Abstract
The objective of this study was to evaluate the feasibility and efficacy of hybrid therapy (combined endarterectomy-endovascular) in patients with complex peripheral multifocal steno-obstructive vascular disease involving the femoral artery bifurcation. Forty-one combined procedures were performed on 40 patients. Although the common femoral artery was usually treated with endarterectomy, endoluminal procedures were performed proximally in 12 patients (group 1), distally in 18 patients (group 2), and both upward and downward in 11 patients (group 3). Patients underwent clinical assessment and ankle-brachial index measurement thereafter. Primary, assisted-primary, and secondary patency rates at 24 months were 59%, 66%, and 72%, respectively. Primary patency rates were lower in group 3 compared with groups 1 and 2 (P = 0.015). The limb salvage rate was 86.4% at the end of the follow-up period. Hybrid procedures provide feasible and effective treatment management of selected patients with multilevel lower extremity arterial disease involving the femoral artery bifurcation.
Keywords: Endarterectomy, Interventional radiography, Arteriosclerosis obliterans, Femoral artery
The indications for the endovascular treatment of peripheral arterial disease have rapidly increased since the introduction of percutaneous transluminal angioplasty (PTA) and stenting.1,2 The advantages of the endovascular approach include lower periprocedural morbidity and mortality. Short-term data from Bypass versus Angioplasty trials in Severe Ischemia of the Leg (BASIL)3 have confirmed this, with similar clinical outcome for the surgical and endovascular approach. Considerable progress has also been made in the endovascular treatment of infrapopliteal arterial occlusion. One study has demonstrated that infrapopliteal angioplasty is a reasonable primary treatment for critical limb ischemia patients with TransAtlantic InterSociety Consensus (TASC) A, B, or C lesions.4
Due to the multilevel nature of peripheral arterial disease, iliac or femoral lesions accompanied by the femoral artery bifurcation (FB) disease are frequently observed.5,6 Endovascular surgery is poorly suited to treating lesions in the FB because they are bulky and eccentric. In addition, the location of the lesions makes ipsilateral access difficult and stent placement impossible. As with the common femoral artery, the deep femoral artery is not generally favorable for endovascular surgery because it usually has either an orifice lesion involving the FB or a diffuse lesion along the length of the artery, which is often into its secondary and tertiary branches.
Simultaneous hybrid endovascular and open lower extremity arterial reconstructive procedures have the advantage of eliminating the need for major surgery and avoiding separate staged interventions and their associated morbidity. Recently, several investigators have published results on several types of combined treatments for various patterns of iliac, femoral, and infrapopliteal diseases with promising outcomes.7–14 Most reports discussed hybrid bypass surgery and endovascular surgery.7–11,13 Although few reported femoral artery endarterectomy combined with iliac artery endovascular therapy,12,14 which did not include the infrainguinal lesions. To our knowledge, the efficacy of hybrid femoral artery endarterectomy and supra and/or infrainguinal artery endovascular treatment has not been discussed separately. The purpose of this study was to evaluate the immediate and mid-term clinical results on patients with iliac or femoral lesions involving the FB who underwent hybrid femoral artery endarterectomy and lower limb artery PTA and/or stenting.
Materials and Methods
Study design
A retrospective study was used and included all patients at our hospital from September 2007 to December 2009 who had obstructive arterial disease in the FB (including the common femoral, femoris profunda, or the origin of the superficial femoral artery), and at least one level among the iliac, femoropopliteal (including the superficial femoral and the supragenicular part of the popliteal artery), and infragenicular were treated with a combination of FB endarterectomy and lower limb artery PTA and/or stenting. These procedures were performed on the same occasion for each patient at a single center. The Institutional Review Board of our hospital approved the clinical protocol, and the patients were given information regarding results, possible complications, and other modalities of treatment.
Patients and data collection
Patient selection was based on the presence of symptomatic lower extremity peripheral arterial disease, as defined by Rutherford et al15 in the “recommended standards for reports dealing with lower extremity ischemia.” Patients who presented emergently with acute lower limb ischemia in the presence of peripheral arterial disease were also included in the study.
Preoperative, intraoperative, and follow-up information was available for all patients, and it was prospectively collected and retrospectively reviewed using hospital charts, operative and outpatient records, and telephone communication.
Individual limbs were counted separately, therefore patients undergoing staged, bilateral procedures were recorded and evaluated as two entries. Demographic and risk factors for arteriosclerosis were collected for each patient. Comorbidities of long-term tobacco use, diabetes, and hypertension; clinical presentation (intermittent claudication or critical limb ischemia); lesion anatomy according to TASC II classification; and perioperative data and follow-up for each limb were collected. All patients underwent preoperative peripheral vascular evaluation with physical examination, ankle brachial index (ABI), computed tomographic angiography with three-dimensional reconstruction to assess images for preoperative planning.
Rutherford classification, as specified by the Society for Vascular Surgery/American Association for Vascular Surgery reporting standards, was used to determine clinical category at the time of presentation.15
Revascularization procedures
The same team of vascular surgeons selected the patients who were deemed suitable for hybrid lower limb arterial reconstruction carried out all the procedures. Most patients (35/40; 88%) underwent the procedure in an endovascular operating room with a moveable radiolucent surgical table and a mobile digital angiographic system using a C-arm (Philips BV Endura, Philips Medical Systems, release 2.2.3, Eindhoven, the Netherlands); the remainder (5/40; 12%) of the cases were performed in a cardiac catheterization laboratory (GE Innova 3100, GE healthcare, Waukesha, Wisconsin, USA).
The patients included in the study were divided into three groups according to the type of revascularization procedure: group 1 included patients who underwent endovascular reconstruction proximal to the site of the FB endarterectomy; group 2 included patients who underwent endovascular reconstruction distal to the site of the FB endarterectomy; and group 3 included patients who underwent open arterial endarterectomy with both proximal and distal endovascular procedures.
Iliac, femoropopliteal, and infrapopliteal lesions were defined according to TASC II.1 In the iliac and femoropopliteal area, TASC A, TASC B, and TASC C lesions were treated with angioplasty, with stenting being reserved for when the angiographic result was inadequate, such as dissection or elastic wall recoil. TASC D lesions received bypass therapy and were excluded from the study. In the infrapopliteal area, lesions were treated with angioplasty alone.
Most procedures were performed under local anesthesia; however, general anesthesia was occasionally used for patients unable to adequately lie still. Epidural anesthesia is preferred versus general anesthesia because of the increased risk of pneumonia in patients with chronic obstructive pulmonary disease. However, perioperative anticoagulant and antiplatelet therapy can lead to serious complications of epidural hemorrhage. It is our preference to perform hybrid operations under local anesthesia or intravenous sedation. All patients received 100 mg of aspirin and 75 mg of clopidogrel before the procedure. The inguinal region was prepped and draped sterilely. Typically, the ipsilateral FB was exposed through a longitudinal inguinal incision. The open arterial endarterectomy with or without patch preceded upward or downward endovascular revascularization in all patients. Placement of the artery sheath is accomplished either through the common femoral artery above the anastomosis or through direct puncture of the prosthetic material (patch). This technique allows for continuous blood flow during the endovascular portion of the procedure. We initially used an 11-cm 7F sheath because it accommodates nearly all types of balloons and stents. Long occlusions are typically crossed with a 0.035-in angled guide wire to avoid subintimal dissection if possible. Tibial lesions are then preferentially crossed with a 0.014- or 0.018-in wire, over which a long, noncompliant low profile angioplasty balloon sized to match the healthy portion of the artery is advanced, and prolonged inflation during 2 to 3 minutes is performed. Stents were selectively used in patients with PTA residual stenosis (>30%) or flow-limiting dissection. Groin exposure is then closed in the standard fashion.
All patients were anticoagulated with heparin during the procedure. After the procedure, patients were continued on aspirin and given clopidogrel for a minimum of 30 days.
Definitions and end points
Technical success was defined as a residual stenosis less than 30% without complications such as distal embolism or in situ thrombosis. All perioperative events including bleeding, myocardial infarction, stroke, or death were recorded. Primary failures were defined as residual stenosis more than 30% using angiographic measurement and included lesions that were unable to be dilated or crossed. Hemodynamic success was defined by an increase in the ABI ≥0.10, according to the reporting standards.1 Categorical improvement (clinic success) was defined as an improvement of at least one clinical category, except when actual tissue loss existed, in which case it should be moved up at least two categories. Complications and death occurring within 30 days of the procedure were considered to be procedure-related morbidity and mortality.
Follow-up
All patients took part in a postoperative surveillance program, which consisted of clinical examination and ABI measurement at 1, 3, and, 6 months and at 6-month intervals thereafter. Ultrasound evaluation was performed every year. Patients with worsening clinical symptoms, physical examinations, and/or noninvasive studies were further assessed with computed-assisted arteriography.
Statistical analysis
All analyses were performed on a per-limb basis. The preoperative characteristics and outcomes were reported as percentages of the sample. Patency and limb salvage analyses were performed using the Kaplan-Meier life table method. The differences in patency rates were determined using the log-rank test. The χ2 test was used to evaluate the differences between the groups of patients for categorical variables (χ2 for independent groups, two-tailed P value). The differences in the ABI were analyzed using the paired Student t test. Statistical significance was assumed for P < 0.05. Statistical analysis was performed with a computer-based statistical software package (SPSS 17 for Windows, SPSS Inc, Chicago, IL).
Results
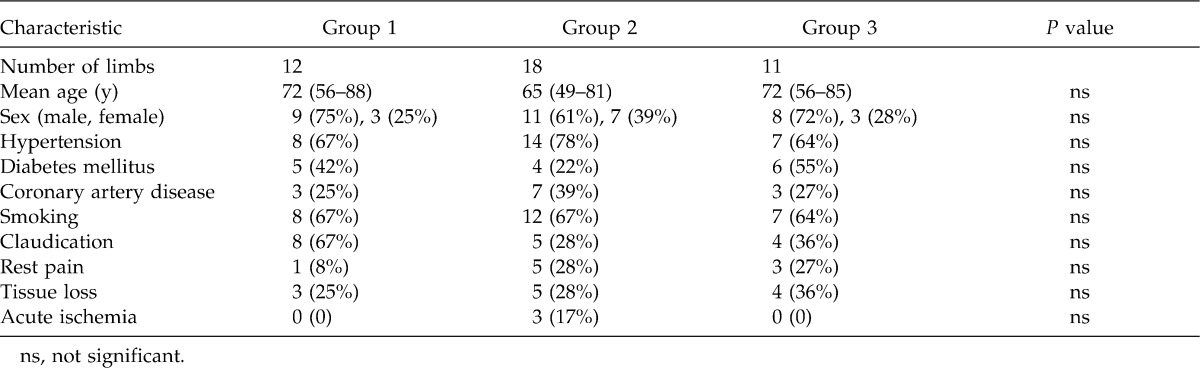
From September 2007 to December 2009, 40 consecutive patients underwent combined endarterectomy of the FB and proximal and/or distal endovascular procedures on 41 limbs. One patient underwent a bilateral lower extremity arterial treatment. Demographic and clinical features of the study groups are shown in Table 1. The average age of the patients was 69.2 years (range, 49–88 years); 67.5% (27/40) of the patients were men. Comorbidity was frequent and included diabetes (14/40; 35%), hypertension (29/40; 72.5%), current smokers (27/40; 67.5%), and coronary artery disease (13/40; 32.5%).
Table 1.
Patient characteristics
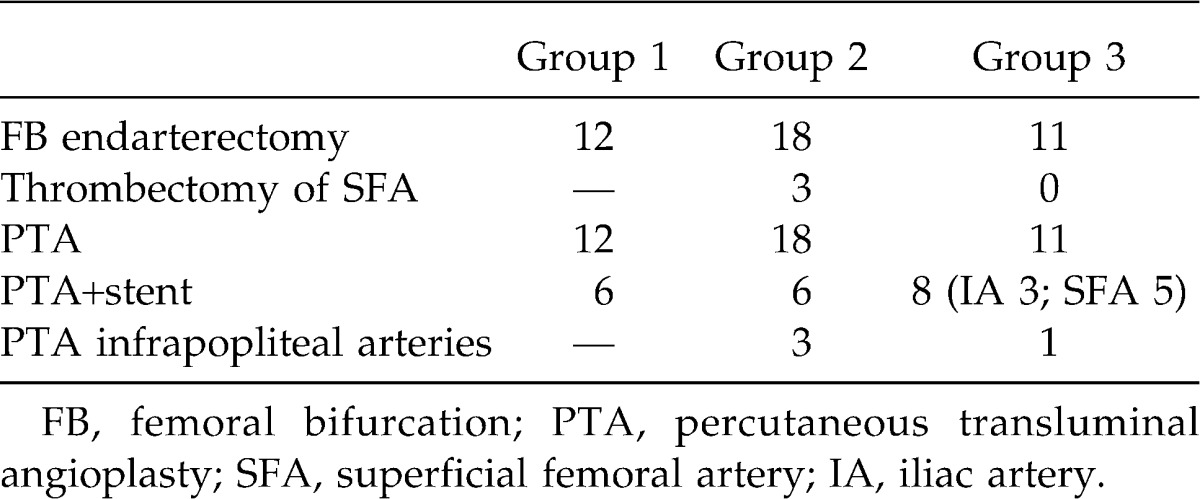
The frequency of the open and endovascular procedures performed in the three groups are presented in Table 2. The most common open procedure was endarterectomy of the FB with and without patch arterioplasty (17/41; 41.6%). Thrombectomy was performed in three cases of acute ischemia in the group 2 patients. Endovascular procedures included angioplasty and/or stenting in the arterial axes upward and/or downward at the site of endarterectomy, in which the iliac artery stenting occurred in 14 patients, and superficial femoral artery stent placement occurred in 11 patients. Angioplasty of the infrapopliteal arteries was performed in four limbs.
Table 2.
Types of open and endovascular procedures
According to the Rutherford grading, 17 limbs (17/41; 42%) were treated for severe intermittent claudication (Rutherford category 3), 9 limbs (9/41; 22%) had persistent rest pain (Rutherford category 4), and 12 limbs (12/41; 29%) had minor tissue loss (Rutherford category 5). In another three limbs (3/41; 7%), the indication for arterial reconstruction was acute ischemia in the presence of underlying peripheral arterial disease. No patient had moderate, intermittent claudication (Rutherford category 2) or major tissue loss/gangrene (Rutherford category 6).
There were no statistically significant differences in the demographic characteristics and clinical presentations among the groups of patients (Table 1).
Procedural details
All patients who underwent endarterectomy were preceded by upward or downward endovascular revascularization. The types of endovascular procedures are presented in Table 2. Group 1 comprised 12 limbs, group 2 comprised 18 limbs, and group 3 included 11 limbs (Tables 1 and 2). Endovascular procedures included angioplasty and stenting. Thrombectomy was performed in three cases of acute ischemia in the presence of previous lower limb arterial occlusive disease. These patients were part of group 2. One patient had superficial femoral artery stent placement. The majority (29/41; 71%) of these hybrid procedures were performed under local anesthesia; the remaining procedures (12/41; 29%) were done under general anesthesia. In 20 limbs (of 41; 48.8%), stent use was necessary, all of which were self-expandable S.M.A.R.T. CONTROL (Cordis Corporation, Hialeah, Florida, USA) or LUMINEXX (Bard, Murray Hill, New Jersey, USA). The average length of lesions treated was 255 mm (range, 58–550 mm). According to the length of treated lesions, patients were divided into two groups: long segment group (>255 mm) and short segment group (<255 mm).
Technical and hemodynamic success
Technical success was obtained in 40 of 41 limbs (98%). There was treatment failure in 1 patient belonging to group 3 due to the guide wire being unable to pass through the occluded segment in the superficial femoral artery. Hemodynamic success was achieved in 38 of 41 limbs (92.7%). The mean ABI increased significantly from 0.38 ± 0.16 preoperatively to 0.67 ± 0.14 after revascularization (P < 0.001). The mean ABI increase was 0.29.
Complications
Perioperative complications occurred in 10/41 procedures, yielding a complication rate of 24.4%: vessel perforation (n = 1) thrombosis (n = 2), surgical wound infection (n = 5), cardiac failure (n = 1) and renal failure (n = 1). One case of acute arterial ischemia resulted in compartment syndrome after revascularization and required surgical decompression. One infrapopliteal arterial was ruptured in the PTA and healed after surgical repair. Cardiac complications (cardiac failure) affected 1 patient (1/40; 2.5%) and acute renal failure occurred in 1 patient (1/40; 2.5%). The cause of renal failure was assumed to be contrast-induced. These complications were successfully managed with appropriate treatment, except for the patient who died from cardiac failure on the fourth postoperative day, resulting in a 2.5% perioperative mortality rate. Two amputations were performed in the immediate postoperative period. The amputations were performed on the 7th and 10th postoperative days because of acutely ischemic limbs caused by thrombosis; attempts at revascularization were unsuccessful. The 30-day postoperative mortality and major amputation rates were 2.5% (1/40) and 5% (2/40), respectively.
Follow-up
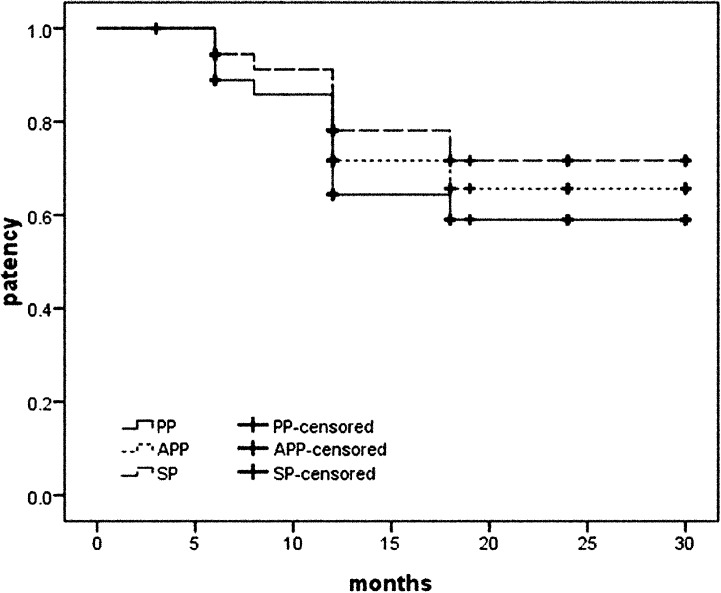
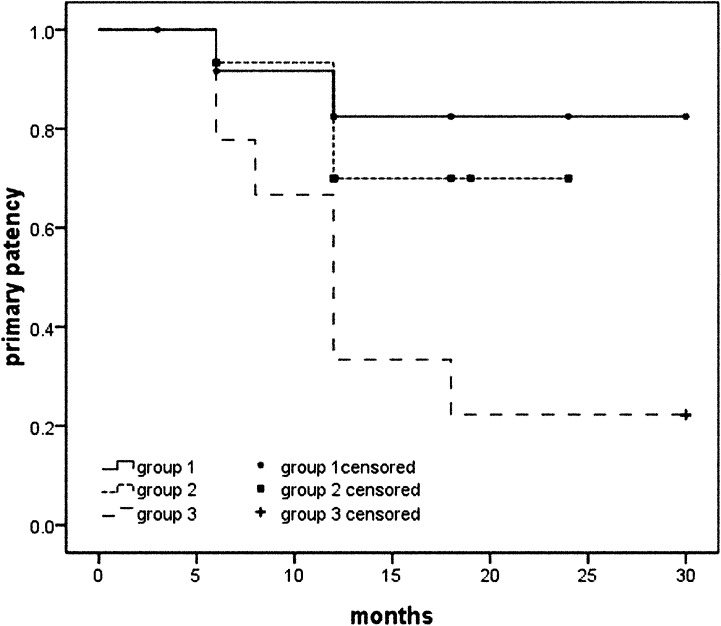
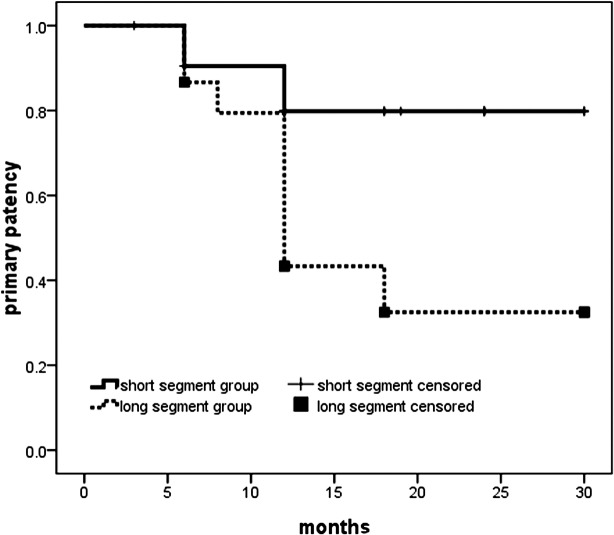
The median follow-up for patients undergoing a combination procedure was 12 months (range, 6–30 months). If patients who died perioperatively, had amputation, and 1 patient who had a technical failure due to the guide wire being unable to pass through the occluded segment were excluded, clinic success was achieved in 28 patients (of 36; 77.8%). The primary, assisted-primary, and secondary patency rates at 12 months were 64%, 72%, and 78%, respectively, and at 24 months were 59%, 66%, and 72%, respectively (Fig. 1). The primary patency rates were lower in group 3 compared with group 1 and 2 patients (Kaplan-Meier analysis, log-rank test, P = 0.015) (Fig. 2). The primary patency rates in long segment group were lower than in the short segment group (Kaplan-Meier analysis, log-rank test, P = 0.018) (Fig. 3). No patient who underwent endarterectomy of the FB and patch arterioplasty failed to retain patency in that segment during the follow-up period. An overall amputation rate of 14.6% (6 limbs) was recorded at the end of the follow-up period.
Figure 1.
Overall primary, assisted primary, and secondary patency (Kaplan-Meier analysis). PP, primary patency; APP, assisted patency; SP, secondary patency.
Figure 2.
Primary patency rates in groups 1, 2, and 3 (Kaplan-Meier analysis). Primary patency rates were lower in group 3 than those in groups 1 and 2 (log-rank test, P = 0.015).
Figure 3.
Primary patency rates in long segment group (total treated length, >255 mm) and short segment group (total treated length, <255 mm) (Kaplan-Meier analysis). The primary patency rates in the long segment group were lower than the rates in the short segment group (Kaplan-Meier analysis, log-rank test, P = 0.018).
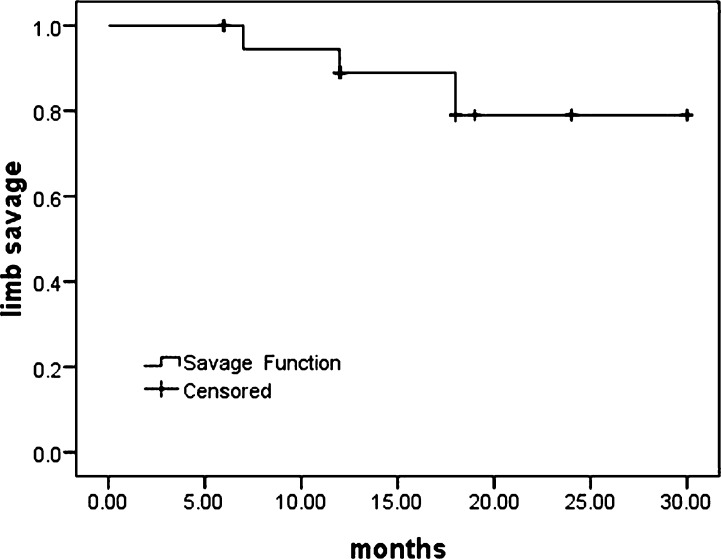
Twenty-four limbs with rest pain, tissue loss, and acute ischemia were evaluated for limb salvage, and there was a limb salvage rate of 79.1% at the end of the follow-up period. If patients who had technical failure because of postoperative acute thrombosis were excluded, 22 limbs were evaluated for limb salvage; the limb salvage rate was 86.4% (Fig. 4). Beyond the perioperative period and until the end of follow-up, 3 patients died: 2 of coronary artery disease, 1 of stroke.
Figure 4.
Cumulative limb salvage after hybrid lower extremity arterial reconstruction (Kaplan-Meier analysis). Twenty-two limbs were evaluated for limb salvage, and the limb salvage rate was 86.4% at the end of the follow-up period.
Discussion
Peripheral occlusive artery disease is estimated to be present in 1.4% to 1.9% of people 40 to 49 years of age, in 6.9% of people 50 to 59 years of age, and in 20% of people 70 years of age, as documented by noninvasive testing.16,17 Until recently, the treatment of these patients was primarily peripheral arterial bypass surgery, such as femoral-popliteal bypass. However, rapid advances in endovascular surgery have significantly changed the patterns of vascular reconstruction. Recent studies on stenting for iliac artery stenosis and occlusion show 3-year primary patency rates of 69% to 92% and 64% to 90%, respectively18–22, whereas the 2-year primary patency rate of stenting for superficial femoral artery stenosis or occlusion is reported to be 60% to 69%.23–26 However, endovascular surgery has less favorable outcomes for some lower extremity arteries, such as the common femoral and deep femoral arteries.27–30 On the other hand, open endarterectomy of the common femoral artery is simple, has low morbidity and high patency rate, and can be combined with any other endovascular technique. In the 1960–1980s, many reports were proving that endarterectomy at the level of the FB is an efficient procedure with a durable outcome.31 Recently, Kang et al32 published a study reporting a 91% primary patency rate at 5 years after endarterectomy of the common femoral artery.
There have been several reports suggesting the efficacy of hybrid surgical and endovascular therapy, such as aortoiliac or superficial femoral artery stenting, as an adjunct to common femoral artery endarterectomy for multifocal peripheral artery disease.33 Nelson et al12 reported early results of external iliac artery stenting combined with common femoral artery endarterectomy, and demonstrated technical and hemodynamic success rates of 100%, as well as acceptable 1-year primary patency and primary-assisted patency rates of 84% and 97%, respectively. Recently the same center reported the largest study to date describing the outcome and long-term patency of this procedure. A total of 171 patients underwent 193 common femoral artery endarterectomies and iliac stent/stent grafting. Stent grafts were used in 41% of patients. Technical success occurred in 98% of patients. Clinical improvement was seen in 92% of patients. The mean ABI increased from 0.38 ± 0.32 to 0.72 ± 0.24. The 30-day mortality rate was 2.3% and the 5-year survival was 60%. Five-year primary, primary-assisted, and secondary patencies were 60%, 97%, and 98%, respectively.14 However, the study did not include infrainguinal lesions. Cotroneo et al13 reported the 2-year results of a study on hybrid surgical and endovascular therapy, including a few cases that involved endovascular procedure combined with common femoral artery endarterectomy, and demonstrated a technical success rate of 100%, as well as acceptable 2-year primary patency and primary-assisted patency rates of 79% and 86%, respectively. Antoniou et al7 reported complete data obtained from 60 patients who underwent 61 single-step hybrid procedures. Technical and hemodynamic success rates were 100% and 95%, respectively. The perioperative mortality rate was 3%. The primary and assisted-primary patency rates at 12 months were 71% and 98%, respectively. Primary patency rates were lower in the group that included patients who underwent open surgery with both proximal and distal endoluminal procedures. These two studies discussed the hybrid treatment of multifocal steno-obstructive vascular disease in which surgical treatment in addition to FB endarterectomy also included vascular bypass. In the present study, we reported on the immediate and mid-term clinical results of hybrid endarterectomy and iliac or infrainguinal endovascular treatment. Unlike the reports by Antoniou7 and Cotroneo13 and their colleagues, in addition to thrombectomy performed in 3 patients with acute ischemia, the unique surgery method used in the present study was femoral artery endarterectomy. Our study population comprised 40 patients with significant comorbid risk factors. In addition, more than half of the patients (61%) were operated on for limb salvage, presenting with rest pain, tissue loss, or an acutely ischemic leg at risk for limb loss. These patients were carefully selected for simultaneous combined open and endovascular interventions, taking into account the operative risk, potential for clinical improvement, and patterns of segmental arterial disease. Surgical procedures were as reported in the literature.7,13,14,33 Most of the procedures (71%) occurred under local anesthesia, and the remaining under general anesthesia. Because of concern of perioperative bleeding complications caused by the use of anticoagulant drugs it is recommended that the use of epidural or spinal anesthesia be avoided. Several combinations of open and endovascular procedures were used, which were categorized into 3 types for practical and grouping purposes. In particular, group 3 comprised patients who received hybrid revascularization of the whole lower extremity arterial axis, from the iliac up to the infrapopliteal level. In our study, we achieved technical and hemodynamic success rates of 98% and 93%, respectively. Perioperative complications occurred in 10 of 41 procedures, yielding a complication rate of 24.4%. These complications were successfully managed with appropriate treatment, except for the patients who died from cardiac failure, resulting in a 2.5% perioperative mortality rate. Two amputations were performed in the immediate postoperative period. Similar results were obtained as those reported in the literature.7,13,14,33 The primary, assisted-primary, and secondary patency rates at 12 months were 64%, 72%, and 78%, and at 24 months the rates were 59%, 66%, and 72%, respectively. Patency rates were worse than those reported in the literature.7,13,14,33 This may be attributable to the higher proportion (26%) of cases that involved open surgery with both proximal and distal endovascular procedures, whereas the rate of open surgery reported by Cotroneo et al13 and Antoniou et al7 were 6.8% and 14.8%, respectively. Our group reflects more widespread and severe atherosclerotic disease, which would be associated with poor outcome. The extensive intervention was performed at multiple segments, which increases the likelihood of failure of primary patency. Primary patency rates were lower in this group.7,13 Similar with the reported literature, the primary patency rates of group 3 patients were significant lower than in groups 1 and 2 (P = 0.015) in our study.
Limitations to our study include the small number of patients involved and the fact that it was a retrospective review of our routine experiences, without control or comparison group data, including patients with an extensive mix of clinical presentations, pre-existing vascular procedures, and therapies performed. In addition, the follow-up period was relatively short.
In conclusion, hybrid surgical and endovascular therapy, such as aortoiliac and/or superficial femoral artery stenting as an adjunct to common femoral artery endarterectomy, can provide a less invasive yet effective and durable option, at least in the mid-term, for patients with multifocal peripheral artery disease. Our data suggest that the immediate results, expressed as technical and hemodynamic success and mid-term outcomes, represented by the patency and limb salvage rates, are satisfactory. More extensive diseases were found to be associated with a worse outcome. Hybrid procedures for the treatment of severe lower extremity arterial disease may provide less invasive therapeutic options tailored to the needs of high risk patients.
Acknowledgments
Junjie Zou and Yongxiang Xia contributed equally to this work.
References
- 1.Norgren L, Hiatt W.R, Dormandy J.A, Nehler M.R, Harris K.A, Fowkes F.G. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg. 2007;45(suppl):S5–S67. doi: 10.1016/j.jvs.2006.12.037. [DOI] [PubMed] [Google Scholar]
- 2.Dormandy J, Rutherford R. Management of peripheral arterial disease (PAD). TASC Working Group. TransAtlantic Inter-Society Consensus (TASC). J Vasc Surg. 2000;31(suppl):S1–S296. [PubMed] [Google Scholar]
- 3.Adam D.J, Beard J.D, Cleveland T, Bell J, Bradbury A.W, Forbes J.F, et al. Bypass versus angioplasty in severe ischemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet. 2005;366(9501):1925–1934. doi: 10.1016/S0140-6736(05)67704-5. [DOI] [PubMed] [Google Scholar]
- 4.Giles K.A, Pomposelli F.B, Spence T.L, Hamdan A.D, Blattman S.B, Panossian H, et al. Infrapopliteal angioplasty for critical limb ischemia: relation of TransAtlantic InterSociety Consensus class to outcome in 176 limbs. J Vasc Surg. 2008;48(1):128–136. doi: 10.1016/j.jvs.2008.02.027. [DOI] [PubMed] [Google Scholar]
- 5.Mavor G.E. The patterns of occlusion in atheroma of lower limb arteries: the correlation of clinical and arteriographic findings. Br J Surg. 1964;5:352–364. doi: 10.1002/bjs.18004318003. [DOI] [PubMed] [Google Scholar]
- 6.Haimovici H. Patterns of atherosclerotic lesions of the lower extremity. Arch Surg. 1967;95(180):918–933. doi: 10.1001/archsurg.1967.01330180066012. [DOI] [PubMed] [Google Scholar]
- 7.Antoniou G.A, Sfyroeras G.S, Karathanos C, Achouhan H, Koutsias S, Vretzakis G, et al. Hybrid endovascular and open treatment of severe multilevel lower extremity arterial disease. Eur J Vasc Endovasc Surg. 2009;38(5):616–622. doi: 10.1016/j.ejvs.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 8.Griffith C.D, Harrison J.D, Gregson R.H, Makin G.S, Hopkinson B.R. Transluminal iliac angioplasty with distal bypass surgery in patients with critical limb ischaemia. J R Coll Surg Edinb. 1989;34(5):253–255. [PubMed] [Google Scholar]
- 9.Wilson S.E, White G.H, Wolf G, Cross A.P. Proximal percutaneous balloon angioplasty and distal bypass for multilevel arterial occlusion. Veterans Administration Cooperative Study no. 1990. Ann Vasc Surg. 1990;4(4):351–355. doi: 10.1007/BF02000498. [DOI] [PubMed] [Google Scholar]
- 10.Schneider P.A, Caps M.T, Ogawa D.Y, Hayman E.S. Intraoperative superficial femoral artery balloon angioplasty and popliteal to distal bypass graft: an option for combined open and endovascular treatment of diabetic gangrene. J Vasc Surg. 2001;33(5):955–962. doi: 10.1067/mva.2001.114210. [DOI] [PubMed] [Google Scholar]
- 11.Lantis J, Jensen M, Benvenisty A, Mendes D, Gendics C, Todd G. Outcomes of combined superficial femoral endovascular revascularization and popliteal to distal bypass for patients with tissue loss. Ann Vasc Surg. 2008;22(3):366–371. doi: 10.1016/j.avsg.2007.09.016. [DOI] [PubMed] [Google Scholar]
- 12.Nelson P.R, Powell R.J, Schermerhorn M.L, Fillinger M.F, Zwolak R.M, Walsh D.B, et al. Early results of external iliac artery stenting combined with common femoral endarterectomy. J Vasc Surg. 2002;35(6):1107–1113. doi: 10.1067/mva.2002.124374. [DOI] [PubMed] [Google Scholar]
- 13.Cotroneo A.R, Iezzi R, Marano G, Fonio P, Nessi F, Gandini G, et al. Hybrid therapy in patients with complex peripheral multifocal steno-obstructive vascular disease: two-year results. Cardiovasc Interv Radiol. 2007;30(3):355–361. doi: 10.1007/s00270-005-0296-5. [DOI] [PubMed] [Google Scholar]
- 14.Chang R.W, Goodney P.P, Baek J.H, Brian B.S, Nolan W. Long-term results of combined common femoral endarterectomy and iliac stenting/stent grafting for occlusive disease. J Vasc Surg. 2008;48(2):362–367. doi: 10.1016/j.jvs.2008.03.042. [DOI] [PubMed] [Google Scholar]
- 15.Rutherford R.B, Baker J.D, Ernst C, Johnston K.W, Porter J.M, Ahn S, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997;26(3):517–538. doi: 10.1016/s0741-5214(97)70045-4. [DOI] [PubMed] [Google Scholar]
- 16.Dormandy J, Mahir M, Ascady G, Balsano F, De Leeuw P, Blombery P, et al. Fate of the patient with chronic leg ischemia: a review article. J Cardiovasc Surg. 1989;30(1):50–57. [PubMed] [Google Scholar]
- 17.Diehm C, Schuster A, Allenberg J.A, Darius H, Haberl R, Lange S. High prevalence of peripheral arterial disease and co-morbidity in 6880 primary care patients: a cross-sectional study. Atherosclerosis. 2004;172(1):195–205. doi: 10.1016/s0021-9150(03)00204-1. [DOI] [PubMed] [Google Scholar]
- 18.Vorwerk D, Guenther R.W, Schürmann K, Wendt G, Peters I. Primary stent placement for chronic iliac artery occlusions: follow-up results in 103 patients. Radiology. 1995;194(3):745–749. doi: 10.1148/radiology.194.3.7862973. [DOI] [PubMed] [Google Scholar]
- 19.Scheinert D, Schröder M, Ludwig J, Bräunlich S, Möckel M, Flachskampf F.A, et al. Stent-supported recanalization of chronic iliac artery occlusions. Am J Med. 2001;110(9):708–715. doi: 10.1016/s0002-9343(01)00727-6. [DOI] [PubMed] [Google Scholar]
- 20.Funovics M.A, Lackner B, Cejna M, Peloschek P, Sailer J, Philipp M.O, et al. Predictors of long-term results after treatment of iliac artery obliteration by transluminal angioplasty and stent placement. Cardiac Intervent Radiol. 2002;25(5):397–402. doi: 10.1007/s00270-002-1877-1. [DOI] [PubMed] [Google Scholar]
- 21.Uher P, Nyman U, Lindh M, Lindblad B, Ivancev K. Long-term results of stenting for chronic iliac artery occlusion. J Endovasc Ther. 2002;9(1):75–79. doi: 10.1177/152660280200900112. [DOI] [PubMed] [Google Scholar]
- 22.Carnevale F.C, De Blas M, Merino S, Merino S, Egaña J.M, Caldas J.G. Percutaneous endovascular treatment of chronic iliac artery occlusion. Cardiovasc Interv Radiol. 2004;27(5):447–452. doi: 10.1007/s00270-004-0086-5. [DOI] [PubMed] [Google Scholar]
- 23.Schillinger M, Sabeti S, Loewe C, Dick P, Amighi J, Mlekusch W, et al. Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery. N Engl J Med. 2006;354(18):1879–1888. doi: 10.1056/NEJMoa051303. [DOI] [PubMed] [Google Scholar]
- 24.Mewissen M.W. Self-expanding nitinol stents in the femoropopliteal segment: technique and mid-term results. Tech Vasc Interv Radiol. 2004;7(1):2–5. doi: 10.1053/j.tvir.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 25.Sabeti S, Schillinger M, Amighi J, Sherif C, Mlekusch W, Ahmadi R, et al. Primary patency of femoropopliteal arteries treated with nitinol versus stainless steel self-expanding stents: propensity score-adjusted analysis. Radiology. 2004;232:516–521. doi: 10.1148/radiol.2322031345. [DOI] [PubMed] [Google Scholar]
- 26.Nishibe T, Kondo Y, Nishibe M, Muto A, Dardik A. Stent placement of femoropoliteal arterial occlusive disease in high-risk patients: preliminary results. Surg Today. 2009;39(1):21–26. doi: 10.1007/s00595-008-3812-9. [DOI] [PubMed] [Google Scholar]
- 27.Bernhard W.M, Ray L.I, Militello J.P. The role of angioplasty of the profunda femoris artery in revascularization of the ischemic limb. Surg Gynecol Obstet. 1976;142(6):840–844. [PubMed] [Google Scholar]
- 28.Johnston K.W, Rae M, Hogg-Johnston S.A, Colapinto R.F, Walker P.M, Baird R.J, et al. 5-year results of a prospective study of percutaneous transluminal angioplasty. Ann Surg. 1987;206(4):403–413. doi: 10.1097/00000658-198710000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Myers K.A. Reporting standards and statistics for evaluating intervention. Cardiovasc Surg. 1995;3(5):455–461. doi: 10.1016/0967-2109(95)94441-x. [DOI] [PubMed] [Google Scholar]
- 30.Diehm N, Savolainen H, Mahler F, Schmidli J, Do D.D, Baumgartner I. Does deep femoral artery revascularization as an isolated procedure play a role in chronic critical limb ischemia? J Endovasc Ther. 2004;11(2):119–124. doi: 10.1583/03-1060.1. [DOI] [PubMed] [Google Scholar]
- 31.Earnshaw J.J. Surgical options for treatment of profunda femoris. In: Greenhalgh R.M, editor. Towards Vascular and Endovascular Consensus. London: Biba Medical; 2005. pp. 431–438. [Google Scholar]
- 32.Kang J.L, Patel V.I, Conrad M.F, Lamuraglia G.M, Chung T.K, Cambria R.P. Common femoral artery occlusive disease: contemporary results following surgical endarterectomy. J Vasc Surg. 2008;48(4):872–877. doi: 10.1016/j.jvs.2008.05.025. [DOI] [PubMed] [Google Scholar]
- 33.Reed A.B. Endovascular as an open adjunct: use of hybrid endovascular treatment in the SFA. Semin Vasc Surg. 2008;21(4):200–203. doi: 10.1053/j.semvascsurg.2008.11.006. [DOI] [PubMed] [Google Scholar]