Abstract
A 38-year-old woman presented for evaluation of a firm mass (measuring 20 × 20 mm) in the upper outer quadrant of her left breast. On the basis of the clinical and radiologic findings, we diagnosed a benign breast tumor and scheduled removal by a hand-held vacuum-assisted biopsy device (VABD) under ultrasonographic guidance. Because the first specimen removed from the tumor was white, flaky, and waxy material, we strongly suspected that the lesion was an epidermal cyst. We continued VABD treatment until the tumor was invisible on real-time ultrasonography. Histologic examination demonstrated that the tumor was composed of mature stratified squamous epithelium and laminated layers of keratin, findings consistent with a diagnosis of epidermal cyst. These cysts rarely occur in the breast and are sometimes difficult to distinguish from breast cancer. To our knowledge, this is the first report of an epidermal cyst treated by VABD.
Keywords: Epidermal cyst, Breast, Vacuum-assisted biopsy device (VABD)
Although an epidermal cyst is commonly found in the skin of the scalp, neck, and back, it is very rare in the breast.1 Such a cyst is sometimes difficult to differentiate from a malignant or benign breast tumor.2,3 Surgical removal of an epidermal cyst is probably appropriate to prevent complications such as rupture, infection, abscess formation, and malignant transformation.1,2,4–6 Here we report a patient with an epidermal cyst of the breast that was treated with a vacuum-assisted biopsy device (VABD).
Case Report
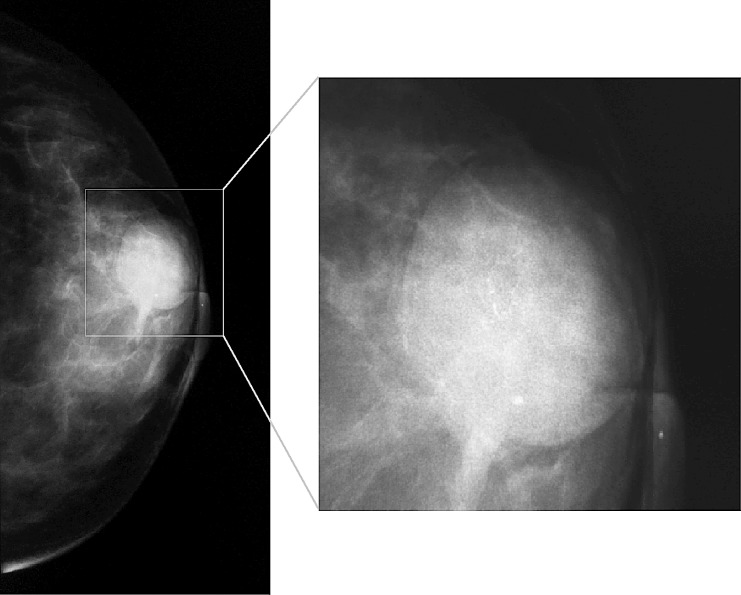
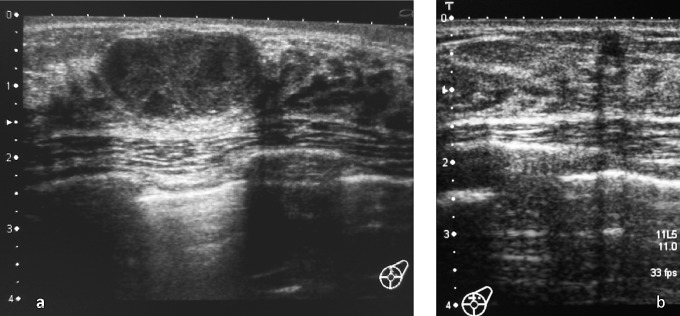
A 38-year-old woman visited our hospital because of a mass in her left breast that had been detected during a regular check-up. On examination, an oval, well-circumscribed mass (20 × 20 mm in diameter) was detected in the left C area. The tumor was firm and freely mobile. There were no changes of the overlying skin. Mammography showed a well-defined, dense mass lesion with heterogeneous calcification (Fig 1). Ultrasound examination revealed a well-circumscribed hypoechoic solid lesion with posterior acoustic enhancement and lateral shadowing (Fig. 2a). The mass was mainly located in the mammary gland.
Fig. 1 .
Mammography showed a well-defined, dense mass with heterogeneous calcification.
Fig. 2 .
Ultrasound revealed a well-circumscribed hypoechoic solid mass with posterior acoustic enhancement and lateral shadowing. The mass is mainly located in the mammary gland (a). Follow-up ultrasonography after 6 months revealed a hypoechoic lesion measuring 3 to 4 mm in diameter (b).
On the basis of these clinical and radiologic findings, the lesion was considered to be a benign breast tumor and we decided to remove it with a hand-held vacuum-assisted biopsy device (Mammotome, Ethicon Endo-Surgery, Johnson & Johnson, Cincinnati, Ohio) under ultrasonographic guidance using an APLIO SSA-700A ultrasound system (Toshiba, Tochigi, Japan) with a 7.5-MHz linear array transducer. After deciding on the site for insertion of the probe by preprocedural ultrasound, a small skin incision was made after infiltration with local anesthesia on the lateral side of the left breast. Then an 11-gauge probe was inserted and advanced to the lesion along its long axis and parallel to the muscle plane under ultrasonographic guidance. Because the first specimen removed from the tumor was white, flaky, and waxy material, we strongly suspected that the lesion was an epidermal cyst and continued the procedure until the tumor was no longer detected at the biopsy site on real-time ultrasonography.
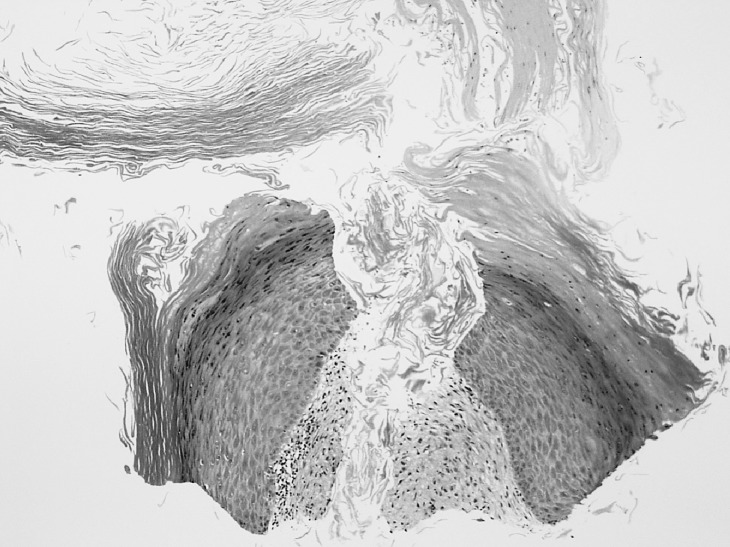
Histologic examination demonstrated that the lesion was composed of mature stratified squamous epithelium and laminated layers of keratin, which were findings consistent with an epidermal cyst (Fig. 3).
Fig. 3 .
Histologic examination demonstrated that the resected lesion was composed of mature stratified squamous epithelium and laminated layers of keratin; findings consistent with an epidermal cyst.
Infection or hematoma did not occur at the biopsy site after treatment and the scar was small and inconspicuous (Fig. 4). Follow-up ultrasonography of the left breast was done at 6 months after treatment, revealing a hypoechoic lesion 3 to 4 mm in diameter (Fig. 2b). Because a residual tumor was suspected, we recommended that the patient undergo additional treatment, but she chose to continue follow-up before having surgery or repeat VABD.
Discussion
Although epidermal cysts are common lesions of the scalp, face, neck, and trunk, these cysts are rarely found in the breast.1,7 In typical cases, it is easy to make a correct diagnose of epidermal cyst based on the clinical and radiologic findings.8 However, it is sometimes difficult to distinguish a cyst from breast cancer,6 especially if the lesions spreads into the breast parenchyma, as seen in our patient,2 or when rupture and infection occur.3,7 In such cases, fine needle aspiration cytology, core needle biopsy, or open biopsy is required to exclude malignancy.3,7
Epidermal cyst of the breast can have several complications, including spontaneous rupture, infection, abscess formation, and the possible risk of malignant transformation,4 therefore surgical removal is probably the most appropriate management.1,2,4–6 Also, patients are often concerned about breast tumors and request removal.1,5
More patients with an epidermal cyst want a less invasive treatment procedure with a good cosmetic outcome. Because standard wide elliptical excision often results in conspicuous scarring, other treatments for epidermal cyst have been recently introduced to minimize or conceal scarring. The punch incision technique9 and minimal excision method10 cause minimal scarring because the cyst wall and contents are removed through a small incision. However, a skin incision above the lesion is still required, therefore scarring can be problematic if the cyst is at a site that is not concealed by clothing. Endoscopic-assisted excision conceals the scar by placing it at an inconspicuous location away from the lesion. However, endoscopic-assisted excision needs general anesthesia, is time-consuming, and requires considerable skill.11
Recently, VABD has been used for removal of benign breast lesions because the procedure is simple and less time-consuming.12,13 It is also suitable for outpatient treatment under local anesthesia and causes minimal scarring.14 To our knowledge, this is the first report on treatment of an epidermal cyst with VABD. Epidermal cysts have wall lined by stratified squamous epithelium and contain soft, flaky keratinous debris.2 VABD sucks tissue through the aperture of the probe into the sampling chamber by creating a vacuum, cuts the tissue with a rotating hollow coaxial cutter, and then removes the specimen into the retrieval chamber.15 Accordingly, multidirectional and multiple specimens can be collected without the need to remove and reinsert the device. The vacuum can easily draw keratinous debris through the aperture of the probe into the sampling chamber and the cyst wall is then resected by the coaxial cutter. Thus, VABD can be use to remove an epidermal cyst without obvious scarring by inserting the probe at an inconspicuous location and has wide potential application for patients who request a good cosmetic outcome. If an epidermal cyst is located in the upper half of the breast, where the skin is sometimes exposed, VADB is an effective procedure for placing the scar at a site concealed by clothing. There is a possibility that a residual epidermal cyst will recur after treatment with VADB. However, it is expected that the residual cyst will be much smaller than the pretreatment cyst if the procedure is continued until the cyst is no longer detected by real-time ultrasonography. It can be treated easily by VABD in the same manner if a residual cyst is found at follow-up. Thus, VADB is another treatment option to consider for patients with epidermal cyst.
Fig. 4 .
At 6 months after the treatment, the scar was small and inconspicuous (arrow).
References
- 1.Crystal P, Shaco-Levy R. Concentric rings within a breast mass on sonography: lamellated keratin in an epidermal inclusion cyst. AJR. 2005;184:S47–S48. doi: 10.2214/ajr.184.3_supplement.01840s47. [DOI] [PubMed] [Google Scholar]
- 2.Taira N, Aogi K, Ohsumi S, Takashima S, Kawamura S, Nishimura R. Epidermal inclusion cyst of the breast. Breast Cancer. 2007;14:434–437. doi: 10.2325/jbcs.14.434. [DOI] [PubMed] [Google Scholar]
- 3.Wang IY, Lee J, Kim JS, Kim KT, Shin O. Ruptured epidermal inclusion cysts in the subareolar area: sonographic findings in two cases. Korean J Radiol. 2007;8:356–359. doi: 10.3348/kjr.2007.8.4.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chantra PK, Tang JT, Stanley TM, Bassett LW. Circumscribed fibrocystic mastopathy with formation of an epidermal cyst. AJR. 1994;163:831–832. doi: 10.2214/ajr.163.4.8092018. [DOI] [PubMed] [Google Scholar]
- 5.Morris PC, Cawson JN, Balasubramaniam GS. Epidermal cysts of the breast: detection in a screening programme. Australasian Radiology. 1999;43:12–15. doi: 10.1046/j.1440-1673.1999.00618.x. [DOI] [PubMed] [Google Scholar]
- 6.Bergmann-Koester CU, Kolberg HC, Rudolf I, Krueger S, Gellissen J, Stoeckelhuber BM. Epidermal cyst of the breast mimicking malignancy: clinical, radiological, and histological correlation. Gynecol Obstet. 2006;273:312–314. doi: 10.1007/s00404-005-0019-9. [DOI] [PubMed] [Google Scholar]
- 7.Kowand LM, Verhulst LA, Copeland CM, Bose B. Epidermal cyst of the breast. Can Med Assoc J. 1984;131:217–219. [PMC free article] [PubMed] [Google Scholar]
- 8.Gerlock AJ. Epidermal inclusion cyst of the breast associated with needle aspiration biopsy. Radiology. 1974;112:69–70. doi: 10.1148/112.1.69. [DOI] [PubMed] [Google Scholar]
- 9.Lee H, Yang C, Chen C, Hong H, Kuan Y. Comparison of the surgical outcomes of punch incision and elliptical excision in treating epidermal inclusion cysts: a prospective, randomized study. Dermatol Surg. 2006;32:520–525. doi: 10.1111/j.1524-4725.2006.32105.x. [DOI] [PubMed] [Google Scholar]
- 10.Zuber TJ. Minimal excision technique for epidermoid (sebaceous) cyst. Am Fam Physician. 2002;65:1409–1412. [PubMed] [Google Scholar]
- 11.Pricola KL, Dutta S. Stealth surgery: subcutaneous endoscopic excision of benign lesions of the trunk and lower extremity. J Pediatr Surg. 2010;45:840–844. doi: 10.1016/j.jpedsurg.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 12.Qutob O, Elahi B, Garimella V, Ihsan N, Drew PJ. Minimally invasive excision of gynecomastia—a novel and effective surgical technique. Ann R Coll Surg Engl. 2010;92:198–200. doi: 10.1308/003588410X12628812458815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iwuagwu O, Drew P. Vacuum-assisted biopsy device-diagnostic and therapeutic applications in breast surgery. The Breast. 2004;13:483–487. doi: 10.1016/j.breast.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 14.Ko EY, Bae Y, Kim M, Lee KS, Lee Y, Kim LS. Factors affecting the efficacy of ultrasound-guided vacuum-assisted percutaneous excision for removal of benign breast lesions. J Ultrasound Med. 2008;27:65–73. doi: 10.7863/jum.2008.27.1.65. [DOI] [PubMed] [Google Scholar]
- 15.Burbank F. Stereotactic breast biopsy: its history, its present, and its future. Am Surg. 1996;(62):128–150. [PubMed] [Google Scholar]