Abstract
The constant quest for finding the ultimate esthetic dental restorative material has led to numerous alternatives. These materials, in addition to possessing optical properties simulating natural teeth, should also have physical properties that can withstand the harsh oral environment. Due to their greater toughness, zirconium oxide materials have been used as a core material for all-ceramic restorations.
Objective
The objective of this study was to evaluate the resin-composite micro-shear bond strength to zirconia using different techniques of surface treatment.
Materials and methods
Fully sintered zirconia (LAVA, 3M-ESPE, Seefeld, Germany) discs were used in combination with resin-composite (Filtek Supreme, 3M-ESPE, Seefeld, Germany) discs and divided into four groups of surface treatments. The micro-shear bond strength was measured by applying an axial load on the bonded interface until failure occurred. Failure load (N) was determined and the samples were examined under a SEM and the failure type was identified. One-way analysis of variance (ANOVA) was used to analyze the data with the level of significance α = 0.05.
Results
Data analysis revealed significant difference between the different tested surface treatments with the group using sandblasting and coated with an experimental primer showing the highest failure load and a cohesive fracture pattern.
Conclusion
Within the limitations of this in vitro study the use of an experimental primer achieved a better bond strength in combination with air-abrasion particles.
Keywords: Zirconia, Micro-shear bond strength
1. Introduction
A need for non-metallic restorative materials with optimal esthetics and characteristics such as biocompatibility, colour stability, high wear resistance and low thermal conductivity is often stated as a reason for the use of ceramics in dentistry (Vult Von Steyern et al., 2001; Oden et al., 1998). Various materials can be used as all-ceramic core materials such as leucite-reinforced ceramics, glass-infiltrated ceramics, lithium disilicate, alumina and zirconia (Aboushelib et al., 2007).
The greater toughness of zirconium oxide ceramics compared to that of aluminum oxide ceramics has made zirconia a favorite choice as core material for all-ceramic restorations (Christel et al., 1989). In contrast to conventional felspathic ceramics, the matrix pressure on the tetragonal particles of zirconium oxide is reduced by tensile stresses that induce a transformation of the tetragonal to a monoclinic phase, known as the transformation-toughening property. This property is associated with a localized volumetric increase of 3–5% resulting in compressive stresses that counteract the external tensile stresses and, in this way, may prevent cracks from propagating (Christel et al., 1989; Luthardt et al., 2002).
Due to their chemical inertness, zirconia frameworks are resistant to aggressive chemical agents such strong acids as hydrofluoric acid (Derand and Derand, 2000), alkalis, and organic and inorganic dissolving agents. Other techniques which are based on increasing their surface roughness failed to establish a strong and durable bond with adhesive resin cements. Different investigations have examined and measured the shear bond strength of different cements on zirconium oxide ceramic surface after different pre-treatments. These studies provide varying and controversial results (Derand and Derand, 2000; Blatz et al., 2004; Wegner and Kern, 2000; Piwowarczyk et al., 2005).
Several coating agents were used to enhance the formation of chemical bonding with zirconia and only those agents that contain a phosphate monomer agent (MDP) were effective in establishing a reliable bond with zirconia materials (Blatz et al., 2004; Wegner and Kern, 2000).
In a recent study, application of MDP monomer on non-retentive (as-sintered) zirconia surface failed to produce any bond with zirconia as most of the specimens demonstrated premature failure which questions the role of this MDP agent (Aboushelib et al., 2008).
Focusing on the long-term zirconia resin bond stability, a recent study shows that it is directly related to the chemistry of the used materials, including primers. The authors suggested that a more hydrophobic compound is required to better resist the detrimental effect of hydrolysis in order to gain full benefit from the used primers (Aboushelib et al., 2009).
As a novel approach to enhance zirconia resin bond strength, selective infiltration-etching (SIE) of zirconia-based materials was introduced to create a retentive surface where the adhesive resin can infiltrate and interlock in order to establish a strong and a durable bond with zirconia (Aboushelib et al., 2007).
The micro-shear bond test method for measuring bond strength was introduced (Mcdonough et al., 2002). Compared with the conventional shear bond test, the stress distribution is more concentrated at the interface in the micro-shear bond test (Banomyong et al., 2007) which reduces the chance of cohesive failure in the material that does not represent the “true” interfacial bond strength.
The aim of this study was to evaluate the resin-composite micro-shear bond strength to zirconia using different techniques of surface treatment. The null hypothesis tested was that there was no difference between different surface treatments on bond strength of resin-composite to zirconia.
2. Materials and methods
2.1. Preparation of the specimens and bonding procedure
Fully sintered zirconia (LAVA, 3M-ESPE, Seefelf, Germany) discs (19.5 mm × 3 mm) were used in combination with resin-composite (Filtek Supreme, 3M-ESPE, Seefeld, Germany) discs (2 mm × 2 mm) and were divided into four groups as follows:
Group 1 (Control): Ten resin-composite discs (n = 10) were bonded on top of the surface of the zirconia disc using a self-cured resin-composite cement (Multilink, Ivoclar-Vivadent, Schaan, Liechtenstein) under a fixed load of 20 N. Excess cement was wiped off using microbrush.
Group 2: n = 10: Same procedure as that for Group 1 but zirconia disc was sandblasted with 120 μm aluminum oxide particles (S-U-Alustral, Schuler-Dental, Ulm, Germany) at 0.35 MPa pressure prior to bonding procedures.
Group 3: n = 10: Same procedure as that for Group 2 but the sandblasted zirconia disc was coated with adhesive agent (Multilink primers A and B) prior to bonding procedures.
Group 4: n = 10: Same procedure as that for Group 2 but the sandblasted zirconia disc was coated with an experimental primer as described by Aboushelib et al. (2008) (The silane monomers used in the primers were 3-acryloyloxypropyltrimethoxysilane, 3-isocyanatopropyltriethoxysilane, styrylethyltrimethoxysilane, 3-methacryloyloxypropyltrimethoxysilane and 3-(N-allylamino)propyltrimethoxysilane.) prior to bonding procedures.
2.2. Testing procedure
The micro-shear bond strength was measured by applying an axial load on the bonded interface using a universal testing machine (Accuforce Elite Test Stand, Ametek, Mansfield & Green Division 8600 Somerset Drive Largo, Florida, USA). Loading was performed at a crosshead speed of 1 mm/min until failure occurred.
Failure load (N) was extracted from the computer-generated data files.
The broken resin discs and zirconia discs were ultrasonically cleaned, dried, gold sputter coated and examined under a SEM (JEOL JSM-6360LV, Japan) and failure type was classified into interfacial failure across the zirconia–resin interface resulting in exposure of the zirconia surface or cohesive failure in the composite material or the adhesive resin.
One-way analysis of variance (ANOVA) was used to analyze the data with the level of significance α = 0.05. The Kolmogorov–Smirnov post-hoc test was used and showed normal distribution.
3. Results
Data analysis revealed significant differences with regard to the mean micro-shear bond strength values measured in MPa units between Groups 1, 2 and 3 (Table 1), while significant difference was noted between the previous groups and Group 4 (F = 25.683, P < 0.001). No significant difference was noted between Groups 2 and 3 (P > 0.001).
Table 1.
Micro-shear bond strength of different tested groups (MPa).
| Group | MSBS (MPa) | SD |
|---|---|---|
| 1A | 11.72 | 4.3 |
| 2B | 20.87 | 7.5 |
| 3B | 22.61 | 7.9 |
| 4C | 34.54 | 10.8 |
Similar superscripts indicate no significant difference (MSBS = Micro-shear bond strength).
SEM observations of the specimens showed predominant interfacial failure type especially in Groups 1, 2 and 3 while in Group 4, there was a predominant cohesive failure type between the adhesive cement and the resin-composite (Fig. 1).
Figure 1.
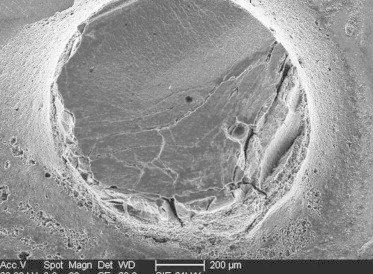
Representative sample of disc from Group 4 demonstrating the cohesive type of failure between the adhesive cement and the resin-composite.
4. Discussion
The results of this study led to the rejection of the null hypothesis tested that there was no significant difference in bond strength between the tested groups.
One of the most common methods for evaluating the adhesive properties of restorative materials is bond strength measurement (Sano et al., 1994; Shimada et al., 2002). Since the development of the micro-tensile bond strength test by Shimada et al. (2002) many micro-bond tests were performed showing the effective method in testing small areas of tooth structure (Senawongse et al., 2004). Micro-shear bond strength allows for straightforward sample preparation giving precise results preserving the uniformity of the testing area (Sano et al., 1994; Kanemura et al., 1999; Senawongse et al., 2004).
The low bond strength obtained in Group 1 (lowest value) with no treatment of the zirconia surface was in agreement with the results reported by other studies (Bottino et al., 2005). Such findings indicated that establishing a strong chemical bond with zirconia is a difficult procedure for MDP-containing resins when not combined with airborne particle abrasion as a recommended surface pre-treatment.
The use of sandblasting as surface treatment increased bond strength indicating that mechanical retention is necessary to gain benefit for MDP resin-composite as reported in a previous study (Amaral et al., 2006), while the combination of sandblasting with bonding agent coating the zirconia disc showed no difference with only sandblasted specimens.
Results of this in vitro study showed that the highest value was observed in Group 4 where the experimental primer was used. This can be explained by the presence of organo functional silanes in the primer composition and their chemical reactivity with the sandblasted zirconia surface enhancing the adhesion between MDP-cement and the treated surface.
SEM observation revealed that in the group using the experimental primer, the predominant failure type was cohesive in the composite material or the adhesive resin. This can be explained by the better adhesion obtained with the novel primer, while the failure type observed in the other groups was more of interfacial type due to the weak bond achieved.
5. Conclusion
Within the limitations of this in vitro study the use of an experimental primer achieved a better bond strength in combination with air-abrasion particles. Further studies are needed to evaluate the optimal zirconia surface treatment in order to enhance the use of bonded-zirconia restorations clinically.
References
- Aboushelib M.N., Kleverlaan C.J., Feilzer A.J. Selective infiltration-etching technique for a strong and durable bond of resin cements to zirconia-based materials. J. Prosthet. Dent. 2007;98:379–388. doi: 10.1016/S0022-3913(07)60123-1. [DOI] [PubMed] [Google Scholar]
- Aboushelib M.N., deJager N., Kleverlaan C.J., Feilzer A.J. Effect of loading method on the fracture mechanics of two layered all-ceramic restorative systems. Dent. Mater. 2007;23:952–959. doi: 10.1016/j.dental.2006.06.036. [DOI] [PubMed] [Google Scholar]
- Aboushelib M.N., Matinlinna J.P., Salameh Z., Ounsi H.F. Innovations in bonding to zirconia-based materials: Part I. Dent. Mater. 2008;24:1268–1272. doi: 10.1016/j.dental.2008.02.010. [DOI] [PubMed] [Google Scholar]
- Aboushelib, M.N., Mirmohamadi, H., Matinlinna, J.P., Kukk, E., Ounsi, H.F., Salameh, Z., 2009. Innovations in bonding to zirconia-based materials Part II: Focusing on chemical interactions. Dent. Mater. March 24 (Epub ahead of print). [DOI] [PubMed]
- Amaral R., Ozcan M., Bottino M.A., Valandro L.F. Microtensile bond strength of a resin cement to glass infiltrated zirconia-reinforced ceramic: the effect of surface conditioning. Dent. Mater. 2006;22:283–290. doi: 10.1016/j.dental.2005.04.021. [DOI] [PubMed] [Google Scholar]
- Banomyong D., Palamara J., Burrow M.F., Messer H.H. Effect of dentin conditioning on dentin permeability and micro-shear bond strength. Eur. J. Oral. Sci. 2007;115:502–509. doi: 10.1111/j.1600-0722.2007.00483.x. [DOI] [PubMed] [Google Scholar]
- Blatz M.B., Sadan A., Martin J., Lang B. In vitro evaluation of shear bond strengths of resin to densely-sintered high-purity zirconium-oxide ceramic after long-term storage and thermal cycling. J. Prosthet. Dent. 2004;91:356–362. doi: 10.1016/j.prosdent.2004.02.001. [DOI] [PubMed] [Google Scholar]
- Bottino M.A., Valandro L.F., Scotti R., Buso L. Effect of surface treatments on the resin bond to zirconium-based ceramic. Int. J. Prosthodont. 2005;18:60–65. [PubMed] [Google Scholar]
- Christel P., Meuniere A., Heller M., Torre J.P., Peille C.N. Mechanical properties and short-term in vivo evaluation of yttrium-oxide partially stabilized zirconia. J. Biomed. Mater. Res. 1989;23:45–61. doi: 10.1002/jbm.820230105. [DOI] [PubMed] [Google Scholar]
- Derand P., Derand T. Bond strength of luting cements to zirconium oxide ceramics. Int. J. Prosthodont. 2000;13:131–135. [PubMed] [Google Scholar]
- Kanemura N., Sano H., Tagami J. Tensile bond strength to and SEM evaluation of ground and intact enamel surfaces. J. Dent. 1999;27:523–530. doi: 10.1016/s0300-5712(99)00008-1. [DOI] [PubMed] [Google Scholar]
- Luthardt R.G., Holzhuter M., Sandkuhl O., Herold V., Schnapp J.D., Kuhlisch E., Walter M. Reliability and properties of ground Y-TZP-Zirconia ceramics. J. Dent. Res. 2002;81:487–491. doi: 10.1177/154405910208100711. [DOI] [PubMed] [Google Scholar]
- Mcdonough W.G., Antonucci J.M., He J., Shimada Y., Chiang M.Y.M., Shumacher G.E., Schultheisz C.R. A microshear test to measure bond strengths of dentin–polymer interfaces. Biomaterials. 2002;23:3603–3608. doi: 10.1016/s0142-9612(02)00089-3. [DOI] [PubMed] [Google Scholar]
- Oden A., Andersson M., Krystek-Ondracek I., Magnusson D. Five-year clinical evaluation of AllCeram crowns. J. Prosthet. Dent. 1998;80:450–456. doi: 10.1016/s0022-3913(98)70010-1. [DOI] [PubMed] [Google Scholar]
- Piwowarczyk A., Lauer H.C., Sorensen J.A. The shear bond strength between luting cement and zirconia ceramics after two pre-treatment. Oper. Dent. 2005;30:382–388. [PubMed] [Google Scholar]
- Sano H., Shono T., Sonoda H., Takatsu T., Ciucchi B., Carvalho R., Pashley D.H. Relationship between surface area for adhesion and tensile bond strength. Evaluation of a micro-tensile bond test. Dent. Mater. 1994;10:236–240. doi: 10.1016/0109-5641(94)90067-1. [DOI] [PubMed] [Google Scholar]
- Senawongse P., Sattabanasuk V., Shimada Y., Otsuki M., Tagami J. Bond strength of current adhesive systems on intact and ground enamel. J. Esthet. Restor. Dent. 2004;16:107–115. doi: 10.1111/j.1708-8240.2004.tb00016.x. [DOI] [PubMed] [Google Scholar]
- Shimada Y., Yamaguchi S., Tagami J. Micro-shear bond strength of dual-cured resin cement to glass ceramics. Dent. Mater. 2002;18:380–388. doi: 10.1016/s0109-5641(01)00054-9. [DOI] [PubMed] [Google Scholar]
- Vult Von Steyern P., Jonsson O., Nilner K. Five-year evaluation of posterior all-ceramic three-unit (In-Ceram) FPDs. Int. J. Prosthodont. 2001;14:379–384. [PubMed] [Google Scholar]
- Wegner S.M., Kern M. Long-term resin bond strength to zirconia ceramic. J. Adhes. Dent. 2000:139–147. [PubMed] [Google Scholar]


