Abstract
Aims
To provide a comprehensive integration of contemporary studies focusing on the relationship between obesity and asthma in paediatric populations.
Background
The simultaneous increase in asthma and obesity prevalence has been widely discussed over the past twenty years. Although studies have discovered a positive correlation between the two, evidence-based findings are needed to develop nursing interventions.
Data Sources
An electronic database search was conducted for studies published between January 1966 - May 2011. Additional articles were identified through the reference lists of reviewed papers.
Review Methods
A quantitative systematic review was undertaken to aggregate evidence regarding the association between obesity and asthma in children. Inclusion/exclusion criteria and quality appraisal were applied to ensure research primarily designed to study the relationship between obesity and asthma in children was included.
Results
The majority of studies support a positive association between obesity and asthma in children. Among correlates recognized as important effect modifiers, gender was the most prominent, with obese girls more likely to have asthma diagnoses than obese boys. Scrutinization of covariates in selected studies revealed that most related to children's demographic characteristics and were inconsistent across the studies.
Conclusions
This review was designed to integrate contemporary scientific findings on the association between obesity and asthma by including a large number of studies with variant research designs. To identify high-risk groups and develop nursing interventions to help children affected by both epidemics, more interdisciplinary and well-designed investigations focusing on an expanded spectrum of correlates including demographic and behavioural factors are warranted.
Keywords: body mass index (BMI), asthma, obesity, overweight, children, systematic review, nursing
Introduction
A concurrent increase in both obesity and asthma among children has been identified worldwide over the past two decades (Chinn & Rona 2001, Wickens et al. 2005), especially in developed countries. In the US, the prevalence of childhood asthma has increased from 3.5% in 1980 - 9.6% in 2009 (Moorman et al. 2007, Zahran et al. 2011). Also, the number of overweight and obese children has also risen significantly over the past twenty years (Ogden et al.2006). According to a recent nationwide survey targeting 0-17 year olds in the USA, nearly 25% and 13% were obese and diagnosed with asthma, respectively. Obesity was significantly associated with asthma especially among children aged 13-17 (Ahmad et al. 2009).
Due to the simultaneous increasing prevalence of both asthma and being overweight or obese, their association has been widely discussed as an area where further inquiry is needed (Beuther 2009). Several studies have reported an association between asthma and being overweight or obese, in both adult and paediatric populations (Chinn 2003). Both cross-sectional (von Kries et al. 2001) and longitudinal (Castro-Rodriguez et al. 2001, Gilliland et al. 2003) studies have revealed positive correlations between asthma and obesity. Some prospective studies support the hypothesis that obesity leads to an increased risk of asthma among children and adults (Burgess et al. 2007, Gilliland et al. 2003). Furthermore, scientists have found that loss of body weight significantly reduced asthma-related symptoms (Eneli et al. 2008).
Although scientists have reviewed studies synthesizing evidence regarding the relationship between asthma and obesity (Beuther et al. 2009), the results from studies conducted with paediatric populations yielded more inconsistent results than those from adult populations (Ford 2005). One meta-analysis focusing on children with asthma concluded that children with high body weight in their early lives (birth weight, high BMI in 10th grade) were more likely to have future asthma even in adulthood. This meta-analysis searched studies from Medline from 1966 until 2004, but excluded all cross-sectional or case-control research and only included 12 longitudinal studies (Flaherman & Rutherford 2006). Synthesizing results from longitudinal studies only provides evidence-based insight regarding causal pathways or mechanisms; however, retrieving and expanding the synthesis to include all relevant studies could extend our insight into important potential confounding factors. A review was conducted recently but only included studies published up to January 2009 and the target population was limited to adolescents (Eneli et al. 2008). With the rapidly accumulating evidences of studies in this area, a more updated systemic review is needed to explore our knowledge and develop theory-based nursing interventions.
The Review
Aim
This review was designed to explore the relationship between asthma and obesity in children by searching studies from January 1966 up to May 2011 and incorporating research findings from publications with a variety of designs. To generate findings comparable to other published reviews (Beuther 2009, Noal et al. 2011), this review includes studies that examined the correlation between asthma prevalence and overweight/obesity as defined by BMI index in children by aggregating evidence from an in-depth analysis of included studies, summarizing shared characteristics and identifying the common confounding or influential factors reported in each investigation. By conducting this review, a comprehensive integration of contemporary studies focusing on the relationship between obesity and asthma in paediatric populations is provided.
Design
The main purpose of this report is to explore the relationship between asthma and obesity in children. The clinical nature of this issue is best resolved by collecting relevant evidence from primary studies in a systematic review (Counsell 1997). Therefore, a quantitative systematic review of the literature was performed following the guidelines published by Centre for Reviews and Dissemination (2009).
Search methods
Before the online literature search process began, two authors met to set up the inclusion and exclusion criteria. Then a two-step selection process was conducted. First, the primary author independently implemented the search strategy across four online databases. Second, after reviewing all the titles and select abstracts, chosen articles were listed and printed for further evaluation by the primary author. Consultation with other two authors determined final eligibility of retrieved articles.
The inclusion criteria for target studies were: (a) research stated that it was primarily designed to examine the relationship between obesity as defined by body mass index (BMI) and asthma diagnosis confirmed by parent/self-reports or/and objective measurements; (b) the target population of the research was children aged 0-18; (c) research was published in English. Exclusion criteria were: (a) case reports, meta-analyses, or systemic review articles that did not adopt a research design; (b) research had no clear definition of childhood overweight or obesity using body mass index (BMI); (c) neither asthma diagnosis nor overweight/obese status was the primary research exposure or outcome. Eligible articles were retrieved from four electronic databases: Pubmed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), The Cochrane Library and Medline. Each of the following keywords: ‘overweight’, ‘obesity’, ‘body mass index’, ‘body weight’ and ‘anthropometry’ were searched concurrent with ‘asthma’. The earliest year surveyed in Medline was 1966 with the final literature checked May, 2011. Additional eligible articles were identified by manually checking the reference lists of included studies.
Search outcome
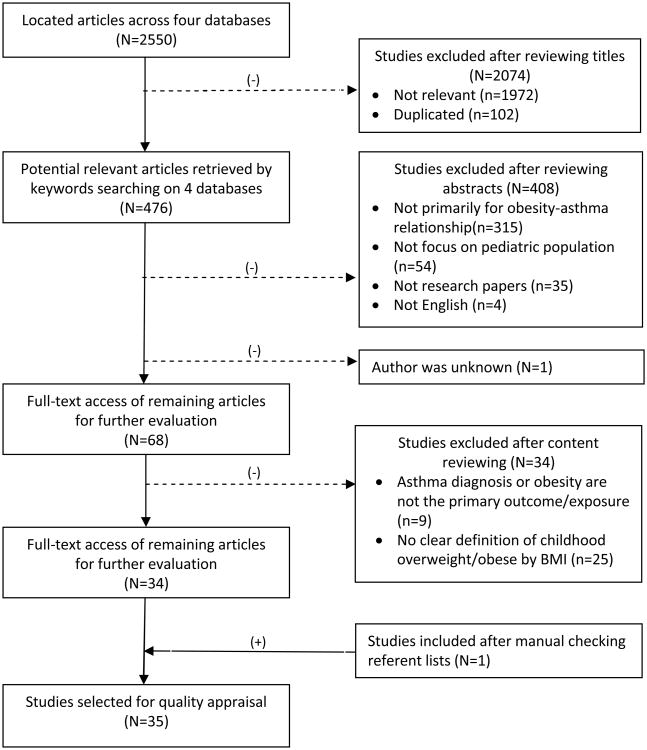
The initial search strategy identified 2550 articles across the four databases. After title review, 2074 reports were excluded as irrelevant or duplicates. Abstract review further ruled out 408 papers that did not meet the inclusion criteria. Most studies were deleted because they were not designed ‘primarily’ to explore the relationship between asthma and obesity. For example, asthma and body mass index (BMI) were co-factors in two studies focusing on the effect of breastfeeding on both asthma and obesity (Mai et al. 2007, Oddy et al. 2004) while the focus of another report was the response to an asthma-specific disease management program of 174 children some of whom were obese (Kwong et al.2006). Other studies were excluded because the majority of study subjects were not children (Chen et al. 2005), or the child subjects had other health concerns (Mai et al. 2004). The full-texts of the remaining 68 articles were accessed online or through the printed publications in the National Taiwan University library or by online transmission from the interlibrary system at the University of Washington. After careful content reading, nine studies were further excluded as asthma or obesity was not the primary outcome or exposure measure including those studies only adopting asthma-related symptoms such as wheezing (Saldiva et al. 2007) or airway hyperresponsiveness (Jang et al. 2006) to validate the asthma diagnose. Twenty-five more studies were ruled out because they failed to clearly define being overweight or obese with BMI cutoff points. After manually checking the references of all the selected papers, one more article was retrieved and included (Rodriguez et al. 2002). Thus, finally a total of 35 studies were included in this review. The detailed process for selection of eligible publications is outlined in Figure 1.
Figure 1. Selection process of included studies.
Quality appraisal
A quality appraisal and validity assessment tool was adapted from previously published review articles (Cummings et al. 2008, Estabrooks et al. 2001, Wulff et al. 2011). Twelve items representing the four major characteristics (research design, samples, measurement and statistical analysis) of each selected study were evaluated. This tool was originally a numeric scale and a total score assigned to each study representing its quality level. However, distinguishing high or low quality studies by using the summary scores is not recommended by Centre for Reviews and Dissemination (2009) and the Cochrane Handbook for Systematic Reviews (Higgins et al. 2011). Therefore, each item was coded as ‘Y’ (yes), ‘N’ (no) or ‘P’ (partial) instead of a total score. The content of the quality appraisal tool and the description of the appraisal results were listed in Table S1 and S2 (see supplementary files in the online version of this article). Two primary authors independently evaluated the quality of selected studies and 80% agreement was achieved.
Data extraction and synthesis
A predefined review matrix was applied to retrieve and organize relevant data from selected reports (Garrard 2007). The primary author then independently extracted and listed each the design/objective, sample size, target population, exposure and outcome indicators, confounding factors, statistical methods and conclusion of each piece of research. After consulting with the other two authors to resolve difficulties in synthesizing or interpreting data, the most common items in selected studies such as study population, asthma and obesity definitions, confounding factors and main study results were listed in separate tables for further analysis and comparison.
Results
Study characteristics
Publication years and recruited sample
More than half of the reviewed articles were published within 7 years (2005-2011). Most of the studies were conducted in the United States (almost 40% of the selected publications). Only a small proportion of studies were from non-western developed countries; three were from Asia (He et al.2009, Leung et al.2009, Yoo et al. 2011) and one was from Israel (Bibi et al.2004). Due to the broad inclusion criteria for study design, 31 were cross-sectional studies and 5 were longitudinal studies.
The developmental stage of the populations recruited in selected studies covered all paediatric age groups from infants (Rodriguezet al. 2002), preschoolers (Vargas et al. 2007) to adolescents (Gennuso et al. 1998, Hasan et al. 2006). A combined school-age and adolescence population was most frequent, but five studies mainly recruited adolescents (Bertolace et al. 2008, Bidad et al. 2007, Cassol et al. 2006, Hasan et al. 2006, Leung, et al. 2009). The numbers of subjects analyzed in each study varied greatly. The smallest number of subjects was 94 children in a case-control designed study led by Henkin et al. (2008). The study with the largest sample (N=102,273) was conducted by Ahmad et al. (2009) in the US.
Several studies used data originally collected for other large-scale surveys (Epstein et al. 2000, Sithole et al.2008, Vahlkvist & Pedersen 2009). Although, a large number of subjects and data can be withdrawn through those national-wide databanks, none of them were designed primarily for examination of the relationship between children asthma and obesity. And many of them completed subject recruiting procedures more than 10 years ago (Belamarich et al. 2000, Figueroa-Munoz et al. 2001, von Mutius et al. 2001).
Definitions of childhood asthma and obesity
The heterogeneity regarding the asthma definitions was noticed in different studies. The majority adopted a parent/self -report of physician-diagnosed asthma as a confirmative indicator of asthma diagnosis. About one third of included research provided objective measurement(s) to confirm asthma such as FEV1 (Forced Expiratory Volume in 1 sec), FVC (Forced Vital Capacity), FEF25-75% (Forced expiratory flow25-75%) and peak expiratory flow rate (PEFR) (Gilliland et al. 2003, Luder et al.1998). Others looked for allergic manifestations by collecting results from bronchial or airway hyper-responsiveness testing (BHR or AHR) (Bibi et al. 2004) or serum lipid profile and IgE level (Leung et al. 2009). In addition, some studies gathered indicators representing asthma severity such as emergency room visits; school days missed, or rescue medication usage to capture a more thorough picture of the children's asthma severity (Belamarich et al. 2000, Bibi et al. 2004, Jacobson et al. 2008, Vargas et al. 2007).
Though there was heterogeneity regarding the definition of childhood obesity across reviewed studies, half of them agreed that the 85th and 95th BMI percentiles were applicable cutoff points to identify overweight/obese children. Children were labeled as ‘overweight’ or ‘risk for overweight’ while their BMI were between 85th and 95th percentiles and ‘obese’ or ‘overweight’ while their BMI were beyond the 95th percentile (Gilliland et al. 2003, Luder et al. 1998).
Relationship between asthma and obesity
Positive association between asthma and obesity
Among the 35 studies included, 27 reports found a positive association between overweight/obesity with asthmatic symptoms. The positive association was confirmed across the whole paediatric age spectrum. Overweight or obese children were found 1.16-6.8 times more likely to have or develop new asthmatic symptoms compared with normal weight children (Castro-Rodriguez et al. 2001, Gilliland et al.2003). The majority of the studies adopted a cross-sectional design (N = 31). Among these, 24 confirmed the positive relationship between childhood obesity and asthma (Table 1). Three of four longitudinal studies also concluded that higher BMI during early childhood predicted future incidence of newly-diagnosed asthma or asthma-like symptoms (Table 2).
Table 1. Cross-sectional studies (N=31).
| Author/population | Definition of | Confounding factors | Main result | |
|---|---|---|---|---|
| Obesity | Asthma | |||
| Ahmad, 2009/N=102,273; 0-17yr; USA | Overweight: BMI ≥85th<95th Obese: BMI≥95th |
Subjective: Parental-report of children ever diagnosed asthma by physician Objective: None |
Age, gender, ethnicity, educational level of family, family structure, poverty level, health insurance, ETS |
|
| Belamarich, 2000/N=1322; 4-9yr; USA | Nonobese: BMI>5th <95th Obese: BMI≥95th |
Subjective: Parental-report of asthma dx by doctor, wheezing episodes, PEFR, emergency visits(EDs) Objective: PEFR |
Age, gender, family income, caretaker's mental health, environmental tobacco smoke (ETS) |
|
| Bertolace, 2008/N=421;15-16yr; Brazil | Overweight: BMI≥85th<95th Obese: BMI≥95th |
Subjective: Self-report of asthma diagnosis or asthmatic symptoms (ISSAC questionnaire) Objective: None |
Age, gender, race, social position, location of residency | No significant positive association between increased BMI and the prevalence of asthma (p=.076). |
| Bibi, 2004/N=5984; around 8yr; Israel | Overweight: None Obese: BMI≥95th |
Subjective: Parental-report of children ever diagnosed asthmatic by a physician Objective: FEV1, FVC, AHR test |
Age, gender, parental education and smoking habits, family crowdedness |
|
| Bidad, 2007/N=2900;11-17yr; Iran | Overweight: BMI≥85th<95th
Obese: BMI≥95th |
Subjective: Self-report of asthma diagnose while interviewed by trained physician Objective: None |
Age, gender, physical scores, waist/hip circumstances, waist-to-hip ratio, gastroesophageal reflux disease hx |
|
| Cassol, 2006/N=4010; 13-14yr; Brazil | Nonobese: BMI<85th and triceps skinfold thickness<85th) Obese: BMI≥85th and triceps skinfold thickness ≥85th |
Subjective: Self-report of wheezing or asthma attacks in the previous year (ISAAC questionnaire)questionnaire Objective: None |
Age, gender |
|
| Epstein, 2000/N=5154;6-16yr; USA | Obese: BMI≥85th | Subjective: Parental-report of children ever diagnosed asthma by a physician Objective: None |
Age, gender, race/ethnicity, TV watching time, family income |
|
| Figueroa-Munoz, 2001/N=14908;4-11y; England/Scotland | Obese: BMI≥90th | Subjective: Parental-report of asthma and asthmatic symptoms Objective: None |
Age, gender, ethnicity, family size, father's social class, living region, ETS | BMI and sum of skinfolds were strongly and significantly associated with each of the asthma outcomes in girls only among inner city samples (OR=1.28, 95% CI: 1.11-1.48) |
| Gennuso, 1998/N=171;4-16yr; USA | Obese: BMI≥85th <95th Very obese: BMI≥95th |
Subjective: None Objective: Medical record review for asthma dx |
Age, gender, ethnicity | Significantly more children with asthma were obese (30.06%) compared with controls (11.6%) (p=.004). |
| Hasan, 2006/N=109; 13-18yr; USA | Overweight: BMI≥85th Obese: None |
Subjective: Self-report of asthma symptoms Objective: Asthma dx confirmed by FEV1, FVC |
Age, gender, ethnicity | Children with asthma almost 1.5 (RR=1.49, 95% CI: 1.015-2.17) times more likely to be overweight compared with children without asthma. |
| He, 2009/N=2179; 8-13yr; China | Overweight: BMI≥85th<95th Obese: BMI≥95th |
Subjective: Parental-report of children ever been diagnosed w/asthma by physicians Objective: FEV1, FVC, FEF25, FEF75, FEF25-75 |
Age, gender, allergy hx, physical activity, parental smoking and allergy | Overweight or obese was positively associated with asthma with significant statistical level (obese boy: OR=1.35, 95% CI: 0.24-7.45; obese girls: OR=2.44, 95% CI: 0.62-9.59). |
| Henkin, 2008/N=94; 4-18yr; England | Risk for overweight: BMI≥85th<95th Overweight: BMI≥95th |
Subjective: None Objective: Medical record review for asthma dx |
Age, gender, atopic dermatitis and allergic rhinitis hx,food allergy or other allergies |
|
| Jacobson, 2008/N=517; 3.4-4.6yr; USA; | Risk for overweight: BMI≥85th<95th Overweight: BMI≥95th |
Subjective: Parental-report of children's asthma dx/symptoms, meds use, EDs Objective: None |
Age, gender, parental hx of asthma, birth place, parental birth place, parental education and employment, sibling's allergies, ETS | Body mass was associated with asthma among girls (OR=2.0, 95% CI: 1.1-3.7), but not boys (OR=1.4, 95% CI: 0.8-2.6). |
| Kuschnir, 2009/N=2858; 13-14yr; Brazil | Only one category—BMI≥85th | Subjective: Self-report of asthma and asthmatic symptoms Objective: None |
Age, gender, household pet, sedentary life, ETS |
|
| Kwon, 2006/N=853; 2-11yr; USA | Risk for Overweight: BMI≥85th<95th Overweight: BMI≥95th |
Subjective: Parental-report of asthma dx, asthma-like symptoms, asthma related EDs Objective: None |
Age, gender, race/ethnicity, nativity, insurance status, ETS |
|
| Leung, 2009/N=486; 14-18yr; Hong Kong | Overweight: BMI≥85th<95th Obese: BMI≥95th |
Subjective: Self-report of asthma dx Objective: lipid profile and inflammatory biomarkers |
Age, gender, allergic rhinitis and eczema hx; serum | Obesity not associated with asthma or atopy in Chinese children (p=.257). |
| Luder, 1998/N=209; 2-18yr;USA | Risk for Overweight: BMI≥85th<95th Overweight: BMI≥95th |
Subjective: Parental report of asthmatic symptoms and meds use Objective: Asthma dx by a doctor PEFR measurement |
Age, gender, race, prematurity, breast feeding, avoidance of foods for asthma, ethnomedical-folk remedies, insurance status, ETS | Prevalence of overweight significantly higher in children with moderate to severe asthma than in their peers (OR=1.34, 95% CI: 0.99-1.82). |
| Mai, 2003/N=457; 11-13yr; Sweden | High BMI: BMI≥75th Overweight: BMI≥95th |
Subjective: Parental-report of ISAAC, asthma dx, current wheezing and asthma severity Objective: AHR test |
Age, gender, SPTs for allergens, episodes of hay fever |
|
| Rodriguez, 2002/N=12388; 2months-16yr;USA | Only one category—BMI≥85th | Subjective: Parental- report of current diagnosed asthma Objective: None |
Age, gender, race/ethnicity, household head's education, family income/size, insurance status, urban status, ETS |
|
| Schachter, 2003/N=5993; 7-12yr; Australia | Overweight: BMI≥85th<95th Obese: BMI≥95th |
Subjective: Recent wheeze hx, recent asthma hx/dx Objective: FEV1, FVC, PEFR |
Age, gender, SPTs for allergens, AHR hx, ETS |
|
| Shamssain, 2006/N=7000; 5-16yr; England | Overweight: BMI≥85th<95th Obese: BMI≥95th |
Subjective: Self-report of asthma diagnose and asthmatic symptoms Objective: None |
Age, gender, ETS |
|
| Sithole, 2008/N=3804; 10-11yr; Canada | Overweight: BMI≥20.4(boys) BMI≥20.5(girls) Obese: BMI≥24.8 (boys) BMI≥25.1 (girls) |
Subjective: Parental-report of children diagnosed with asthma Objective: None |
Age, gender, parental education, household income, neighborhood income | A unit increase of BMI associated with 6% increase of prevalence for asthma both in boys and girls. |
| To,2004/N= 11199; 4-11yr; Canada; | Obese: BMI≥85th | Subjective: Parental- report of asthma dx, prescribed inhalants, asthma attacks, limited activities by asthma Objective: None |
Age, gender, single child status; parental smoking, maternal asthma hx and depression, SES | No statistical association between obesity and asthma among Canadian children age 4 to 11 years. |
| Tsai, 2007/N=2290; 5th-graders; Taiwan | Risk for Overweight: BMI≥85th<95th Overweight: BMI≥95th |
Subjective: Self-report physician diagnosed asthma and respiratory symptoms Objective: None |
Age, gender, TV-watching time, Physical activity | Obesity was positively associated with an increased risk of suspected asthma in boys (aOR=1.56, 95% CI: 1.07-2.29), but not in girls. |
| Vargas, 2007/N=1029; 3-5yr; USA | Risk for Overweight: BMI≥85th<95th Overweight: BMI≥95th |
Subjective: Parental-report of asthma morbidity, symptoms, health care/meds use, school days missed, quality of life Objective: Physician diagnosed or algorithm identified asthma |
Age, gender, ETS, SPTs | Prevalence of overweight significantly higher in children with asthma compared with the two control groups (Arkansas prekindergarten group: p=.05 and National Health and Nutrition Examination Survey [NHANES]: p<.001, respectively). |
| Vázquez-Nava, 2010/N=1160; 4-6yr; Mexico | Overweight: BMI≥85th<95th Obese: BMI≥95th |
Subjective: Parental-report of children diagnosed with asthma Objective: None |
Age, gender, related symptoms (dry cough, wheezing, sleep disturbance), ETS, physical activity, intake of high sugar/oil food |
|
| Vignolo, 2005/N=1179; 2.2-16.1yr; Italy | Only one category—BMI-SDS(BMI standard deviation score units) ≥2 | Subjective: None Objective: Medical record review for asthma dx, FEV1, FVC, FEF25-75% |
Age, gender, allergic symptoms, IgE, SPTs for allergens |
|
| von Kries, 2001/N=9357; 5-6yr; German | Overweight: BMI>90th≤97th Obese: BMI>97th |
Subjective: Parental-report of asthma diagnosed by physician and asthma severity. Objective: None |
Age, gender, prematurity, breast-feeding, febrile episodes in 0-1 yr, full-fat milk consumption; parental education and atopic diseases hx, living environment, ETS |
|
| von Mutius, 2001/N=7505; 4-17yr; USA; | Obese: BMI≥75th | Subjective: Parental-report of diagnosed or treated for asthma, or still had asthma Objective: None |
Age, gender, ethnicity, ETS, birth weight, breast fed, household size; SPTs for allergens |
|
| Wickens, 2005/N=305;10.1-12.6yr;New Zealand | Overweight: Boys:BMIat10y≥19.8BMIat12.5y≥21.6 Girls:BMIat10y≥19.9 BMIat12.5y≥22.1 Obese: Boys:BMIat10y≥24.0BMIat12.5y≥26.4 Girls:BMIat10y≥24.1 BMIat12.5y≥27.2 |
Subjective: Parental-report of wheezing and asthma dx, meds use and hospital admissions for asthma Objective: PEFR variability before and after exercise, AHR to exercise test |
Age, gender, ethnicity, birth weight; family allergic hx, family size, ETS, father's education, frequency of exercise and hamburger consumption;SPTs for allergens |
|
| Yoo, 2011/N=717; 15-17yr; Korean | Overweight: BMI≥85th | Subjective: Self-report of Self-report of asthma and asthmatic symptoms (ISAAC questionnaire) Objective: AHR test |
Age, gender, recent physical activity, current smoking, parental smoking/education, family hx of allergic dx |
|
ATS: American Thoracic Society
Table 2. Longitudinal studies (N=4).
| Author/population | Definition of | Confounding factors | Main result | |
|---|---|---|---|---|
| Obesity | Asthma | |||
| Castro-Rodriguez, 2001/N=1246; 6,8,11,13yr; USA | Overweight: BMI≥85th<95th Obese: BMI≥95th |
Subjective: Parental-report of wheezing episodes,classified into frequent/infrequent or incident/persistent wheezing Objective: PEF variability, broncho-dilator response test |
Age, gender, start of puberty, exercise, SPTs for allergens, esinophil counts and methacholine challenge; parental allergic hx, maternal smoking and education, number of siblings | Females who became overweight or obese between 6yr and 11yr were between 5.5 (95% CI: 1.3-23.3)and 6.8(95% CI: 2.4-19.4) times more likely to develop new asthma at 11 or 13yr compared with females who did not become overweight or obese during the same time period. |
| Chinn, 2001/N=8983;8-9yr; England | Overweight: ≥25th BMI<30th Obese: BMI≥30th |
Subjective: Parental-report of asthma or wheezing Objective: None |
Age, gender, ethnicity, birth weight, length of gestation, parental smoking, number of siblings |
|
| Gilliland, 2003/N=3792;7-18y; USA | Overweight: BMI≥85th<95th Obese: BMI≥95th |
Subjective: Parental-report of a new physician diagnose of asthma Objective:FEV1, FVC, FEF25-75% |
Age, gender, ethnicity, birth weight, puberty onset age, team sports, smoking hx, parental allergic hx, insurance status, ETS, household characteristics |
|
| Mannino, 2006/N=4393; Enrolled from birth and 14yr at follow up; USA | High BMI: BMI≥85th | Subjective: Parental-report of asthma dx, meds use and doctors' visits Objective: None |
Age, gender, ethnicity, birth weight, prenatal maternal smoking, poverty status |
|
In addition to identification of a positive relationship between BMI and asthma in the majority of studies included, some were able to elucidate the pattern of the relationship. Both Kwon et al. (2006) and Sithole et al. (2008) found a linear relationship between BMI and asthma prevalence in 2-11 year old girls and in both boys and girls age 10-11 years old. A U-shaped relationship between BMI and asthma prevalence in boys age 2-11 years was identified by Kwon et al. (2006). Two cross-sectional studies (Sithole et al. 2008, von Kries et al. 2001) reported a dose-response relationship among BMI and asthma prevalence. Sithole et al. (2008) estimated that a unit increase of body mass index was associated with a 6% increase in asthma prevalence.
Among those studies that tried to correlate obesity with both atopy and asthma, the relationship between high BMI and asthmatic symptoms is conflicting. However, half of the above mentioned studies that identified a positive association between obesity and asthma all failed to recognize a coexistence of any allergic disease (Bibi et al. 2004, Mai et al. 2003, von Kries et al. 2001). Interestingly, the other half that discovered a negative finding in the association between obesity and atopic diseases could also not verify a positive correlation between asthma and obesity (Leung et al. 2009, Schachter et al. 2003, Vignolo et al. 2005). This result may justify the implication that the obesity-asthma linkage is more noticeable in nonatopic children.
Effect modifiers of the association between asthma/asthmatic symptoms and obesity
Rather than being controlled as confounders, some factors were identified in reviewed studies as effect modifiers of the interaction between asthma and obesity (Kwon et al. 2006). Gender, appeared to be the most discussed effect modifier. More than one fourth of reviewed studies (N = 12) reported a gender effect on the relationship between obesity and asthma or asthmatic symptoms; nine of these studies used cross-sectional (Figueroa-Munoz et al.2001, Jacobson et al. 2008, Kwon et al. 2006, Kuschnir &da Cunha 2009, Schachter et al. 2003, Shamssain 2006, Tsai et al. 2007, von Kries et al. 2001, Yoo et al. 2011) and three longitudinal designs (Castro-Rodriguez et al. 2001, Gilliland et al. 2003, Mannino et al. 2006). More than half of the studies concluded that the association between BMI and asthma was stronger in girls than boys (Castro-Rodriguez et al. 2001, Figueroa-Munoz et al. 2001, Jacobson et al. 2008, Kuschnir &da Cunha 2009, Schachter et al. 2003, von Kries et al. 2001). Complicating a parsimonious explanation, Kwon et al. (2006) found a U-shape BMI-asthma relationship among boys but a linear BMI-asthma correlation among girls.
Other than gender, some researchers also discovered that ethnicity may mediate the association between obesity and asthma. Kwon et al. (2006) revealed that Hispanic children accounted for a larger portion of children who were both overweight/obese and had asthma than Black and non-Hispanic children. Ahmad et al. (2009) also concluded that the asthma-obesity association was more prominent among black children than white children.
Factors scrutinized in studies on the asthma and obesity association
Factors other than obesity and asthma indicators that were incorporated in the reviewed studies are inconsistent. The number of related factors included in studies ranged widely from only two (Cassol et al. 2006) to more than ten (Gilliland et al. 2003). Most were treated as confounders and controlled when examining the relationship between asthma and obesity. This inconsistency may result from the various interests and objectives emphasized by different researchers and be associated with the variant purposes of original surveys.
Those scrutinized factors in reviewed papers can be categorized into two major different types. First and the most gathered was the type of factors conveying mostly the demographic information such as household income, social class, ethnicity, parents' education level, allergic disease history of children/families and active or passive environmental tobacco smoke (ETS) exposure. The other less scrutinized type consisted of modifiable factors concerning the children's risk behaviour such as children's dietary habits or patterns (Luder et al. 1998, Vázquez-Nava et al. 2010, von Kries et al. 2001, Wickens et al. 2005), exercise (Wickens et al. 2005), physical activity (Yoo et al. 2011), TV-watching time (Epstein et al. 2000) and sedentary life style (Kuschnir & da Cunha 2009).
Discussion
The findings from this review support a positive relationship between obesity and asthma in all paediatric populations from infants to young adults. Among the 35 studies included, the majority of them found a positive association between being overweight/obese and asthmatic symptoms. In addition, three of four studies conducted with a longitudinal or prospective design concluded that higher BMI during early childhood predicted future increased incidence of newly-diagnosed asthma or asthma-like symptoms. The prospective studies included in this review help clarify the causal relationship between obesity and asthma as did the meta-analysis of longitudinal studies conducted earlier (Flaherman & Rutherford 2006).
Several of the reviewed articles did not identify an association between obesity and asthma (Chinn &Rona 2001, Henkin et al. 2008, Leung et al. 2009, Schachter et al. 2003, To et al. 2004, Vázquez-Nava et al. 2010, Vignolo et al. 2005). However, some of those negative results need further careful consideration. All these studies, except one longitudinal survey conducted by Chinn and Rona (2001), were cross-sectional. Henkin et al. (2008) only drew their results from a small population (N=94). Vázquez-Nava et al. (2010) drew conclusions out of non-significant statistical results (P > 0.05); and none of these studies used USA samples and other non-USA samples did show positive relationships between obesity and asthma.
This review reveals that the obesity-asthma link appears to be more prominent in girls, which is consistent with several study findings in adult populations where obese women are more likely to have asthma or worse asthma control (Beckett et al. 2001, Guerra et al. 2002, Varraso et al. 2005). Both Castro-Rodriguez et al. (2001) and Herrera-Trujillo et al. (2005) identified a stronger correlation between asthma and obesity in girls with early onset of puberty. There is still no satisfactory explanation of the underlying mechanism; however, hormones or changing body composition have been implicated since early onset of puberty in children is positively related to persistent asthma after puberty (Guerra et al. 2004).
Compared with sex modification in the relationship between obesity and asthma, the evidence of other correlated factors interacting both with obesity and asthma seems to be less consistent. Only Kwon et al. (2006) and Ahmad et al. (2009) reported ethnicity as a mediating factor in asthma and obesity. They concluded that children with different ethnic backgrounds may be differentially affected singularly by both obesity and asthma. The paucity of constant findings regarding the effect of ethnicity may result from the inconsistency of incorporating diverse populations into studies and analyzing ethnic data as an important effecter. Ethnic disparity has been identified in obesity and asthma prevalence respectively in paediatric populations (Eaton et al. 2010, Zahran et al. 2011). More cross ethnic group or cross nation studies are needed to clarify the role of ethnicity in the obesity-asthma linkage.
The discord regarding the number and type of confounders controlled or examined in the articles included in this review prevented the generation or integration of a more comprehensive result. However, as the health conditions related to both obesity and asthma are complex and related to a tangled set of host and environmental risk factors, the lack of a ‘standard’ list of correlates in obesity-asthma studies is not unexpected (Bateman et al. 2008, Davison & Birch 2001). Two tentative explanations may be proposed for this absence. First, as previously noted, scientists of several reviewed studies picked up associated variables from a set of correlates selected for a pre-existing databank's original research objectives. Although researchers can readily benefit from retrieving information from the large amount of samples contained in each databank, using this approach, some important variables modifying or confounding the obesity-asthma correlation may be omitted or neglected. Second, there does not seem to be a precedent protocol which can be adopted to guide the variable selection process. This can be illustrated by the observation that even though both Epstein et al. (2000) and von Mutius et al. (2001) analyzed data from the same databank (NHANES III), they ended up controlling for a different set of covariates when evaluating the asthma-obesity relationship.
Although scientists incorporated variant correlates in evaluation of the obesity-asthma linkage, most covariates controlled or reviewed in selected studies were indices conveying demographic information. Fewer studies elucidated behavioural contributors mediating or moderating these two epidemics. However, both obesity- or asthma-focused studies have already recognized many important behavioural variables affecting obese or asthmatic status such as diet or physical activity, respectively (Berntsen 2011, Devereux & Seaton 2005, Ludwig et al.2001, Trost et al. 2001). Although several investigations included in this review have already explored the role of behavioural variables in the obesity-asthma association, more well-constructed studies may achieve more conclusive findings (Vázquez-Nava et al. 2010, Wickens et al. 2005). The exploratory nature of the studies included in this review may explain why the demographic features were more discussed. However, by accumulating more solid evidence confirming the positive relationship between asthma and obesity, scientists can take the next step to further explore the impact from other ‘mutable’ behavioural correlates contributing to both health problems. The identified ‘modifiable’ or ‘mutable’ behavioural risk factors may guide investigators to develop practical preventive strategies for clinicians and help children stay away from adopting detrimental behaviours or lifestyles that threaten their health (Beckett et al. 2001).
Accumulating evidence from recent research points to the advent of a distinct ‘obesity asthma’ phenotype and suggests that obesity may contribute to asthma through a non-allergic pathway (Jensen et al. 2011, Lugogo et al. 2010). Reports with positive findings have concluded that the obesity-asthma association is somehow independent from allergic sensitization, which is in accordance with the findings found in an adult population (van Veen et al. 2008). The speculation about a new phenotype called ‘obesity asthma’ not only recognizes the importance of obesity with respect to its impact on the development and severity of asthma, but may also persuade researchers to adopt innovative rather than conventional strategies to explore the underlying mechanism. Based on this preliminary finding generated by this review, the next step for upcoming systematic reviews or meta-analyses may mainly focus on those studies with objective measurements of childhood asthma so that the linkage of obesity to a specific asthma phenotype may be found. In addition, larger scale collaboration with scientists from various specialties and fields contributing their ideas to formulate an integrated mechanism delineating the interplay between asthma and obesity is also warranted.
Although scientists are still looking for a satisfactory explanation delineating the interplay between obesity and asthma, we nurses and other clinical health providers are already challenged by the deviated response to regular asthmatic treatment in children with these two epidemics. In parallel with effort to identify the demographic attributes related to both epidemics, identifying the behavioural factors correlated with both diseases is also important. Conducting more prospective research incorporating a broader spectrum of correlates will help to identify high-risk groups with specific demographic attributes and also help develop effective interventions focusing on eliminating risk behaviours contributing to both obesity and asthma. Given the evidence that weight reduction has been found significantly related to improvement in asthma outcome in an adult population (Eneli et al. 2008), the role of behavioural factors or lifestyles should be one of the leading areas of study in the future obesity-asthma research (Jensen et al. 2011, Lang 2010). Only by identifying and targeting modifiable behaviours detrimental to both obesity and asthma can scientists further conceive practical interventions to alleviate the double health burden among children suffering from both epidemics (Lang 2010).
Limitations
To formulate a concrete result from this review, preset criteria for including or excluding related reports was adopted; however, applying those criteria to article selection may have resulted in limitations. First, including studies mainly concentrating on the relationship between obesity and asthma may have omitted some investigations with positive outcomes relating obesity to asthma. In one excluded report, obesity was only treated as one risk factor leading to the development of asthma (Rodriguez et al. 2002); in another report BMI index was only controlled as one confounder to explain the other exposure's effect on the asthma incidence (Oddy & Sherriff 2003). Although these studies generated results confirming a significant association between obesity and asthma, they jeopardize the integrated process of this review increasing heterogeneity and ambiguity.
Second, the selection of studies using BMI as a primary index to define obesity filtered out some reports, particularly those targeting younger paediatric populations such as infants (Guerra et al. 2004, Taveras et al. 2008). It is possible to argue that BMI is not a favorable standard by which to identify childhood obesity (Musaad et al. 2009); however, it remains a popular and reasonable indicator for large epidemiologic surveys worldwide (Barlow 2007, Lazarus et al.1996).
Third, only incorporating published papers with a clear BMI cutoff point to confirm obese or overweight status also ruled out some studies which may have positive findings. Reports excluded in this category mostly manipulated BMI as a continuous variable. Most of them concluded that higher BMI was accompanied by higher asthma prevalence and many of them were longitudinally designed and thus would have provided further evidence for the obesity-asthma link making our interpretations more conservative in nature (Davis et al.2007, Guerra, et al. 2004, Hancox et al. 2005, Michelson et al. 2009). Using BMI cutoff points to define obesity may yield acceptable specificity and sensitivity to identify subgroups with greater risk for potential comorbidity (Lazarus et al. 1996).
Another limitation relates to the definition of childhood asthma. In the absence of a ‘gold standard’ to measure or diagnose childhood asthma (Remes et al. 2002), the heterogeneity of asthma definitions from included studies seems to be inevitable. Though adopting objective measurements can ensure scientists with more confidence to confirm childhood asthma, data gaining from pulmonary tests is somehow unreliable and not recommended as a standard diagnostic procedure especially in children aged 5 or younger (Pedersen et al. 2011, Werk et al. 2000). To aggregate evidence from contemporary research with a wide spectrum of age groups, the inclusion of studies containing this young population may limit the interpretation of this review. However, after excluding a significant amount of studies failing to provide any subjective or objective evidence to confirm asthma diagnosis, this concern should be eliminated to certain extent. Although most studies confirmed the asthma status by subjective reports of a physician-diagnosed asthma, it is a widely accepted strategy to identify childhood asthma in many epidemiologic surveys (van Wonderen et al. 2010) and found relatively accurate in children (Joesch et al. 2006). Though there was no study excluded during the quality appraisal process, the description listed in Table S2 presenting how each study scored on each appraised item can fully report the quality of reviewed studies (Higgins et al. 2011). Also, common biases especially for the performance and detection biases were also taken into account by exaniminig and presenting the appraisal results of the measurements (BMI measurement and asthma indicators) adopted by each study (Table S1 and S2).
Conclusions
This review includes a large number of studies on the relationship between obesity and asthma with various research designs. Although the inclusion of investigations with variant research methods may compromise the validity of the evidence, by conducting this review we provide a comprehensive integration of contemporary studies focusing on the relationship between obesity and asthma in paediatric populations. Data from this review provide ongoing evidence that there is a positive relationship between high BMI and asthma in children. The nature of the association appears to be complex; however, with studies identifying linear, U-shape and dose-dependent relationships between BMI and asthma (Kwon et al. 2006, Sithole et al. 2008, von Kries et al. 2001). Similar to previous meta-analyses in adult and child populations, most longitudinal studies reviewed agreed that children who were overweight or obese in early life have an increased risk of newly diagnosed asthma in the future.
Female gender and ethnicity were recognized as important effect modifiers that alter the relationship between asthma and obesity. In accordance with research results found in adults, the obesity-asthma linkage seems to be more prominent in girls though more well-constructed studies are needed to achieve a more conclusive result. The lack of a standard set of confounders controlled in the included studies and a lack of studies looking at the impact of behavioural factors on the relationship between obesity and asthma were revealed by this review. Conducting more prospective or cohort studies with a collection of meaningful factors based on previous obesity-asthma focused studies, rather than solely relying on pre-existing databanks, may generate further knowledge of the underlying mechanisms of the association.
While scientists are still looking for a satisfactory explanation of the interplay between obesity and asthma, we nurses and other clinicians are already challenged by the deviated responses from obese and asthmatic children treated with the regular regimen. Given the evidence found in adults that weight reduction is significantly associated with improvement in asthma outcome, the role of behavioural factors or lifestyles should be one of the major areas of study in future obesity-asthma research. Nurses as the primary healthcare providers should help children and their families by developing effective nursing interventions to avoid unhealthy life-styles or behaviours leading to the comorbidity of both health burdens. However, a larger scale of interdisciplinary collaboration for conducting more well-designed research by scrutinizing an expanded spectrum of correlates (demographic to behavioural risk factors) related to both epidemics is needed to identify high-risk groups with specific demographic attributes and develop effective nursing interventions applicable to the primary and clinical settings.
Supplementary Material
Summary Statements.
What is already known about this topic
The concurrent increase in asthma and obesity prevalence has been noticed and discussed in many research papers.
Studies conducted in different populations have confirmed a positive association between asthma and obesity, but the research conclusions pertaining to children are more inconsistent than those from adults.
What this paper adds
Although some studies did not recognize the relationship between asthma and obesity in children, the majority of studies reviewed supported a correlation between childhood asthma and obesity.
Using retrieval of data from pre-existing databanks may not only preclude further exploration of influential correlates or effect modifiers that interact with both epidemics but also relate to insufficient consideration of the impact of behavioural factors on the relationship between obesity and asthma.
Among several important effect modifiers, gender was the most consistent and prominent in the relationship between asthma and obesity; the obesity-asthma linkage seems to be more obvious in girls.
Implications for practice and/or policy
More well-structured studies primarily designed to investigate the relationship between asthma and obesity in children are needed to elucidate the complex interplay between asthma, obesity and most influential covariates.
Prospective investigations should incorporate an expanded spectrum of correlates representing children's demographic and behavioural attributes so that scientists can develop effective intervention targeting not only of high-risk subgroups but also children with detrimental life-styles or behaviours.
Larger scale of interdisciplinary collaboration for conducting well-designed research by scrutinizing demographic and behavioural risk factors related to both epidemics is needed to identify high-risk groups and develop effective nursing interventions to help high-risk children and family to adopt healthier life-styles and behaviours.
References
- Ahmad N, Biswas S, Bae S, Meado KE, Huang R, Singh KP. Association between obesity and asthma in US children and adolescents. Journal of Asthma. 2009;46(7):642–646. doi: 10.1080/02770900802503123. [DOI] [PubMed] [Google Scholar]
- Barlow SE. Expert committee recommendations regarding the prevention, assessment and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl. 4):S164–192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, Gibson P, Ohta K, O'Byrne P, Pedersen SE, Pizzichini E, Sullivan SD, Wenzel SE, Zar HJ. Global strategy for asthma management and prevention: GINA executive summary. European Respiratory Journal. 2008;31(1):143–178. doi: 10.1183/09031936.00138707. [DOI] [PubMed] [Google Scholar]
- Beckett WS, Jacobs DR, Jr, Yu X, Iribarren C, Williams OD. Asthma is associated with weight gain in females but not males, independent of physical activity. American Journal of Respiratory and Critical Care Medicine. 2001;164(11):2045–2050. doi: 10.1164/ajrccm.164.11.2004235. [DOI] [PubMed] [Google Scholar]
- Belamarich PF, Luder E, Kattan M, Mitchell H, Islam S, Lynn H, Crain EF. Do obese inner-city children with asthma have more symptoms than nonobese children with asthma? Pediatrics. 2000;106(6):1436–1441. doi: 10.1542/peds.106.6.1436. [DOI] [PubMed] [Google Scholar]
- Berntsen S. Physical activity and aerobic fitness in childhood: associated with asthma? Clinical Respiratory Journal. 2011;5(1):59. doi: 10.1111/j.1752-699X.2010.00197.x. [DOI] [PubMed] [Google Scholar]
- Bertolace MdPC, Toleda E, Jorge PPdO, Liberatore RDR., Jr Association between obesity and asthma among teenagers. Sao Paulo Medical Journal. 2008;126:285–287. doi: 10.1590/S1516-31802008000500008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beuther DA. Obesity and asthma. Clinical Chest Medicine. 2009;30(3):479–488. doi: 10.1016/j.ccm.2009.05.002. [DOI] [PubMed] [Google Scholar]
- Bibi H, Shoseyov D, Feigenbaum D, Genis M, Friger M, Peled R, Sharff S. The relationship between asthma and obesity in children: is it real or a case of over diagnosis? Journal of Asthma. 2004;41(4):403–410. doi: 10.1081/jas-120026097. [DOI] [PubMed] [Google Scholar]
- Bidad K, Anari S, Aghamohammadi A, Pourpak Z, Moayeri H. Prevalence of asthma related to BMI in adolescents in Tehran, Iran, 2004-2005. European Journal of Pediatrics. 2007;166(5):453–454. doi: 10.1007/s00431-006-0259-0. [DOI] [PubMed] [Google Scholar]
- Burgess JA, Walters EH, Byrnes GB, Giles GG, Jenkins MA, Abramson MJ, Dharmage SC, et al. Childhood adiposity predicts adult-onset current asthma in females: a 25-yr prospective study. European Respiratory Journal. 2007;29(4):668–675. doi: 10.1183/09031936.00080906. [DOI] [PubMed] [Google Scholar]
- Cassol VE, Rizzato TM, Teche SP, Basso DF, Centenaro DF, Maldonado M, Moraes EZ, Hirakata VN, Solé D, Menna-Barreto SS. Obesity and its relationship with asthma prevalence and severity in adolescents from southern Brazil. Journal of Asthma. 2006;43(1):57–60. doi: 10.1080/02770900500448597. [DOI] [PubMed] [Google Scholar]
- Castro-Rodriguez JA, Holberg CJ, Morgan WJ, Wright AL, Martinez FD. Increased incidence of asthmalike symptoms in girls who become overweight or obese during the school years. American Journal of Respiratory & Critical Care Medicine. 2001;163(6):1344–1349. doi: 10.1164/ajrccm.163.6.2006140. [DOI] [PubMed] [Google Scholar]
- Centre for Reviews and Dissemination. Systematic Reviews: CRD's Guidance for Undertaking Reviews in Health Care. University of York, York; 2009. Retrieved from http://www.york.ac.uk/inst/crd/systematic_reviews_book.htm on 5 August 2012. [Google Scholar]
- Chen Y, Rennie D, Cormier Y, Dosman J. Sex specificity of asthma associated with objectively measured body mass index and waist circumference: the Humboldt study. Chest. 2005;128(4):3048–3054. doi: 10.1378/chest.128.4.3048. [DOI] [PubMed] [Google Scholar]
- Chinn S. Obesity and asthma: evidence for and against a causal relation. Journal of Asthma. 2003;40(1):1–16. doi: 10.1081/jas-120017202. [DOI] [PubMed] [Google Scholar]
- Chinn S, Rona RJ. Can the increase in body mass index explain the rising trend in asthma in children? Thorax. 2001;56(11):845–850. doi: 10.1136/thorax.56.11.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Counsell C. Formulating questions and locating primary studies for inclusion in systematic reviews. Annals of Internal Medicine. 1997;127:380–387. doi: 10.7326/0003-4819-127-5-199709010-00008. [DOI] [PubMed] [Google Scholar]
- Cummings G, Lee H, Macgregor T, Davey M, Wong C, Paul L, Stafford E. Factors contributing to nursing leadership: a systematic review. Journal of health services research and policy. 2008;13(4):240–248. doi: 10.1258/jhsrp.2008.007154. [DOI] [PubMed] [Google Scholar]
- Davis A, Lipsett M, Milet M, Etherton M, Kreutzer R. An association between asthma and BMI in adolescents: results from the California Healthy Kids Survey. Journal of Asthma. 2007;44(10):873–879. doi: 10.1080/02770900701752656. [DOI] [PubMed] [Google Scholar]
- Davison KK, Birch LL. Childhood overweight: a contextual model and recommendations for future research. Obesity Review. 2001;2(3):159–171. doi: 10.1046/j.1467-789x.2001.00036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devereux G, Seaton A. Diet as a risk factor for atopy and asthma. Journal of Allergy and Clinical Immunology. 2005;115(6):1109–1117. doi: 10.1016/j.jaci.2004.12.1139. [DOI] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Lim C, Whittle L, Brener ND, Wechsler H, Wechsler H. Youth risk behaviour surveillance - United States, 2009. MMWR Surveillence Summary. 2010;59(5):1–142. [PubMed] [Google Scholar]
- Eneli IU, Skybo T, Camargo CA. Weight loss and asthma: a systematic review. Thorax. 2008;63(8):671–676. doi: 10.1136/thx.2007.086470. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Wu YW, Paluch RA, Cerny FJ, Dorn JP. Asthma and maternal body mass index are related to pediatric body mass index and obesity: results from the Third National Health and Nutrition Examination Survey. Obesity Research. 2000;8(8):575–581. doi: 10.1038/oby.2000.74. [DOI] [PubMed] [Google Scholar]
- Estabrooks C, Goel V, Thiel E, Pinfold P, Sawka C, Williams I. Decision aids: are they worth it? A systematic review. Journal of Health Services Research and Policy. 2001;6(3):170–182. doi: 10.1258/1355819011927431. [DOI] [PubMed] [Google Scholar]
- Figueroa-Munoz JI, Chinn S, Rona RJ. Association between obesity and asthma in 4-11 year old children in the UK. Thorax. 2001;56(2):133–137. doi: 10.1136/thorax.56.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flaherman V, Rutherford GW. A meta-analysis of the effect of high weight on asthma. Archives of Disease in Childhood. 2006;91(4):334–339. doi: 10.1136/adc.2005.080390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford ES. The epidemiology of obesity and asthma. Journal of Allergy and Clinical Immunology. 2005;115(5):897–909. doi: 10.1016/j.jaci.2004.11.050. quiz 910. [DOI] [PubMed] [Google Scholar]
- Garrard J. Health sciences literature review made easy: The matrix method. Sudbury, MA: Jones and Bartlett Publishers; 2007. [Google Scholar]
- Gennuso J, Epstein LH, Paluch RA, Cerny F. The relationship between asthma and obesity in urban minority children and adolescents. Archives of Pediatrics & Adolescent Medicine. 1998;152(12):1197–1200. doi: 10.1001/archpedi.152.12.1197. [DOI] [PubMed] [Google Scholar]
- Gilliland FD, Berhane K, Islam T, McConnell R, Gauderman WJ, Gilliland SS, Avol E, Peters JM. Obesity and the risk of newly diagnosed asthma in school-age children. American Journal of Epidemiology. 2003;158(5):406–415. doi: 10.1093/aje/kwg175. [DOI] [PubMed] [Google Scholar]
- Guerra S, Sherrill DL, Bobadilla A, Martinez FD, Barbee RA. The relation of body mass index to asthma, chronic bronchitis and emphysema. Chest. 2002;122(4):1256–1263. doi: 10.1378/chest.122.4.1256. [DOI] [PubMed] [Google Scholar]
- Guerra S, Wright AL, Morgan WJ, Sherrill DL, Holberg CJ, Martinez FD. Persistence of asthma symptoms during adolescence: role of obesity and age at the onset of puberty. American Journal of Respiratory and Critical Care Medicine. 2004;170(1):78–85. doi: 10.1164/rccm.200309-1224OC. [DOI] [PubMed] [Google Scholar]
- Hancox RJ, Milne BJ, Poulton R, Taylor DR, Greene JM, McLachlan CR, Cowan JO, Flannery EM, Herbison GP, Sears MR. Sex differences in the relation between body mass index and asthma and atopy in a birth cohort. American Journal of Respiratory and Critical Care Medicine. 2005;171(5):440–445. doi: 10.1164/rccm.200405-623OC. [DOI] [PubMed] [Google Scholar]
- Hasan RA, Zureikat GY, Nolan BM, LaChance JL, Campe JL, Amin R. The relationship between asthma and overweight in urban minority children. Journal of the National Medical Association. 2006;98(2):138–142. [PMC free article] [PubMed] [Google Scholar]
- He QQ, Wong TW, Du L, Jiang ZQ, Qiu H, Gao Y, Liu JW, Wu JG, Yu IT. Respiratory health in overweight and obese Chinese children. Pediatric Pulmonology. 2009;44(10):997–1002. doi: 10.1002/ppul.21091. [DOI] [PubMed] [Google Scholar]
- Henkin S, Brugge D, Bermudez OI, Gao X. A case-control study of body mass index and asthma in Asian children. Annals of Allergy, Asthma and Immunology. 2008;100(5):447–451. doi: 10.1016/S1081-1206(10)60469-3. [DOI] [PubMed] [Google Scholar]
- Herrera-Trujillo M, Barraza-Villarreal A, Lazcano-Ponce E, Hernandez B, Sanin LH, Romieu I. Current wheezing, puberty and obesity among mexican adolescent females and young women. Journal of Asthma. 2005;42(8):705–709. doi: 10.1080/02770900500265306. [DOI] [PubMed] [Google Scholar]
- Higgins JPT. Cochrane handbook for systematic reviews of interventions. S.l.: Cochrane Collaboration; 2011. [Google Scholar]
- Jacobson JS, Mellins RB, Garfinkel R, Rundle AG, Perzanowski MS, Chew GL, andrews HF, Goldstein IF. Asthma, body mass, gender and Hispanic national origin among 517 preschool children in New York City. Allergy. 2008;63(1):87–94. doi: 10.1111/j.1398-9995.2007.01529.x. [DOI] [PubMed] [Google Scholar]
- Jang AS, Lee JH, Park SW, Shin MY, Kim DJ, Park CS. Severe airway hyperresponsiveness in school-aged boys with a high body mass index. Korean Journal of Internal Medicine. 2006;21(1):10–14. doi: 10.3904/kjim.2006.21.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen ME, Collins CE, Gibson PG, Wood LG. The Obesity Phenotype in Children with Asthma. Pediatric Respiratory Reviews. 2011;12(3):152–159. doi: 10.1016/j.prrv.2011.01.009. [DOI] [PubMed] [Google Scholar]
- Joesch JM, Kim H, Kieckhefer GM, Greek AA, Baydar N. Does Your Child Have Asthma? Filled Prescriptions and Household Report of Child Asthma. Journal of Pediatric Health Care. 2006;20(6):374–383. doi: 10.1016/j.pedhc.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Kuschnir FC, da Cunha AL. Association of overweight with asthma prevalence in adolescents in Rio de Janeiro, Brazil. Journal of Asthma. 2009;46(9):928–932. doi: 10.3109/02770900903231566. [DOI] [PubMed] [Google Scholar]
- Kwon HL, Ortiz B, Swaner R, Shoemaker K, Jean-Louis B, Northridge ME, Vaughan RD, Marx T, Goodman A, Borrell LN, Nicholas SW. Childhood asthma and extreme values of body mass index: the Harlem Children's Zone Asthma Initiative. Journal of Urban Health. 2006;83(3):421–433. doi: 10.1007/s11524-006-9050-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwong KY, Rhandhawa I, Saxena J, Morphew T, Jones CA. Ability to control persistent asthma in obese versus non-obese children enrolled in an asthma-specific disease management program (breathmobile) Journal of Asthma. 2006;43(9):661–666. doi: 10.1080/02770900600925270. [DOI] [PubMed] [Google Scholar]
- Lang JE. Obesity and childhood asthma. Pediatric Respiratory Reviews. 2010;11(Suppl. 1):S62–S66. [Google Scholar]
- Lazarus R, Baur L, Webb K, Blyth F. Body mass index in screening for adiposity in children and adolescents: systematic evaluation using receiver operating characteristic curves. The American Journal of Clinical Nutrition. 1996;63(4):500–506. doi: 10.1093/ajcn/63.4.500. [DOI] [PubMed] [Google Scholar]
- Leung TF, Kong AP, Chan IH, Choi KC, Ho CS, Chan HM, So WY, Lam CW, Wong GW, Chan JC. Association between Obesity and Atopy in Chinese Schoolchildren. International Archives of Allergy and Immunology. 2009;149(2):133–140. doi: 10.1159/000189196. [DOI] [PubMed] [Google Scholar]
- Luder E, Melnik TA, DiMaio M. Association of being overweight with greater asthma symptoms in inner city black and Hispanic children. Journal of Pediatrics. 1998;132(4):699–703. doi: 10.1016/s0022-3476(98)70363-4. [DOI] [PubMed] [Google Scholar]
- Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. The Lancet. 2001;357(9255):505–508. doi: 10.1016/S0140-6736(00)04041-1. [DOI] [PubMed] [Google Scholar]
- Lugogo NL, Kraft M, Dixon AE. Does obesity produce a distinct asthma phenotype? Journal of Applied Physiology. 2010;108(3):729–734. doi: 10.1152/japplphysiol.00845.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mai XM, Nilsson L, Axelson O, Braback L, Sandin A, Kjellman NI, Björkstén B. High body mass index, asthma and allergy in Swedish schoolchildren participating in the International Study of Asthma and Allergies in Childhood: Phase II. Acta Pediatrica (Oslo, Norway: 1992) 2003;92(10):1144–1148. [PubMed] [Google Scholar]
- Mai XM, Bottcher MF, Leijon I. Leptin and asthma in overweight children at 12 years of age. Pediatric Allergy Immunology: Official Publication of the European Society of Pediatric Allergy and Immunology. 2004;15(6):523–530. doi: 10.1111/j.1399-3038.2004.00195.x. [DOI] [PubMed] [Google Scholar]
- Mai XM, Becker AB, Sellers EA, Liem JJ, Kozyrskyj AL. The relationship of breast-feeding, overweight and asthma in preadolescents. The Journal of Allergy and Clinical Immunology. 2007;120(3):551–556. doi: 10.1016/j.jaci.2007.05.004. [DOI] [PubMed] [Google Scholar]
- Mannino DM, Mott J, Ferdinands JM, Camargo CA, Friedman M, Greves HM, Redd SC. Boys with high body masses have an increased risk of developing asthma: findings from the National Longitudinal Survey of Youth (NLSY) International Journal of Obesity. 2006;30(1):6–13. doi: 10.1038/sj.ijo.0803145. [DOI] [PubMed] [Google Scholar]
- Michelson PH, Williams LW, Benjamin DK, Barnato AE. Obesity, inflammation and asthma severity in childhood: data from the National Health and Nutrition Examination Survey 2001-2004. Annals of Allergy, Asthma and Immunology. 2009;103(5):381–385. doi: 10.1016/S1081-1206(10)60356-0. [DOI] [PubMed] [Google Scholar]
- Moorman JE, Rudd RA, Johnson CA, King M, Minor P, Bailey C, Scalia MR, Akinbami LJ. National surveillance for asthma--United States, 1980-2004. MMWR Surveillence Summary. 2007;56(8):1–54. [PubMed] [Google Scholar]
- Musaad SM, Patterson T, Ericksen M, Lindsey M, Dietrich K, Succop P, Khurana Hershey GK. Comparison of anthropometric measures of obesity in childhood allergic asthma: central obesity is most relevant. Journal of Allergy and Clinical Immunology. 2009;123(6):1321–1327. doi: 10.1016/j.jaci.2009.03.023. e1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noal RB, Menezes AM, Macedo SE, Dumith SC. Childhood body mass index and risk of asthma in adolescence: a systematic review. Obesity Reviews. 2011;12(2):93–104. doi: 10.1111/j.1467-789X.2010.00741.x. [DOI] [PubMed] [Google Scholar]
- Oddy WH, Sherriff JL. Breastfeeding, body mass index, asthma and atopy in children. Asia-Pacific Journal of Public Health. 2003;15(Suppl):S15–17. doi: 10.1177/101053950301500S05. [DOI] [PubMed] [Google Scholar]
- Oddy WH, Sherriff JL, de Klerk NH, Kendall GE, Sly PD, Beilin LJ, Blake KB, Landau LI, Stanley FJ. The relation of breastfeeding and body mass index to asthma and atopy in children: a prospective cohort study to age 6 years. American Journal of Public Health. 2004;94(9):1531–1537. doi: 10.2105/ajph.94.9.1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Remes ST, Pekkanen J, Remes K, Salonen RO, Korppi M. In search of childhood asthma: questionnaire, tests of bronchial hyperresponsiveness and clinical evaluation. Thorax. 2002;57(2):120–126. doi: 10.1136/thorax.57.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen SE, Hurd SS, Lemanske RF, Jr, Becker A, Zar HJ, Sly PD, Soto-Quiroz M, Wong G, Bateman ED. Global strategy for the diagnosis and management of asthma in children 5 years and younger. Pediatric Pulmonology. 2011;46(1):1–17. doi: 10.1002/ppul.21321. [DOI] [PubMed] [Google Scholar]
- Rodriguez MA, Winkleby MA, Ahn D, Sundquist J, Kraemer HC. Identification of population subgroups of children and adolescents with high asthma prevalence: findings from the Third National Health and Nutrition Examination Survey. Archive Pediatric Adolescence Medicine. 2002;156:269–275. doi: 10.1001/archpedi.156.3.269. [DOI] [PubMed] [Google Scholar]
- Saldiva SRDM, Escuder MM, Venâncio SI, Benicio MHA, Assis AMO, Oliveira LPM, Barreto ML. Is overweight a risk factor for wheezing in pre-school children? A study in 14 Brazilian communities. Public Health Nutrition. 2007;10(9):878–882. doi: 10.1017/S1368980007352464. [DOI] [PubMed] [Google Scholar]
- Schachter LM, Peat JK, Salome CM. Asthma and atopy in overweight children. Thorax. 2003;58(12):1031–1035. doi: 10.1136/thorax.58.12.1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shamssain MH. The association between overweight and respiratory symptoms in schoolchildren. Pediatric Asthma, Allergy and Immunology. 2006;19(1):19–25. [Google Scholar]
- Sithole F, Douwes J, Burstyn I, Veugelers P. Body mass index and childhood asthma: a linear association? Journal of Asthma. 2008;45(6):473–477. doi: 10.1080/02770900802069117. [DOI] [PubMed] [Google Scholar]
- Taveras EM, Rifas-Shiman SL, Camargo CA, Jr, Gold DR, Litonjua AA, Oken E, Weiss ST, Gillman MW. Higher adiposity in infancy associated with recurrent wheeze in a prospective cohort of children. Journal of Allergy and Clinical Immunology. 2008;121(5):1161–1166.1163e. doi: 10.1016/j.jaci.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- To T, Vydykhan TN, Dell S, Tassoudji M, Harris JK. Is obesity associated with asthma in young children? The Journal of Pediatrics. 2004;144(2):162–168. doi: 10.1016/j.jpeds.2003.09.047. [DOI] [PubMed] [Google Scholar]
- Trost SG, Kerr LM, Ward DS, Pate RR. Physical activity and determinants of physical activity in obese and non-obese children. International Journal of Obesity and Related Metabolic Disorders. 2001;25(6):822–829. doi: 10.1038/sj.ijo.0801621. [DOI] [PubMed] [Google Scholar]
- Tsai HJ, Tsai AC, Nriagu J, Ghosh D, Gong M, Sandretto A. Associations of BMI, TV-watching time and physical activity on respiratory symptoms and asthma in 5th grade schoolchildren in Taipei, Taiwan. Journal of Asthma. 2007;44(5):397–401. doi: 10.1080/02770900701364304. [DOI] [PubMed] [Google Scholar]
- Vahlkvist S, Pedersen S. Fitness, daily activity and body composition in children with newly diagnosed, untreated asthma. Allergy. 2009;64(11):1649–1655. doi: 10.1111/j.1398-9995.2009.02081.x. [DOI] [PubMed] [Google Scholar]
- van Veen IH, Ten Brinke A, Sterk PJ, Rabe KF, Bel EH. Airway inflammation in obese and nonobese patients with difficult-to-treat asthma. Allergy. 2008;63(5):570–574. doi: 10.1111/j.1398-9995.2007.01597.x. [DOI] [PubMed] [Google Scholar]
- Van Wonderen KE, Van Der Mark LB, Mohrs J, Bindels PJ, Van Aalderen WM, Ter Riet G. Different definitions in childhood asthma: how dependable is the dependent variable? European Respiratory Journal. 2010;36(1):48–56. doi: 10.1183/09031936.00154409. [DOI] [PubMed] [Google Scholar]
- Vargas PA, Perry TT, Robles E, Jo CH, Simpson PM, Magee JM, Felid CR, Hakkak R, Carroll PA, Jones SM. Relationship of body mass index with asthma indicators in head start children. Annals of Allergy, Asthma and Immunology. 2007;99(1):22–28. doi: 10.1016/S1081-1206(10)60616-3. [DOI] [PubMed] [Google Scholar]
- Varraso R, Siroux V, Maccario J, Pin I, Kauffmann F. Asthma Severity Is Associated with Body Mass Index and Early Menarche in Women. American Journal of Respiratory and Critical Care Medicine. 2005;171(4):334–339. doi: 10.1164/rccm.200405-674OC. [DOI] [PubMed] [Google Scholar]
- Vázquez-Nava F, Morales Romero J, Crodova Fernandez JA, Saldivar-Gonzalez AH, Vázquez-Rodriguez CF, Barrientos Gomez Mdel C, Lin-Ochoa D, Vázquez Rodriguez EM. Association between obesity and asthma in preschool Mexican children. ScientificWorldJournal. 2010;10:1339–1346. doi: 10.1100/tsw.2010.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vignolo M, Silvestri M, Parodi A, Pistorio A, Battistini E, Rossi GA, Aicardi G. Relationship between body mass index and asthma characteristics in a group of Italian children and adolescents. Journal of Asthma. 2005;42(3):185–189. [PubMed] [Google Scholar]
- von Kries R, Hermann M, Grunert VP, von Mutius E. Is obesity a risk factor for childhood asthma? Allergy. 2001;56(4):318–322. doi: 10.1034/j.1398-9995.2001.00727.x. [DOI] [PubMed] [Google Scholar]
- von Mutius E, Schwartz J, Neas LM, Dockery D, Weiss ST. Relation of body mass index to asthma and atopy in children: the National Health and Nutrition Examination Study III. Thorax. 2001;56(11):835–838. doi: 10.1136/thorax.56.11.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werk LN, Steinbach S, Adams WG, Bauchner H. Beliefs about diagnosing asthma in young children. Pediatrics. 2000;105(3 Pt 1):585–590. doi: 10.1542/peds.105.3.585. [DOI] [PubMed] [Google Scholar]
- Wickens K, Barry D, Friezema A, Rhodius R, Bone N, Purdie G, Crane J. Obesity and asthma in 11-12 year old New Zealand children in 1989 and 2000. Thorax. 2005;60(1):7–12. doi: 10.1136/thx.2002.001529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wulff K, Cummings GG, Marck P, Yurtseven O. Medication administration technologies and patient safety: a mixed-method systematic review. Journal of Advanced Nursing. 2011;67(10):2080–2095. doi: 10.1111/j.1365-2648.2011.05676.x. [DOI] [PubMed] [Google Scholar]
- Yoo S, Kim HB, Lee SY, Kim BS, Kim JH, Yu JH, Kim BJ, Hong SJ. Association between obesity and the prevalence of allergic diseases, atopy and bronchial hyperresponsiveness in Korean adolescents. International Archives of Allergy and Immunology. 2011;154(1):42–48. doi: 10.1159/000319207. [DOI] [PubMed] [Google Scholar]
- Zahran HS, Bailey C, Garbe P. Vital signs: asthma prevalence, disease characteristics and self-management education: United States, 2001--2009. MMWR Surveillence Summary. 2011;60(17):547–552. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.