Abstract
At the time of diagnosis, 20% to 25% of patients with colorectal cancer already have liver metastases, the presence of which is a most important prognostic factor. A 64-year-old man was admitted to our hospital for investigation of anemia and multiple liver tumors. Examinations revealed ascending colon carcinoma with more than 40 liver metastases and 2 lung metastases. We performed right hemicolectomy with lymph node dissection, which was followed by 5-fluorouracil/leucovorin, oxaliplatin, plus bevacizumab (FOLFOX-BV). After 4 courses of chemotherapy, the lung metastases were in complete remission and the liver metastases had shrunk. We suggested the option of radical liver resection, but the patient declined initially as he had not suffered any severe side effects of FOLFOX-BV. After 23 courses of the chemotherapy, he agreed to undergo hepatectomy. We performed extended right lobectomy with partial left and caudal lobe resection. All of the macroscopic metastatic lesions were resected. Histopathologically, viable cancer cells were recognized in 7 of the 43 liver metastatic lesions. Postoperatively, FOLFOX-BV was restarted and continued for 10 months. At the time of writing, 15 months after the hepatectomy, the patient was well without evidence of recurrence of the cancer.
Keywords: Liver metastases, Liver resection, Lung metastases, Colorectal cancer, FOLFOX
Colorectal cancer is one of most prevalent cancers in the world. The liver is the most common organ of metastasis1 and it has been reported that 80% to 90% of colorectal metastases would involve the liver and in 50% of patients it was the only organ involved.2 Unfortunately, at the time of presentation 20% to 25% of patients present with synchronous hepatic metastases and an additional 40% to 50% patients develop metachronous liver metastases after radical primary colorectal resection.3–5 As advances in surgical planning, operative technique, and perioperative care have resulted in improved outcomes, hepatic resection has obtained acceptance as the most effective therapy for patients with colorectal metastases.6 According to recent reports, new regimens consisting of 5-fluorouracil/leucovorin, oxaliplatin, or irinotecan with novel molecular targeted agents, such as bevacizumab, cetuximab, and panitumumab, have resulted in dramatic responses.7–11 This is improving the overall survival of patients with initially unresectable disease, by following tumor downstaging and complete resection.12 We report our successful treatment of ascending colon carcinoma with 43 hepatic metastases and 2 lung metastases, achieved by the combination of radical hepatic resection and perioperative chemotherapy.
Case Report
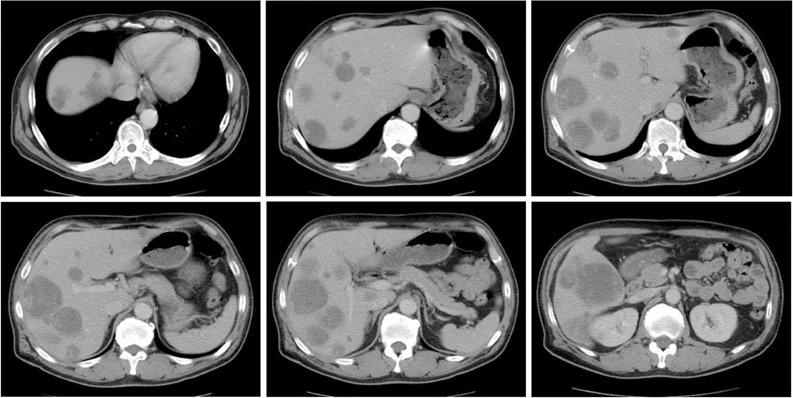
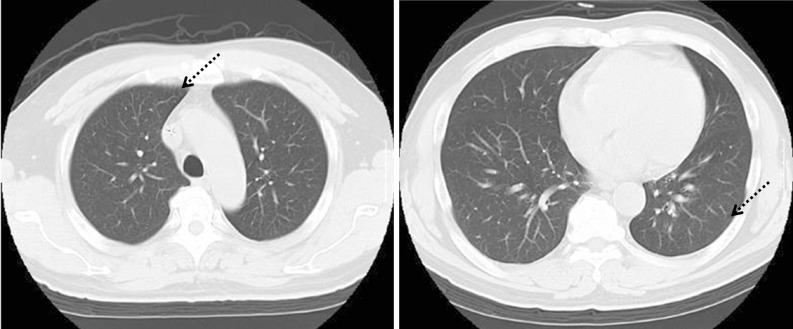
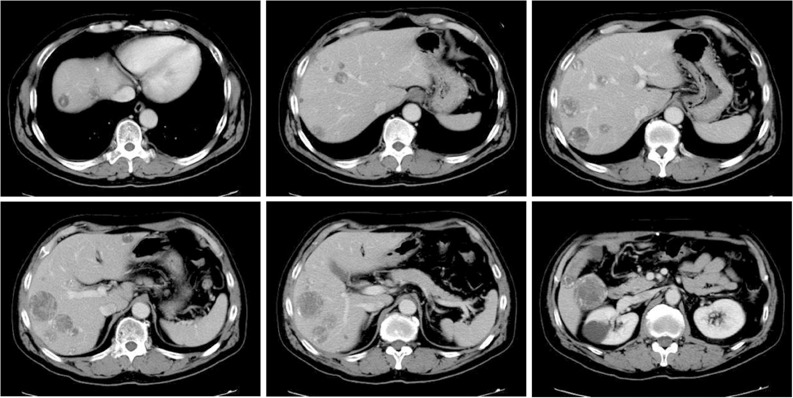
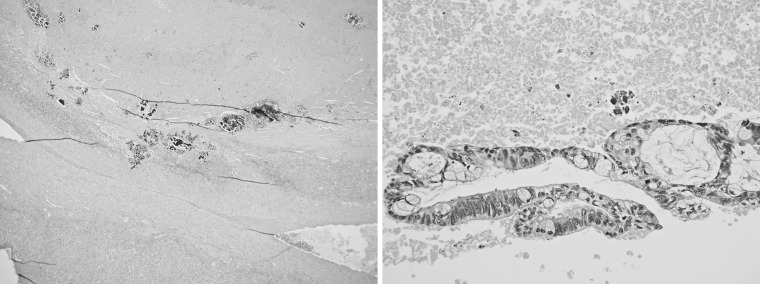
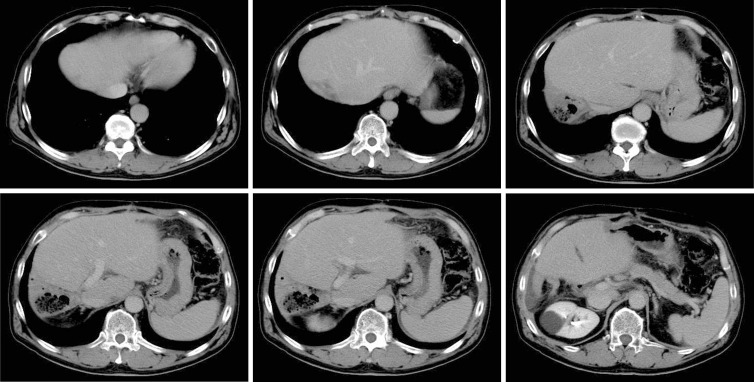
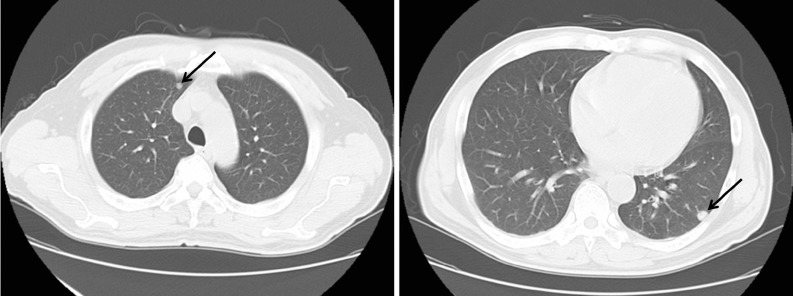
A 64-year-old man was referred to the Department of Gastroenterology at Ohta Nishinouchi General Hospital for investigation of multiple (more than 40) liver tumors and a lesion in each of the bilateral lobes of the lung. The abnormal laboratory test results were as follows: total protein, 7.1 g/dL; albumin, 4.1 g/dL; serum total bilirubin, 0.23 mg/dL; aspartate aminotransferase, 22 U/L; alanine aminotransferase, 16 U/L; low-density lipoprotein, 347 U/L; alkaliphosphatase, 380 U/L; γ-guanosine-5′-triphosphate, 106 U/L; white blood cell count, 6100/uL; hemoglobin, 8.9 g/dL; hematocrit, 29.1%; and platelets, 63.1 × 10,000/uL. The tumor markers, carcinoembryonic antigen and carbohydrate antigen 19-9 were 359.2 ng/dL and 1173.1 U/mL, respectively. Abdominal and chest computed tomography (CT) showed multiple liver tumors and 2 lung tumors: 1 in each bilobe (Fig. 1). Colonoscopy revealed ascending colon cancer; therefore, we diagnosed the multiple tumors in the liver and lung as metastases from ascending colon cancer. Because the multiple liver metastases were an impediment to performing complete resection and the lung metastases were in the bilobes, we could not perform right colectomy, liver and lung resection, as a 1-stage surgery. Thus, we performed right colectomy and lymph node dissection as the first-stage surgery. The histopathologic diagnosis was well-differentiated adenocarcinoma, with subserosal, lymphovascular, and venous invasion, but no lymph node metastasis (Fig. 2). The patient was started on 5-fluorouracil/leucovorin, oxaliplatin, plus bevacizumab (FOLFOX-BV) after this operation. A CT scan done after 4 courses of FOLFOX-BV showed complete remission of the lung metastases (Fig. 3a). Apart from slight numbness and tingling in his fingers, the patient did not suffer any severe side effects of the chemotherapy, therefore he decided against undergoing liver resection at that stage. However, after a total of 23 courses of FOLFOX-BV, he agreed to undergo hepatectomy. At that time, abdominal CT showed a shrunken tumor, which was enhanced in isodensity by contrast medium, but chest CT showed no lung metastases (Fig. 3b). Thus, we performed extended right lobectomy and partial resection of the left and caudal lobes. Enhanced contrast intraoperative ultrasound was performed to detect small metastases and all 43 metastatic lesions detected were resected (Fig. 4a). Histopathologically, viable cancer cells were found in 7 of the 43 liver metastatic lesions (Fig. 4b) and neither hepatic steatosis nor sinusoidal obstruction syndrome was recognized. The postoperative course was uneventful and FOLFOX-BV was continued for 10 months as adjuvant chemotherapy after liver resection. At the time of writing, 15 months after hepatectomy and 28 months after the initial colectomy, the patient was doing well without any sign of recurrence (Fig. 5).
Figure 1a.
Abdominal computed tomography (CT) scans showed multiple hepatic tumors in the bilobes of the liver. There were more than 40 tumors, the largest of which was 7 cm in diameter.
Figure 2.
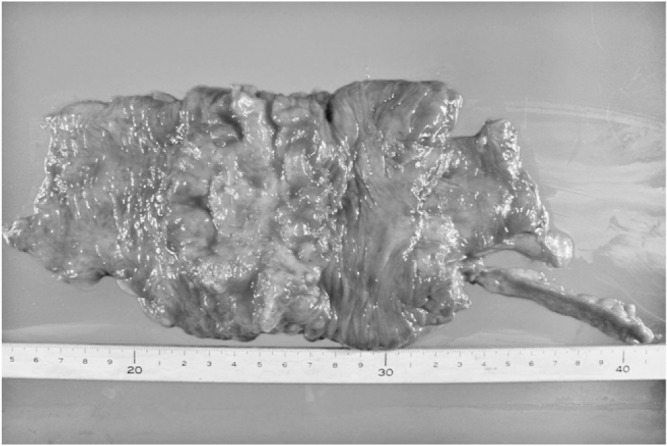
The resected right colon and ascending colon cancer. Histopathologically, well-differentiated adenocarcinoma invaded beyond the serosa, but lymph node metastasis was not recognized.
Figure 3a.
After 4 courses of FOLFOX-BV, the lung metastases were seen to be in complete remission. Arrows indicate the location of the lung metastases.
Figure 3b.
Abdominal computed tomography (CT) after 23 courses of FOLFOX-BV administration showed that the liver metastases had shrunk. Enhancement showed the tumors as isodense images instead of low-density images. FOLFOX-BV, 5-fluorouracil/leucovorin, oxaliplatin, plus bevacizumab.
Figure 4a.
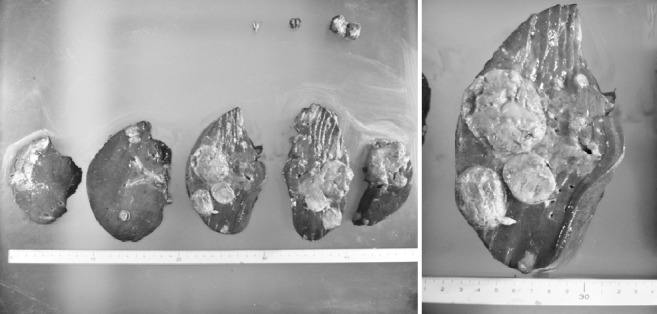
The resected liver contained the extended right lobe, parts of subsegment 2 and 3, and the Spiegel lobe. Most of the tumors were necrotic. Histopthologic examination revealed 43 liver metastases, most of which were necrotic.
Figure 4b.
Viable cancer cells were recognized in only 7 of these tumors.
Figure 5.
Abdominal computed tomography revealed no liver metastases postoperatively.
Figure 1b.
Chest CT showed a tumor (arrows) in each of the lungs.
Discussion
At present, liver resection is the only treatment that offers a chance of long-term survival for patients with metastases of colorectal cancer.3,13–17 However, until recently, the rate of resectability for metastases already present at the time of diagnosis was low.18–22 Previously, liver metastases considered unresectable were treated by palliative chemotherapy and the median survival of these patients was less than 24 months.23 With recent advances in chemotherapy for colorectal cancer, the survival of patients with inoperable metastases has been prolonged.9 Therefore, the management of asymptomatic and minimally symptomatic patients with stage IV colorectal cancer is under debate whether to operate first or administrate chemotherapy first.24
In the present case, more than 40 liver metastases and 2 lung metastases with ascending colon cancer were detected at the time of diagnosis. Anemia was obvious, therefore, resection of primary tumor was required promptly. We decided to perform right hemicolectomy as the first planned operation because 1-stage resection of colon, liver, and lung would have been too invasive. FOLFOX-BV was started after the colectomy, and achieved complete remission in the lung within 4 courses. We recommended that the patient undergo liver resection at the time; first, because it is the only treatment that offers a chance for long-term survival to a patient with stage IV colorectal cancer; and second, because we feared that he may begin to experience some of the severe side effects of FOLFOX-BV, such as immunosuppression, chemotherapy-associated liver injury, severe numbness and tingling, which would have forced us to cease its administration. However, he tolerated 23 courses of FOLFOX-BV before undergoing hepatectomy and in fact, did not suffer any severe side effects during the total 47 courses of perioperative chemotherapy he ultimately received. Some reports have described the pathologic response and chemotherapy-associated liver injury induced by preoperative chemotherapy against colorectal liver metastases.25,26 The Texas groups recently reported that the degree of pathologic response to chemotherapy predicts survival after preliver resection chemotherapy and resection of colorectal liver metastases.27 Other reports describe how bevacizumab improves pathologic response with oxaliplatin-based chemotherapy and more recently, that bevacizumab reduces the incidence of oxaliplatin-related sinusoidal injury.28 Therefore, we usually select FOLFOX-BV as first-line chemotherapy for colorectal liver metastases. Different forms of chemotherapy-related hepatotoxicity are caused by different chemotherapy regimens. Treatment with 5-fluorouracil-based treatment has been associated with an increase in steatosis, with increased postoperative morbidity.29,30 Oxaliplatin therapy increases the risk of vascular lesions and sinusoidal obstruction syndrome.25,31 Bevacizumab is associated with hypertension and relatively low rates of certain potentially serious events, such as bleeding, gastrointestinal perforation, and arterial thromboembolism.9,12,32 Kishi et al33 reported that extended preoperative FOLFOX-BV did not improve pathologic response and increased postoperative hepatotoxicity. Of the 43 liver metastases in our patient, histologic examination revealed only 7 (16.3%) with viable cancer cells remaining. Not only was it a sensitive regimen for our patient, but despite 44 weeks of continuous chemotherapy, chemotherapy-induced hepatic injury was not recognized in the resected liver histopathologically.
As adjuvant chemotherapy after liver resection, FOLFOX-BV proved effective by achieving complete remission of the lung metastases and remarkable shrinkage of the multiple liver metastases and also targeting micrometastases in the lung and remnant liver without severe side effects. We took into consideration the high risk of recurrence in this patient, and the fact that FOLFOX-BV has not gained consensus as adjuvant chemotherapy after liver resection, preserving another chemotherapy regimen for the future.
This case clearly demonstrates the potential of FOLFOX-BV as a preoperative and postoperative chemotherapy regimen, if the patient does not suffer its severe side effects. Radical surgery and aggressive chemotherapy can collaborate to prolong the survival of colorectal cancer patients with liver and lung metastases.
References
- 1.Poston G.J, Adam R, Alberts S, Curley S, Figueras J, Haller D, et al. OncoSurge: a strategy for improving resectability with curative intent in metastatic colorectal cancer. J Clin Oncol. 2005;23(28):7125–7134. doi: 10.1200/JCO.2005.08.722. [DOI] [PubMed] [Google Scholar]
- 2.Galizia G, Lieto E, Orditura M, Castellano P, Imperatore V, Pinto M, et al. First-line chemotherapy vs bowel tumor resection plus chemotherapy for patients with unresectable synchronous colorectal hepatic metastases. Arch Surg. 2008;143(4):352–358. doi: 10.1001/archsurg.143.4.352. [DOI] [PubMed] [Google Scholar]
- 3.Stangl R, Altendorf-Hofmann A, Charnley R.M, Scheele J. Factors influencing the natural history of colorectal liver metastases. Lancet. 1994;343(8910):1405–1410. doi: 10.1016/s0140-6736(94)92529-1. [DOI] [PubMed] [Google Scholar]
- 4.Scheele J, Stangl R, Altendorf-Hofmann A. Hepatic metastases from colorectal carcinoma: impact of surgical resection on the natural history. Br J Surg. 1990;77(11):1241–1246. doi: 10.1002/bjs.1800771115. [DOI] [PubMed] [Google Scholar]
- 5.Sugarbaker P.H. Surgical decision making for large bowel cancer metastatic to the liver. Radiology. 1990(3 Pt 1);174:621–626. doi: 10.1148/radiology.174.3.2406776. [DOI] [PubMed] [Google Scholar]
- 6.Registry of Hepatic Metastases. Resection of the liver for colorectal carcinoma metastases: a multi-institutional study of indications for resection. Surgery. 1988;103(3):278–288. [PMC free article] [PubMed] [Google Scholar]
- 7.Goldberg R.M, Sargent D.J, Morton R.F, Fuchs C.S, Ramanathan R.K, Williamson S.K, et al. A randomized controlled trial of fluorouracil plus leucovorin, irinotecan, and oxaliplatin combinations in patients with previously untreated metastatic colorectal cancer. J Clin Oncol. 2004;22(1):23–30. doi: 10.1200/JCO.2004.09.046. [DOI] [PubMed] [Google Scholar]
- 8.Grothey A, Sargent D, Goldberg R.M, Schmoll H.J. Survival of patients with advanced colorectal cancer improves with the availability of fluorouracil-leucovorin, irinotecan, and oxaliplatin in the course of treatment. J Clin Oncol. 2004;22(7):1209–1214. doi: 10.1200/JCO.2004.11.037. [DOI] [PubMed] [Google Scholar]
- 9.Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350(23):2335–2342. doi: 10.1056/NEJMoa032691. [DOI] [PubMed] [Google Scholar]
- 10.Van Cutsem E, Kohne C.H, Hitre E, Zaluski J, Chang Chien C.R, Makhson A, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med. 2009;360(14):1408–1417. doi: 10.1056/NEJMoa0805019. [DOI] [PubMed] [Google Scholar]
- 11.Douillard J.Y, Siena S, Cassidy J, Tabernero J, Burkes R, Barugel M, et al. Randomized, phase III trial of panitumumab with infusional fluorouracil, leucovorin, and oxaliplatin (FOLFOX4) versus FOLFOX4 alone as first-line treatment in patients with previously untreated metastatic colorectal cancer: the PRIME study. J Clin Oncol. 2010;28(31):4697–4705. doi: 10.1200/JCO.2009.27.4860. [DOI] [PubMed] [Google Scholar]
- 12.Okines A, Puerto O.D, Cunningham D, Chau I, Van Cutsem E, Saltz L, et al. Surgery with curative-intent in patients treated with first-line chemotherapy plus bevacizumab for metastatic colorectal cancer First BEAT and the randomised phase-III NO16966 trial. Br J Cancer. 2009;101(7):1033–1038. doi: 10.1038/sj.bjc.6605259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tomlinson J.S, Jarnagin W.R, DeMatteo R.P, Fong Y, Kornprat P, Gonen M, et al. Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol. 2007;25(29):4575–4580. doi: 10.1200/JCO.2007.11.0833. [DOI] [PubMed] [Google Scholar]
- 14.Scheele J, Stang R, Altendorf-Hofmann A, Paul M. Resection of colorectal liver metastases. World J Surg. 1995;19(1):59–71. doi: 10.1007/BF00316981. [DOI] [PubMed] [Google Scholar]
- 15.Jaeck D, Bachellier P, Guiguet M, Boudjema K, Vaillant J.C, Balladur P, et al. Long-term survival following resection of colorectal hepatic metastases. Association Francaise de Chirurgie. Br J Surg. 1997;84(7):977–980. doi: 10.1002/bjs.1800840719. [DOI] [PubMed] [Google Scholar]
- 16.Fong Y, Fortner J, Sun R.L, Brennan M.F, Blumgart L.H. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230(3):309–318. doi: 10.1097/00000658-199909000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adam R, Pascal G, Azoulay D, Tanaka K, Castaing D, Bismuth H. Liver resection for colorectal metastases: the third hepatectomy. Ann Surg. 2003;238(6):871–883. doi: 10.1097/01.sla.0000098112.04758.4e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cook A.D, Single R, McCahill L.E. Surgical resection of primary tumors in patients who present with stage IV colorectal cancer: an analysis of surveillance, epidemiology, and end results data, 1988 to 2000. Ann Surg Oncol. 2005;12(8):637–645. doi: 10.1245/ASO.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 19.Lee W.S, Yun H.R, Yun S.H, Chun H.K, Lee W.Y, Kim S.J, et al. Treatment outcomes of hepatic and pulmonary metastases from colorectal carcinoma. J Gastroenterol Hepatol. 2008;23(8 Pt 2):e367–e372. doi: 10.1111/j.1440-1746.2007.05178.x. [DOI] [PubMed] [Google Scholar]
- 20.Arru M, Aldrighetti L, Castoldi R, Di Palo S, Orsenigo E, Stella M, et al. Analysis of prognostic factors influencing long-term survival after hepatic resection for metastatic colorectal cancer. World J Surg. 2008;32(1):93–103. doi: 10.1007/s00268-007-9285-y. [DOI] [PubMed] [Google Scholar]
- 21.Taniai N, Akimaru K, Yoshida H, Tajiri T. Surgical treatment for better prognosis of patients with liver metastases from colorectal cancer. Hepatogastroenterology. 2007;54(78):1805–1809. [PubMed] [Google Scholar]
- 22.Lau W.Y, Lai E.C. Hepatic resection for colorectal liver metastases. Singapore Med J. 2007;48(7):635–639. [PubMed] [Google Scholar]
- 23.Giacchetti S, Itzhaki M, Gruia G, Adam R, Zidani R, Kunstlinger F, et al. Long-term survival of patients with unresectable colorectal cancer liver metastases following infusional chemotherapy with 5-fluorouracil, leucovorin, oxaliplatin and surgery. Ann Oncol. 1999;10(6):663–669. doi: 10.1023/a:1008347829017. [DOI] [PubMed] [Google Scholar]
- 24.Stillwell A.P, Buettner P.G, Ho Y.H. Meta-analysis of survival of patients with stage IV colorectal cancer managed with surgical resection versus chemotherapy alone. World J Surg. 2011;34(3):797–807. doi: 10.1007/s00268-009-0366-y. [DOI] [PubMed] [Google Scholar]
- 25.Vauthey J.N, Pawlik T.M, Ribero D, Wu T.T, Zorzi D, Hoff P.M, et al. Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J Clin Oncol. 2006;24(13):2065–2072. doi: 10.1200/JCO.2005.05.3074. [DOI] [PubMed] [Google Scholar]
- 26.Pawlik T.M, Olino K, Gleisner A.L, Torbenson M, Schulick R, Choti M.A. Preoperative chemotherapy for colorectal liver metastases: impact on hepatic histology and postoperative outcome. J Gastrointest Surg. 2007;11(7):860–868. doi: 10.1007/s11605-007-0149-4. [DOI] [PubMed] [Google Scholar]
- 27.Blazer D.G, 3rd, Kishi Y, Maru D.M, Kopetz S, Chun Y.S, Overman M.J, et al. Pathologic response to preoperative chemotherapy: a new outcome end point after resection of hepatic colorectal metastases. J Clin Oncol. 2008;26(33):5344–5351. doi: 10.1200/JCO.2008.17.5299. [DOI] [PubMed] [Google Scholar]
- 28.Ribero D, Wang H, Donadon M, Zorzi D, Thomas M.B, Eng C, et al. Bevacizumab improves pathologic response and protects against hepatic injury in patients treated with oxaliplatin-based chemotherapy for colorectal liver metastases. Cancer. 2007;110(12):2761–2767. doi: 10.1002/cncr.23099. [DOI] [PubMed] [Google Scholar]
- 29.Zorzi D, Laurent A, Pawlik T.M, Lauwers G.Y, Vauthey J.N, Abdalla E.K. Chemotherapy-associated hepatotoxicity and surgery for colorectal liver metastases. Br J Surg. 2007;94(3):274–286. doi: 10.1002/bjs.5719. [DOI] [PubMed] [Google Scholar]
- 30.Kooby D.A, Fong Y, Suriawinata A, Gonen M, Allen P.J, Klimstra D.S, et al. Impact of steatosis on perioperative outcome following hepatic resection. J Gastrointest Surg. 2003;7(8):1034–1044. doi: 10.1016/j.gassur.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 31.Rubbia-Brandt L, Audard V, Sartoretti P, Roth A.D, Brezault C, Le Charpentier M, et al. Severe hepatic sinusoidal obstruction associated with oxaliplatin-based chemotherapy in patients with metastatic colorectal cancer. Ann Oncol. 2004;15(3):460–466. doi: 10.1093/annonc/mdh095. [DOI] [PubMed] [Google Scholar]
- 32.Hochster H.S, Hart L.L, Ramanathan R.K, Childs B.H, Hainsworth J.D, Cohn A.L, et al. Safety and efficacy of oxaliplatin and fluoropyrimidine regimens with or without bevacizumab as first-line treatment of metastatic colorectal cancer: results of the TREE study. J Clin Oncol. 2008;26(21):3523–3529. doi: 10.1200/JCO.2007.15.4138. [DOI] [PubMed] [Google Scholar]
- 33.Kishi Y, Zorzi D, Contreras C.M, Maru D.M, Kopetz S, Ribero D, et al. Extended preoperative chemotherapy does not improve pathologic response and increases postoperative liver insufficiency after hepatic resection for colorectal liver metastases. Ann Surg Oncol. 2010;17(11):2870–2876. doi: 10.1245/s10434-010-1166-1. [DOI] [PubMed] [Google Scholar]