Abstract
The aim of this study is to analyze the risk factors for complications and recurrence in pilonidal sinus disease. The prospective study consisted of 144 patients with pilonidal sinus disease who were operated on at Dicle University Medical Faculty, Department of General Surgery, between February 2008 and December 2010. Patients receiving the Limberg flap totaled 106 (73.6%), while 38 (26.4%) had primary closure. Postoperative complications developed in 42 subjects (29.2%), and recurrence occurred in 19 (13.2%). The Limberg flap method was statistically considered as a risk factor for postoperative complications (P = 0.039). Regarding recurrence, family tendency (P = 0.011), sinus number (P = 0.005), cavity diameter (P = 0.002), and primary closure (P = 0.001) were found to be risk factors. Postoperative complication rate is higher in the Limberg flap method than primary closure method. The risk of recurrence is related to family tendency, sinus number, cavity diameter and anesthesia type and is also higher in primary closure.
Keywords: Pilonidal sinus disease, Postoperative complication, Recurrence
Pilonidal sinus disease (PSD), diagnosed by the penetration of hair follicles into one or more sinus walls, attacks younger subjects more frequently and chronically develops with acute and subacute instances of infection.1 Frequently seen in the midline of the sacrococcygeal region,1 it limits the patient’s lifestyle and results in loss of productive power.2 For treatment, various noninvasive3 and surgical methods (simple incision and drainage, lying open, marsupialization, excision and primary closure, or rhomboid excision and Limberg flap) have been performed.4–6 Despite these methods, the disease often leads to postoperative complications and recurrence. Male gender, obesity, smoking, family tendency, poor body hygiene, sinus size, and the surgical procedures performed have been confirmed in a number of studies as primary risk factors for postoperative complications and recurrence.1,7–13 In this study, we aimed to analyze the risk factors for postoperative complications and recurrence in PSD.
Patients and Methods
The prospective study included 144 consecutive patients with PSD who underwent surgery between February 2008 and November 2010. Physical signs and patient’s history were reviewed. In terms of postoperative complications and recurrence, age, gender, time from the onset of the symptoms, systemic and congenital diseases, skin color (fair-skinned or dark-skinned), family tendency, body mass index (BMI), smoking habits, duration of the disease, abscess formation and number (if any), drainage type (closed-suction drain or not), sinus number, hematocrit value, type of anesthesia (local or spinal), surgical method (primary closure or Limberg flap), necessity of drainage, extent of the excised cavity, pathologic results, hospital stay, and duration of wound healing were studied. The patients with recurrent pilonidal sinuses and diabetes mellitus, and who had previously received phenol treatment were excluded from the study. The BMI for each patient was calculated based upon their height and weight [weight (kg)/height (m)2]. Depending on the BMI range, 20–25.9, 26–29.9, and over 30, patients were classified as normal range, overweight, and obese, respectively. The patients in which infection or an abscess was detected underwent surgical operation 8 weeks after having received simple drainage and antibiotic treatment.14
The classification of patients into 2 groups was made arbitrarily and without any bias as follows: group 1 (primary closure group) and group 2 (Limberg flap group), according to the surgical procedures.
In the primary closure group, the patients were placed in the jackknife position; the area to be excised was marked on the skin, and a rhomboid incision to the presacral fascia including the sinus and its extensions was made longitudinally, from superior to inferior. A closed-suction drain was then placed in several patients. The skin edges were approximated without tension using interrupted sutures of absorbable 3/0 suture or liquid skin adhesive.
In the Limberg flap group, the patients were also placed in the jackknife position, and the area to be excised, as well as the Limberg flap, was marked on the skin. This was followed by a rhomboid incision, including the sinus and its extensions, made to the presacral fascia. The flap was then constructed, extending the incision laterally and inferiorly to the gluteal fascia. The flap was transposed, and the defect was covered. A closed-suction drain was placed, and the skin was closed with nonabsorbable, monofilament, interrupted sutures.
Family tendency about PSD
Presence of PSD in one or more family members is a possible occurrence in the patients with family tendency. Complete healing date was determined by the date of removal of the suture in primary healing or epithelization of the sacral wound in healing by secondary intention, sick leave, and clinic visit.
The postoperative complications in the first month included wound infection signs such as pain, tenderness, and erythema, along with hematoma, seroma, and wound separation.15 The patients were followed and evaluated for recurrence in a median period of 27.5 months.
Statistical method
All statistical analysis in this study was performed using SPSS software (Version 13.0, SPSS Inc, Chicago, IL). For group comparisons, Student t test was used for parametric data, while Mann-Whitney U test was used for nonparametric data. Chi-square test was used for comparing 2 categorical variables. Risk factors for complications and recurrence were evaluated by multivariable logistic regression analysis. For all P values, P = 0.05 was considered to indicate statistical significance, and odds-ratios (OR) were calculated for each variable.
Results
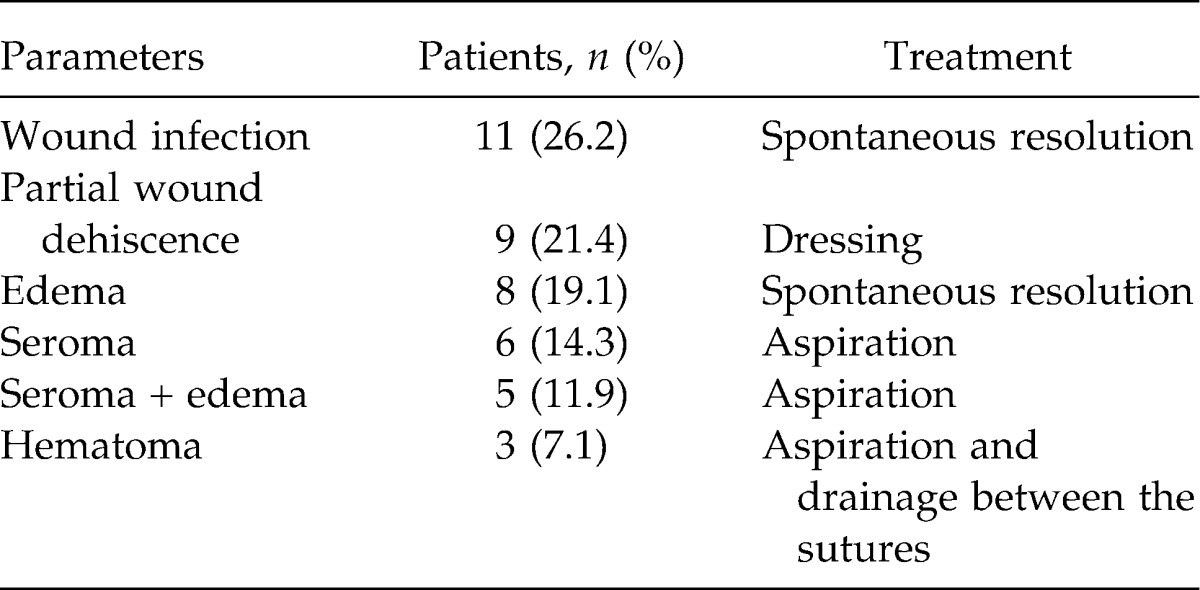
The demographic characteristics of the patients are given in Table 1. Also, demographic characteristics and findings according to the groups are given in Table 2. The presence of symptom duration, the number of sinuses, the diameter of the cavity, the length of hospital stay, the healing time, and the rate of postoperative complications were higher in group 2, but the recurrence rate was significantly lower in group 2 compared with group 1. The most common complication was wound infection, and it was detected in 12 (26.2%) subjects as shown in Table 3, together with other morbidities and treatment protocols. No patients developed a complication that required surgical intervention. Recurrence occurred in 19 (13.2%) patients during the median follow-up period of 27.5 months. The pathologic results revealed basal cell carcinoma in one patient, and the remaining 143 subjects were reported as benign.
Table 1.
The demographic characteristics of the patients
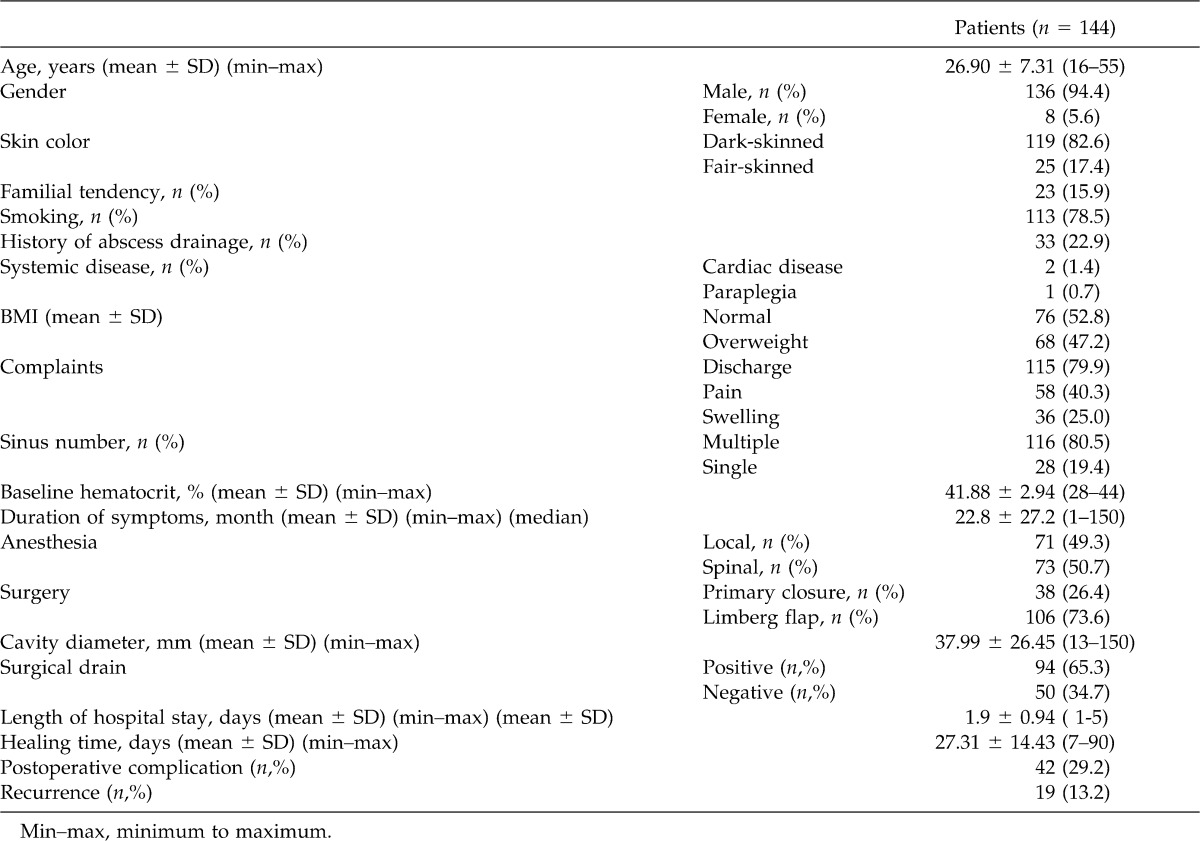
Table 2.
The demographic characteristics and findings according to the treatment groups
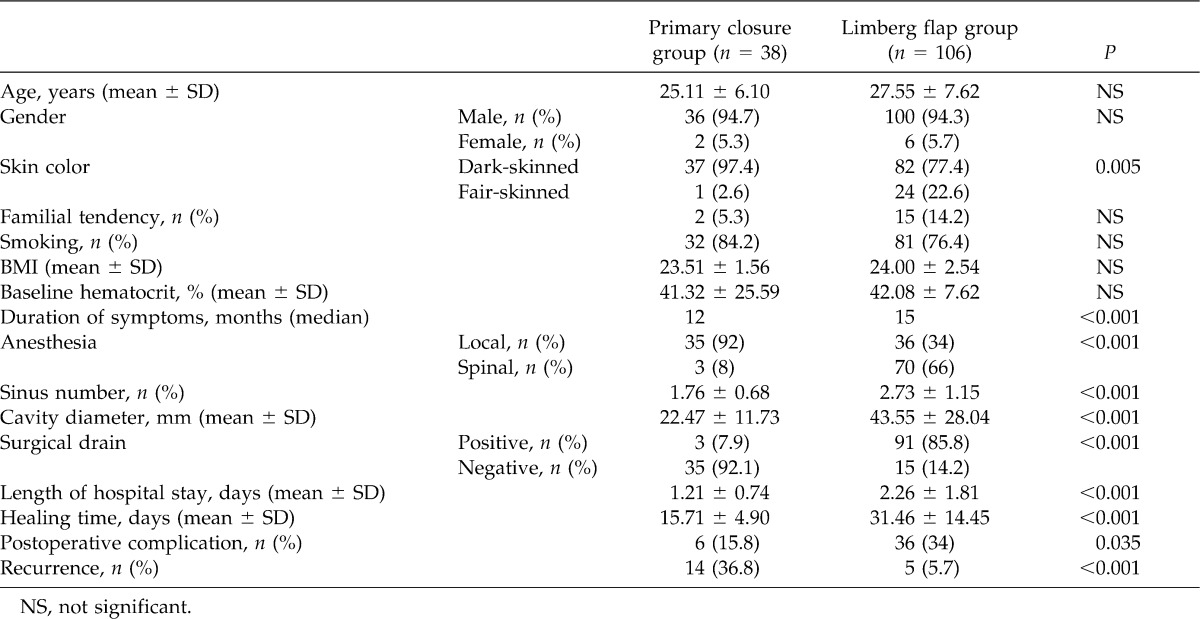
Table 3.
Postoperative complications and treatment
Following univariate analysis, wound healing time was assessed as 24.17 ± 11.65 days for the patients without postoperative complications, while patients with complications displayed a wound healing time of 34.93 ± 17.54 days (P = 0.001). Performing Limberg flap and closure methods upon postoperative complications was found as a risk factor by univariate analysis (P = 0.039). Regarding recurrence, family tendency (P = 0.011), sinus numbers (P = 0.005), the cavity diameter (P = 0.002), application of local anesthesia (P = 0.010), and primary closure (P = 0.001) were assessed as risk factors.
Multivariate analysis proved the Limberg flap method as an independent risk factor for postoperative complications (P = 0.004). As for recurrence, cavity diameter (P = 0.001), primary closure (P = 0.007), and family tendency (P = 0.008) were found as independent risk factors.
Discussion
PSD is an important disease that seems simple but leads to high rates of postoperative complication and recurrence. However, there is not a consensus on the ideal treatment type for PSD despite many alternatives. It has a high incidence rate of 26 to 700 of 100,000 people. It is more common in male subjects between the ages of 20 and 25 years.16 The disease was seen 4.1 to 8.1 times more in males than in females.17,18 The reason that higher frequency exists in puberty and lower frequency exists for those over 40 years of age could be explained by the effect of more active sex hormones during puberty on pilosebaceous glands. The affected girls were younger than the boys, likely because of the earlier onset of puberty in females.19 Among the patients in the present study, males had a rate of 94.4% with an average age of onset of 26.9 years, while females displayed a rate of 5.6% with an average age of onset of 27.9 years. The ratio of females versus males was 1:17. In our study, age and gender were not proven as risk factors for postoperative complications and recurrence. However, the ratio between female and male PSD patients in Turkey is reported to be lower than ratios in Western countries. Also, the mean age for females is found to be older, which could be associated with the notion that our female patients, as with other anorectal diseases, refrain from seeing a doctor for PSD until the discomfort becomes unbearable and partially because of social bias. In the etiology, PSD was previously believed to result from postcoxygeal cells or remnant glands, whereas acquired factors are considered to play the greatest part today. Karydakis attributed the hair insertion process to 3 main factors: the invader, the force which causes the insertion, and the vulnerability of the skin to the insertion of hair at the depth of the natal cleft.9 Family tendency is also an important factor. Sondenaa et al20 have reported it to be 38%, and Doll et al7 reported that family tendency accelerates the development of PSD, causing higher risk of recurrence, while suggesting that the positive patients should be closely followed up. Family tendency was evident in 15.9% of our patients. Despite the lack of significance for postoperative complications, it was evident as an important risk factor for recurrence. This could be due to the results presented by similar body types and hair characteristics as well as similar hygienic conditions. PSD is reported to be more common in hirsute people with dark skin and dark hair, with a smaller frequency in black and Asian people.3,7 Nonetheless, 119 (82.6%) of our patients were dark skinned, but they did not present a significant distribution in terms of postoperative complications and recurrence.
Obesity has been reported as an important risk factor and to be related to higher rates of postoperative complication and recurrence in PSD.8,20–22 Cubukcu et al23 did not detect a statistical significance between BMI and PSD. Because of the deeper structure of the intergluteal cleft and the fragility with wetness as a result of oversweat, obese people are more vulnerable to PSD. Indeed, the softness of the surface structure in intergluteal region in obese people raises this vulnerability. However, in terms of etiology, PSD is not confined to the obese alone but is also a concern in those with excessive pilosity, oversweat, poor body hygiene, irregular presacral shaving, and unsuitable diets.9,10,24 Sixty-eight (47.2%) of our patients were overweight, yet they did not correlate with postoperative complication and recurrence.
Smoking leads to hypoxia development in peripheral structures, causing the proliferation of bacteria in the wound area. This also triggers separation in the wound area, reducing the restraining capacity of sutures while promoting the impairment of collagen synthesis. Further, it weakens oxidative killing by neutrophils.11,12 In our study, patients who smoked developed postoperative complications with a rate of 32.7%, although this did not provide a statistical significance.
In connection with its shape and follow-up duration, the diameter of the sinus is an important matter for recurrence.25 Another possible reason for recurrence includes inadequate excision of the sinus tract.13,26 It was found that there was a positive correlation between an elevated number of sinus tracts and recurrence. It was believed that curative surgery becomes undoable when some sinuses remain as residues as a result of higher numbers of sinuses during surgery. The diameter of the cavity in PSD is concerned with the width and depth of the wound as well as the number of sinus tracts opening to the cavity. Definitive treatment in PSD is achieved through complete removal of infected tissues in one block.27 The cavity extent in the nonrecurrence group was significant, convincing the investigators that no residual tracts occurred in the study.
There was a statistical significance between the groups that had spinal anesthesia and those that had local anesthesia in terms of the cavity extent. It was noted that the use of local anesthesia did not enable effective surgery because of the pain in the wound area and the discomfort experienced by the patient and the surgeon, and that it limited the surgical area of operation, all of which influenced the recurrence rate.
The basic step in PSD treatment is surgical excision. However, there is no consensus on an ideal method for excision. This is owing to the conviction that there is a direct relationship between closure method and the risk of recurrence. Primary closure method is more popular because it accelerates wound healing, shortens the times of surgery and hospitals stays, and has proven to be practical.22 Recurrence rates of 7% to 42% have been reported with this method.20,28 Possible reasons among postprimary recurrence include scar formation in gluteal cleft and tension.29 A number of studies have reported a recurrence rate of zero to 3% after rhomboid excision and Limberg flap repair.5,30,31 In the present study, the flap method led to higher postoperative complications, while primary closure resulted in a higher recurrence rate. Drainage in PSD is used not only to prevent postoperative complications and hematoma but also to eliminate the potential cavity following excision.19,32 In this study, drainage was not correlated with postoperative complication or recurrence. Postoperative healing time for PSD ranged between 13 and 30 days.18,32 The group with postoperative complications in the present study had a healing period of over 1 month. Though rare, malignant formation is also possible during long-term PSD follow-ups. The formations are generally squamous cell carcinomas.33 Only one patient in this study was diagnosed with basal cell carcinoma.
Conclusion
In PSD, postoperative complication is a rare development when using primary closure, yet it is frequent in the Limberg flap method. The recurrence rates are also significantly higher in primary closure than in Limberg flap. Additionally, family tendency, sinus number, cavity diameter, and local anesthesia are among the risk factors for recurrence.
References
- 1.Harlak A., Mentes O., Kilic S., Coskun K., Duman K., Yilmaz F. Sacrococcygeal pilonidal disease: analysis of previously proposed risk factors. Clinics. 2010;65(2):125–131. doi: 10.1590/S1807-59322010000200002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harlak A., Mentes O., Ozer M. T., Ersoz N., Coskun A. K. Evaluation of history and physical examination data of 587 patients with sacrococcygeal pilonidal disease. Eurasian J Med. 2006;38(3):103–106. [Google Scholar]
- 3.Kaymakcioglu N., Yagci G., Simsek A., Unlu A., Tekin O. F., Cetiner S., et al. Treatment of pilonidal sinus by phenol application and factors affecting the recurrence. Tech Coloproctol. 2005;9(1):21–24. doi: 10.1007/s10151-005-0187-4. [DOI] [PubMed] [Google Scholar]
- 4.Lee H. C., Ho Y. H., Seow C. F., Eu K. W., Nyam D. Pilonidal disease in Singapore: clinical features and management. Aust N Z J Surg. 2000;70(3):196–198. doi: 10.1046/j.1440-1622.2000.01785.x. [DOI] [PubMed] [Google Scholar]
- 5.Mentes B. B., Leventoglu S., Cihan A., Tatlicioglu E., Akin M., Oguz M. Modified Limberg transposition flap for sacrococcygeal pilonidal sinus. Surg Today. 2004;34(5):419–423. doi: 10.1007/s00595-003-2725-x. [DOI] [PubMed] [Google Scholar]
- 6.Cihan A., Mentes B. B., Tatlicioglu E., Ozmen S., Leventoglu S., Ucan B. H. Modified Limberg flap reconstruction compares favorably with primary repair for pilonidal sinus surgery. ANZ J Surg. 2004;74(4):238–242. doi: 10.1111/j.1445-2197.2004.02951.x. [DOI] [PubMed] [Google Scholar]
- 7.Doll D., Matevossian E., Wietelmann K., Evers T., Kriner M., Petersen S. Family history of pilonidal sinus predisposes to earlier onset of disease and a 50% long-term recurrence rate. Dis Colon Rectum. 2009;52(9):1610–1615. doi: 10.1007/DCR.0b013e3181a87607. [DOI] [PubMed] [Google Scholar]
- 8.Arda I. S., Guney L. H., Sevmis S., Hiçsonmez A. High body mass index as a possible risk factor for pilonidal sinus disease in adolescents. World J Surg. 2005;29(4):469–471. doi: 10.1007/s00268-004-7533-y. [DOI] [PubMed] [Google Scholar]
- 9.Hull T. L., Wu J. Pilonidal disease. Surg Clin North Am. 2002;82(6):1169–1185. doi: 10.1016/s0039-6109(02)00062-2. [DOI] [PubMed] [Google Scholar]
- 10.Cubukcu A., Gonullu N. N., Paksoy M., Alponat A., Kuru M., Özbay O. The role of obesity on the recurrence of pilonidal sinus disease in patients, who were treated by excision and Limberg flap transposition. Int J Colorectal Dis. 2000;15(3):173–175. doi: 10.1007/s003840000212. [DOI] [PubMed] [Google Scholar]
- 11.Sorensen L. T., Horby J., Friis E., Pilsgaard B., Jorgensen T. Smoking as a risk factor for wound healing and infection in breast cancer surgery. Eur J Surg Oncol. 2002;28(8):815–820. doi: 10.1053/ejso.2002.1308. [DOI] [PubMed] [Google Scholar]
- 12.Al-Khayat H., Al-Khayat H., Sadeq A., Groof A., Haider H. H., Hayati H., et al. Risk factors for wound complication in pilonidal sinus procedures. J Am Coll Surg. 2007;205(3):439–444. doi: 10.1016/j.jamcollsurg.2007.04.034. [DOI] [PubMed] [Google Scholar]
- 13.Aldean I., Shankar P. J., Mathew J., Safarani N., Haboubi N. Y. Simple excision and primary closure of pilonidal sinus: a simple modification of conventional technique with excellent results. Colorectal Dis. 2005;7(1):81–85. doi: 10.1111/j.1463-1318.2004.00736.x. [DOI] [PubMed] [Google Scholar]
- 14.Vahedian J., Nabavizadeh F., Nakhaee N., Vahedian M., Sadeghpour A. Comparison between drainage and curettage in the treatment of acute pilonidal abscess. Saudi Med J. 2005;26(4):553–555. [PubMed] [Google Scholar]
- 15.Sessler D. I. Supplemental oxygen and surgical site infection. Arch Surg. 2011;146(10):1221–1222. doi: 10.1001/archsurg.2011.290. [DOI] [PubMed] [Google Scholar]
- 16.Can M. F., Sevinc M. M., Yilmaz M. Comparison of Karydakis flap reconstruction versus primary midline closure in sacrococcygeal pilonidal disease: results of 200 military service members. Surg Today. 2009;39(7):580–586. doi: 10.1007/s00595-008-3926-0. [DOI] [PubMed] [Google Scholar]
- 17.Osmanoglu G., Yetisir F. Limberg flap is better for the surgical treatment of pilonidal sinus: results of a 767 patients series with an at least five years follow-up period. Chirurgia (Bucur) 2011;106(4):491–494. [PubMed] [Google Scholar]
- 18.Anderson J. H., Yip C. O., Nagabhushan J. S., Connelly S. J. Day-Case Karydakis flap for pilonidal sinus. Dis Colon Rectum. 2008;51(1):134–138. doi: 10.1007/s10350-007-9150-y. [DOI] [PubMed] [Google Scholar]
- 19.Serour F., Somekh E., Krutman B., Gorenstein A. Excision with primary closure and suction drainage for pilonidal sinus in adolescent patients. Pediatr Surg Int. 2002;18(2-3):159–161. doi: 10.1007/s003830100683. [DOI] [PubMed] [Google Scholar]
- 20.Sondenaa K., Andersen E., Nesvik I., Soreide J. A. Patient characteristics and symptoms in chronic pilonidal sinus disease. Int J Colorectal Dis. 1995;10(1):39–42. doi: 10.1007/BF00337585. [DOI] [PubMed] [Google Scholar]
- 21.Kayadibi A., Hasanoğlu A., Akkuş M. A. The relationship between occupation, age, sex, body mass index and pilonidal sinus disease. Turkish Med J. 2007;1:123–127. [Google Scholar]
- 22.Sakr M., El-Hammadi H., Moussa M., Arafa S., Rasheed M. The effect of obesity on the results of Karydakis technique for the management of chronic pilonidal sinus. Int J Colorectal Dis. 2003;18(1):36–39. doi: 10.1007/s00384-002-0407-6. [DOI] [PubMed] [Google Scholar]
- 23.Cubukcu A., Carkman S., Gonullu N. N., Alponat A., Kayabası B., Eyupoglu E. Lack of evidence that obesity is a cause of pilonidal sinus disease. Eur J Surg. 2000;167(4):297–298. doi: 10.1080/110241501300091525. [DOI] [PubMed] [Google Scholar]
- 24.Balik O., Balik A. A., Polat K. Y., Aydinli B., Kantarci M., Aliagaoglu C., Akcay M. N. The importance of local subcutaneous fat thickness in pilonidal disease. Dis Colon Rectum. 2006;49(11):1755–1757. doi: 10.1007/s10350-006-0672-5. [DOI] [PubMed] [Google Scholar]
- 25.Mentes O., Bagci M., Bilgin T., Coskun I., Ozgul O., Ozdemir M. Management of pilonidal sinus disease with oblique excision and primary closure: results of 493 patients. Dis Colon Rectum. 2006;49(1):104–108. doi: 10.1007/s10350-005-0226-2. [DOI] [PubMed] [Google Scholar]
- 26.Kulacoglu H., Dener C., Tumer H., Aktimur R. Total subcutaneous fistulectomy combined with Karydakis flap for sacrococcygeal pilonidal disease with secondary perianal opening. Colorectal Dis. 2006;8(2):120–123. doi: 10.1111/j.1463-1318.2005.00872.x. [DOI] [PubMed] [Google Scholar]
- 27.Spivak H., Brooks V. L., Nussbaum M., Friedman I. Treatment of chronic pilonidal disease. Dis Colon Rectum. 1996;39(10):1136–1139. doi: 10.1007/BF02081415. [DOI] [PubMed] [Google Scholar]
- 28.Lesalnieks I., Furst A., Rentsch M., Jauch K. W. Primary midline closure after excision of a pilonidal sinus is associated with a high recurrence rate. Chirurg. 2003;74(5):461–468. doi: 10.1007/s00104-003-0616-8. [DOI] [PubMed] [Google Scholar]
- 29.Akinci O. F., Coskun A., Uzunköy A. Simple and effective surgical treatment of pilonidal sinus. Dis Colon Rectum. 2000;43(5):701–707. doi: 10.1007/BF02235591. [DOI] [PubMed] [Google Scholar]
- 30.Eryilmaz R., Sahin M., Alimoglu O., Dasiran F. Surgical treatment of sacrococcygeal pilonidal sinus with the Limberg transposition flap. Surgery. 2003;134(5):745–749. doi: 10.1016/s0039-6060(03)00163-6. [DOI] [PubMed] [Google Scholar]
- 31.Kapan M., Kapan S., Pekmezci S., Durgun V. Sacrococcygeal pilonidal sinus disease with Limberg flap repair. Tech Coloproctol. 2002;6(1):27–32. doi: 10.1007/s101510200005. [DOI] [PubMed] [Google Scholar]
- 32.Gurer A., Gomceli I., Ozdogan M., Ozlem N., Sozen S., Aydin R. Is routine cavity drainage necessary in Karydakis flap operation? A prospective, randomized trial. Dis Colon Rectum. 2005;48(9):1797–1799. doi: 10.1007/s10350-005-0108-7. [DOI] [PubMed] [Google Scholar]
- 33.De Bree E., Zoetmulder F. A., Christodoulakis M., Aleman B. M., Tsiftsis D. D. Treatment of malignancy arising in pilonidal disease. Ann Surg Oncol. 2001;8(1):60–64. doi: 10.1007/s10434-001-0011-y. [DOI] [PubMed] [Google Scholar]


