Abstract
Complications of post-splenectomy, especially intra-abdominal hemorrhage can be fatal, with delayed or inadequate treatment having a high mortality rate. The objective of this study was to investigate the cause, prompt diagnosis, and outcome of the fatal complications after splenectomy with a focus on early diagnosis and management of hemorrhage after splenectomy. The medical files of patients who underwent splenectomy between January 1990 and March 2011 were reviewed retrospectively. The cause, characteristics, management, and outcome in patients with post-splenectomy hemorrhage were analyzed. Fourteen of 604 patients (1.19%) undergoing splenectomy had intraperitoneal hemorrhage: reoperation was performed in 13 patients, and 3 patients died after reoperation, giving the hospital a mortality rate of 21.43%; whereas, 590 of 604 patients (98%) had no hemorrhage following splenectomy, and the mortality rate (0.34%) in this group was significantly lower (P < 0.001). The complications following splenectomy, including pneumonia pancreatitis, gastric fistula, gastric flatulence, and thrombocytosis, in patients with postoperative hemorrhage were significantly higher than those without hemorrhage (P < 0.001). According to the reasons for splenectomy, 14 patients with post-splenectomy hemorrhage were grouped into two groups: splenic trauma (n = 9, group I) and portal hypertension (n = 5, group II). The median interval between splenectomy and diagnosis of hemorrhage was 15.5 hours (range, 7.25–19.5 hours). No differences were found between groups I and II in terms of incidence of postoperative hemorrhage, time of hemorrhage after splenectomy, volume of hemorrhage, and mortality of hemorrhage, except transfusion. Intra-abdominal hemorrhage after splenectomy is associated with higher hospital mortality rate and complications. Early massive intraperitoneal hemorrhage is often preceded by earlier sentinel bleeding; careful clinical inquiry and ultrasonography are the mainstays of early diagnosis.
Keywords: Splenectomy, Intra-abdominal hemorrhage, Postoperative complications, Splenic trauma, Portal hypertension
Splenectomy is usually performed for patients with severe splenic trauma, portal hypertension, splenomegaly due to hematologic diseases, or splenic tumors. Intraperitoneal hemorrhage is a fatal complication following splenectomy.1–3 It is associated with surgical manipulation and hematologic coagulation. For prompt management of bleeding, it is important to make the diagnosis promptly by carefully observing the clinical manifestation, monitoring the blood hemoglobin level, and imaging with ultrasonography.
The literature on intraperitoneal hemorrhage after splenectomy is sparse. The exact incidence of post-splenetic hemorrhage is not clear. The aim of this study was to analyze the hospital mortality, the incidence of postoperative hemorrhage, and the prompt diagnosis and treatment of hemorrhage following splenectomy.
Materials and Methods
After approval by the institutional review board, medical and surgical index databases were used to identify all consecutive patients undergoing splenectomy from January 1990 to March 2011. The inclusion conditions were all patients who underwent total splenectomy. Exclusion conditions were patients with gastrointestinal (GI) hemorrhage or patients with splenic trauma who were treated conservatively with no operation, partial splenectomy, or splenic autograft transplantation after total splenectomy.
The variables were extracted from the medical files of patients who underwent splenectomy, including demographics, comorbidity, and etiology of splenectomy, clinical manifestation, site of hemorrhage, and time of postoperative complications. GI hemorrhage referred to the presence of hematemesis, melaena, hematochezia, or blood in the nasogastric tube. Postoperative hemorrhage was defined as an acute decrease of hemoglobin concentration of 20 g/L or more in a surgical patient with overt hemorrhage or hemodynamic instability in an otherwise stable patient without septic shock or abdominal compartment syndrome. Intraperitoneal fluid was defined as blood emanating from the abdominal cavity through drains, or abdominal distension and hemodynamic instability in patients without drains, or intra-abdominal hemorrhage confirmed by ultrasonography or computed tomography (CT) scan. Sentinel hemorrhage was defined as blood extravasating around the abdominal drain. Patients with thrombocytosis were recorded. Aspirin (100 mg/d) was given orally to patients with platelet counts greater than 500 × 109/L.
Statistical analysis was performed with the χ2 test, the 2-tailed Fisher's exact test and the Mann-Whitney U analysis, when applicable. A P value <0.05 was defined as statistically significant. SPSS software (13.0) was used for analysis.
Results
The mortality and complications including pancreatitis, gastric flatulence, pneumonia, and thrombocytosis requiring medical treatment were compared (Table 1). A total of 604 patients underwent splenectomy for splenic trauma (n = 291) and portal hypertension (n = 313). Overall, 14 patients (2.32 %) with hemorrhage complications were identified.
Table 1 .
Complications in patients with hemorrhage versus no hemorrhage after splenectomy
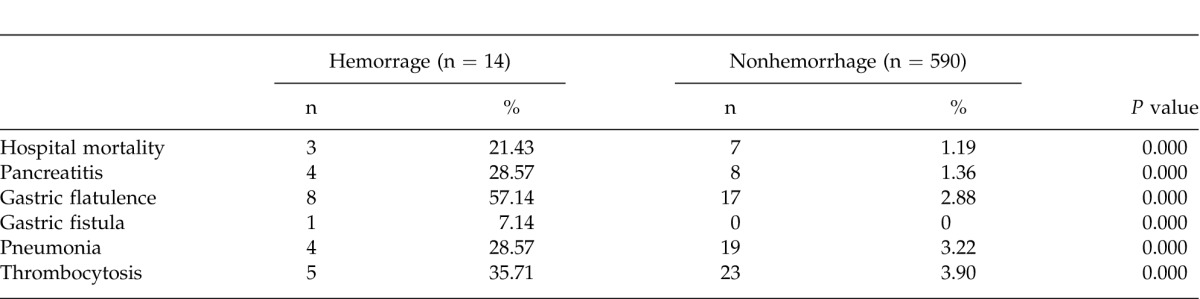
Mortality
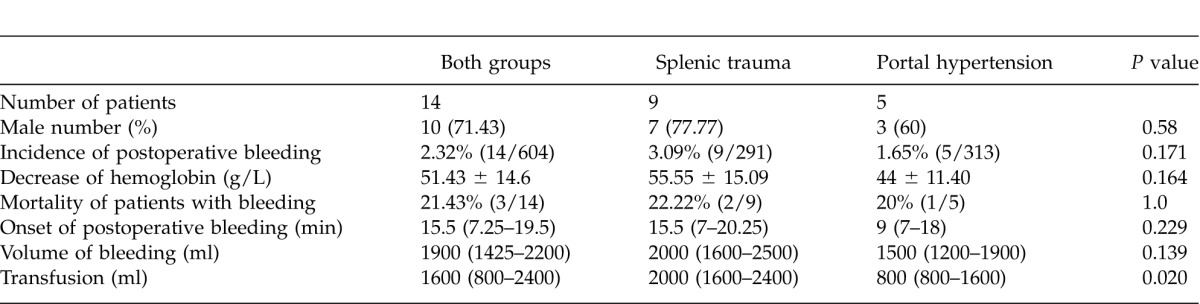
Of 604 patients undergoing splenectomy, 10 patients died in hospital, giving the overall hospital mortality of 1.66% (10 of 604 patients). The hospital mortality rate in patients with hemorrhage after splenectomy (hemorrhage group) was 21.43% (3 of 14 patients), whereas 7 of 590 patients with no hemorrhage after splenectomy (non-hemorrhage group) died of multiple organ failure after splenectomy, giving the mortality rate of 1.19%; the difference in mortality in both groups was significant (P < 0.0001) (Table 1). The mortality rate in patients undergoing splenectomy because of splenic trauma versus portal hypertension was similar (22.22% versus 20%, P > 0.05) (Table 2).
Table 2 .
Comparison of hemorrhage after splenectomy for splenic trauma and portal hypertension
Three patients with postsplenic hemorrhage died. In patient one, the amylase level was abnormally high in the bloody abdominal drainage. Active hemorrhage from the pancreatic tail and splenic bed, pancreatic tail injury, and pancreatitis were noticed on the second surgical exploration. Bloody drainage with a high level of pancreatic amylase persisted after the operation; thus a third exploration was performed, and the patient eventually died from hemorrhagic shock and multiple organ failure following the third operation. The second patient had hemorrhage from the short gastric artery. Even hemostasis was ensured with extensive suturing and ligation during the second operation; the gastric fistula occurred later, and the patient died 20 days after the second operation. The third patient had portal hypertension with hepatic failure and coagulopathy; extensive hemorrhage from the splenic bed and pancreatic tail was found during the laparotomy, and the patient died from hepatic failure and coagulopathy.
Clinical manifestation of hemorrhage
Fourteen patients had postoperative intraperitoneal bleeding: 12 patients had hemorrhage within 24 hours after splenectomy; 1 patient had hemorrhage on day 4 after splenectomy; and 1 patient, on day 6 after splenectomy. All patients with intraperitoneal hemorrhage were explored surgically, except one who received conservative treatment. Twelve of 14 patients experienced a sudden fall in hemoglobin level within 24 hours after surgery. The median interval from the ending of splenectomy to the diagnosis of hemorrhage was 15.5 hours (range, 7.25–19.5 hours).
Management of hemorrhage
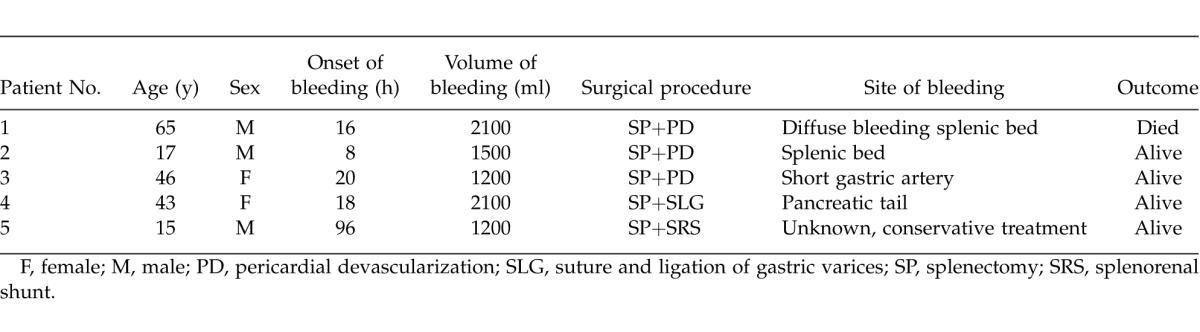
Tables 3 and 4 summarize the time and sites of hemorrhage, the therapeutic approaches, and the outcome of patients with postoperative hemorrhage. Blood was transfused at a median volume of 1600 ml (range, 800-2400 ml) for all patients. The hemoglobin level was decreased at 51.43 ± 14.6 g/L. The hemorrhage sites were splenic bed (n = 6), short gastric artery (n = 4), pancreatic tail (n = 4), and splenic artery (n = 1). Minor blood loss around the surgical drains (sentinel bleeding) was found in 6 patients in group I and in 2 patients in group II. The sentinel hemorrhage occurred a few hours prior to sudden massive intra-abdominal bleeding (Tables 3 and 4).
Table 3 .
Intraperitoneal hemorrhage after splenectomy in 9 patients with traumatic splenic injury
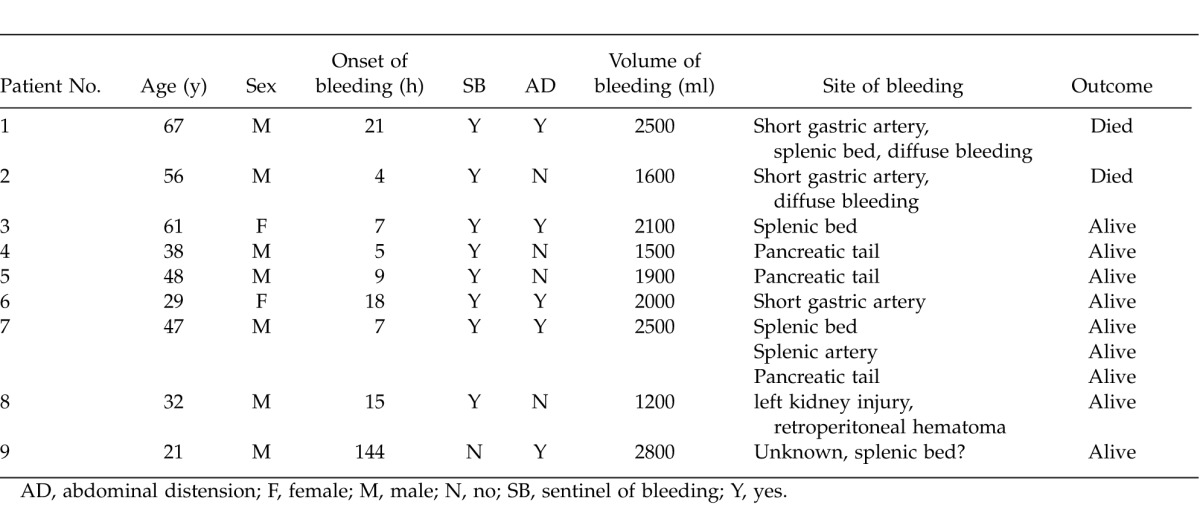
Table 4 .
Overview of hemorrhage after splenectomy in 5 patients with portal hypertension
Delayed intra-abdominal hemorrhage
Delayed hemorrhage occurred in 2 patients at 96 hours and 144 hours after splenectomy, respectively. One patient with portal hypertension underwent splenectomy and distal splenorenal (Warren) shunt; 140 ml and 20 ml of bloody collection was drained on postoperative day 1 and day 2, respectively; on day 3, no blood was drained from the intra-abdominal drainage tube, therefore, the drainage catheter was removed.
As the blood platelet count increased to 790 × 109/L, aspirin 100 mg/d and clopidogrel 75 mg/d were administered orally. On day 4, this patient experienced progressive abdominal pain and was managed as intestinal colic. On day 6, this patient became pale, his abdomen was extended, and the pain could not be controlled with meperidine. The intra-abdominal fluid was detected by duplex ultrasonography, and 1200 ml of uncoagulated blood was aspirated from the abdominal cavity. The anticoagulant (aspirin and clopidogrel) was terminated, and the patient was treated conservatively with blood transfusion (800 ml) and colloid solution. The coagulation profiles had been normal after surgery.
The second patient had been uneventful within the first 2 days after surgery, yet on postoperative day 3, the blood platelet count increased to 910 × 109/L; 3000 IU low molecular weight heparin was injected subcutaneously, and aspirin 100 mg/d and clopidogrel 75 mg/d were administered orally. On day 4, the platelet count increased to 1080 × 109/L, the patient started experiencing progressive but tolerable abdominal pain; the pain peaked on the sixth postoperative day and was not controlled by morphine. The patient complained of intolerable shifting pain from abdomen to penis and then anus, severe abdominal pain, and distension. Massive abdominal fluid was detected on duplex ultrasound, urgent exploration was performed, and a massive blood clot was found and evacuated from the splenic bed all the way to the pelvic cavity along the mesenteric root. Hematoma and injury on the intestinal wall were found in the vicinity of the drainage tube. Then, hemostasis was ensured.
Discussion
Massive intraperitoneal hemorrhage after splenectomy is not common; the mortality rate in patients with hemorrhage after splenectomy is rarely reported. Our patients were grouped into hemorrhage after splenectomy (14 patients) and nonhemorrhage post-splenectomy (590 patients). Three patients died in the hemorrhage group, making the hospital mortality rate 21.43%, whereas 7 patients in the nonhemorrhage group died of traumatic multiple organ failure, making the hospital mortality rate 1.19%, the former is significantly higher than the latter (P < 0.0001). The high mortality rate in patients with hemorrhage after splenectomy is associated with perioperative massive bleeding, postoperative complications, and subsequent reoperation. The mortality rates in open splenectomy have been reported as 1.1% to 1.63%,1,2 and the overall mortality in our group was 1.66%, which is in agreement with the literature.
The incidences of intraperitoneal hemorrhage after splenectomy is varied.3 In the present series, the incidence of hemorrhage is 2.32% among patients undergoing splenectomy; this is comparable with 2.4% reported in the literature.2 Common sources of hemorrhage following splenectomy include the raw edges of the divided splenic attachments, short gastric or hilar vessel remnants, and surrounding structures such as the pancreatic tail.4 Post-splenic hemorrhage requiring reoperation is rare yet has been reported as 1.6% in one series.4 In our hemorrhage group, 13 of 14 patients required reoperation to control the unstable hemodynamic conditions. The postoperative hemorrhage is related to surgical manipulation in most cases as well as severe trauma to patients.
In the present series, some medical conditions such as the use of anticoagulant agents, pancreatic injury during surgery, or pancreatic fistula were identified, which might be the risk factors leading to hemorrhage after splenectomy. More important, the postoperative hemorrhage is associated with surgical skills in manipulation of the splenic artery and the short gastric artery for patients with traumatic splenic injury or splenomegaly. In portal hypertension, splenomegaly has extensive adhesion with surrounding and collateral tissue, hemorrhage occurs easily in the operation for massive splenomegaly because of the friability of dilated veins. Careful hemostasis is critical in preventing postoperative bleeding. Intraabdominal hemorrhage after splenectomy usually occurs in patients who undergo splenectomy for thrombocytopenia, especially those in whom the platelet count does not respond to splenectomy; however, it could also occur in patients on anticoagulants to control the tendency of increased levels of platelets after splenectomy, as with 2 patients in our series.
The incidence of thrombosis after splenectomy is approximately 5% and accounts for about 19% of cases in hospitalized patients.5 It usually occurs 2 days after splenectomy; there is a compelling evidence for a hypercoagulable state following splenectomy.6 Extreme thrombocytosis may cause thrombotic events such as acute myocardial infarction, mesenteric vein thrombosis, and pulmonary embolism. When the platelet count is greater than 500 × 109/L, prophylactic use of anticoagulants is indicated. Use of anticoagulant prophylaxis after splenectomy to prevent thrombosis has increased the risk of hemorrhage. Two patients in our series had increased platelet counts, therefore aspirin, clopidogrel, or enoxaparin were administered prophylactically for 2 to 3 days, and these 2 patients had delayed intra-abdominal bleeding. The anticoagulant might resolve the clot in small vessels that were not hemorrhaging due to spasm of small artery or thrombosis in the small vessel during and after surgery even though these vessels may not be tied firmly during surgery. However, this explanation is not substantiated with convincing evidence because 3.9% patients with no hemorrhage had thrombocytosis and were treated with anticoagulants as well; no hemorrhage occurred (Table 1).
Injury to the pancreas occurs in 1% to 3% of patients who undergo splenectomy. It may be clinically unrecognized with high serum amylase level or cause clinical pancreatitis and pancreatic fistula. Serum amylase or lipase determination on the second to fourth day after surgery may help to identify the pancreatic injury. Symptoms and signs usually develop within 4 to 5 days after splenectomy. The incidence of pancreatitis in patients with hemorrhage was 28.57%, which is significantly higher than in those with no hemorrhage (1.36%). Careful manipulation of pancreatic tail during splenectomy would prevent this complication.7
During splenectomy, the short gastric vessels should be clearly divided and ligated or even sutured, distended stomach could cause the loss of ties on the stomach. The incidence of gastric flatulence in patients with hemorrhage was higher than those with no hemorrhage (57.14% versus 2.88%, P < 0.0001). Gastric fistula can result from necrosis of the gastric wall due to ligation of the short gastric vessels where gastric wall tissue is incorporated into the suture ligature. In our series, one gastric fistula occurred following ligation of short gastric vessels during hemostasis despite the use of nasogastric decompression for 3 days to prevent gastric distension. Thus, care should be taken to reinforce the gastric wall if the short gastric vessels have been clipped or ligated too close to the gastric wall.
A persistent abdominal pain after splenectomy may predict an early sign of intra-abdominal hemorrhage and warrants the medical staff to suspect postoperative bleeding. In general, intraperitoneal drain within 24 hours after splenectomy is usually less than 200 to 400 ml; drained solution is usually dark bloody in color, and the drained volume is then gradually decreased. Ultrasonography was established in 7 of 10 patients undergoing ultrasound scan in the present series; ultrasonography was helpful in diagnosing and confirming hemorrhage. Although CT angiography (CTA) has been suggested to locate the hemorrhage site,8 this was not verified in the present study.
Reoperation to gain hemostasis is indicated if fresh hemorrhage continues after coagulation abnormalities are corrected or if drained blood is more than 500 ml within 24 hours, or hemodynamic instability occurs. Correct timing of laparotomy and a less aggressive and more careful surgical technique, as well as meticulous positioning of drains to avoid close proximity to major blood vessels, may help reduce postoperative hemorrhage.
The present study was limited by retrospective nature and small number of patients with hemorrhage post-splenectomy. In addition, the hemorrhage source could not be located in a few patients.
In conclusion, intra-abdominal hemorrhage after splenectomy is associated with a higher hospital mortality rate and complications. Early massive intraperitoneal hemorrhage is often preceded by earlier sentinel bleeding; careful clinical inquiry and ultrasonography are the mainstays of early diagnosis. Prompt diagnosis and meticulous management of hemorrhage after splenectomy is paramount for satisfactory prognosis.
References
- 1.Kojouri K, Vesely SK, Terrell DR, George JN. Splenectomy for adult patients with idiopathic thrombocytopenic purpura: a systematic review to assess long-term platelet count responses, prediction of response, and surgical complications. Blood. 2004;104(9):2623–2634. doi: 10.1182/blood-2004-03-1168. [DOI] [PubMed] [Google Scholar]
- 2.Donini A, Baccarani U, Terrosu G, Corno V, Ermacora A, Pasqualucci A, et al. Laparoscopic vs open splenectomy in the management of hematologic diseases. Surg Endosc. 1999;13(12):1220–1225. doi: 10.1007/pl00009625. [DOI] [PubMed] [Google Scholar]
- 3.Winslow ER, Brunt M. Perioperative outcomes of laparoscopic versus open splenectomy: a meta-analysis with an emphasis on complications. Surgery. 2003;134(4):647–655. doi: 10.1016/s0039-6060(03)00312-x. [DOI] [PubMed] [Google Scholar]
- 4.Shackford SR, Molin M. Management of splenic injuries. Surg Clin North Am. 1990;70(3):595. doi: 10.1016/s0039-6109(16)45132-7. [DOI] [PubMed] [Google Scholar]
- 5.Maung AA, Kaplan LJ, Frankel HL, Collins KA. Diagnosis and management of splenic injury in the adult trauma patient. 2012 Available at: http://www.uptodate.com/contents/diagnosis-and-management-of-splenic-injury-in-the-adult-trauma-patient?source=search_result&search=bleeding+after+splenectomy&selectedTitle=21%7E150. Accessed August 2, [Google Scholar]
- 6.Crary SE, Buchanan GR. Vascular complications after splenectomy for hematologic disorders. Blood. 2009;114(14):2861–2868. doi: 10.1182/blood-2009-04-210112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ren S, Liu P, Zhou N, Dong J, Liu R. Complications after pancreaticoduodenectomy for pancreatic cancer: a retrospective study. Int Surg. 2011;96(3):220–227. doi: 10.9738/cc17.1. [DOI] [PubMed] [Google Scholar]
- 8.Anderson SW, Varghese JC, Lucey BC, Burke PA, Hirsch EF, Soto JA. Blunt splenic trauma: delayed-phase CT for differentiation of active hemorrhage from contained vascular injury in patients. Radiology. 2007;243(1):88–95. doi: 10.1148/radiol.2431060376. [DOI] [PubMed] [Google Scholar]


