Abstract
Aim:
The aim of our study was to evaluate the advantages and disadvantages of 3D plating system in the treatment of mandibular fractures.
Patients and Methods:
20 mandibular fractures in 18 patients at various anatomic locations and were treated by open reduction and internal fixation using 3D plates. All patients were followed at regular intervals of 4th, 8th and 12th weeks respectively. Patients were assessed post-operatively for lingual splay and occlusal stability. The incidence of neurosensory deficit, infection, masticatory difficulty, non-union, malunion was also assessed.
Results:
A significant reduction in lingual splay (72.2%) and occlusal stability (72.2%) was seen. The overall complication rate was (16.6%) which included two patients who developed post-operative paresthesia of lip, three patients had infection and two cases of masticatory difficulty which later subsided by higher antibiotics and 4 weeks of MMF. No evidence of non-union, malunion was noted.
Conclusion:
A single 3D 2 mm miniplate with 2 mm × 8 mm screws is a reliable and an effective treatment modality for mandibular fracture.
Keywords: 3D plates, mandible fractures, miniplates, lingual splay
Several techniques for treatment of mandibular fracture have evolved significantly in the past decade. From the time of hippocrates, many different techniques for treating mandibular fractures have been described the principle of which has always been repositioning and immobilization of the bony fragments. However, during the past 50 years, perfection of anesthetic and radiographic methods, introduction of antibiotics, specially designed instruments, and advances in biomaterials have allowed maxillofacial surgeons to improve outcomes of treatment of mandibular fracture while reducing morbidity.
Over the years, the management of trauma has evolved from various forms of splinting to circum mandibular wiring, extra oral pins and semi rigid fixation with transosseus wiring followed by rigid fixation technique, which has lately given way to semi - rigid fixation with miniplate (Champy et al.).[1] The currently used conventional miniplate techniques require Maxillomandibular fixation for a short period and are unable to render 3D stability at the fracture site. Farmand, Dupoirieux (1992)[2] presented a new system of plates made of titanium (3D plates). The quadrangular geometry of the plate assured good stability in three dimensions of the space. Easy use, good resistance against torque and compact form of the plate were some of the advantages.
A major breakthrough in the field was achieved when Mostafa Farmand (1992)[3] developed a new miniplate system, which takes advantage of the bio-geometry to provide stable fixation and he called it a “3D plating system”. The shortcomings of rigid and semi rigid fixation led to the development of 3D miniplates,[4] consisting of 2 × 4-hole miniplates joined by four interconnecting cross struts. The 3D plating systems are based on the principle of obtaining support through geometrically stable configuration. The quadrangle geometry of plate assures a good stability in three dimensions of fracture, since it offers good resistance against torque forces. Lai (1997)[5] operated on 30 patients with maxillo-mandibular fracture using 3D titanium miniplates system. He was of the opinion that the internal rigid fixation by 3D titanium miniplates is a promising method of treating fractures of maxilla and is better tolerated by the patient and technically easy for the surgeon.
Patients and Methods
20 mandibular fractures in 18 patients treated in our Department of Oral and Maxillo Facial Surgery, Vinayaka Mission’s Sankarachariyar Dental College during April 2007-April 2008.
Ages of the patients included in the study were from 20 years to 40 years. Both sexes were included and patients had no other associated fractures. Anatomical distribution of fracture consisted of nine parasymphysis, two symphysis, seven angle, two body. All patients who did not meet these criteria were excluded from the study.
All the patients were operated under general anesthesia via naso-tracheal intubation Pre-operative arch bars or ivy loops were placed. An intraoral mucosal incision/extra oral incision were made depending upon the anatomical location of fracture. Extraction of teeth in line of fracture, included impacted third molars, was performed if indicated. The fracture fragments were reduced in accurate anatomic pretraumatic occlusion state by open method and internal fixation was done using 3D 2.0-mm stainless steel miniplate, and 2 mm × 8 mm screws [Figure 1]. The intra oral incision sites were closed with resorbable sutures and same for extra oral incisions. All patients were given intravenous antibiotics from the time of admission until discharge. On discharge, patients were prescribed a 5-7-day course of oral antibiotics All patients were instructed to continue on soft diet for 4 weeks. Patients were observed for post-operative complication like Paresthesia, infection, masticatory difficulty, nonunion and malunion. The following parameters were observed and recorded:
Figure 1.

3D plate fixation of mandibular fracture
Case history record
A standard proforma was used to collect necessary information regarding each case.
Photographic records
Pre-operative, intra-operative and post-operative photographs were made.
Radiographic record
Pre-operative panoramic view and mandibular occlusal view were done to evaluate the site and type of fracture.
Immediate post-operative panoramic and occlusal view was taken to evaluate the fracture reduction and placements of plates and lingual splay.
Follow up panoramic view and occlusal radiographs were taken at 12th week of post-operative healing process.
Post-operative evaluation
Assesment of occlusal stability and lingual splaying
-
The occlusion achieved after fixation of mandibular fracture is recorded and is evaluated for change and stability during the first, second, fourth and 12th weeks following surgery. Occlusal score proforma is given to operative surgeon who gives score accordingly:
−1 - Complete bilateral loss of occlusal contact of molars or cross bite or open bite.
0 - Unilateral loss of molar relationship.
+1 - No/minimal loss of molar relationship.
Patient is questioned about symptoms of possible complications and clinically evaluated post-operatively in the first, second, fourth and 12th weeks following surgery and details were recorded. The amount of mouth opening and patient’s ability to return to normal activities were recorded.
-
b
The amount of reduction of lingual splay is evaluated by the operating surgeon using occlusal radiographs taken pre-operatively and 3rd post-operative day. The score for lingual splay evaluation is given as follows:
−1 - There is increase in lingual splay.
0 - Minimal/no change in lingual splay.
+1 - Significant reduction in lingual splay.
Results
This study consisted of eighteen patients who had sustained mandibular fractures at various anatomic locations and were treated by open reduction and internal fixation using 3D plates in Vinayaka Missions Sankarachariyar Dental College between April 2007 and April 2008.They underwent clinical examination and radiographic examination. The following data were collected and recorded.
Table 1 shows the scores of lingual splay evaluation and occlusal stability out of the total 18 patients, 13 patients (72.2%) showed significant reduction in lingual splay. three patients (16.6%) showed minimal or no change in lingual splay reduction post-operatively and two patients, (11.1%) had increase in lingual splay was recorded. Evaluation of occlusal stability showed that occlusion was stable with no or minimal loss of molar relationship in 13 out of 18 patients (72.2%). Three patients (16.6%) showed ipsilateral loss of molar relationship and two cases (11.1%) complete bilateral loss of molar relation.
Table 1.
Lingual splay evaluation and occlusal stability scores
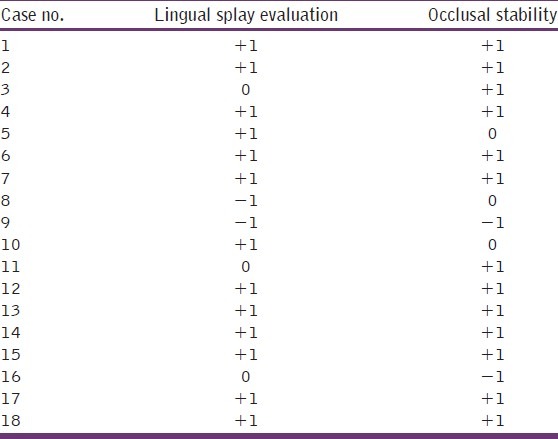
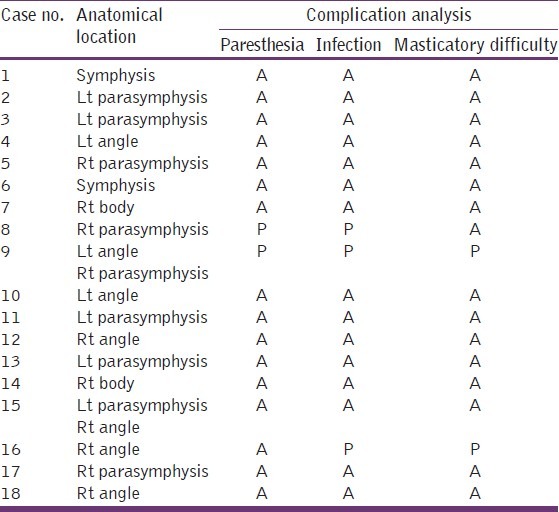
Table 2 shows the post-operative complications encountered in the present study at the end of 4th week. None of the patients complained of difficulty in mouth opening. Two patients (11.1%) complained of masticatory difficulty and both these patient showed bilateral loss of molar relation along with infection. Two patients (11.1%) developed paresthesia of lower lip. Both these cases were associated with infection. Three patients (16.6%) developed infection post-operatively and they were managed by higher antibiotics and Maxillomandibular fixation using arch bar for a period of 4 weeks.
Table 2.
Complication analysis(4th week review)
Discussion
The most common cause of fracture was a result of road traffic accident accounting for 61.1%. The next common etiology of fracture was inter-personal violence accounting for the remaining 38.8% of total cases. This was similar to the study by Fridrich et al.,[6] The anatomical distribution of fracture was as follows: Parasymphysis fracture (38.8%), Symphysis (11.1%), Angle (27.7%), Body (11.1%), Angle with Parasymphysis (11.1%) which was also seen in the study reported by Marisa Aparecida Cabrini Gabrielli et al.[7]
Mostafa Farmand[3] stated that stable plate osteosynthesis has become an indispensable component of craniomaxillofacial surgery in treatment of fractures. So compression plate fixations in craniomaxillofacial surgery are nowadays replaced more and more by functionally oriented miniplating system. The ideal miniplate should resist forces depending on the location and be biocompatible and especially easily adaptable, without dislocation of the fragments. These points are influenced by form, size, and material of the plates. Mostafa Farmand introduced new 3D plating system in which stability of the 3D plate is achieved by its configuration, not by thickness or length. These unique plates are composed of linear, square or rectangular units and may theoretically provide increased torsional stability. We typically use these plates for symphysis fractures, which are under a greater degree of torsional strain than other areas of the mandible.
We evaluated the lingual splay of the fractured mandible using pre- and post-operative occlusal radiographs as was done by Claude Guimond.[8] Post-operative occlusal radiographs were taken on the 3rd post-operative day. In 13 out of total 18 patients (72.2%) significant reduction in lingual splay was observed. Three patients (16.6%) showed minimal or no change in lingual splay reduction. Two patients showed (11.1%) increase in lingual splay. Both of the patients who showed an increase in lingual splay subsequently developed infection and had complaints of persistent post-operative paresthesia. Additionally infection was also seen in another one case that later developed loss of occlusion bilaterally. All the three patients with post-operative infection were managed by higher antibiotics (C. amoxycillin 500 mg + cloxacillin 500 mg, T. Metronidazole thrice-daily/tid). One patient was surgically treated by incision and drainage. All the three patients were treated with additional Maxillomandibular fixation for a period of four weeks. These patients who complained of paresthesia of lower lip recovered fully in 6 weeks.
Occlusal stability was evaluated for change and stability in the first, second, fourth and 12th weeks following surgery. The occlusion achieved was stable in 13 (72.2%) with no or minimal loss of molar relationship and three patients (16.6%) had ipsilateral loss of molar relationship, two cases (11.1%), had bilateral loss of molar relation was. Both of the patients had post-operative infection. One of the patient′s occlusal radiographs showed increase in lingual splay post-operatively. Both of them complained of masticatory difficulty. They were treated by intermaxillary fixation for 4 weeks. The common complications of semi-rigid fixation as stated by Winstanley, et al.[9] were paresthesia of lip, infection, malunion, non-union, occlusal deformity. Our patients were reviewed by radiographic examination on 3rd post surgical day using occlusal radiograph and panoramic views.
The overall complication rate was 16.6%. They were reviewed in the 1st, 2nd, 4th and 12th weeks following surgery and details were recorded. The complications we observed were paresthesia of lip, infection, loss of occlusal stability. Infection was the most common complication seen in 3 out of 18 patients (16.6%). Paresthesia of lip was observed in 2 out of 18 patients accounting for (11.1%). Loss of occlusal stability was seen in two cases, which resulted in patient complaining of masticatory difficulty. This was seen in (11.1%) of all patient included in our study.
Conclusion
In the present study, 18 patients who sustained mandibular fractures were treated with 3D stainless steel mini plates to evaluate the clinical usefulness of these miniplates. The surgical technique and instrumentation used in this study were in accordance with the established technique of miniplates osteosynthesis. The results of our study were put to comparison with previous studies on fracture mandible and were found to be in accordance with them. All the patients in our study appreciated early recovery of normal jaw function, uneventful healing and good union at the fracture site with minimal weight loss due to early reinstatement of the masticatory function. There was great patient acceptance of this treatment modality.
During the course of our study the 3D miniplates was found to be standard in profile, strong yet malleable, facilitating reduction and stabilization at both the superior and inferior borders giving 3D stability at fracture site. To the best of our knowledge, there have been relatively few studies on the clinical use of 3D plates for mandibular fractures specifically.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Champy M, Loddé JP, Schmitt R, Jaeger JH, Muster D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J Maxillofac Surg. 1978;6:14–21. doi: 10.1016/s0301-0503(78)80062-9. [DOI] [PubMed] [Google Scholar]
- 2.Farmand M, Dupoirieux L. The value of 3-dimensional plates in maxillofacial surgery. Rev Stomatol Chir Maxillofac. 1992;93:353–7. [PubMed] [Google Scholar]
- 3.Farmand M. The 3d plating system in maxillofacial surgery. J Oral Maxillofac Surg. 1993;51:166–7. [Google Scholar]
- 4.Farmand M. Three dimensional plate fixation of fractures and osteotomies: Facial plastic surgery. Clin North Am. 1995;3:39–56. [Google Scholar]
- 5.Lai G. The three-dimensional titanium miniplate rigid fixation in the treatment of fracture of maxilla. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 1997;11:196–8. [PubMed] [Google Scholar]
- 6.Fridrich KL, Pena-Velasco G, Olson RA. Changing trends with mandibular fractures: A review of 1,067 cases. J Oral Maxillofac Surg. 1992;50:586–9. doi: 10.1016/0278-2391(92)90438-6. [DOI] [PubMed] [Google Scholar]
- 7.Cabrini Gabrielli MA, Real Gabrielli MF, Marcantonio E, Hochuli-Vieira E. Fixation of mandibular fractures with 2.0-mm miniplates: Review of 191 cases. J Oral Maxillofac Surg. 2003;61:430–6. doi: 10.1053/joms.2003.50083. [DOI] [PubMed] [Google Scholar]
- 8.Guimond C, Johnson JV, Marchena JM. Fixation of mandibular angle fractures with a 2.0-mm 3-dimensional curved angle strut plate. J Oral Maxillofac Surg. 2005;63:209–14. doi: 10.1016/j.joms.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 9.Winstanley RP. The management of fractures of the mandible. Br J Oral Maxillofac Surg. 1984;22:170–7. doi: 10.1016/0266-4356(84)90094-9. [DOI] [PubMed] [Google Scholar]


