Abstract
Gingival recession is defined as the apical migration of the junctional epithelium with exposure of root surfaces. It is a common condition seen in both dentally aware populations and those with limited access to dental care. The etiology of the condition is multifactorial but is commonly associated with underlying alveolar morphology, tooth brushing, mechanical trauma and periodontal disease. Given the high rate of gingival recession defects among the general population, it is imperative that dental practitioners have an understanding of the etiology, complications and the management of the condition. The following review describes the surgical techniques to treat gingival recession.
1. Introduction
Gingival recession is the exposure of the root surface resulting from migration of the gingival margin apical to the cementoenamel junction (CEJ). It may be localized or generalized and can be associated with one or more tooth surfaces (Kassab and Cohen, 2003).
Epidemiological studies show that more than 50% of subjects in the populations studied have one or more sites with recession of at least 1 mm, buccal sites being most commonly affected. Higher levels of recession have been found in males than females (Susin et al., 2004). Recession at the buccal surfaces is common in populations with good oral hygiene (Serino et al., 1994; Neely et al., 2005; Sangnes and Gjermo, 1976) whereas with poor standards of oral hygiene it may affect other tooth surfaces (Baelum et al., 1986). Gingival recession at the lingual surfaces of lower anterior teeth showed a strong association with the presence of supragingival and subgingival calculus (van Palenstein Helderman et al., 1998).
The etiology of the condition is multifactorial and may include plaque-induced inflammation, calculus and restorative iatrogenic factors, trauma from improper oral hygiene practices, tooth malpositions, high frenum attachment, improper periodontal treatment procedures, and uncontrolled orthodontics movements (Wennstrom, 1996; Tugnait and Clerehugh, 2001). Gingival recession is also a common outcome of the therapies delivered to treat periodontal disease.
Eventhough gingival recession may occur without any symptoms it can give rise to pain from exposed dentine, patient concern about loss of the tooth, poor esthetics or root caries. The denuded root surfaces cause deterioration in the esthetic appearance, dentin hypersensitivity, and inability to perform proper oral hygiene procedures (Zucchelli et al., 2006; Seichter, 1987).
The management of gingival recession and its sequelae is based on a thorough assessment of the etiological factors and the degree of tissue involvement. The initial part of the management of the patient with gingival recession should be directed towards correcting the etiological factors. The degree of gingival recession has to be monitored for signs of further progression. Surgical root coverage is indicated when esthetics is the prime concern and periodontal health is good.
2. Classification of gingival recession
Two main types of marginal gingival recession have been identified. A generalized one, which may involve interproximal areas, is mainly found in periodontally untreated populations with poor oral hygiene. The other type is usually related to traumatic factors and often involves only a few teeth or a group of teeth. The latter frequently occurs in buccal areas where the lesions commonly are associated with plaque-free, smooth, and well polished hard tissue defects (Maynard, 2004; Miller, 1987).
Miller (1985) proposed a useful recession defect classification based on the height of the interproximal papillae and interdental bone adjacent to the defect area, and the relation of the gingival margin to the mucogingival junction (Table 1) (Miller, 1985). This classification is useful when deciding on treatment options (Maynard, 2004).
Table 1.
Miller’s classification of gingival recession defects (1985).
| Class I | Recession within attached gingiva. No loss of interdental bone and soft tissue papillae covering interdental bone at full height |
| Class II | Recession extending to or beyond the mucogingival junction. No loss of interdental bone and soft tissue papillae covering interdental bone at full height |
| Class III | Recession extending to or beyond the mucogingival junction. Loss of interdental bone but interdental bone height coronal to apical extent of recession defect. Reduction in height of the soft tissue papillae covering interdental bone |
| Class IV | Recession extending to or beyond the mucogingival junction. Loss of interdental bone apically to recession defect. Gross flattening of interdental soft tissue papillae |
3. Surgical procedures
The techniques used for root coverage are based on tissue displacement whether by translation (pedicle flap procedures) or by grafting (free gingival or connective tissue graft procedures), and use of resorbable and non-resorbable membranes according to the principles of guided tissue regeneration (GTR) (Wennstrom, 1996). Several modifications to the conventional techniques have been developed in an attempt to obtain optimal root coverage and a better esthetic integration.
Surgical procedures may be broadly divided into two different types:
Pedicle soft tissue graft procedures. These types of graft remain attached at their base and involve the positioning of soft tissue over the recession defect; they retain their own blood, supply during their transfer to a new location. Examples include:
-
•
Rotational flap procedures, including laterally positioned flap, double papilla flap.
-
•
Flap advancement procedures, including coronally repositioned flap.
Free soft tissue graft procedures. Soft tissues are transferred from an area distant to the recession to cover the defect. These techniques are used where there is inadequate donor tissue close to the recipient site or where the aim of treatment is to increase tissue thickness.
-
•
Free gingival graft.
-
•
Subepithelial connective tissue graft.
In periodontal practice, root coverage therapies for gingival recession defects require daily clinical decisions. Numerous studies have been reported to support the efficacy and predictability of different proposed surgical techniques. The selection of the surgical techniques should be dictated by several factors, including the anatomy of the defect site, such as the size of the recession defect, the presence or absence of keratinized tissue adjacent to the defect, the width and height of the interdental soft tissue, and the depth of the vestibule or the presence of frenula (Zucchelli et al., 2006; Haghighati et al., 2009). Moreover, the existence of esthetic considerations, the desired outcome, and the evidence-based predictability of various procedures should be also evaluated (Kerner et al., 2009).
Among patient-related factors, the attempt to reduce the number of surgeries and intraoral surgical sites, together with the patient’s expectations must be considered. Age of the patient, medical conditions and smoking status may also affect the results of root coverage surgical procedures. The surgeon’s clinical experience may be a potential factor influencing judgments, case selection, and surgical skills. However, case selection has proven the critical beneficial in promoting clinical outcomes (Andia et al., 2008; Clauser et al., 2003).
4. Presurgical preparation
Root surfaces are mechanically prepared prior to any mucogingival procedure to allow biological attachment of the grafted tissue to it. The root surface is thoroughly debrided with ultrasonic or hand instruments and irrigated with sterile saline. Mechanical modification of the root surface as well as root conditioning procedures have been used prior to the surgical root coverage techniques to achieve improved results (Miller, 1985). Root surface modification using agents such as citric acid or tetracycline hydrochloride has been advocated in an effort to promote the healing response following root surface coverage, although clinical studies have failed to show any improvement in root surface coverage when using such agents (Tolmie et al., 1991; Zucchelli et al., 2009; Pini-Prato et al., 1999).
5. Pedicle grafts
5.1. Coronally advanced flap (Fig. 1)
Figure 1.
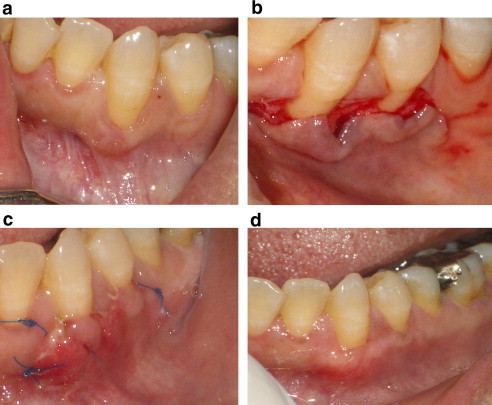
Coronally advanced flap. (a) Gingival recession defect affecting the mandibular canine, (b) a partial thickness flap is elevated and the papillae de-epithelialized, (c) the flap is coronally advanced and secured in place with interrupted sutures, (d) 3 months postoperative appearance.
This technique is relatively straightforward providing good esthetic results, but is only indicated when adequate sulcular depth exists (Huang et al., 2005). Pedicle flap surgical techniques (coronally advanced or rotated flaps) are recommended if there is adequate keratinized tissue close to the recession defect. In this surgical approach, the soft tissue utilized to cover the root exposure is similar to that originally present at the buccal aspect of the tooth with the recession defect and thus the esthetic result is more satisfactory. Two vertical incisions are made extending beyond the mucogingival junction and a full thickness flap is raised. The flap is undermined by dissection to free the periosteum. The flap is repositioned in a coronal position and is securely sutured into place. Furthermore, the postoperative course is less troublesome since other surgeries in donor sites are not involved (Milano, 1998).
The coronally advanced flap is commonly used to treat the Miller Classes I and II recession defects. Optimum root coverage results, good colour matching to adjacent soft tissues, and recuperation of the original morphology of the gingival margin can be accomplished using this surgical approach (Kerner et al., 2009). Furthermore, the coronally advanced flap is very effective in treating multiple recession defects with obvious advantages for the patient in terms of esthetics and morbidity (Harris et al., 2005). Several factors might have influenced the final outcome of the coronally advanced flap; such as the height of the interdental papilla, the amount of keratinized gingiva, the presence of gingival cleft extending in alveolar mucosa, the deep cervical wear, the frenum attachment, and the vestibular depth (Huang et al., 2005).
Semilunar coronally advanced flap procedure was proposed first by Tarnow in 1986. This technique causes no disturbance of the adjacent papilla, no shortening of the vestibule, and no tension on the flap (Tarnow, 1986). An adequate gingival thickness allowing partial thickness flap dissection is required to avoid alveolar bone fenestrations (Haghighat, 2006).
5.2. Laterally positioned grafts (Fig. 2)
Figure 2.
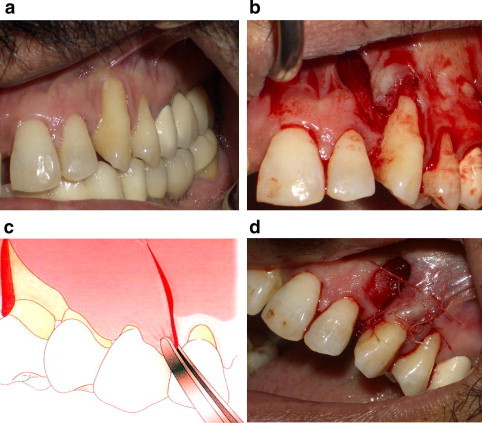
Laterally positioned grafts. (a) Recession at the maxillary canine, (b) pedicle graft from the lateral incisor area, (c) diagram showing the flap design, (e) laterally positioned graft covering the defect.
These flaps are indicated when a narrow defect exists with adequate attached gingiva at the donor site (Zucchelli et al., 2004). To have root coverage, the marginal gingival tissues around the tooth are excised by a beveled incision to the base of the gingival pocket. Incisions into the gingival margin and interdental papilla of the donor site are made. A vertical relieving incision is made in an apical direction from the gingival margin at the distal surface of the donor site to a sulcular position, which slightly exceeds that of the defect to be covered. A partial thickness flap is raised as leaving the periosteum intact will accelerate healing of the donor site. The donor flap is rotated into place to cover the defect and firmly adapted to the defect and sutured into place. Instability and movement of all flaps will result in flap failure. Good adaptation of the flap to the underlying tissues is essential for adequate diffusion, so care must be taken on preparing the recipient bed and cutting the graft to the exact size required to ensure a good fit.
The analysis of the literature revealed that the limiting condition for performing the laterally positioned flap as a root recession treatment approach was the presence of keratinized tissue lateral to the recession defect. As previously reported in the literature, better root coverage outcomes were only achieved in cases with adequate height and width of keratinized tissue (Wennstrom, 1996). Stability and dimensions of the laterally moved flap (the wider the pedicle, the greater the blood supply to the marginal portion of the flap) are critical for accomplishing root coverage. Tissue thickness of the flap is an important aspect on the root coverage predictability and an improvement in esthetic outcome (Hwang and Wang, 2006).
The stability of a flap over a denuded avascular root surface can be achievable by increasing the flap tissue thickness. Furthermore, a certain amount of the lateral periosteum tissue, in fact, must be preserved in situ to prevent the appearance of an unesthetic scar following the healing of the exposed bone area at the adjacent donor site, while the remaining part is used to cover the exposed root surface (Kerner et al., 2009). Studies have shown that with a rigid case selection the laterally positioned flap is an effective method in treating isolated gingival recession (Zucchelli et al., 2004).
6. Free soft tissue graft procedures
Free soft tissue grafts include both epithelialized (free gingival) grafts and connective tissue grafts. Free soft tissue grafts are obviously devoid of a blood supply and when used as an onlay graft they rely on a nutrient supply of serum from their recipient bed.
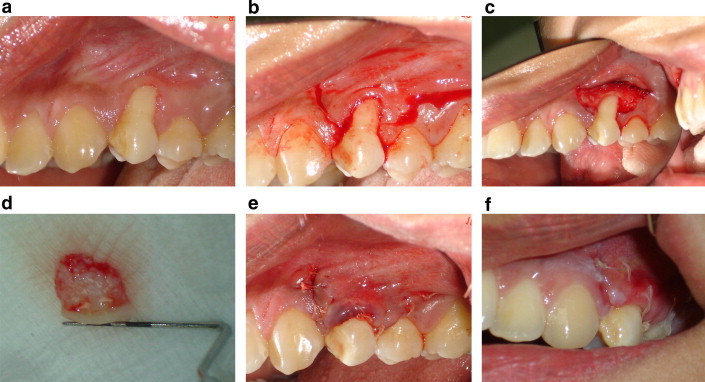
6.1. Free gingival graft (Fig. 3)
Figure 3.

Free gingival graft. (a) Mandibular incisors with recession and lack of attached gingiva, (b) preparation of the recipient site, (c) the graft is sutured to the recipient bed, (d) 2 months postoperative appearance.
While free gingival grafts can be used to treat mild recession, they are often used as part of a two-stage approach, providing adequate keratinized tissue for subsequent coronal advancement. In this techniques graft comprising both epithelium and underlying connective tissue is taken, usually from the palate, and sutured into position in a recipient site prepared using a splint-thickness flap. The recipient bed should extend at least 3 mm laterally and apically to the recession defect, as this will be the only nutrient supply to the graft during the initial healing phase. If the defect extends into the depth of the sulcus, the soft tissues (as well as any muscle or fraenal insertions) should be removed by sharp dissection to ensure that the graft lies passively with no movement occurring during function. Tin-foil templates can be used to measure the size of the defect to be filled. These templates are transferred to the palate as a guide to the graft size from which a graft of 2–3 mm thickness is removed. Care must be taken to avoid the palatine blood vessels.
As revascularization of the graft takes few days, the vitality of the tissue initially depends on the diffusion of nutrients from the recipient site connective tissue. Good adaptation of the flap to the underlying tissues is essential for adequate diffusion, so care must be taken on preparing the recipient bed and cutting the graft to the exact size required to ensure a good fit.
6.2. Connective tissue grafts (Fig. 4)
Figure 4.
Connective tissue grafts. (a) Recession at maxillary first premolar, (b) vertical incision, (c) partial thickness flap reflection, (d) the harvested graft tissue, (e) the graft sutured in position, (f) 2 weeks healing.
Free gingival grafts have a number of disadvantages. Esthetics may be compromised because of the colour difference between the graft and recipient site tissues, while there is also the problem of a large denuded site in the palate, which must heal by secondary intention. These disadvantages have been overcome by the use of connective tissue (CT) grafts, which involve placement of de-epithelialized connective tissue into the recession defect. Healing of the donor site is by primary intention, reducing discomfort for the patient. The colour match with the tissues is also better. Connective tissue grafts are commonly harvested from the palate, provided there is adequate thickness of tissue. The retro-molar pad area can also be used because of the thickness of the sub-mucosa in this area. This graft material is carefully sutured into place and a coronally advanced flap placed and sutured over it.
Among the various surgical approaches used to treat gingival recession, connective tissue graft in combination with the coverage of the graft by overlying flap can be considered the gold standard for treating gingival recession defects (Al-Zahrani et al., 2004; Bruno, 1994; Langer and Langer, 1985). Because the success and predictability of this surgical technique, various modifications have been proposed, including connective tissue graft with or without epithelial collar, partially or totally covered by pedicle flap, with an envelope or tunnel design preparations covered by undetached papilla (Harris et al., 2007; Allen, 1994; Santarelli et al., 2001).
The main advantages of the connective tissue graft procedures are thought to derive from the availability of two sources of blood supply to the graft: one from the recipient bed and the other from the overlying flap, and the perfect chromatic integration and an optimal esthetic outcome (Wilcko et al., 2005). Since the success rate of root coverage depends on the survival of graft tissue itself, it has been suggested that the overlying flap should cover most of the graft. This is thought to provide enough blood supply to nourish the underneath portion of the graft over the denuded root (Souza et al., 2008).
The proper flap design is also an important step toward obtaining satisfactory root coverage outcomes with connective tissue grafting approach. Langer and Langer (1985) proposed the use of vertical releasing incisions, which might compromise the gingival margin vascularization at the early stages of wound healing resulting in fibrotic scars. Therefore, numerous other authors have provided variations on the techniques and provided support to the original techniques (Wennstrom, 1996). An envelope or a pouch flap design was proposed by Raetzke (1985) eliminating vertical incisions (Fig. 5). The advantages of the technique are the maintenance of the blood supply to the flap, a close adaptation to the graft, and reduction in postoperative discomfort and scarring. Allen (1993) reported the use of a technique where a connective tissue graft is placed in a tunnel preparation (Fig. 6). This technique allows the maintenance of a greater thickness flap apical to the recession, which will cover the denuded root surface for multiple adjacent recession defects (Santarelli et al., 2001).
Figure 5.

An envelope flap. (a) Gingival recession affecting #22, (b) the envelope flap created, (c) the graft and the flap are sutured, (d) healing after 3 months.
Figure 6.

Tunnel preparation. (a) Recession #23, 24, 25, 26 regions, (b) incision at palatal donor site, (c) palatal flap sutured after harvesting the tissue, (d) the graft sutured under the tunnel flap, (e) healing after 2 weeks, (f) 4 months later.
6.3. Palatal donor sites
The main donor site for a connective tissue graft is the palate or the maxillary tuberosity area. The success of this technique depends on the thickness of the graft tissue obtained. Therefore, the thickness and volume of the tissue to be grafted from the donor site are important factors in determining the appropriate treatment method and for predicting the prognosis (Monnet-Corti et al., 2006; Wara-aswapati et al., 2001).
One of the concerns of harvesting the graft tissue from is the potential risk of damaging the greater palatine artery due to variation in the anatomy of the palatal vault. Reiser et al. (1996) proposed to subdivide the palatal vault into three groups, high, average, and shallow, and suggested that, caution should be observed not to endanger the greater palatine artery when dealing with a shallow palatal vault. Therefore, it was of interest to assess the maximum dimensions that can be harvested from the palatal tissue in terms of height and length in relation to the usual course of the greater palatine artery (Monnet-Corti et al., 2006). There are various methods for testing the thickness of the palatal tissue such as direct bone sounding using a periodontal probe, an endodontic reamer, or an injection needle after local anesthesia. Recently, clinical assessment of the palatal tissue thickness using computerized tomography and an ultrasonic device has also been suggested (Song et al., 2008). A variety of harvesting techniques were proposed including parallel incisions or a single incision to minimize the size of the palatal wound that can allow for primary closure of the donor site, which may result in reduced postoperative pain (Monnet-Corti et al., 2006; Harris, 2003).
7. Guided tissue regeneration techniques (Fig. 7)
Figure 7.
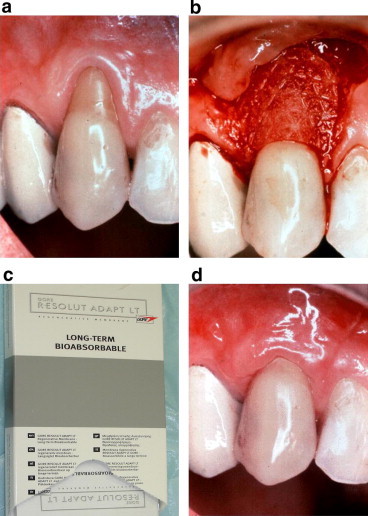
Guided tissue regeneration. (a) Tooth #23 with gingival recession, (b) full thickness flap is reflected, (c) the reabsorbable membrane used, (d) healing after 3 months.
The use of guided tissue regeneration (GTR) procedures for root coverage includes evidence of regeneration of a new periodontal tissue attachment. The outcomes have been attempted with promising clinical and histological results (Harris, 2002). GTR allow the selective repopulation of a root surface by periodontal ligament cells that can form new connective tissue attachment between the root surface and alveolar bone.
Prevention of the migration of cells incapable of forming new attachment onto the root surface is achieved by the placement of a membrane barrier closely adapted to the root surface. These regenerative techniques have mostly been used in conjunction with other techniques for root surface coverage, for example with pedicle grafts where the membrane is placed between the graft and the root to favour repopulation of the root with periodontal ligament cells and true new periodontal ligament attachment formation.
The creation and maintenance of a space between the root surface and the overlying barrier membrane remains the main principle in GTR. A variety of surgical techniques aimed at creating and maintaining space along dehisced or exposed root surfaces have been attempted. These methods have included utilizing titanium-reinforced membranes, grinding the root surface to a concave shape, bending membranes with sutures or screws, and injecting a thick film of sealing fibrin–fibronectin system under the membrane (Lins et al., 2003; Dodge et al., 2000; Trombelli et al., 1995). Encouraging results could be also achieved when bone grafts were added underneath collagen membranes to create and maintain the space that is needed for tissue regeneration during GTR-based root coverage (Fig. 8) (Lee et al., 2002; Wang et al., 2002). One of the factors that may negatively influence the success of this procedure is tissue thickness. A minimum of 1.0 mm of gingival tissue thickness at the site of recession is required if a predictable outcome is to be achieved (Shieh et al., 1997; Muller et al., 2001).
Figure 8.

Bone graft with membrane. (a) Tissue fenestration at #12 region, (b) prepared recipient site, (c) xenogenic bone graft in place, (d) collagen membrane trimmed and placed, (e) flap secured, (f) healing after 1 month.
8. Acellular dermal matrix (ALLODERM®)
The disadvantages of harvesting free soft tissue autografts lie in the postoperative discomfort associated with an extra surgical site, as well as the limitations of available donor tissue. Consequently, several soft tissue allograft alternatives have been introduced. These include an acellular dermal matrix (ADM) allograft which used as a substitute for autografts soft tissue in mucogingival surgeries (Fig. 9) (Murata et al., 2008).
Figure 9.

Acellular dermal matrix (Alloderm®). (a) Partial thickness flap raised, (b) the AlloDerm® sutured to the de-epithelialized papillae, (c) the AlloDerm® material prepared, (d) 2 months after surgery.
Acellular dermal matrix (ADM) allograft is processed from human donor skin obtained from approved tissue banks. The preparation of this dermal allograft involves cell component removal and preservation of the ultrastructural integrity (Harris, 2000). ADM became widely utilized in the grafting of burn patients during the 1990s. Intraorally, ADM has since been utilized in a wide range of dental applications such as soft tissue augmentation, augmentation of keratinized gingiva, as a barrier membrane, as a soft tissue grafting material to cover amalgam tattoos, and for root coverage procedures (Harris, 2004; Joly et al., 2007). Many clinical studies revealed the effectiveness of ADM in the treatment of gingival recession defects. A meta-analysis comparing the efficacy of ADM-allografts to other methods concluded that ADM-based root coverage therapy can be used successfully to repair gingival recession defects and to increase keratinized gingival (Gapski et al., 2005).
9. Long-term predictable outcomes
The goals of the treatment of gingival recession have changed with time, from preventing further progression of gingival recession by increasing the amount of gingival tissue (by means of a gingival graft) apical to the recession margin to achieving predictable root coverage to solve patients’ esthetic demands (Zucchelli and De Sanctis, 2005). The overall esthetic outcome of root coverage procedures has become a concern, depending on the final colour and tissue blend of the treated area.
Since the true benefit for the patient is not only improved esthetics but also the stability of the result over time, it is relevant to evaluate whether or not these successful outcomes remain stable for long term. Unfortunately, the vast majority of studies have relatively short follow-up periods. In a review of root coverage literatures, only few studies had follow-up periods of over 2 years (Agudio et al., 2008).
The initial graft tissue thickness is the critical factor associated with complete root coverage procedure. Other anatomical factors have been proposed as essential factors to maintain long term complete root coverage (Huang et al., 2005). The level of adjacent periodontal tissue, i.e., interdental papilla and alveolar bone, showed direct impact to the final results (Haghighati et al., 2009). It can promote an adequate vascularization in the flaps and grafts, which is the main prerequisite for long term wound healing. If these conditions are not satisfied, tissue necrosis and scarred healing will occur, resulting in a reparative and not a regenerative process (Zucchelli et al., 2006; Miller, 1987).
10. Conclusion
The management of gingival recession and its sequelae is based on a thorough assessment of the etiological factors and the degree of involvement of the tissues. The initial part of the management of the patient with gingival recession should be preventive and any pain should be managed and disease should be treated. The degree of gingival recession should be monitored for signs of further progression. When esthetics is the priority and periodontal health is good then surgical root coverage is a potentially useful therapy. Numerous therapeutic solutions for recession defects have been proposed in the periodontal literature and modified with time according to the evolution of clinical knowledge. Careful case selection and surgical management are critical if a successful outcome is to be achieved.

References
- Agudio G., Nieri M., Rotundo R., Cortellini P., Pini Prato G. Free gingival grafts to increase keratinized tissue: a retrospective long-term evaluation (10 to 25 years) of outcomes. J. Periodontol. 2008;79(4):587–594. doi: 10.1902/jop.2008.070414. [DOI] [PubMed] [Google Scholar]
- Allen E.P. Pedicle flaps, gingival grafts, and connective tissue grafts in aesthetic treatment of gingival recession. Pract. Periodont. Aesthet. Dent. 1993;5(5):29–38. 40; quiz 40. [PubMed] [Google Scholar]
- Allen A.L. Use of the supraperiosteal envelope in soft tissue grafting for root coverage. I. Rationale and technique. Int. J. Periodont. Rest. Dent. 1994;14(3):216–227. [PubMed] [Google Scholar]
- Al-Zahrani M.S., Bissada N.F., Ficara A.J., Cole B. Effect of connective tissue graft orientation on root coverage and gingival augmentation. Int. J. Periodont. Rest. Dent. 2004;24(1):65–69. [PubMed] [Google Scholar]
- Andia D.C., Martins A.G., Casati M.Z., Sallum E.A., Nociti F.H. Root coverage outcome may be affected by heavy smoking: a 2-year follow-up study. J. Periodontol. 2008;79(4):647–653. doi: 10.1902/jop.2008.070471. [DOI] [PubMed] [Google Scholar]
- Baelum V., Fejerskov O., Karring T. Oral hygiene, gingivitis and periodontal breakdown in adult Tanzanians. J. Periodontal Res. 1986;21(3):221–232. doi: 10.1111/j.1600-0765.1986.tb01454.x. [DOI] [PubMed] [Google Scholar]
- Bruno J.F. Connective tissue graft technique assuring wide root coverage. Int. J. Periodont. Rest. Dent. 1994;14(2):126–137. [PubMed] [Google Scholar]
- Clauser C., Nieri M., Franceschi D., Pagliaro U., Pini-Prato G. Evidence-based mucogingival therapy. Part 2: ordinary and individual patient data meta-analyses of surgical treatment of recession using complete root coverage as the outcome variable. J. Periodontol. 2003;74(5):741–756. doi: 10.1902/jop.2003.74.5.741. [DOI] [PubMed] [Google Scholar]
- Dodge J.R., Greenwell H., Drisko C., Wittwer J.W., Yancey J., Rebitski G. Improved bone regeneration and root coverage using a resorbable membrane with physically assisted cell migration and DFDBA. Int. J. Periodont. Rest. Dent. 2000;20(4):398–411. [PubMed] [Google Scholar]
- Gapski R., Parks C.A., Wang H.L. Acellular dermal matrix for mucogingival surgery: a meta-analysis. J. Periodontol. 2005;76(11):1814–1822. doi: 10.1902/jop.2005.76.11.1814. [DOI] [PubMed] [Google Scholar]
- Haghighat K. Modified semilunar coronally advanced flap. J. Periodontol. 2006;77(7):1274–1279. doi: 10.1902/jop.2006.050426. [DOI] [PubMed] [Google Scholar]
- Haghighati F., Mousavi M., Moslemi N., Kebria M.M., Golestan B. A comparative study of two root-coverage techniques with regard to interdental papilla dimension as a prognostic factor. Int. J. Periodont. Rest. Dent. 2009;29(2):179–189. [PubMed] [Google Scholar]
- Harris R.J. A comparative study of root coverage obtained with an acellular dermal matrix versus a connective tissue graft: results of 107 recession defects in 50 consecutively treated patients. Int. J. Periodont. Rest. Dent. 2000;20(1):51–59. [PubMed] [Google Scholar]
- Harris R.J. GTR for root coverage: a long-term follow-up. Int. J. Periodont. Rest. Dent. 2002;22(1):55–61. [PubMed] [Google Scholar]
- Harris R.J. Root coverage in molar recession: report of 50 consecutive cases treated with subepithelial connective tissue grafts. J. Periodontol. 2003;74(5):703–708. doi: 10.1902/jop.2003.74.5.703. [DOI] [PubMed] [Google Scholar]
- Harris R.J. A short-term and long-term comparison of root coverage with an acellular dermal matrix and a subepithelial graft. J. Periodontol. 2004;75(5):734–743. doi: 10.1902/jop.2004.75.5.734. [DOI] [PubMed] [Google Scholar]
- Harris R.J., Miller L.H., Harris C.R., Miller R.J. A comparison of three techniques to obtain root coverage on mandibular incisors. J. Periodontol. 2005;76(10):1758–1767. doi: 10.1902/jop.2005.76.10.1758. [DOI] [PubMed] [Google Scholar]
- Harris R.J., Harris L.E., Harris C.R., Harris A.J. Evaluation of root coverage with two connective tissue grafts obtained from the same location. Int. J. Periodont. Rest. Dent. 2007;27(4):333–339. [PubMed] [Google Scholar]
- Huang L.H., Neiva R.E., Wang H.L. Factors affecting the outcomes of coronally advanced flap root coverage procedure. J. Periodontol. 2005;76(10):1729–1734. doi: 10.1902/jop.2005.76.10.1729. [DOI] [PubMed] [Google Scholar]
- Hwang D., Wang H.L. Flap thickness as a predictor of root coverage: a systematic review. J. Periodontol. 2006;77(10):1625–1634. doi: 10.1902/jop.2006.060107. [DOI] [PubMed] [Google Scholar]
- Joly J.C., Carvalho A.M., da Silva R.C., Ciotti D.L., Cury P.R. Root coverage in isolated gingival recessions using autograft versus allograft: a pilot study. J. Periodontol. 2007;78(6):1017–1022. doi: 10.1902/jop.2007.060428. [DOI] [PubMed] [Google Scholar]
- Kassab M.M., Cohen R.E. The etiology and prevalence of gingival recession. J. Am. Dent. Assoc. 2003;134(2):220–225. doi: 10.14219/jada.archive.2003.0137. [DOI] [PubMed] [Google Scholar]
- Kerner S., Sarfati A., Katsahian S., Jaumet V., Micheau C., Mora F. Qualitative cosmetic evaluation after root-coverage procedures. J. Periodontol. 2009;80(1):41–47. doi: 10.1902/jop.2009.080413. [DOI] [PubMed] [Google Scholar]
- Langer B., Langer L. Subepithelial connective tissue graft technique for root coverage. J. Periodontol. 1985;56(12):715–720. doi: 10.1902/jop.1985.56.12.715. [DOI] [PubMed] [Google Scholar]
- Lee E.J., Meraw S.J., Oh T.J., Giannobile W.V., Wang H.L. Comparative histologic analysis of coronally advanced flap with and without collagen membrane for root coverage. J. Periodontol. 2002;73(7):779–788. doi: 10.1902/jop.2002.73.7.779. [DOI] [PubMed] [Google Scholar]
- Lins L.H., de Lima A.F., Sallum A.W. Root coverage: comparison of coronally positioned flap with and without titanium-reinforced barrier membrane. J. Periodontol. 2003;74(2):168–174. doi: 10.1902/jop.2003.74.2.168. [DOI] [PubMed] [Google Scholar]
- Maynard J.G. The value of periodontal plastic surgery-root coverage. Int. J. Periodont. Rest. Dent. 2004;24(1):9. [PubMed] [Google Scholar]
- Milano F. A combined flap for root coverage. Int. J. Periodont. Rest. Dent. 1998;18(6):544–551. [PubMed] [Google Scholar]
- Miller P.D., Jr. A classification of marginal tissue recession. Int. J. Periodont. Rest. Dent. 1985;5(2):8–13. [PubMed] [Google Scholar]
- Miller P.D., Jr. Root coverage using the free soft tissue autograft following citric acid application. III. A successful and predictable procedure in areas of deep-wide recession. Int. J. Periodont. Rest. Dent. 1985;5(2):14–37. [PubMed] [Google Scholar]
- Miller P.D., Jr. Root coverage with the free gingival graft. Factors associated with incomplete coverage. J. Periodontol. 1987;58(10):674–681. doi: 10.1902/jop.1987.58.10.674. [DOI] [PubMed] [Google Scholar]
- Monnet-Corti V., Santini A., Glise J.M., Fouque-Deruelle C., Dillier F.L., Liebart M.F. Connective tissue graft for gingival recession treatment: assessment of the maximum graft dimensions at the palatal vault as a donor site. J. Periodontol. 2006;77(5):899–902. doi: 10.1902/jop.2006.050047. [DOI] [PubMed] [Google Scholar]
- Muller H.P., Stahl M., Eger T. Failure of root coverage of shallow gingival recessions employing GTR and a bioresorbable membrane. Int. J. Periodont. Rest. Dent. 2001;21(2):171–181. [PubMed] [Google Scholar]
- Murata M., Okuda K., Momose M., Kubo K., Kuroyanagi Y., Wolff L.F. Root coverage with cultured gingival dermal substitute composed of gingival fibroblasts and matrix: a case series. Int. J. Periodont. Rest. Dent. 2008;28(5):461–467. [PubMed] [Google Scholar]
- Neely A.L., Holford T.R., Loe H., Anerud A., Boysen H. The natural history of periodontal disease in humans: risk factors for tooth loss in caries-free subjects receiving no oral health care. J. Clin. Periodontol. 2005;32(9):984–993. doi: 10.1111/j.1600-051X.2005.00797.x. [DOI] [PubMed] [Google Scholar]
- Pini-Prato G., Baldi C., Pagliaro U., Nieri M., Saletta D., Rotundo R. Coronally advanced flap procedure for root coverage. Treatment of root surface: root planning versus polishing. J. Periodontol. 1999;70(9):1064–1076. doi: 10.1902/jop.1999.70.9.1064. [DOI] [PubMed] [Google Scholar]
- Raetzke P.B. Covering localized areas of root exposure employing the “envelope” technique. J. Periodontol. 1985;56(7):397–402. doi: 10.1902/jop.1985.56.7.397. [DOI] [PubMed] [Google Scholar]
- Reiser G.M., Bruno J.F., Mahan P.E., Larkin L.H. The subepithelial connective tissue graft palatal donor site: anatomic considerations for surgeons. Int. J. Periodont. Rest. Dent. 1996;16(2):130–137. [PubMed] [Google Scholar]
- Sangnes G., Gjermo P. Prevalence of oral soft and hard tissue lesions related to mechanical toothcleansing procedures. Community Dent. Oral Epidemiol. 1976;4(2):77–83. doi: 10.1111/j.1600-0528.1976.tb01607.x. [DOI] [PubMed] [Google Scholar]
- Santarelli G.A., Ciancaglini R., Campanari F., Dinoi C., Ferraris S. Connective tissue grafting employing the tunnel technique: a case report of complete root coverage in the anterior maxilla. Int. J. Periodont. Rest. Dent. 2001;21(1):77–83. [PubMed] [Google Scholar]
- Seichter U. Root surface caries: a critical literature review. J. Am. Dent. Assoc. 1987;115(2):305–310. doi: 10.14219/jada.archive.1987.0236. [DOI] [PubMed] [Google Scholar]
- Serino G., Wennstrom J.L., Lindhe J., Eneroth L. The prevalence and distribution of gingival recession in subjects with a high standard of oral hygiene. J. Clin. Periodontol. 1994;21(1):57–63. doi: 10.1111/j.1600-051x.1994.tb00278.x. [DOI] [PubMed] [Google Scholar]
- Shieh A.T., Wang H.L., O’Neal R., Glickman G.N., MacNeil R.L. Development and clinical evaluation of a root coverage procedure using a collagen barrier membrane. J. Periodontol. 1997;68(8):770–778. doi: 10.1902/jop.1997.68.8.770. [DOI] [PubMed] [Google Scholar]
- Song J.E., Um Y.J., Kim C.S., Choi S.H., Cho K.S., Kim C.K. Thickness of posterior palatal masticatory mucosa: the use of computerized tomography. J. Periodontol. 2008;79(3):406–412. doi: 10.1902/jop.2008.070302. [DOI] [PubMed] [Google Scholar]
- Souza S.L., Macedo G.O., Tunes R.S., Silveira e Souza A.M., Novaes A.B., Jr., Grisi M.F. Subepithelial connective tissue graft for root coverage in smokers and non-smokers: a clinical and histologic controlled study in humans. J. Periodontol. 2008;79(6):1014–1021. doi: 10.1902/jop.2008.070479. [DOI] [PubMed] [Google Scholar]
- Susin C., Haas A.N., Oppermann R.V., Haugejorden O., Albandar J.M. Gingival recession: epidemiology and risk indicators in a representative urban Brazilian population. J. Periodontol. 2004;75(10):1377–1386. doi: 10.1902/jop.2004.75.10.1377. [DOI] [PubMed] [Google Scholar]
- Tarnow D.P. Semilunar coronally repositioned flap. J. Clin. Periodontol. 1986;13(3):182–185. doi: 10.1111/j.1600-051x.1986.tb01456.x. [DOI] [PubMed] [Google Scholar]
- Tolmie P.N., Rubins R.P., Buck G.S., Vagianos V., Lanz J.C. The predictability of root coverage by way of free gingival autografts and citric acid application: an evaluation by multiple clinicians. Int. J. Periodont. Rest. Dent. 1991;11(4):261–271. [PubMed] [Google Scholar]
- Trombelli L., Schincaglia G.P., Scapoli C., Calura G. Healing response of human buccal gingival recessions treated with expanded polytetrafluoroethylene membranes. A retrospective report. J. Periodontol. 1995;66(1):14–22. doi: 10.1902/jop.1995.66.1.14. [DOI] [PubMed] [Google Scholar]
- Tugnait A., Clerehugh V. Gingival recession – its significance and management. J. Dent. 2001;29(6):381–394. doi: 10.1016/s0300-5712(01)00035-5. [DOI] [PubMed] [Google Scholar]
- van Palenstein Helderman W.H., Lembariti B.S., van der Weijden G.A., van’t Hof M.A. Gingival recession and its association with calculus in subjects deprived of prophylactic dental care. J. Clin. Periodontol. 1998;25(2):106–111. doi: 10.1111/j.1600-051x.1998.tb02416.x. [DOI] [PubMed] [Google Scholar]
- Wang H.L., Kimble K., Eber R. Use of bone grafts for the enhancement of a GTR-based root coverage procedure: a pilot case study. Int. J. Periodont. Rest. Dent. 2002;22(2):119–127. [PubMed] [Google Scholar]
- Wara-aswapati N., Pitiphat W., Chandrapho N., Rattanayatikul C., Karimbux N. Thickness of palatal masticatory mucosa associated with age. J. Periodontol. 2001;72(10):1407–1412. doi: 10.1902/jop.2001.72.10.1407. [DOI] [PubMed] [Google Scholar]
- Wennstrom J.L. Mucogingival therapy. Ann. Periodontol. 1996;1(1):671–701. doi: 10.1902/annals.1996.1.1.671. [DOI] [PubMed] [Google Scholar]
- Wilcko M.T., Wilcko W.M., Murphy K.G., Carroll W.J., Ferguson D.J., Miley D.D. Full-thickness flap/subepithelial connective tissue grafting with intramarrow penetrations: three case reports of lingual root coverage. Int. J. Periodont. Rest. Dent. 2005;25(6):561–569. [PubMed] [Google Scholar]
- Zucchelli G., De Sanctis M. Long-term outcome following treatment of multiple Miller class I and II recession defects in esthetic areas of the mouth. J. Periodontol. 2005;76(12):2286–2292. doi: 10.1902/jop.2005.76.12.2286. [DOI] [PubMed] [Google Scholar]
- Zucchelli G., Cesari C., Amore C., Montebugnoli L., De Sanctis M. Laterally moved, coronally advanced flap: a modified surgical approach for isolated recession-type defects. J. Periodontol. 2004;75(12):1734–1741. doi: 10.1902/jop.2004.75.12.1734. [DOI] [PubMed] [Google Scholar]
- Zucchelli G., Testori T., De Sanctis M. Clinical and anatomical factors limiting treatment outcomes of gingival recession: a new method to predetermine the line of root coverage. J. Periodontol. 2006;77(4):714–721. doi: 10.1902/jop.2006.050038. [DOI] [PubMed] [Google Scholar]
- Zucchelli G., Mounssif I., Stefanini M., Mele M., Montebugnoli L., Sforza N.M. Hand and ultrasonic instrumentation in combination with root-coverage surgery: a comparative controlled randomized clinical trial. J. Periodontol. 2009;80(4):577–585. doi: 10.1902/jop.2009.080485. [DOI] [PubMed] [Google Scholar]


