Abstract
Colovesical fistulas secondary to diverticular disease may be considered a contraindication to the laparoscopic approach. The feasibility of laparoscopic management of complicated diverticulitis and mixed diverticular fistulas has been demonstrated. However, few studies on the laparoscopic management of diverticular colovesical fistulas exist. A retrospective analysis was performed of 15 patients with diverticular colovesical fistula, who underwent laparoscopic-assisted anterior resection and bladder repair. Median operating time was 135 minutes and median blood loss, 75 mL. Five patients were converted to an open procedure (33.3%) with an associated increase in hospital stay (P = 0.035). Median time to return of bowel function was 2 days and median length of stay, 6 days. Overall morbidity was 20% with no major complications. There was no mortality. There was no recurrence during median follow-up of 12.4 months. These results suggest that laparoscopic management of diverticular colovesical fistulas is both feasible and safe in the setting of appropriate surgical expertise.
Keywords: Laparoscopy, Colovesical fistula, Diverticulosis, Diverticulitis, Minimally invasive surgical procedures
Laparoscopic management of diverticulitis has become widely accepted, including anterior resection for recurrent uncomplicated disease and lavage or drainage for purulent peritonitis and abscesses that cannot be drained percutaneously.1 Many studies have demonstrated the safety and feasibility of the laparoscopic approach in complicated diverticulitis.2,3 However colovesical fistulas are still considered a contraindication as a result of previously reported increased operating times and conversion rates.4–7
A review of the literature indicated very few studies on the laparoscopic management of diverticular colovesical fistulas exist.4,8,9 The outcomes of recent studies are difficult to interpret as many have incorporated both recurrent uncomplicated and complicated disease, have not differentiated between colovesical fistulas and other diverticular fistulas,10–15 or have included fistulas of various aetiologies.16–20 Other studies have not used a total laparoscopic approach but have performed technically challenging aspects with a resection-facilitated or hand-assisted technique.4,21–23 While these techniques improve operating times and preserve tactile feedback, their outcomes may not be comparable with a totally laparoscopic technique with intracorporeal suturing, and the inherent benefits of minimally invasive surgery are reduced.
Our study represents the largest series of diverticular colovesical fistulas treated with a totally laparoscopic approach including intracorporeal bowel anastomosis and bladder repair. We also present a review of the current literature regarding the laparoscopic management of complicated diverticular disease, diverticular fistulas, and colovesical fistulas.
Materials and Methods
A retrospective analysis of 15 consecutive patients undergoing elective laparoscopic-assisted anterior resection for diverticular disease complicated by colovesical fistula during the period November 2004 to November 2011. All patients had presented earlier with acute diverticulitis and were diagnosed with colovesical fistulas either clinically or radiologically. They underwent outpatient review and investigations including computed tomography (CT), colonoscopy, and/or cystoscopy before undergoing surgery no earlier than 6 weeks after resolution of acute diverticulitis.
The medical records were retrospectively reviewed and data were collected including patient characteristics, symptoms, investigation results, operative statistics, postoperative complications, and evidence of recurrence during follow-up. Operating time was defined as the time interval between incision and closure of the skin. The χ2 test was used to analyze for statistical significance, with a P value <0.05 considered significant.
Following administration of general anaesthesia, the patient was placed in the lithotomy position. A Hasson trocar was placed at the umbilicus and pneumoperitoneum established. A 10- to 15-mm port was inserted at the right lower quadrant and 5.5-mm ports were inserted at both upper quadrants and the suprapubic region, all under direct vision. Additional ports were inserted throughout the procedure as required. The patient was placed in a steep Trendelenburg position to displace the small bowel into the upper abdomen, allowing thorough laparoscopic assessment of the abdominal cavity and pelvis. The sigmoid colon was then dissected from adhesions and the bladder. The left colon was then mobilized laterally from the rectum past the splenic flexure to the distal transverse colon. The left ureter and gonadal vessels were identified and preserved in each instance. The inferior mesenteric artery and vein were ligated individually at high tie position, and the mesorectum was transected just below the anterior peritoneal reflection at healthy, nonfibroused bowel. The rectum was then transected with a laparoscopic linear stapler after irrigation with povidone iodine solution.
Significant bladder defects were repaired with intracorporeal suturing using interrupted 2/0 polyglactin 910 sutures (Vicryl, Ethicon Inc, Somerville, New Jersey). The bladder was then decompressed with an indwelling catheter for 5 days.
A 4-cm muscle-splitting incision was then made at the left lower quadrant, and the specimen was delivered through a protected wound. The proximal resection was performed, and an anvil was placed into the proximal segment and secured with a purse-string suture. The colon was then returned to the abdominal cavity, with the rectus sheath closed in layers and the pneumoperitoneum reestablished. An intraluminal circular stapler was introduced through the anus, and under laparoscopic guidance, the anvil and central rod were connected to create a colorectal anastomosis. The anastomosis was tested with air insufflation while immersed in water. Hemostasis was performed, and a routine rectal tube and pelvic drain were placed. The ports were closed routinely, with the Carter Thomason (Cooper Surgical, Trumbull, Connecticut) closure device used for larger port sites. Patients were encouraged to take oral clear fluids on the first postoperative day, followed by rapid diet escalation and early mobilization.
Results
The patients comprised 10 men and 5 women. One of the female patients had a history of hysterectomy with radiation therapy for uterine malignancy. The median age was 63.3 years (range, 39–83 years). The most common presenting symptom was pneumaturia (86.7%), followed by recurrent urinary tract infection (66.7%), abdominal pain (46.7%), and fecaluria (40%). Seven patients (46.7%) had a history of previous abdominal surgery.
All patients underwent preoperative colonoscopy and CT abdomen/pelvis to confirm diverticular disease and exclude other pathology including Crohn's disease and malignancy. Five patients (33.3%) had CT evidence of pneumaturia without previous instrumentation of the bladder. Two patients (13.3%) underwent preoperative cystoscopy.
The median operating time was 135 minutes (range, 85–240 minutes). The median estimated blood loss was 75 mL (range, 16–350 mL). Five patients (33.3%) were converted to an open procedure either via midline laparotomy or in one case, through a limited Pfannensteil incision. The most common reason for conversion (3 cases, 60%) was the presence of dense adhesions secondary to previous abdominal surgery. One patient had a large inflammatory mass with associated adhesions that was suggestive of malignancy and necessitated en bloc dissection. Malignancy was subsequently excluded on histopathology. One patient had a history of uterine cancer treated with hysterectomy and radiation therapy. She had very friable tissues, and small bowel loops were adhered to the pelvis. The decision to convert was made as early as possible, following initial laparoscopic assessment.
Despite optimizing for infection after acute diverticulitis by treating with antibiotics and delaying surgery for at least 6 weeks, 8 patients (53.3%) had intraoperative evidence of active diverticulitis with either gross or microscopic abscess formation and/or purulent discharge.
The median duration until return of bowel function, defined as passage of feces, was 2 days (range, 1–3 days). The median length of postoperative stay was 6 days (range, 4–12 days). All converted patients were admitted for longer than the median length of stay, compared with only 20% of nonconverted patients (P = 0.035).
Three patients had minor postoperative complications (20%) comprising a prolonged ileus, superficial wound infection, and lower respiratory tract infection. There were no major complications (including anastomotic leak) and no postoperative mortality. No patients had recurrence of diverticulitis or fistula at follow-up (mean, 12.4 months; range, 1–37 months).
Discussion
Diverticular disease and colovesical fistula
Diverticular disease is complicated by fistulas in 4% to 20% of patients. Colovesical fistulas are the most common, representing up to 65% of diverticular fistulas.24,25 Similarly, diverticulitis is the most common cause of colovesical fistulas (60%–70%) along with malignancy, inflammatory bowel disease, and radiation therapy.26–29 The pathogenesis involves direct extension of a ruptured diverticulum or erosion of a peridiverticular abscess into the bladder.29 They are more common in males and in women who have previously undergone hysterectomy.
It is widely agreed that there is no gold standard for the diagnosis of colovesical fistulas. A clinical diagnosis is based on pathognomonic signs including pneumaturia, fecaluria, and recurrent urinary tract infections with mixed organisms.27,29 The role of investigations is predominantly to identify the cause of the fistula.28 Colonoscopy and cystoscopy have a limited role in diagnosis because of poor sensitivity but are useful for clarifying anatomy and excluding strictures and malignancy. While all of our patients underwent preoperative colonoscopy, only 2 selectively underwent cystoscopy, where we needed to exclude bladder malignancy and identify any involvement of the ureteric orifices.
CT is the preferred diagnostic imaging modality owing to its high sensitivity (over 90%). Fistulas may be demonstrated by gas or contrast in the bladder, or local colonic and bladder wall thickening.24,29 While CT only demonstrated colovesical fistula in 35.7% of our patients, we utilized it routinely to assess the degree of pelvic inflammation and to determine optimal timing for surgery. Magnetic resonance imaging (MRI) is highly sensitive but expensive and less accessible.30
Management of diverticular disease
The surgical management of diverticular disease has evolved but still remains governed by clinical classification, namely, recurrent uncomplicated disease versus complicated disease. Initially, the surgical approach involved open resection in a 2- or 3-stage procedure, before trends shifted toward a single-stage procedure with primary anastomosis. The former is still recommended for perforated diverticulitis with fecal peritonitis, or purulent peritonitis where intraoperative conditions are unfavorable for primary anastomosis.1
As laparoscopic surgery became more popular, studies demonstrated the safety and efficacy of laparoscopic colorectal surgery with the advantages of decreased pain, better cosmesis, fewer wound complications, shorter hospital stay, and earlier return of bowel function.31–35 The overall cost reduction is also significant.36 The role of laparoscopic resection in diverticulitis was initially controversial, given the inflammatory nature of the disease. Not surprising, studies found longer operating times and higher risk of conversion with associated morbidity.37–40 However, with increased laparoscopic experience, refinement in technique, and advances in surgical technology, the indications broadened. Laparoscopic resection was demonstrated to be feasible and safe in recurrent uncomplicated disease.1,23,41–44 A randomized controlled trial comparing laparoscopic versus open surgery for symptomatic sigmoid diverticulitis found reduced major complication rates, shorter hospital stay, and improved quality of life in the laparoscopic group. There was an overall 27% reduction in postoperative morbidity, and long-term outcomes were comparable.45,46
However, the safety of laparoscopic surgery in complicated disease remained controversial. Many studies found that severity of disease was a predictor for conversion,5,21,37,47–50 but others could not demonstrate a significant difference.22,51,52 Conversion has traditionally been associated with higher morbidity,6,7,53 but this has been challenged.5,37 In a multi-center prospective study of laparoscopic management of diverticulitis, Scheidbach et al found that complication and conversion rates were initially higher in complicated disease but improved with surgeon experience.54 In a recent comparative analysis between laparoscopic versus open anterior resection for recurrent and complicated diverticulitis, Lu et al demonstrated significantly shorter operating times, earlier return of bowel function, shorter hospital stay, and a low conversion rate (3%). There was no significant difference in morbidity. Over 50% of the laparoscopic group had complicated disease, and 21% had a history of multiple previous abdominal surgeries.3 Overall, recent studies of laparoscopic management of complicated diverticulitis have demonstrated that in capable hands, operating times and conversion rates are acceptable, and morbidity and mortality rates are comparable with open surgery.2,6,7,43,55–58
Management of colovesical fistula
Despite the consensus that colovesical fistulas should be managed operatively, some reports have described successful nonoperative management in patients with comorbidities precluding surgery.26,59,60 Lynn et al suggested conservative management for patients with “complex” fistulas, including those with a history of radiation therapy and urethral, prostate, or rectal involvement as they have a higher recurrence rate.26 Given the inherent risk of sepsis associated with colovesical fistulas and the morbidity associated with complicated diverticular disease, we agree with the consensus that surgical intervention is warranted.
Surgical management of colovesical fistulas depends on the underlying etiology, with the fundamental principle being removal of the fistula and diseased segment of colon in order to prevent recurrence.28,61,62 In the setting of diverticular disease, the creation of a colorectal anastomosis is the most important predictor of recurrence, rather than the surgical approach used.1,2,63,64 Simple proximal diversion may provide symptomatic relief but rarely results in closure of the fistula, leading to recurrence upon restoration of continuity.28 Colovesical fistulas were traditionally managed with 2- or 3-stage procedures before a single-stage approach was found to have lower morbidity and shorter hospital stay.25,27,65 Despite this finding, morbidity rates remain high for open procedures (4% to 49%), and reoperation is commonly required (up to 17%).28,61
Bladder management
There is limited consensus over management of the bladder in colovesical fistula repair. Various techniques have been described including: the “pinch off” technique followed by simple closure; use of an omental patch to close the bladder defect; or wedge resection of the affected bladder area with closure using sutures or an omental patch. Simple decompression with an indwelling catheter alone may be sufficient for small defects.61,66,67 Lynn et al found the risk of recurrence was significantly higher in advanced bladder repairs, although this study included non-diverticular colovesical fistulas.26 Initially, it was recommended that the indwelling catheter remain in situ for 14 days; however, recent studies have shown no difference between early or late removal, and prolonged catheter use was associated with an increased risk of infection. There was no clear advantage to placement of ureteric stents.61
Laparoscopic management
Despite the growing support for laparoscopic management of complicated diverticulitis, colovesical fistulas are still considered a contraindication1 and have been identified as a risk factor for conversion and increased morbidity.5,37,68 However, many studies of laparoscopic resection for complicated diverticulitis have included colovesical fistulas and demonstrated acceptable results.3,7,48,50,54,56,58,69 In their comparative study of laparoscopic management of recurrent uncomplicated disease versus complicated disease, Zapletal et al included 8 colovesical fistulas and reported no mortality, major complications, or conversions in these patients.70 Pugliese et al reported no mortality, 10% morbidity, and 2.9% conversion rate in a study of 103 patients with complicated disease, including 17 with colovesical fistula.57
Our study represents the largest series of laparoscopically treated diverticular colovesical fistulas to date. There are very few studies focusing purely on colovesical fistula in the literature. Reports typically include fistulas of mixed etiology or mixed diverticular fistulas (colovaginal, colocutaneous, enterocolic), thus making the outcomes difficult to interpret. Puente et al described 2 cases that were managed without conversion or complication; however, the operating times were long (over 5 hours).8 Tsivian et al described another successful laparoscopic resection with a shorter operating time (230 minutes).9 In the current study, operating times were significantly lower (median 135 minutes) and compared favorably with those reported for laparoscopic management of complicated diverticular disease, diverticular fistulas, and mixed fistulas (see Table 1). Shorter operating times likely reflect the surgeon's experience and the evolution of surgical technology.
Table 1 .
Overall postoperative outcomes in the current literature compared with results of the current study—described as the range of reported percentage, time, or mean/median values
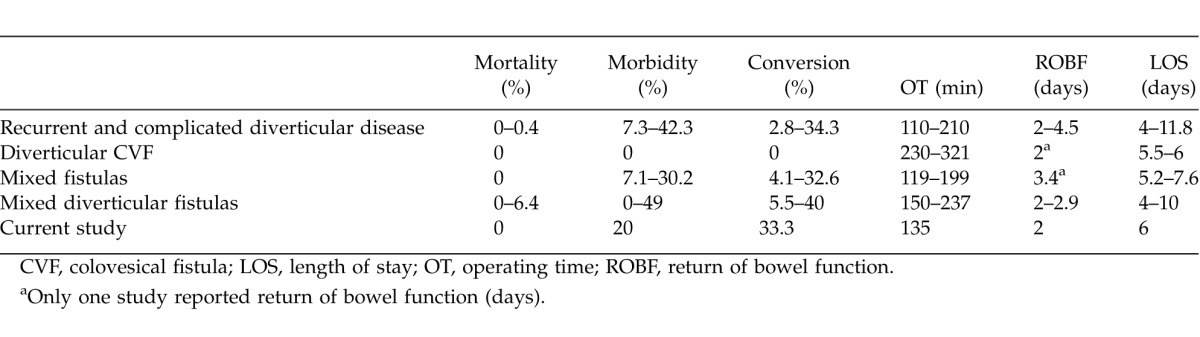
A recent meta-analysis of laparoscopic versus open surgery for sigmoid diverticulitis showed a significantly shorter length of hospital stay and earlier return of bowel function with the laparoscopic approach.2 Studies focusing on recurrent and complicated diverticular disease, mixed diverticular fistulas, and fistulas of mixed etiology have demonstrated similar results (Table 1), and the current study compared favorably. Of note, converted patients had a significantly longer hospital stay than nonconverted patients. Despite this, there was no significant difference in morbidity.
Studies on laparoscopic management of fistulas of mixed etiology have demonstrated overall morbidity between 7.1% and 30.2%.16–20 In a study of 43 patients including 9 with colovesical fistula, Pokala et al reported less morbidity (11% versus 30.2% overall) in the colovesical fistula group.20 Similar results have been reported for mixed diverticular fistulas (see Table 2), with morbidity ranging between 8% and 48%. In an early study that included 15 colovesical fistula patients, Menenakos et al reported 27.7% morbidity.11 More recent studies have demonstrated morbidity rates between 12% and 15%.12–14 The current study demonstrated an overall morbidity rate of 20%, with no major complications or laparoscopy-related complications. There was a higher rate of complications in converted patients (40% versus 11% for nonconverted), but this was not statistically significant (P = 0.925). Smeenk et al recently studied 40 patients (35 with colovesical fistula) and reported 48% morbidity, predominantly related to an anastomotic leak rate of 28%,15 which was unusually high compared with previous open and laparoscopic reports.11,14,25,28,62,65,66 They recommended routine defunctioning ileostomy with primary anastomoses; however, most authors agree that a primary anastomosis should be safe if created without tension and in the absence of gross purulence or distal obstruction.1,55 Bartus et al reported 8% morbidity in patients treated with the hand-assisted technique; however, the conversion rate and operating time were comparable with the laparoscopic approach.4 We suggest that with increased experience, similar low morbidity rates could be achieved with the totally laparoscopic technique.
Table 2 .
Overall postoperative outcomes in current literature for laparoscopic management of mixed diverticular fistulas (top) and diverticular colovesical fistulas (bottom).
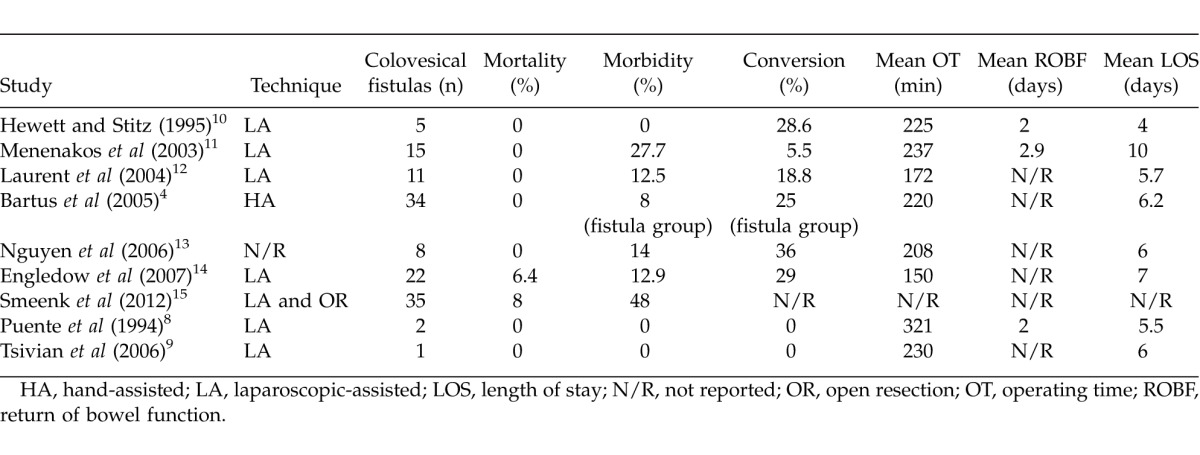
Studies of mixed fistulas have demonstrated conversion rates between 4.1% and 32.6%; however, they included fistulas caused by various etiologies. Pokala et al found a lower conversion rate (15.4% versus 32.6%) in colovesical fistula patients.20 Studies of diverticular fistulas have reported similar results. In an early retrospective study of 7 patients, Hewett et al demonstrated the laparoscopic approach was feasible, but conversion was required in 2 of the 5 patients (40%) with colovesical fistula.10 The current study had a conversion rate of 33.3%, which was comparable with rates from previous studies (see Table 2). Menenakos and Laurent et al reported lower conversion rates, perhaps owing to differences in the patient cohort.11,12 Overall, these results support previous suggestions that complicated disease is a risk factor for conversion. However, the relationship between conversion rates and surgical experience has been well documented.12–14 The current study followed this trend, with 4 conversions occurring during the first 4 years and only 1 conversion occurring during the last 4 years. It should be emphasised that appropriate early conversion can reduce intraoperative complications and postoperative morbidity.5,52,71 Some have advocated the use of resection-facilitated and hand-assisted techniques to reduce conversion rates. In a comparative study of laparoscopic versus resection-facilitated management of complicated diverticulitis, Eijsbouts et al demonstrated improved outcomes with the resection-facilitated approach.23 Lee et al found the trend towards increased conversion in complicated disease persisted even when using the hand-assisted technique, and Bartus et al demonstrated a conversion rate of 25% in their retrospective study of 34 diverticular colovesical fistulas treated with the same technique.4,21 Given these comparable results, we recommend using the totally laparoscopic technique where possible in order to maintain the advantages of minimally invasive surgery.
Limitations
Previous studies have been limited by the inclusion of other types of diverticular fistulas or fistulas caused by various pathologies, thus making it difficult to extrapolate results. The current study represents the largest series of laparoscopically treated diverticular colovesical fistulas in the literature. Limitations include the retrospective nature of the analysis and the small cohort. The patients were selected for elective resection by a single Colorectal surgeon experienced in advanced laparoscopic surgery, therefore selection bias may have occurred. Diverticular colovesical fistulas are relatively rare, making it difficult to perform a large cohort study. Given the known poor outcomes of open surgery, a comparative study of laparoscopic versus hand-assisted or resection-facilitated approaches may be more appropriate. However, it has been clearly demonstrated that the outcomes of laparoscopic management are highly dependent on the experience of the surgeon. These techniques may prove useful during the learning curve, but the authors suggest that with increased experience and the evolution of surgical technology, the totally laparoscopic approach will become routine in the setting of appropriate laparoscopic expertise.
Conclusion
The current study has demonstrated that in capable hands, laparoscopic management of diverticular colovesical fistulas is both feasible and safe with acceptable operating times, morbidity, conversion rates, and excellent postoperative recovery. Our outcomes were comparable with those reported for laparoscopic management of recurrent and complicated diverticular disease, mixed fistulas, and diverticular fistulas. Owing to the complex inflammatory nature of the underlying pathology, operating times tend to be longer and conversion rates higher than for uncomplicated disease. However, we emphasize the importance of appropriate early conversion in order to reduce intraoperative complications and postoperative morbidity. These procedures should be performed by a surgeon experienced in advanced laparoscopy and intracorporeal suturing. Alternative techniques such as hand-assisted and resection-facilitated approaches may be useful when experience is limited.
Acknowledgments
This article was previously presented at the 38th Biennial World Congress of the International College of Surgeons, Brisbane, Australia.
References
- 1.Kohler L, Sauerland S, Neugebauer E. Diagnosis and treatment of diverticular disease: results of a consensus development conference. The Scientific Committee of the European Association for Endoscopic Surgery. Surg Endosc. 1999;13(4):430–436. doi: 10.1007/s004649901007. [DOI] [PubMed] [Google Scholar]
- 2.Siddiqui MR, Sajid MS, Khatri K, Cheek E, Baig MK. Elective open versus laparoscopic sigmoid colectomy for diverticular disease: a meta-analysis with the Sigma trial. World J Surg. 2010;34(12):2883–2901. doi: 10.1007/s00268-010-0762-3. [DOI] [PubMed] [Google Scholar]
- 3.Lu CT, Ho YH. Elective laparoscopic surgical management of recurrent and complicated sigmoid diverticulitis. Tech Coloproctol. 2008;12(3):201–206. doi: 10.1007/s10151-008-0421-y. [DOI] [PubMed] [Google Scholar]
- 4.Bartus CM, Lipof T, Sarwar CMS, Vignati PV, Johnson KH, Sardella WV, et al. Colovesical fistula: not a contraindication to elective laparoscopic colectomy. Dis Colon Rectum. 2005;48(2):233–236. doi: 10.1007/s10350-004-0849-8. [DOI] [PubMed] [Google Scholar]
- 5.Le Moine MC, Fabre JM, Vacher C, Navarro F, Picot MC, Domergue J. Factors and consequences of conversion in laparoscopic sigmoidectomy for diverticular disease. Br J Surg. 2003;90(2):232–236. doi: 10.1002/bjs.4035. [DOI] [PubMed] [Google Scholar]
- 6.Alves A, Panis Y, Slim K, Heyd B, Kwiatkowski F, Mantion G. French multicentre prospective observational study of laparoscopic versus open colectomy for sigmoid diverticular disease. Br J Surg. 2005;92(12):1520–1525. doi: 10.1002/bjs.5148. [DOI] [PubMed] [Google Scholar]
- 7.Jones OM, Stevenson AR, Clark D, Stitz RW, Lumley JW. Laparoscopic resection for diverticular disease: follow-up of 500 consecutive patients. Ann Surg. 2008;248(6):1092–1097. doi: 10.1097/SLA.0b013e3181884923. [DOI] [PubMed] [Google Scholar]
- 8.Puente I, Sosa JL, Desai U, Sleeman D, Hartmann R. Laparoscopic treatment of colovesical fistulas: technique and report of two cases. Surg Laparosc Endosc. 1994;4(2):157–160. [PubMed] [Google Scholar]
- 9.Tsivian A, Kyzer S, Shtricker A, Benjamin S, Sidi AA. Laparoscopic treatment of colovesical fistulas: technique and review of the literature. Int J Urol. 2006;13(5):664–667. doi: 10.1111/j.1442-2042.2006.01382.x. [DOI] [PubMed] [Google Scholar]
- 10.Hewett PJ, Stitz R. The treatment of internal fistulae that complicate diverticular disease of the sigmoid colon by laparoscopically assisted colectomy. Surg Endosc. 1995;9(4):411–413. doi: 10.1007/BF00187162. [DOI] [PubMed] [Google Scholar]
- 11.Menenakos E, Hahnloser D, Nassiopoulos K, Chanson C, Sinclair V, Petropoulos P. Laparoscopic surgery for fistulas that complicate diverticular disease. Langenbecks Arch Surg. 2003;388(3):189–193. doi: 10.1007/s00423-003-0392-4. [DOI] [PubMed] [Google Scholar]
- 12.Laurent SR, Detroz B, Detry O, Degauque C, Honore P, Meurisse M. Laparoscopic sigmoidectomy for fistulized diverticulitis. Dis Colon Rectum. 2005;48(1):148–152. doi: 10.1007/s10350-004-0745-2. [DOI] [PubMed] [Google Scholar]
- 13.Nguyen SQ, Divino CM, Vine A, Reiner M, Katz LB, Salky B. Laparoscopic surgery for diverticular disease complicated by fistulae. JSLS. 2006;10(2):166–168. [PMC free article] [PubMed] [Google Scholar]
- 14.Engledow AH, Pakzad F, Ward NJ, Arulampalam T, Motson RW. Laparoscopic resection of diverticular fistulae: a 10-year experience. Colorectal Dis. 2007;9(7):632–634. doi: 10.1111/j.1463-1318.2007.01268.x. [DOI] [PubMed] [Google Scholar]
- 15.Smeenk RM, Plaisier PW, van der Hoeven JA, Hesp WL. Outcome of surgery for colovesical and colovaginal fistulas of diverticular origin in 40 patients. J Gastrointest Surg. 2012;16(8):1559–1565. doi: 10.1007/s11605-012-1919-1. [DOI] [PubMed] [Google Scholar]
- 16.Joo JS, Agachan F, Wexner SD. Laparoscopic surgery for lower gastrointestinal fistulas. Surg Endosc. 1997;11(2):116–118. doi: 10.1007/s004649900310. [DOI] [PubMed] [Google Scholar]
- 17.Poulin EC, Schlachta CM, Mamazza J, Seshadri PA. Should enteric fistulas from Crohn's disease or diverticulitis be treated laparoscopically or by open surgery? Dis Colon Rectum. 2000;43(5):621–627. doi: 10.1007/BF02235574. [DOI] [PubMed] [Google Scholar]
- 18.Regan JP, Salky BA. Laparoscopic treatment of enteric fistulas. Surg Endosc. 2004;18(2):252–254. doi: 10.1007/s00464-003-8904-4. [DOI] [PubMed] [Google Scholar]
- 19.Moorthy K, Shaul T, Foley RJ. The laparoscopic management of benign bowel fistulas. JSLS. 2004;8(4):356–358. [PMC free article] [PubMed] [Google Scholar]
- 20.Pokala N, Delaney CP, Brady KM, Senagore AJ. Elective laparoscopic surgery for benign internal enteric fistulas: a review of 43 cases. Surg Endosc. 2005;19(2):222–225. doi: 10.1007/s00464-004-8801-5. [DOI] [PubMed] [Google Scholar]
- 21.Lee SW, Yoo J, Dujovny N, Sonoda T, Milsom JW. Laparoscopic vs. hand-assisted laparoscopic sigmoidectomy for diverticulitis. Dis Colon Rectum. 2006;49(4):464–469. doi: 10.1007/s10350-006-0500-y. [DOI] [PubMed] [Google Scholar]
- 22.Pendlimari R, Touzios JG, Azodo A, Chua HK, Dozois EJ, Cima RR, et al. Short-term outcomes after elective minimally invasive colectomy for diverticulitis. Br J Surg. 2011;98(3):431–435. doi: 10.1002/bjs.7345. [DOI] [PubMed] [Google Scholar]
- 23.Eijsbouts QA, de Haan J, Berends F, Sietses C, Cuesta MA. Laparoscopic elective treatment of diverticular disease: a comparison between laparoscopic-assisted and resection-facilitated techniques. Surg Endosc. 2000;14(8):726–730. doi: 10.1007/s004640000111. [DOI] [PubMed] [Google Scholar]
- 24.Goldman SM, Fishman EK, Gatewood OM, Jones B, Brendler C, Siegelman SS. CT demonstration of colovesical fistulae secondary to diverticulitis. J Comput Assist Tomogr. 1984;8(3):462–468. doi: 10.1097/00004728-198406000-00019. [DOI] [PubMed] [Google Scholar]
- 25.Woods RJ, Lavery IC, Fazio VW, Jagelman DG, Weakley FL. Internal fistulas in diverticular disease. Dis Colon Rectum. 1988;31(8):591–596. doi: 10.1007/BF02556792. [DOI] [PubMed] [Google Scholar]
- 26.Lynn ET, Ranasinghe NE, Dallas KB, Divino CM. Management and outcomes of colovesical fistula repair. Am Surg. 2012;78(5):514–518. [PubMed] [Google Scholar]
- 27.Pollard SG, MacFarlane R, Greatorex R, Everett WG, Hartfall WG. Colovesical fistula. Ann R Coll Surg Engl. 1987;69(4):163–165. [PMC free article] [PubMed] [Google Scholar]
- 28.Garcea G, Majid I, Sutton CD, Pattenden CJ, Thomas WM. Diagnosis and management of colovesical fistulae: six-year experience of 90 consecutive cases. Colorectal Dis. 2006;8(4):347–352. doi: 10.1111/j.1463-1318.2005.00928.x. [DOI] [PubMed] [Google Scholar]
- 29.Najjar SF, Jamal MK, Savas JF, Miller TA. The spectrum of colovesical fistula and diagnostic paradigm. Am J Surg. 2004;188(5):617–621. doi: 10.1016/j.amjsurg.2004.08.016. [DOI] [PubMed] [Google Scholar]
- 30.Ravichandran S, Ahmed HU, Matanhelia SS, Dobson M. Is there a role for magnetic resonance imaging in diagnosing colovesical fistulas? Urology. 2008;72(4):832–837. doi: 10.1016/j.urology.2008.06.036. [DOI] [PubMed] [Google Scholar]
- 31.Schwenk W, Haase O, Neudecker J, Muller JM. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2006;20(3) doi: 10.1002/14651858.CD003145.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ramos JM, Beart RW, Goes R, Ortega AE, Schlinkert RT. Role of laparoscopy in colorectal surgery: a prospective evaluation of 200 cases. Dis Colon Rectum. 1995;38(5):494–501. doi: 10.1007/BF02148849. [DOI] [PubMed] [Google Scholar]
- 33.Chen HH, Wexner SD, Weiss EG, Nogueras JJ, Alabaz O, Iroatulam AJ. Laparoscopic colectomy for benign colorectal disease is associated with a significant reduction in disability as compared with laparotomy. Surg Endosc. 1998;12(12):1397–1400. doi: 10.1007/s004649900867. [DOI] [PubMed] [Google Scholar]
- 34.Phillips EH, Franklin M, Carroll BT, Fallas M, Ramos R, Rosenthal D. Laparoscopic colectomy. Ann Surg. 1992;216(6):703–707. doi: 10.1097/00000658-199212000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wexner SD, Reissman P, Pfeifer J, Bernstein M, Geron N. Laparoscopic colorectal surgery: analysis of 140 cases. Surg Endosc. 1996;10(2):133–136. doi: 10.1007/BF00188358. [DOI] [PubMed] [Google Scholar]
- 36.Senagore AJ, Duepree HJ, Delaney CP, Dissanaike S, Brady KM, Fazio VW. Cost structure of laparoscopic and open sigmoid colectomy for diverticular disease: similarities and differences. Dis Colon Rectum. 2002;45(4):485–490. doi: 10.1007/s10350-004-6225-x. [DOI] [PubMed] [Google Scholar]
- 37.Vargas HD, Ramirez RT, Hoffman GC, Hubbard GW, Gould RJ, Wohlgemuth SD, et al. Defining the role of laparoscopic-assisted sigmoid colectomy for diverticulitis. Dis Colon Rectum. 2000;43(12):1726–1731. doi: 10.1007/BF02236858. [DOI] [PubMed] [Google Scholar]
- 38.Schwandner O, Schiedeck TH, Bruch HP. The role of conversion in laparoscopic surgery—do predictive factors exist? Surg Endosc. 1999;13(2):151–156. doi: 10.1007/s004649900927. [DOI] [PubMed] [Google Scholar]
- 39.Slim K, Pezet D, Riff Y, Clark E, Chipponi J. High morbidity rate after converted laparoscopic colorectal surgery. Br J Surg. 1995;82(10):1406–1408. doi: 10.1002/bjs.1800821036. [DOI] [PubMed] [Google Scholar]
- 40.Marusch F, Gastinger I, Schneider C, Scheidbach H, Konradt J, Bruch HP, et al. Importance of conversion for results obtained with laparoscopic colorectal surgery. Dis Colon Rectum. 2001;44(2):207–214. doi: 10.1007/BF02234294. [DOI] [PubMed] [Google Scholar]
- 41.Kohler L, Rixen D, Troidl H. Laparoscopic colorectal resection for diverticulitis. Int J Colorectal Dis. 1998;13(1):43–47. doi: 10.1007/s003840050130. [DOI] [PubMed] [Google Scholar]
- 42.Kockerling F, Schneider C, Reymond MA, Scheidbach H, Scheuerlein H, Konradt J, et al. Laparoscopic resection of sigmoid diverticulitis: results of a multicenter study. Surg Endosc. 1999;13(6):567–571. doi: 10.1007/s004649901042. [DOI] [PubMed] [Google Scholar]
- 43.Franklin ME, Dorman JP, Jacobs M, Plasencia G. Is laparoscopic surgery applicable to complicated colonic diverticular disease? Surg Endosc. 1997;11(10):1021–1025. doi: 10.1007/s004649900516. [DOI] [PubMed] [Google Scholar]
- 44.Bruce CJ, Coller JA, Murray JJ, Schoetz DJ, Roberts PL, Rusin LC. Laparoscopic resection for diverticular disease. Dis Colon Rectum. 1996;39(10):S1–S6. doi: 10.1007/BF02053798. [DOI] [PubMed] [Google Scholar]
- 45.Klarenbeek BR, Veenhof AA, Bergamaschi R, van der Peet DL, van den Broek WT, de Lange ES, et al. Laparoscopic sigmoid resection for diverticulitis decreases major morbidity rates: a randomized control trial: short-term results of the Sigma trial. Ann Surg. 2009;249(1):39–44. doi: 10.1097/SLA.0b013e31818e416a. [DOI] [PubMed] [Google Scholar]
- 46.Klarenbeek BR, Bergamaschi R, Veenhof AA, van der Peet DL, van den Broek WT, de Lange ES, et al. Laparoscopic versus open sigmoid resection for diverticular disease: follow-up assessment of the randomized control Sigma trial. Surg Endosc. 2011;25(4):1121–1126. doi: 10.1007/s00464-010-1327-0. [DOI] [PubMed] [Google Scholar]
- 47.Sher ME, Agachan F, Bortul M, Nogueras JJ, Weiss EG, Wexner SD. Laparoscopic surgery for diverticulitis. Surg Endosc. 1997;11(3):264–267. doi: 10.1007/s004649900340. [DOI] [PubMed] [Google Scholar]
- 48.Garrett KA, Champagne BJ, Valerian BT, Peterson D, Lee EC. A single training center's experience with 200 consecutive cases of diverticulitis: can all patients be approached laparoscopically? Surg Endosc. 2008;22(11):2503–2508. doi: 10.1007/s00464-008-9818-y. [DOI] [PubMed] [Google Scholar]
- 49.Reissfelder C, Buhr HJ, Ritz JP. Can laparoscopically assisted sigmoid resection provide uncomplicated management even in cases of complicated diverticulitis? Surg Endosc. 2006;20(7):1055–1059. doi: 10.1007/s00464-005-0529-3. [DOI] [PubMed] [Google Scholar]
- 50.Martel G, Bouchard A, Soto CM, Poulin EC, Mamazza J, Boushey RP. Laparoscopic colectomy for complex diverticular disease: a justifiable choice? Surg Endosc. 2010;24(9):2273–2280. doi: 10.1007/s00464-010-0951-z. [DOI] [PubMed] [Google Scholar]
- 51.Stevenson AR, Stitz RW, Lumley JW, Fielding GA. Laparoscopic assisted anterior resection for diverticular disease: follow-up of 100 consecutive patients. Ann Surg. 1998;227(3):335–342. doi: 10.1097/00000658-199803000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hassan I, Cima RR, Larson DW, Dozois EJ, Byrne MM, Larson DR, et al. The impact of uncomplicated and complicated diverticulitis on laparoscopic surgery conversion rates and patient outcomes. Surg Endosc. 2007;21(10):1690–1694. doi: 10.1007/s00464-007-9413-7. [DOI] [PubMed] [Google Scholar]
- 53.Berthou JC, Charbonneau P. Elective laparoscopic management of sigmoid diverticulitis: results in a series of 110 patients. Surg Endosc. 1999;13(5):457–460. doi: 10.1007/s004649901012. [DOI] [PubMed] [Google Scholar]
- 54.Scheidbach H, Schneider C, Rose J, Konradt J, Gross E, Barlehner E, et al. Laparoscopic approach to treatment of sigmoid diverticulitis: changes in the spectrum of indications and results of a prospective, multicenter study on 1,545 patients. Dis Colon Rectum. 2004;47(11):1883–1888. doi: 10.1007/s10350-004-0715-8. [DOI] [PubMed] [Google Scholar]
- 55.Schwandner O, Farke S, Fischer F, Eckmann C, Schiedeck TH, Bruch HP. Laparoscopic colectomy for recurrent and complicated diverticulitis: a prospective study of 396 patients. Langenbecks Arch Surg. 2004;389(2):97–103. doi: 10.1007/s00423-003-0454-7. [DOI] [PubMed] [Google Scholar]
- 56.Trebuchet G, Lechaux D, Lecalve JL. Laparoscopic left colon resection for diverticular disease: results from 170 consecutive cases. Surg Endosc. 2002;16(1):18–21. doi: 10.1007/s004640090122. [DOI] [PubMed] [Google Scholar]
- 57.Pugliese R, Di Lernia S, Sansonna F, Scandroglio I, Maggioni D, Ferrari C, et al. Laparoscopic treatment of sigmoid diverticulitis: a retrospective review of 103 cases. Surg Endosc. 2004;18(9):1344–1348. doi: 10.1007/s00464-003-9178-6. [DOI] [PubMed] [Google Scholar]
- 58.Liberman MA, Phillips EH, Carroll BJ, Fallas M, Rosenthal R. Laparoscopic colectomy vs traditional colectomy for diverticulitis: outcome and costs. Surg Endosc. 1996;10(1):15–18. doi: 10.1007/s004649910002. [DOI] [PubMed] [Google Scholar]
- 59.Solkar MH, Forshaw MJ, Sankararajah D, Stewart M, Parker MC. Colovesical fistula—is a surgical approach always justified? Colorectal Dis. 2005;7(5):467–471. doi: 10.1111/j.1463-1318.2005.00863.x. [DOI] [PubMed] [Google Scholar]
- 60.Amin M, Nallinger R, Polk HC. Conservative treatment of selected patients with colovesical fistula due to diverticulitis. Surg Gynecol Obstet. 1984;159(5):442–444. [PubMed] [Google Scholar]
- 61.Scozzari G, Arezzo A, Morino M. Enterovesical fistulas: diagnosis and management. Tech Coloproctol. 2010;14(4):293–300. doi: 10.1007/s10151-010-0602-3. [DOI] [PubMed] [Google Scholar]
- 62.Walker KG, Anderson JH, Iskander N, McKee RF, Finlay IG. Colonic resection for colovesical fistula: 5-year follow-up. Colorectal Dis. 2002;4(4):270–274. doi: 10.1046/j.1463-1318.2002.00353.x. [DOI] [PubMed] [Google Scholar]
- 63.Frizelle FA, Dominguez JM, Santoro GA. Management of post-operative recurrent diverticulitis: a review of the literature. J R Coll Edinb. 1997;42(3):186–188. [PubMed] [Google Scholar]
- 64.Thaler K, Baig MK, Berho M, Weiss EG, Nogueras JJ, Arnaud JP, et al. Determinants of recurrence after sigmoid resection for uncomplicated diverticulitis. Dis Colon Rectum. 2003;46(3):385–388. doi: 10.1007/s10350-004-6560-y. [DOI] [PubMed] [Google Scholar]
- 65.Mileski WJ, Joehl RJ, Rege RV, Nahrwold DL. One-stage resection and anastomosis in the management of colovesical fistula. Am J Surg. 1987;153(1):75–79. doi: 10.1016/0002-9610(87)90204-2. [DOI] [PubMed] [Google Scholar]
- 66.Rao PN, Knox R, Barnard RJ, Schofield PF. Management of colovesical fistula. Br J Surg. 1987;74(4):362–363. doi: 10.1002/bjs.1800740511. [DOI] [PubMed] [Google Scholar]
- 67.Steele M, Deveney C, Burchell M. Diagnosis and management of colovesical fistulas. Dis Colon Rectum. 1978;22(1):27–30. doi: 10.1007/BF02586752. [DOI] [PubMed] [Google Scholar]
- 68.Schlachta CM, Mamazza J, Seshadri PA, Cadeddu MO, Poulin EC. Predicting conversion to open surgery in laparoscopic colorectal resections: a simple clinical model. Surg Endosc. 2000;14(12):1114–1117. doi: 10.1007/s004640000309. [DOI] [PubMed] [Google Scholar]
- 69.Siriser F. Laparoscopic-assisted colectomy for diverticular sigmoiditis: a single-surgeon prospective study of 65 patients. Surg Endosc. 1999;13(8):811–813. doi: 10.1007/s004649901106. [DOI] [PubMed] [Google Scholar]
- 70.Zapletal C, Woeste G, Bechstein WO, Wullstein C. Laparoscopic sigmoid resections for diverticulitis complicated by abscesses or fistulas. Int J Colorectal Dis. 2007;22(12):1515–1521. doi: 10.1007/s00384-007-0359-y. [DOI] [PubMed] [Google Scholar]
- 71.Marusch F, Gastinger I, Schneider C, Scheidbach H, Konradt J, Bruch HP, et al. Experience as a factor influencing the indications for laparoscopic colorectal surgery and the results. Surg Endosc. 2001;15(2):116–120. doi: 10.1007/s004640000340. [DOI] [PubMed] [Google Scholar]


