Abstract
Context:
Insomnia is a major health problem with significant psychological, health, and economic consequences. However, availability to one of the most effective insomnia treatments, Cognitive Behavioral Therapy (CBT), is significantly limited. The Internet may be a key conduit for delivering this intervention.
Objective:
To evaluate the efficacy of a structured behavioral Internet intervention for adults with insomnia.
Design, Setting, and Participants:
45 adults were randomly assigned to an Internet intervention (n=22) or wait-list control group (n=23). 44 eligible participants were included in the analyses (mean age, 44.86±11.03 years; 34 women), who had, on average, a history of sleep difficulties greater than 10 years (10.59±8.89).
Intervention:
The Internet intervention is based on well-established face-to-face CBT, incorporating the primary components of sleep restriction, stimulus control, sleep hygiene, cognitive restructuring, and relapse prevention.
Main Outcome Measure(s):
The Insomnia Severity Index (ISI) and daily sleep diary data were used to determine changes in insomnia severity and the main sleep variables, including wake after sleep onset (WASO) and sleep efficiency (SE).
Results:
Intent-to-treat analyses showed that scores on the ISI significantly improved from 15.73 (95% CI, 14.07-17.39) to 6.59 (95% CI, 4.73-8.45) for the Internet group, but did not change for the control group, 16.27 (95% CI, 14.61-17.94) to 15.50 (95% CI, 13.64-17.36), F (1, 42) = 29.64, p<.001. The Internet group maintained their gains at six month follow-up. Internet participants also achieved significant decreases in WASO (55%; 95% CI, 34%-76%) and increases in SE (16%; 95% CI, 9%-22%) compared to the non-significant control group changes of WASO (8%; 95% CI, −17%-33%) and SE (3%; 95% CI, −4%-9%).
Conclusions:
Participants who received the Internet intervention for insomnia significantly improved their sleep, whereas the control group did not change. The Internet appears to have considerable potential in delivering a structured behavioral program for insomnia.
INTRODUCTION
Insomnia is a significant public health problem, with one-third of the adult population reporting symptoms of insomnia, and approximately 10% who meet diagnostic criteria for an insomnia disorder1-4. The considerable costs of insomnia include psychological ramifications (decreased quality of life and impaired daytime functioning)4, 5, personal and public health consequences (impaired cognitive functioning and increased health services utilization)4, 6, 7, and staggering economic impact (estimated $41 billion in annual reduced productivity)8, 9. In spite of its prevalence and cost, only a small percentage of individuals with insomnia actually receive any type of treatment2, 10.
Cognitive Behavioral Therapy (CBT) for insomnia11, 12, a psychological treatment that targets the maladaptive behaviors and dysfunctional thoughts that perpetuate sleep problems, is one of the most effective treatments for insomnia13, 14. The 2005 NIH State-of-the-Science Conference on insomnia concluded that CBT “has been found to be as effective as prescription medications are for short-term treatment of chronic insomnia. Moreover, there are indications that the beneficial effects of CBT, in contrast to those produced by medications, may last well beyond the termination of active treatment”15. In addition, individuals receiving CBT rate this intervention as more effective and acceptable than medication16, 17.
Unfortunately, availability of CBT is severely limited for many reasons, including lack of trained clinicians, poor geographical distribution of knowledgeable professionals, expense, and inaccessibility to treatment and clinicians18. One way to overcome these barriers is to use the Internet to deliver treatment, potentially making this highly effective intervention more widely available to an underserved patient population. The Internet has already become a critical source of health-care and medical information19, 20. Although the vast majority of health websites provide static information19, 21, there is a growing research literature on the development and evaluation of “Internet Interventions”22-25. These online programs are typically behaviorally-based interventions that have been operationalized and transformed for delivery via the Internet. They are usually highly structured; self or semi-self guided; based on effective face-to-face treatment; personalized to the user; interactive; enhanced by graphics, animations, audio, and possibly video; and tailored to provide follow-up and feedback24.
The current study investigates the feasibility and efficacy of using the Internet to deliver a fully automated CBT intervention for adults with primary insomnia. This Internet program, SHUTi (Sleep Healthy Using The Internet, www.shuti.net), incorporates the primary treatment components of CBT for insomnia, including sleep restriction, stimulus control, cognitive restructuring, sleep hygiene, and relapse prevention. We hypothesized that adults randomly assigned to receive SHUTi would experience significant reductions in the overall severity of insomnia as well as show greater improvements compared to those in a wait-list control group in wake after sleep onset (WASO) and sleep onset latency (SOL). We also expected Internet participants to show significant improvements in sleep efficiency (SE%), total sleep time (TST), number of nighttime awakenings, and self-ratings of sleep restoration and restfulness upon awakening.
METHODS
Participants
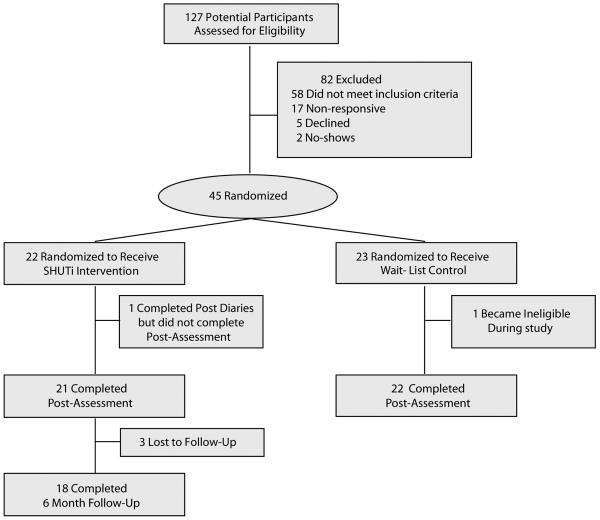
Participants were recruited through newspaper advertisements, online postings, radio broadcasts, public service announcements, flyers, and physician referrals in the central Virginia area (see Figure 1). To participate in the study, adults between 18-65 years old had to meet criteria for Primary Insomnia (DSM-IV-TR)26, report sleep complaints for at least six months (difficulty initiating sleep, maintaining sleep, and/or early morning awakenings), endorse sleep difficulties three or more nights per week, report significant daytime impairments due to their sleep disturbance (e.g., fatigue, performance impairment), and have regular Internet access. Participants were ineligible if they met criteria for other sleep disorders (e.g., Sleep Apnea) or major medical or psychiatric disorders that could account for the sleep disruption. Participants were also excluded for the following reasons: 1) current psychological treatment, 2) unstable medication regimens, 3) shift work interfering with the establishment of regular sleep patterns, and 4) pregnancy during the study. This study was approved by the Internal Review Board at the University of Virginia Health System. Written, informed consent was obtained from all individuals who participated. Participants were compensated $100 for completion of both in-person assessments.
Figure 1.
Study Enrollment Flow
Study Procedures
Interested individuals were screened sequentially through an online Interest Form, a 15-minute phone screen, and an in-person semi-structured interview. Participants also completed questionnaires to further assess sleep behaviors and psychological functioning. After initial assessment, participants were taught how to complete sleep diaries and navigate the online program. To protect confidentiality, participants were assigned unique usernames and passwords for purposes of login.
Participants were randomly assigned to either the experimental (Internet) or control condition following pre-assessment based on a pre-set computer-generated randomization schedule established by the study project coordinators (F.T. and D.S.). Participants completed, at baseline, ten sleep diary entries within a two week period before being notified of their group assignment by email. Automated reminders to complete diary entries were sent daily via email. Internet participants were then granted access to the intervention for nine weeks. After the nine-week intervention period, all participants completed an additional ten days of online sleep diaries within a two week period and then returned to the research center to complete a second in-person assessment. Internet participants were contacted at six month follow-up and asked to complete a brief online questionnaire that included the Insomnia Severity Index (ISI)11, 27. Control participants were given access to SHUTi following post-assessment, but no follow-up data was collected.
Procedures for the Internet intervention for insomnia
SHUTi is based on well-established face-to-face CBT for insomnia11, 28. It can be conceptualized as six Cores that include behavioral, educational, and cognitive techniques. These Cores make up the treatment content of SHUTi. The first Core, Overview, introduces the intervention and provides a rationale for treatment. There are two Behavioral Cores that incorporate sleep restriction29 and stimulus control30, 31, providing a set of “rules” to follow in order to regulate the sleep-wake schedule and strengthen the association between the bed/bedroom, bedtime, and sleep. Stimulus control procedures involve: going to bed only when sleepy, getting out of bed when unable to sleep and returning to bed only when sleep is imminent, curtailing sleep-incompatible activities in the bedroom (e.g., reading, problem-solving, watching TV), avoiding daytime napping, and arising at the same hour every day. Sleep restriction involves putting a limit on the amount of time spent in bed (sleep window) to the actual amount of sleep in order to strengthen the homeostatic sleep drive and increase sleep efficiency. The Educational Core (also called Sleep Hygiene) focuses on general education about sleep and improving sleep hygiene practices (e.g., increasing exercise; avoiding nicotine, caffeine, and drinking alcohol before bedtime). The Cognitive Core (also called Cognitive Restructuring) attempts to address and change the unhelpful beliefs (e.g., the absolute necessity for 8 hours of sleep) and thoughts (e.g., worry about the consequences of insomnia) about sleep/insomnia that may exacerbate sleep difficulties. Finally, the last Core, Consolidation/Relapse Prevention, integrates the behavioral, educational, and cognitive elements; promotes adherence; generalizes the information; helps identify risk situations; and incorporates strategies to reduce relapse. The structured nature of insomnia treatment makes it an ideal intervention for adaptation as a Web program and delivered via the Internet.
At the beginning of each new Core, participants completed the ISI online and received new recommendations for sleep restriction treatment based on the participant's previous week of sleep diaries. These individually-tailored recommendations were computed automatically using algorithms developed for the Internet intervention. On subsequent visits to the website during the seven days before beginning new treatment Cores, participants were encouraged to complete their daily online sleep diary and review relevant information from completed treatment Cores. Participants were unable to move forward to the next Core until the prescribed time elapsed. If participants completed fewer than five diaries in a given week, they could move forward to the next Core, but they were not given new recommendations for sleep restriction.
The highly interactive intervention presents information through the use of text, graphics, and animations. It also utilizes vignettes, quizzes, and brief games as a way of delivering pertinent information. Automated emails are also sent when it is time to complete a new treatment Core, and mid-week reminders to enter sleep diaries, implement learned strategies, and begin the new Core in four days. Other automated emails include disuse reminders and relapse prevention prompts.
Dependent Measures
Interviews
At pre- and post-assessment, participants were asked a series of descriptive and demographic questions as well as their retrospective accounts of their sleep history and sleep impairment. The in-person interview was based on a clinical interview11 designed to obtain a sleep history and assess for psychiatric and medical comorbidity, including other sleep disorders. The PRIME-MD32 was also administered to further screen for co-morbid psychiatric disorders.
Sleep Diary11
Participants completed online sleep diaries every day during the pre- and post-assessment periods (10 diaries within a two week period were required to move forward in the study). Internet participants were also encouraged to complete sleep diaries each day while using the Internet intervention. The diary consisted of ten standard questions, including: time to fall asleep; number and time length of any awakenings at night; time of awakening and arising from bed in the morning; length of any naps; subjective sense of how refreshed they felt upon awakening, as well as how sound they slept during the night; and amount of medication/alcohol/drug use. Data suggests that tracking sleep parameters through these diaries can provide a more comprehensive understanding of sleep problems than can typically be achieved using polysomnography administered over one or two nights33.
Insomnia Severity Index (ISI)11, 27
This seven-item measure provides a quantitative index of overall sleep impairment. Participants rate severity of problems with sleep onset, sleep maintenance, and early morning awakening; interference with daytime functioning; how noticeable the impairment is to others; distress/concern caused by the sleep problem; and satisfaction with the current sleep pattern on a 5-point Likert Scale. Scores range from 0-28, with higher scores indicating more severe insomnia. The ISI has been shown to be a valid and reliable measure, sensitive to changes in treatment studies27. It was administered at pre- and post-assessment for all participants as well as at six month follow-up and before each of the program Cores for participants who received SHUTi.
Statistical Analysis
Descriptive statistics were computed, including age, gender, marital status, education, comfort with the Internet, history of sleep difficulties, and nights per week experiencing sleep difficulties. One-way ANOVAs were used to compare the groups on the continuous variables (e.g., age, education), and chi-square tests were used with the categorical variables (e.g., gender, race) at baseline. Because the main sleep outcome variables met parametric assumptions, 2 (Internet and control group) X 2 (pre- and post-assessment) repeated-measures ANOVAs were conducted to compare pre- to post- changes. Paired-sample t-tests were used to examine time effects within each condition if the overall interaction effect was significant, as well as to examine the changes in ISI scores from post to six month follow-up. An intent-to-treat analysis was conducted to analyze the ISI data using last observation carried forward (LOCF). Completers analyses were used for the sleep diary data as all participants provided pre and post diary data. Sample-size calculations were based on previous CBT self-help for insomnia trial data34 reporting effect size differences between the Internet intervention and wait-list control conditions on pre to post changes on key sleep variables, including the ISI (d=1.26), WASO (d=.74), SOL (d=.26), SE (d=.68). Therefore, expecting differences at post treatment between a self-help Internet intervention for insomnia and a wait-list control group using a medium effect size of .5, with power of 80%, p=.01, and 15% attrition, a minimum of 40 subjects (20 in each group) was needed. All analyses were conducted using the Statistical Package for the Social Sciences (SPSS for Windows version 14 SPSS Inc, Chicago, Ill).
RESULTS
Forty-five participants were enrolled from February, 2007 to June, 2008, with 22 participants randomly assigned to receive immediate Internet (SHUTi) treatment and 23 serving as wait-list controls. Attrition was 4% (2 of 45 participants) from pre- to post-assessment, with one participant (Internet condition) completing post online sleep diaries but not returning to complete the in-person post-assessment, and one participant (control) being dropped from analyses after he began a night-shift job during the study (exclusionary criteria) and became ineligible. We obtained data from 18 of the 22 Internet participants (82%) at six month follow-up. Intention-to-treat for the ISI analyses are based on our final subject pool of 44 participants (22 Internet and 22 control).
No significant differences were found between the Internet intervention and wait-list control groups on any of the baseline characteristics, including age, gender, years of education, marital status, history of sleep difficulties, and sleep problem nights/week (See Table 1). Participants were mostly married (68%) females (77%), approximately 45 years old (44.86±11.03), with more than 16 years of education (16.59±2.86). Participants reported sleep difficulties an average of over 10 years (127.09±106.73 months), and were experiencing disruptive sleep more than 5 nights per week (5.52±1.43). This sample is comparable to the baseline demographic and clinical characteristics of other trials of insomnia34-38. Overall, 95% of the participants indicated that they considered themselves at least “comfortable” (a 2 on a 0-4 scale) using the Internet. All participants reported that they check their email and use the Internet at least once each week; 91% stated that they check email at least daily; and 86% stated that they use the Internet at least daily. There were no significant group differences on comfort with and use of the Internet and email.
Table 1.
Baseline Characteristics of Participants
| Characteristic | Internet (n = 22) |
Control (n = 22) |
Total (n = 44) |
P Value* |
|---|---|---|---|---|
| Age | 44.68 (10.61) | 45.05 (11.67) | 44.86 (11.03) | .91 |
| Gender | ||||
| Women | 18 | 16 | 34 | .47 |
| Men | 4 | 6 | 10 | |
| Marital Status | ||||
| Married | 18 | 12 | 30 | .10 |
| Separated/Divorced | 0 | 5 | 5 | |
| Never Married | 3 | 4 | 7 | |
| Other | 1 | 1 | 2 | |
| Years of Education | 16.50 (3.11) | 16.68 (2.64) | 16.59 (2.86) | .84 |
| History of Sleep Difficulties, Mean Months | 121.73 (99.12) | 132.45 (115.94) | 127.09 (106.73) | .74 |
| Sleep Difficulties (Nights per Week)** | 5.14 (1.54) | 5.91 (1.24) | 5.52 (1.43) | .07 |
P values are based on analysis of variance or Pearson χ2 tests.
Nights per Week refers to the number of nights per week experiencing sleep difficulties.
Insomnia Severity
To evaluate changes in insomnia severity, participants completed the ISI at pre- and post-assessment. The Internet group also completed the ISI at six month follow-up. For the pre- to post-assessment, there was a significant Group X Time interaction effect showing a marked improvement from pre- to post-assessment in the Internet group, and little change in the control group, F (1, 42) = 29.64, p<.001. At pre-assessment, there were no differences in insomnia severity between the two groups (Internet and control group means = 15.73 (95% CI, 14.07-17.39) and 16.27 (95% CI, 14.61-17.94), respectively), but mean ISI scores at post-assessment were 6.59 (95% CI, 4.73-8.45) for the Internet group and 15.50 (95% CI, 13.64-17.36) for the control group. The Internet group also maintained these gains at six months (7.32, 95% CI, 5.05-9.59), with no significant increase in ISI scores from post to six month follow-up (see Figure 2).
Figure 2.
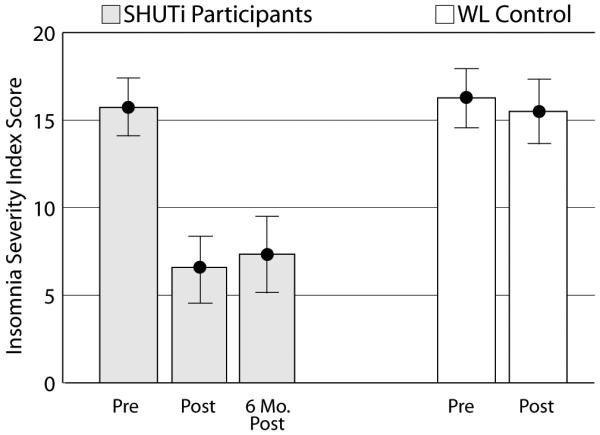
ISI Scores at Pre-, Post-, and Six Month Follow-Up
A significant Group X Time interaction effect showed a marked improvement from pre- to post-assessment in the Internet intervention group, and little change in the control group, F (1, 42) = 29.64, p<.001. The Internet group maintained their gains at 6 month follow-up (no significant change in ISI scores). Error bars indicate 95% confidence intervals.
Changes in ISI scores indicate not only statistically significant improvements after using SHUTi but clinically significant improvements as well. At baseline, no participant in either group fell in the “no clinically significant insomnia” category as defined by an ISI score of less than eight27. However, after SHUTi, 16 of the 22 (73%) Internet participants were in remission and in this category at post-assessment, whereas no control participant met this criterion, χ2 = 25.14, p <.001. At six month follow-up, 11 of the 18 (61%) Internet participants were still in remission, not a significant change from post-assessment.
Internet participants also completed the ISI before each treatment core, with 20 of the 22 participants completing the ISI at all seven time points. Review of the insomnia severity ratings throughout the Internet intervention indicate that the largest changes in scores occurred after completing the first behavior core stressing sleep restriction and stimulus control (ES = .32) and the final core stressing relapse prevention (ES = .26).
Sleep Variables
Repeated measures ANOVA examining the pre and post diary data showed a significant Time X Group interaction for WASO (p=.002), with the Internet group experiencing a 55% decrease (p≤.001; 95% CI, 34%-76%) and the control group decreasing WASO by only 8% (n.s.; 95% CI, −17%-33%). There was no significant interaction for SOL even though the Internet group decreased by 43% (95% CI, 13%-73%), while the control group decreased by 8% (95% CI, −19%-34%).
There was also a significant Time X Group interaction for sleep efficiency (p=.006), with a 16% (95% CI, 9%-22%) increase for the Internet group (p≤.001), and a 3% (95% CI, −4%-9%) increase for the control group (n.s.). There was a significant Time X Group interaction for number of nighttime awakenings (p = .01), with nighttime awakenings decreasing by 36% (p=.005; 95% CI, 16%-56%) for the Internet group, and the control group increasing awakenings by 1% (n.s.; 95% CI, −21%-19%). There was a trend toward a significant Time X Group interaction for total sleep time (p=.09), and no significant Time X Group interaction for time in bed. Participants were also asked to rate on the sleep diaries how restored they felt each morning and how restless/sound their sleep was each night. There were trends toward significant Time X Group interactions for feeling restored (p=.02) and soundness of sleep (p=.09).
Although medication titration was not specifically addressed in the intervention, exploratory analyses were conducted examining changes in prescription medication use. At baseline, 15 of the 44 participants (6 Internet and 9 control) reported taking prescription medication for sleep (including benzodiazepine receptor agonists or sedating antidepressants), with no significant differences between groups. At post-assessment, 4 Internet and 10 control participants reported taking these sleep medications (χ2 = 3.77, p=.05). No changes in medication use were noted between post-assessment and six month follow-up for the Internet participants.
COMMENT
This study demonstrates that using the Internet to deliver an interactive and tailored behavioral intervention for adults with insomnia can significantly decrease insomnia severity and contribute to overall sleep improvements. These results suggest that an Internet-based CBT for insomnia program may be an effective first step in providing care to adults with insomnia. Overall severity of insomnia, as measured by the ISI, significantly decreased for those who received the Internet intervention. While participants, on average, initially fell in the moderate severity range for insomnia, those who received SHUTi no longer met criteria for clinically significant insomnia at post-assessment and six month follow-up. Based on sleep diary data, significant improvements were found for wake after sleep onset, sleep efficiency, and number of nighttime awakenings for those who received the online program.
These findings contribute to the relatively small but growing Internet intervention literature24, 25, 39-41. Only one other published trial has examined the use of the Internet in treating insomnia in a program created and tested by researchers in Sweden42. However, that study found significant sleep improvements in both the treatment and control groups and had more substantial attrition than our study, making the findings difficult to interpret. They also utilized human support (therapists responding via e-mail) to promote adherence and monitor assignments, reducing the ability to widely disseminate that intervention without significant increase in cost.
The improvements in sleep after using SHUTi are very similar to those from other insomnia treatment outcome trials. In fact, the percentage change in sleep efficiency (+16%), was almost identical to that found in other CBT self-help bibliotherapy (+16%)34, group (15%)43, phone (21%)43, and face-to-face studies (+17%)37, as well as pharmacotherapy (+13%)44 studies. The results of this study are also consistent with the conclusions from a 2006 systematic and seminal review of the effectiveness of psychological and behavioral treatment of insomnia14. It is important to highlight that the treatment effect sizes found using this Internet intervention, which was delivered with no human support and at relatively low cost, are comparable to those found in face-to-face studies.
Although these findings are promising, they should be considered in light of several methodological limitations: (1) The sample used in this study was small and relatively homogenous, well-educated, and restricted to individuals with primary insomnia and no co-morbidities. Future studies should enroll larger and more heterogeneous samples to improve the generalizability of the findings. For example, it will be important to assess whether similar sleep improvements are found in patients with insomnia comorbid with medical or psychiatric problems. (2) This study had remarkably low attrition (4% at post-assessment), a rate much lower than the average attrition found in other Internet interventions (21%)40, which is likely due to the seemingly motivated, self-selected sample in this study. The level of motivation exhibited by this sample, reflected in their willingness to complete sleep diaries and the intervention Cores, may not be representative of the larger population of individuals with insomnia. (3) The findings presented here are based on self-report measures. Although sleep diaries represent a core assessment component in insomnia research45, polysomnography would be needed to confirm objective changes in sleep. (4) Participants were not blinded to their group assignment. Following completion of the initial diaries, participants knew whether they were receiving SHUTi or in the wait-list control group resulting in the potential for some bias in self-report measures. (5) Finally, this study utilized a wait-list control group which does not control for all nonspecific effects, such as participant expectation. Future studies should include placebo control groups who are provided with some type of intervention (such as patient education websites)22.
In summary, these findings provide support for the Internet as an efficacious method for delivering cognitive-behavioral treatment for insomnia. An Internet intervention has the potential of meeting the large unmet treatment need of the insomnia population by providing effective treatment through the Web. Although an Internet intervention may not be the treatment of choice for all patients, it may be a significant first step in a stepped care model of treatment46. Treating as many patients as possible with the least intensive treatment necessary to reach clinically significant outcomes allows more intensive resources (e.g., face-to-face CBT) to be allocated to those who require additional care. Although some patients may prefer face-to-face care, others may prefer treatment delivered over the Internet. An effective and inexpensive Internet intervention would expand treatment options for large numbers of adults with insomnia, especially those whose geographical location prohibits access to relevant care, and could be a substantive first-line treatment choice.
Table 2.
Sleep Diary Data Changes by Treatment Condition
| Internet | Control | |||||
|---|---|---|---|---|---|---|
| Sleep Variable & Time Period |
M (SD) | % Imp |
M (SD) | % Imp |
F | P Value |
| Primary Variables | ||||||
| WASO (N) | 22 | 22 | ||||
| Pre | 66.71 (40.81) | 56.43 (19.38) | F(1,42)=10.80 | p=.002 | ||
| Post | 29.89 (19.83)* | −55% | 51.81 (26.58) | −8% | ||
| SOL (N) | 22 | 22 | ||||
| Pre | 31.84 (27.90) | 35.43 (21.43) | F(1,42)=2.74 | p=.11 | ||
| Post | 18.12 (12.84) | −43% | 32.75 (16.49) | −8% | ||
| Secondary Variables | ||||||
| Sleep Efficiency (N) | 22 | 22 | ||||
| Pre | 77.3 (14.7) | 79.6 (7.7) | F(1,42)=8.29 | p=.006 | ||
| Post | 89.3 (5.0)* | 16% | 81.6 (7.3) | 3% | ||
| Total Sleep Time (N) | 22 | 22 | ||||
| Pre | 349.92 (88.00) | 365.65 (61.46) | F(1,42)=2.95 | p=.09 | ||
| Post | 404.92 (61.46) | 16% | 380.04 (59.82) | 4% | ||
| # of Awakenings (N) | 22 | 22 | ||||
| Pre | 2.38 (1.48) | 2.38 (1.02) | F(1,42)=6.80 | p=.01 | ||
| Post | 1.52 (1.07)** | −36% | 2.40 (1.39) | 1% | ||
| Time in Bed (N) | 22 | 22 | ||||
| Pre | 448.70 (61.66) | 457.50 (53.41) | F(1,42)=.01 | p=.92 | ||
| Post | 453.55 (67.38) | 1% | 464.59 (51.90) | 2% | ||
| Restored (N) | 22 | 22 | ||||
| Pre | 2.69 (.65) | 2.71 (.62) | F(1,42)=5.69 | p=.02 | ||
| Post | 3.21 (.70) | 19% | 2.88 (.66) | 6% | ||
| Restless (N) | 22 | 22 | ||||
| Pre | 2.83 (.59) | 2.83 (.64) | F(1,42)=3.12 | p=.09 | ||
| Post | 3.23 (.61) | 14% | 2.94 (.74) | 4% | ||
p ≤ .001 P value is based on paired-samples t tests to examine time effects within each treatment condition.
p = .005 P value is based on paired-samples t tests to examine time effects within each treatment condition.
Acknowledgments
Funding/Support: This study was funded by grant R34MH70805 from the National Institutes of Health/National Institute of Mental Health.
Role of the Sponsors: The National Institutes of Health reviewed the design of the study and annual progress reports, but did not participate in conducting the study; in the collection, management, analysis, or interpretation of the data; and in the preparation, review, or approval of the manuscript.
We thank Jonathan Cole Sletten and Dominion Digital for their expertise in developing the SHUTi program. Also, we thank William Pascarella, BS, for his technical support, Holly Lord, PhD, for her statistical support, Michelle Hilgart, M.Ed., for design expertise, and Kaveh Ardalan for his help examining the medication usage data. Compensation or course credit was provided to these individuals in association with their work.
Footnotes
Trial Registration: ClinicalTrials.gov identifier: NCT00328250; URL: http://clinicaltrials.gov/ct2/show/NCT00328250
Financial Disclosures: None reported.
Previous Presentations: Data reported here has been or is scheduled to be presented in part at the following conferences: Third Meeting of the International Society for Research on Internet Interventions, October 11, 2007, Charlottesville, Virginia; 22nd Annual Meeting of the Associated Professional Sleep Societies, June 11, 2008, Baltimore, Maryland; 19th Congress of the European Sleep Research Society, September 12, 2008, Glasgow, Scotland; Association for Behavioral and Cognitive Therapies 42nd Annual Convention, November 14, 2008, Orlando, Florida.
REFERENCES
- 1.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders, an opportunity for prevention? JAMA. 1989;262:1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 2.Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and its treatment: Prevalence and correlates. Arch Gen Psychiatry. 1985;42:225–232. doi: 10.1001/archpsyc.1985.01790260019002. [DOI] [PubMed] [Google Scholar]
- 3.Ohayon MM. Epidemiology of insomnia: What we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 4.Simon GE, VonKorff M. Prevalence, burden, and treatment of insomnia in primary care. Am J Psychiatry. 1997;154:1417–1423. doi: 10.1176/ajp.154.10.1417. [DOI] [PubMed] [Google Scholar]
- 5.Leger D, Scheuermaier K, Philip P, Paillard M, Guilleminault C. SF-36: Evaluation of quality of life in severe and mild insomniacs compared with good sleepers. Psychosom Med. 2001;63:49–55. doi: 10.1097/00006842-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Moul DE, Nofzinger EA, Pilkonis PA, Houck PR, Miewald JM, Buysse DJ. Symptom reports in severe chronic insomnia. Sleep. 2002;25:553–563. [PubMed] [Google Scholar]
- 7.Kapur VK, Redline S, Nieto FJ, Young TB, Newman AB, Henderson JA. The relationship between chronically disrupted sleep and healthcare use. Sleep. 2002;25:289–296. [PubMed] [Google Scholar]
- 8.Stoller MK. Economic effects of insomnia. Clin Ther. 1994;16:873–97. discussion 854. [PubMed] [Google Scholar]
- 9.Ozminkowski RJ, Wang S, Walsh JK. The direct and indirect costs of untreated insomnia in adults in the United States. Sleep. 2007;30:263–273. doi: 10.1093/sleep/30.3.263. [DOI] [PubMed] [Google Scholar]
- 10.WB&A Market Research . 2007 Sleep in America Poll: Summary of findings. National Sleep Foundation; Washington, DC: 2007. [Google Scholar]
- 11.Morin CM. Insomnia: Psychological Assessment and Management. The Guilford Press; New York: 1993. [Google Scholar]
- 12.Morin CM, Espie CA. Insomnia: A Clinical Guide to Assessment and Treatment. Kluwer Academic/Plenum Publishers; New York: 2003. [Google Scholar]
- 13.Edinger JD, Wohlgemuth WK, Radtke RA, Marsh GR, Quillian RE. Does cognitive-behavioral insomnia therapy alter dysfunctional beliefs about sleep? Sleep. 2001;24:591–599. doi: 10.1093/sleep/24.5.591. [DOI] [PubMed] [Google Scholar]
- 14.Morin CM, Bootzin RR, Buysse DJ, Edinger JD, Espie CA, Lichstein KL. Psychological and behavioral treatment of insomnia: Update of the recent evidence (1998-2004) Sleep. 2006;29:1398–1414. doi: 10.1093/sleep/29.11.1398. [DOI] [PubMed] [Google Scholar]
- 15.NIH State-of-the-Science Panel Manifestations and management of chronic insomnia in adults. 2005;22:1–30. [PubMed] [Google Scholar]
- 16.Morin CM, Gaulier B, Barry T, Kowatch RA. Patients' acceptance of psychological and pharmacological therapies for insomnia. Sleep. 1992;15:302–305. doi: 10.1093/sleep/15.4.302. [DOI] [PubMed] [Google Scholar]
- 17.Morin CM, Colecchi C, Stone J, Sood R, Brink D. Behavioral and pharmacological therapies for late-life insomnia: A randomized controlled trial. JAMA. 1999;281:991–999. doi: 10.1001/jama.281.11.991. [DOI] [PubMed] [Google Scholar]
- 18.Edinger JD, Means MK. Cognitive-behavioral therapy for primary insomnia. Clin Psychol Rev. 2005;25:539–558. doi: 10.1016/j.cpr.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 19.Fox S, Fallows D. Internet health resources. Pew Internet & American Life Project; Washington, DC: 2003. Available from: http://www.pewinternet.org/PPF/r/165/report_display.asp. [Google Scholar]
- 20.Fox S. Health information online. Pew Internet & American Life Project; Washington, DC: 2005. [Google Scholar]
- 21.Rabasca L. Taking telehealth to the next step. Monitor on Psychology. 2000;31:36–37. [Google Scholar]
- 22.Tate DF, Wing RR, Winett RA. Using internet technology to deliver a behavioral weight loss program. JAMA. 2001;285:1172–1177. doi: 10.1001/jama.285.9.1172. [DOI] [PubMed] [Google Scholar]
- 23.Tate DF, Jackvony EH, Wing RR. Effects of internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: A randomized trial. JAMA. 2003;289:1833–1836. doi: 10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- 24.Ritterband LM, GonderFrederick LA, Cox DJ, Clifton AD, West RW, Borowitz SM. Internet interventions: In review, in use, and into the future. Prof Psychol Res Pr. 2003;34:527–534. [Google Scholar]
- 25.Marks IM, Cavanagh K, Gega L. Hands-on Help: Computer-Aided Psychotherapy. Psychology Press; Hove, England and New York: 2007. [Google Scholar]
- 26.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Fourth Edition ed. American Psychiatric Association; Washington, D.C.: 2000. [Google Scholar]
- 27.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 28.Morin CM. Relief from Insomnia: Getting the Sleep of Your Dreams. Doubleday; New York: 1996. [Google Scholar]
- 29.Spielman AJ, Saskin P, Thorpy MJ. Treatment of chronic insomnia by restriction of time in bed. Sleep. 1987;10:45–56. [PubMed] [Google Scholar]
- 30.Bootzin RR. Stimulus control treatment for insomnia. Proceedings of the American Psychological Association. 1972;7:395–396. [Google Scholar]
- 31.Bootzin RR. Effects of self-control procedures for insomnia. American Journal of Clinical Biofeedback. 1979;2:70–77. [Google Scholar]
- 32.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 33.Morin CM, Hauri PJ, Espie CA, Spielman AJ, Buysse DJ, Bootzin RR. Nonpharmacologic treatment of chronic insomnia: An American Academy of Sleep Medicine review. Sleep. 1999;22:1134–1156. doi: 10.1093/sleep/22.8.1134. [DOI] [PubMed] [Google Scholar]
- 34.Mimeault V, Morin CM. Self-help treatment for insomnia: Bibliotherapy with and without professional guidance. J Consult Clin Psychol. 1999;67:511–519. doi: 10.1037//0022-006x.67.4.511. [DOI] [PubMed] [Google Scholar]
- 35.Morin CM, Beaulieu-Bonneau S, LeBlanc M, Savard J. Self-help treatment for insomnia: A randomized controlled trial. Sleep. 2005;28:1319–1327. doi: 10.1093/sleep/28.10.1319. [DOI] [PubMed] [Google Scholar]
- 36.Belleville G, Guay C, Guay B, Morin CM. Hypnotic taper with or without self-help treatment of insomnia: A randomized clinical trial. J Consult Clin Psychol. 2007;75:325–335. doi: 10.1037/0022-006X.75.2.325. [DOI] [PubMed] [Google Scholar]
- 37.Edinger JD, Wohlgemuth WK, Radtke RA, Marsh GR, Quillian RE. Cognitive behavioral therapy for treatment of chronic primary insomnia: A randomized controlled trial. JAMA. 2001;285:1856–1864. doi: 10.1001/jama.285.14.1856. [DOI] [PubMed] [Google Scholar]
- 38.Harvey AG, Stinson K, Whitaker KL, Moskovitz D, Virk H. The subjective meaning of sleep quality: A comparison of individuals with and without insomnia. Sleep. 2008;31:383–393. doi: 10.1093/sleep/31.3.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Murray E, Burns J, See TS, Lai R, Nazareth I. Interactive health communication applications for people with chronic disease. Cochrane Database Syst Rev. 2005:CD004274. doi: 10.1002/14651858.CD004274.pub4. [DOI] [PubMed] [Google Scholar]
- 40.Wantland D, Portillo C, Holzemer W, Laughter R, McGhee E. The effectiveness of web-based vs. non-web-based interventions: A meta-analysis of behavioral change outcomes. J Med Internet Res. 2004;6:e40. doi: 10.2196/jmir.6.4.e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Griffiths KM, Christensen H. Review of randomised controlled trials of internet interventions for mental health disorders and related conditions. Clin Psychol. 2006;10:16–29. [Google Scholar]
- 42.Strom L, Pettersson R, Andersson G. Internet-based treatment for insomnia: A controlled evaluation. J Consult Clin Psychol. 2004;72:113–120. doi: 10.1037/0022-006X.72.1.113. [DOI] [PubMed] [Google Scholar]
- 43.Bastien CH, Morin CM, Ouellet MC, Blais FC, Bouchard S. Cognitive-behavioral therapy for insomnia: Comparison of individual therapy, group therapy, and telephone consultations. J Consult Clin Psychol. 2004;72:653–659. doi: 10.1037/0022-006X.72.4.653. [DOI] [PubMed] [Google Scholar]
- 44.Sivertsen B, Omvik S, Pallesen S, et al. Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: A randomized controlled trial. JAMA. 2006;295:2851–2858. doi: 10.1001/jama.295.24.2851. [DOI] [PubMed] [Google Scholar]
- 45.Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29:1155–1173. doi: 10.1093/sleep/29.9.1155. [DOI] [PubMed] [Google Scholar]
- 46.Haaga DA. Introduction to the special section on stepped care models in psychotherapy. J Consult Clin Psychol. 2000;68:547–548. [PubMed] [Google Scholar]