Abstract
Appendiceal mucocele is a rare disease. Sometimes it is discovered accidentally and sometimes it resembles acute appendicitis. Correct diagnosis before surgery is very important for the selection of adequate surgical treatment to avoid intraoperative and postoperative complications. Ultrasonography, and particularly computed tomography, should be used extensively for this purpose. If mucocele is treated incorrectly pseudomyxoma peritonei, which is characterized by malignant process, may develop. We present a case of a 54-year-old man who was admitted to the emergency department with the signs of acute appendicitis. Open surgery was performed. At the time of surgery, a cystic mass of the appendix with dimensions 7 × 4 ×3 cm, with inflamed walls, but without perforation was discovered in the right iliac fossa. No discharge was found in the peritoneal cavity. Diagnosis of mucocele was suspected. Only appendectomy was performed because no pathologic process was found in the base of the appendix and lymph nodes were not increased in size. Hystopathologic diagnosis was mucinous cystadenoma. After 2 years, the patient is feeling well.
Keywords: Mucocele, Appendix, Mucinous cystadenoma, Appendicitis
Appendiceal mucocele is an obstructive dilatation of the appendix caused by intraluminal accumulation of mucoid material. It is a rare disease. The incidence is 0.2% to 0.7% of all appendectomied specimens.1–4 There are 4 histologic types of appendiceal mucocele: retention cyst, mucosal hyperplasia, mucinous cystadenoma, and mucinous cystadenocarcinoma.5,6
This disease does not have a typical clinical picture. Sometimes the patient has pain in the lower right quadrant of the abdomen, therefore a surgeon may mistaken it for acute appendicitis. This is one of the most common surgical diseases.3,7–9 It is important to differentiate between these two pathologies before surgery and select adequate surgical tactics. If treated improperly, the mucocele may progress, epithelial cells may escape into the peritoneal cavity, and pseudoyxoma peritonei may develop, which has a high mortality.8
We present the case when the 2 diseases were not differentiated before surgery and appendiceal mucocele was diagnosed intraoperatively.
Case Report
A 54-year-old man was referred to the emergency department. His complaints were pain in the right lower quadrant of the abdomen, nausea, and fever. The symptoms started 4 days prior. When palpating the lower right quadrant of the abdomen the patient felt pain, muscles were moderately rigid, and rebound tenderness was noted. Body temperature was 37.5°C. Leukocytosis (11.5 × 109/L) was notable from laboratory test results. Ultrasonography (USG) showed the loops of the intestines puffed up with gases in the right lower quadrant of the abdomen. The patient was diagnosed with acute appendicitis and open surgery was performed. At the time of surgery, a cystic mass of the appendix (7 × 4 × 3 cm), with inflamed walls, but without perforation, was discovered in the right iliac fossa. No discharge was found in the peritoneal cavity. A mucocele was suspected. Only appendectomy was performed because no pathologic process was found in the base of the appendix and the lymph nodes were not increased in size. Hystopathologic diagnosis was mucinous cystadenoma (Figs. 1 to 3). There were no complications in the postoperative period. The patient was released from the clinic on the fourth day. Two years after the surgery the patient is feeling well.
Fig. 1.
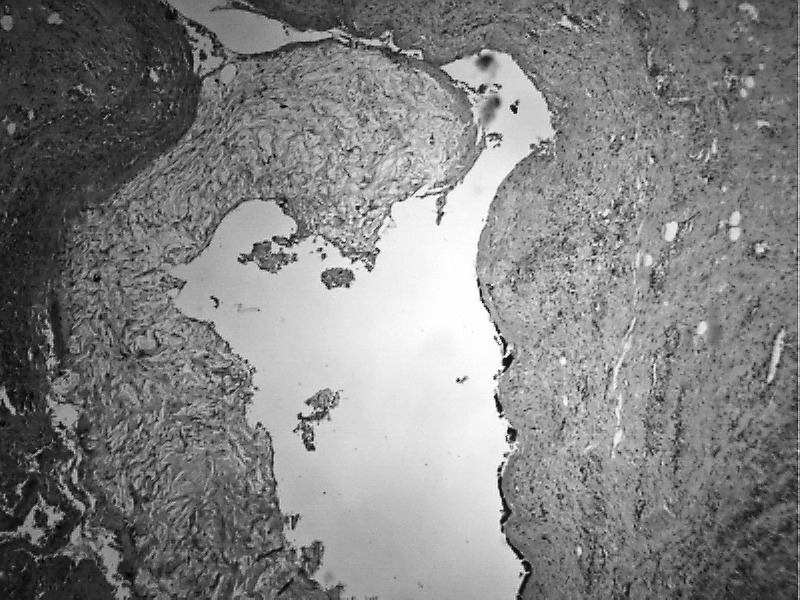
Lumen of the appendix is cystically dilated and contains mucus (hematoxylin and eosin ×100).
Fig. 2.
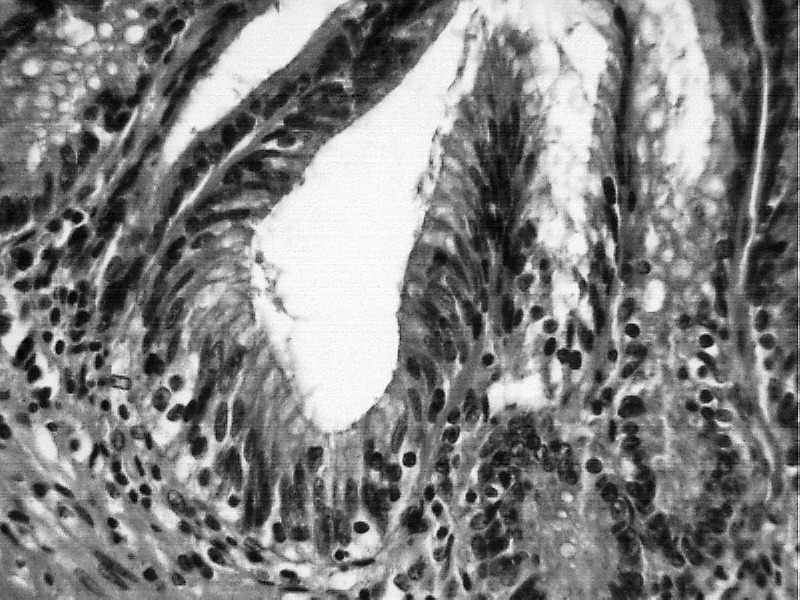
Appendiceal wall is lined with monolayer mucous cylindrical epithelium (hematoxylin and eosin ×400).
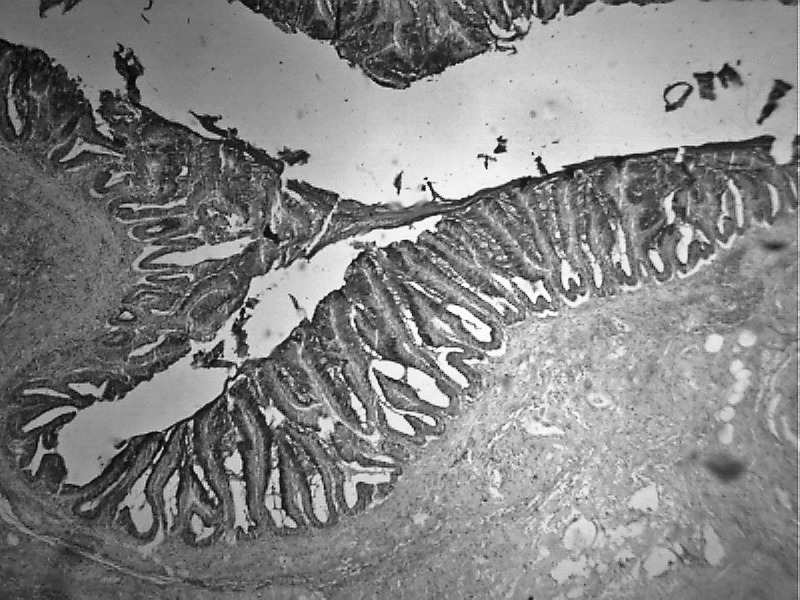
Fig. 3. Mucous epithelium (alcian blue ×200).
Discussion
Mucocele of the appendix was first described by Rokitansky.10 This disease is characterized by dilatation of a lumen as a result of an accumulation of a large amount of mucus. The appendix is lined by epithelium containing more goblet cells than the colon. As a result, most appendiceal epithelial tumors are mucinous and start as mucoceles.11 It falls under the category of rare diseases. Its incidence ranges between 0.2% and 0.7% of all excised appendixes.1–4,9,12 This condition can have benign as well as malignant processes. According to modern classification, there are 4 histologic types: retention cyst, mucosal hyperplasia, mucinous cystadenoma, and mucinous cystadenocarcinoma.5,6
The clinical flow of the disease does not have a specific picture. It often flows asymptomatically. In about 50% of cases it is discovered accidentally during radiologic and endoscopic examinations or at surgery. A patient's clinical symptoms may include pain in the right lower quadrant of the abdomen, palpable abdominal mass, nausea, vomiting, weight loss, gastrointestinal bleeding, and signs of intussusception of the intestines.3,8,9,13–18
Preoperative diagnosis of appendicular mucocele is very important for the selection of an adequate surgical method to prevent peritoneal dissemination, to prevent intraoperative and postoperative complication, and repeated surgery.8,13 USG, computed tomography (CT), and colonoscopy is used for diagnostics. USG is the first-line diagnostic method for patients with acute abdominal pain. USG can be used to differentiate between mucocele and acute appendicitis. In case of acute appendicitis, the outer diameter threshold of the appendix is 6 mm, and 15 mm and more indicates the presence of a mucocele, with 83% sensitivity and 92% specificity.12,19–21 CT is regarded as the most accurate method of diagnostics. CT can be used to discover the signs specific to mucocele with high accuracy: appendix lumen more than 1.3 cm, its cystic dilatation, and wall calcification.3,7,9,17,19,22 By colonoscopy an elevation of the appendiceal orifice is seen and a yellowish mucous discharge would be visible from this orifice. Furthermore, synchronous and metachronous tumors of colon can be identified.3,9,17,23,24 In our patient USG did not provide the correct information; we thought that this was acute appendicitis and did not perform CT. In our opinion, this was a mistake because every patient more than 50 years old who has pain in the right lower quadrant of the abdomen must undergo CT.
One of the cardinal principles of surgical treatment of this disease is that intact mucoceles do not pose a threat for the patient. If it is perforated and the filling turns up in the peritoneal cavity, there is a high probability that pseudomyxoma peritonei will develop, for which treatment is very problematic and long-term results are quite unsatisfactory.8,13,25 Therefore, the selection of an adequate surgical method is very important. Some surgeons think that open surgery should be favored against laparoscopy. If the surgery was launched using a laparoscopic method and it appears that there is an appendiceal mucocele, it must be converted into open surgery. This has 2 objectives: (1) to perform surgery carefully so the cyst is not ruptured and the filling is not scattered into the peritoneal cavity and (2) with an open surgery compared to the laparoscopic method, it is possible to have a fuller inspection, palpation, and direct inspection of the spots in the abdomen where mucinous tumors are most common.8,13,17,26 Some surgeons consider that the operation can be performed using a laparoscopic method by adhering to safety rules, especially when removing the mucocele from the abdomen and an endobag must be used.1,27,28
An algorithm for the selection of the type of surgery has been furnished by Dhage-Ivatury and Sugarbaker.13 It envisages several factors: (1) whether or not a mucocele is perforated; (2) whether the base of the appendix (margins of resection) is involved in the process; and (3) whether there are positive lymph nodes of mesoappendix and ileocolic. As a result patients may require different operations: appendectomy to the right colectomy, including cytoreductive surgery, heated intraoperative intraperitoneal chemotherapy, early postoperative intraperitoneal chemotherapy.13 In our patient the mucocele was not perforated (no discharge into the peritoneum cavity), there was no pathologic process in the base of the appendix (negative margins of resection), and the regional lymph nodes were negative. Therefore, only appendectomy was performed, which is an adequate surgery in such a case. Also, according to the algorithm, no long-term follow-up is advised for our patient.
In conclusion, appendiceal mucocele is a rare disease and has a clinical picture that resembles acute appendicitis. A correct diagnosis before surgery is very important for the selection of surgical technique to avoid severe intraoperative and postoperative complications. USG, particularly CT, should be used extensively for this purpose. In our opinion, every patient more than 50 years old who arrives at the emergency department with clinical symptoms of acute appendicitis must undergo CT and open surgery should be favored against laparoscopic surgery.
References
- 1.Rangarajan M., Palanivelu C., Kavalakat A. J., Parthasarathi R. Laparoscopic appendectomy for mucocele of the appendix. Report 8 cases. Indian J Gastroenterol. 2006;25(5):256–257. [PubMed] [Google Scholar]
- 2.Marudanayagam R., Williams G. T., Rees B. I. Review of the pathological results of 2660 appendectomy specimens. J Gastroenterol. 2006;41(8):745–749. doi: 10.1007/s00535-006-1855-5. [DOI] [PubMed] [Google Scholar]
- 3.Ruiz-Tovar J., Teruel D. G., Gastineires V. M., Dehesa A. S., Quindos P. L., Molina E. M. Mucocele of the appendix. World J Surg. 2007;31(3):542–548. doi: 10.1007/s00268-006-0454-1. [DOI] [PubMed] [Google Scholar]
- 4.Smeenk R. M., van Velthuysen M. L., Verwaal V. J., Zoetmulder F. A. Appendiceal neoplasms and pseudomyxoma peritonei: a population-based study. Eur J Surg Oncol. 2008;34(2):196–201. doi: 10.1016/j.ejso.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Aho A., Heinonen R., Lauren P. Benign and malignant mucocele of the appendix. Acta Chir Scand. 1973;139(4):392–400. [PubMed] [Google Scholar]
- 6.Higa E., Rosai J., Pizzimbono C. A., Wise L. Mucosal hyperplasia, mucinous cystadenoma and mucinous cystadenocarcinoma of the appendix. A re-evaluation of appendiceal mucocele. Cancer. 1973;32(6):1525–1541. doi: 10.1002/1097-0142(197312)32:6<1525::aid-cncr2820320632>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 7.Pickhardt P. J., Levy A. D., Rohrmann C. A., Jr, Kende A. L. Primary neoplasms of the appendix manifesting as acute appendicitis: CT findings with pathologic comparison. Radiology. 2002;224(3):775–781. doi: 10.1148/radiol.2243011545. [DOI] [PubMed] [Google Scholar]
- 8.Sugarbaker P. H. Appendiceal Epithelial Neoplasms and Pseudomyxoma Peritonei, a Distinct Clinical Entity with Distinct Treatments. In: Bland K. J., Büchler M. W., Csendes A., Garden O. Y., Saar M. G., Wong J., editors. General Surgery. Principles and International Practice. London-Limited: Springer; 2009. pp. 885–893. (eds) [Google Scholar]
- 9.Garcia Lozano A., Vazques Tarrago A., Castro Garcia C., Richart Aznar J., Gomez Abril S., Martinez Abad M. Mucocele of the appendix: presentation of 31 cases. Cir Esp. 2010;87(2):108–112. doi: 10.1016/j.ciresp.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 10.Rokitansky C. F. A Manual of Pathological Anatomy. Vol. 2. Philadelphia: Blanchard & Lea; 1855. [Google Scholar]
- 11.Sugarbaker P. H. Epithelial appendiceal neoplasms. Cancer J. 2009;15(3):225–235. doi: 10.1097/PPO.0b013e3181a9c781. [DOI] [PubMed] [Google Scholar]
- 12.Lien W. C., Huang S. P., Chi C. L., Liu K. L., Lin M. T., Lai T. I., et al. Appendiceal outer diameter as an indicator for differentiating appendiceal mucocele from appendicitis. Am J Emerg Med. 2006;24(7):801–805. doi: 10.1016/j.ajem.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 13.Dhage-Ivatury S., Sugarbaker P. H. Update on the surgical approach to mucocele of the appendix. J Am Coll Surg. 2006;202(4):680–684. doi: 10.1016/j.jamcollsurg.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 14.Papaziogas B., Koutelidakis I., Tsiaousis P., Goula O. C., Lakis S., Atmatzidis S., et al. Appendiceal mucocele. A retrospective analysis of 19 cases. J Gastrointest Cancer. 2007;38(2–4):141–147. doi: 10.1007/s12029-008-9030-2. [DOI] [PubMed] [Google Scholar]
- 15.Haritopoulos K. N., Brown D. C., Lewis P., Mansour F., Eltayar A. R., Labruzzo C., et al. Appendiceal mucocele: a case report and review of literature. Int Surg. 2001;86(4):259–262. [PubMed] [Google Scholar]
- 16.Vriens B. H., Klaase J. M. Giant mucinous cystadenoma of the appendix. Am J Surg. 2007;194(3):392–393. doi: 10.1016/j.amjsurg.2006.11.041. [DOI] [PubMed] [Google Scholar]
- 17.Karakaya K., Barut F., Emre A. U., Ucan H. B., Cakmak G. K., Irkorucu O., et al. Appendiceal mucocele: case reports and review of current literature. World J Gastroenterol. 2008;14(14):2280–2283. doi: 10.3748/wjg.14.2280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ashrafi M., Joshi V., Zammit M., Telford K. Intussusception of the appendix secondary to mucinous cystadenoma: a rare cause of abdominal pain. Int J Surg Case Rep. 2011;2(2):26–27. doi: 10.1016/j.ijscr.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Francica G., Lapiccirella G., Giardibello C., Scarano F., Angelone G., De Marino F., et al. Giant mucocele of the appendix: clinical and imaging finding in 3 cases. J Ultrasound Med. 2006;25(5):643–648. doi: 10.7863/jum.2006.25.5.643. [DOI] [PubMed] [Google Scholar]
- 20.Birnbaum B. A., Wilson S. R. Appendicitis at the millennium. Radiology. 2000;215(2):337–348. doi: 10.1148/radiology.215.2.r00ma24337. [DOI] [PubMed] [Google Scholar]
- 21.Sasaki K., Ishida H., Komatsuda T., Suzuki T., Konno K., Ohtaka M., et al. Appendiceal mucocele: sonographic findings. Abdom Imaging. 2003;28(1):15–18. doi: 10.1007/s00261-001-0175-8. [DOI] [PubMed] [Google Scholar]
- 22.Benett G. L., Tanpitukponqse T. P., Macari M., Cho K. C., Babb J. S. CT diagnosis of mucocele of the appendix in patients with acute appendicitis. AJR Am J Roentgenol. 2009;192(3):103–110. doi: 10.2214/AJR.08.1572. [DOI] [PubMed] [Google Scholar]
- 23.Zanati S. A., Martin J. A., Baker J. P., Streutker C. J., Marcon N. E. Colonoscopic diagnosis of mucocele of the appendix. Gastrointest Endosc. 2005;62(3):452–456. doi: 10.1016/j.gie.2005.04.018. [DOI] [PubMed] [Google Scholar]
- 24.Kim-Fuchs C., Kuruvilla Y. C., Angst E., Weimann R., Gloor B., Candinas D. Appendiceal mucocele in an elderly patient: how much surgery? Case report. Gastroenterology. 2011;5(3):516–522. doi: 10.1159/000331438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Misdraji J., Yantiss R. K., Grame-Cook F. M., Balis U. J., Young R. H. Appendiceal mucinous neoplasms. A clinicopathologic analysis of 107 cases. Am J Surg Pathol. 2003;27(8):1089–1103. doi: 10.1097/00000478-200308000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Khan M. R., Ahmed R., Saleem T. Intricacies in the surgical management of appendiceal mucinous cystadenoma: a case report and review of literature. J Med Case Reports. 2010;5(4):129. doi: 10.1186/1752-1947-4-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chiu C. C., Wei P. L., Huang M. T., Wang W., Chen T. C., Lee W. J. Laparoscopic resection of appendiceal mucinous cystadenoma. J Laparoendosc Adv Surg Tech A. 2005;15(3):325–328. doi: 10.1089/lap.2005.15.325. [DOI] [PubMed] [Google Scholar]
- 28.Liberale G., Lemaitre P., Noterman D., Moerman C., de Neubourg E., Sirtaine N., et al. How should we treat mucinous appendiceal neoplasm? By laparoscopy or palarotomy? A case report. Acta Chir Belg. 2010;110(2):203–207. doi: 10.1080/00015458.2010.11680598. [DOI] [PubMed] [Google Scholar]


