Abstract
Gingivitis and periodontitis are most common inflammatory diseases of supporting tissues of teeth. Role of microbial etiology and host response in progression of gingival and periodontal diseases has been well established. Because of the beneficial biological effects of ozone, due to its antimicrobial and immunostimulating effect, it is well indicated in the treatment of gingival and periodontal diseases. The objective of this article is to provide a general review about clinical applications of ozone in treatment of periodontal diseases and to summarize the available in vitro and in vivo studies in Periodontics in which ozone has been used.
Keywords: Anti-hypoxic, immunostimulating, oxidizer
Ozone is a colorless gas form of oxygen and is present in atmosphere. It is one of the most important gases in the stratosphere due to its ability to filter ultraviolet rays, which is critical for the maintenance of biological balance in the biosphere. It has been used to purify water throughout the world for many years as it is highly effective in killing bacteria present in different forms. It effectively kills bacteria, fungi, viruses and parasites at a lower concentration.[1]
Ozone is a chemical compound consisting of three oxygen atoms (O3-triatomic oxygen), a higher energetic form than normal atmospheric oxygen (O2). Molecular weight of ozone is 41.98 g/mol. It is a powerful oxidizer.[2]
It protects living organisms by surrounding the earth at altitudes of 50,000-100,000 feet. One molecule of ozone is equal to 3000-10,000 molecules of chlorine and kills pathogenic organism′s 3500 times faster.[3] The use of ozonated fluids in dental care is upcoming. Extensive research has been carried out over the past 50 years into the use of ozonated fluids for infection control and wound management. Ozone has been proposed as an alternative oral antiseptic in dentistry. There are many known action of ozone on human body such as immunostimulating, analgesic, antihypoxic, detoxicating and antimicrobial properties. This new notion has given rise to a number of procedures and aims in eliminating only the infected and demineralized dental tissue and hence conserves and protects the tooth structure. [4]
Ozone is naturally produced by the photo dissociation of molecular oxygen into activated oxygen atoms which then react with further oxygen molecules. This transient radical anion rapidly becomes protonated, which in turn decomposes to an even powerful oxidant, the hydroxyl radical OH.[5]
History
In 1785, Van Marum noticed that air near his electrostatic machine acquired a characteristic odor when electric sparks were passed. In 1801, Cruickshank observed the same odor at the anode during electrolysis of water. In 1840, Schonbein named the substance “Ozein” which is a Greek word for smell. In 1856, ozone was used to disinfect operating rooms. In 1857, Werner Von Siemens designed an ozone generator, cylindrical dielectric type that makes up most of the commercially available ozone generators and called it the “Siemens type” ozone generator. In 1860, Monaco first used the ozone generator in water treatment plant. In 1870, ozone was first used for the medical application, when Dr. C. Lender purified blood in test tubes. In 1901, Wiesbaden used ozone in a municipal water supply. In 1931, Dr. E. A. Fisch, a dentist used ozonated water for dental procedures and pioneered its use in medicine.[6]
Mechanism of Action
Application of ozone in Periodontics comes as a result of its physic-chemical properties. Its known actions on human body are antimicrobial, analgesic, immunostimulating, antihypoxic and detoxicating.[7]
Composition of Medical Grade Ozone
It is a mixture of pure oxygen and pure ozone in the ratio of 0.05-5% of O3 and 95-99.5% of O2. Due to the instability of O3 molecule, it must be prepared immediately before use and cannot be stored over long periods of time.
Routes of Administration
Gaseous ozone - Ozone can be used in gaseous form via an open system or via a sealing suction system to avoid inhalation and its adverse effects.
Ozonated water - Ozonated water has been shown to be very effective against bacteria, fungi and viruses.
Ozonized oil - In addition to gaseous and aqueous form, oils that are ozonized also seems extremely convenient.
Though gaseous ozone was shown to have more effective microbicidal properties than aqueous form, due to its toxic effects if inhaled, ozonated water is the most preferred form for use in dentistry. Therefore a safe system for applying gaseous ozone into the periodontal pocket that avoids inhalation still needs to be developed.[8]
Generators of Ozone
The first ozone generator was developed by Werner Von Siemens in Germany in 1857. There are several different techniques used to produce therapeutic grade ozone.[9]
They are:
Ultraviolet system: Produces low concentrations of ozone. It is used in esthetics, saunas and fro air purification.
Corona discharge system: Produces high concentrations of ozone. Most common system used in medical and dental field. It is easy to handle and it has a high controlled ozone production.
Cold plasma system: Used in air and water purification.
Advantages
Disinfectant.
Anti-inflammatory.
Activation of intracellular metabolism of oral mucosa and dental wounds.
Improvement of regional circulation.
Stimulation of regenerative processes.
Hemostasis in capillary bleedings.
Painless procedures.
Disadvantages
Ozone toxicity if the level increases at 0.0007% per application.
Instability.
Not readily available.
Indications
Chronic or recurrent infections in the oral cavity.[10]
Prophylaxis and prevention of dental caries.
Remineralization of pit and fissure caries, root and smooth surface caries.
Bleaching of discolored root canal treated teeth.
Sterilization of cavities, root canals, periodontal pockets, herpetic lesions.
Desensitization of extremely sensitive tooth necks.
Pre-washing of surgical sites.
Plaque control.
Contamination control.
Goals of ozone therapy
Inactivates viruses, bacteria, yeast, fungus and protozoa.
Stimulates the immune system, cleans arteries, veins, and improves circulation.[13]
Purifies the blood and lymph.
Normalizes harmone and enzyme production.
Reduces inflammation and pain.
Stops bleeding.
Prevents shock and stroke damage.
Reduces cardiac arrhythmia.
Improves brain function and memory.
Oxidizes toxins allowing their excretion, chelates heavy metals.
Ozone Intoxification
Patient must be placed in supine position
Inhale humid oxygen
Ascorbic acid
Vitamin E
Acetylcystein
Biological Actions
Antimicrobial effect
Ozone works destructively against bacteria, fungi and viruses. The antimicrobial effect of ozone is a result of its action on cells by damaging its cytoplasmic membrane due to ozonolysis of dual bonds and also ozone-induced modification of intracellular contents because of secondary oxidant effects. This action is selective to microbial cells but does not damage human body cells because of their major antioxidative ability.[14]
Immunostimulating effect
Ozone influences cellular and humoral immune system. It stimulates proliferation of immunocompetent cells and synthesis of immunoglobulins. It also activates function of macrophages and increases sensitivity of microorganisms to phagocytosis. Ozone causes the synthesis of biologically active substances such as interleukins, leukotrienes, and prostaglandins which is beneficial in reducing inflammation and wound healing. Ozone in high concentrations causes immunodepressive effect whereas in its low concentration immunostimulating effect.[15]
Antihypoxic effect
Ozone improves the transportation of oxygen in blood, which results in change of cellular metabolism-activation of aerobic processes (glycolysis, Krebs cycle, β-oxidation of fatty acids) and use of energetic resources. Ozone improves the metabolism of inflamed tissues by increasing their oxygenation and reducing total inflammatory processes.[16]
Biosynthetic effect
It activates mechanisms of protein synthesis increases amount of ribosomes and mitochondria in the cells. These changes on the cellular level explain elevation of functional activity and regeneration potential of tissues and organs.
Application Modalities of Ozone in Periodontal Therapy
According to the clinical case, different applications modalities are available using ozone gas, irrigation with ozonated water and in-office use of ozonized oil as well as home use.[17]
Ozone in gaseous form
A customized suck down thermoformed hard or medium-soft dental appliance should extend 2-3 mm beyond the affected gingival area, leaving a free space for gas circulation. 2 ports should be attached for the gas inlet and outlet respectively at the distal and mesial of the treatment area. The edges of the appliance should be reclined with light or medium body silicone. Light-cured dam can also be applied as an extra safety precaution to completely seal the borders. The ports to the generator and the suction pump should then be attached. This procedure will treat both hard and soft tissues of the affected area. Poly vinyl chloride (PVC) or silicone cap can be used to treat individually all the indicated areas in difficult situations where such an appliance is hard to use or uncomfortable to the patient.
Irrigation with ozonated water
Ozonated water can be used to irrigate the affected area during and after scaling, root surface planning, and non-surgical pocket curettage.
In-office and home use of ozonized olive oil
After in-office treatment with ozone gas or ozonated water, pockets can be filled with ozonized olive oil using a blunt 25 G needle or any other appropriate tip. Patient can be given some of the oils for home use. In-office ozonized oil application can be repeated once a week.
Surgical procedures
Ozonated water can be used as an irrigant during the surgical procedure and/or as a final surgical site lavage. The sutures can be covered with a thin layer of ozonized oil and the patient can be instructed to apply the oil 3-4 times a day.
Peri-implantitis
Peri-implantitis is very bothering to both the dentist and the patient. Laser and/or manual debridement along with antiseptic solutions and topical anti-microbial medicines are commonly performed with a varying degree of success. Ozone can play an important role and be used as gas or in aqueous form. Ozone gas infiltrations can also be used in this situation. Ozonated water can be used as an irrigant during debridement and curettage. Patient can be advised to apply ozonized oil on the treated area 3-4 times/day.
Ozone in the Treatment of Periodontal Diseases
Periodontal disease is a multifactorial disease process in the mouth. The role of microorganisms, hostresponse, in the etiology of periodontal disease is well established.
The undisputed disinfection power of ozone over other antiseptics makes the use of ozone in treatment of periodontitis a very good alternative and/or an additional disinfectant to standard antiseptics.
Ozonated water (4 mg/l) was found effective for killing gram-positive and gram-negative oral microorganisms and oral Candida albicans in pure culture as well as bacteria in plaque biofilm and therefore might be useful as a mouth rinse to control oral infectious microorganisms in dental plaque. In implant dentistry, the use of ozone is currently being investigated for the decontamination of the implant surface in Peri-implant therapy.
Thanomsub et al. 2002 tested the effects of ozone treatment on cell growth and ultra-structural changes in bacteria (Escherichia coli, Salmonella sp., Staphylococcus aureus and Bacillus subtilis). It was discovered that ozone at 0.167 mg/min/l can be used to sterilize water, which is contaminated with up to 105 cfu/ml bacteria within 30 min. Destroying of bacterial cell membrane was observed, subsequently producing intercellular leakage and eventually causing cell lysis. Nevertheless, these ozone concentrations have no significant effect on the cell viability in bacterial cultures at higher concentrations of 106 and 107 cfu/ml.[18]
Ebensberger et al. in 2002 evaluated the effect of irrigation with ozonated water on the proliferation of cells in the periodontal ligament adhering to the root surfaces of 23 freshly extracted completely erupted third molars. The teeth were randomly treated by intensive irrigation with ozonated water for 2 min or irrigation with a sterile isotonic saline solution, serving as a control group. The periodontal cells of these teeth were studied immunohistochemically to mark proliferating cell nuclear antigen. It was observed that the labeling index (the number of positive cells compared to the total number of cells suggesting enhancement of metabolism) was higher among the teeth irrigated with ozone (7.8% vs. 6.6%); however, the difference was not statistically significant (P = 0.24). They concluded that the 2 min irrigation of the avulsed teeth with non-isotonic ozonated water might lead not only to a mechanical cleansing, but also decontaminate the root surface, with no negative effect on periodontal cells remaining on the tooth surface.[19]
Holmes in 2003, observed effect of Kavo healozone device on Primary root carious lesions (PRCL) followed-by professionally-applied remineralizing solution containing xylitol, fluoride, calcium, phosphate and zinc. This treatment modality was applied to 89 patients, aged from 60 to 82 years. After 18 months, 100% of ozone-treated PRCL′s had improved. In control group, where lesions were left without treatment, only 1 PRCL had improved. In 62% of cases the status remained leathery, while in 37% of PRCL′s had worsened from leathery to soft.[5]
Nagayoshi et al. 2004 tested the efficacy of ozonated water on survival and permeability of oral micro-organisms. Gram negative bacteria, such as Porphyromonas endodontalis and Porphyromonas gingivalis were substantially more sensitive to ozonated water than gram positive oral streptococci and c. albicans in pure culture. Furthermore ozonated water had strong bactericidal activity against bacteria in plaque biofilm. In addition, ozonated water inhibited the accumulation of experimental dental plaque in vitro.[20]
Hems and Gulabivala, 2005 evaluated the potential of ozone as an anti-bacterial agent using Enterococcus faecalis as a test species. Ozone was used both gasiform (produced by Purezone device), and aqueous (optimal concentrations 0.68 mg/l). It was concluded that ozone in solutions was antibacterial against planctonic Enterococcus faecalis after 240 s treatment. However it was not effective against Enterococcus faecalis cells in a biofilm unless they were displaced into the surrounding medium by agitation. Gaseous ozone was not effective on the Enterococcus faecalis biofilm.[21]
Ramzy et al. in 2005 irrigated the periodontal pockets by ozonized water in 22 patients suffering from aggressive periodontitis. Periodontal pockets were irrigated with 150 ml of ozonized water over 5-10 min once weekly for a clinical 4 weeks study using a blunt tipped sterile plastic syringe. High significant improvement regarding pocket depth plaque index gingival index and bacterial count was recorded related to quadrants treated by scaling and rootplaning together with ozone application. They also reported significant reduction in bacterial count in sites treated with ozonized water.[22]
Huth et al. in 2006, in their study declared that the aqueous form of ozone, as a potential antiseptic agent, showed less cytotoxicity than gaseous ozone or established anti microbials (chlorhexidine digluconate [CHX]: 2%, 0.2%; sodium hypochlorite 5.25%, 2.25%; hydrogen peroxide-H2 O2 3%) under most conditions. Therefore, aqueous ozone fulfills optimal cell biological characteristics in terms of biocompatibility for oral application.[23]
Muller et al. in 2007 compared the influence of ozone gas with photodynamic therapy (PDT) and known antiseptic agents (2% chlorhexidine, 0.5 and 5% hypocholrate solutions) on a multispecies oral biofilm in vitro. Actinomyces naeslundii, Veillonella dispar, Fusobacterium nucleatum, Streptococcus sobrinus, Streptococcus oralis and c. albicans were studied. Gasiform ozone was produced by vacuum ozone delivery system Kavo Healozone. They concluded that the matrix-embedded microbial populations in biofilm are well protected towards antimicrobial agents. Only 5% hypochlorate solution was able to eliminate all bacteria effectively. Usage of gasiform ozone or PDT was not able to reduce bacteria in the biofilm.[24]
Kronusova 2007 used ozone in following cases: Prevention of dental caries in fissures of the first permanent molars in children, application of ozone in prepared cavity, after tooth extraction, in case of post extractional complications, in patients with chronic gingivitis, periodontitis and periodontal abscesses, herpes labialis, purulent periodontitis, dentition difficilis, etc., Almost all patients with gingivitis showed subjective and objective improvement of their status, as well as patients with periodontal abscess, where no exudation was observed. Application of ozone after tooth extraction was found also quite useful - only 10% of patients suffered from such complication as alveolitis sicca, but even in these cases the clinical course was shorter and more moderate.[25]
Karapetian et al. in a study of peri-implantitis, treatment with conventional, surgical and ozone therapy methods was investigate and it was found that the most effective bacteria reduction was in the ozone-treated group.[26]
Kshitish and Laxman in 2010 conducted a randomized, double-blind, crossover split-mouth study on 16 patients suffering from generalized chronic periodontitis. The study period of 18 days was divided into two time-intervals, i.e., baseline (0 days) to the 7th day, with a wash out period of 4 days followed by a second time-interval of 7 days. Subgingival irrigation of each half of the mouth with either ozone or chlorhexidine was done at different time intervals. They observed a higher percentage of reduction in plaque index (12%), gingival index (29%), and bleeding index (26%) using ozone irrigation as compared to chlorhexidine. The percentile reduction of Aa (25%) using ozone was appreciable as compared to no change in Aa occurrence using chlorhexidine. By using O3 and chlorhexidine, there was no anti-bacterial effect on Porphyromonas gingivalis (Pg) and Tannerella forsythensis. The anti-fungal effect of ozone from baseline (37%) to 7th day (12.5%) was pronounced during the study period, unlike CHX, which did not demonstrate any anti-fungal effect. No anti-viral property of ozone was observed. The anti-viral efficacy of chlorhexidine was better than that of ozone. They concluded that despite the substantivity of chlorhexidine, the single irrigation of ozone is quite effective to inactivate microorganisms.[27]
Fillippi. A observed the influence of ozonized water on the epithelial wound healing process in the oral cavity. It was found that ozonized water applied on daily basis can accelerate the healing rate in oral mucosa.[28]
Huth, et al. in 2011 compared the effectiveness of ozone with that of the established antiseptic CHX, against periodontal microorganisms. There were no significant differences in the effectiveness of aqueous ozone (20 μg ml [−1]) or gaseous ozone (≥4 g [−3]) compared with 2% CHX but they were more effective than 0.2% CHX. Therefore, high-concentrated gaseous and aqueous ozone merit further investigation as antiseptics in periodontitis therapy.[29]
Dodwad et al. in 2011 compared the effect of oral irrigation with ozonated water, 0.2% Chlorhexidine and 10% Povidone iodine in patients with chronic periodontitis. The study concluded that local ozone application can serve as potent atraumatic, antimicrobial agent to treat periodontal disease non-surgically both for home care and professional practice. It may also serve as good tool during supportive periodontal therapy.[30]
Conclusions
Since its introduction in 1840, ozone therapy is proving to be a new therapeutic modality with great benefits to the patients. The potent antimicrobial power of ozone, along with its capacity to stimulate the circulatory system and modulate the immune response, makes it a therapeutic agent of choice in the treatment of medical pathologies and infectious oral diseases. Oxidative effect of ozone on the microbiota has been shown in several studies. There is good evidence of in vitro biocompatibility of aqueous ozone with human oral epithelial cells, gingival fibroblast cells and periodontal cells. Further, the use of ozone is an easy and painless treatment modality.
The clinical application of ozone has not achieved strong level of efficacy and cost effectiveness. This divergence of the study outcomes may be related to the methodological differences linked to the lack of in vitro and in vivo, long term randomized controlled trials and double blind studies. There is still a need for the highest level of evidence, i.e., well designed; double-blind randomized clinical trials to justify the routine use of ozone as a treatment modality in dentistry. Scientific support, as suggested by demonstrated studies, show ozone to be a potential use in dentistry.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Grootveld M, Baysan A, Siddiqui N, Sim J, Silwood C, Lynch E. History of clinical publications of ozone. In: Lynch E, editor. Ozone: the revolution in dentistry. London: Quintessence Publishing Co; 2004. pp. 23–30. [Google Scholar]
- 2.Stopka P. Ozon. Progresdent. 2003;6:8–11. [Google Scholar]
- 3.Filippia A. The effect of ozonated water on epithelial wound healing. Douch Dent J. 2001;143:96–101. [Google Scholar]
- 4.Sunnan GV. Ozone in medicine: Overview and future directions. J Adv Med. 1988;1:159–74. [Google Scholar]
- 5.Holmes J. Clinical reversal of root caries using ozone, double-blind, randomised, controlled 18-month trial. Gerodontology. 2003;20:106–14. doi: 10.1111/j.1741-2358.2003.00106.x. [DOI] [PubMed] [Google Scholar]
- 6.Sameer M, Monica M. Ozone treating dental infections. Ind J Stomatol. 2011;2:256–9. [Google Scholar]
- 7.Bocci V. Biological and clinical effects of ozone. Has ozone therapy a future in medicine? Br J Biomed Sci. 1999;56:270–9. [PubMed] [Google Scholar]
- 8.Priyamak AA. Ozone: The Revolution in Dentistry. Copenhagen: Quintessence Publishing; 2004. pp. 155–64. [Google Scholar]
- 9.Nogales CG, Ferrari PA, Kantorovich EO, Lage-Marques JL. Ozone therapy in medicine and dentistry. J Contemp Dent Pract. 2008;4:75–84. [PubMed] [Google Scholar]
- 10.Baysan A, Lynch E. The use of ozone in dentistry and medicine. Prim Dent Care. 2005;12:47–52. doi: 10.1308/1355761053695158. [DOI] [PubMed] [Google Scholar]
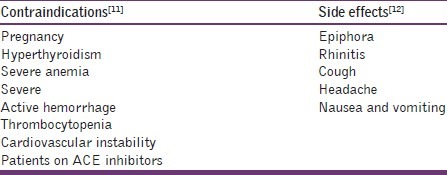
- 11.Stübinger S, Sader R, Filippi A. The use of ozone in dentistry and maxillofacial surgery: A review. Quintessence Int. 2006;37:353–9. [PubMed] [Google Scholar]
- 12.Bocci V. Ozone as a bioregulator. Pharmacology and toxicology of ozonetherapy today. J Biol Regul Homeost Agents. 1996;10:31–53. [PubMed] [Google Scholar]
- 13.Mollica P, Harris R. Integrating oxygen/ ozone therapy into your practice. [Last cited on 2010 January 13]. [Online] Available from: URL: http://www.Toxin free smile. Dom/ images/ozone integrating % 20 oxygen ozone 20% therapy your practice.Pdf .
- 14.Seidler V, Linetskiy I, Hubálková H, Stanková H, Smucler R, Mazánek J. Ozone and its usage in general medicine and dentistry. A review article. Prague Med Rep. 2008;109:5–13. [PubMed] [Google Scholar]
- 15.Teresa B, Wolanska E, Cieszko-Buk M, Orlowski M, Chalas R. Practical use of ozone in dentistry-comments. Ann Universitalis Maria Curie-Sklodowska Lubin-Polonia. 2008;LXIII:28. [Google Scholar]
- 16.Seaverson K, Tschetter D, Kaur T. Patient guide to oxygen/ozone therapy. Health centered cosmetic dentistry. [Last cited on 2010 January 13]. Available from: URL: http://www.toothbythelake.net/ozone_therapy.html .
- 17.Gupta G, Mansi B. Ozone therapy in periodontics. J Med Life. 2012;5:59–67. [PMC free article] [PubMed] [Google Scholar]
- 18.Thanomsub B, Anupunpisit V, Chanphetch S, Watcharachaipong T, Poonkhum R, Srisukonth C. Effects of ozone treatment on cell growth and ultrastructural changes in bacteria. J Gen Appl Microbiol. 2002;48:193–9. doi: 10.2323/jgam.48.193. [DOI] [PubMed] [Google Scholar]
- 19.Ebensberger U, Pohl Y, Filippi A. PCNA-expression of cementoblasts and fibroblasts on the root surface after extraoral rinsing for decontamination. Dent Traumatol. 2002;18:262–6. doi: 10.1034/j.1600-9657.2002.00087.x. [DOI] [PubMed] [Google Scholar]
- 20.Nagayoshi M, Fukuizumi T, Kitamura C, Yano J, Terashita M, Nishihara T. Efficacy of ozone on survival and permeability of oral microorganisms. Oral Microbiol Immunol. 2004;19:240–6. doi: 10.1111/j.1399-302X.2004.00146.x. [DOI] [PubMed] [Google Scholar]
- 21.Hems RS, Gulabivala K, Ng YL, Ready D, Spratt DA. An in vitro evaluation of the ability of ozone to kill a strain of Enterococcus faecalis. Int Endod J. 2005;38:22–9. doi: 10.1111/j.1365-2591.2004.00891.x. [DOI] [PubMed] [Google Scholar]
- 22.Ramzy MI, Gomaa HE, Mostafa MI. Management of aggressive periodontitis using ozonized water. Egypt Med J NRC. 2005;6:229–45. [Google Scholar]
- 23.Huth KC, Jakob FM, Saugel B, Cappello C, Paschos E, Hollweck R, et al. Effect of ozone on oral cells compared with established antimicrobials. Eur J Oral Sci. 2006;114:435–40. doi: 10.1111/j.1600-0722.2006.00390.x. [DOI] [PubMed] [Google Scholar]
- 24.Müller P, Guggenheim B, Schmidlin PR. Efficacy of gasiform ozone and photodynamic therapy on a multispecies oral biofilm in vitro. Eur J Oral Sci. 2007;115:77–80. doi: 10.1111/j.1600-0722.2007.00418.x. [DOI] [PubMed] [Google Scholar]
- 25.Seidler V, Linetskiy I, Hubalkova H, Stankova H, Šmucler R, Mazanek J. Ozone and its usage in general medicine and dentistry. A review article. Prague Medical Report. 2008;109:5–13. [PubMed] [Google Scholar]
- 26.Karapetian VE, Neugebauer J, Clausnitzer CE, Zoller JE. Comparison of Different Periimplantitis Treatment Methods. [Last accessed on 2013 January 29]. Available from: http://www.helbo.at/datasheets/poster_karapetian_0304.pdf .
- 27.Kshitish D, Laxman VK. The use of ozonated water and 0.2% chlorhexidine in the treatment of periodontitis patients: A clinical and microbiologic study. Indian J Dent Res. 2010;21:341–8. doi: 10.4103/0970-9290.70796. [DOI] [PubMed] [Google Scholar]
- 28.Fillipi A. Clinic of Oral Surgery, Radiology and Oral Medicine. Switzerldand: University of Basel; [Last accessed on 2013 January 29]. The influence of ozonised water on the epithelial wound healing process in the oral cavity. Available at: WWW.OXYPLUS.NET . [Google Scholar]
- 29.Huth KC, Quirling M, Lenzke S, Paschos E, Kamereck K, Brand K, et al. Effectiveness of ozone against periodontal pathogenic microorganisms. Eur J Oral Sci. 2011;119:204–10. doi: 10.1111/j.1600-0722.2011.00825.x. [DOI] [PubMed] [Google Scholar]
- 30.Dodwad V, Gupta S, Kumar K, Sethi M, Masamatti S. Changing paradigm in pocket therapy-ozone versus conventional irrigation. Int J Public Health Dent. 2011;2:7–12. [Google Scholar]


