Abstract
Ectodermal dysplasia represents a group of rare inherited conditions in which two or more ectodermally derived anatomical structures fail to develop. Early dental intervention can improve patient′s appearance, thereby minimizing associated emotional and psychological problems in these patients. Treatment requires a teamwork by medical personnel along with dental professionals of various specialties. Here, a rare case of a young female patient is presented with prosthetic management with implant supported fixed partial denture.
Keywords: Ectodermal, fixed partial denture, implant
Ectodermal dysplasia (ED) is defined by National Foundation for Ectodermal Dysplasia as a large heterogeneous group of inherited disorder that is defined by primary defect in the development of two or more tissues derived from embryonic ectoderm.[1] Thurnam published the first report of a patient with ED in 1848,[2] but the term was not coined until 1929 [3] by Weech. It is congenital diffuse and nonprogressive disorder. It is of two types: Hypoanhidrotic ED (HAED) X-linked and hypohidrotic ED (HED).[4] ED of the hypohidrotic form is distinguished by a faulty ectodermal tissue development that includes complete or partial absence of sweat glands and is also known as Christ-Siemens-Touraine syndrome which affects one to seven individuals per 10,000 live birth.[5]
ED patients have a well-defined characteristic appearance which is well documented. Freire-Maia defined ED[5] as any syndrome that exhibits at least two of the following features: Trichodysplasia (abnormal hairs), abnormal dentition, onchodysplasia (abnormal nails), and dyshidrosis (abnormal or missing sweat glands). Other orofacial characteristic of this syndrome includes anodontia or hypodontia, hypoplastic conical teeth, hypotrichosis, and protuberant lips.
Prosthetic options for management of ED can include fixed, removable, or implant-supported prosthesis;[6] that may be employed individually or in combination to provide an optimal result.[2,3] Here we report with a case of HAED in a 22-year-old female patient and present the prosthetic management of a young female patient with implant supported fixed partial denture (FPD).
Case Report
A 22-year-old female reported with complaints of multiple missing teeth in upper and lower anterior region. Patient also complained of skin appeared dry with decreased sweating. Patient gave history of difficulty in mastication and swallowing. On examination, patient′s skin was dry and soft on face and increased thickness of nails; palm and sole were normal. She is normotensive and febrile with no mental retardation. She did not give positive family history. Her chest and skull radiographs and organ function tests were normal. Intraoral examination showed normal appearing mucosa and salivary output was apparently normal. The patient had 18, 15, 12, 22, 27, 28, 38, 45, and 48 missing teeth with generalized microdontia. The canines had cone shaped clinical crowns, and molars appeared malformed [Figure 1] with obliterated occlusal tables. Permanent maxillary right central incisor was present, which is a rare finding. Vertical dimensions were reduced due to a lack of occlusion and vertical stop causing protuberant lips. The panoramic radiograph confirmed presence of retained primary teeth in both the arches. With the above findings and orthopantomogram (OPG) figure, we came to a conclusion and diagnosed as HAED.
Figure 1.

Intraoral photograph
Treatment objective
To restore the missing teeth[6]
To increase the vertical dimension
To correct size of teeth
Alignment of teeth.[7]
Treatment plan included compensating microdontia by increasing tooth size using FPD retained by implant. To use implants, enough space was required; so orthodontic alignment of teeth was required. As teeth were distributed unevenly, it had to be aligned to gain space for implants.
Retained deciduous teeth were extracted and orthodontic correction [Figure 2] done with aligning and leveling. Enough space for implant was created within 1 year.
Figure 2.

Orthopantomograph during orthodontic correction treatment
Two implants [Figure 3] were placed in region of 12, 13 and one in the region of 45.
Figure 3.
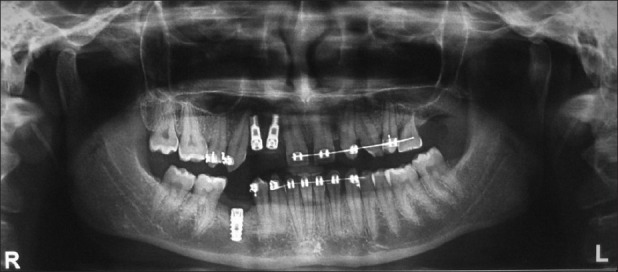
Orthopantomograph with implants
Three months were given for osseointegration. In the meantime, crown preparation was done for required teeth for FPD. Wax try-in was done for FPD to restore vertical dimension. Final FPD [Figure 4] was given and orthopantomograph [Figure 5] taken posttreatment.
Figure 4.

Intraoral photograph posttreatment
Figure 5.

Orthopantomograph posttreatment
The prosthetic rehabilitation provides the patient with esthetic, functional, and phonetic benefits, as well as a better outlook towards her social life and peers oral hygiene instructions, were given to the patient, and he was asked to report for follow up and assessment of her fixed prosthetic appliance after 6 months.
Discussion
The typical treatment of a patient with ED is achieved in several phases, depending on the craniofacial development, thus requiring a comprehensive and multidisciplinary approach. The different treatment modalities are dictated by manifestation of level of hypodontia[8] and resulting malocclusions. Numerous clinical reports have demonstrated importance of prosthetic dental treatment in ED patients for psychological and psychosocial reasons. A number of reviews regarding treatment of ED has showed that implant therapy in early infancy or adolescent age while little information is present in literature for ED patient above 18 years of age.[8] Prosthodontic treatment of ED can include fixed, removable, or implant supported prosthesis of which implant and fixed partial prosthodontics are the most frequent modalities.[9]
In removable prosthesis, frequently the oral mucosa is dry due to a decrease in the number of mucous glands and lesser quantity of saliva which makes retention of removable prosthesis more difficult. Overdentures can be used to restore ideal occlusion and usually allow preservation of existing dentition, but these require rigorous oral hygiene regimes to avoid development of caries and periodontal problems.[10] This case report describes a routine method for fixed prosthodontic[11] treatment of a patient with ED. As the patient was older than 18 years, the growth period was assumed to be over that would have resulted in the failure of FPDs as shown by Hogeboom.[12] A study by Guckes et al.,[13,14] showed that patients younger than 18 years had a hazard ratio of 2.8 compared to the patients older than 18 years. So for young patients, FPDs should be avoided as they could interfere with jaw growth and implants should be recommended and vice versa in patients > 18 years. Excellent oral hygiene is crucial for successful treatment of patients with this condition. The dental appearance of patients affected by ED has to be improved for physiologic and psychologic reasons, so that they can lead a normal social life with self-esteem.
Conclusion
This clinical report demonstrates the implant retained FPD as a suitable treatment while treating an adult patient with ED. This treatment option gives excellent result, which not only improves masticatory function but also enhances esthetics, allowing patients to lead a normal social life.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Thurnam J. Two cases in which skin, hair and teeth were very imperfectly developed. Med Chir Trans. 1848;31:71–82. doi: 10.1177/095952874803100108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weech AA. Hereditary ectodermal dysplasia (congenital ectodermal defect) Am J Dis Child. 1929;37:766–9. [Google Scholar]
- 3.Rajendran R, Sivapathasundaram B. Shafer′s textbook of oral pathology. 5th ed. Philadelphia: Saunders; 1983. [Google Scholar]
- 4.Yenisey M, Guler A, Unal U. Orthodontic and prosthodontic treatment of ectodermal dysplasia: A case report. Br Dent J. 2004;196:677–9. doi: 10.1038/sj.bdj.4811344. [DOI] [PubMed] [Google Scholar]
- 5.Pigno MA, Blackman RB, Cronin RJ, Cavazos E. Prosthodontic management of ectodermal dysplasia: A review of literature. J Prosthet Dent. 1996;76:541–5. doi: 10.1016/s0022-3913(96)90015-3. [DOI] [PubMed] [Google Scholar]
- 6.NaBadalung DP. Prosthodontic rehabilitation of an anhidrotic ectodermal dysplasia patient: A clinical report. J Prosthet Dent. 1999;81:499–502. doi: 10.1016/s0022-3913(99)70200-3. [DOI] [PubMed] [Google Scholar]
- 7.Suri S, Carmichael RP, Tompson BD. Simultaneous functional and fixed applied therapy for growth modification and dental alignment prior to prosthetic habilitation in hypohidrotic ectodermal dysplasia: A clinical report. J Prosthet Dent. 2004;92:428–33. doi: 10.1016/j.prosdent.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 8.Hobkirk JA, Brook AH. The management of patients with severe hypodontia. J Oral Rehabil. 1980;7:289–98. doi: 10.1111/j.1365-2842.1980.tb00447.x. [DOI] [PubMed] [Google Scholar]
- 9.Winstanley RB. Prosthodontic treatment of patients with hypodontia. J Prosthet Dent. 1984;52:687–91. doi: 10.1016/0022-3913(84)90142-2. [DOI] [PubMed] [Google Scholar]
- 10.Itthagarun A, King NM. Ectodermal dysplasia: A review and case report. Quintessence Int. 1997;28:595–602. [PubMed] [Google Scholar]
- 11.Hickey AJ, Vergo JT. Prosthetic treatments for patients with ectodermal dysplasia. J Prosthet Dent. 2001;86:364–8. doi: 10.1067/mpr.2001.118876. [DOI] [PubMed] [Google Scholar]
- 12.Hogeboom FE. Restorative procedures for children with ectodermal dysplasia. ASDC J Dent Child. 1961;28:62–72. [Google Scholar]
- 13.Guckes AD, Scurria MS, King TS, McCarthy GR, Brahim JS. Prospective clinical trial of dental implants in persons with ectodermal dysplasia. J Prosthet Dent. 2002;88:21–5. [PubMed] [Google Scholar]
- 14.Guckes AD, Brahim JS, McCarthy GR, Rudy SF, Cooper LF. Using endosseous dental implants for patients with ectodermal dysplasia. J Am Dent Assoc. 1991;122:59–62. doi: 10.14219/jada.archive.1991.0307. [DOI] [PubMed] [Google Scholar]


