across settings in important ways. A well-designed fidelity measure has recently been published (Parham et al., 2011), however, and its use is likely to ensure greater consistency and fidelity in the application of sensory integration procedures.
Finally, maintenance, the fifth element of RE–AIM, is defined broadly both as program sustainability and as the long-term effects of the intervention. Sustainable interventions with evidence for long-term retention of therapeutic gains have a greater likelihood of implementation and follow-through. Thus, in the research design phase, researchers should carefully formulate plans for long-term follow-up studies and strategies to sustain the program.
Researchers can easily use the RE–AIM framework in the planning of a research program to evaluate the efficacy and effectiveness of occupational therapy interventions that, if demonstrated to be beneficial, will have a high likelihood of being readily implemented in practice. The many elements of an intervention’s applicability—its measurable impact on health, quality of life, and economic outcomes; its ease in being consistently delivered in real-world settings; its feasibility; and its long-term sustainability—are determining factors in the ultimate translation of the research and thus are elements that researchers should pay attention to early on in the process of delineating the various steps in a long-term research program.
Implementation Science: Managing Practitioner Uptake
The whole-system change typically required for wide-scale implementation of efficacious occupational therapy interventions may also necessitate transformation at the practitioner and institutional levels. Altering practice patterns, mindsets, and beliefs at the practitioner level and culture at the institutional level is admittedly a challenging task. The concepts discussed in the paragraphs that follow offer promising launch points.
Practitioner Level: Mindlines
If occupational therapy practitioners are to consistently implement evidence-based practice in the therapy they provide, it is essential that their mindlines—that is, the ways they think during practice—be identified to facilitate change. In an impressive ethnography of clinical decision making, Gabbay and Le May (2011) defined mindlines as clinicians’ internalized guidelines for treatment that, in turn, are translated into the treatment choices they make. Ultimately, practitioners determine the extent to which evidence-based interventions are actually used in practice. Each clinician’s mindline is shaped by myriad factors, including experiential knowledge from practice; textbook knowledge; “grazing” of professional and commercial literature; conversations with colleagues; experiences with patients; and social, economic, and organizational demands. A clinician’s mindline continually evolves as he or she takes in new information, and ideally, new evidence-based interventions are incorporated into his or her treatment repertoire through a process called mindline expansion.
How do mindlines change, expand, and incorporate new information? According to Gabbay and Le May (2011), mindlines expand through a process of knowledge integration in which explicit knowledge that is gathered from research and other external sources, such as the media, is transformed into tacit knowledge and then externalized into actions and clinical decisions (e.g., clinicians’ treatment plans). This transformation process is largely one of internalization and socialization and thus is highly influenced by a practitioner’s colleagues and work setting. Practically speaking, then, transformational leaders within the workplace have the ability to powerfully influence the mindline expansion of their fellow practitioners. This is what happened at the setting where Clark was employed in 1974. The sensory integration effectiveness study was launched because one charismatic and respected clinician had attended several of Ayres’ lectures given in the context of continuing education. She influenced Clark and her fellow practitioners (1978) to attend sensory integration continuing education programs, to give this approach a salient place in their mindlines, and ultimately to implement their study.
Transformational leaders work with their colleagues to expand their mindlines rather than simply try to impose their beliefs about practice on them. These leaders encourage opportunities at work to critically appraise evidence, facilitate dialogue on how to incorporate new findings into the specific practice contexts they see every day, and urge their fellow practitioners to take relevant courses. Not only do they obtain the latest evidence on best practice from well-vetted sources, but they also are trusted and respected by their peers. Finally, they work with others so that together they can set the workplace standard for implementation. Through these practices, transformational leaders can facilitate ongoing expansion in the mindlines of others and concomitant alterations in best practice approaches in particular clinical settings.
Institutional Level: Promoting Action on Research Implementation in Health Services
The underlying assumption of the Promoting Action on Research Implementation in Health Services (PARiHS) framework is that successful implementation of evidence-based practice is a function of the interplay among three core elements: evidence, context, and facilitation (Kitson, Harvey, & McCormack, 1998). In this way, the PARiHS framework succinctly brings together the ideas previously presented in this article; however, the process of research translation is depicted on an institutional scale.
We have already described how the first element, evidence, which is obtained from the research literature, interacts with clinical experience, patient experience, and local context-specific information to shape a clinician’s mindline. To this, the PARiHS framework adds the second component, context, emphasizing the critical importance of an organization’s context on the extent to which evidence-based interventions are implemented at a particular setting or in a service delivery system.
Context encompasses an organization’s culture, mandated protocols, leadership structure, and evaluation mechanisms, all of which support or hinder the likelihood of an evidence-based practice being adopted. For example, an organization’s culture dictates whether continuing education is encouraged or whether practitioners are likely to regularly read cutting-edge rehabilitation journals and discuss their content with colleagues. Leadership structures determine whether clearly defined roles exist among colleagues and whether teamwork to implement new evidence-based practices can be effective. Evaluation mechanisms enable tracking of progress in the use of and corresponding outcomes of innovative interventions. These features of the context render it a powerful determinant of the degree to which implementation is successful in particular settings.
The third core element highlighted in the PARiHS framework is facilitation, defined as the support provided to enable change in attitudes, habits, skills, ways of thinking, and work (Kitson et al., 2008). Viewed as the active force that promotes change, facilitation is set into motion by people who possess the qualities of transformational leaders. Facilitation methods may vary in approach and support style over time; for example, early on they may be more directive, but later they may be less so and may take on an enabling and empowering role (Harvey et al., 2002). When facilitation methods are extremely effective, facilitators are able to draw out the inherent potential of others and concomitantly pursue their own change process in ways that are personally meaningful and relevant.
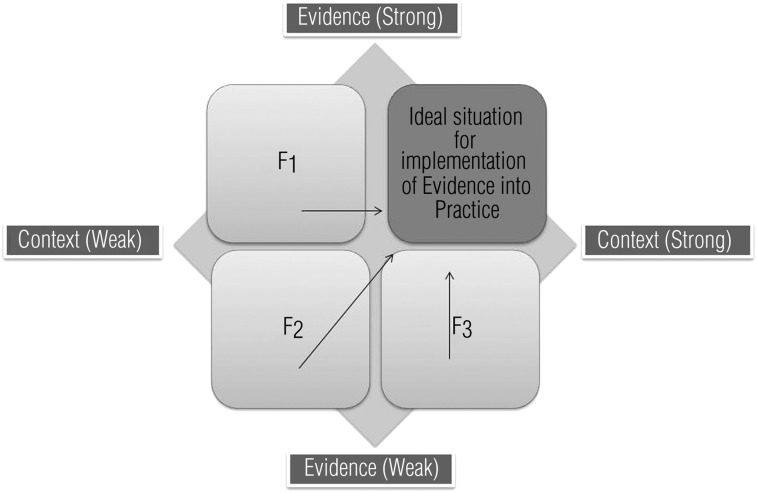
In the PARiHS framework, the interaction between these three core elements—evidence, context, and facilitation—is seen as determining how successful implementation of an evidence-based intervention will be. As illustrated in Figure 4, the optimal situation for translation of evidence into practice occurs when sound evidence works together with broad reach, a strong context, and skillful facilitation. Research programs with the aim of demonstrating the efficacy of a novel intervention need to address variations that are likely across multiple settings. To anticipate these differences at the outset, it is helpful to envision the populations to whom and settings in which the intervention will apply, anticipate the challenges the context may impose, conceptualize how the facilitation process can be expedited, and provisionally identify who will assume the roles of transformational leaders.
Figure 4.
Role of facilitation in outcomes.
Note. From “Enabling the Implementation of Evidence Based Practice: A Conceptual Framework,” by A. Kitson, G. Harvey, & B. McCormack, 1998, Quality in Health Care, 7, 153, http://dx.doi.org/10.1136/qshc.7.3.149. Copyright © 1998 by BMJ Publishing Group Ltd. Adapted with permission.
Dissemination and Engagement of Policymakers
The research translation models previously discussed add to an understanding of the implementation of efficacious interventions by drawing attention to research design, practitioner, and institutional considerations. The final element required for successful implementation is to proactively communicate the results of the research to consumers and policymakers.
First, the importance of engaging stakeholders in the research process cannot be overstated. Stakeholders—the people who have an invested interest in the intervention or the population for which it is designed—may be community members, advocacy groups, patients, businesses, policymakers, or community-based organizations and can serve as valuable resources during both the trial and dissemination phases. Generally speaking, researchers should engage stakeholders at the very beginning stages of the research program. They may invite stakeholders to give input by serving on a community advisory committee or participating in a town hall forum (Katz, 2006). Stakeholders who see the importance of the proposed research can then aid in recruiting participants, identifying partners for collaboration, recognizing potential pitfalls, and ensuring real-world relevance. Moreover, alterations made in the design of the research program that are responsive to their input are likely to facilitate the probability that the intervention will be implementable in the future should it prove effective. Beyond this, stakeholders can be enormously helpful in raising the public profile of the intervention through word-of-mouth dissemination.
Second, it is important to communicate the benefits of an efficacious intervention directly to consumers in language that they can easily understand. Potential recipients of an efficacious intervention for stroke survivors, for example, will probably not be interested in the soundness of the statistical analysis but will want to know how the intervention will improve their lives. They will probably want to ascertain the extent to which the intervention has been shown to be responsive to practical concerns, such as whether it has beneficial effects on independence or disability or whether it decreases out-of-pocket health care expenditures. Forming partnerships with consumer interest and advocacy groups can help researchers identify outcome measures that matter to consumers and build linkages to networks of potential intervention recipients.
Third, researchers need to become savvy in using the media to disseminate study findings. The formulation of a coherent media strategy counteracts sporadic, fragmented, or limited media dissemination. Katz (2006) suggested calling reporters directly in addition to sending press releases to newspapers and television media outlets and providing contact information for people not directly involved with the study who can articulate what is compelling about the work to the public.
Fourth, researchers need to reach out to legislators and policymakers, recognizing that these people are under enormous time pressures and do not typically read rehabilitation or occupational therapy peer-reviewed journals. The best approach to alerting them to study findings is to contact them oneself and try to arrange a meeting either with the policymaker or his or her staff. For such meetings, one should bring copies of publications along with a one-page summary that clearly identifies which groups support the intervention and why. As with communication to consumers, it is important to succinctly tailor one’s message to the interests and priorities of this audience. How cost-effective is the intervention? What will the effect be on communitywide health outcomes? What portion of the policymaker’s constituents will benefit from this intervention?
Conclusion
In this article, we have illustrated that demonstrating the effectiveness or even the cost-effectiveness of an intervention does not guarantee its implementation in clinical practice. The process of doing clinical trials research has two phases: (1) developing and demonstrating the beneficial outcomes of an intervention and (2) implementing it in the real world so that it becomes incorporated as a best practice. When Phase 2 of the clinical trials research process—adoption of best practices in the community—is carefully planned, the likelihood that the intervention will actually improve practice and service delivery to consumers is increased. Scientists developing a clinical trials research program should incorporate an implementation plan at the outset of their research program that addresses concerns such as the following:
The reach of the intervention
The kinds of settings for which it is applicable
Who its transformational leaders will be
What groups constitute its stakeholders
What challenges will emerge to its infusion into the mindlines of occupational therapy practitioners.
Acknowledgments
We acknowledge Alison Cogan, Charlotte Deng, Monique Wolkoff, Vivian Tang, and Katherine Thompson for their valuable contribution to the production of this article. They performed the initial review of the implementation science literature that informed our early conceptualization of its relevance to occupational science and occupational therapy and greatly assisted with the development of the Advancing Clinical Trials and Outcomes Research (ACTOR) slide presentation that served as the foundation of this article. Finally, they contributed their technical expertise and computer skills in formatting the article and figures to American Psychological Association style specifications. An earlier version of this article was presented at the ACTOR Conference, Fairfax, VA, December 2011.
Contributor Information
Florence Clark, Florence Clark, PhD, OTR/L, FAOTA, is Professor and Associate Dean and Chair, Division of Occupational Science and Occupational Therapy, School of Dentistry, University of Southern California, 1540 Alcazar Street, CHP-133, Los Angeles, CA 90089; fclark@usc.edu.
Daniel J. Park, Daniel J. Park, OTD, OTR/L, is Assistant Professor of Clinical Occupational Therapy, Division of Occupational Science and Occupational Therapy, School of Dentistry, University of Southern California, Los Angeles
Janice P. Burke, Janice P. Burke, PhD, OTR/L, FAOTA, is Dean, Jefferson School of Health Professions, and Professor and Chair, Department of Occupational Therapy, Thomas Jefferson University, Philadelphia
References
- American Occupational Therapy Association. 2010 occupational therapy compensation and workforce study. Bethesda, MD: AOTA Press; 2010. [Google Scholar]
- Arluke A. The transformation and fate of formal knowledge: The case of sensory integration. Current Research on Occupations and Professions. 1991;6:179–199. [Google Scholar]
- Ayres A. J. Improving academic scores through sensory integration. Journal of Learning Disabilities. 1972;5:338–343. http://dx.doi.org/10.1177/002221947200500605 . [Google Scholar]
- Brekke J., Ell K., Palinkas L. Translational science at the National Institute of Mental Health: Can social work take its rightful place. Research on Social Work Practice. 2007;17:123–133. http://dx.doi.org/10.1177/1049731506293693 . [Google Scholar]
- Burke J. P., Gitlin L. N. The Issue Is—How do we change practice when we have the evidence? American Journal of Occupational Therapy. 2012;66:e85–e88. doi: 10.5014/ajot.2012.004432. http://dx.doi.org/10.5014/ajot.2012.004432 . [DOI] [PubMed] [Google Scholar]
- Clark F., Azen S. P., Zemke R., Jackson J., Carlson M., Mandel D., Lipson L. Occupational therapy for independent-living older adults: A randomized controlled trial. JAMA. 1997;278:1321–1326. http://dx.doi.org/10.1001/jama.1997.03550160041036 . [PubMed] [Google Scholar]
- Clark F., Jackson J., Carlson M., Chou C. P., Cherry B. J., Jordan-Marsh M., Azen S. P. Effectiveness of a lifestyle intervention in promoting the well-being of independently living older people: Results of the Well Elderly 2 randomised controlled trial. Journal of Epidemiology and Community Health. 2012;66:782–790. doi: 10.1136/jech.2009.099754. http://dx.doi.org/10.1136/jech.2009.099754 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark F. A., Miller L. R., Thomas J. A., Kucherawy D. A., Azen S. P. A comparison of operant and sensory integrative methods on developmental parameters in profoundly retarded adults. American Journal of Occupational Therapy. 1978;32:86–92. [PubMed] [Google Scholar]
- Eccles M. P., Mittman B. S. Welcome to implementation science. Implementation Science. 2006;1:1. http://dx.doi.org/10.1186/1748-5908-1-1 . [Google Scholar]
- Flay B. R. Efficacy and effectiveness trials (and other phases of research) in the development of health promotion programs. Preventive Medicine. 1986;15:451–474. doi: 10.1016/0091-7435(86)90024-1. http://dx.doi.org/10.1016/0091-7435(86)90024-1 . [DOI] [PubMed] [Google Scholar]
- Gabbay J., Le May A. Practice-based evidence for healthcare: Clinical mindlines. New York: Routledge; 2011. [Google Scholar]
- Glasgow R. E. Translating research to practice: Lessons learned, areas for improvement, and future directions. Diabetes Care. 2003;26:2451–2456. doi: 10.2337/diacare.26.8.2451. http://dx.doi.org/10.2337/diacare.26.8.2451 . [DOI] [PubMed] [Google Scholar]
- Glasgow R. E., Emmons K. M. How can we increase translation of research into practice? Types of evidence needed. Annual Review of Public Health. 2007;28:413–433. doi: 10.1146/annurev.publhealth.28.021406.144145. http://dx.doi.org/10.1146/annurev.publhealth.28.021406.144145 . [DOI] [PubMed] [Google Scholar]
- Glasgow R. E., Lichtenstein E., Marcus A. C. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. American Journal of Public Health. 2003;93:1261–1267. doi: 10.2105/ajph.93.8.1261. http://dx.doi.org/10.2105/AJPH.93.8.1261 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenspan S. I., Wieder S. Engaging autism: Using the floortime approach to help children relate, communicate, and think. Cambridge, MA: Da Capo Press; 2009. [Google Scholar]
- Grol R. Knowledge transfer in mental health care: How do we bring evidence into day-to-day practice? Canadian Journal of Psychiatry. 2008;53:275–276. doi: 10.1177/070674370805300501. [DOI] [PubMed] [Google Scholar]
- Grol R., Grimshaw J. From best evidence to best practice: Effective implementation of change in patients’ care. Lancet. 2003;362:1225–1230. doi: 10.1016/S0140-6736(03)14546-1. http://dx.doi.org/10.1016/S0140-6736(03)14546-1 . [DOI] [PubMed] [Google Scholar]
- Harvey G., Loftus-Hills A., Rycroft-Malone J., Titchen A., Kitson A., McCormack B., Seers K. Getting evidence into practice: The role and function of facilitation. Journal of Advanced Nursing. 2002;37:577–588. doi: 10.1046/j.1365-2648.2002.02126.x. http://dx.doi.org/10.1046/j.1365-2648.2002.02126.x . [DOI] [PubMed] [Google Scholar]
- Katz M. Study design and statistical analysis: A practical guide for clinicians. Cambridge, England: Cambridge University Press; 2006. [Google Scholar]
- Katz M. Evaluating clinical and public health interventions: A practical guide to study design and statistics. Cambridge, England: Cambridge University Press; 2010. [Google Scholar]
- Kitson A., Harvey G., McCormack B. Enabling the implementation of evidence based practice: A conceptual framework. Quality in Health Care. 1998;7:149–158. doi: 10.1136/qshc.7.3.149. http://dx.doi.org/10.1136/qshc.7.3.149 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitson A. L., Rycroft-Malone J., Harvey G., McCormack B., Seers K., Titchen A. Evaluating the successful implementation of evidence into practice using the PARiHS framework: Theoretical and practical challenges. Implementation Science. 2008;3:1. doi: 10.1186/1748-5908-3-1. http://dx.doi.org/10.1186/1748-5908-3-1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund A., Michelet M., Kjeken I., Wyller T. B., Sveen U. Development of a person-centred lifestyle intervention for older adults following a stroke or transient ischaemic attack. Scandinavian Journal of Occupational Therapy. 2012;19:140–149. doi: 10.3109/11038128.2011.603353. http://dx.doi.org/10.3109/11038128.2011.603353 . [DOI] [PubMed] [Google Scholar]
- Mesibov G. B., Shea V., Schopler E. The TEACCH approach to autism spectrum disorders. New York: Springer; 2004. [Google Scholar]
- National Institute for Health and Clinical Excellence. Occupational therapy and physical activity interventions to promote the mental wellbeing of older people in primary and residential care. London: Author; 2008. Retrieved from http://www.nice.org.uk/guidance/index.jsp?action=byID&o=11999. [Google Scholar]
- Parham L. D., Roley S. S., May-Benson T. A., Koomar J., Brett-Green B., Burke J. P., Schaaf R. C. Development of a fidelity measure for research on the effectiveness of the Ayres Sensory Integration® intervention. American Journal of Occupational Therapy. 2011;65:133–142. doi: 10.5014/ajot.2011.000745. http://dx.doi.org/10.5014/ajot.2011.000745 . [DOI] [PubMed] [Google Scholar]
- Peters C. Powerful occupational therapists: A community of professionals, 1950–1980. Occupational Therapy in Mental Health. 2011;27(3–4):199–410. http://dx.doi.org/10.1080/0164212X.2011.597328 . [Google Scholar]
- Prizant B. M., Wetherby A. M., Rubin E., Laurent A. C. The SCERTS model: A transactional, family-centered approach to enhancing communication and socioemotional abilities of children with autism spectrum disorder. Infants and Young Children. 2003;16:296–316. http://dx.doi.org/10.1097/00001163-200310000-00004 . [Google Scholar]
- Rogers S. J., Dawson G. Early start Denver model for young children with autism: Promoting language, learning, and engagement. New York: Guilford Press; 2009. [Google Scholar]
- Schopler E. Implementation of TEACCH philosophy. In: Cohen D. J., Volkmar F. R., editors. Handbook of autism and pervasive developmental disorders. 2nd ed. New York: Wiley; 1997. pp. 767–795. [Google Scholar]