Abstract
Periodontal problems due to the use of elastic bands have been documented in the past. A 9-year-old girl reported to a periodontist with complaints of bleeding from gums and tooth mobility of upper right central incisor. This case, reports the early diagnosis and treatment of an acute localized periodontitis arising from the incorrect use of orthodontic elastic rubber bands to close a maxillary midline diastema. The elastic band induced periodontitis was treated with a combination of surgery, splinting, antibiotics and orthodontics. Removal of the etiologic agent improved the condition of the tooth.
Keywords: Periodontal destruction, Bone loss, Tooth mobility, Orthodontic elastic band, Iatrogenic, Periodontitis, Splinting
1. Introduction
Periodontal destruction due to use of elastic bands was first reported in the dentistry way back in 1980s. During different phases of orthodontic treatment, small elastics or rubber bands are used for generating a continuous force to achieve individual tooth movement. Elastics have long been used for the correction of orthodontic problems such as diastema, crossbites, and malposed teeth (Waggoner and Ray, 1989). Elastics are also used for the intentional non-surgical removal of teeth in cases of hemophilia and also in patients treated with bisphosphonates (Regev et al., 2008) or some other anti coagulant medication (Spouge, 1964). As a part of reducing the expenses, many patients choose the use orthodontic rubber bands as a treatment option for closing diastemas (Adcock, 1999). But it is quiet common that the improper use of rubber bands can lead to severe periodontal destruction and tooth loss (Pan et al., 1991; St George and Donachie, 2002). The periodontal destruction caused by orthodontic elastic bands could be iatrogenic (Zilberman et al., 1976). There are only few published reviews of the literature (Vandersall and Varble, 1978) and case studies in the recent years, reporting the effect of orthodontic elastic bands that are retained in the gingival tissues. Periodontal lesions induced by elastic bands are complex to diagnose but have quite a few features in common that may assist in diagnosis and treatment. This could be due to the absence of local etiologic factors, lack of information gathered from the patients and no history of recent trauma or history of orthodontic treatment. Elastic rubber bands because of their elasticity, have a tendency to creep toward the narrower portion of the tooth and the roots, especially when there is no specific attachment mechanisms (Olsen and Pollard, 1998). As the band moves apically, it causes periodontal ligament destruction (Haralabakis et al., 2006), resulting in extrusive movement of the tooth. The elastic band acts as a foreign body resulting in inflammatory reaction in the soft tissues, thereby weakening the periodontal attachments (Regev et al., 2008). Study by Diedrich et al. (2001) reported that the inflammatory reactions close to subgingivally extending rubber bands are independent of the degree of plaque colonization. The granulation tissue that is formed around the root pushes the teeth out of the socket but the bone will not be exposed (Merlini et al., 1983). In some literature, the exfoliation of tooth that results from the periodontal destruction induced by elastic bands is termed as bloodless extraction (Redlich et al., 1997).
The preferred methods of treatment for this situation includes, splinting, flap surgery, elastic band removal and intrusion of the teeth with the help of orthodontic appliance. If indicated endodontic root canal treatment is also considered. Depending on the case, osseous grafting (Caldwell et al., 1980; Finkbeiner et al., 1997) and reimplantation (Finkbeiner et al., 1997) are also being done. In cases where maxillary central incisors with satisfactory prognosis are involved, flap surgeries are usually performed (Caldwell et al., 1980; Pan et al., 1991; Zilberman et al., 1976).
Recent reports by Moghaddas and Pezeshkfar (2010) and Harrington and Darbar (2007) demonstrate the surgical management of localized periodontitis associated with a sub gingival orthodontic elastic bands around a central incisor and upper right first premolar, respectively. The case report by Finkbeiner et al. (1997), describes the successful management of elastic band-induced periodontitis in two children with a combination of laser treatment, antibiotics, splinting and orthodontics. The aim of this report is to present the management of a patient with severe periodontal destruction around the upper right central incisor due to an orthodontic elastic band impeded into the gingiva.
2. Case report
A 9-year-old girl was referred to the author on March 2008. Her chief complaint was pain and mobility of front tooth (upper right central incisor). The patient was reported to have bleeding while brushing, pain and swelling and also mobility for the past 4 months. The dental history revealed orthodontic treatment for closure of diastema by an elastic band. This was done by a general practitioner in June 2007. The treatment was completed in 6 months time.
On clinical examination, there was an abscess with pus discharge in relation to upper right central incisor (#11) (Fig. 1). The tooth showed grade 3 mobility. On percussion the tooth was tender. Deep pockets on all sites were noticed on probing. Probing depths up to 10 mm were recorded. Tooth was vital on pulp testing. The tissues were erythematous, flaccid, and the interdental papillae were markedly enlarged.
Figure 1.

Pre-surgical clinical facial view showing swelling and malaligned #11.
Pre-surgical periapical X-rays were done. On radiographic examination an arc-like severe bone loss was observed around the upper right central incisor (Fig. 2) and also in some areas, an increased radiodensity was noticed. The presence of very deep pockets all around the tooth lead to the provisional diagnosis as severe periodontal destruction in relation to the upper right central incisor (#11) most probably due to the foreign body which could have impeded into the gingiva or it could have been due to trauma.
Figure 2.

Pre-surgical radiograph showing the arch like defect.
Prognosis for tooth #11 was very poor due to severe periodontal destruction (severe bone loss, deep periodontal pockets, grade 3 mobility and severe inflammation).
3. Management
Treatment options were discussed, and the decision to save the tooth was pursued. The parents were informed on the necessity of splinting, periodontal surgery and subsequent orthodontic repositioning of the tooth. The parents were also informed that prognosis of the tooth was poor.
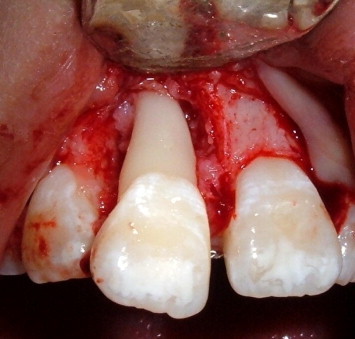
On April 2008 the treatment was initiated. With the consent of the parents, the patient was subjected to periodontal surgery. Under local anesthesia, crevicular horizontal incisions were made on the labial and palatal surfaces of the tooth and were extended to the adjacent teeth to gain more accessibility to the area around #11. Full thickness flaps were reflected and blunt dissection was performed. When the site was surgically exposed, severe periodontal destruction on the facial, mesial, distal and palatal surfaces of the upper right central incisor was observed. An elastic band enveloped within the granulation tissue was observed (Fig. 3). The granulation tissue was curetted; the elastic bands were cut and removed (Fig. 4). Scaling and root planning were also performed. The root surfaces were conditioned with hydrogen peroxide and tetracycline (Fig. 5). As the bone destruction was obvious all around the tooth, bone graft (Bio-Oss® bovine bone graft – Geistlich Pharma AG, Bahnhofstrsse 40, 6110 Wolhusen, Switzerland) mixed with tetracycline was placed into the bony defects this was then covered by a resorbable bilayer membrane (Bio-Gide® collagen membrane – Geistlich Pharma AG, Bahnhofstrsse 40, 6110 Wolhusen, Switzerland). The flaps were sutured back with non-absorbable black silk material (Fig. 6). The tooth was kept splinted to the adjacent teeth from the lingual aspect using a 0.016 by 0.022 in. arch wire (Fig. 7). Post-surgical instructions were given and a soft diet was suggested. Amoxicillin 500 mg every 8 h for 7 days, ibuprofen 200 mg every 6 h and chlorohexidine mouth wash were prescribed. The patient was called for follow up appointment and suture removal after 2 weeks. The patient was asked to report every alternate week in a month for follow up appointments for next 6 months (Fig. 8). Prophylaxis was performed at each appointment and oral hygiene instructions were reinforced. By the end of 6 months all clinical parameters (periodontal pocket depth, bleeding on probing, mobility, etc.) were checked. Tooth was stable and comparatively healthy except for the malalignment. The gingival condition showed an increase in firmness and a reduction of erythema, decrease in probing depth, decrease in bleeding on probing and mobility. The post-surgical radiograph revealed narrowing of the arc-like defects.
Figure 3.
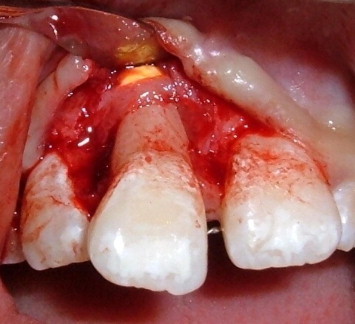
Elastic band exposed on reflecting the flap.
Figure 4.

Elastic band cut and removed.
Figure 5.
Site after cleaning and debridement.
Figure 6.

Flap sutured back after surgery.
Figure 7.

Central incisor fixed to the adjacent teeth from the lingual aspect, 2 months after surgery.
Figure 8.

Clinical facial view 2 months after surgery.
On request by the patient and her parents, she was referred to an orthodontist for a limited orthodontic treatment to align the upper right central incisor. During this period regular follow up visits were maintained every 3 months (Figs. 9 and 10). Alignment of the tooth was achieved at 1 year post-surgical treatment and a comprehensive orthodontic treatment was recommended later. Two years after surgery, patient started a comprehensive orthodontic treatment and is still under treatment. Until now the patient is on a regular review for supporting periodontal therapy and the periodontal condition around the upper right central incisor is stable.
Figure 9.

Post-treatment, clinical facial view, 1 year after surgery, post-limited orthodontic alignment.
Figure 10.

Post-treatment, radiographic view, 1 year after surgery, post-limited orthodontic alignment.
4. Discussion
Rubber elastic bands have long been used for the correction of orthodontic problems such as diastema, crossbites, and malposed teeth (Waggoner and Ray, 1989). This case highlights the advantages of early diagnosis and prompt treatment. The patient showed signs of marginal inflammation and the information so gathered from the case history aided in the early diagnosis of the case. On surgical management the elastic bands within a granulomatous tissue envelope were exposed. The use of osseous graft in this case will definitely aid in bone regeneration. This case clearly illustrates the incorrect management of a transitional diastema in the “ugly duckling” stage of the mixed dentition. In this case, the dentist had used latex elastics to close the diastema for optimal esthetic results which slipped subgingivally. There are a few published articles (Adcock, 1999; Caldwell et al., 1980; Finkbeiner et al., 1997; Olsen and Pollard, 1998; Sanchez-Perez et al., 2006) illustrating the successful retention and management of teeth, affected by periodontitis induced by iatrogenic misapplication of orthodontic elastic bands. The signs of localized periodontal inflammation, such as redness, edema, tooth mobility, and tenderness to percussion, sulcular pus discharge and detailed dental history, will aid in the early diagnosis and management of the tooth before the loss of the tooth occurs. The important point is that foreign bodies should be suspected in patients with localized acute or chronic periodontitis that does not respond to treatment and may show one or more of the following signs and symptoms like pain, rapid onset of deep pocket, increased tooth mobility and extrusion. In such situations, it is suggested to carry out periodontal exploration and surgical intervention, at the earliest. The use of elastics in orthodontics and for intermaxillary fixation is quiet common. Dentists using elastics should be alert to the iatrogenic extraction potential when it is used inappropriately. To prevent the complications with elastic bands, it is better to stabilize it by attachments or bracket, either bonding this directly to the teeth or welding to the orthodontic bands (Diedrich et al., 2001). It is up to the practitioner to reduce the hazard. It is suggested to the manufacturers of orthodontic elastic bands that radiopaque materials should be incorporated into the elastics. This will aid in radiographic diagnosis.
Following the removal of displaced elastic, it is very important to have a multidisciplinary effort by an oral surgeon, periodontist, and orthodontist, in combination with good standards of oral hygiene by the patient, so as to improve the prognosis of the tooth as well as to successfully retain the otherwise damned teeth.
5. Conclusion
The improper use of elastic bands leads to severe periodontal destruction, which may even result in tooth loss. Meticulous clinical and radiographical examination with the detailed dental history is very important in diagnosing the case as well as determining its prognosis. The early diagnosis and proper management of such cases can definitely change the life of the affected teeth. The management of the situation should be planned accordingly. The above case report is one of its kind where the patient has benefited from both early diagnosis as well as correct management.
References
- Adcock J.E. Exfoliation of maxillary central incisors due to misapplication of orthodontic rubber bands. Tex. Dent. J. 1999;116:8–13. [PubMed] [Google Scholar]
- Caldwell C.R., Worms F.W., Gatto D.J. Orthodontic and surgical intervention to arrest tooth loss secondary to subgingival elastic. Am. J. Orthod. 1980;78:273–278. doi: 10.1016/0002-9416(80)90272-9. [DOI] [PubMed] [Google Scholar]
- Diedrich P., Rudzki-Janson I., Wehrbein H., Fritz U. Effects of orthodontic bands on marginal periodontal tissues. A histologic study on two human specimens. J. Orofac. Orthop. 2001;62:146–156. doi: 10.1007/pl00001923. [DOI] [PubMed] [Google Scholar]
- Finkbeiner R.L., Nelson L.S., Killebrew J. Accidental orthodontic elastic band-induced periodontitis: orthodontic and laser treatment. J. Am. Dent. Assoc. 1997;128:1565–1569. doi: 10.14219/jada.archive.1997.0097. [DOI] [PubMed] [Google Scholar]
- Haralabakis N.B., Tsianou A., Nicolopoulos C. Surgical intervention to prevent exfoliation of central incisors from elastic wear. J. Clin. Orthod. 2006;40:51–54. [PubMed] [Google Scholar]
- Harrington Z., Darbar U. Localised periodontitis associated with an ectopic orthodontic separator. Prim. Dent. Care. 2007;14:5–6. doi: 10.1308/135576107779398101. [DOI] [PubMed] [Google Scholar]
- Merlini C., Gallini G., Canzi D. Severe iatrogenic lesions from the improper use of elastics in the correction of inter-incisive diastema. Mondo. Ortod. 1983;8:35–41. [PubMed] [Google Scholar]
- Moghaddas H., Pezeshkfar A. Severe gingival recession caused by orthodontic rubber band: a case report. J. Periodontol. Impl. Dent. 2010;2:83–86. [Google Scholar]
- Olsen C.B., Pollard A.W. Severe bone loss caused by orthodontic rubber bands; management and nine-year follow-up: report of case. ASDC J. Dent. Child. 1998;65:25–28. [PubMed] [Google Scholar]
- Pan W.L., Chan C.P., Su C.P. Localized periodontitis induced by rubber bands. Report of two cases. Changgeng Yi Xue Za Zhi. 1991;14:54–60. [PubMed] [Google Scholar]
- Redlich M., Galun E.A., Zilberman Y. Orthodontic–prosthetic treatment to replace maxillary incisors exfoliated because of improper use of orthodontic elastics: a case report. Quintessence Int. 1997;28:241–244. [PubMed] [Google Scholar]
- Regev E., Lustmann J., Nashef R. Atraumatic teeth extraction in bisphosphonate-treated patients. J. Oral Maxillofac. Surg. 2008;66:1157–1161. doi: 10.1016/j.joms.2008.01.059. [DOI] [PubMed] [Google Scholar]
- Sanchez-Perez A., Moya-Villaescusa M.J., Gambin-Manzano M.C., Bravo-Gonzalez L.A. Loss of a clinical attachment level in a child: differential diagnosis with aggressive periodontitis. Case report. Br. Dent. J. 2006;201:281–282. doi: 10.1038/sj.bdj.4813972. [DOI] [PubMed] [Google Scholar]
- Spouge J.D. Hemostasis in dentistry, with special reference to hemocoagulation. II. Principles underlying clinical hemostatic practices in normal patients. Oral Surg. Oral Med. Oral Pathol. 1964;18:583–592. doi: 10.1016/0030-4220(64)90055-6. [DOI] [PubMed] [Google Scholar]
- St George G., Donachie M.A. Case report: orthodontic separators as periodontal ligatures in periodontal bone loss. Eur. J. Prosthodont. Restor. Dent. 2002;10:97–99. [PubMed] [Google Scholar]
- Vandersall D.C., Varble D.L. The missing orthodontic elastic band, a periodontic–orthodontic dilemma. J. Am. Dent. Assoc. 1978;97:661–663. doi: 10.14219/jada.archive.1978.0354. [DOI] [PubMed] [Google Scholar]
- Waggoner W.F., Ray K.D. Bone loss in the permanent dentition as a result of improper orthodontic elastic band use: a case report. Quintessence Int. 1989;20:653–656. [PubMed] [Google Scholar]
- Zilberman Y., Shteyer A., Azaz B. Iatrogenic exfoliation of teeth by the incorrect use of orthodontic elastic bands. J. Am. Dent. Assoc. 1976;93:89–93. doi: 10.14219/jada.archive.1976.0628. [DOI] [PubMed] [Google Scholar]


