Abstract
OBJECTIVES. The level of children’s motor skill proficiency may be an important determinant of their physical activity behaviors. This study assessed the efficacy of an intervention on gross motor skill performance, physical activity, and weight status of preschoolers.
METHOD. The Food Friends: Get Movin’ With Mighty Moves® program was conducted in four Head Start centers. Measurements included the Peabody Developmental Motor Scales, pedometer counts, and body mass index (BMI) z scores.
RESULTS. The intervention led to significant changes in gross motor skills in the treatment group (n = 98) compared with the control group (n = 103) and was a strong predictor of overall gross motor performance (gross motor quotient), locomotor, stability, and object manipulation skills. No intervention effect was found for physical activity levels or weight status.
CONCLUSION. The intervention dose was adequate for enhancing gross motor skill performance but not for increasing physical activity levels or reducing BMI.
MeSH TERMS: body weight; child, preschool; exercise; motor activity; motor skills
Obesity rates in preschool-age children have increased dramatically over recent years. In the United States, 24.4% of children ages 2–5 yr are considered overweight or obese (Ogden, Carroll, & Flegal, 2008). Declining levels of physical activity may play a significant role in the rising childhood obesity rates. Although adults have been shown to overestimate the level of physical activity of youth, most data support the conclusion that the majority of children tend to be physically inactive (Dolinsky, Brouwer, Evenson, Siega-Riz, & Østbye, 2011; Pate, McIver, Dowda, Brown, & Addy, 2008; Williams et al., 2008).
Reasons for low activity levels among preschoolers are not well understood; however, a relationship has been posited between the status of children’s motor skill performance and their levels of physical activity (Williams et al., 2008; Wrotniak, Epstein, Dorn, Jones, & Kondilis, 2006). Several studies have shown that children with poorer motor skill performance were less active than children with better-developed motor skills (Fisher et al., 2005; McKenzie et al., 2002; Williams et al., 2008; Wrotniak et al., 2006). Williams et al. found that children with higher levels of locomotor performance spent significantly more time in both moderate-to-vigorous physical activity and vigorous physical activity and less time in sedentary behaviors than children with lower levels of locomotor performance.
The improvement in motor skills for preschoolers is critical because many children never develop certain mature motor skills and as a result perform poorly as they grow older (Garcia, Garcia, Floyd, & Lawson, 2002). These early failures can damage the child’s self-esteem and lead to avoidance of movement. Children with low motor skills know that they cannot move efficiently and feel awkward and inhibited, leading to decreased movement and physical activity (Garcia et al., 2002). Efforts to enhance motor skill proficiency in young children are warranted because such efforts may lead to increased physical activity levels and enjoyment.
The child care setting holds great potential as a venue for interventions focusing on physical activity and gross motor development (Larson, Ward, Neelon, & Story, 2011). In the United States, an estimated 57% of young children attend center-based child care (National Center for Education Statistics, 2006). Because of the large numbers enrolled, child care centers provide opportunities for children to obtain the necessary amount of physical activity and to reinforce adoption of a physically active lifestyle (Ward, 2010). However, research exploring child care–based obesity prevention strategies is limited at this time (Larson et al., 2011; Ward, Vaughn, McWilliams, & Hales, 2010). Few intervention studies for increasing physical activity or gross motor skills in child care exist; thus, there is a great need for additional intervention research.
The Food Friends: Get Movin’ With Mighty Moves® program was developed to enhance motor skill performance and provide opportunities to increase physical activity offerings in the preschool setting (Bellows, 2007; Bellows, Anderson, Davies, & Kennedy, 2009; Bellows, Anderson, Gould, & Auld, 2008). It was designed by experts in nutrition, occupational therapy, and exercise science. To test the efficacy of the program, we conducted a randomized intervention study in eight Head Start centers. Study objectives were to determine whether physical activity relates to motor skill performance, assess whether children participating in the Mighty Moves intervention improved their gross motor skill performance and physical activity levels, and assess the impact of the Mighty Moves program on the weight status of preschool-age children.
Method
Research Design
Mighty Moves was a randomized intervention study targeting 3- to 5-yr-old children enrolled in eight Head Start centers across rural and urban settings who had previously implemented the Food Friends® Fun With New Foods nutrition program.
Participants
Head Start centers were recruited and randomly assigned to participate in the Mighty Moves intervention or the control condition. Staff and teachers assisted with participant recruitment by providing parents with an informational packet (in English or Spanish) containing study details and consent forms. This research was approved by a university institutional review board.
Instruments
Sociodemographic Variables.
Birth dates were provided on the consent form to calculate the child’s chronological age. Gender and ethnicity were recorded at the time of the on-site assessment, and when necessary, information was confirmed with teachers and center staff.
Anthropometric Measures.
Height was measured using a portable stadiometer (Seca Corp., Hamburg, Germany). Weight was measured using an electronic scale (Lifesource ProFit UC321, Milpitas, CA). Body mass index (BMI), BMI percentiles, and BMI z scores were calculated by EpiInfo (Centers for Disease Control and Prevention [CDC], Atlanta, GA). Children’s weight status was classified using their sex- and age-specific BMI percentile derived from CDC’s growth charts (Kuczmarski et al., 2000).
Peabody Developmental Motor Scales, Second Edition.
The Peabody Developmental Motor Scales, Second Edition (PDMS–2; Folio & Fewell, 2000) is a norm- and criterion-referenced fine and gross motor skill test designed for children from birth through age 5 yr. Reliability and validity of the PDMS–2 are reported in the test manual (Folio & Fewell, 2000). Reliability coefficients for the gross motor scales used in this study were high for content sampling (.89–.96), time sampling (.89–.94), and interrater reliability (.96–.99). Additionally, test–retest reliability on the gross motor scale was high (.98) and was responsive to change (Wang, Liao, & Hsieh, 2006). Content validity was determined to be satisfactory (Folio & Fewell, 2000).
The three subtests composing the gross motor scales (i.e., stability, locomotor, and object manipulation) were conducted. Administration and scoring were carried out according to the standardized methods described in the manual. Testing time averaged 20–25 min. Raw scores for each subtest were calculated and transformed into standard scores. A gross motor quotient (GMQ) using all three subtests was also calculated (Folio & Fewell, 2000).
Pedometers.
Pedometers have been shown to be a valid measure of preschoolers’ physical activity levels, particularly when the goal is to demonstrate relative changes in physical activity (Cardon & De Bourdeaudhuij, 2007; Pate, O’Neill, & Mitchell, 2010). A Walk4Life pedometer (Model W4L Classic; Walk4Life Inc., Plainfield, IL) with safety strap was sent home along with a log to record the number of daily steps. Parents were asked to put the pedometer on the child when the child got out of bed and to take it off when the child went to bed and to record the number of total steps taken each day for 6 days (4 weekdays and 2 weekend days). Mean steps for all 6 days and separate averages for weekdays and weekend days were calculated. Families were compensated $20 for completing the pedometer logs.
Intervention
The Mighty Moves intervention lasted 18 wk and was conducted in the classroom 4 days per week for 15–20 min each day, for a total of 72 lessons. Lessons comprised multiple activities (143 total activities) and were led by the classroom teacher. Each week’s activities focused on a skill or group of skills from one of the three gross motor skill categories: stability (trunk strength), locomotor (running, hopping, skipping), or manipulation (ball skills). Early in each week, children were introduced to a motor skill, and movement concepts were added as the week progressed. Later in the program, skill patterns were incorporated into activities.
In addition to Mighty Moves for intervention classrooms, both intervention and control classrooms implemented Food Friends, a 12-wk nutrition program shown to increase children’s willingness to try new foods (Johnson, Bellows, Beckstrom, & Anderson, 2007). As part of Food Friends, children are introduced to Food Friends characters and learn about and taste new foods. Although the Food Friends characters are used in both the nutrition program and Mighty Moves, they are otherwise two distinct programs.
For the intervention, graphics depicting each of the Food Friends characters participating in different physical activities were developed (Bellows et al., 2009). These activities represented different motor skills, which were presented to children as “mighty moves.” In addition to having a mighty move, each character also had a superpower. Characters introduced gross motor skills and movement concepts and led children on imaginary musical journeys through the town of Healthadelphia®. Materials supporting the lessons, as well as creative themes and concepts, were provided as a kit for each intervention classroom and included a teacher activity binder, a custom music CD, activity mats, flashcards, puppets, scarves, balls, beanbags, ropes, and parent materials (Bellows et al., 2009). Home connection materials were sent home throughout the program, including educational handouts and a copy of the Mighty Moves music CD (Bellows et al., 2011).
All children participated in classroom activities, whereas only children with parent consent participated in the various assessments.
Fidelity
Before the study, both intervention and control teachers were required to attend training on the study protocol. Intervention teachers received additional training on gross motor development and age-appropriate physical activity. Six program surveys were administered (every 3 wk) to ascertain teachers’ fidelity to and impressions of program lessons. Fidelity to lessons was measured using a 5-point Likert scale, with 5 being the most positive response, and an option of “did not do.” Eighteen teachers completed the surveys. The average ranking for all activities was 4.04 (out of 5), and the average percentage of activities conducted was 93.9% (range = 81%–100%).
Data Collection
Data were collected at each center by research staff over a 2-day period for anthropometric and gross motor measures at baseline and immediately after the 18-wk intervention. Before initiating the study, personnel collecting data were trained by the occupational therapist (author Davies) consistent with evaluation criteria established during the pilot phase of this study (Curtis, 2007). During the pilot phase, data collectors performed assessments and their data were compared with an expert’s (Davies’) score. All data collectors were trained until their scores on individual items matched those of the expert. It was not possible to collect interrater reliability data in the community settings; thus, the data collectors were randomly assigned to participants across conditions and sites so that any variability across data collectors’ scores would not systematically influence the results. Follow-up training was conducted as necessary. Because of the nature of community-based research and the need for research staff to play multiple roles, blinding of data collection was not possible.
Data Analysis
Data were analyzed using IBM SPSS Version 19.0 for Windows (IBM, Armonk, NY). Descriptive statistics (percentage, mean, standard deviation) were obtained for demographic, anthropometric, and weight status variables. Independent t tests were conducted, and no significant difference existed at baseline between treatment groups (intervention and control) and geographic locations (urban and rural) for outcome variables. Thus, data for the two geographic groups were collapsed by treatment group. Pearson product–moment correlations were conducted to determine the relationship between physical activity and motor skills. Correlations of .00–.24 were interpreted as representing a weak relationship, .25–.50 as fair, .50–.75 as moderate, and >.75 as good to excellent (Portney & Watkins, 2000).
Several two-factor analyses of variance (ANOVAs) with a within-factor variable (time) with two levels (baseline and posttest) and a between-factor variable (treatment group) with two levels (intervention and control) were used to evaluate the intervention effect on motor skills. When significant interactions occurred, post hoc t tests were used to assess differences between baseline and posttest outcome variables for each group and difference between groups at both time points. A follow-up regression analysis was conducted to examine the intervention effect on motor skills while accounting for the other variables. Two-factor ANOVAs were used to assess a difference in physical activity and weight status between groups (between-factor, intervention and control) across time (within-factor, baseline and posttest). These ANOVAs were repeated using classroom, ethnicity, gender, and age as covariates. BMI z score was also included as a covariate for physical activity.
Results
Participant Demographics
Two hundred seventy-four children and their parents consented to participate in the study at baseline. Baseline data for on-site measures—child weight status and gross motor skills—were collected on 263 children (intervention group, n = 132 across 18 classrooms; control group, n = 131 across 13 classrooms). Posttest data were collected on 201 children, representing 76% retention. Sixty-two children (n = 34 in the treatment group; n = 28 in the control group) were lost to follow-up because they were absent during data collection or were no longer enrolled at the center. Pedometer logs were returned by 182 families at baseline and 101 families at posttest, for a response rate of 68% and 50%, respectively. Demographic characteristics of the 201 participants were 55% boys, 45% girls, 59% Hispanic, and 32% White. All participants were considered to have low socioeconomic status because of their enrollment in Head Start. No significant differences in participant characteristics existed between groups at baseline.
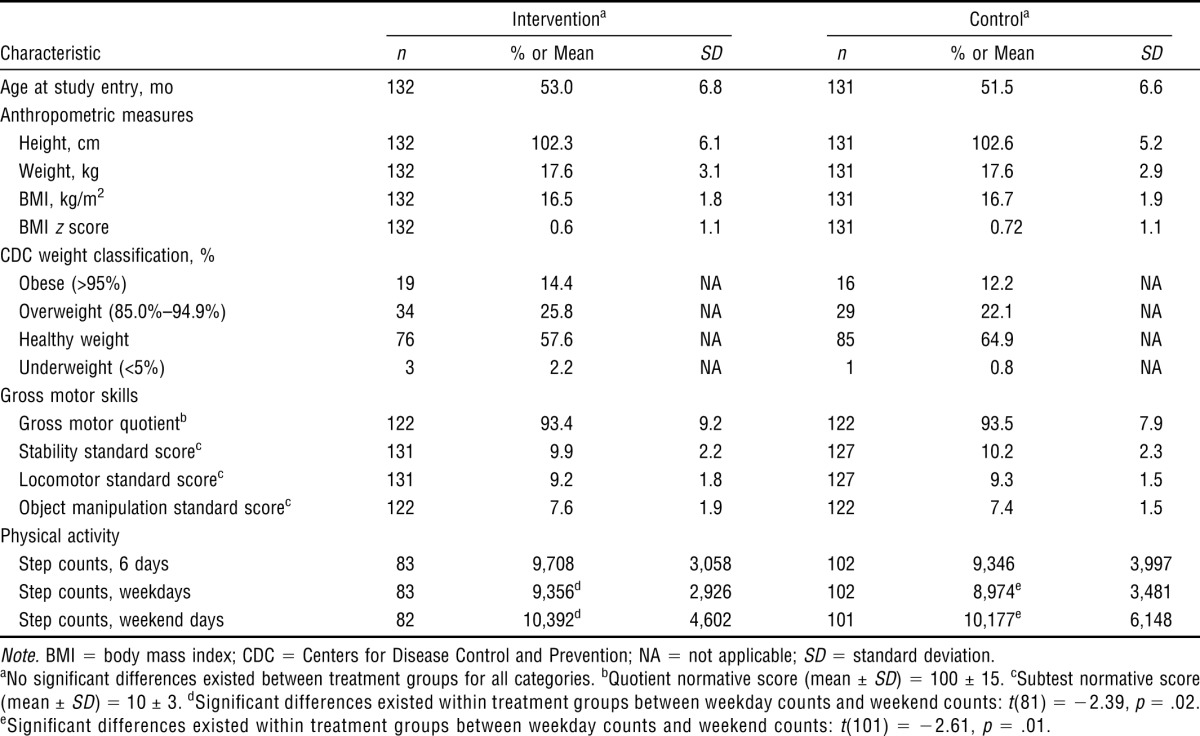
Baseline Data
Anthropometric, gross motor skill, and physical activity baseline data are presented in Table 1. No significant differences were found between the intervention and control groups at baseline.
Table 1.
Child Characteristics at Baseline, by Treatment Group
| Interventiona | Controla | |||||
| Characteristic | n | % or Mean | SD | n | % or Mean | SD |
| Age at study entry, mo | 132 | 53.0 | 6.8 | 131 | 51.5 | 6.6 |
| Anthropometric measures | ||||||
| Height, cm | 132 | 102.3 | 6.1 | 131 | 102.6 | 5.2 |
| Weight, kg | 132 | 17.6 | 3.1 | 131 | 17.6 | 2.9 |
| BMI, kg/m2 | 132 | 16.5 | 1.8 | 131 | 16.7 | 1.9 |
| BMI z score | 132 | 0.6 | 1.1 | 131 | 0.72 | 1.1 |
| CDC weight classification, % | ||||||
| Obese (>95%) | 19 | 14.4 | NA | 16 | 12.2 | NA |
| Overweight (85.0%–94.9%) | 34 | 25.8 | NA | 29 | 22.1 | NA |
| Healthy weight | 76 | 57.6 | NA | 85 | 64.9 | NA |
| Underweight (<5%) | 3 | 2.2 | NA | 1 | 0.8 | NA |
| Gross motor skills | ||||||
| Gross motor quotientb | 122 | 93.4 | 9.2 | 122 | 93.5 | 7.9 |
| Stability standard scorec | 131 | 9.9 | 2.2 | 127 | 10.2 | 2.3 |
| Locomotor standard scorec | 131 | 9.2 | 1.8 | 127 | 9.3 | 1.5 |
| Object manipulation standard scorec | 122 | 7.6 | 1.9 | 122 | 7.4 | 1.5 |
| Physical activity | ||||||
| Step counts, 6 days | 83 | 9,708 | 3,058 | 102 | 9,346 | 3,997 |
| Step counts, weekdays | 83 | 9,356d | 2,926 | 102 | 8,974e | 3,481 |
| Step counts, weekend days | 82 | 10,392d | 4,602 | 101 | 10,177e | 6,148 |
Note. BMI = body mass index; CDC = Centers for Disease Control and Prevention; NA = not applicable; SD = standard deviation.
No significant differences existed between treatment groups for all categories.
Quotient normative score (mean ± SD) = 100 ± 15.
Subtest normative score (mean ± SD) = 10 ± 3.
Significant differences existed within treatment groups between weekday counts and weekend counts: t(81) = −2.39, p = .02.
Significant differences existed within treatment groups between weekday counts and weekend counts: t(101) = −2.61, p = .01.
Relationship Between Physical Activity and Gross Motor Skills
A significant relationship between physical activity measured by the average number of steps recorded across weekdays and weekend days and gross motor skills (i.e., GMQ) was found before the intervention for all children, r(170) = .163, p = .034. A significant relationship also existed between physical activity and the locomotor subtest standard score, r(170) = .182, p = .014. Significant relationships between physical activity and the other two subtests, stability and manipulation skills, were not found. When examining physical activity separately for steps on weekdays and weekend days, the relationship with GMQ, r(168) = .194, p = .012, and locomotor subscale, r(178) = .234, p = .002, existed only on weekend days, but not on weekdays. For the posttest data, no significant relationships were found between physical activity and motor skills.
Gross Motor Skills
Children receiving the Mighty Moves intervention demonstrated significant changes in gross motor skills when compared with the control group, shown by analyses of variance. For the PDMS–2 GMQ, the ANOVA resulted in a significant main effect for time, F(1, 186) = 14.79, p < .0005; a significant interaction between time and treatment group, F(1, 186) = 22.62, p < .0005; and a significant main effect for treatment group, F(1, 186) = 7.89, p = .006. For the stability subtest of the PDMS–2, the ANOVA showed a significant interaction between time and treatment group, F(1, 194) = 17.73, p < .0005, and a significant main effect for treatment group, F(1, 194) = 4.85, p = .032. The main effect for time was not significant, F(1, 194) = 0.45, p = .501. For the locomotor subtest of the PDMS–2, the ANOVA showed a significant main effect for time, F(1, 194) = 28.87, p < .0005, and a significant interaction between time and treatment group, F(1, 194) = 10.44, p = .001. The main effect for treatment group was not significant, F(1, 194) = 2.94, p = .089. For the manipulation subtest of the PDMS–2, the ANOVA resulted in a significant main effect for time, F(1, 186) = 9.47, p = .002; a significant interaction between time and treatment group, F(1, 186) = 8.26, p = .005; and a significant main effect for treatment group, F(1, 186) = 8.71, p = .004.
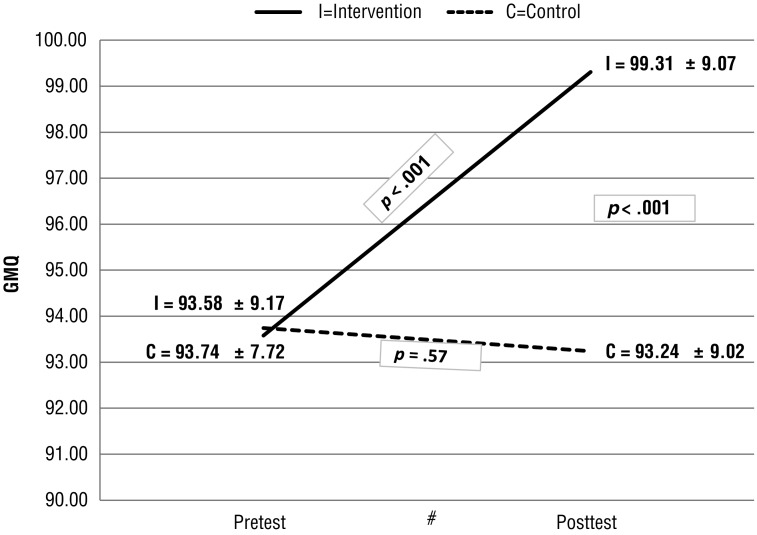
Post hoc t tests further illuminated the significant increase in gross motor skills for children participating in the Mighty Moves program, including a significant increase in GMQ (mean difference from baseline to posttest = 5.73; Figure 1). Similar significant increases were found for each of the three motor subtests in the intervention group but not the control group. A decrease in GMQ was found in the control group (mean difference = −0.50) as well as a significant decrease in stability skills (mean difference = −0.63). These changes are not indicative of a decrease in skill but rather a potentially slower rate of motor development when compared with normative data.
Figure 1.
Pretest-to-posttest change in gross motor quotient (GMQ), by treatment condition.
Note. No significant differences existed between groups at pretest in quotient normative score. Mean ± standard deviation = 100 ± 15. Higher scores reflect more advanced gross motor skills.
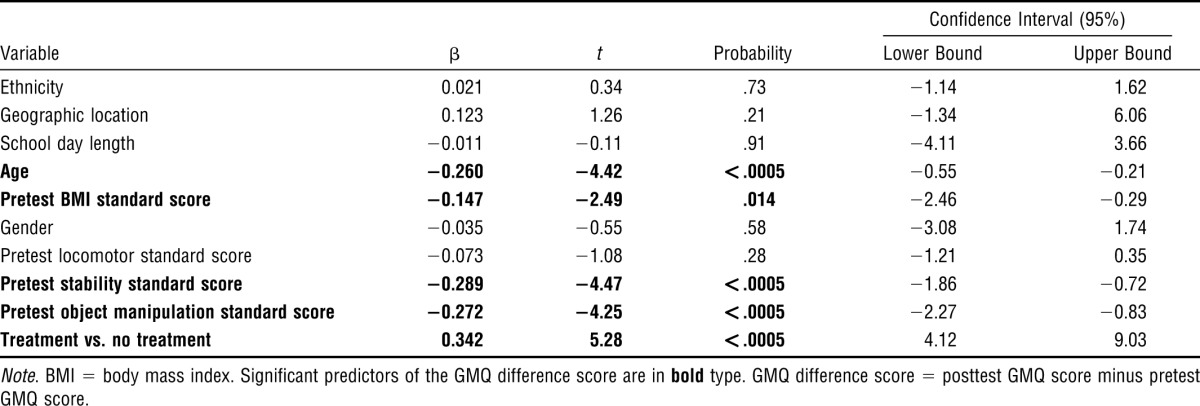
To demonstrate the effects of the intervention, a multivariate approach was used to understand the interrelationship of the variables. Four regression analyses were conducted to examine what variables predicted the change in scores from pretest to posttest for the GMQ, locomotor, stability, and object manipulation subscales. In the first step of the analyses, control variables that were not expected to affect the development of motor skills were entered (i.e., ethnicity, geographic location, length of school day). Variables that were likely to relate to the development of motor skills were entered in the second step (i.e., age, gender, pretest BMI standard score, pretest scores for each of the three subscales of the PDMS–2). Finally, the treatment variable (intervention vs. control) was entered in the third step. For the GMQ, all variables together accounted for 38.2% of the variance of the GMQ difference score, F(10, 177) = 12.58, p < .0005. Intervention alone accounted for 9.2% of the variance accounted for in the GMQ difference score, F(1, 177) = 27.92, p < .0005. The treatment variable had the largest β weight in predicting the change score in overall motor skill performance (i.e., GMQ; Table 2). Age, pretest BMI standard score, and pretest scores for the stability and object manipulation subscales, in addition to the intervention effect, were significant predictors of the changed score.
Table 2.
Summary of Regression Analysis for Variables Predicting Gross Motor Quotient (GMQ) Difference Score
| Confidence Interval (95%) |
|||||
| Variable | β | t | Probability | Lower Bound | Upper Bound |
| Ethnicity | 0.021 | 0.34 | .73 | −1.14 | 1.62 |
| Geographic location | 0.123 | 1.26 | .21 | −1.34 | 6.06 |
| School day length | −0.011 | −0.11 | .91 | −4.11 | 3.66 |
| Age | −0.260 | −4.42 | <.0005 | −0.55 | −0.21 |
| Pretest BMI standard score | −0.147 | −2.49 | .014 | −2.46 | −0.29 |
| Gender | −0.035 | −0.55 | .58 | −3.08 | 1.74 |
| Pretest locomotor standard score | −0.073 | −1.08 | .28 | −1.21 | 0.35 |
| Pretest stability standard score | −0.289 | −4.47 | <.0005 | −1.86 | −0.72 |
| Pretest object manipulation standard score | −0.272 | −4.25 | <.0005 | −2.27 | −0.83 |
| Treatment vs. no treatment | 0.342 | 5.28 | <.0005 | 4.12 | 9.03 |
Note. BMI = body mass index. Significant predictors of the GMQ difference score are in bold type. GMQ difference score = posttest GMQ score minus pretest GMQ score.
For the locomotor subscale, all variables entered accounted for 25% of the variance in the locomotor difference score, F(10, 177) = 7.25, p < .0005. Intervention alone accounted for 2% of the variance in the locomotor difference score, F(1, 177) = 5.10, p < .025. Age and locomotor score at pretest also were significant predictors of change in the locomotor score. All variables accounted for 57.2% of the variance in the stability subscale, F(10, 177) = 25.96, p < .0005, with intervention alone accounting for 4.4% of the variance, F(1, 177) = 19.25, p < .0005.
Additional variables that predicted the change score in the stability subscale were age, initial BMI standard score, and pretest scores on the locomotor and stability subscales. For the object manipulation subscale, all variables accounted for 43.5% of the variance of the difference score for the object manipulation subscale, F(10, 177) = 14.84, p < .0005. Intervention alone accounted for 7.3% of the variance, F(1, 177) = 23.66, p < .0005. Intervention, along with the length of school day, gender, and pretest scores on the stability and object manipulation subscales predicted the change score in object manipulation. Girls made more improvement in the objective manipulation skills compared with boys. No other gender effects on motor skill performance were found.
Significant age effects were demonstrated in the post hoc examination of children receiving the intervention. The 3-yr-olds demonstrated a significant improvement in GMQ, locomotor, and stability difference scores, whereas the 5-yr-olds did not. Related to BMI prescore as predicting change in GMQ and stability scores, regression analysis revealed that the lower the child’s BMI at the outset of the study, the more changes he or she made in motor skill performance compared with children with high BMIs. Moreover, healthy-weight1 children had significant increases in all four motor skill categories demonstrated by post hoc t tests, whereas overweight and obese children had significant improvements only in locomotor skills.
Physical Activity
The mean daily step count at baseline was 9,509 (standard deviation = 3,599). No significant differences were found between treatment groups in gender, ethnicity, weight status, and age. Weekday step counts were found to be significantly lower than weekend counts for the treatment group, t(81) = −2.39, p = .02, and for the control group, t(101) = −2.61, p = .01. ANOVAs revealed no intervention effect for physical activity levels from baseline to posttest for total, weekday, or weekend steps. When covariates were used, the results also were not significant.
Child Weight Status
ANOVAs indicated nonsignificant differences between treatment groups in BMI and BMI z score, whether controlling for covariates or not. Further analysis using post hoc t tests examining changes from baseline to posttest in the treatment group by age and weight status showed no significant increases in weight gain (BMI and BMI z score) for 3-yr-olds and overweight and obese children. Significant increases for 4- and 5-yr-olds and for healthy-weight children were seen.
Discussion
The Mighty Moves intervention demonstrated significant changes in gross motor skills among preschoolers. No significant changes occurred in physical activity levels or weight status. These findings suggest that the 18-wk dose (15–20 min, 4 days per week) of classroom programming was adequate for enhancing gross motor skill performance but not for increasing physical activity levels or reducing weight status.
Few intervention studies have examined motor skill outcomes in the child care setting (Logan, Robinson, Wilson, & Lucas, 2012). In a review by Ward et al. (2010) of child care–based physical activity interventions, only five studies targeting motor skill outcomes were identified. All five of the studies had positive effects on some aspect of children’s motor skills; however, only one, the Movement and Activity Glasgow Intervention in Children (MAGIC) study conducted by Reilly et al. (2006), had a strong research design with a large number of participants. Findings from the MAGIC study, like those of our Mighty Moves study, demonstrated improvements in preschoolers’ motor skills but not in BMI or physical activity levels (Reilly et al., 2006).
In Ward et al.’s (2010) review, it was suggested that 90 min of weekly structured physical activity seems to be sufficient to achieve improvements in motor skills; however, a greater dose may be required to increase physical activity levels in children, possibly 30–45 min per day, 5–6 days per week. The dose of structured physical activity provided by Mighty Moves, 60–80 min per week, was sufficient to achieve improvements in gross motor performance and feasible for teachers to incorporate into lesson plans as demonstrated by high fidelity reports.
Studies have shown that children with poorer motor skills are less active than children with better-developed motor skills (Fisher et al., 2005; McKenzie et al., 2002; Williams et al., 2008; Wrotniak et al., 2006). Thus, the level of motor skill performance may be an important factor in promoting a physically active lifestyle in preschool children. This Mighty Moves study demonstrated a significant relationship between physical activity and the GMQ and the locomotor subtest score in preschoolers at baseline. However, increases in motor skill performance did not result in increases in physical activity levels after an 18-wk intervention. Improvements in motor skill performance may have an impact on physical activity in the long term but not the short term.
In terms of weight status, this study did not see significant reductions in BMI z scores. Because obesity is a multifaceted issue, it is unlikely that enhancing gross motor skills alone would have an impact on weight status. Weight status did, however, have an impact on gross motor skill performance. Our regression analyses demonstrate that children with lower BMI z scores made more improvements in motor skill performance than children with higher BMI z scores. Nervik, Martin, Rundquist, and Cleland (2011), who also used the PDMS–2, found a significant relationship between high BMI and low gross motor skills. Overweight and obese children with low motor skills may, over time, be less physically active than their healthy-weight counterparts and at risk for further weight gain.
This study contributes to the literature because of the limited number of published physical activity interventions conducted with preschool-age children (Ward et al., 2010). Other strengths include the use of a norm- and criterion-referenced measure of all major gross motor skills, an objective measure of physical activity, and an intervention-based design to examine changes in motor skills performance and physical activity. Finally, classroom teachers facilitated program activities on a daily basis. The fidelity of program implementation was high; thus, the use of classroom teachers is a strategy that allows for future sustainability of the program. The Mighty Moves program is consistent with the recommendation to embed interventions within existing community organizations (Ziviani, Poulsen, & Hansen, 2009).
Limitations
Although the PDMS–2 test is a valid and reliable tool for young children from birth to age 5, we may have seen a ceiling effect in some older children. Thus, the sensitivity to detect change over the intervention period, especially for the 5-yr-olds, may have been diminished. Second, with the use of pedometers, reporting bias may exist, and because the pedometers could not be sealed, there was a chance of premature resetting. However, no evidence in the literature suggests that children react to pedometers (e.g., by resetting; Pate et al., 2010). Next, because this study was conducted in Head Start centers with a low-income, high-Hispanic population, data presented here may not be generalizable to preschoolers or child care centers as a whole. Finally, although the study population is representative of the state Head Start population, some selection bias as to who enrolled in the study may have existed.
Implications for Occupational Therapy Practice
Occupational therapy practitioners can play an important role in addressing childhood obesity. Results of this study provide the following examples of how occupational therapists can address childhood obesity:
Occupational therapists can be instrumental in developing and implementing physical activity interventions.
Occupational therapists can provide training and support for teachers and parents to engage children in physical activity throughout the day.
Interdisciplinary teams of professionals working to enhance healthy lifestyles in children should include occupational therapists along with nutrition and exercise specialists.
Conclusion
This study demonstrated that children who participated in the Mighty Moves program showed an increase in motor skill performance, but participation did not affect child factors such as BMI. Longitudinal studies are needed to see if improvements in gross motor skill performance in preschool translate to increased physical activity levels later in childhood.
Acknowledgments
The project was supported by National Research Initiative Grant 2005-35215-15386 from the U.S. Department of Agriculture’s Cooperative State Research, Education, and Extension Service and by the U.S. Department of Health and Human Services Office of Head Start. We thank the participating Head Start centers, those who assisted with data collection, Bill Gavin for his statistical guidance, and The SHiFT Agency for their work on this project.
Footnotes
The CDC (2011) defines healthy weight for children as having BMI from the 5th to less than the 85th percentile relative to children of the same sex and age.
Contributor Information
Laura L. Bellows, Laura L. Bellows, PhD, MPH, RD, is Assistant Professor and Extension Specialist, Department of Food Science and Human Nutrition, Colorado State University, Fort Collins, CO 80523-1571; laura.bellows@colostate.edu
Patricia L. Davies, Patricia L. Davies, PhD, OTR, is Professor, Department of Occupational Therapy, Colorado State University, Fort Collins
Jennifer Anderson, Jennifer Anderson, PhD, RD, is Professor and Extension Specialist, Department of Food Science and Human Nutrition, Colorado State University, Fort Collins.
Catherine Kennedy, Catherine Kennedy, PhD, is Associate Professor, Department of Health and Exercise Science, Colorado State University, Fort Collins.
References
- Bellows L. Development and evaluation of Food Friends Get Movin’ With Mighty Moves: A physical activity program to prevent obesity in low-income preschoolers. Fort Collins: Colorado State University; 2007. Unpublished doctoral dissertation. [Google Scholar]
- Bellows L., Anderson J., Davies P., Kennedy C. Integration of social marketing elements in the design of a physical activity program for preschoolers. Social Marketing Quarterly. 2009;15:2–21. http://dx.doi.org/10.1080/15245000802695190 . [Google Scholar]
- Bellows L., Anderson J., Gould S. M., Auld G. Formative research and strategic development of a physical activity component to a social marketing campaign for obesity prevention in preschoolers. Journal of Community Health. 2008;33:169–178. doi: 10.1007/s10900-007-9079-z. http://dx.doi.org/10.1007/s10900-007-9079-z . [DOI] [PubMed] [Google Scholar]
- Bellows L., Silvernail S., Caldwell L., Bryant A., Kennedy C., Davies P., Anderson J. Parental perception on the efficacy of a physical activity program for preschoolers. Journal of Community Health. 2011;36:231–237. doi: 10.1007/s10900-010-9302-1. http://dx.doi.org/10.1007/s10900-010-9302-1 . [DOI] [PubMed] [Google Scholar]
- Cardon G., De Bourdeaudhuij I. Comparison of pedometer and accelerometer measures of physical activity in preschool children. Pediatric Exercise Science. 2007;19:205–214. doi: 10.1123/pes.19.2.205. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. About BMI for children and teens. 2011. Retrieved August 28, 2012, from www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html.
- Curtis J. Relationship of the environment, motor skills, and physical activity and the impact on obesity in preschool-aged children: A pilot study. Fort Collins: Colorado State University; 2007. [Google Scholar]
- Dolinsky D. H., Brouwer R. J., Evenson K. R., Siega-Riz A. M., Østbye T. Correlates of sedentary time and physical activity among preschool-aged children. Preventing Chronic Disease. 2011;8:A131. [PMC free article] [PubMed] [Google Scholar]
- Fisher A., Reilly J. J., Kelly L. A., Montgomery C., Williamson A., Paton J. Y., Grant S. Fundamental movement skills and habitual physical activity in young children. Medicine and Science in Sports and Exercise. 2005;37:684–688. doi: 10.1249/01.mss.0000159138.48107.7d. http://dx.doi.org/10.1249/01.MSS.0000159138.48107.7D . [DOI] [PubMed] [Google Scholar]
- Folio M. R., Fewell R. R. Peabody Developmental Motor Scales. 2nd ed. Austin, TX: Pro-Ed; 2000. [Google Scholar]
- Garcia C., Garcia L., Floyd J., Lawson J. Improving public health through early childhood movement programs. Journal of Physical Education, Recreation and Dance. 2002;73:27–31. [Google Scholar]
- Johnson S. L., Bellows L., Beckstrom L., Anderson J. Evaluation of a social marketing campaign targeting preschool children. American Journal of Health Behavior. 2007;31:44–55. doi: 10.5555/ajhb.2007.31.1.44. http://dx.doi.org/10.5993/AJHB.31.1.5 . [DOI] [PubMed] [Google Scholar]
- Kuczmarski R. J., Ogden C. L., Grummer-Strawn L. M., Flegal K. M., Guo S. S., Wei R., …, Johnson C. L. CDC growth charts: United States. Advance Data. 2000;314:1–27. [PubMed] [Google Scholar]
- Larson N., Ward D. S., Neelon S. B., Story M. What role can child care settings play in obesity prevention? A review of the evidence and call for research efforts. Journal of the American Dietetic Association. 2011;111:1343–1362. doi: 10.1016/j.jada.2011.06.007. http://dx.doi.org/10.1016/j.jada.2011.06.007 . [DOI] [PubMed] [Google Scholar]
- Logan S. W., Robinson L. E., Wilson A. E., Lucas W. A. Getting the fundamentals of movement: A meta-analysis of the effectiveness of motor skill interventions in children. Child: Care, Health and Development. 2012;38:305–315. doi: 10.1111/j.1365-2214.2011.01307.x. http://dx.doi.org/10.1111/j.1365-2214.2011.01307.x . [DOI] [PubMed] [Google Scholar]
- McKenzie T. L., Sallis J. F., Broyles S. L., Zive M. M., Nader P. R., Berry C. C., Brennan J. J. Childhood movement skills: Predictors of physical activity in Anglo American and Mexican American adolescents. Research Quarterly for Exercise and Sport. 2002;73:238–244. doi: 10.1080/02701367.2002.10609017. [DOI] [PubMed] [Google Scholar]
- National Center for Education Statistics. Table 45. Child care arrangements of 3- to 5-year-old children who are not yet in kindergarten, by age and race/ethnicity: Various years, 1991 through 2005. Digest of Education Statistics. 2006 Retrieved December 12, 2010, from http://nces.ed.gov/programs/digest/d09/tables/dt09_045.asp. [Google Scholar]
- Nervik D., Martin K., Rundquist P., Cleland J. The relationship between body mass index and gross motor development in children aged 3 to 5 years. Pediatric Physical Therapy. 2011;23:144–148. doi: 10.1097/PEP.0b013e318218d356. http://dx.doi.org/10.1097/PEP.0b013e318218d356 . [DOI] [PubMed] [Google Scholar]
- Ogden C. L., Carroll M. D., Flegal K. M. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–2405. doi: 10.1001/jama.299.20.2401. http://dx.doi.org/10.1001/jama.299.20.2401 . [DOI] [PubMed] [Google Scholar]
- Pate R. R., McIver K., Dowda M., Brown W. H., Addy C. Directly observed physical activity levels in preschool children. Journal of School Health. 2008;78:438–444. doi: 10.1111/j.1746-1561.2008.00327.x. http://dx.doi.org/10.1111/j.1746-1561.2008.00327.x . [DOI] [PubMed] [Google Scholar]
- Pate R. R., O’Neill J. R., Mitchell J. Measurement of physical activity in preschool children. Medicine and Science in Sports and Exercise. 2010;42:508–512. doi: 10.1249/MSS.0b013e3181cea116. [DOI] [PubMed] [Google Scholar]
- Portney L. G., Watkins M. P. Foundations of clinical research. 2nd ed. Upper Saddle River, NJ: Prentice Hall Health; 2000. [Google Scholar]
- Reilly J. J., Kelly L., Montgomery C., Williamson A., Fisher A., McColl J. H., …, Grant S. Physical activity to prevent obesity in young children: Cluster randomised controlled trial. BMJ. 2006;333:1041. doi: 10.1136/bmj.38979.623773.55. http://dx.doi.org/10.1136/bmj.38979.623773.55 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H. H., Liao H. F., Hsieh C. L. Reliability, sensitivity to change, and responsiveness of the Peabody Developmental Motor Scales–Second Edition for children with cerebral palsy. Physical Therapy. 2006;86:1351–1359. doi: 10.2522/ptj.20050259. http://dx.doi.org/10.2522/ptj.20050259 . [DOI] [PubMed] [Google Scholar]
- Ward D. S. Physical activity in young children: The role of child care. Medicine and Science in Sports and Exercise. 2010;42:499–501. doi: 10.1249/MSS.0b013e3181ce9f85. [DOI] [PubMed] [Google Scholar]
- Ward D. S., Vaughn A., McWilliams C., Hales D. Interventions for increasing physical activity at child care. Medicine and Science in Sports and Exercise. 2010;42:526–534. doi: 10.1249/MSS.0b013e3181cea406. [DOI] [PubMed] [Google Scholar]
- Williams H. G., Pfeiffer K. A., O’Neill J. R., Dowda M., McIver K. L., Brown W. H., Pate R. R. Motor skill performance and physical activity in preschool children. Obesity. 2008;16:1421–1426. doi: 10.1038/oby.2008.214. http://dx.doi.org/10.1038/oby.2008.214 . [DOI] [PubMed] [Google Scholar]
- Wrotniak B. H., Epstein L. H., Dorn J. M., Jones K. E., Kondilis V. A. The relationship between motor proficiency and physical activity in children. Pediatrics. 2006;118:e1758–e1765. doi: 10.1542/peds.2006-0742. [DOI] [PubMed] [Google Scholar]
- Ziviani J., Poulsen A., Hansen C. Movement skills proficiency and physical activity: A case for Engaging and Coaching for Health (EACH)–Child. Australian Occupational Therapy Journal. 2009;56:259–265. doi: 10.1111/j.1440-1630.2008.00758.x. [DOI] [PubMed] [Google Scholar]