Abstract
Breast cancer is a heterogeneous disease comprised of at least 5 major tumor subtypes that coalesce as the second leading cause of cancer death in women in the United States. Although metastasis clearly represents the most lethal characteristic of breast cancer, our understanding of the molecular mechanisms that govern this event remains wholly inadequate. Clinically, ~30% of breast cancer patients diagnosed with early-stage disease undergo metastatic progression, an event that (i) severely limits treatment options, (ii) typically results in chemoresistance and low response rates, and (iii) greatly contributes to aggressive relapses and dismal survival rates. Transforming growth factor-β (TGF-β) is a pleiotropic cytokine that regulates all phases of post-natal mammary gland development, including branching morphogenesis, lactation, and involution. TGF-β also plays a prominent role in suppressing mammary tumorigenesis by preventing mammary epithelial cell (MEC) proliferation, or by inducing MEC apoptosis. Genetic and epigenetic events that transpire during mammary tumorigenesis conspire to circumvent the tumor suppressing activities of TGF-β, thereby permitting late-stage breast cancer cells to acquire invasive and metastatic phenotypes in response to TGF-β. Metastatic progression stimulated by TGF-β also relies on its ability to induce epithelial-mesenchymal transition (EMT) and the expansion of chemoresistant breast cancer stem cells. Precisely how this metamorphosis in TGF-β function comes about remains incompletely understood; however, recent findings indicate that the initiation of oncogenic TGF-β activity is contingent upon imbalances between its canonical and noncanonical signaling systems. Here we review molecular and cellular contributions of noncanonical TGF-β effectors to mammary tumorigenesis and metastatic progression.
Keywords: Epithelial-mesenchymal Transition, Metastasis, Signal Transduction, Transforming growth factor-β, Tumor Microenvironment
Introduction
Breast cancer and its associated metastases are the second leading cause of cancer death in women, accounting for more than 40,000 deaths and 211,000 new invasive cancer cases annually in the United States (1). Metastasis is devastating and underlies the deaths of ~90% of patients with solid tumors (2, 3), including those originating in the breast (4, 5). Indeed, the 5 year survival rate of breast cancer patients diagnosed with localized disease is 98%, a figure that drops precipitously to 23% in patients diagnosed with evidence of metastatic disease (6). The dissemination of breast cancer cells, which occurs most frequently to the brain, liver, bone, and lung (7), involves a complex cascade of gene expression and repression that coalesce in an orderly manner to engender distinct stages of the metastatic process, including (i) local invasion through the basement membrane; (ii) intravasation into the vasculature to traverse the circulation; and (iii) extravasation, infiltration, and eventual colonization of secondary organ sites (2, 8-11). Clonal selection theory paints metastasis as the ultimate developmental rung achieved by evolving breast cancer; however, recent evidence indicates that many breast cancers disseminate long before their primary tumors become symptomatic, and in fact, 33% of women diagnosed with mammary tumors (4 mm) already harbor disseminated breast cancer cells in their bone marrow (12-14). Moreover, these micrometastases can remain dormant for years before reemerging as incurable secondary tumors that are surprisingly insensitive to neoadjuvant chemotherapies that originally attacked the primary tumor (15, 16). These clinical correlates point to the presence of a molecular bifurcation in the signaling events that underlie metastatic outgrowth versus those operant in promoting primary tumor development. Presently, science and medicine lack sufficient knowledge to synthesize novel pharmaceuticals capable of specifically targeting and alleviating metastatic progression in cancers of the breast. Although genomic approaches have offered some molecular insights into how genetically distinct breast cancer subtypes may be identified and treated, these analyses have yet to provide information related to (i) “how and when” metastasis transpires during mammary tumorigenesis; (ii) the overall metastatic potential of distinct breast cancer subtypes; and (iii) the impact of conventional chemotherapies and treatment regimens to influence, either positively or negatively, breast cancer metastasis and disease recurrence. Thus, metastasis may in fact represent the last unknown frontier to be interrogated by science and medicine.
Transforming growth factor-β (TGF-β) is a multifunctional cytokine that plays essential roles during branching morphogenesis, lactation, and involution phases of post-natal mammary glands (17, 18). TGF-β is also a powerful tumor suppressor that governs essentially every aspect of the pathophysiology of mammary epithelial cells (MECs), including their ability to proliferate, migrate, differentiate, and survive (5, 19, 20). During mammary tumorigenesis, genetic and epigenetic events undermine the tumor suppressive functions of TGF-β, thereby enhancing the development and progression of evolving breast cancers. Mammary tumorigenesis also elicits dramatic alterations in the architecture of breast cancers and their accompanying microenvironments (e.g., desmoplastic and fibrotic reactions), which further inactivate the tumor suppressing activities of TGF-β (19, 21, 22). Even more remarkably, these abnormal events coalesce to confer TGF-β the ability to stimulate the invasion and metastasis of late-stage breast cancer cells. This peculiar conversion in TGF-β function is known as the “TGF-β Paradox,” which underlies the lethality of TGF-β in metastatic breast cancer cells (19, 23, 24). An emerging explanation for the dichotomous functions of TGF-β may reflect its ability to generate cancer stem cells via its stimulation of epithelial-mesenchymal transition (EMT), an event essential for the initiation of oncogenic TGF-β signaling in breast cancer cells (5, 19). Along these lines, breast cancer resistance to chemotherapies is clearly associated with the acquisition of EMT (25-28), particularly that driven by TGF-β (29, 30), and with alterations in the tumor microenvironment (31). Precisely how TGF-β participates in these inappropriate events remains an active area of scientific research; however, recent findings suggest that imbalances between canonical and noncanonical TGF-β signaling inputs manifest the “TGF-β Paradox” and the acquisition of oncogenic activity by TGF-β.
Here we review recent findings that directly impact our understanding of the role of noncanonical TGF-β signaling systems in regulating its oncogenic activities and ability to promote metastatic progression and EMT in developing mammary carcinomas.
TGF-β Signaling Systems
Canonical TGF-β Signaling
Canonical TGF-β signaling refers to messages transduced by the activation of the latent transcription factors, Smad2 and Smad3, and as such, canonical TGF-β signaling is synonymous with Smad-dependent TGF-β signaling. All intracellular signals stimulated by TGF-β commence upon its binding to three high-affinity transmembrane receptors, namely TGF-β receptors type I (TβR-I), type II (TβR-II), and type III (TβR-III or betaglycan). Mammals express three genetically unique TGF-β cytokines (i.e., TGF-βs 1-3) whose mature and biologically active forms are ~97% identical and exhibit virtually indistinguishable actions in vitro (32, 33). Interestingly, individual TGF-β ligands are expressed in a spatiotemporal manner during embryogenesis and tissue morphogenesis, which contributes to the array of diverse and nonredundant phenotypes displayed by mice lacking distinct TGF-β isoforms (34). Once synthesized, TGF-β ligands are secreted into the extracellular matrix (ECM) as inactive latent complexes whose conversion to active forms transpires through several mechanisms, including proteolysis, reactive oxygen species, acidic microenvironments, and binding to integrins (35, 36). Following their activation, only TGF-βs 1 and 3 can bind directly to TβR-II, while that of TGF-β2 must first bind TβR-III to facilitate presentation to TβR-II. Although TβR-III lacks intrinsic enzymatic activity, TβR-I and TβR-II both possess Ser/Thr protein kinases in their cytoplasmic domains that serve to initiate downstream signaling (19, 37). Indeed, ligand engagement of TβR-II leads to the recruitment, phosphorylation, and activation of TβR-I, which subsequently binds, phosphorylates, and stimulates Smad2/3 (19, 38). Once activated, Smad2/3 rapidly interact physically with the common Smad, Smad4, thereby exposing cryptic nuclear localization sequences that permit these heterotrimeric complexes to accumulate in the nucleus. Upon gaining entry into the nucleus, Smad2/3/4 complexes function in conjunction with a host of transcription factors, enhancers, and repressors that collectively bring about dramatic alterations in gene expression in a cell- and context-specific manner [Fig. 1, left panel; (19, 38)]. In addition, the amplitude and duration of Smad2/3 responses are impacted by their interaction with a variety of adapter molecules, including SARA (39), Hgs (40), PCTA (41), and Dab2 (42, 43). Interestingly, altered expression of SARA and Dab2 have both been linked to the ability of TGF-β to regulate the plasticity of MECs (44-47), suggesting that imbalances in Smad2/3 signaling contribute to oncogenic TGF-β signaling. Along these lines, the focal adhesion adapter protein, p130Cas, can bind and promote the degradation of Smad3, leading to diminished cytostatic activity by TGF-β (48). We showed that mammary tumorigenesis upregulates the expression of p130Cas, an event that enhances TGF-β stimulation of metastatic progression in part via amplifying the coupling of TGF-β to its noncanonical effectors relative to signals derived from their Smad2/3 counterparts (49). The activation of Smad2/3 by TβR-I is governed by the inhibitory Smad, Smad7, whose binding to TβR-I occludes its ability to phosphorylate Smad2/3 (50-52), as well as recruits the E3 ubiquitin ligase, Smurf1/2, to promote TGF-β receptor ubiquitination, internalization, and degradation (53, 54). In addition, the functions of Smad7 are positively regulated by its binding to STRAP (55), but negatively regulated by its interactions with AMSH2 (56) and Arkadia (57). Finally, canonical TGF-β signaling can be terminated through several distinct mechanisms, including (i) dephosphorylation of Smad2/3 by the nuclear phosphatase PPM1A (58); (ii) degradation of Smad2/3 following their ubiquitination by Smurf1, Smurf2, and SCF/Roc1 (59-62); and (iii) reversible monoubiquitination of Smad4 by that governs its binding to activated Smad2/3 (63).
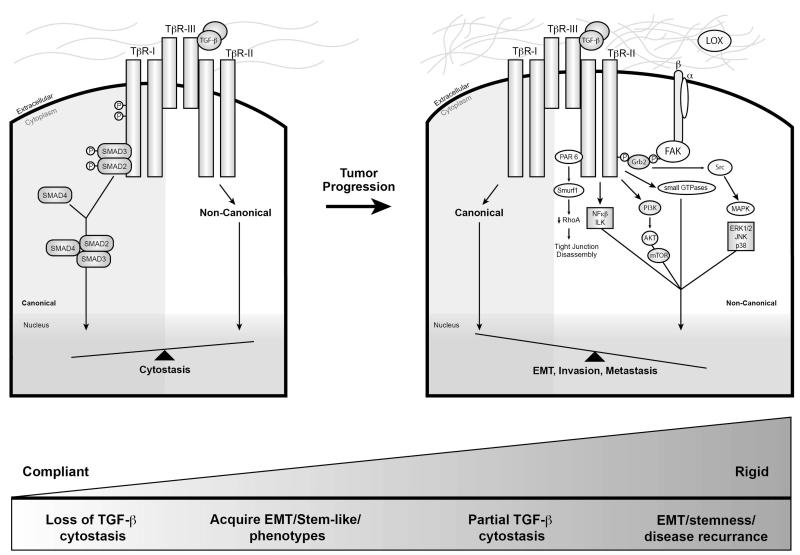
Figure 1.
Schematic depicting the canonical and noncanonical TGF-β signaling systems activated during mammary tumorigenesis. Transmembrane signaling by TGF-β is stimulated upon its binding and activation of the Ser/Thr protein kinase receptors, TβR-I and TβR-II. The physical interaction of TGF-β with either TβR-III or TβR-II facilitates the recruitment and transphosphorylation of TβR-I, resulting in its activation and subsequent phosphorylation of the receptor-activated Smads, Smad2 and Smad3. Once activated, Smad2/3 form heterocomplexes with Smad4 and translocate to the nucleus to regulate the expression of TGF-β-responsive genes in concert with an ever expanding list of transcriptional coactivators and repressors. This branch of the bifurcated TGF-β signaling system represents the “canonical” or “Smad2/3-dependent” TGF-β pathway, which is the predominant pathway coupled to cytostasis and activated by TGF-β in normal MECs (left panel). Alternatively, TGF-β also activates a variety of “noncanonical” or “Smad2/3-independent” effectors, including Par6, NF-κB, ILK, FAK, Src, Rho-family GTPases, MAP kinases, and the PI3K:AKT:mTOR signaling axis (right panel). During EMT and mammary tumorigenesis, the balance between canonical and noncanonical TGF-β signaling systems becomes distorted and favors coupling to noncanonical effector systems, an event that manifests the “TGF-β Paradox” and the initiation of EMT, invasion, and metastasis. These events are further exacerbated by elevated deposition and eventual cross-linking of ECM molecules within tumor microenvironments (LOX, right panel), an event that promotes tumor rigidity and the activation of mechanotransduction pathways operant in amplifying noncanonical TGF-β signaling and its oncogenic activities in mammary tumors. See text for additional details.
The essential function of Smad2/3 and canonical TGF-β signaling in suppressing tumorigenesis, including those occurring in the breast, is well documented in the scientific literature (see (38, 64, 65)). Unfortunately, it remains unclear as to the extent to which canonical TGF-β signaling collaborates with its noncanonical counterparts in mediating the oncogenic activities of TGF-β in late-stage breast cancer. For instance, both canonical and noncanonical TGF-β signaling are essential for TGF-β stimulation of EMT in MECs (5, 66-69). Moreover, cross-talk between Smad2/3 and the noncanonical TGF-β effector, Ras, is sufficient in driving EMT and metastasis (70, 71). We have shown that sustained EMT induced by TGF-β selectively diminishes Smad3 expression following the activation of several noncanonical TGF-β effectors, including p130Cas (49), GSK-3β (72), and a NF-κB:Cox-2:PGE2:EP2 signaling axis (72-75). Yet how these individual events coalesce during distinct stages of metastatic progression remain purely speculative, as is the nature of these signaling collaborations to the behaviors of normal MECs. The molecular readouts of Smad2/3 signaling are also regulated by the phosphorylation of their proline-rich linker domains by a host of Ser/Thr protein kinases. Indeed, activated Ras promotes ERK1/2-mediated phosphorylation of Smad2/3 linker domains, leading to a reduction in their ability to undergo nuclear translocation (76). However, ERK1/2-mediated phosphorylation of the MH1 domain of Smad2/3 was shown to enhance its transcriptional activity (77), suggesting that the location of the phospho-accepting residue has dramatic effects on Smad2/3 function. Likewise, stimulating JNK or its upstream activator, MEKK1, both enhance Smad2/3 signaling in response to TGF-β (78, 79), as does that mediated by casein kinase I-ε (80). In stark contrast, the phosphorylation of Smad2/3 by PKC (81), calmodulin kinase II (82), and GSK-3 (83) all suppress the intracellular communications propagated by canonical TGF-β signaling. Collectively, these studies highlight the complexities associated with TGF-β signaling and the need to further dissect the molecular interactions between Smad2/3 and their noncanonical counterparts in mediating the biology and pathology of TGF-β in normal and malignant MECs.
Noncanonical TGF-β Signaling Systems
In addition to its ability to activate Smad2/3, TGF-β also regulates the pathophysiology of MECs by stimulating an ever expanding array of noncanonical signaling molecules (i.e., Smad2/3-independent), whose activation and biological activities span all cellular compartments. Recent studies by our group (49, 72-75, 84-91) and others (92, 93) support the idea that inappropriate imbalances between canonical and noncanonical TGF-β signaling pathways manifest the “TGF-β Paradox” and the acquisition of oncogenic signaling by TGF-β in developing and progressing mammary tumors (Fig. 1, right panel). In the succeeding sections, we highlight prominent noncanonical effectors activated by TGF-β and discuss their role in mediating oncogenic TGF-β signaling in cancers of the breast.
Integrin and Focal Adhesion Signaling
Integrins are heterodimeric transmembrane receptors that specialize in linking the ECM to the cytoskeletal apparatus within normal and malignant cells (94). Interestingly, individual tissues bear a unique “fingerprint” through their expression of unique and distinguishing ECM signatures (95), which are readily recognized and complemented by an equally diverse array of integrin expression. Importantly, carcinoma cells undergoing neoplastic development can alter their integrin expression profiles to reflect changes within the tumor microenvironment, as well as those necessary for metastatic progression (94). Indeed, integrin activation and signaling is essential to cell proliferation, survival, migration, and invasion, and to the development of chemoresistance in breast cancer cells (96). These integrin-mediated functions are surprisingly reminiscent of those attributed to TGF-β during its stimulation of metastatic progression of mammary tumors, and as such, these observations suggest the potential involvement of integrins in oncogenic TGF-β signaling. Accordingly, integrins αvβ6 and αvβ8 function in binding and activating latent TGF-β complexes, a mechanism that involves matrix metalloproteinase (MMP)-14 and the proteolytic release of active TGF-β to affect the behaviors of neighboring cells (97, 98). Furthermore, TGF-β stimulates the expression of αvβ3 integrin, which confers migratory and invasive phenotypes to normal and malignant MECs, as well as mediates pulmonary metastasis induced by TGF-β in late-stage breast cancer cells (85-87). Mechanistically, elevated expression of β3 integrin interacts physically with TβR-II and promotes its phosphorylation on Tyr284 by Src. Following its phosphorylation, Tyr284 serves as a docking site for ShcA and Grb2, leading to the amplified activation of p38 MAPK and the acquisition of EMT phenotypes by MECs (85-87). Importantly, pharmacologic or genetic manipulations to inactivate this noncanonical signaling axis are sufficient in blocking oncogenic TGF-β signaling and its stimulation of EMT and metastasis in malignant MECs (85-87). Along these lines, administration of TβR-I inhibitors to mice prevents the metastasis of breast cancer cells to bone and the lungs in part via diminished expression of αvβ3 integrin (99, 100). Subsequent studies established focal adhesion kinase (FAK) as the adapter molecule operant in bridging the formation of β3 integrin:TβR-II complexes (88), and as an essential mediator for TGF-β to (i) stimulate EMT and metastasis in breast cancer cells (49, 88), (ii) induce macrophage infiltration into developing mammary tumors (88); and (iii) facilitate EGFR-dependent metastatic progression in malignant MECs (89). In the presence of degraded ECM fragments, the scaffolding functions of FAK enable the formation of complexes comprised of β1 integrins and TGF-β receptors, which initiate oncogenic TGF-β signaling in a ligand-independent manner (101). Besides FAK, we also identified p130Cas as a molecular fulcrum that governs the balance between canonical and noncanonical TGF-β signaling during mammary tumorigenesis. Indeed, the phosphorylation and activation of p130Cas enables this adapter molecule to form heteromeric complexes with TβR-I and Smad3, resulting in the degradation of Smad3 and the initiation of metastatic progression stimulated by TGF-β (48, 49). Elevated expression of p130Cas occurs frequently during the progression of mammary tumors and is associated with the development of resistance to adriamycin and tamoxifen (102, 103), and with the increased malignancy of ErbB2 tumors due to enhanced signaling via Src, FAK, Rac1, and MMP-9 (104, 105). Finally, signaling downstream of β1 integrin also mediates TGF-β stimulation of p38 MAPK, JNK, and Dab2 expression, all of which are essential for the acquisition of EMT phenotypes in MECs (46, 106). Along these lines, we recently discovered a novel interaction between β1 and β3 integrins in regulating oncogenic TGF-β, such that pharmacologic or genetic inactivation of β1 integrin engenders a dramatic compensatory upregulation of β3 integrin expression sufficient to restore oncogenic TGF-β signaling in metastatic MECs (J.G. Parvani and W.P. Schiemann, unpublished observation). Thus, metastatic breast cancers may have evolved the means necessary to evade single agent integrin-based therapies through “integrin-switching” (107, 108), and if so, future studies need to identify the collection of integrins operant in mediating the oncogenic activities of TGF-β.
PI3K, AKT, and mTOR
Oncogenic TGF-β signaling is also associated with the activation of phosphoinositide-3-kinase (PI3K) and its downstream target, AKT/PKB, which collectively serve in enhancing breast cancer proliferation, survival, and motility (109). In addition, activation of the PI3K:AKT signaling axis also enables TGF-β to induce EMT and metastatic progression in malignant MECs, doing so via either the direct coupling of TGF-β receptors to the PI3K machinery (110) or indirectly through the ability of TGF-β to transactivate the receptors for EGF (111) and PDGF (112). In fact, dual activation of the receptors for TGF-β and EGF can produce a hyper-EMT response related to the stimulation of PI3K/AKT and ERK1/2. Interestingly, antagonizing PI3K/AKT activity pharmacologically has no effect on the morphological features of EMT, but was sufficient in preventing elevated cell motility and invasion associated with EMT phenotypes (113). These findings suggest that the morphologic and motile phenotypes of EMT may in fact be distinct physiological entities, each coupled to unique branches of the noncanonical TGF-β signaling system. Accordingly, inactivating mTOR (mammalian target of rapamycin) also failed to alter the morphological features of EMT stimulated by TGF-β, but did prevent its ability to induce the invasion of post-EMT MECs (114). The complexities of connecting PI3K:AKT signaling to the oncogenic activities of TGF-β are further highlighted by the ability of AKT to interact physically with Smad3 and prevent its nuclear translocation in response to TGF-β, thereby diminishing the cytostatic activities of TGF-β by enhancing cell survival (115, 116). Finally, recent studies have established AKT2 as an essential mediator of EMT stimulated by TGF-β (45, 47). For instance, heterogeneous nuclear ribronucleoprotein E1 (hnRNP E1) strongly binds to structural elements in the 3′-UTRs of Dab2 and interleukin-like EMT inducer (ILEI) transcripts, thereby repressing their translation and subsequent induction of EMT in polarized MECs. In response to TGF-β, Akt2 readily phosphorylates and inactivates hnRNP E1, leading to its release from Dab2 and ILEI mRNA and the initiation of EMT and metastatic progression in MECs (45, 47). Thus, the ability of TGF-β to regulate the translation and elongation of transcripts associated with the EMT process may represent a unique clinical target to alleviate breast cancer metastasis by overriding noncanonical TGF-β signaling inputs coupled to PI3K:AKT:mTOR activation.
Rho-family GTPases
Recent studies have implicated members of the Rho GTPase family (i.e., RhoA/B/C, Rac1, and Cdc42) in mediating the initiation of oncogenic TGF-β signaling (69, 117, 118). Indeed, these small plasma membrane-associated GTP-binding proteins collaborate with integrins and other receptor systems to regulate a wide array of cellular functions, including alterations in cell adhesion, morphology, and motility reflecting the generation of filopodia (e.g., Cdc42), lamellipodia (e.g., Rac1), and actin stress fibers (e.g., RhoA) (119, 120). Thus, these findings implicate Rho-family GTPases as potential participants in all stages of the metastatic cascade. Accordingly, TGF-β stimulation of EMT requires RhoA activation, as well as that of its downstream effector, p160ROCK (121). Additionally, the phosphorylation of Par6 by TβR-II results in the ubiquitination and degradation of RhoA (122, 123), presumably leading to upregulated Snail expression that promotes the E-cadherin deficiencies associated with EMT phenotypes (124). On a similar note, the ability of TGF-β to suppress RhoC expression also elicits the dissolution of junctional complexes by inducing the proteosomal degradation of E-cadherin (124). More recently, TGF-β has been observed to induce the phosphorylation of CdGAP, a RhoGAP that only targets Rac1 and Cdc42, leading to elevated cell motility and invasion in ErbB2-positive breast cancers (125). Independent of its ability to bind ligand, TβR-III bound to β-arrestin2 elicits constitutive activation of Cdc42, which inhibits directional migration of ovarian and breast cancer cells (126). Finally, RhoA expression is differentially regulated by TGF-β-responsive microRNAs (miRs), such that TGF-β stimulation of miR-155 expression promotes EMT by degrading RhoA (127), while that of miR-31 suppresses breast cancer metastasis in part by reducing RhoA expression (128, 129). Taken together, these findings highlight the functional complexities associated with the expression and activation of Rho-family GTPases during metastatic progression stimulated by TGF-β.
MAP Kinases
A major mechanism whereby TGF-β induces EMT and metastatic progression is through the stimulation of members of the MAP kinase family of dual-specificity protein kinases, which includes ERK1/2 (extracellular signal-related kinase 1 and 2), JNK (c-Jun N-terminal kinase, and p38 MAPK (106, 130-132). Indeed, TGF-β stimulation of EMT and its accompanying delocalization of E-cadherin and ZO-1 from the plasma membrane requires ERK1/2 activation, a cellular reaction abrogated by administration of MEK1/2 inhibitors (132). Likewise, rendering MECs deficient in Dab2 expression prevents TGF-β from stimulating JNK, and from promoting MEC migration and fibronectin expression during EMT (46). Elevated tumor expression of type I collagen has been shown to induce JNK activation (133). As such, pharmacological inhibition of either JNK or PI3K activity abrogates the ability of type I collagen to promote the migration and metastasis of breast cancer cells (134). The activation of p38 MAPK by TGF-β in normal and malignant MECs requires these cells to express either β1 (106) or β3 integrins (85-87). As mentioned previously, we defined a novel signaling axis comprised of αvβ3 integrin:Src:FAK:p130Cas:TβR-II:Grb2 that is critical for TGF-β stimulation of p38 MAPK, EMT, and pulmonary metastasis of breast cancer cells (49, 85-88). In addition, this signaling axis also confers oncogenic activity to EGF, including its ability to facilitate p38 MAPK activation and metastatic progression in post-EMT populations of breast cancer cells (89). Recently, an alternative mechanism operant in activating JNK and p38 MAPK by TGF-β has been elucidated. Indeed, following their activation by cytokine, TGF-β receptors interact physically with TRAF6 (TNF receptor-associated factor 6), thereby enabling this E3 ligase to ubiquitinate and activate TAK1 and its eventual stimulation of JNK and p38 MAPK (135, 136). Importantly, depleting MECs of TRAF6 expression fails to affect canonical TGF-β signaling; however, this same cellular condition prevents TGF-β from activating JNK and p38 MAPK, as well as from stimulating EMT (135, 136). Collectively, these studies highlight the importance of MAP kinases in mediating the acquisition of oncogenic signaling by TGF-β, leading to the hypothesis that chemotherapeutic targeting of MAP kinase pathways may reinstate the cytostatic function of TGF-β by normalizing the inherent balance between its canonical and noncanonical signaling systems.
Nuclear Factor-κB
NF-κB is an essential mediator of inflammation associated with the growth, survival, invasion and angiogenesis of developing neoplasms (137). TGF-β typically represses NF-κB activity in normal cells by inducing the expression of IκBα (138, 139), or by preventing the degradation of IκBα via the formation of TβR-III:β-arrestin2 complexes (140). In stark contrast, mammary tumorigenesis paradoxically converts TGF-β from an inhibitor to a stimulator of NF-κB activity. In doing so, TGF-β acquires the ability to form TβR-I:xIAP:TAB1:TAK1:IKKβ complexes in malignant MECs, as well as in their normal counterparts undergoing EMT in response to TGF-β (72-74). Uncoupling TGF-β from NF-κB activation dramatically inhibits (i) mammary tumor development in mice in part via regulation of the innate immune system (73), and (ii) the acquisition of EMT and invasive phenotypes in normal and malignant MECs (72-74, 141). Along these lines, the coupling of TGF-β to NF-κB facilitates Ras-transformed breast cancer cells to undergo EMT and colonize the lung (142), as well as promotes the formation of an autocrine Cox-2:PGE2:EP2 signaling cascade essential for metastatic progression and EMT induced by TGF-β (72, 75). Future studies need to assess the relative contribution of NF-κB in the acquisition of chemoresistant phenotypes displayed by late-stage mammary tumors, particularly those subjected to the oncogenic activities of TGF-β.
Lysyl oxidase (LOX)
Lysyl oxidase (LOX) belongs to a five member gene family of copper-dependent amine oxidases (LOX, LOXL1, LOXL2, LOXL3, and LOXL4) that function in cross-linking collagen and elastin in the ECM (143, 144). The cross-linking activity of LOX leads to increased ECM tension and rigidity in developing mammary tumors, which enhances integrin-mediated mechanotransduction coupled to the induction of breast cancer invasion and metastasis (145, 146). Elevated LOX expression is also associated with hypoxia-induced metastasis of breast cancer cells in mice, and with increased metastatic burden and poor survival in breast cancer patients (147, 148). Interestingly, the hydrogen peroxide produced as a byproduct of LOX activity leads to Rac1 activation through the assembly of p130Cas/Crk/Dock180 complexes (149). Along these lines, we recently observed LOX expression and secretion to be stimulated by TGF-β in normal and malignant MECs, and in 4T1 mammary tumors produced in mice (90). Additionally, antagonizing the expression and activity of LOX impairs the ability of TGF-β to induce EMT and invasion, as well as partially uncouples TGF-β from the activation of p38 MAPK in metastatic cells (90). Even more remarkably, we demonstrated that exposing late-stage breast cancer cells to compliant microenvironments is sufficient in reinstating the cytostatic function of TGF-β, a reaction that is readily reversed by rendering these same 3D-organotypic cultures mechanically rigid by the inclusion of type I collagen. Importantly, inhibiting the activities of TGF-β or LOX, or degrading hydrogen peroxide in rigid cultures abrogates oncogenic TGF-β signaling (90), thereby implicating LOX as an important mediator of breast cancer progression stimulated by TGF-β. Finally, the formation of premetastatic niches has been linked to LOX and its ability to stimulate collagen cross-linking and fibronectin production, which coalesce to recruit bone marrow-derived cells (BMDCs) to future sites of metastasis (147). TGF-β also induces BMDC recruitment to premetastatic niches (150), suggesting a clinically important link between TGF-β and its stimulation of LOX expression in mediating the establishment of premetastatic niches. Future studies need to demonstrate the validity of this supposition, as well as determine the chemotherapeutic effectiveness of preventing LOX expression or activation as a novel means to alleviate oncogenic TGF-β signaling in cancers of the breast.
Noncanonical TGF-β Signaling and MEC Plasticity
EMT
The ability of TGF-β to promote metastatic progression is strongly linked to EMT, which represents a transdifferentiation process that enables immotile, polarized MECs to acquire highly motile, apolar fibroblastoid-like phenotypes (5, 69, 151). For instance, MECs undergoing EMT exhibit several unique features, including (i) the loss of cell polarity due to downregulated expression of epithelial cell markers (e.g., E-cadherin, ZO-1, and β4 integrin); (ii) cytoskeletal architecture reorganization and intracellular organelle redistribution; (iii) upregulated expression of fibroblastoid markers (e.g., vimentin, N-cadherin, α-smooth muscle actin); and (iv) elevated invasion factors (e.g., MMP-9, fibronectin) (5, 69, 151, 152). Generally speaking, these steps underlie the pathophysiological of EMT, which were recently categorized into three distinct subtypes: (i) Type 1 EMT, which refers to the plasticity exhibited by epithelial cells during embryogenesis and tissue morphogenesis; (ii) Type 2 EMT, which refers to the plasticity exhibited by epithelial cells during tissue regeneration and fibrotic reactions; and (iii) Type 3 EMT, which refers to the plasticity exhibited by carcinoma cells during metastatic progression (153). Indeed, Type 3 EMT has been observed to confer carcinoma cells a selective invasive advantage to exit both the primary tumor (88) and the circulation at sites of dissemination (89, 154). At first blush, this classification scheme acknowledges that the extent to which an EMT reaction transpires likely reflects the overall health and well-being of the epithelium and its immediate microenvironment. Unfortunately, the vast majority of EMT studies employ “cell-centric” approaches to assess the functional consequences of EMT in normal and malignant cells, and as such, the contributions of the microenvironment to regulating epithelial plasticity remains a critical and underexplored question. Readers desiring in-depth summaries pertaining to the molecular mechanisms whereby TGF-β promotes EMT are directed to several recent reviews (5, 69, 151, 152).
Junctional Dissolution
Tight Junctions
Tight Junctions are localized to lateral cell membranes where they coalesce to form a permeability seal that physically restricts solutes from entering intercellular spaces (155, 156). Structurally, tight junctions are formed by the actions of the transmembrane proteins, claudins, occludins, and JAMs (Junctional Adhesion Molecules), which require ZO-1, -2, and -3 scaffolding proteins for linkage to the actin cytoskeleton (157, 158). Once formed, tight junctions and their constituents play essential roles in regulating the architecture and homeostasis of MECs, and in preventing the initiation of EMT and tumorigenesis (159). TGF-β is a master regulator of the expression and localization of several tight junction components, particularly during EMT. For example, phosphorylation of Par6 in response to TGF-β promotes the ubiquitination and degradation of RhoA, resulting in the dissolution of tight junctions during EMT stimulated by TGF-β (122, 123). By stimulating the formation of Snail1:Smad3:Smad4 complexes in MECs, TGF-β downregulates the expression of the tight junction proteins CAR (coxsackie and adenovirus receptor), occludin, and claudin-3, as well as that of the adherens junction protein, E-cadherin (160, 161). As mentioned previously, TGF-β delocalizes ZO-1 away from tight junctions by activating PI3K and ERK1/2 (110, 132), while co-administration of TGF-β and EGF reduces claudin-1 and occludin expression concomitantly with a loss of epithelial barrier function (162). Somewhat surprisingly, the loss of claudin-1 expression requires Smad4 and β-catenin activity, but was independent of TGF-β and its receptors (163). Finally, recent studies implicate a role of occludin in localizing TGF-β receptors to basolateral (164) or lateral (165) cell surfaces, a sorting reaction that requires the cytoplasmic domains of these receptors (165). Conversely, the secretion of TGF-β ligands is localized specifically to the apical surface in non-transformed cells and to the basolateral surface of transformed cells (165, 166). Collectively, these studies highlight the importance of tight junctions in regulating MEC homeostasis, as well as their potential to coordinate the responses of MECs to TGF-β in a spatiotemporal manner.
Adherens Junctions
E-cadherin is the primary molecule responsible for forming adherens junctions in polarized MECs (167, 168), and the loss of E-cadherin expression in neoplastic MECs leads to their acquisition of EMT, invasive, and metastatic phenotypes that correlate with poor clinical outcomes in breast cancer patients expression (169-171). TGF-β transcriptionally silences E-cadherin expression in malignant MECs by activating a variety of EMT-responsive transcription factors, including Snail, ZEB1/2, or Twist (172). Interestingly, as MECs transdifferentiate and acquire mesenchymal phenotypes they typically undergo “cadherin switching” whereby epithelial E-cadherin is replaced by the upregulated expression of mesenchymal N-cadherin or cadherin-11 (167, 173). Adherens junctions are stabilized by the binding of cadherins to the actin cytoskeleton via their interaction with α- and β-catenins and plakoglobin (167, 168). These events are readily disrupted by TGF-β and its targeting of α- and β-catenins for Tyr-phosphorylation, an event that reduces cell-cell adhesion and alters the actin cytoskeleton (174-176). The ability of TGF-β to downregulate E-cadherin-based cell-cell adhesion depends upon the formation of Smad2:β-catenin complexes (174, 175), and upon the integration of PI3K and PTEN signaling inputs (177). Future studies need to define the precise role that “cadherin switching” plays during metastatic progression stimulated by TGF-β, as well as delineate the relative contributions of canonical and noncanonical TGF-β signaling inputs in mediating these events.
Microenvironments and MEC Plasticity
The biology of TGF-β can largely be divided into two broad categories: regulation of cell cycling versus regulation of cell microenvironments (i.e., extracellular matrix (ECM) remodeling, angiogenesis, fibroblast activation, and immune cell infiltration). Thus, in addition to inducing cytostasis in MECs, TGF-β also governs the behaviors of adjacent fibroblasts, adipocytes, and endothelial cells, as well as their synthesis of paracrine factors and ECM molecules that collectively suppress carcinoma development. During mammary tumorigenesis, the tumor microenvironment readily develops a variety of cellular and structural abnormalities that have a profound impact on TGF-β signaling. For example, targeted inactivation of the TGF-β signaling system in fibroblasts (178) or T cells (179) both elicit carcinoma development due to disruptions of tumor suppressing paracrine signaling networks. Likewise, conditional deletion of TβR-II in mammary gland fibroblasts greatly enhances their proliferative potential and elicits abnormal ductal development (180). Additionally, TβR-II-deficient mammary fibroblasts promote the growth and invasion of breast cancer cells in part via upregulated expression of TGF-α, MSP (macrophage-stimulating protein), and HGF (hepatocyte growth factor) (22, 178, 180, 181). Similar inactivation of TβR-II in breast cancer cells is observed to promote their metastatic progression through the initiation of two inappropriate paracrine signaling axes – namely, SDF-1:CXCR4 and CXCL5:CXCR2 (150). The net-effect of these events result in the recruitment of immature GR1+CD11b+ myeloid cells that drive breast cancer metastasis by inhibiting host tumor immunosurveillance, and by inducing MMP expression (150). Collectively, these findings touch upon the importance of the microenvironment and paracrine signaling networks in dictating the pathophysiological activities of TGF-β in the mammary gland. Readers desiring more in-depth analyses and descriptions of the role of fibroblasts in regulating mammary development and tumorigenesis are directed the accompanying review by Moses and colleagues. In the succeeding sections, we highlight the role of fibronectin and collagen in promoting metastatic progression stimulated by TGF-β.
Fibronectin
TGF-β has long been recognized as a principle player operant in stimulating fibronectin expression and incorporation into the ECM (182). Importantly, elevated fibronectin expression enables dormant MEC micrometastases to reinitiate cell proliferation in a β1 integrin-dependent manner (183). Along these lines, upregulated fibronectin expression in conjunction with that of activated Ras significantly alters MEC integrin expression profiles in a manner reminiscent of “cadherin switching,” such that epithelial α6β4 integrins are replaced by mesenchymal α5β1 integrins. Collectively, these events enhance TGF-β stimulation of EMT and its induction of MEC motility and survival signaling (184). Interestingly, the ability of TGF-β to bestow anchorage-independent properties to responsive cells can be recapitulated by fibronectin administration, a reaction dependent upon integrin signaling (182). Fibronectin production is also associated with the formation of the “premetastatic niche,” which recruits BDMCs to provide a permissive metastatic microenvironment for the arrival of disseminated breast cancer cells (147, 185). Finally, a recent study established the importance of TGF-β secreted by mammary tumors to assemble a fibronectin matrix that is three times more mechanically rigid than matrices assembled by normal MECs (186). Collectively, these findings implicate fibronectin as an essential mediator of metastatic progression stimulated by TGF-β, particularly its ability to respond to signaling inputs derived from integrins and mechanotransduction.
Collagen
In addition to its stimulation of fibronectin expression, TGF-β also has a longstanding relationship with collagen (182), whose elevated expression in mammary tumors associates with increased tumor occurrence and metastasis, as well as with poor clinical outcomes (187, 188). Increased collagen deposition also promotes ECM rigidity, which contributes greatly to the development and progression of mammary tumors (145, 146). Interestingly, TGF-β stimulates basal-like breast cancer cells to express Endo180, which is a cell surface receptor that promotes the (i) growth and motility of highly invasive breast cancer cells, and (ii) internalization and intracellular degradation of collagen (189). Recently, collagen was observed to activate TGF-β receptors in a ligand-independent manner, leading to the dual stimulation of canonical and noncanonical TGF-β effectors in breast cancer cells (101). Collectively, these findings highlight the intimate relationship between collagen and TGF-β in promoting disease progression in breast cancer patients, and suggest that measures capable of neutralizing upregulated collagen expression and activity may offer new inroads to alleviate oncogenic TGF-β signaling.
Novel Modes of MEC Plasticity Regulated by TGF-β
microRNAs
microRNAs are small, noncoding RNAs that (i) typically range from 20-25 base pairs in length, and (ii) play essential roles in suppressing gene expression through their ability to bind to the 3′-UTRs of target mRNAs, which induces either their degradation or translational repression (190). Interestingly, the majority of miRs identified to date localize to fragile genomic regions associated with cancer (191), leading to the notion that microRNA-based expression signatures may be developed as diagnostic platforms for cancer patients. Accordingly, microRNA expression profiling studies have demonstrated the ability of microRNA signatures to readily distinguish normal tissues from their tumorigenic counterparts, as well as to stage and classify human mammary tumors (192-194). Along these lines, differential microRNA expression can function in either suppressing or promoting mammary tumorigenesis, and in governing specific steps of the metastatic cascade, including the induction of MEC migration, invasion, and EMT (195-198). The pathophysiological processes regulated by miRs are highly reminiscent of those controlled by TGF-β, and as such, it is not surprising to learn that microRNAs are active participants in regulating MEC response to TGF-β. For instance, TGF-β stimulation of EMT downregulates the expression of the miR-200 family of miRs, which normally suppresses the expression of the EMT-responsive transcription factors, ZEB1 and ZEB2/SIP1 (199). Consequently, elevated ZEB1 and ZEB2 expression initiate EMT in part by repressing E-cadherin expression in breast cancer cells (199). EMT induced by TGF-β has also been linked to its stimulation of miR-21 expression (200), which enhances the migration and invasion of breast cancers by downregulating the expression of tropomyosin (197, 201). Clinically, high miR-21 expression in early-stage breast cancers is associated with decreased disease-free survival, as well as with significantly elevated expression of TGF-β (202). Canonical TGF-β signaling was recently observed to regulate miR-21 activity by enhancing the processing of its pri-miR-21 transcripts to their pre-miR-21 counterparts, a post-translational mechanism supported by the formation of Smad2/3:DROSHA complexes (203). Finally, canonical TGF-β signaling regulates the differential expression of 28 miRs in MECs undergoing EMT in response to TGF-β. Of these EMT-related miRs, the expression of miR-155 is essential in mediating MEC motility and tight junction dissolution due to a loss of RhoA expression in transitioning MECs (127). Collectively, these studies demonstrate the role of TGF-β in directing microRNA expression in normal and malignant MECs, doing so via employment of intricate transcriptional and post-translational mechanisms. Future studies need to comprehensively map the microRNAome governed by TGF-β, as well as the extent to which targeting microRNA expression can abrogate metastatic progression stimulated by TGF-β in developing mammary tumors.
Acquisition of Stemness
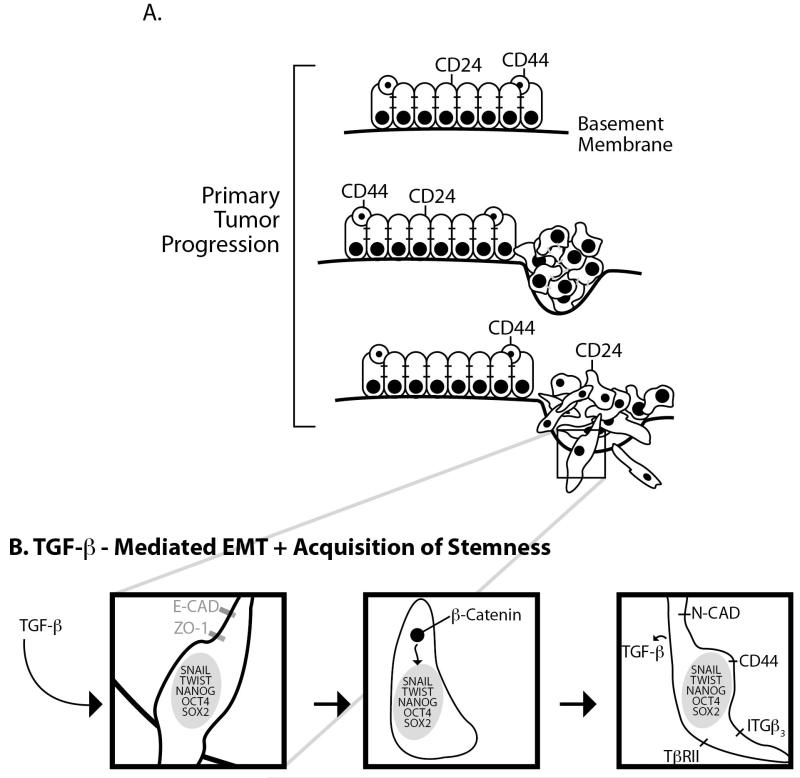
Heterogeneity in cell morphology, gene signatures, and sensitivity to chemotherapeutics are all hallmarks of various human cancers, including those of the breast (204-207). The phenotypic changes associated with oncogenic Type 3 EMT can give rise to the generation and expansion of cancer-initiating cells that possess stem cell-like characteristics (29, 208), including the ability to undergo self-renewal and asymmetrical cell division (204, 205, 209). At present, the origins of cancer stem cells (CSCs) remain controversial; however, recent findings do suggest CSCs may arise through their ability to commandeer a core set of transcription factors during the malignant transformation of normal stem cells, or during the dedifferentiation of bulk tumor cells [Fig. 2; (210-214)]. Transcription factors underlying cellular reprogramming coupled to pluripotency include Nanog, Oct4, Sox2, Klf4, and c-Myc (215), all of which are regulated by TGF-β (216-219).
Figure 2.
The exodus of invasive breast cancer cells from the primary tumor may require EMT and its induction of acquired stemness. A Normal mammary epithelium is comprised of CD24+ luminal cells and CD44+ basal cells (top panel). Tumor initiation in either cell type may confer a proliferative advantage and deregulated growth (middle panel). Disease progression ultimately results in the local invasion of breast cancer cells, followed by their dissemination into the circulation (bottom panel). B Metastatic progression stimulated by TGF-β is coupled to EMT and its ability to (i) induce the expression EMT- and developmentally-responsive transcription factors (left panel); (ii) promote the dissolution of adherens and tight junctional complexes, as well as the downregulation of epithelial phenotypic markers (middle panel); and (iii) stimulate the upregulation of mesenchymal and stem-like phenotypic markers, including CD44.
With respect to breast cancer, recent studies have identified a small CSC population that possess stem cell-like properties and exhibit a CD44high/CD24low antigenic phenotype (209). Interestingly, terminally differentiated luminal MECs readily express ER-α and CD24, which contrasts sharply with their mammary progenitor-like counterparts that express CD44, but not ER-α (30). When stimulated by TGF-β or in response to enforced expression of either Twist or Snail, MECs undergo an EMT program that generates a CD44high/CD24low population of cells that posses stem cell-like and mammosphere forming features (29). The loss of E-cadherin expression that transpires during EMT reinforces these events by permitting the nuclear translocation of β-catenin and its stimulation of CD44 expression (220). Moreover, pharmacological inhibition of TGF-β signaling in breast CSCs suppresses their tumorigenicity in part by restoring E-cadherin expression via mesenchymal-epithelial transitions (30). Interestingly, genomic analysis of primary breast tumors identified clonal genetic differences existing between CD44high/CD24low and CD44low/CD24high breast cancer cells, suggesting that these malignant MEC populations undergo independent evolutionary routes during mammary tumorigenesis. The importance of TGF-β signaling, particularly that mediated by the stem cell markers and noncanonical TGF-β effectors β1 (CD29) and β3 (CD61) integrin, in regulating CSC evolution is supported by the finding that TβR-II is readily expressed in CD44high/CD24low populations as compared to their CD44low/CD24high counterparts, which transcriptionally silences this TGF-β receptor (30). Future studies need to establish the role of “stemness” in manifesting the “TGF-β Paradox” and its initiation of oncogenic TGF-β signaling during mammary tumorigenesis.
Unanswered Questions and Future Directions
Mammary Tumor Heterogeneity and Metastatic Progression
Mammary tumor microenvironments play an essential role governing the growth, metastasis, and chemosensitivity of developing breast cancers (22, 181), as does the relative heterogeneity and clonality displayed by individual carcinoma cells housed within evolving mammary tumors (221). The ability of MECs to undergo “integrin switching” during EMT and metastatic progression stimulated by TGF-β implicates integrins as master regulators in coordinating the interactions between reactive stroma and malignant MECs (85-87, 184). Moreover, changes in integrin expression not only dictate the coupling of TGF-β to its canonical and noncanonical signaling systems (49, 85-89), but also govern the ability of malignant MECs to respond and interact with components in their microenvironments, including reactive fibroblasts, adipocytes, lymphocytes, and endothelial cells (22, 181). Collectively, these dynamic interactions coalesce in aiding MECs to successfully navigate the metastatic cascade and establish secondary lesions at distant organ sites. Simultaneous stimulation of αvβ3 integrin (by vitronectin) and TGF-β receptors is essential in mediating the acquisition of EMT and invasive phenotypes by normal and malignant MECs, and in promoting metastatic progression in triple-negative breast cancer cells (49, 85-88). Thus, the differential vitronectin expression within tumor microenvironments and throughout the periphery may dictate the preferential metastasis of breast cancer cells to the liver, lung, brain, and bone based on integrin expression profiles (7). The importance of β3 integrin to these events is underscored by our recent observation that rendering metastatic MECs deficient in β1 integrin actually enhances, not suppresses, metastatic progression at earlier stages of tumor development (J.P. Parvani and W.P. Schiemann, unpublished observation). Interestingly, targeted inactivation of β3 integrin expression in these same cells abrogates TGF-β stimulation of pulmonary metastasis (87). Thus, while MECs possess considerable plasticity related to their integrin expression profiles, it appears that only a select repertoire of integrins may in fact couple TGF-β to metastatic progression in mammary tumors. Future studies need to establish the repertoire of integrins operant in mediating canonical TGF-β signaling and its cytostatic function versus those integrins operant in mediating oncogenic TGF-β signaling and its aberrantly amplified activation of noncanonical TGF-β effectors.
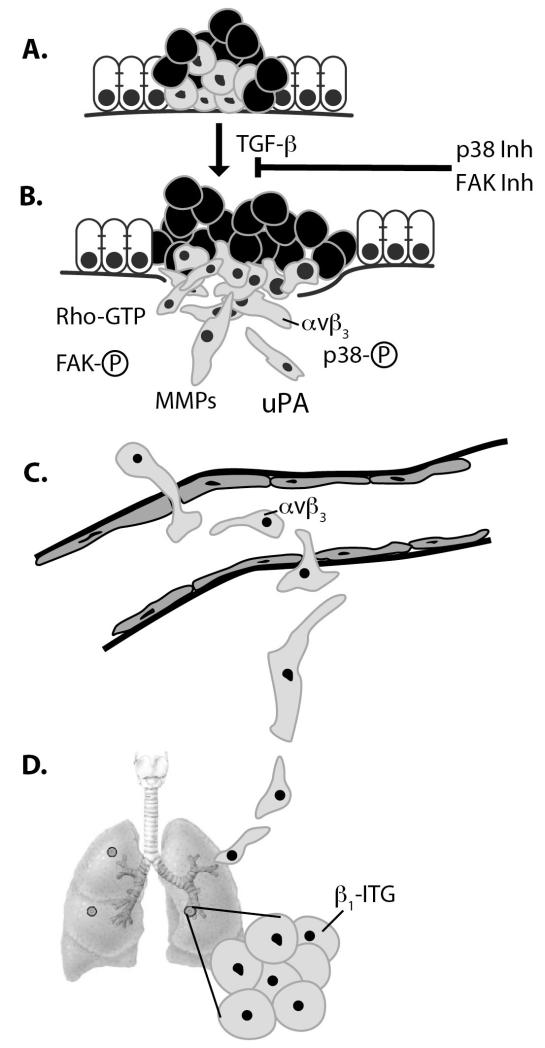
Investigating the role of integrins during cell:cell or cell:ECM interactions is complicated by the intratumoral heterogeneity of carcinoma cells within primary mammary tumors, of which only a minute fraction are actually endowed with the abilities to survive the metastatic cascade [Fig. 3; (204, 222)]. Thus, analyzing the interactions of bulk tumors with their surrounding ECM and microenvironment may be misleading and unrepresentative of the reactions necessary in driving the egress of carcinoma cells out of these dysregulated microenvironments. Along these lines, the extent to which symbiotic relationships between epithelial-like and mesenchymal-like cooperate in mediating completion of the metastatic cascade remain largely unexplored. For instance, in studying several human and murine isogeneic breast cancer progression series (222-224), we have repeatedly identified weakly tumorigenic derivatives that are highly invasive as compared to their more malignant counterparts that are surprisingly noninvasive (M.K Wendt and W.P. Schiemann, unpublished observation). Thus, do weakly tumorigenic and highly invasive MECs generate a readily available route for their weakly invasive counterparts to escape the confines of the primary tumor? And if so, do these “worker cells” traverse the circulation in tandem with their metastatic “queen cells” to facilitate their efficient exodus from the vasculature at suitable metastatic niches? And finally, what role does TGF-β and its noncanonical effectors play in regulating these collective events (Fig. 3). Although future studies need to address these questions, several recent studies do support a collective and collaborative effort in facilitating breast cancer metastasis. First, epithelial-like (non-EMT and noninvasive) and mesenchymal-like (EMT and invasive) MECs were singularly unable to colonize the lungs of mice; however, engrafting both lines simultaneously resulted in robust pulmonary metastasis (225), suggesting that both MEC populations cooperate to complete the metastatic cascade. Along these lines, indolent breast micrometastases can be reactivated by BMDCs mobilized into the circulation by systemic instigation derived from signals (e.g., osteopontin) originating from the primary mammary tumor (226). Finally, aggressive circulating breast caner cells have been observed to “self-seed” and infiltrate established tumors, thereby accelerating metastatic progression in recipient mammary tumors (227). Clearly, future studies need to expand these findings and determine the extent to which these events are either regulated by TGF-β or participate in manifesting the “TGF-β Paradox.”
Figure 3.
Cooperation between distinct subpopulations of breast cancer cells may underlie local invasion and metastasis. A Carcinoma cell heterogeneity is a hallmark of primary mammary tumors and represented as “gray” and “black” breast cancer cells. B TGF-β signaling within the primary tumor microenvironment induces a subpopulation of breast cancer cells to undergo EMT and local invasion (gray cells), doing so via the activation of αvβ3 integrin, FAK, p38 MAPK, and Rho GTPases and their coupling to the production of MMPs and uPA. The efficiency of these events may be enhanced and bolstered by the cooperation of nonmetastatic cells (black cells) to produce “prometastatic” microenvironments. C Once liberated from the primary tumor, metastatic breast cancer cells intravasate the endothelium to gain access to the vascular for systemic dissemination. Surviving transport through the circulatory system is essential for the metastatic cascade and may be linked to upregulated expression of αvβ3 integrin, which is also essential for disseminated breast cancer cells to extravasate the vasculature. D) Colonization and eventual outgrowth of the metastatic lesion is associated with β1 integrin expression.
Smad2/3 Signaling and Metastasis: Prominent Players or Innocent Bystanders?
Although Smads 2 and 3 are often referred to as being a single entity in the scientific literature, recent findings have established distinct roles for Smad2 versus Smad3 in mediating the pathophysiology of TGF-β. For instance, targeted deletion of Smad2 elicits embryonic lethality (228, 229), while Smad3-deficient mice are viable and are highly susceptible to inflammation-induced colon tumorigenesis (230-232). Along these lines, the gene expression profiles coupled specifically to Smad2 activation are readily distinguishable from those coupled to the activation of Smad3 (233-235), findings that offer unique insights into how TGF-β modulates cell growth, motility, and survival (236). With respect to cancers of the breast, experimental inactivation Smad2 augmented breast cancer metastasis to bone, while similar inactivation of Smad3 attenuated this metastatic response by reducing tumor angiogenesis and VEGF expression (237). Likewise, rendering early-stage breast cancer cells deficient in Smad2/3 signaling enhanced their malignancy, while similar manipulations in their late-stage counterparts prevented these breast cancer cells from colonizing the lungs (238, 239). Interestingly, a TβR-I mutant unable to activate Smad2/3 failed to support the ability of breast cancer cells to colonize the lung (240), suggesting that canonical and noncanonical TGF-β signaling inputs coalesce in facilitating metastatic outgrowth. At present, the precise molecular mechanisms that enable these disparate signaling systems to collaborate in promoting metastatic progression by TGF-β remains unclear. Addressing this question is critical to unraveling the mysteries of the “TGF-β Paradox.” For instance, a recent study demonstrated that the administration of bisphosphonates was only effective in suppressing osteolytic bone lesions and canonical TGF-β signaling at early stages of the metastatic process, not in fully established lesions (241). These findings indicate that canonical TGF-β signaling is differentially regulated during specific stages of the metastatic cascade. Accordingly, transient activation of Smad2/3 by TGF-β converted the migration of breast cancer cells from cohesive to single cell programs (242, 243). Quite intriguingly, reinitiation of proliferation programs necessary for pulmonary metastatic outgrowth of these breast cancer cells required them to first inactivate Smad2/3 signaling (242, 243). Thus, it is tempting to speculate that altered elastic moduli govern the coupling of TGF-β to Smad2/3. In support of this supposition, we recently determined that canonical TGF-β signaling is selectively silenced in (i) compliant 3D-organotypic cultures relative to rigid tissue culture plastic, and (ii) pulmonary metastases relative to their site of origin (M.A. Taylor, M.K. Wendt and W.P. Schiemann, unpublished observation). Taken together, these intriguing findings demonstrate the plasticity present in the TGF-β signaling system as carcinoma cells undergo EMT and metastatic outgrowth, presumably reflecting a shift from canonical (i.e., Smad2/3-based) to noncanonical (i.e., non-Smad2/3-based) signaling that originates from altered mechanotransduction and integrin signaling. Future studies need define which stages of the metastatic process are dependent upon TGF-β signaling, as well as delineate which branches of the TGF-β signaling system engender these deadly events.
The Future of TGF-β Targeted Chemotherapies
The challenge in designing pharmaceuticals effective in targeting TGF-β signaling lies in the ability of these agents to circumvent the principles of the “TGF-β Paradox.” For instance, an ideal anti-TGF-β agent would be expected to specifically inactivate the oncogenic activities of TGF-β, while simultaneously preserving and/or enhancing its tumor suppressing functions. Currently, all chemotherapeutics developed against the TGF-β pathway universally function as pan-TGF-β antagonists, and as such, the preclinical and clinical use of these drugs has been shown to enhance the tumorigenicity of early-stage cancers as predicted by the “TGF-β Paradox” (24). We previously hypothesized that the specific targeting of noncanonical TGF-β effectors might provide a novel means to restore its cytostatic function in developing mammary tumors (24). In support of this supposition, we recently discovered three novel noncanonical TGF-β signaling axes that drive EMT and metastatic progression by TGF-β: (i) αvβ3 integrin:FAK: p130Cas:Src:pY284-TβR-II:Grb2:p38 MAPK (49, 85-88); (ii) TAB1:TAK1:IKKβ:xIAP:NF-κB (73, 74); and (iii) Cox-2:PGE2:EP2 (72, 75). Importantly, preventing TGF-β from activating any of these pathways is sufficient in alleviating its metastatic behavior, as well as in partially reinstating its cytostatic function in breast cancer cells. Future studies need to gauge the extent to which these events can be translated into clinical settings to prevent breast cancer metastasis and disease recurrence.
We also envision two additional approaches to offer new opportunities to selectively inhibit noncanonical TGF-β signaling. First, the activation of mechanotransduction by ECM rigidity clearly plays an important role in promoting breast cancer development and progression (145, 147, 244-246), including that stimulated by TGF-β (90). These findings suggest that pharmacological targeting of the tumor microenvironment and its accompanying desmoplastic reactions may provide novel avenues to treat metastatic progression stimulated by TGF-β. Indeed, co-administration of LOX and integrin inhibitors may simultaneously abrogate the oncogenic activities of TGF-β and mechanotransduction in developing mammary tumors. Along these lines, the use of iRGD peptides directed at αv integrins to deliver chemotherapeutics has also proven effective in enhancing drug penetration into breast cancers (247). Thus, employment of iRGD peptides for the delivery of anti-TGF-β agents to mammary tumors may facilitate the specific inactivation of TGF-β signaling at the invasive front, thereby reducing metastatic burden. Second, the development of microRNA-based therapies may permit the fine-tuning of TGF-β behavior by targeting the MicroRNAome in mammary tumors. Indeed, tumor progression has been inhibited in a variety of preclinical models by overexpressing of tumor suppressive miRs (248-250), or by neutralizing the activities of oncogenic miRs (251-254). Given the role of microRNAs in mediating EMT and TGF-β signaling, it stands to reason that identifying the MicroRNAome regulated by TGF-β during its induction of metastatic progression may offer new inroads to enhance the overall survival of breast cancer patients.
Acknowledgements
We thank members of the Schiemann Laboratory for critical comments and reading of the manuscript. W.P.S. was supported by grants from the National Institutes of Health (CA129359), the Komen Foundation (BCTR0706967), and the Department of Defense (BC084651), while M.A.T. was supported by the Department of Defense (BC093128).
Financial Support: W.P.S. was supported by grants from the National Institutes of Health (CA129359), the Komen Foundation (BCTR0706967), and the Department of Defense (BC084651), while M.A.T. was supported by the Department of Defense (BC093128).
Abbreviations
- AKT/PKB
protein kinase B
- BMDC
bone marrow-derived cell
- CSC
cancer stem cell
- ECM
extracellular matrix
- EGF
epidermal growth factor
- EMT
epithelial-mesenchymal transition
- ERK
extracellular signal-regulated kinase
- FAK
focal adhesion kinase
- HGF
hepatocyte growth factor
- hnRNP E1
heterogeneous nuclear ribronucleoprotein E1
- ILEI
interleukin-like EMT inducer
- JNK
c-Jun N-terminal kinase
- MAP kinase
mitogen-activated protein kinase
- MEC
mammary epithelial cell
- MET
mesenchymal-epithelial transition
- miR
microRNA
- MMP
matrix metalloproteinase
- MSP
macrophage-stimulating protein
- MTA3
metastasis associated protein 3
- mTOR
mammalian target of rapamycin
- NF-κB
nuclear factor-κB
- PAI
plasminogen activator inhibitor
- PDGF
platelet-derived growth factor
- PI3K
phosphoinositide-3-kinase
- TβR-I
TGF-β type I receptor
- TβR-II
TGF-β type II receptor
- TβR-III
TGF-β type III receptor
- TGF-β
transforming growth factor-β
- TRAF6
TNF receptor-associated factor 6
- uPA
urokinase plasminogen activator
- uPAR
uPA receptor
- ZO-1
zonula occluden-1
References
- 1.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60(5):277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 2.Nguyen DX, Bos PD, Massague J. Metastasis: from dissemination to organ-specific colonization. Nat Rev Cancer. 2009;9(4):274–84. doi: 10.1038/nrc2622. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen DX, Massague J. Genetic determinants of cancer metastasis. Nat Rev Genet. 2007;8(5):341–52. doi: 10.1038/nrg2101. [DOI] [PubMed] [Google Scholar]
- 4.Yang J, Weinberg RA. Epithelial-mesenchymal transition: at the crossroads of development and tumor metastasis. Dev Cell. 2008;14(6):818–29. doi: 10.1016/j.devcel.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 5.Taylor MA, Parvani JG, Schiemann WP. The pathophysiology of epithelial-mesenchymal transition induced by transforming growth factor-β in normal and malignant mammary epithelial cells. J Mammary Gland Biol Neoplasia. 2010;15(2):169–90. doi: 10.1007/s10911-010-9181-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Altekruse SF, Kosary CL, Krapcho M, Neyman N, Aminous R, Waldron W, et al. SEER Cancer Statistics Review 1975-1007. National Cancer Institute. 2010 2010. [Google Scholar]
- 7.Kennecke H, Yerushalmi R, Woods R, Cheang MC, Voduc D, Speers CH, et al. Metastatic behavior of breast cancer subtypes. J Clin Oncol. 2010;28(20):3271–7. doi: 10.1200/JCO.2009.25.9820. [DOI] [PubMed] [Google Scholar]
- 8.Chiang AC, Massague J. Molecular basis of metastasis. N Engl J Med. 2008;359(26):2814–23. doi: 10.1056/NEJMra0805239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chambers AF, Groom AC, MacDonald IC. Dissemination and growth of cancer cells in metastatic sites. Nat Rev Cancer. 2002;2(8):563–72. doi: 10.1038/nrc865. [DOI] [PubMed] [Google Scholar]
- 10.Weinstat-Saslow D, Steeg PS. Angiogenesis and colonization in the tumor metastatic process: basic and applied advances. FASEB J. 1994;8(6):401–7. doi: 10.1096/fasebj.8.6.7513289. [DOI] [PubMed] [Google Scholar]
- 11.Scheel C, Onder T, Karnoub A, Weinberg RA. Adaptation versus selection: the origins of metastatic behavior. Cancer Res. 2007;67(24):11476–9. doi: 10.1158/0008-5472.CAN-07-1653. [DOI] [PubMed] [Google Scholar]
- 12.Talmadge JE. Clonal selection of metastasis within the life history of a tumor. Cancer Res. 2007;67(24):11471–5. doi: 10.1158/0008-5472.CAN-07-2496. [DOI] [PubMed] [Google Scholar]
- 13.Talmadge JE, Fidler IJ. AACR centennial series: the biology of cancer metastasis: historical perspective. Cancer Res. 2010;70(14):5649–69. doi: 10.1158/0008-5472.CAN-10-1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spratt JS, Spratt JA. Growth Rates. In: Donegan WL, Spratt JS, editors. Cancer of the Breast. 2002. pp. 443–476. [Google Scholar]
- 15.Gupta GP, Massague J. Cancer metastasis: building a framework. Cell. 2006;127(4):679–95. doi: 10.1016/j.cell.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 16.Li F, Tiede B, Massague J, Kang Y. Beyond tumorigenesis: cancer stem cells in metastasis. Cell Res. 2007;17(1):3–14. doi: 10.1038/sj.cr.7310118. [DOI] [PubMed] [Google Scholar]
- 17.Serra R, Crowley MR. TGF-β in mammary gland development and breast cancer. Breast Dis. 2003;18:61–73. doi: 10.3233/bd-2003-18107. [DOI] [PubMed] [Google Scholar]
- 18.Serra R, Crowley MR. Mouse models of transforming growth factor β impact in breast development and cancer. Endocr Relat Cancer. 2005;12(4):749–60. doi: 10.1677/erc.1.00936. [DOI] [PubMed] [Google Scholar]
- 19.Tian M, Schiemann WP. The TGF-β paradox in human cancer: an update. Future Oncol. 2009;5(2):259–71. doi: 10.2217/14796694.5.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barcellos-Hoff MH, Akhurst RJ. Transforming growth factor-β in breast cancer: too much, too late. Breast Cancer Res. 2009;11(1):202. doi: 10.1186/bcr2224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tian M, Neil JR, Schiemann WP. Transforming growth factor-β and the hallmarks of cancer. Cell Signal. 2010 doi: 10.1016/j.cellsig.2010.10.015. PMID: 20940046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bierie B, Moses HL. Tumour microenvironment: TGFβ: the molecular Jekyll and Hyde of cancer. Nat Rev Cancer. 2006;6(7):506–20. doi: 10.1038/nrc1926. [DOI] [PubMed] [Google Scholar]
- 23.Rahimi RA, Leof EB. TGF-β signaling: a tale of two responses. J Cell Biochem. 2007;102(3):593–608. doi: 10.1002/jcb.21501. [DOI] [PubMed] [Google Scholar]
- 24.Schiemann WP. Targeted TGF-β chemotherapies: friend or foe in treating human malignancies? Expert Rev Anticancer Ther. 2007;7(5):609–11. doi: 10.1586/14737140.7.5.609. [DOI] [PubMed] [Google Scholar]
- 25.Sharma SV, Lee DY, Li B, Quinlan MP, Takahashi F, Maheswaran S, et al. A chromatin-mediated reversible drug-tolerant state in cancer cell subpopulations. Cell. 2010;141(1):69–80. doi: 10.1016/j.cell.2010.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Taube JH, Herschkowitz JI, Komurov K, Zhou AY, Gupta S, Yang J, et al. Core epithelial-to-mesenchymal transition interactome gene-expression signature is associated with claudin-low and metaplastic breast cancer subtypes. Proc Natl Acad Sci USA. 2010;107(35):15449–54. doi: 10.1073/pnas.1004900107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Creighton CJ, Li X, Landis M, Dixon JM, Neumeister VM, Sjolund A, et al. Residual breast cancers after conventional therapy display mesenchymal as well as tumor-initiating features. Proc Natl Acad Sci USA. 2009;106(33):13820–5. doi: 10.1073/pnas.0905718106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Farmer P, Bonnefoi H, Anderle P, Cameron D, Wirapati P, Becette V, et al. A stroma-related gene signature predicts resistance to neoadjuvant chemotherapy in breast cancer. Nat Med. 2009;15(1):68–74. doi: 10.1038/nm.1908. [DOI] [PubMed] [Google Scholar]
- 29.Mani SA, Guo W, Liao MJ, Eaton EN, Ayyanan A, Zhou AY, et al. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell. 2008;133(4):704–15. doi: 10.1016/j.cell.2008.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shipitsin M, Campbell LL, Argani P, Weremowicz S, Bloushtain-Qimron N, Yao J, et al. Molecular definition of breast tumor heterogeneity. Cancer Cell. 2007;11(3):259–73. doi: 10.1016/j.ccr.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 31.Albini A, Sporn MB. The tumour microenvironment as a target for chemoprevention. Nat Rev Cancer. 2007;7(2):139–47. doi: 10.1038/nrc2067. [DOI] [PubMed] [Google Scholar]
- 32.Blobe GC, Schiemann WP, Lodish HF. Role of transforming growth factor β in human disease. N Engl J Med. 2000;342(18):1350–8. doi: 10.1056/NEJM200005043421807. [DOI] [PubMed] [Google Scholar]
- 33.Massague J. TGF-β signal transduction. Annu Rev Biochem. 1998;67:753–91. doi: 10.1146/annurev.biochem.67.1.753. [DOI] [PubMed] [Google Scholar]
- 34.Chang H, Brown CW, Matzuk MM. Genetic analysis of the mammalian transforming growth factor-β superfamily. Endocr Rev. 2002;23(6):787–823. doi: 10.1210/er.2002-0003. [DOI] [PubMed] [Google Scholar]
- 35.Nishimura SL. Integrin-mediated transforming growth factor-β activation, a potential therapeutic target in fibrogenic disorders. Am J Pathol. 2009;175(4):1362–70. doi: 10.2353/ajpath.2009.090393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rifkin DB. Latent transforming growth factor-β (TGF-β) binding proteins: orchestrators of TGF-β availability. J Biol Chem. 2005;280(9):7409–12. doi: 10.1074/jbc.R400029200. [DOI] [PubMed] [Google Scholar]
- 37.Massague J, Gomis RR. The logic of TGFβ signaling. FEBS Lett. 2006;580(12):2811–20. doi: 10.1016/j.febslet.2006.04.033. [DOI] [PubMed] [Google Scholar]
- 38.Massague J, Seoane J, Wotton D. Smad transcription factors. Genes Dev. 2005;19(23):2783–810. doi: 10.1101/gad.1350705. [DOI] [PubMed] [Google Scholar]
- 39.Tsukazaki T, Chiang TA, Davison AF, Attisano L, Wrana JL. SARA, a FYVE domain protein that recruits Smad2 to the TGFβ receptor. Cell. 1998;95(6):779–91. doi: 10.1016/s0092-8674(00)81701-8. [DOI] [PubMed] [Google Scholar]
- 40.Miura S, Takeshita T, Asao H, Kimura Y, Murata K, Sasaki Y, et al. Hgs (Hrs), a FYVE domain protein, is involved in Smad signaling through cooperation with SARA. Mol Cell Biol. 2000;20(24):9346–55. doi: 10.1128/mcb.20.24.9346-9355.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Faresse N, Colland F, Ferrand N, Prunier C, Bourgeade MF, Atfi A. Identification of PCTA, a TGIF antagonist that promotes PML function in TGF-β signalling. EMBO J. 2008;27(13):1804–15. doi: 10.1038/emboj.2008.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hocevar BA, Smine A, Xu XX, Howe PH. The adaptor molecule Disabled-2 links the transforming growth factor β receptors to the Smad pathway. EMBO J. 2001;20(11):2789–801. doi: 10.1093/emboj/20.11.2789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Penheiter SG, Singh RD, Repellin CE, Wilkes MC, Edens M, Howe PH, et al. Type II transforming growth factor-β receptor recycling is dependent upon the clathrin adaptor protein Dab2. Mol Biol Cell. 2010;21(22):4009–19. doi: 10.1091/mbc.E09-12-1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Runyan CE, Hayashida T, Hubchak S, Curley JF, Schnaper HW. Role of SARA (SMAD anchor for receptor activation) in maintenance of epithelial cell phenotype. J Biol Chem. 2009;284(37):25181–9. doi: 10.1074/jbc.M109.032847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chaudhury A, Hussey GS, Ray PS, Jin G, Fox PL, Howe PH. TGF-β-mediated phosphorylation of hnRNP E1 induces EMT via transcript-selective translational induction of Dab2 and ILEI. Nat Cell Biol. 2010;12(3):286–93. doi: 10.1038/ncb2029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hocevar BA, Prunier C, Howe PH. Disabled-2 (Dab2) mediates transforming growth factor β (TGFβ)-stimulated fibronectin synthesis through TGFβ-activated kinase 1 and activation of the JNK pathway. J Biol Chem. 2005;280(27):25920–7. doi: 10.1074/jbc.M501150200. [DOI] [PubMed] [Google Scholar]
- 47.Hussey GS, Chaudhury A, Dawson AE, Lindner DJ, Knudsen CR, Wilce MC, et al. Identification of an mRNP complex regulating tumorigenesis at the translational elongation step. Mol Cell. 2011;41(4):419–31. doi: 10.1016/j.molcel.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim W, Seok Kang, Y Soo, Kim J, Shin NY, Hanks SK, Song WK. The integrin-coupled signaling adaptor p130Cas suppresses Smad3 function in transforming growth factor-β signaling. Mol Biol Cell. 2008;19(5):2135–46. doi: 10.1091/mbc.E07-10-0991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wendt MK, Smith JA, Schiemann WP. p130Cas is required for mammary tumor growth and transforming growth factor-β-mediated metastasis through regulation of Smad2/3 activity. J Biol Chem. 2009;284(49):34145–56. doi: 10.1074/jbc.M109.023614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hayashi H, Abdollah S, Qiu Y, Cai J, Xu YY, Grinnell BW, et al. The MAD-related protein Smad7 associates with the TGFβ receptor and functions as an antagonist of TGFβ signaling. Cell. 1997;89:1165–73. doi: 10.1016/s0092-8674(00)80303-7. [DOI] [PubMed] [Google Scholar]
- 51.Nakao A, Afrakht M, Moren A, Nakayama T, Christian JL, Heuchel R, et al. Identification of Smad7, a TGFβ-inducible antagonist of TGF-β signalling. Nature. 1997;389:631–5. doi: 10.1038/39369. [DOI] [PubMed] [Google Scholar]
- 52.Souchelnytskyi S, Nakayama T, Nakao A, Moren A, Heldin CH, Christian JL, et al. Physical and functional interaction of murine and xenopus Smad7 with bone morphogenetic protein receptors and transforming growth factor-β receptors. J Biol Chem. 1998;273:25364–70. doi: 10.1074/jbc.273.39.25364. [DOI] [PubMed] [Google Scholar]
- 53.Ebisawa T, Fukuchi M, Murakami G, Chiba T, Tanaka K, Imamura T, et al. Smurf1 interacts with transforming growth factor-β type I receptor through Smad7 and induces receptor degradation. J Biol Chem. 2001;276(16):12477–80. doi: 10.1074/jbc.C100008200. [DOI] [PubMed] [Google Scholar]
- 54.Kavsak P, Rasmussen RK, Causing CG, Bonni S, Zhu H, Thomsen GH, et al. Smad7 binds to Smurf2 to form an E3 ubiquitin ligase that targets the TGFβ receptor for degradation. Mol Cell. 2000;6(6):1365–75. doi: 10.1016/s1097-2765(00)00134-9. [DOI] [PubMed] [Google Scholar]
- 55.Datta PK, Moses HL. STRAP and Smad7 synergize in the inhibition of transforming growth factor β signaling. Mol Cell Biol. 2000;20(9):3157–67. doi: 10.1128/mcb.20.9.3157-3167.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ibarrola N, Kratchmarova I, Nakajima D, Schiemann WP, Moustakas A, Pandey A, et al. Cloning of a novel signaling molecule, AMSH-2, that potentiates transforming growth factor β signaling. BMC Cell Biol. 2004;5:2. doi: 10.1186/1471-2121-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Koinuma D, Shinozaki M, Komuro A, Goto K, Saitoh M, Hanyu A, et al. Arkadia amplifies TGF-β superfamily signalling through degradation of Smad7. EMBO J. 2003;22(24):6458–70. doi: 10.1093/emboj/cdg632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lin X, Duan X, Liang YY, Su Y, Wrighton KH, Long J, et al. PPM1A functions as a Smad phosphatase to terminate TGFβ signaling. Cell. 2006;125(5):915–28. doi: 10.1016/j.cell.2006.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lin X, Liang M, Feng XH. Smurf2 is a ubiquitin E3 ligase mediating proteasome-dependent degradation of Smad2 in transforming growth factor-β signaling. J Biol Chem. 2000;275(47):36818–22. doi: 10.1074/jbc.C000580200. [DOI] [PubMed] [Google Scholar]
- 60.Lo RS, Massague J. Ubiquitin-dependent degradation of TGF-β-activated Smad2. Nat Cell Biol. 1999;1(8):472–8. doi: 10.1038/70258. [DOI] [PubMed] [Google Scholar]
- 61.Fukuchi M, Imamura T, Chiba T, Ebisawa T, Kawabata M, Tanaka K, et al. Ligand-dependent degradation of Smad3 by a ubiquitin ligase complex of ROC1 and associated proteins. Mol Biol Cell. 2001;12(5):1431–43. doi: 10.1091/mbc.12.5.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Izzi L, Attisano L. Regulation of the TGFβ signalling pathway by ubiquitin-mediated degradation. Oncogene. 2004;23(11):2071–8. doi: 10.1038/sj.onc.1207412. [DOI] [PubMed] [Google Scholar]
- 63.Dupont S, Mamidi A, Cordenonsi M, Montagner M, Zacchigna L, Adorno M, et al. FAM/USP9x, a deubiquitinating enzyme essential for TGFβ signaling, controls Smad4 monoubiquitination. Cell. 2009;136(1):123–35. doi: 10.1016/j.cell.2008.10.051. [DOI] [PubMed] [Google Scholar]
- 64.Derynck R, Akhurst RJ, Balmain A. TGF-β signaling in tumor suppression and cancer progression. Nat Genet. 2001;29(2):117–29. doi: 10.1038/ng1001-117. [DOI] [PubMed] [Google Scholar]
- 65.Massague J. TGFβ in cancer. Cell. 2008;134(2):215–30. doi: 10.1016/j.cell.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Derynck R, Akhurst RJ. Differentiation plasticity regulated by TGF-β family proteins in development and disease. Nat Cell Biol. 2007;9(9):1000–4. doi: 10.1038/ncb434. [DOI] [PubMed] [Google Scholar]
- 67.Piek E, Moustakas A, Kurisaki A, Heldin CH, ten Dijke P. TGF-β type I receptor/ALK-5 and Smad proteins mediate epithelial to mesenchymal transdifferentiation in NMuMG breast epithelial cells. J Cell Sci. 1999;112:4557–68. doi: 10.1242/jcs.112.24.4557. [DOI] [PubMed] [Google Scholar]
- 68.Valcourt U, Kowanetz M, Niimi H, Heldin CH, Moustakas A. TGF-β and the Smad signaling pathway support transcriptomic reprogramming during epithelial-mesenchymal cell transition. Mol Biol Cell. 2005;16(4):1987–2002. doi: 10.1091/mbc.E04-08-0658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wendt MK, Allington TM, Schiemann WP. Mechanisms of the epithelial-mesenchymal transition by TGF-β. Future Oncol. 2009;5(8):1145–68. doi: 10.2217/fon.09.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Oft M, Akhurst RJ, Balmain A. Metastasis is driven by sequential elevation of H-Ras and Smad2 levels. Nat Cell Biol. 2002;4(7):487–94. doi: 10.1038/ncb807. [DOI] [PubMed] [Google Scholar]
- 71.Lehmann K, Janda E, Pierreux CE, Rytomaa M, Schulze A, McMahon M, et al. Raf induces TGFβ production while blocking its apoptotic but not invasive responses: a mechanism leading to increased malignancy in epithelial cells. Genes Dev. 2000;14(20):2610–22. doi: 10.1101/gad.181700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Neil JR, Johnson KM, Nemenoff RA, Schiemann WP. Cox-2 inactivates Smad signaling and enhances EMT stimulated by TGF-β through a PGE2-dependent mechanisms. Carcinogenesis. 2008;29(11):2227–35. doi: 10.1093/carcin/bgn202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Neil JR, Schiemann WP. Altered TAB1:IκB kinase interaction promotes transforming growth factor β-mediated nuclear factor-κB activation during breast cancer progression. Cancer Res. 2008;68(5):1462–70. doi: 10.1158/0008-5472.CAN-07-3094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Neil JR, Tian M, Schiemann WP. x-linked inhibitor of apoptosis protein and its E3 ligase activity promote transforming growth factor-β-mediated nuclear factor-κB activation during breast cancer progression. J Biol Chem. 2009;284(32):21209–17. doi: 10.1074/jbc.M109.018374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tian M, Schiemann WP. PGE2 receptor EP2 mediates the antagonistic effect of COX-2 on TGF-β signaling during mammary tumorigenesis. FASEB J. 2010;24(4):1105–16. doi: 10.1096/fj.09-141341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kretzschmar M, Doody J, Timokhina I, Massague J. A mechanism of repression of TGFβ/Smad signaling by oncogenic Ras. Genes Dev. 1999;13(7):804–16. doi: 10.1101/gad.13.7.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Funaba M, Zimmerman CM, Mathews LS. Modulation of Smad2-mediated signaling by extracellular signal-regulated kinase. J Biol Chem. 2002;277(44):41361–8. doi: 10.1074/jbc.M204597200. [DOI] [PubMed] [Google Scholar]
- 78.Brown JD, DiChiara MR, Anderson KR, Gimbrone MA, Jr., Topper JN. MEKK-1, a component of the stress (stress-activated protein kinase/c-Jun N-terminal kinase) pathway, can selectively activate Smad2-mediated transcriptional activation in endothelial cells. J Biol Chem. 1999;274(13):8797–805. doi: 10.1074/jbc.274.13.8797. [DOI] [PubMed] [Google Scholar]
- 79.Engel ME, McDonnell MA, Law BK, Moses HL. Interdependent SMAD and JNK signaling in transforming growth factor-β-mediated transcription. J Biol Chem. 1999;274(52):37413–20. doi: 10.1074/jbc.274.52.37413. [DOI] [PubMed] [Google Scholar]
- 80.Waddell DS, Liberati NT, Guo X, Frederick JP, Wang XF. Casein kinase Iepsilon plays a functional role in the transforming growth factor-β signaling pathway. J Biol Chem. 2004;279(28):29236–46. doi: 10.1074/jbc.M400880200. [DOI] [PubMed] [Google Scholar]
- 81.Yakymovych I, Ten Dijke P, Heldin CH, Souchelnytskyi S. Regulation of Smad signaling by protein kinase C. FASEB J. 2001;15(3):553–5. doi: 10.1096/fj.00-0474fje. [DOI] [PubMed] [Google Scholar]
- 82.Wicks SJ, Lui S, Abdel-Wahab N, Mason RM, Chantry A. Inactivation of smad-transforming growth factor β signaling by Ca(2+)-calmodulin-dependent protein kinase II. Mol Cell Biol. 2000;20(21):8103–11. doi: 10.1128/mcb.20.21.8103-8111.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Guo X, Ramirez A, Waddell DS, Li Z, Liu X, Wang XF. Axin and GSK3β control Smad3 protein stability and modulate TGF-β signaling. Genes Dev. 2008;22(1):106–20. doi: 10.1101/gad.1590908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Allington TM, Galliher-Beckley AJ, Schiemann WP. Activated Abl kinase inhibits oncogenic transforming growth factor-β signaling and tumorigenesis in mammary tumors. FASEB J. 2009;23(12):4231–43. doi: 10.1096/fj.09-138412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Galliher AJ, Schiemann WP. β3 integrin and Src facilitate transforming growth factor-β mediated induction of epithelial-mesenchymal transition in mammary epithelial cells. Breast Cancer Res. 2006;8(4):R42. doi: 10.1186/bcr1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Galliher AJ, Schiemann WP. Src phosphorylates Tyr284 in TGF-β type II receptor and regulates TGF-β stimulation of p38 MAPK during breast cancer cell proliferation and invasion. Cancer Res. 2007;67(8):3752–8. doi: 10.1158/0008-5472.CAN-06-3851. [DOI] [PubMed] [Google Scholar]
- 87.Galliher-Beckley AJ, Schiemann WP. Grb2 binding to Tyr284 in TβR-II is essential for mammary tumor growth and metastasis stimulated by TGF-β. Carcinogenesis. 2008;29(2):244–51. doi: 10.1093/carcin/bgm245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wendt MK, Schiemann WP. Therapeutic targeting of the focal adhesion complex prevents oncogenic TGF-β signaling and metastasis. Breast Cancer Res. 2009;11(5):R68. doi: 10.1186/bcr2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wendt MK, Smith JA, Schiemann WP. Transforming growth factor-β-induced epithelial-mesenchymal transition facilitates epidermal growth factor-dependent breast cancer progression. Oncogene. 2010;29(49):6485–98. doi: 10.1038/onc.2010.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Taylor MA, Amin J, Kirschmann DA, Schiemann WP. Lysyl oxidase and hydrogen peroxide promote oncogenic signaling by transforming growth factor-β in mammary epithelial cells. Neoplasia. 2011;13 doi: 10.1593/neo.101086. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lee YH, Albig AR, Regner M, Schiemann BJ, Schiemann WP. Fibulin-5 initiates epithelial-mesenchymal transition (EMT) and enhances EMT induced by TGF-β in mammary epithelial cells via a MMP-dependent mechanism. Carcinogenesis. 2008;29(12):2243–51. doi: 10.1093/carcin/bgn199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Moustakas A, Heldin CH. Non-Smad TGF-β signals. J Cell Sci. 2005;118(Pt 16):3573–84. doi: 10.1242/jcs.02554. [DOI] [PubMed] [Google Scholar]
- 93.Kang JS, Liu C, Derynck R. New regulatory mechanisms of TGF-β receptor function. Trends Cell Biol. 2009;19(8):385–94. doi: 10.1016/j.tcb.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 94.Desgrosellier JS, Cheresh DA. Integrins in cancer: biological implications and therapeutic opportunities. Nat Rev Cancer. 2010;10(1):9–22. doi: 10.1038/nrc2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Egeblad M, Nakasone ES, Werb Z. Tumors as organs: complex tissues that interface with the entire organism. Dev Cell. 2010;18(6):884–901. doi: 10.1016/j.devcel.2010.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zutter MM. Integrin-mediated adhesion: tipping the balance between chemosensitivity and chemoresistance. Adv Exp Med Biol. 2007;608:87–100. doi: 10.1007/978-0-387-74039-3_6. [DOI] [PubMed] [Google Scholar]
- 97.Munger JS, Huang X, Kawakatsu H, Griffiths MJ, Dalton SL, Wu J, et al. The integrin αvβ6 binds and activates latent TGFβ1: a mechanism for regulating pulmonary inflammation and fibrosis. Cell. 1999;96(3):319–28. doi: 10.1016/s0092-8674(00)80545-0. [DOI] [PubMed] [Google Scholar]
- 98.Mu D, Cambier S, Fjellbirkeland L, Baron JL, Munger JS, Kawakatsu H, et al. The integrin αvβ8 mediates epithelial homeostasis through MT1-MMP-dependent activation of TGF-β1. J Cell Biol. 2002;157(3):493–507. doi: 10.1083/jcb.200109100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sloan EK, Pouliot N, Stanley KL, Chia J, Moseley JM, Hards DK, et al. Tumor-specific expression of αvβ3 integrin promotes spontaneous metastasis of breast cancer to bone. Breast Cancer Res. 2006;8(2):R20. doi: 10.1186/bcr1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bandyopadhyay A, Agyin JK, Wang L, Tang Y, Lei X, Story BM, et al. Inhibition of pulmonary and skeletal metastasis by a transforming growth factor-β type I receptor kinase inhibitor. Cancer Res. 2006;66(13):6714–21. doi: 10.1158/0008-5472.CAN-05-3565. [DOI] [PubMed] [Google Scholar]
- 101.Garamszegi N, Garamszegi SP, Samavarchi-Tehrani P, Walford E, Schneiderbauer MM, Wrana JL, et al. Extracellular matrix-induced transforming growth factor-β receptor signaling dynamics. Oncogene. 2010;29(16):2368–80. doi: 10.1038/onc.2009.514. [DOI] [PubMed] [Google Scholar]
- 102.van der Flier S, Chan CM, Brinkman A, Smid M, Johnston SR, Dorssers LC, et al. BCAR1/p130Cas expression in untreated and acquired tamoxifen-resistant human breast carcinomas. Int J Cancer. 2000;89(5):465–8. doi: 10.1002/1097-0215(20000920)89:5<465::aid-ijc11>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 103.Ta HQ, Thomas KS, Schrecengost RS, Bouton AH. A novel association between p130Cas and resistance to the chemotherapeutic drug adriamycin in human breast cancer cells. Cancer Res. 2008 Nov 1;68(21):8796–804. doi: 10.1158/0008-5472.CAN-08-2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cabodi S, Tinnirello A, Bisaro B, Tornillo G, del Pilar Camacho-Leal M, Forni G, et al. p130Cas is an essential transducer element in ErbB2 transformation. FASEB J. 2010;24(10):3796–808. doi: 10.1096/fj.10-157347. [DOI] [PubMed] [Google Scholar]
- 105.Cabodi S, Tinnirello A, Di Stefano P, Bisaro B, Ambrosino E, Castellano I, et al. p130Cas as a new regulator of mammary epithelial cell proliferation, survival, and HER2-neu oncogene-dependent breast tumorigenesis. Cancer Res. 2006;66(9):4672–80. doi: 10.1158/0008-5472.CAN-05-2909. [DOI] [PubMed] [Google Scholar]
- 106.Bhowmick NA, Zent R, Ghiassi M, McDonnell M, Moses HL. Integrin β1 signaling is necessary for transforming growth factor-β activation of p38MAPK and epithelial plasticity. J Biol Chem. 2001;276(50):46707–13. doi: 10.1074/jbc.M106176200. [DOI] [PubMed] [Google Scholar]
- 107.Mizejewski GJ. Role of integrins in cancer: survey of expression patterns. Proc Soc Exp Biol Med. 1999;222(2):124–38. doi: 10.1177/153537029922200203. [DOI] [PubMed] [Google Scholar]
- 108.Weaver VM, Lelievre S, Lakins JN, Chrenek MA, Jones JC, Giancotti F, et al. β4 integrin-dependent formation of polarized three-dimensional architecture confers resistance to apoptosis in normal and malignant mammary epithelium. Cancer Cell. 2002;2(3):205–16. doi: 10.1016/s1535-6108(02)00125-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Engelman JA. Targeting PI3K signalling in cancer: opportunities, challenges and limitations. Nat Rev Cancer. 2009;9(8):550–62. doi: 10.1038/nrc2664. [DOI] [PubMed] [Google Scholar]
- 110.Bakin AV, Tomlinson AK, Bhowmick NA, Moses HL, Arteaga CL. Phosphatidylinositol 3-kinase function is required for transforming growth factor β-mediated epithelial to mesenchymal transition and cell migration. J Biol Chem. 2000;275(47):36803–10. doi: 10.1074/jbc.M005912200. [DOI] [PubMed] [Google Scholar]
- 111.Murillo MM, del Castillo G, Sanchez A, Fernandez M, Fabregat I. Involvement of EGF receptor and c-Src in the survival signals induced by TGF-β1 in hepatocytes. Oncogene. 2005;24(28):4580–7. doi: 10.1038/sj.onc.1208664. [DOI] [PubMed] [Google Scholar]
- 112.Jechlinger M, Sommer A, Moriggl R, Seither P, Kraut N, Capodiecci P, et al. Autocrine PDGFR signaling promotes mammary cancer metastasis. J Clin Invest. 2006;116(6):1561–70. doi: 10.1172/JCI24652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Uttamsingh S, Bao X, Nguyen KT, Bhanot M, Gong J, Chan JL, et al. Synergistic effect between EGF and TGF-β1 in inducing oncogenic properties of intestinal epithelial cells. Oncogene. 2008;27(18):2626–34. doi: 10.1038/sj.onc.1210915. [DOI] [PubMed] [Google Scholar]
- 114.Lamouille S, Derynck R. Cell size and invasion in TGF-β-induced epithelial to mesenchymal transition is regulated by activation of the mTOR pathway. J Cell Biol. 2007;178(3):437–51. doi: 10.1083/jcb.200611146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Conery AR, Cao Y, Thompson EA, Townsend CM, Jr., Ko TC, Luo K. Akt interacts directly with Smad3 to regulate the sensitivity to TGF-β induced apoptosis. Nat Cell Biol. 2004;6(4):366–72. doi: 10.1038/ncb1117. [DOI] [PubMed] [Google Scholar]
- 116.Remy I, Montmarquette A, Michnick SW. PKB/Akt modulates TGF-β signalling through a direct interaction with Smad3. Nat Cell Biol. 2004;6(4):358–65. doi: 10.1038/ncb1113. [DOI] [PubMed] [Google Scholar]
- 117.Xu J, Lamouille S, Derynck R. TGF-β-induced epithelial to mesenchymal transition. Cell Res. 2009;19(2):156–72. doi: 10.1038/cr.2009.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Heldin CH, Landstrom M, Moustakas A. Mechanism of TGF-β signaling to growth arrest, apoptosis, and epithelial-mesenchymal transition. Curr Opin Cell Biol. 2009;21(2):166–76. doi: 10.1016/j.ceb.2009.01.021. [DOI] [PubMed] [Google Scholar]
- 119.Hall A. Rho GTPases and the control of cell behaviour. Biochem Soc Trans. 2005;33(Pt 5):891–5. doi: 10.1042/BST20050891. [DOI] [PubMed] [Google Scholar]
- 120.Hall A. The cytoskeleton and cancer. Cancer Metastasis Rev. 2009;28(1-2):5–14. doi: 10.1007/s10555-008-9166-3. [DOI] [PubMed] [Google Scholar]
- 121.Bhowmick NA, Ghiassi M, Bakin A, Aakre M, Lundquist CA, Engel ME, et al. Transforming growth factor-β1 mediates epithelial to mesenchymal transdifferentiation through a RhoA-dependent mechanism. Mol Biol Cell. 2001;12(1):27–36. doi: 10.1091/mbc.12.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Viloria-Petit AM, David L, Jia JY, Erdemir T, Bane AL, Pinnaduwage D, et al. A role for the TGFβ-Par6 polarity pathway in breast cancer progression. Proc Natl Acad Sci USA. 2009;106(33):14028–33. doi: 10.1073/pnas.0906796106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ozdamar B, Bose R, Barrios-Rodiles M, Wang HR, Zhang Y, Wrana JL. Regulation of the polarity protein Par6 by TGFβ receptors controls epithelial cell plasticity. Science. 2005;307(5715):1603–9. doi: 10.1126/science.1105718. [DOI] [PubMed] [Google Scholar]
- 124.Hutchison N, Hendry BM, Sharpe CC. Rho isoforms have distinct and specific functions in the process of epithelial to mesenchymal transition in renal proximal tubular cells. Cell Signal. 2009;21(10):1522–31. doi: 10.1016/j.cellsig.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 125.He Y, Northey JJ, Primeau M, Machado RD, Trembath R, Siegel PM, et al. CdGAP is required for transforming growth factor β- and Neu/ErbB-2-induced breast cancer cell motility and invasion. Oncogene. 2010;30(9):1032–45. doi: 10.1038/onc.2010.477. [DOI] [PubMed] [Google Scholar]
- 126.Mythreye K, Blobe GC. The type III TGF-β receptor regulates epithelial and cancer cell migration through β-arrestin2-mediated activation of Cdc42. Proc Natl Acad Sci USA. 2009;106(20):8221–6. doi: 10.1073/pnas.0812879106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kong W, Yang H, He L, Zhao JJ, Coppola D, Dalton WS, et al. MicroRNA-155 is regulated by the transforming growth factor β/Smad pathway and contributes to epithelial cell plasticity by targeting RhoA. Mol Cell Biol. 2008;28(22):6773–84. doi: 10.1128/MCB.00941-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Valastyan S, Benaich N, Chang A, Reinhardt F, Weinberg RA. Concomitant suppression of three target genes can explain the impact of a microRNA on metastasis. Genes Dev. 2009;23(22):2592–7. doi: 10.1101/gad.1832709. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 129.Valastyan S, Reinhardt F, Benaich N, Calogrias D, Szasz AM, Wang ZC, et al. A pleiotropically acting microRNA, miR-31, inhibits breast cancer metastasis. Cell. 2009;137(6):1032–46. doi: 10.1016/j.cell.2009.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 130.Atfi A, Djelloul S, Chastre E, Davis R, Gespach C. Evidence for a role of Rho-like GTPases and stress-activated protein kinase/c-Jun N-terminal kinase (SAPK/JNK) in transforming growth factor β-mediated signaling. J Biol Chem. 1997;272(3):1429–32. doi: 10.1074/jbc.272.3.1429. [DOI] [PubMed] [Google Scholar]
- 131.Bakin AV, Rinehart C, Tomlinson AK, Arteaga CL. p38 mitogen-activated protein kinase is required for TGFβ-mediated fibroblastic transdifferentiation and cell migration. J Cell Sci. 2002;115(Pt 15):3193–206. doi: 10.1242/jcs.115.15.3193. [DOI] [PubMed] [Google Scholar]
- 132.Xie L, Law BK, Chytil AM, Brown KA, Aakre ME, Moses HL. Activation of the Erk pathway is required for TGF-β1-induced EMT in vitro. Neoplasia. 2004;6(5):603–10. doi: 10.1593/neo.04241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Shintani Y, Hollingsworth MA, Wheelock MJ, Johnson KR. Collagen I promotes metastasis in pancreatic cancer by activating c-Jun NH(2)-terminal kinase 1 and up-regulating N-cadherin expression. Cancer Res. 2006;66(24):11745–53. doi: 10.1158/0008-5472.CAN-06-2322. [DOI] [PubMed] [Google Scholar]
- 134.Shintani Y, Wheelock MJ, Johnson KR. Phosphoinositide-3 kinase-Rac1-c-Jun NH2-terminal kinase signaling mediates collagen I-induced cell scattering and up-regulation of N-cadherin expression in mouse mammary epithelial cells. Mol Biol Cell. 2006;17(7):2963–75. doi: 10.1091/mbc.E05-12-1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sorrentino A, Thakur N, Grimsby S, Marcusson A, von Bulow V, Schuster N, et al. The type I TGF-β receptor engages TRAF6 to activate TAK1 in a receptor kinase-independent manner. Nat Cell Biol. 2008;10(10):1199–207. doi: 10.1038/ncb1780. [DOI] [PubMed] [Google Scholar]
- 136.Yamashita M, Fatyol K, Jin C, Wang X, Liu Z, Zhang YE. TRAF6 mediates Smad-independent activation of JNK and p38 by TGF-β. Mol Cell. 2008;31(6):918–24. doi: 10.1016/j.molcel.2008.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Karin M. Nuclear factor-κB in cancer development and progression. Nature. 2006;441(7092):431–6. doi: 10.1038/nature04870. [DOI] [PubMed] [Google Scholar]
- 138.Sovak MA, Arsura M, Zanieski G, Kavanagh KT, Sonenshein GE. The inhibitory effects of transforming growth factor β1 on breast cancer cell proliferation are mediated through regulation of aberrant nuclear factor-κB/Rel expression. Cell Growth Differ. 1999;10(8):537–44. [PubMed] [Google Scholar]
- 139.Arsura M, Wu M, Sonenshein GE. TGF β1 inhibits NF-κB/Rel activity inducing apoptosis of B cells: transcriptional activation of IκBα. Immunity. 1996;5(1):31–40. doi: 10.1016/s1074-7613(00)80307-6. [DOI] [PubMed] [Google Scholar]
- 140.You HJ, How T, Blobe GC. The type III transforming growth factor-β receptor negatively regulates nuclear factor κB signaling through its interaction with β-arrestin2. Carcinogenesis. 2009;30(8):1281–7. doi: 10.1093/carcin/bgp071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Chua HL, Bhat-Nakshatri P, Clare SE, Morimiya A, Badve S, Nakshatri H. NF-κB represses E-cadherin expression and enhances epithelial to mesenchymal transition of mammary epithelial cells: potential involvement of ZEB-1 and ZEB-2. Oncogene. 2007;26(5):711–24. doi: 10.1038/sj.onc.1209808. [DOI] [PubMed] [Google Scholar]
- 142.Huber MA, Azoitei N, Baumann B, Grunert S, Sommer A, Pehamberger H, et al. NF-κB is essential for epithelial-mesenchymal transition and metastasis in a model of breast cancer progression. J Clin Invest. 2004;114(4):569–81. doi: 10.1172/JCI21358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kagan HM, Li W. Lysyl oxidase: properties, specificity, and biological roles inside and outside of the cell. J Cell Biochem. 2003;88(4):660–72. doi: 10.1002/jcb.10413. [DOI] [PubMed] [Google Scholar]
- 144.Payne SL, Hendrix MJ, Kirschmann DA. Paradoxical roles for lysyl oxidases in cancer--a prospect. J Cell Biochem. 2007;101(6):1338–54. doi: 10.1002/jcb.21371. [DOI] [PubMed] [Google Scholar]
- 145.Paszek MJ, Zahir N, Johnson KR, Lakins JN, Rozenberg GI, Gefen A, et al. Tensional homeostasis and the malignant phenotype. Cancer Cell. 2005;8(3):241–54. doi: 10.1016/j.ccr.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 146.Levental KR, Yu H, Kass L, Lakins JN, Egeblad M, Erler JT, et al. Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell. 2009;139(5):891–906. doi: 10.1016/j.cell.2009.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Erler JT, Bennewith KL, Cox TR, Lang G, Bird D, Koong A, et al. Hypoxia-induced lysyl oxidase is a critical mediator of bone marrow cell recruitment to form the premetastatic niche. Cancer Cell. 2009;15(1):35–44. doi: 10.1016/j.ccr.2008.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Erler JT, Bennewith KL, Nicolau M, Dornhofer N, Kong C, Le QT, et al. Lysyl oxidase is essential for hypoxia-induced metastasis. Nature. 2006;440(7088):1222–6. doi: 10.1038/nature04695. [DOI] [PubMed] [Google Scholar]
- 149.Payne SL, Hendrix MJ, Kirschmann DA. Lysyl oxidase regulates actin filament formation through the p130(Cas)/Crk/DOCK180 signaling complex. J Cell Biochem. 2006;98(4):827–37. doi: 10.1002/jcb.20792. [DOI] [PubMed] [Google Scholar]
- 150.Yang L, Huang J, Ren X, Gorska AE, Chytil A, Aakre M, et al. Abrogation of TGF beta signaling in mammary carcinomas recruits Gr-1+CD11b+ myeloid cells that promote metastasis. Cancer Cell. 2008;13(1):23–35. doi: 10.1016/j.ccr.2007.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Moustakas A, Heldin CH. Signaling networks guiding epithelial-mesenchymal transitions during embryogenesis and cancer progression. Cancer Sci. 2007;98(10):1512–20. doi: 10.1111/j.1349-7006.2007.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Tomaskovic-Crook E, Thompson EW, Thiery JP. Epithelial to mesenchymal transition and breast cancer. Breast Cancer Res. 2009;11(6):213. doi: 10.1186/bcr2416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Kalluri R, Weinberg RA. The basics of epithelial-mesenchymal transition. J Clin Invest. 2009;119(6):1420–8. doi: 10.1172/JCI39104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Padua D, Zhang XH, Wang Q, Nadal C, Gerald WL, Gomis RR, et al. TGFβ primes breast tumors for lung metastasis seeding through angiopoietin-like 4. Cell. 2008;133(1):66–77. doi: 10.1016/j.cell.2008.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Furuse M. Molecular basis of the core structure of tight junctions. Cold Spring Harb Perspect Biol. 2010;2(1):a002907. doi: 10.1101/cshperspect.a002907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Martin TA, Jiang WG. Loss of tight junction barrier function and its role in cancer metastasis. Biochim Biophys Acta. 2009;1788(4):872–91. doi: 10.1016/j.bbamem.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 157.Ebnet K, Suzuki A, Ohno S, Vestweber D. Junctional adhesion molecules (JAMs): more molecules with dual functions? J Cell Sci. 2004;117(Pt 1):19–29. doi: 10.1242/jcs.00930. [DOI] [PubMed] [Google Scholar]
- 158.Schneeberger EE, Lynch RD. The tight junction: a multifunctional complex. Am J Physiol Cell Physiol. 2004;286(6):C1213–28. doi: 10.1152/ajpcell.00558.2003. [DOI] [PubMed] [Google Scholar]
- 159.Itoh M, Bissell MJ. The organization of tight junctions in epithelia: implications for mammary gland biology and breast tumorigenesis. J Mammary Gland Biol Neoplasia. 2003;8(4):449–62. doi: 10.1023/B:JOMG.0000017431.45314.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Lacher MD, Tiirikainen MI, Saunier EF, Christian C, Anders M, Oft M, et al. Transforming growth factor-β receptor inhibition enhances adenoviral infectability of carcinoma cells via up-regulation of Coxsackie and Adenovirus Receptor in conjunction with reversal of epithelial-mesenchymal transition. Cancer Res. 2006;66(3):1648–57. doi: 10.1158/0008-5472.CAN-05-2328. [DOI] [PubMed] [Google Scholar]
- 161.Vincent T, Neve EP, Johnson JR, Kukalev A, Rojo F, Albanell J, et al. A SNAIL1-SMAD3/4 transcriptional repressor complex promotes TGF-β mediated epithelial-mesenchymal transition. Nat Cell Biol. 2009;11(8):943–50. doi: 10.1038/ncb1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Grande M, Franzen A, Karlsson JO, Ericson LE, Heldin NE, Nilsson M. Transforming growth factor-β and epidermal growth factor synergistically stimulate epithelial to mesenchymal transition (EMT) through a MEK-dependent mechanism in primary cultured pig thyrocytes. J Cell Sci. 2002;115(Pt 22):4227–36. doi: 10.1242/jcs.00091. [DOI] [PubMed] [Google Scholar]
- 163.Shiou SR, Singh AB, Moorthy K, Datta PK, Washington MK, Beauchamp RD, et al. Smad4 regulates claudin-1 expression in a transforming growth factor-β-independent manner in colon cancer cells. Cancer Res. 2007;67(4):1571–9. doi: 10.1158/0008-5472.CAN-06-1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Barrios-Rodiles M, Brown KR, Ozdamar B, Bose R, Liu Z, Donovan RS, et al. High-throughput mapping of a dynamic signaling network in mammalian cells. Science. 2005;307(5715):1621–5. doi: 10.1126/science.1105776. [DOI] [PubMed] [Google Scholar]
- 165.Murphy SJ, Dore JJ, Edens M, Coffey RJ, Barnard JA, Mitchell H, et al. Differential trafficking of transforming growth factor-β receptors and ligand in polarized epithelial cells. Mol Biol Cell. 2004;15(6):2853–62. doi: 10.1091/mbc.E04-02-0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Yakovich AJ, Huang Q, Du J, Jiang B, Barnard JA. Vectorial TGFβ signaling in polarized intestinal epithelial cells. J Cell Physiol. 2010;224(2):398–404. doi: 10.1002/jcp.22135. [DOI] [PubMed] [Google Scholar]
- 167.Cavallaro U, Christofori G. Cell adhesion and signalling by cadherins and Ig-CAMs in cancer. Nat Rev Cancer. 2004;4(2):118–32. doi: 10.1038/nrc1276. [DOI] [PubMed] [Google Scholar]
- 168.Agiostratidou G, Hulit J, Phillips GR, Hazan RB. Differential cadherin expression: potential markers for epithelial to mesenchymal transformation during tumor progression. J Mammary Gland Biol Neoplasia. 2007;12(2-3):127–33. doi: 10.1007/s10911-007-9044-6. [DOI] [PubMed] [Google Scholar]
- 169.Gravdal K, Halvorsen OJ, Haukaas SA, Akslen LA. A switch from E-cadherin to N-cadherin expression indicates epithelial to mesenchymal transition and is of strong and independent importance for the progress of prostate cancer. Clin Cancer Res. 2007;13(23):7003–11. doi: 10.1158/1078-0432.CCR-07-1263. [DOI] [PubMed] [Google Scholar]
- 170.Tomita K, van Bokhoven A, van Leenders GJ, Ruijter ET, Jansen CF, Bussemakers MJ, et al. Cadherin switching in human prostate cancer progression. Cancer Res. 2000;60(13):3650–4. [PubMed] [Google Scholar]
- 171.Hazan RB, Phillips GR, Qiao RF, Norton L, Aaronson SA. Exogenous expression of N-cadherin in breast cancer cells induces cell migration, invasion, and metastasis. J Cell Biol. 2000;148(4):779–90. doi: 10.1083/jcb.148.4.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Micalizzi DS, Farabaugh SM, Ford HL. Epithelial-mesenchymal transition in cancer: parallels between normal development and tumor progression. J Mammary Gland Biol Neoplasia. 2010;15(2):117–34. doi: 10.1007/s10911-010-9178-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Christofori G. Changing neighbours, changing behaviour: cell adhesion molecule-mediated signalling during tumour progression. EMBO J. 2003;22(10):2318–23. doi: 10.1093/emboj/cdg228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Kim KK, Wei Y, Szekeres C, Kugler MC, Wolters PJ, Hill ML, et al. Epithelial cell α3β1 integrin links β-catenin and Smad signaling to promote myofibroblast formation and pulmonary fibrosis. J Clin Invest. 2009;119(1):213–24. doi: 10.1172/JCI36940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Kim Y, Kugler MC, Wei Y, Kim KK, Li X, Brumwell AN, et al. Integrin α3β1-dependent β-catenin phosphorylation links epithelial Smad signaling to cell contacts. J Cell Biol. 2009;184(2):309–22. doi: 10.1083/jcb.200806067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Tian YC, Phillips AO. Interaction between the transforming growth factor-β type II receptor/Smad pathway and β-catenin during transforming growth factor-β1-mediated adherens junction disassembly. Am J Pathol. 2002;160(5):1619–28. doi: 10.1016/s0002-9440(10)61109-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Vogelmann R, Nguyen-Tat MD, Giehl K, Adler G, Wedlich D, Menke A. TGFβ-induced downregulation of E-cadherin-based cell-cell adhesion depends on PI3-kinase and PTEN. J Cell Sci. 2005;118(Pt 20):4901–12. doi: 10.1242/jcs.02594. [DOI] [PubMed] [Google Scholar]
- 178.Bhowmick NA, Chytil A, Plieth D, Gorska AE, Dumont N, Shappell S, et al. TGF-β signaling in fibroblasts modulates the oncogenic potential of adjacent epithelia. Science. 2004;303(5659):848–51. doi: 10.1126/science.1090922. [DOI] [PubMed] [Google Scholar]
- 179.Kim BG, Li C, Qiao W, Mamura M, Kasprzak B, Anver M, et al. Smad4 signalling in T cells is required for suppression of gastrointestinal cancer. Nature. 2006;441(7096):1015–9. doi: 10.1038/nature04846. [DOI] [PubMed] [Google Scholar]
- 180.Cheng N, Bhowmick NA, Chytil A, Gorksa AE, Brown KA, Muraoka R, et al. Loss of TGF-β type II receptor in fibroblasts promotes mammary carcinoma growth and invasion through upregulation of TGF-α-, MSP- and HGF-mediated signaling networks. Oncogene. 2005;24(32):5053–68. doi: 10.1038/sj.onc.1208685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Bhowmick NA, Neilson EG, Moses HL. Stromal fibroblasts in cancer initiation and progression. Nature. 2004;432(7015):332–7. doi: 10.1038/nature03096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Ignotz RA, Massague J. Transforming growth factor-β stimulates the expression of fibronectin and collagen and their incorporation into the extracellular matrix. J Biol Chem. 1986;261(9):4337–45. [PubMed] [Google Scholar]
- 183.Barkan D, Kleinman H, Simmons JL, Asmussen H, Kamaraju AK, Hoenorhoff MJ, et al. Inhibition of metastatic outgrowth from single dormant tumor cells by targeting the cytoskeleton. Cancer Res. 2008;68(15):6241–50. doi: 10.1158/0008-5472.CAN-07-6849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Maschler S, Wirl G, Spring H, Bredow DV, Sordat I, Beug H, et al. Tumor cell invasiveness correlates with changes in integrin expression and localization. Oncogene. 2005;24(12):2032–41. doi: 10.1038/sj.onc.1208423. [DOI] [PubMed] [Google Scholar]
- 185.Wels J, Kaplan RN, Rafii S, Lyden D. Migratory neighbors and distant invaders: tumor-associated niche cells. Genes Dev. 2008;22(5):559–74. doi: 10.1101/gad.1636908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Chandler EM, Saunders MP, Yoon CJ, Gourdon D, Fischbach C. Adipose progenitor cells increase fibronectin matrix strain and unfolding in breast tumors. Phys Biol. 2011;8(1):015008. doi: 10.1088/1478-3975/8/1/015008. [DOI] [PubMed] [Google Scholar]
- 187.Barkan D, El Touny LH, Michalowski AM, Smith JA, Chu I, Davis AS, et al. Metastatic growth from dormant cells induced by a col-I-enriched fibrotic environment. Cancer Res. 2010;70(14):5706–16. doi: 10.1158/0008-5472.CAN-09-2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Bianchini G, Qi Y, Alvarez RH, Iwamoto T, Coutant C, Ibrahim NK, et al. Molecular anatomy of breast cancer stroma and its prognostic value in estrogen receptor-positive and - negative cancers. J Clin Oncol. 2010;28(28):4316–23. doi: 10.1200/JCO.2009.27.2419. [DOI] [PubMed] [Google Scholar]
- 189.Wienke D, Davies GC, Johnson DA, Sturge J, Lambros MB, Savage K, et al. The collagen receptor Endo180 (CD280) Is expressed on basal-like breast tumor cells and promotes tumor growth in vivo. Cancer Res. 2007;67(21):10230–40. doi: 10.1158/0008-5472.CAN-06-3496. [DOI] [PubMed] [Google Scholar]
- 190.Bartel DP. MicroRNAs: target recognition and regulatory functions. Cell. 2009 Jan 23;136(2):215–33. doi: 10.1016/j.cell.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Calin GA, Sevignani C, Dumitru CD, Hyslop T, Noch E, Yendamuri S, et al. Human microRNA genes are frequently located at fragile sites and genomic regions involved in cancers. Proc Natl Acad Sci USA. 2004;101(9):2999–3004. doi: 10.1073/pnas.0307323101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Smeets A, Daemen A, Vanden Bempt I, Gevaert O, Claes B, Wildiers H, et al. Prediction of lymph node involvement in breast cancer from primary tumor tissue using gene expression profiling and miRNAs. Breast Cancer Res Treat. 2010 doi: 10.1007/s10549-010-1265-5. PMID: 21116709. [DOI] [PubMed] [Google Scholar]
- 193.Iorio MV, Ferracin M, Liu CG, Veronese A, Spizzo R, Sabbioni S, et al. MicroRNA gene expression deregulation in human breast cancer. Cancer Res. 2005;65(16):7065–70. doi: 10.1158/0008-5472.CAN-05-1783. [DOI] [PubMed] [Google Scholar]
- 194.Volinia S, Calin GA, Liu CG, Ambs S, Cimmino A, Petrocca F, et al. A microRNA expression signature of human solid tumors defines cancer gene targets. Proc Natl Acad Sci USA. 2006;103(7):2257–61. doi: 10.1073/pnas.0510565103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Huang Q, Gumireddy K, Schrier M, le Sage C, Nagel R, Nair S, et al. The microRNAs miR-373 and miR-520c promote tumour invasion and metastasis. Nat Cell Biol. 2008;10(2):202–10. doi: 10.1038/ncb1681. [DOI] [PubMed] [Google Scholar]
- 196.Ma L, Teruya-Feldstein J, Weinberg RA. Tumour invasion and metastasis initiated by microRNA-10b in breast cancer. Nature. 2007;449(7163):682–8. doi: 10.1038/nature06174. [DOI] [PubMed] [Google Scholar]
- 197.Zhu S, Wu H, Wu F, Nie D, Sheng S, Mo YY. MicroRNA-21 targets tumor suppressor genes in invasion and metastasis. Cell Res. 2008;18(3):350–9. doi: 10.1038/cr.2008.24. [DOI] [PubMed] [Google Scholar]
- 198.Tavazoie SF, Alarcon C, Oskarsson T, Padua D, Wang Q, Bos PD, et al. Endogenous human microRNAs that suppress breast cancer metastasis. Nature. 2008;451(7175):147–52. doi: 10.1038/nature06487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Gregory PA, Bert AG, Paterson EL, Barry SC, Tsykin A, Farshid G, et al. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat Cell Biol. 2008;10(5):593–601. doi: 10.1038/ncb1722. [DOI] [PubMed] [Google Scholar]
- 200.Zavadil J, Narasimhan M, Blumenberg M, Schneider RJ. Transforming growth factor-β and microRNA:mRNA regulatory networks in epithelial plasticity. Cells Tissues Organs. 2007;185(1-3):157–61. doi: 10.1159/000101316. [DOI] [PubMed] [Google Scholar]
- 201.Zhu S, Si ML, Wu H, Mo YY. MicroRNA-21 targets the tumor suppressor gene tropomyosin 1 (TPM1) J Biol Chem. 2007;282(19):14328–36. doi: 10.1074/jbc.M611393200. [DOI] [PubMed] [Google Scholar]
- 202.Qian B, Katsaros D, Lu L, Preti M, Durando A, Arisio R, et al. High miR-21 expression in breast cancer associated with poor disease-free survival in early stage disease and high TGF-β1. Breast Cancer Res Treat. 2009;117(1):131–40. doi: 10.1007/s10549-008-0219-7. [DOI] [PubMed] [Google Scholar]
- 203.Davis BN, Hilyard AC, Lagna G, Hata A. SMAD proteins control DROSHA-mediated microRNA maturation. Nature. 2008;454(7200):56–61. doi: 10.1038/nature07086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Singh A, Settleman J. EMT, cancer stem cells and drug resistance: an emerging axis of evil in the war on cancer. Oncogene. 2010;29(34):4741–51. doi: 10.1038/onc.2010.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Pardal R, Clarke MF, Morrison SJ. Applying the principles of stem-cell biology to cancer. Nat Rev Cancer. 2003;3(12):895–902. doi: 10.1038/nrc1232. [DOI] [PubMed] [Google Scholar]
- 206.Gupta PB, Chaffer CL, Weinberg RA. Cancer stem cells: mirage or reality? Nat Med. 2009;15(9):1010–2. doi: 10.1038/nm0909-1010. [DOI] [PubMed] [Google Scholar]
- 207.Zhou BB, Zhang H, Damelin M, Geles KG, Grindley JC, Dirks PB. Tumour-initiating cells: challenges and opportunities for anticancer drug discovery. Nat Rev Drug Discov. 2009;8(10):806–23. doi: 10.1038/nrd2137. [DOI] [PubMed] [Google Scholar]
- 208.Polyak K, Weinberg RA. Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nat Rev Cancer. 2009;9(4):265–73. doi: 10.1038/nrc2620. [DOI] [PubMed] [Google Scholar]
- 209.Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF. Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci USA. 2003;100(7):3983–8. doi: 10.1073/pnas.0530291100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Bonnet D, Dick JE. Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat Med. 1997;3(7):730–7. doi: 10.1038/nm0797-730. [DOI] [PubMed] [Google Scholar]
- 211.Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126(4):663–76. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 212.Yu J, Vodyanik MA, Smuga-Otto K, Antosiewicz-Bourget J, Frane JL, Tian S, et al. Induced pluripotent stem cell lines derived from human somatic cells. Science. 2007;318(5858):1917–20. doi: 10.1126/science.1151526. [DOI] [PubMed] [Google Scholar]
- 213.Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139(5):871–90. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 214.Pera MF, Tam PP. Extrinsic regulation of pluripotent stem cells. Nature. 2010;465(7299):713–20. doi: 10.1038/nature09228. [DOI] [PubMed] [Google Scholar]
- 215.Stadtfeld M, Hochedlinger K. Induced pluripotency: history, mechanisms, and applications. Genes & development. 2010;24(20):2239–63. doi: 10.1101/gad.1963910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Greber B, Lehrach H, Adjaye J. Fibroblast growth factor 2 modulates transforming growth factor β signaling in mouse embryonic fibroblasts and human ESCs (hESCs) to support hESC self-renewal. Stem Cells. 2007 Feb;25(2):455–64. doi: 10.1634/stemcells.2006-0476. [DOI] [PubMed] [Google Scholar]
- 217.James D, Levine AJ, Besser D, Hemmati-Brivanlou A. TGFβ/activin/nodal signaling is necessary for the maintenance of pluripotency in human embryonic stem cells. Development. 2005;132(6):1273–82. doi: 10.1242/dev.01706. [DOI] [PubMed] [Google Scholar]
- 218.Wellner U, Schubert J, Burk UC, Schmalhofer O, Zhu F, Sonntag A, et al. The EMT-activator ZEB1 promotes tumorigenicity by repressing stemness-inhibiting microRNAs. Nat Cell Biol. 2009;11(12):1487–95. doi: 10.1038/ncb1998. [DOI] [PubMed] [Google Scholar]
- 219.Li HX, Han M, Bernier M, Zheng B, Sun SG, Su M, et al. Kruppel-like factor 4 promotes differentiation by transforming growth factor-β receptor-mediated Smad and p38 MAPK signaling in vascular smooth muscle cells. J Biol Chem. 2010;285(23):17846–56. doi: 10.1074/jbc.M109.076992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Wielenga VJ, Smits R, Korinek V, Smit L, Kielman M, Fodde R, et al. Expression of CD44 in Apc and Tcf mutant mice implies regulation by the WNT pathway. Am J Pathol. 1999;154(2):515–23. doi: 10.1016/S0002-9440(10)65297-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Bennett CN, Green JE. Unlocking the power of cross-species genomic analyses: identification of evolutionarily conserved breast cancer networks and validation of preclinical models. Breast Cancer Res. 2008;10(5):213. doi: 10.1186/bcr2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Aslakson CJ, Miller FR. Selective events in the metastatic process defined by analysis of the sequential dissemination of subpopulations of a mouse mammary tumor. Cancer Res. 1992;52(6):1399–405. [PubMed] [Google Scholar]
- 223.Santner SJ, Dawson PJ, Tait L, Soule HD, Eliason J, Mohamed AN, et al. Malignant MCF10CA1 cell lines derived from premalignant human breast epithelial MCF10AT cells. Breast Cancer Res Treat. 2001;65(2):101–10. doi: 10.1023/a:1006461422273. [DOI] [PubMed] [Google Scholar]
- 224.Rak JW, McEachern D, Miller FR. Sequential alteration of peanut agglutinin binding-glycoprotein expression during progression of murine mammary neoplasia. Br J Cancer. 1992;65(5):641–8. doi: 10.1038/bjc.1992.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Tsuji T, Ibaragi S, Shima K, Hu MG, Katsurano M, Sasaki A, et al. Epithelial-mesenchymal transition induced by growth suppressor p12CDK2-AP1 promotes tumor cell local invasion but suppresses distant colony growth. Cancer Res. 2008;68(24):10377–86. doi: 10.1158/0008-5472.CAN-08-1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.McAllister SS, Gifford AM, Greiner AL, Kelleher SP, Saelzler MP, Ince TA, et al. Systemic endocrine instigation of indolent tumor growth requires osteopontin. Cell. 2008;133(6):994–1005. doi: 10.1016/j.cell.2008.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Kim MY, Oskarsson T, Acharyya S, Nguyen DX, Zhang XH, Norton L, et al. Tumor self-seeding by circulating cancer cells. Cell. 2009;139(7):1315–26. doi: 10.1016/j.cell.2009.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Nomura M, Li E. Smad2 role in mesoderm formation, left-right patterning and craniofacial development. Nature. 1998;393(6687):786–90. doi: 10.1038/31693. [DOI] [PubMed] [Google Scholar]
- 229.Waldrip WR, Bikoff EK, Hoodless PA, Wrana JL, Robertson EJ. Smad2 signaling in extraembryonic tissues determines anterior-posterior polarity of the early mouse embryo. Cell. 1998;92(6):797–808. doi: 10.1016/s0092-8674(00)81407-5. [DOI] [PubMed] [Google Scholar]
- 230.Zhu Y, Richardson JA, Parada LF, Graff JM. Smad3 mutant mice develop metastatic colorectal cancer. Cell. 1998;94(6):703–14. doi: 10.1016/s0092-8674(00)81730-4. [DOI] [PubMed] [Google Scholar]
- 231.Datto MB, Frederick JP, Pan L, Borton AJ, Zhuang Y, Wang XF. Targeted disruption of Smad3 reveals an essential role in transforming growth factor β-mediated signal transduction. Mol Cell Biol. 1999;19(4):2495–504. doi: 10.1128/mcb.19.4.2495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Yang X, Letterio JJ, Lechleider RJ, Chen L, Hayman R, Gu H, et al. Targeted disruption of SMAD3 results in impaired mucosal immunity and diminished T cell responsiveness to TGF-β. EMBO J. 1999;18(5):1280–91. doi: 10.1093/emboj/18.5.1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Kretschmer A, Moepert K, Dames S, Sternberger M, Kaufmann J, Klippel A. Differential regulation of TGF-β signaling through Smad2, Smad3 and Smad4. Oncogene. 2003;22(43):6748–63. doi: 10.1038/sj.onc.1206791. [DOI] [PubMed] [Google Scholar]
- 234.Dzwonek J, Preobrazhenska O, Cazzola S, Conidi A, Schellens A, van Dinther M, et al. Smad3 is a key nonredundant mediator of transforming growth factor β signaling in Nme mouse mammary epithelial cells. Mol Cancer Res. 2009;7(8):1342–53. doi: 10.1158/1541-7786.MCR-08-0558. [DOI] [PubMed] [Google Scholar]
- 235.Piek E, Ju WJ, Heyer J, Escalante-Alcalde D, Stewart CL, Weinstein M, et al. Functional characterization of transforming growth factor β signaling in Smad2- and Smad3-deficient fibroblasts. J Biol Chem. 2001;276(23):19945–53. doi: 10.1074/jbc.M102382200. [DOI] [PubMed] [Google Scholar]
- 236.Brown KA, Pietenpol JA, Moses HL. A tale of two proteins: differential roles and regulation of Smad2 and Smad3 in TGF-β signaling. J Cell Biochem. 2007;101(1):9–33. doi: 10.1002/jcb.21255. [DOI] [PubMed] [Google Scholar]
- 237.Petersen M, Pardali E, van der Horst G, Cheung H, van den Hoogen C, van der Pluijm G, et al. Smad2 and Smad3 have opposing roles in breast cancer bone metastasis by differentially affecting tumor angiogenesis. Oncogene. 2010;29(9):1351–61. doi: 10.1038/onc.2009.426. [DOI] [PubMed] [Google Scholar]
- 238.Tian F, DaCosta Byfield S, Parks WT, Yoo S, Felici A, Tang B, et al. Reduction in Smad2/3 signaling enhances tumorigenesis but suppresses metastasis of breast cancer cell lines. Cancer Res. 2003;63(23):8284–92. [PubMed] [Google Scholar]
- 239.Tang B, Vu M, Booker T, Santner SJ, Miller FR, Anver MR, et al. TGF-β switches from tumor suppressor to prometastatic factor in a model of breast cancer progression. J Clin Invest. 2003;112(7):1116–24. doi: 10.1172/JCI18899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Tian F, Byfield SD, Parks WT, Stuelten CH, Nemani D, Zhang YE, et al. Smad-binding defective mutant of transforming growth factor β type I receptor enhances tumorigenesis but suppresses metastasis of breast cancer cell lines. Cancer Res. 2004;64(13):4523–30. doi: 10.1158/0008-5472.CAN-04-0030. [DOI] [PubMed] [Google Scholar]
- 241.Korpal M, Yan J, Lu X, Xu S, Lerit DA, Kang Y. Imaging transforming growth factor-β signaling dynamics and therapeutic response in breast cancer bone metastasis. Nature medicine. 2009;15(8):960–6. doi: 10.1038/nm.1943. [DOI] [PubMed] [Google Scholar]
- 242.Giampieri S, Manning C, Hooper S, Jones L, Hill CS, Sahai E. Localized and reversible TGFβ signalling switches breast cancer cells from cohesive to single cell motility. Nat Cell Biol. 2009;11(11):1287–96. doi: 10.1038/ncb1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Giampieri S, Pinner S, Sahai E. Intravital imaging illuminates transforming growth factor β signaling switches during metastasis. Cancer Res. 2010;70(9):3435–9. doi: 10.1158/0008-5472.CAN-10-0466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Butcher DT, Alliston T, Weaver VM. A tense situation: forcing tumour progression. Nat Rev Cancer. 2009;9(2):108–22. doi: 10.1038/nrc2544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Paszek MJ, Weaver VM. The tension mounts: mechanics meets morphogenesis and malignancy. J Mammary Gland Biol Neoplasia. 2004;9(4):325–42. doi: 10.1007/s10911-004-1404-x. [DOI] [PubMed] [Google Scholar]
- 246.Kumar S, Weaver VM. Mechanics, malignancy, and metastasis: the force journey of a tumor cell. Cancer Metastasis Rev. 2009;28(1-2):113–27. doi: 10.1007/s10555-008-9173-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Sugahara KN, Teesalu T, Karmali PP, Kotamraju VR, Agemy L, Girard OM, et al. Tissue-penetrating delivery of compounds and nanoparticles into tumors. Cancer Cell. 2009;16(6):510–20. doi: 10.1016/j.ccr.2009.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Kota J, Chivukula RR, O’Donnell KA, Wentzel EA, Montgomery CL, Hwang HW, et al. Therapeutic microRNA delivery suppresses tumorigenesis in a murine liver cancer model. Cell. 2009;137(6):1005–17. doi: 10.1016/j.cell.2009.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Tsuda N, Ishiyama S, Li Y, Ioannides CG, Abbruzzese JL, Chang DZ. Synthetic microRNA designed to target glioma-associated antigen 1 transcription factor inhibits division and induces late apoptosis in pancreatic tumor cells. Clin Cancer Res. 2006;12(21):6557–64. doi: 10.1158/1078-0432.CCR-06-0588. [DOI] [PubMed] [Google Scholar]
- 250.Bhardwaj A, Singh S, Singh AP. MicroRNA-based Cancer Therapeutics: Big Hope from Small RNAs. Mol Cell Pharmacol. 2010;2(5):213–9. doi: 10.4255/mcpharmacol.10.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Weiler J, Hunziker J, Hall J. Anti-miRNA oligonucleotides (AMOs): ammunition to target miRNAs implicated in human disease? Gene Ther. 2006;13(6):496–502. doi: 10.1038/sj.gt.3302654. [DOI] [PubMed] [Google Scholar]
- 252.Krutzfeldt J, Rajewsky N, Braich R, Rajeev KG, Tuschl T, Manoharan M, et al. Silencing of microRNAs in vivo with ‘antagomirs’. Nature. 2005;438(7068):685–9. doi: 10.1038/nature04303. [DOI] [PubMed] [Google Scholar]
- 253.Gumireddy K, Young DD, Xiong X, Hogenesch JB, Huang Q, Deiters A. Small-molecule inhibitors of microrna miR-21 function. Angew Chem Int Ed Engl. 2008;47(39):7482–4. doi: 10.1002/anie.200801555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Ebert MS, Neilson JR, Sharp PA. MicroRNA sponges: competitive inhibitors of small RNAs in mammalian cells. Nat Methods. 2007;4(9):721–6. doi: 10.1038/nmeth1079. [DOI] [PMC free article] [PubMed] [Google Scholar]