Abstract
Background
Trachoma, caused by ocular Chlamydia trachomatis infection, is the leading infectious cause of blindess, but its prevalence is now falling in many countries. As the prevalence falls, an increasing proportion of individuals with clinical signs of follicular trachoma (TF) is not infected with C. trachomatis. A recent study in Tanzania suggested that other bacteria may play a role in the persistence of these clinical signs.
Methodology/Principal Findings
We examined associations between clinical signs of TF and ocular colonization with four pathogens commonly found in the nasopharnyx, three years after the initiation of mass azithromycin distribution. Children aged 0 to 5 years were randomly selected from 16 Gambian communitites. Both eyes of each child were examined and graded for trachoma according to the World Health Organization (WHO) simplified system. Two swabs were taken from the right eye: one swab was processed for polymerase chain reaction (PCR) using the Amplicor test for detection of C. trachomatis DNA and the second swab was processed by routine bacteriology to assay for the presence of viable Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus and Moraxella catarrhalis. Prevalence of TF was 6.2% (96/1538) while prevalence of ocular C. trachomatis infection was 1.0% (16/1538). After adjustment, increased odds of TF were observed in the presence of C. trachomatis (OR = 10.4, 95%CI 1.32–81.2, p = 0.03), S. pneumoniae (OR = 2.14, 95%CI 1.03–4.44, p = 0.04) and H. influenzae (OR = 4.72, 95% CI 1.53–14.5, p = 0.01).
Conclusions/Significance
Clinical signs of TF can persist in communities even when ocular C. trachomatis infection has been controlled through mass azithromycin distribution. In these settings, TF may be associated with ocular colonization with bacteria commonly carried in the nasopharnyx. This may affect the interpretation of impact surveys and the determinations of thresholds for discontinuing mass drug administration.
Author Summary
Trachoma, the world's leading infectious cause of blindness, is caused by ocular infection with the bacterium Chlamydia trachomatis. In low-prevalence settings and following mass treatment campaigns, clinically active follicular trachoma (TF) can be found in the absence of C. trachomatis infection. We carried out this study to investigate associations between ocular carriage of non-chlamydial pathogens and a clinical diagnosis of TF following a mass treatment campaign in The Gambia. We found that children who carried Streptococcus pneumoniae or Haemophilus influenza in their eyes were more likely to have been diagnosed with TF than children who did not carry these pathogens. In The Gambia, non-chlamydial pathogens may be inducing or exacerbating TF in the absence of C. trachomatis infection.
Introduction
Trachoma, caused by ocular infection with the intracellular bacterium Chlamydia trachomatis, remains the leading infectious cause of blindness world-wide. In 1986, The Gambia's first national blindness survey indicated that trachoma was a significant cause of blindness in the country with active trachoma affecting 17% of children aged 0–14 years and very high rates of trichiasis in those 15 years and older [1], [2]. In response to these findings, the National Eye Health Programme (formerly the National Eye Care Programme), supported by SightSavers International, established a network of Community Ophthalmic Nurses (CONs) trained and equipped to screen communities for active trachoma and to conduct trichiasis surgery. Since the 1980s, many trachoma endemic communities may have also benefited from water and sanitation interventions such as well digging and latrine construction programmes via the Departments of Water Resources and Community Development. A Healthy Eyes curriculum, focused on preventive eye care, was introduced into primary schools and a network of individuals (Nyateros or ‘Friends of the Eye’) trained in eye health and ocular first aid was established at the community level.
A decade later, the 1996 national survey found a substantially reduced prevalence of active trachoma (to just over 5% in 0–14 year olds nationally), but which remained above 10% in four regions of the country [2], [3]. In 2006, in the absence of a national survey, trachoma surveys were conducted in two regions (North Bank and Lower River Regions) and showed little change in overall trachomatous inflammation, follicular (TF) prevalence from 1996 [4]. On the basis of these data, The Gambia's plan for trachoma control using mass drug administration (MDA) with azithromycin was approved by the Director of Medical Services in 2006 and The Gambia received over 400,000 doses of azithromycin from the International Trachoma Initiative (ITI) to be distributed in 23 priority health districts. The Partnership for the Rapid Elimination of Trachoma trial (PRET) [5], [6] was embedded in this plan, with communities in four priority districts randomized to receive treatment annually for three years [as currently recommended by the World Health Organization (WHO)] or to stop treatment if the prevalence of TF or detected ocular C. trachomatis infection fell below 5%. The PRET study areas now have very low rates of both disease and C. trachomatis infection [7].
As the prevalence of TF has fallen in The Gambia, a disparity between clinical signs of disease and ocular C. trachomatis infection has been documented [4], [6], [8]. This finding has been mirrored in other communities following implementation of mass treatment [9]–[12] and in communitites where prevalence of TF is low [13]–[16]. It has been suggested that at least some of the TF now observed may be due to organisms other than C. trachomatis [4], [16]. In the present study, we aimed to investigate possible associations between ocular colonization with four bacterial pathogens commonly found in the nasopharnyx and a clinical diagnosis of TF following the implementation of the MDA campaign in The Gambia.
Methods
Ethics statement
Ethical approval was obtained from the London School of Hygiene and Tropical Medicine Ethics Committee and The Gambia Government/Medical Research Council Unit, The Gambia Joint Ethics Committee under study numbers SCC 1107v2 and L2011.25. Oral consent was obtained from the community leaders and informed written (thumbprint or signature) consent was obtained from each child's guardian at the time of examination. The use of thumbprints in the consent procedure was specifically approved by the ethics committees. The consent form was further signed by an independent witness.
Study design
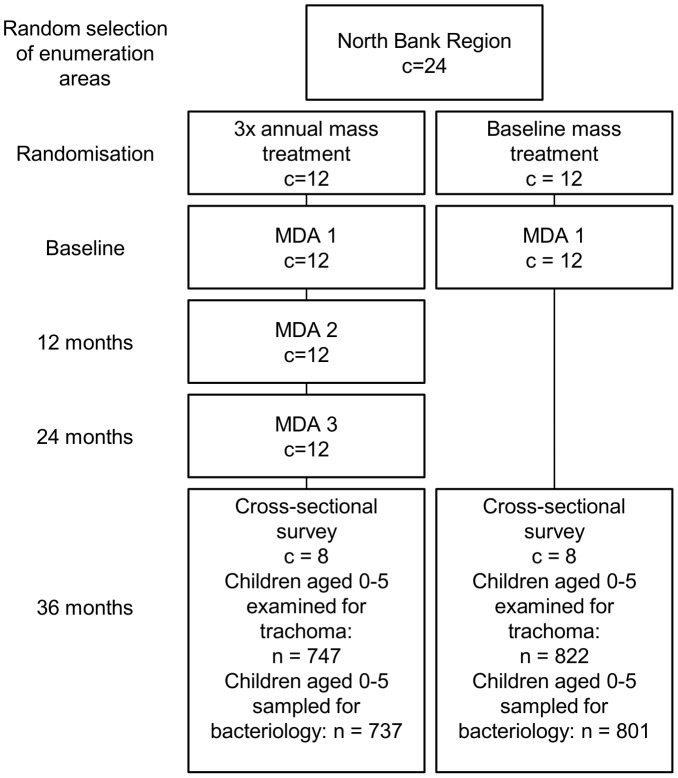
The PRET trial (ClinicalTrials.gov NCT00792922) was a cluster randomized trial (CRT) carried out in The Gambia, the design of which has been described elsewhere [5]. Briefly, clusters, or enumerations areas (EAs, population 600–800 individuals), were randomly sampled from four districts (two districts in the North Bank Region, two districts from the Western Region; 12 EAs per district). Twenty-four EAs received three annual, community-wide azithromycin treatments and 24 EAs received just one mass treatment at baseline. The 48 EAs were further randomized in a 2×2 factorial design to receive standard treatment coverage (one day visit to EAs by treatment team) versus enhanced coverage (two visits to each EA) during the mass treatments that took place. Randomization of EAs was stratified by district (six EAs per district allocated to either three mass treatments or one). The study described here is ancillary to the PRET trial; 16 of the 24 EAs from North Bank Region were included in this study (8 from each frequency allocation arm, Fig.? 1).
Figure 1. Study allocation.
Field methods
A cross-sectional survey took place during May and June 2011, coinciding with the 36 month follow-up survey of the PRET trial. For EAs randomized to receive three annual rounds of mass treatment, sample collection took place 12 months following the last round; for EAs randomized to receive a single treatment round, sample collection took place 36 months following treatment (Fig.? 1). One hundred children aged 0–5 years were randomly selected from each EA for participation. Eligible children were: resident in the EA, did not have an ocular condition precluding examination or specimen collection, willing to have a sample taken and had a guardian willing to provide consent. Children's faces were initially observed for the presence of nasal and ocular discharge and flies on the eyes. The upper eyelids of each child were everted and the tarsal conjunctiva graded for signs of clinical trachoma using the WHO simplified grading system [17]. Two photographs were then taken of the right everted upper tarsal conjunctiva for use in quality assurance as detailed elsewhere [7]. Samples were collected from the upper tarsal conjunctiva and lower fornix of the right eye using a Dacron swab. Upper tarsal conjunctival swabs were placed into dry vials while lower fornix swabs were placed into vials containing 1 ml skimmed-milk-tryptone-glucose glycerol transport medium (STGG) [18]. Samples were kept on wet ice in the field and frozen at −20°C within 10 hours. Samples were transferred to −70°C upon arrival at the MRC laboratory, within 2 weeks' time.
Laboratory methods
Upper tarsal conjunctival samples were processed for C. trachomatis infection using the Amplicor CT/NG kit (Roche Molecular Systems, Branchburg, NJ, USA) as previously described [5]. Lower fornix swabs were thawed at room temperature and cultured on blood and chocolate agar plates for the detection of Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus and Moraxella catarrhalis. Blood agar plates were incubated at 37°C in either 5% CO2 or under anaerobic conditions. Chocolate agar plates were incubated at 37°C in 5% CO2. Isolates were identified using conventional bacteriology techniques. All laboratory personnel were masked to the clinical trachoma grade.
Sample size
A sample size of 1568 subjects is required to detect an odds ratio (OR) of 2 for a univariate association between TF (anticipated to be 7%) and a bacterial pathogen (assumed to be present in 15% of participants without TF), assuming 80% power to detect univariate associations with 95% confidence. It was expected that a sample size of approximately 1600 children would be achieved from 16 EAs in which a random sample of 100 children was to be taken from each.
Analysis methods
Overall unadjusted prevalence is presented with corresponding exact binomial 95% confidence intervals (CI). Prevalence is also presented adjusted for age, sex and district using random effects logistic regression models to account for any underlying variation detected between households and between EAs.
The prevalence of TF was tabulated by each pathogen, age, sex, district, C. trachomatis infection and time since mass treatment (12 months for those in the annual treatment arm versus 36 months for those in the baseline treatment arm). Clustering of TF and bacterial pathogens at household and EA level was investigated using random effects logistic regression models with random intercepts for household and EAs. Likelihood ratio tests (LRTs) were used to compare models with and without the additional random effects terms.
Univariate associations with TF were determined using random effects logistic regression models with and without the exposure of interest. To assess confounding of the association between each pathogen and TF, unadjusted Mantel-Haenszel ORs for the effect of each pathogen on TF were compared to the ORs adjusted for each exposure. A 10% change in the OR was considered to indicate confounding, if the exposure was associated with both the pathogen of interest and TF. Modification of the effect of each pathogen on TF by other exposures was assessed in exploratory analyses using Mantel-Haenszel methods.
Following identification of univariate associations with TF and confounders of the effect of each pathogen on TF, a multivariate model was built adjusting for each pathogen associated with TF and including any confounding exposures. Independent risk factors for TF were also considered for inclusion in the final model on the basis of a LRT p-value<0.1. The strength of association with TF for each pathogen and exposure in the final model was estimated from a LRT comparing adjusted models with and without the pathogen of exposure.
Predictors of discharge (nasal and ocular) were identified using random effects logistic regression with discharge as the outcome, accounting for between household and/or between EA variation where appropriate and building a final multivariable model using the same approach as for TF.
Results
In the 16 EAs under study, 1569 children aged 0–5 years were randomly sampled for measurement of trachoma outcomes as part of the PRET CRT. Of these, laboratory results for both C. trachomatis PCR and conventional bacteriology were obtained for 1538 children (98.0%). For the 31 children with missing laboratory results, tabulations showed no evidence that children were not missing at random. Analysis was restricted to the results obtained for those 1538 children with complete data.
Prevalence of bacterial colonization
Bacteriology culture detected at least one non-chlamydial pathogen in the eyes of 475 (30.9%) children. S. aureus and S. pneumoniae were most commonly detected occuring in more than 14% of children (Table? 1). Colonization with H. influenzae and M. catarrhalis was less common. Sixteen children (1.0%) had evidence of C. trachomatis infection.
Table 1. Prevalence of ocular bacterial colonization, C. trachomatis infection and TF.
| N | Colonization, n | Prevalence (exact binomial 95% CI, percent scale) | Adjusted Prevalence* (95% CI, percent scale) | |
| S. pneumoniae | 1538 | 219 | 14.2 (12.5–16.1) | 12.5 (11.0–13.8) |
| H. influenzae | 1538 | 57 | 3.7 (2.8–4.8) | 2.6 (1.6–3.6) |
| S. aureus | 1538 | 233 | 15.2 (13.4–17.0) | 14.7 (13.9–15.6) |
| M. catarrhalis | 1538 | 19 | 1.2 (0.7–1.9) | 1.1 (0.8–1.5) |
| C. trachomatis | 1538 | 16 | 1.0 (0.6–1.7) | 1.0 (0.8–1.1) |
| TF | 1538 | 96 | 6.2 (5.1–7.6) | 6.1 (5.4–6.9) |
Adjusted for age (0–1, 2–3, 4–5 years), sex, district and any underlying variation between households and/or EAs as appropriate.
Dual colonization was detected in 53 (3.4%) children; most commonly with S. pneumoniae and S. aureus (37 children, 2.4%). Dual colonization with S. pneumonaie and H. influenza was found in 10 children (0.7%). Six children positive for C. trachomatis infection carried one non-chlamydial pathogen concurrently (0.4%); 2 children had C. trachomatis and H. influenzae, 2 children had C. trachomatis with S. aureus and 2 children had C. trachomatis and M. catarrhalis. No children were found to have C. trachomatis infection concurrent with S. pneumoniae.
In random effects logistic regression adjusting for each pathogen alone (null models), there was evidence that children carrying S. pneumoniae were clustered at the household level as demonstrated by evidence of between-household variation (p<0.001) but not at EA level, after accounting for clustering by household (p = 0.11). H. influenzae carriage also clustered at household level (p = 0.01) but not at EA level (p = 0.46). The reverse was found for M. catarrhalis carriage, which clustered at EA level (p = 0.01) but not household (p = 1.00). S. aureus carriage clustered at both household and EA levels (p<0.001). C. trachomatis infection cases were clustered at EA level (p<0.001).
Associations with TF
Ninety-six children (6.2%) were found to have clinical signs of TF; no children were diagnosed as having trachomatous inflammation – intense (TI). TF cases were clustered at both EA and household levels (p<0.001). After accounting for between-household and between-EA variation, age (p = 0.004), C. trachomatis infection (p = 0.04) and district (p = 0.08) were associated with TF in univariate analyses (Table? 2). Sex (p = 0.64), time since mass treatment was carried out in the EA (whether 12 or 36 months previously; p = 0.76) and flies on the eyes (p = 0.317) were not associated with TF.
Table 2. Associations between bacterial pathogens and TF in 0–5 year olds.
| Characteristic | N | TF, n (%) | Univariate OR (95% CI)* | p-value | Multivariate OR (95% CI)* | p-value | |
| All children | 1538 | 96 (6.2) | - | - | - | ||
| S. pneumoniae | No | 1319 | 78 (5.9) | 1 | 1 | ||
| Yes | 219 | 18 (8.2) | 1.69 (0.85–3.33) | 0.140 | 2.14 (1.03–4.44) | 0.044 | |
| H. influenzae | No | 1481 | 88 (5.9) | 1 | 1 | ||
| Yes | 57 | 8 (14.0) | 3.40 (1.20–9.66) | 0.027 | 4.72 (1.53–14.5) | 0.009 | |
| S. aureus | No | 1305 | 81 (6.2) | 1 | - | ||
| Yes | 233 | 15 (6.4) | 1.30 (0.63–2.67) | 0.480 | - | ||
| M. catarrhalis | No | 1519 | 96 (6.3) | - | - | ||
| Yes | 19 | 0 (0) | - | - | - | ||
| At least one non-chlamydial pathogen | No | 1063 | 60 (5.6%) | 1 | - | ||
| Yes | 475 | 36 (7.6%) | 1.93 (1.09–3.43) | 0.022 | - | ||
| Number of non-chlamydial pathogens | 0 | 1036 | 60 (5.6%) | 1 | 0.072 | - | |
| 1 | 422 | 31 (7.4%) | 1.96 (1.07–3.57) | - | |||
| 2 | 53 | 5 (9.4%) | 1.79 (0.51–6.31) | - | |||
| Age (years) | 0–1 | 464 | 17 (3.7) | 1 | 0.012 | 1 | 0.004 |
| 2–3 | 588 | 47 (8.0) | 2.72 (1.36–5.43) | 3.24 (1.55–6.75) | |||
| 4–5 | 486 | 32 (6.6) | 1.89 (0.93–3.87) | 2.46 (1.14–5.32) | |||
| Sex | Male | 820 | 54 (6.6) | 1 | - | ||
| Female | 718 | 42 (5.9) | 0.89 (0.53–1.47) | 0.637 | - | ||
| C. trachomatis | No | 1522 | 93 (6.1) | 1 | 1 | ||
| Yes | 16 | 3 (18.8) | 8.54 (1.21–60.4) | 0.041 | 10.4 (1.32–81.2) | 0.033 | |
| District | Lower Baddibu | 726 | 30 (4.1) | 1 | 1 | ||
| Central Baddibu | 812 | 66 (8.1) | 2.25 (0.95–5.34) | 0.075 | 2.32 (0.94–5.70) | 0.076 | |
| Time since mass treatment | 12 months | 737 | 44 (6.0) | 1 | - | ||
| 36 months | 801 | 52 (6.5) | 1.16 (0.45–2.99) | 0.757 | - | ||
| Flies on the eyes† | No | 227 | 16 (7.1) | 1 | - | ||
| Yes | 1309 | 80 (6.1) | 1.44 (0.71–2.90) | 0.317 | - | ||
Univariate and multivariate ORs are estimated from random effects logistic regression models accounting for between-household and between-EA variation.
2 missing values for flies on the eyes.
In the univariate analysis accounting for between-household and between-EA variation of TF but no other covariates, increased odds of TF were observed in the presence of S. pneumoniae (OR = 1.69, 95%CI 0.85–3.33, p = 0.14), H. influenzae (OR = 3.40, 95%CI 1.20–9.66, p = 0.027) and S. aureus (OR = 1.30, 95%CI 0.63–2.67, p = 0.48) but a significant effect was observed only for H. influenzae in this analysis (Table? 2). There were no signs of TF amongst any of the children with ocular M. catarrhalis carriage. Dual carriage with more than one non-chlamydial pathogen was not associated with TF (p = 0.072).
The presence of S. pneumoniae was associated with age (p<0.001), with fewer older children having the organism. A similar association was found between H. influenzae and age (p<0.001). After adjustment for age, the association between S. pneumoniae and TF was significant at the 5% level (OR = 2.08, 95%CI 1.01–4.30, p = 0.05). The effect of H. influenzae also appeared stronger after adjustment for age (OR = 4.45, 95%CI 1.44–13.7, p = 0.01). C. trachomatis infection was not associated with age (p = 0.54).
In building a final random effects regression model accounting for between-household and between-EA variation, H. influenzae and S. pneumoniae were added in turn, followed by age since this was identified as a confounder of the effect of both H. influenzae and S. pneumoniae on TF. C. trachomatis infection and district were also added to the model in turn as independent risk factors for TF.
Multivariable results suggest a two-fold increase in the odds of TF for children with ocular S. pneumoniae carriage and a four-fold increase for carriers of H. influenzae (Table? 2). C. trachomatis infection was significantly associated with TF, but estimates of the magnitude of effect were imprecise due to low prevalence of C. trachomatis infection and TF in the sample.
Predictors of nasal and ocular discharge
Overall, 839 (54.6%) children were observed to have nasal discharge on the day of screening. In the final regression model, after adjustment for underlying variation at household level, S. pneumoniae (p = 0.02), M. catarrhalis (p = 0.01) and TF (p = 0.05) were associated with increased odds of nasal discharge (Table? 3). Age was also associated with nasal discharge (p<0.001) with increased odds observed for 2–3 year olds versus 0–1 year olds and decreased odds for 4–5 year olds versus 0–1 year olds. In the univariate analysis, flies on the eyes were associated with nasal discharge (p<0.001) but we have not included this variable in the multivariate model as it is not clear whether nasal discharge is the casual effect for flies on the eyes.
Table 3. Associations with nasal discharge in 0–5 year olds.
| Characteristic | N | Nasal discharge, n (%) | Univariable OR (95% CI)* | p-value | Multivariable OR (95% CI)* | p-value | |
| All children | 1538 | 839 (54.6) | - | - | - | ||
| S. pneumoniae | No | 1319 | 700 (53.1) | 1 | 1 | ||
| Yes | 219 | 139 (63.5) | 1.59 (1.15–2.20) | 0.005 | 1.52 (1.08–2.13) | 0.015 | |
| H. influenzae | No | 1481 | 808 (54.6) | 1 | - | ||
| Yes | 57 | 31 (54.9) | 0.99 (0.55–1.78) | 0.965 | - | ||
| S. aureus | No | 1305 | 715 (54.8) | 1 | - | ||
| Yes | 233 | 124 (53.2) | 0.94 (0.69–1.28) | 0.698 | - | ||
| M. catarrhalis | No | 1519 | 824 (54.3) | 1 | 1 | ||
| Yes | 19 | 15 (79.0) | 3.58 (1.09–11.8) | 0.022 | 4.07 (1.22–13.6) | 0.013 | |
| TF | No | 1442 | 776 (53.8) | 1 | 1 | ||
| Yes | 96 | 63 (65.6) | 1.67 (1.03–2.72) | 0.034 | 1.63 (0.99–2.68) | 0.051 | |
| C. trachomatis | No | 1522 | 827 (54.3) | 1 | - | ||
| Yes | 16 | 12 (75.0) | 2.67 (0.75–9.49) | 0.114 | - | ||
| Age (years) | 0–1 | 464 | 260 (56.1) | 1 | <0.001 | 1 | <0.001 |
| 2–3 | 588 | 368 (62.6) | 1.36 (1.03–1.79) | 1.40 (1.06–1.85) | |||
| 4–5 | 486 | 211 (43.4) | 0.57 (0.43–0.75) | 0.59 (0.44–0.79) | |||
| Sex | Male | 820 | 455 (55.5) | 1 | - | ||
| Female | 718 | 384 (53.5) | 0.90 (0.72–1.21) | 0.342 | - | ||
| District | Lower Baddibu | 726 | 393 (54.1) | 1 | - | ||
| Central Baddibu | 812 | 446 (54.9) | 1.00 (0.79–1.28) | 0.972 | - | ||
| Time since mass treatment | 12 months | 737 | 395 (53.6) | 1 | - | ||
| 36 months | 801 | 444 (55.4) | 1.10 (0.86–1.41) | 0.433 | - | ||
| Flies on the eyes† | No | 227 | 65 (28.6) | 1 | - | ||
| Yes | 1309 | 634 (48.4) | 2.54 (1.78–3.60) | <0.001 | - | ||
Univariable and multivariable ORs are estimated from random effects logistic regression models accounting for between-household and between-EA variation, as appropriate.
2 missing values for flies on the eyes.
Ocular discharge was observed for 190 (12.4%) children. A final model adjusted for household and EA level clustering of cases. Results suggest increased odds of ocular discharge in children carrying H. influenzae (p = 0.06) and possibly in male children (p = 0.07) (Table? 4). Age was again associated with ocular discharge (p = 0.04) with the same pattern as for nasal discharge; increased odds in 2–3 year olds versus 0–1 year olds and decreased odds for 4–5 years versus 0–1 year olds.
Table 4. Associations with ocular discharge in 0–5 year olds.
| Characteristic | N | Ocular discharge, n (%) | Univariable OR (95% CI)* | p-value | Multivariable OR (95% CI)* | p-value | |
| All children | 1538 | 190 (12.4) | - | - | - | - | |
| S. pneumoniae | No | 1319 | 166 (12.6) | 1 | - | ||
| Yes | 219 | 24 (11.0) | 0.85 (0.52–1.39) | 0.502 | - | ||
| H. influenzae | No | 1481 | 177 (12.0) | 1 | 1 | ||
| Yes | 57 | 13 (22.8) | 2.24 (1.09–4.60) | 0.035 | 2.07 (1.00–4.31) | 0.059 | |
| S. aureus | No | 1305 | 163 (12.5) | 1 | - | ||
| Yes | 233 | 27 (11.6) | 0.97 (0.60–1.56) | 0.884 | - | ||
| M. catarrhalis | No | 1519 | 188 (12.4) | 1 | - | ||
| Yes | 19 | 2 (10.5) | 0.81 (0.17–4.00) | 0.795 | - | ||
| TF | No | 1442 | 172 (11.9) | 1 | - | ||
| Yes | 96 | 18 (18.8) | 1.49 (0.81–2.76) | 0.213 | - | ||
| C. trachomatis | No | 1522 | 187 (12.3) | 1 | - | ||
| Yes | 16 | 3 (18.8) | 1.86 (0.43–8.13) | 0.426 | - | ||
| Age (years) | 0–1 | 464 | 64 (13.8) | 1 | 0.030 | 1 | 0.038 |
| 2–3 | 588 | 82 (14.0) | 1.06 (0.72–1.56) | 1.11 (0.75–1.63) | |||
| 4–5 | 486 | 44 (9.1) | 0.63 (0.40–0.97) | 0.66 (0.42–1.02) | |||
| Sex | Male | 820 | 113 (13.8) | 1 | 1 | ||
| Female | 718 | 77 (10.7) | 0.74 (0.53–1.04) | 0.082 | 0.73 (0.52–1.03) | 0.069 | |
| District | Lower Baddibu | 726 | 85 (11.7) | 1 | - | ||
| Central Baddibu | 812 | 105 (12.9) | 1.18 (0.62–2.25) | 0.615 | - | ||
| Time since mass treatment | 12 months | 737 | 77 (10.5) | 1 | - | ||
| 36 months | 801 | 113 (14.1) | 1.40 (0.76–2.57) | 0.288 | - | ||
| Flies on the eyes† | No | 227 | 193 (85.0) | 1 | - | ||
| Yes | 1309 | 1155 (88.2) | 1.25 (0.80–1.96) | 0.338 | - | ||
Univariable and multivariable ORs are estimated from random effects logistic regression models accounting for between-household and between-EA variation, as appropriate.
2 missing values for flies on the eyes.
Discussion
The PRET trial documented a near disapperance of ocular C. trachomatis infection from a catchment area of greater than 65,000 people in the two years following the intitiation of MDA; biannual surveys carried out in the four study districts showed no evidence of ocular C. trachomatis infection 12 and 18 months post-MDA initiation and just 0.1% prevalence at 6 and 24 months [7]. Yet prevalence of TF over the same time period remained relatively high, reaching more than 10% in some EAs in the North Bank Region of the country. While one cannot rule-out episodes of C. trachomatis infection in the intervening months, it is difficult to see how C. trachomatis infection alone could sustain the clinical signs of disease during that time. Low-level exposure to C. trachomatis may not be detected by the Amplicor PCR method but it is unclear whether such low bacterial loads result in onward transmission of the microorganism.
In the 16 EAs included in this study, prevalence of ocular C. trachomatis infection 36 months post-MDA was 1% while prevalence of clinical signs of TF was 6%. While the association between active ocular C. trachomatis infection and TF was strong, it does not account for all the TF recorded. Clinical signs of TF were also associated with ocular S. pneumoniae and H. influenzae carriage. Both S. pneumoniae and H. influenzae are well known causes of bacterial conjunctivitis although not generally assocaited with follicular conjunctivitis [19]. It may be that localised inflammation caused by these microorganims recalls a follicular response in children who have previously been exposed to C. trachomatis. Alternatively, ocular carriage could predispose the eye to infection by C. trachomatis thereby inducing subsequent TF. In the present study, ocular carriage with S. pneumoniae was associated with nasal discharge while H. influenzae was associated with ocular discharge. Musca sorbens, which in some environments can act as the vector of trachoma, is more often found on the faces of children with ocular and nasal discharge than on children with no discharge [20], [21]; in our study flies on the eyes was associated with nasal discharge. If ocular colonization with these pathogens itself causes discharge, this may in turn increase the risk of C. trachomatis transmission.
One limitation of this study was that samples were kept frozen at −20°C for approximately two weeks before transport to the laboratory and subsequent storage at −70°C. Published data suggest these handling conditions are sufficient for cultivation of these respiratory pathogens [22], [23] however, we cannot discount the possibilty that storage conditions negatively impacted the viability of our samples resulting in an underestimate in ocular carriage prevalence. In addition, it is unclear whether the isolation of non-chlamydial, bacterial pathogens from the conjunctiva in a cross-sectional survey such as this is indicative of established ocular infection. A positive bacteriology culture may simply indicate transient carriage in the conjunctiva following introduction of bacteria by fingers or fomites. Indeed, nasopharyngeal (NP) carriage rates of S. pneumoniae in The Gambia are high with up to 90% of children under the age of five years being carriers [24], [25]. It is likely that children continually self-inoculate their eyes by touching their hands to their faces, possibly causing clinical signs of trachoma in children who have previously been exposed to C. trachomatis.
Our study has also shown that prevalence of ocular carriage of S. aureus is high, yet no association of this pathogen with TF was found and its carriage was not associated with either nasal or ocular discharge. Unlike the other pathogens detected, S. aureus is a part of the normal skin flora and imprecise sampling of the lower fornix could have introduced skin contamination into the swabs. However, the prevalence of ocular S. aureus carriage that we have detected (15%) is consistent with an earlier study carried out in Gambian communities where 11% of adults presenting for trichiasis surgery were found to carry the pathogen [15]. Another study detected S. aureus in the eyes of 30% of adults with trachomatous scarring and in 30% of healthy controls' however, the sample size of this study was small (13 cases and 7 controls [26]).
Previous studies on the role of non-chlamydial pathogens in trachoma have been conducted in The Gambia but with a focus on trachomatous scarring (TS) and trichiasis (TT) rather than on TF [15], [26]. Bacterial pathogens were more frequently isolated from eyes with TS than from control eyes however, this difference was not statistically significant [26]. In contrast, TT was significantly assocaited with bacterial pathogens in the eye, an association strengthened with increasing disease severity as measured by the number of lashes touching the eye [15], [26]. S. pneumoniae was the most common pathogen isolated from TT cases [26].
The role of non-chlamydial pathogens in TF has recently been studied in a trachoma endemic community in Tanzania, in this case prior to rather than post-MDA [16]. Prevalence of TF was higher than that reported here, with 13.7% of children under 10 years of age displaying signs of active disease. Prevalence of ocular C. trachomatis infection was also higher (5.3%) yet no association was seen between TF and a positive Amplicor PCR result. Ocular S. pneumoniae and H. influenzae carriage however, were both found to be associated with TF, consistent with our present findings.
The prevalence of ocular carriage of S. pneumoniae in the Tanzanian study was modestly lower than that which we report here (10.2% versus 14.2%). This may reflect the broader age distribution of children sampled in the Tanzanian study (all children under 10 years of age) as NP carriage rates are known to be higher in younger children. However, prevalence of NP carriage also appears to be lower in Tanzania than in The Gambia, although data are limited [27], [28]. The heptavalent pneumococal conjungate vaccine (PCV-7) was introduced into the Expanded Programme of Immunization (EPI) in The Gambia in August 2009; those children who were less than two years of age when recruited into our study were likely vaccinated. Available evidence however, suggests prevalence of NP carriage of S. pneumonaie in The Gambia is not affected by PCVs due to replacement with non-vaccine serotypes [25], [29]. Indeed we found younger children were more likely to carry S. pneumoniae than older children, consistent with data of NP carriage from this country indicating prevalence of carriage is assocaited with decreasing age [24].
H. influenzae carriage rates were markedly different between the two studies with H. influenzae type B (Hib) being isolated from 14% and non-Hib H. influenzae from 9% of children in the Tanzaian study. We found ocular H. influenzae colonization in just 3.7% of children sampled. Hib conjugate vaccine has been used in the Gambian EPI since 1997 and coverage rates are believed to be high [30]. Prevalence of NP Hib carriage in Western Gambia fell from 12% pre-vaccination to 0.25% five years following introduction of the vaccine into the EPI [31]. We therefore did not type for Hib in the present study. It is likely that high Hib vaccine coverage has contributed to the low levels of ocular H. influenzae carriage reported here; while Hib vaccination does not cross protect against other H. influenzae serotypes, there are only limited data to support the assertion that Hib vaccination results in serotype replacement by other capsulated strains in carriage [32]. Although we did not use molecular techniques to characterise the H. influenzae isolates, we speculate the majority of them would be unencapsulated (non-typeable) strains, which are unaffected by the Hib vaccine. Such strains are often associated with conjunctivitis [33] and recently were shown to account for most of the H. influenzae carried in the nasopharnyx of a cohort of Gambian infants [34]. Despite the lower prevalence of ocular H. influenzae carriage seen in The Gambia as compared to Tanzania, we also found an association between TF and this pathogen.
The Gambia is one of many countries incorporating MDA into its national trachoma control strategy. The ITI has distributed more than 250 million azithromycin treatments in 19 trachoma endemic countries and plans to be active in 42 countries by 2015. While MDA with azithromycin is associated with a significant decrease in pharyngeal carriage of S. pneumoniae, this effect is short-lived with carriage rates returning to baseline within two months following a single round of treatment [35], [36]. Repeated MDA at six or 12 month intervals also fails to affect prevalence of NP carriage of S. pneumoniae in the long-term [37]–[39]. The effect of MDA with azithromycin on carriage of H. influenzae is less well characterized, yet available data from The Gambia indicate pharyngeal carriage of the bacterium is unaffected by three doses (20 mg/kg) given over the course of two weeks [40]. It is therefore likely that as ocular C. trachomatis infection is controlled through mass azithromycin distribution, the contribution of these non-chlamydial pathogens to clinical signs of TF will become more apparent.
According to WHO policy, the prevalence of TF is currently the principal determinant for discontinuing MDA [41]. If non-chlamydial pathogens are inducing or exacerbating TF in the absence of C. trachomatis infection, communities may end up receiving unnecessary treatment. Furthermore, proposed criteria for trachoma elimination also relate to prevalence of clinical signs [42], [43] and as countries strive to reach their control targets, the information obtained from surveillance may be misleading. The role of these pathogens in the persistence of TF post-MDA therefore warrants further study; the key question is whether TF in these circumstances is likely to progress to conjunctival scarring and blindness.
Acknowledgments
We thank Pateh Makalo, Mass Laye, Sarjo Dibba, Muhamed Jallow, Robyn Damary-Homan, Jane Whitton, Anita Wadagni and Omar Camara for their work in the field. We would also like to thank the community leaders and villagers for their participation in the study.
Funding Statement
This study was supported by the Bill and Melinda Gates Foundation (http://www.gatesfoundation.org/), grant number 48027. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Faal H, Minassian D, Sowa S, Foster A (1989) National survey of blindness and low vision in The Gambia: results. Br? J? Ophthalmol 73: 82–87 Available:http://bjo.bmj.com/content/73/2/82.short. Accessed 11 March 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dolin P, Faal H, Johnson G (1998) Trachoma in the Gambia. Br? J? Ophthalmol 82: 930–933 Available:http://bjo.bmj.com/content/82/8/930.short. Accessed 11 March 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Faal H, Minassian DC, Dolin PJ, Mohamed a a, Ajewole J, et al. (2000) Evaluation of a national eye care programme: re-survey after 10 years. The British journal of ophthalmology 84: 948–951 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1723659&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Harding-Esch EM, Edwards T, Sillah A, Sarr I, Roberts CH, et al. (2009) Active trachoma and ocular Chlamydia trachomatis infection in two Gambian regions: on course for elimination by 2020? PLoS neglected tropical diseases 3: e573 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2791206&tool=pmcentrez&rendertype=abstract. Accessed 29 September 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Stare D, Harding-Esch E, Munoz B, Bailey R, Mabey D, et al. (2011) Design and baseline data of a randomized trial to evaluate coverage and frequency of mass treatment with azithromycin: the Partnership for Rapid Elimination of Trachoma (PRET) in Tanzania and The Gambia. Ophthalmic epidemiology 18: 20–29 Available:http://www.ncbi.nlm.nih.gov/pubmed/21275593. Accessed 31 August 2012. [DOI] [PubMed] [Google Scholar]
- 6. Harding-Esch EM, Edwards T, Mkocha H, Munoz B, Holland MJ, et al. (2010) Trachoma prevalence and associated risk factors in the gambia and Tanzania: baseline results of a cluster randomised controlled trial. PLoS neglected tropical diseases 4: e861 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2970530&tool=pmcentrez&rendertype=abstract. Accessed 5 September 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Harding-Esch EM, Sillah A, Edwards T, Burr SE, Hart JD, et al. (2013) Mass Treatment with Azithromycin for Trachoma: When Is One Round Enough? Results from the PRET Trial in The Gambia. PLoS neglected tropical diseases 7: e2115 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3681669&tool=pmcentrez&rendertype=abstract. Accessed 24 June 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Burton MJ, Holland MJ, Makalo P, Aryee EAN, Sillah A, et al. (2010) Profound and sustained reduction in Chlamydia trachomatis in The Gambia: a five-year longitudinal study of trachoma endemic communities. PLoS neglected tropical diseases 4: e835 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2950148&tool=pmcentrez&rendertype=abstract. Accessed 3 October 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Solomon AW, Holland MJ, Alexander NDE, Massae P a, Aguirre A, et al. (2004) Mass treatment with single-dose azithromycin for trachoma. The New England journal of medicine 351: 1962–1971 Available:http://www.ncbi.nlm.nih.gov/pubmed/15525721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Solomon AW, Harding-Esch E, Alexander NDE, Aguirre A, Holland MJ, et al. (2008) Two doses of azithromycin to eliminate trachoma in a Tanzanian community. The New England journal of medicine 358: 1870–1871 Available:http://www.ncbi.nlm.nih.gov/pubmed/18434662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cumberland P, Edwards T, Hailu G, Harding-Esch E, Andreasen A, et al. (2008) The impact of community level treatment and preventative interventions on trachoma prevalence in rural Ethiopia. International journal of epidemiology 37: 549–558 Available:http://www.ncbi.nlm.nih.gov/pubmed/18356196. Accessed 16 November 2012. [DOI] [PubMed] [Google Scholar]
- 12. Biebesheimer JB, House J, Hong KC, Lakew T, Alemayehu W, et al. (2009) Complete local elimination of infectious trachoma from severely affected communities after six biannual mass azithromycin distributions. Ophthalmology 116: 2047–2050 Available:http://www.ncbi.nlm.nih.gov/pubmed/19744717. Accessed 16 November 2012. [DOI] [PubMed] [Google Scholar]
- 13. Baral K, Osaki S, Shreshta B, Panta CR, Boulter A, et al. (1999) Reliability of clinical diagnosis in identifying infectious trachoma in a low-prevalence area of Nepal. Bulletin of the World Health Organization 77: 461–466 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2557684&tool=pmcentrez&rendertype=abstract. Accessed 16 November 2012. [PMC free article] [PubMed] [Google Scholar]
- 14. Thein J, Zhao P, Liu H, Xu J, Jha H, et al. (2002) Does clinical diagnosis indicate ocular chlamydial infection in areas with a low prevalence of trachoma? Ophthalmic epidemiology 9: 263–269 Available:http://www.ncbi.nlm.nih.gov/pubmed/12187424. Accessed 16 November 2012. [DOI] [PubMed] [Google Scholar]
- 15. Burton MJ, Kinteh F, Jallow O, Sillah a, Bah M, et al. (2005) A randomised controlled trial of azithromycin following surgery for trachomatous trichiasis in the Gambia. The British journal of ophthalmology 89: 1282–1288 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1772881&tool=pmcentrez&rendertype=abstract. Accessed 8 December 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Burton MJ, Hu VH, Massae P, Burr SE, Chevallier C, et al. (2011) What is causing active trachoma? The role of nonchlamydial bacterial pathogens in a low prevalence setting. Investigative ophthalmology & visual science 52: 6012–6017 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3176035&tool=pmcentrez&rendertype=abstract. Accessed 13 November 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Thylefors B, Dawson CR, Jones BR, West SK, Taylor HR (1987) A simple system for the assessment of trachoma and its complications. Bulletin of the World Health Organization 65: 477–483 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2491032&tool=pmcentrez&rendertype=abstract. Accessed 13 November 2012. [PMC free article] [PubMed] [Google Scholar]
- 18. GIBSON LF, KHOURY JT (1986) Storage and survival of bacteria by ultra-freeze. Letters in Applied Microbiology 3: 127–129 Available:http://doi.wiley.com/10.1111/j.1472-765X.1986.tb01565.x. Accessed 16 November 2012. [Google Scholar]
- 19.Krachmer JH, Mannis MJ, Holland EJ (1997) Cornea: cornea and external disease: clinical diagnosis and management. Volume 2. St. Louis, Missouri: Mosby-Year Book, Inc. p. [Google Scholar]
- 20. Emerson PM, Bailey RL, Mahdi OS, Walraven GE, Lindsay SW (2000) Transmission ecology of the fly Musca sorbens, a putative vector of trachoma. Transactions of the Royal Society of Tropical Medicine and Hygiene 94: 28–32 Available:http://www.ncbi.nlm.nih.gov/pubmed/10748893. Accessed 2 October 2012. [DOI] [PubMed] [Google Scholar]
- 21. Miller K, Pakpour N, Yi E, Melese M, Alemayehu W, et al. (2004) Pesky trachoma suspect finally caught. The British journal of ophthalmology 88: 750–751 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1772198&tool=pmcentrez&rendertype=abstract. Accessed 2 October 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. O'Brien KL, Bronsdon MA, Dagan R, Yagupsky P, Janco J, et al. (2001) Evaluation of a medium (STGG) for transport and optimal recovery of Streptococcus pneumoniae from nasopharyngeal secretions collected during field studies. Journal of clinical microbiology 39: 1021–1024 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=87867&tool=pmcentrez&rendertype=abstract. Accessed 2 October 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kaijalainen T, Ruokokoski E, Ukkonen P, Herva E (2004) Survival of Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis frozen in skim milk- tryptone-glucose-glycerol medium. Journal of clinical microbiology 42: 412–414 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=321668&tool=pmcentrez&rendertype=abstract. Accessed 2 October 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hill PC, Akisanya A, Sankareh K, Cheung YB, Saaka M, et al. (2006) Nasopharyngeal carriage of Streptococcus pneumoniae in Gambian villagers. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 43: 673–679 Available:http://www.ncbi.nlm.nih.gov/pubmed/16912937. Accessed 16 November 2012. [DOI] [PubMed] [Google Scholar]
- 25. Cheung Y-B, Zaman SM a, Nsekpong ED, Van Beneden C a, Adegbola R a, et al. (2009) Nasopharyngeal carriage of Streptococcus pneumoniae in Gambian children who participated in a 9-valent pneumococcal conjugate vaccine trial and in their younger siblings. The Pediatric infectious disease journal 28: 990–995 Available:http://www.ncbi.nlm.nih.gov/pubmed/19536041. Accessed 5 July 2011. [DOI] [PubMed] [Google Scholar]
- 26. Burton MJ, Adegbola R a, Kinteh F, Ikumapayi UN, Foster A, et al. (2007) Bacterial infection and trachoma in the gambia: a case control study. Investigative ophthalmology & visual science 48: 4440–4444 Available:http://www.ncbi.nlm.nih.gov/pubmed/17898263. Accessed 24 July 2012. [DOI] [PubMed] [Google Scholar]
- 27. Leung MHY, Oriyo NM, Gillespie SH, Charalambous BM (2011) The adaptive potential during nasopharyngeal colonisation of Streptococcus pneumoniae. Infection, genetics and evolution: journal of molecular epidemiology and evolutionary genetics in infectious diseases 11: 1989–1995 Available:http://www.ncbi.nlm.nih.gov/pubmed/21925618. Accessed 16 November 2012. [DOI] [PubMed] [Google Scholar]
- 28. Moyo SJ, Steinbakk M, Aboud S, Mkopi N, Kasubi M, et al. (2012) Penicillin resistance and serotype distribution of Streptococcus pneumoniae in nasopharyngeal carrier children under 5 years of age in Dar es Salaam, Tanzania. Journal of medical microbiology 61: 952–959 Available:http://www.ncbi.nlm.nih.gov/pubmed/22442292. Accessed 16 November 2012. [DOI] [PubMed] [Google Scholar]
- 29. Egere U, Townend J, Roca A, Akinsanya A, Bojang A, et al. (2012) Indirect effect of 7-valent pneumococcal conjugate vaccine on pneumococcal carriage in newborns in rural Gambia: a randomised controlled trial. PloS one 7: e49143 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3504064&tool=pmcentrez&rendertype=abstract. Accessed 15 May 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. World Health Organization (2012) WHO UNICEF coverage estimates WHO World Health Organization: Immunization, Vaccines And Biologicals. Vaccine preventable diseases Vaccines monitoring system 2012 Global Summary Reference Time Series: GMB Available:http://apps.who.int/immunization_monitoring/en/globalsummary/timeseries/TSWUcoverageByCountry.cfm?country=GMB. Accessed 29 January 2013. [Google Scholar]
- 31. Adegbola RA, Secka O, Lahai G, Lloyd-Evans N, Njie A, et al. (2005) Elimination of Haemophilus influenzae type b (Hib) disease from The Gambia after the introduction of routine immunisation with a Hib conjugate vaccine: a prospective study. Lancet 366: 144–150 Available:http://www.ncbi.nlm.nih.gov/pubmed/16005337. Accessed 2 October 2012. [DOI] [PubMed] [Google Scholar]
- 32. Dabernat H, Plisson-Sauné M-A, Delmas C, Séguy M, Faucon G, et al. (2003) Haemophilus influenzae carriage in children attending French day care centers: a molecular epidemiological study. Journal of clinical microbiology 41: 1664–1672 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=153885&tool=pmcentrez&rendertype=abstract. Accessed 16 November 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Murphy TF, Faden H, Bakaletz LO, Kyd JM, Forsgren A, et al. (2009) Nontypeable Haemophilus influenzae as a pathogen in children. The Pediatric infectious disease journal 28: 43–48 Available:http://www.ncbi.nlm.nih.gov/pubmed/19057458. Accessed 2 October 2012. [DOI] [PubMed] [Google Scholar]
- 34. Kwambana BA, Barer MR, Bottomley C, Adegbola RA, Antonio M (2011) Early acquisition and high nasopharyngeal co-colonisation by Streptococcus pneumoniae and three respiratory pathogens amongst Gambian new-borns and infants. BMC infectious diseases 11: 175 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3129300&tool=pmcentrez&rendertype=abstract. Accessed 17 July 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Leach AJ, Shelby-James TM, Mayo M, Gratten M, Laming AC, et al. (1997) A prospective study of the impact of community-based azithromycin treatment of trachoma on carriage and resistance of Streptococcus pneumoniae. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 24: 356–362 Available:http://www.ncbi.nlm.nih.gov/pubmed/9114185. Accessed 23 August 2012. [DOI] [PubMed] [Google Scholar]
- 36. Batt SL, Charalambous BM, Solomon AW, Knirsch C, Massae PA, et al. (2003) Impact of azithromycin administration for trachoma control on the carriage of antibiotic-resistant Streptococcus pneumoniae. Antimicrobial agents and chemotherapy 47: 2765–2769 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=182606&tool=pmcentrez&rendertype=abstract. Accessed 28 March 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Fry a M, Jha HC, Lietman TM, Chaudhary JSP, Bhatta RC, et al. (2002) Adverse and beneficial secondary effects of mass treatment with azithromycin to eliminate blindness due to trachoma in Nepal. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 35: 395–402 Available:http://www.ncbi.nlm.nih.gov/pubmed/12145722. [DOI] [PubMed] [Google Scholar]
- 38. Gaynor BD, Chidambaram JD, Cevallos V, Miao Y, Miller K, et al. (2005) Topical ocular antibiotics induce bacterial resistance at extraocular sites. The British journal of ophthalmology 89: 1097–1099 Available:http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1772818&tool=pmcentrez&rendertype=abstract. Accessed 31 January 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Haug S, Lakew T, Habtemariam G, Alemayehu W, Cevallos V, et al. (2010) The decline of pneumococcal resistance after cessation of mass antibiotic distributions for trachoma. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 51: 571–574 Available:http://www.ncbi.nlm.nih.gov/pubmed/20649409. Accessed 23 August 2012. [DOI] [PubMed] [Google Scholar]
- 40. Adegbola RA, Mulholland EK, Bailey R, Secka O, Sadiq T, et al. (1995) Effect of azithromycin on pharyngeal microflora. The Pediatric infectious disease journal 14: 335–337 Available:http://www.ncbi.nlm.nih.gov/pubmed/7603826. Accessed 23 August 2012. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization (2003) World Health Organization Report of the 2nd Global Scientific Meeting on Trachoma. Available:http://www.who.int/blindness/2nd GLOBAL SCIENTIFIC MEETING.pdf.
- 42.Organization WH (2011) Report of the fifteenth meeting of the WHO alliance for the elimination of blinding trachoma by 2020. Available:http://www.who.int/blindness/publications/GET15REPORT4.pdf. Accessed 1 February 2013.
- 43.World Health Organization (2012) Report of the sixteenth meeting of the WHO alliance for the Elimination of Blinding Trachoma by 2020 pp. 14–16. Available:http://www.who.int/blindness/publications/GET16Report.pdf.