Abstract
People detained in prisons and other closed settings are at elevated risk of infection with hepatitis C virus (HCV). We undertook a systematic review and meta-analysis with the aim of determining the rate of incident HCV infection and the prevalence of anti-HCV among detainees of closed settings. We systematically searched databases of peer-reviewed literature and widely distributed a call for unpublished data. We calculated summary estimates of incidence and prevalence among general population detainees and detainees with a history of injecting drug use (IDU), and explored heterogeneity through stratification and meta-regression. The summary prevalence estimates were used to estimate the number of anti-HCV positive prisoners globally. HCV incidence among general detainees was 1·4 per 100 person-years (py; 95% CI: 0·1, 2·7; k=4), and 16·4 per 100py (95% CI: 0·8, 32·1; k=3) among detainees with a history of IDU. The summary prevalence estimate of anti-HCV in general detainees was 26% (95% CI: 23%, 29%; k=93), and in detainees with a history of IDU, 64% (95% CI: 58%, 70%; k=51). The regions of highest prevalence were Central Asia (38%; 95% CI 32%, 43%; k=1) and Australasia (35%; 95% CI: 28%, 43%; k=9). We estimate that 2·2 million (range: 1·4 million – 2·9 million) detainees globally are anti-HCV positive, with the largest populations in North America (668,500; range: 553,500–784,000) and East and Southeast Asia (638,000; range: 332,000–970,000).
Conclusion
HCV is a significant concern in detained populations, with one in four detainees anti-HCV positive. Epidemiological data on the extent of HCV infection in detained populations is lacking in many countries. Greater attention towards prevention, diagnosis and treatment of HCV infection among detained populations is urgently required.
Keywords: epidemiology, people who inject drugs, prisoners, injecting drug use, viral hepatitis
An estimated 2–3% of people are infected with the hepatitis C virus (HCV) globally (1, 2). The primary routes of transmission are injecting drug use (IDU) and, in developing countries, medical procedures using non-sterile syringes and needles (3). Perhaps two-thirds of the approximately 16 million people who inject drugs are HCV antibody (anti-HCV) positive (4, 5).
Prisons and other closed settings (i.e. prisons, jails, juvenile detention facilities, pre-trial detention centres and extra-judicial detention centres for people who use drugs (6); psychiatric institutions and immigration detention are not included in this definition for our purposes) are of particular importance in understanding the HCV epidemic due to the high prevalence of risk behaviours in the detainee population. A history of IDU is common among detainees (7) and injecting may continue while detained (8–10), with attendant disease transmission risks. Tattooing in closed settings may also be a risk factor for HCV transmission (11, 12). Finally, there is increasing evidence of a significant risk of HCV transmission among HIV-infected men who have sex with men (13); given the often high background prevalence of both infections and the lack of condom access in closed settings, this is potentially a serious concern.
Despite the evidence of risk, there have been limited efforts to examine the global extent of this problem. A clearer understanding of the epidemiology of HCV in closed settings is essential for determining the scale of the problem, providing a basis for public advocacy efforts and the development of prevention and treatment interventions. This is particularly so in light of recent advances in HCV therapies and the promise of all-oral, interferon-free treatment in the near future (14, 15). We undertook a systematic review and meta-analysis with the aim of determining the rate of incident HCV infection and the prevalence of anti-HCV among detainees of closed settings.
Methods
This study is reported in line with the PRISMA checklist (16). Throughout this paper, we use the term ‘detainees’ to refer to the population of people detained in closed settings. This term was selected as it is inclusive of people who are incarcerated in prisons and jails, as well as those held in less common and less well-known types of closed settings.
We used multiple search strategies to identify relevant literature. Four databases of peer-reviewed literature (Medline, Embase, Criminal Justice Abstracts and the National Criminal Justice Reference Service) were searched in July 2012. Search strings were developed in consultation with a librarian at the National Drug and Alcohol Research Centre, University of New South Wales. Search strings for Medline and Embase were adapted from Nelson et al. (5) (see supplementary materials for additional details). Additionally, reference lists of prior reviews on this topic (17–19) were examined and the literature database of the HCV Synthesis Project (20) was searched for citations potentially relevant to closed settings.
Grey literature, defined as publications and communications that are not formally published by commercial publishers or peer-reviewed journals, was identified through searches of websites of relevant organizations (e.g. European Monitoring Centre for Drugs and Drug Addiction), regional literature databases (e.g. Latin American and Caribbean Health Sciences), online conference archives (e.g. International AIDS Society conferences) and country-specific government departments (21).
Finally, an email was sent to relevant contacts of all authors, requesting data that may not have been identified in our search. The email was redistributed by the initial recipients as they saw appropriate. Data collection ceased in September 2012.
Study selection
Initial literature search results were catalogued using Endnote X5. Titles and abstracts were screened by SL, HK and a research intern to produce a shortlist of potentially relevant sources. Sources that were clearly outside the remit of the review (e.g. editorial in nature; did not contain primary data) were excluded. Full-text versions of shortlisted sources were retrieved and read in full to determine eligibility for inclusion in the review. For sources in languages other than English, determination of eligibility was based on information available in published English translations of abstracts.
Sources were eligible for inclusion if they: reported data from a closed setting (defined as a prison, jail, juvenile detention facility, pre-trial detention centre or extra-judicial detention centre for people who use drugs (6, 22)); conducted serological or saliva testing for anti-HCV; and presented an estimate of anti-HCV prevalence or HCV incidence (defined as HCV antibody seroconversion) among either general population detainees or detainees with a history of IDU. General population samples were those that included any detainee of a closed setting without selection by history of drug use or offence type. Incidence sources were restricted to those in which seroconversion was known to have occurred while detained; that is, the source sample included only persons who were continuously detained from baseline to follow-up, and measures were taken to exclude the possibility of seroconversion prior to incarceration. There were no restrictions on year or language of publication, or the age of the sampled population.
Sources were ineligible if they: were based on secondary data, self-reported HCV status or notifications of HCV infections (e.g. to infectious diseases databases); reported the results of HCV RNA testing without results of anti-HCV testing; or reported HCV incidence in case studies or cohorts of people who were not continuously detained throughout study follow-up. Sources with sample sizes of less than 40 or with no information regarding sample size were also ineligible (5). Several repeated surveys (i.e. re-sampling of the same closed settings using the same sampling strategy over time) were identified during the literature search. In these cases, only the most recent data were included in meta-analyses. The list of included sources was circulated to the authors in September 2012 for final approval.
Data extraction
Data from all sources were extracted by SL and checked for accuracy by HK, with discrepancies resolved through discussion and referral to LD as necessary. For each source, sample characteristics were extracted, including ‘types’ of detainees sampled (e.g. general population, detainees with a history of IDU), age (adult or juvenile sample, median and/or mean age) and sex.
Data were extracted for all detainee ‘types’ within each sample; for example, a source presenting data on a general population sample with a sub-sample of detainees with a history of IDU would have data extracted for both the general population sample and the sub-sample. For mixed-sex samples, data were extracted for the total sample and also disaggregated by sex, if possible. If disaggregation by detainee type or sex resulted in a sample size of less than 40, that sub-sample was excluded.
For sources reporting incidence data, the sample size, number of incident HCV cases, person-years of observation and incidence rate were extracted. For prevalence sources, the sample size, number of anti-HCV positive participants and prevalence were extracted. Some sources did not report all incidence or prevalence variables; in these cases, missing variables were calculated from other reported values (i.e. numerator calculated from reported denominator and prevalence).Study design and sampling variables (geographical region; type of closed setting; prospectively or retrospectively defined cohort; random or convenience sampling; restriction of recruitment to serving inmates or new entrants; year/s of data collection; percentage of sample male and percentage injecting) were extracted in order to explore heterogeneity in reported HCV incidence and prevalence. Geographical regions were defined consistent with other recent global epidemiological reviews (4, 5).
Data analysis
Data analyses were conducted in Stata version 12 (StataCorp LP, Texas USA) using the metan (23) and metareg (24) commands. Given the expected heterogeneity between studies, all meta-analyses were performed using random effects models, which account for inter-study variation. Meta-analyses of HCV incidence were undertaken for sources reporting on general population detainees and detainees with a history of injecting drug use. Heterogeneity was assessed using the I2 statistic, which describes the percentage of variation between studies that is due to heterogeneity rather than chance (25). Interpretation of I2 was as in Higgins et al. (25). The small number of sources of incidence data prevented further stratification or meta-regression.
Meta-analyses of anti-HCV prevalence were conducted for general population detainees and detainees with a history of IDU, stratified by geographical region. Heterogeneity was assessed using the I2 statistic, as above, and also explored through meta-regression. Variables used in meta-regressions were cohort ascertainment (prospective vs. retrospective); sampling (random vs. convenience); detainee status at the time of recruitment (current detainees or current detainees and new entrants vs. new entrants only); type of HCV antibody test undertaken (blood/sera vs. saliva); mean or median age of the sample; percentage of the sample that was male; percentage of the sample with a history of IDU; and year of completion of data collection. For sources where this latter variable was not reported, it was assumed that data collection ceased two years prior to year of publication (26). Sex-specific summary prevalence estimates were calculated using sources that reported on male- or female-only samples. We had planned to determine summary prevalence estimates for detainees of extra-judicial detention centres for people who use drugs; however, there were very few relevant data sources. Results for these sources are instead presented descriptively.
A meta-analysis was undertaken to determine the summary anti-HCV prevalence estimate in juvenile detainees, with heterogeneity examined via meta-regression using the same independent variables as for adult samples. There were few data sources reporting on juvenile detainees with a history of IDU; results from these sources are presented descriptively.
To estimate the number of anti-HCV positive detainees globally, we obtained data on regional prisoner populations from the World Prison Brief of the International Centre for Prison Studies (http://www.prisonstudies.org). The World Prison Brief does not include detainees of extra-judicial detention centres for people who use drugs; thus this estimate relates only to the prisoner population. We applied our regional prevalence estimates for general population detainees (who, by definition, are not detainees of extra-judicial detention centres) to the number of prisoners in each region. For regions without prevalence data, the global general population prevalence estimate was applied to the number of prisoners in the region.
Results
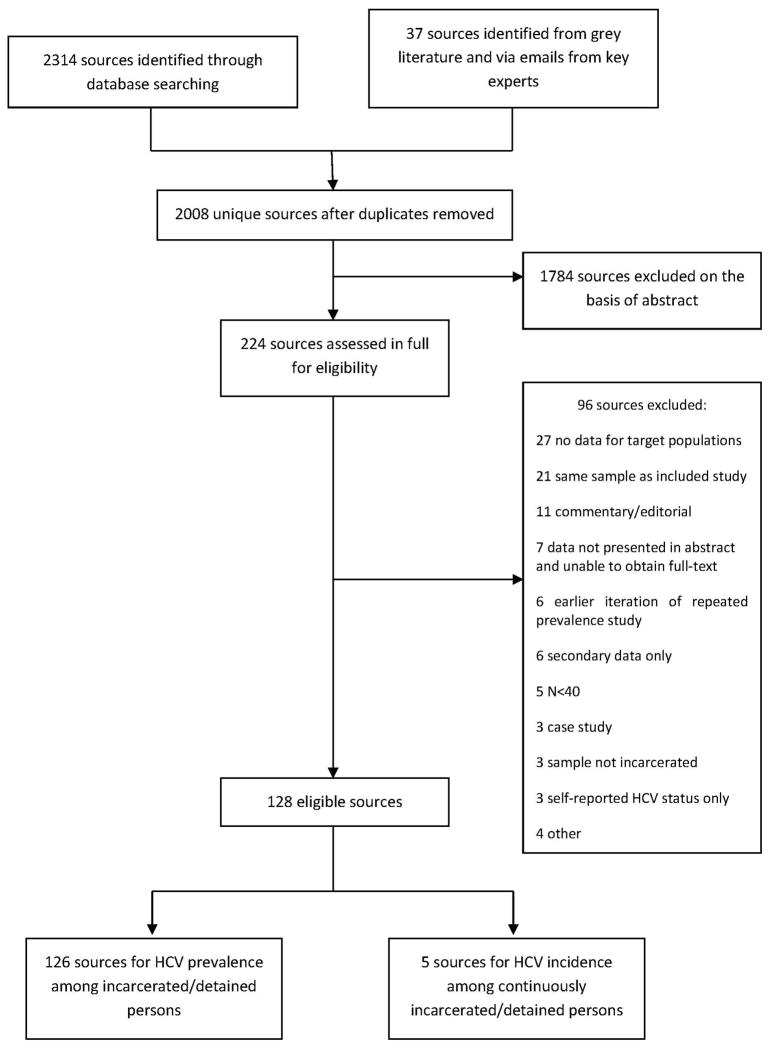
Searches of the peer-reviewed literature returned 2,314 data sources potentially relevant to the review. A further 37 data sources were identified from the grey literature or via emails from key experts. Following removal of duplicates, there were 2,008 data sources; of these, 1,784 were excluded on the basis of the abstract, leaving 224 sources which were assessed in full. Ninety-three sources were excluded, for reasons shown in Figure 1, leaving 128 eligible sources: five reported on HCV incidence in continuously detained persons, and 126 reported on anti-HCV prevalence among detainees of prisons and other closed settings (i.e. three sources reported on both incidence and prevalence) (Figure 1). Sources reported data for 39 countries (see supplementary materials); 21 sources were in languages other than English. Fifteen of the included sources were obtained from the grey literature; they included reports of government agencies, conference abstracts, academic reports and personal communications. Half the sources were published from 2004 onwards (see supplementary materials). Details of studies included in each meta-analysis described below are available in the supplementary materials.
Figure 1.
Selection of studies for inclusion in systematic review of hepatitis C virus prevalence and incidence in prisons and other closed settings
HCV incidence
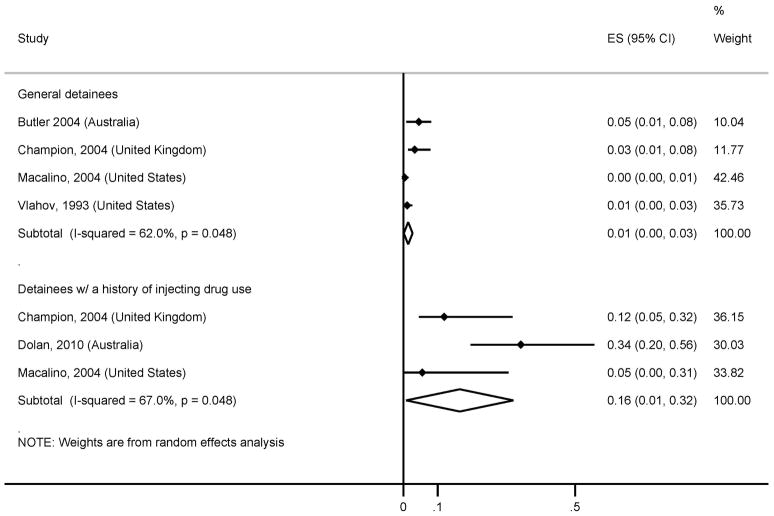
Four sources provided data on HCV incidence in general detainee samples, and three provided data from samples of inmates who inject drugs. Incidence among general detainees ranged from 0·04 per 100 person-years (py) to 4·5 per 100py. The summary incidence estimate was 1·4 per 100py (95% CI: 0·1, 2·7), with moderate heterogeneity (I2=62%, 95% CI: 0%, 87%) (Figure 2). Incidence among detainees with a history of IDU ranged from 5·5 per 100py to 34·2 per 100py. The summary incidence estimate was 16·4 per 100py (95% CI: 0·8, 32·1), with moderate heterogeneity (I2=67%, 95% CI: 0%, 90%) (Figure 2).
Figure 2. Hepatitis C virus antibody incidence in general population detainees and detainees with a history of injecting drug use.
Notes: ES; effect size
HCV antibody prevalence
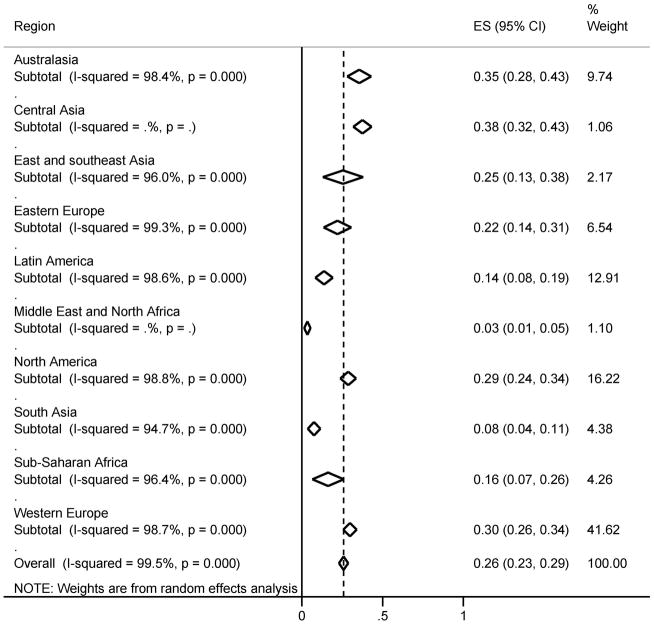
There were 93 sources of data for anti-HCV prevalence among general detainee samples. The summary anti-HCV prevalence estimate among general population detainees was 26% (95% CI: 23%, 29%), with high heterogeneity (I2=100%, 95% CI: 100%, 100%) (Figure 3). A sub-analysis by geographical region revealed wide variations in prevalence. The lowest estimated regional prevalence was 3% (95% CI: 2%, 5%) in the Middle East and North Africa; however, this was based on only one source (27). The highest estimated regional prevalence was 38% (95% CI: 32%, 43%) in Central Asia; again, this was based on only one source (personal communication, S. Karymbaeva, September 15 2012). The most important source of heterogeneity was the proportion of the sample with a history of injecting drug use (meta-regression coefficient=0·005, p<·0001, adjusted R2=49·23%) (Table 1); year of data collection was also a significant source of heterogeneity, with more recent sources having lower anti-HCV prevalence (meta-regression coefficient=&0·009, p=0·001, adjusted R2=12·57%). Prevalence was also lower in sources with data derived from random samples compared to convenience samples (18% vs 28%, meta-regression coefficient 0·096, p=0·042, adjusted R2=3·92%).
Figure 3. HCV antibody prevalence estimates for adult general population detainees, by region and in total.
Notes: Based on 93 sources. No sources were identified for the Pacific Islands or the Caribbean. Details of included sources available in supplementary materials. ES; effect size
Table 1.
Meta-regression for HCV antibody prevalence in adult general population detainees and adult detainees with a history of injecting drug use
| General population detainees | Detainees with a history of IDU | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| N sources | Anti-HCV prevalence % (95% CI) | Meta-regression coefficient | Adj. R2 | p | N sources | Anti-HCV prevalence % (95% CI) | Meta-regression coefficient | Adj. R2 | p | |
|
| ||||||||||
| Retrospective cohort | 11 | 31 (22, 40) | 3 | 67 (43, 91) | ||||||
| Prospective cohort | 79 | 25 (22, 28) | −0·055 | 0·31% | 0·267 | 46 | 65 (59, 72) | −0·016 | −2·16% | 0·900 |
|
| ||||||||||
| Random sample | 11 | 18 (10, 26) | 4 | 67 (44, 90) | ||||||
| Convenience sample | 70 | 28 (24, 31) | 0·096 | 3·92% | 0·042 | 43 | 67 (61, 73) | −0·003 | −2·25% | 0·977 |
|
| ||||||||||
| Blood/sera | 69 | 24 (21, 27) | 37 | 65 (58, 72) | ||||||
| Saliva | 8 | 20 (14, 26) | 0·035 | −0·80% | 0·505 | 5 | 58 (38, 78) | 0·074 | −1·05% | 0·457 |
|
| ||||||||||
| Current only or mixed current/entrant | 35 | 24 (19, 29) | 14 | 63 (50, 76) | ||||||
| New entrants only | 23 | 30 (25, 34) | 0·047 | 1·03% | 0·206 | 16 | 76 (69, 82) | 0·126 | 8·12% | 0·073 |
|
| ||||||||||
| Mean/median age | 46 | - | 0·003 | −1·97% | 0·707 | 8 | - | 0·00003 | −17·01% | 0·999 |
|
| ||||||||||
| Percentage male | 79 | - | −0·0008 | 1·61% | 0·139 | 26 | - | 0·001 | −1·04% | 0·413 |
|
| ||||||||||
| Percentage with history of IDU | 50 | - | 0·005 | 49·23% | <·0001 | - | - | - | - | - |
|
| ||||||||||
| Year of data collection completion* | ||||||||||
| Pre-1995 | 16 | 38 (32, 45) | 7 | 77 (65, 88) | ||||||
| 1995–1999 | 23 | 25 (19, 31) | 13 | 68 (54, 82) | ||||||
| 2000–2004 | 21 | 27 (22, 32) | 15 | 65 (55, 75) | ||||||
| 2005–2012 | 33 | 20 (17, 23) | −0·009 | 12·57% | <·0001 | 16 | 55 (44, 66) | −0·139 | 12·67% | 0·007 |
N studies varies due to variable reporting in data sources. HCV, hepatitis C virus. IDU, injecting drug use.
Meta-regressions conducted using year of data collection completion as a continuous variable. Year categories based on five-year increments except for 2005–2012. Year category prevalence estimates and confidence intervals determined via stratified meta-analysis.
Among general detainee data sources, 62 contributed data for male-only samples, with a summary prevalence estimate of 24% (95% CI: 21%, 27%; I2=99%,95% CI: 99%, 99%). There were 37 female-only samples, and estimated summary prevalence was 32% (95% CI: 26%, 38%; I2=98%, 95% CI: 98%, 99%).
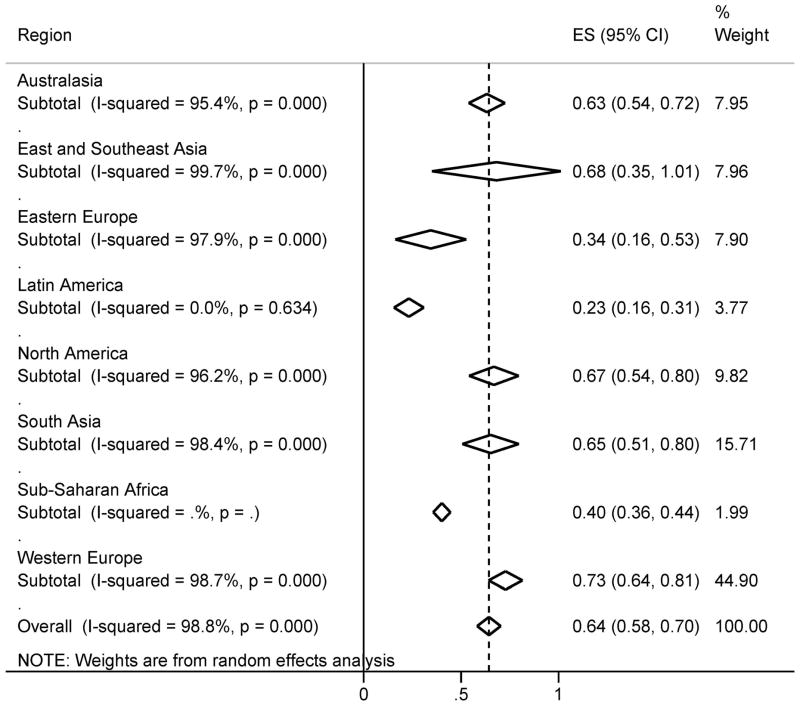
Fifty-one sources contributed data on anti-HCV prevalence among detainees with a history of IDU. History of IDU was determined through self-report in 49 sources, and physician examination in two sources. The estimated summary anti-HCV prevalence was 64% (95% CI: 58%, 70%), with high heterogeneity I2=99%, 95% CI: 99%, 99%) (Figure 4). Regional prevalence estimates ranged from 23% (95% CI: 16%, 31%) in Latin America to 73% (95% CI: 64%, 81%) in Western Europe. Prevalence was lower in more recent sources (meta-regression coefficient=−0·139, p=0·007, R2=12·67%) (Table 1). The summary prevalence estimate in men with history of IDU (26 sources) was 67% (95% CI: 58%, 75%; I2=99%,95% CI: 99%, 99%); among women with a history of IDU (seven sources), it was 64% (95% CI: 52%, 77%; I2=94%, 95% CI: 90%, 96%).
Figure 4. Pooled HCV antibody prevalence estimates for adult detainees with a history of injecting drug use, by region and in total.
Notes: Based on 51 sources. No sources were identified for countries of Central Asia, the Middle East and North Africa, the Pacific Islands or the Caribbean. Details of included sources available in supplementary materials. ES; effect size
Only two eligible data sources reported anti-HCV prevalence in extra-judicial detention centres for people who use drugs. In Chu et al. (28), anti-HCV prevalence among 753 male detainees of a Taiwanese centre was 31% (95% CI: 27%, 34%); among detainees with a history of IDU (n=192), it was 90% (95% CI: 84%, 94%). In an Iranian centre for male injecting drug users, anti-HCV prevalence was 80% (363/454; 95% CI: 76%, 84%)(29).
Among juvenile detainee samples (n=18), estimated summary prevalence was 4% (95% CI: 3%, 6%) with high heterogeneity (I2=92%, 95% CI: 88%–94%). The only significant variable in meta-regressions was the proportion with IDU history (meta-regression co-efficient 0·004, p=0·032, adjusted R2=52·3%). Among juvenile detainees with a history of IDU (two sources) prevalence was 66% (45/68; 95% CI: 54%, 77%) in a mixed-sex sample in Bulgaria (30) and 36% (19/53; 95% CI: 24%, 49%) in a male sample from Australia (31).
Table 2 shows the regional coverage of our data sources and prevalence of anti-HCV among detainees. Extrapolating our findings to the global prisoner population, we estimate that 2·2 million prison detainees are anti-HCV positive (range 1·4 million–2·9 million) (Table 3). The largest populations of anti-HCV positive prisoners are in North America (668,500 persons, range 553,500–784,000) and East and South-East Asia (638,000 persons, range 332,000–970,000).
Table 2.
Estimated global and regional prevalence of hepatitis C virus antibodies among prison detainees
| N included sources | % of general detainee populations with HCV antibody prevalence data | Pooled HCV antibody prevalence (95% CI) | Prison detainee population | Estimated number of HCV antibody positive prison detainees | |||
|---|---|---|---|---|---|---|---|
| Low | Mid | High | |||||
| Sub-Saharan Africa | 4 | 8 | 16 (7, 26) | 785,00 | 55,000 | 125,500 | 204,000 |
| Western Europe | 39 | 92 | 30 (26, 34) | 478,500 | 124,500 | 143,500 | 162,500 |
| Eastern Europe | 6 | 16 | 22 (14, 31) | 1,199,000 | 168,000 | 263,500 | 371,500 |
| Latin America | 12 | 68 | 14 (8, 19) | 1,161,000 | 93,000 | 162,500 | 220,500 |
| Australasia | 9 | 78 | 35 (28, 43) | 37,500 | 10,500 | 13,000 | 16,000 |
| North America | 14 | 100 | 29 (24, 34) | 2,306,00 | 553,500 | 668,500 | 784,000 |
| South Asia | 4 | 56 | 8 (4, 11) | 827,000 | 33,000 | 66,000 | 91,000 |
| Middle East and North Africa | 1 | 1 | 3 (1, 5) | 491,500 | 5,000 | 14,500 | 24,500 |
| East and Southeast Asia | 2 | 8 | 25 (13, 38) | 2,552,000 | 332,000 | 638,000 | 970,000 |
| Central Asia | 1 | 8 | 38 (32, 43) | 123,500 | 39,500 | 47,000 | 53,000 |
| Pacific Islands | - | 0 | - | 8,500 | - | - | - |
| Caribbean | - | 0 | - | 34,000 | - | - | - |
| Extrapolated global | 92 | 45 | 26 (23, 29) | 10,004,000 | 1,423,000 | 2,154,500 | 2,910,000 |
Note: ‘Prison’ includes all institutions for adults charged with, awaiting trial or sentenced for a criminal offence. It does not include compulsory detoxification centres. All figures rounded to the nearest 500 people. Extrapolated global figure totalled from regional estimates prior to rounding. “-“ indicates there were no data on HCV prevalence located in this region. These regions were included in the extrapolated global estimate by applying the total estimated HCV prevalence to the prison detainee population for these regions. Data on detainee populations obtained from the World Prison Brief of the International Centre for Prison Studies (http://www.prisonstudies.org/).
Additional analyses of anti-HCV prevalence among detainees who have injected drugs or obtained tattoos while detained are provided in the supplementary materials.
Discussion
Hepatitis C virus infection is an extensive problem among detainees of prisons and other closed settings globally. One in four detainees overall, and two in three detainees with a history of drug injection, are anti-HCV positive. With at least 10 million people detained in prisons or other closed settings at any point in time (32), this translates to 2·2 million prisoners being anti-HCV positive; several times that number pass through a closed setting each year, making transmission both in and outside of detention a serious concern.
HCV incidence
We found consistent evidence that incident HCV infection occurs in closed settings, particularly among detainees who inject drugs. Widespread implementation of preventive measures is urgently needed to address HCV transmission in prisons and other closed settings. Multi-component interventions that combine evidence-based drug dependence treatment and access to sterile needles and syringes are most effective in reducing HCV seroconversion among people who inject drugs (33, 34). These interventions can be provided safely in closed settings and have the additional benefit of reducing HIV transmission risk (35, 36), but have rarely been implemented (37, 38). Although there is value in providing risk reduction education and counselling to detainees, this approach alone is not considered sufficient to prevent HCV transmission (34).
Anti-HCV prevalence
In addition to their role in HCV prevention, our findings suggest that closed settings are important sites for the diagnosis and treatment of prevalent infection. Voluntary HCV testing of detainees has the potential to vastly increase the number of people who are aware of their infection, enabling them to take steps to address their personal risks for disease progression (e.g. alcohol use) and to prevent onward transmission, both in closed settings and following their return to the community. HCV testing is warranted at entry to a closed setting, and persons who are anti-HCV negative should be offered testing periodically or if clinically indicated in order to identify incident infection. Detainees screening positive for anti-HCV should be offered vaccination against hepatitis A and B; and information regarding risks for disease progression and onward transmission. If identified, acute HCV infection should be treated, as sustained virological response rates are higher than observed in the treatment of chronic infection (39).
Treatment for chronic HCV infection can be provided in closed settings with sustained virological response rates comparable to those in community settings (40, 41). Providing treatment in closed settings would not only aid detainees but also generate substantial public health benefits, including reducing the pool of infection (thereby reducing the likelihood of exposure among people engaging in risk behaviours) and reducing the burden of disease associated with chronic HCV infection. There are, however, substantial barriers to widespread implementation of treatment. HCV treatment remains costly and places significant financial burdens on the healthcare budgets of closed settings. Additionally, aspects of life in detention such as high detainee turnover, unpredictable access to healthcare workers, lockdowns, and inadequate nutrition may interfere with demanding treatment regimens that require medication to be taken at regular intervals and careful monitoring of side effects. Meeting these challenges will be crucial as we enter a new era of HCV therapy (14), as widespread treatment in closed settings has the potential to dramatically reduce the burden of HCV-related disease and should be a public health priority.
Extra-judicial detention centres for people who use drugs
Only two sources presented data on anti-HCV prevalence among detainees of extra-judicial detention centres for people who use drugs. In these two studies, prevalence was 80% and 90%-higher than the overall summary estimate of anti-HCV prevalence among detainees with a history of injecting drug use. There are few data enumerating the total population of these detention centres, which exist in China, Lao PDR, Vietnam, Iran, Taiwan and Thailand, among others (4, 22). In China alone, perhaps 300,000 people who use drugs are detained in these centres annually; in Vietnam, in excess of 60,000 people are detained at any one time (4). It is a matter of great concern that there were so few data sources relating to detainees of extra-judicial detention centres for people who use drugs, and that the two available data sources indicated extremely high anti-HCV prevalence. This finding supports the United Nations call for the closure of extra-judicial detention centres for people who use drugs and, pending closure, dramatic improvements in the health services provided to detainees (42).
Limitations
A limitation of this study is variation in the manner in which HCV incidence and prevalence data were collected and reported in primary sources. The majority of included sources employed convenience sampling, and so sampled detainees may not have been representative of the broader detainee population. Reinforcing this point, sources reporting data from random samples of general population detainees had significantly lower anti-HCV prevalence than sources with convenience samples.
We used all identified data sources to estimate the summary prevalence of anti-HCV; however, older studies reported higher anti-HCV prevalence than more recent studies. As a result, our summary prevalence estimates may over-estimate the true anti-HCV burden. In evaluating our estimates, it is also important to note that very few data sources were located for some regions known to have high prevalence of anti-HCV among people who inject drugs, such as East and South-east Asia (5). Despite a broad-based search strategy, no data were located for several countries with large incarcerated populations, including Russia, which has the world’s second largest prisoner population, and China, which, as noted above, operates a large network of extra-judicial detention centres for people who use drugs in addition to correctional facilities operating under the criminal justice system. No data could be located for countries of the Caribbean and the Pacific Islands. Even in well-represented regions, such as Western Europe and North America, data frequently related to single institutions or institutions within a defined geographical area. Systematic data collection at the country or jurisdictional level is urgently required to allow for accurate appraisal of the scale of this issue, and to inform policy and clinical responses.
Conclusion
The burden of hepatitis C virus in detained populations, particularly in areas where injecting drug use is highly prevalent among detainees, is a major public health concern. Despite this, epidemiologic data on the extent of HCV infection in detained populations is lacking in many countries. The global response to HCV in closed settings has been limited, with few countries implementing the necessary preventive interventions or providing treatment for HCV-infected detainees. Greater attention towards HCV prevention, diagnosis, and effective delivery of treatment to detained populations is urgently required.
Supplementary Material
Acknowledgments
Funding support
Financial support for this study was provided by the HIV/AIDS Department of the World Health Organization. SL is supported by an Australian National Health and Medical Research Council Early Career (NHMRC) Research Fellowship (1035149). CGB is supported by a US National Institutes of Health (NIH) Career Development Award (NIDA K23DA021095). JDR is supported by a NIH Midcareer Investigator Award in Patient Oriented Research (NIDA K24DA022112). LD is supported by an NHMRC Senior Research Fellowship (10417142). The National Drug and Alcohol Research Centre receives core funding from the Australian Government Department of Health and Ageing. The Lifespan/Tufts/Brown Center for AIDS Research is funded by the NIH (NIAID P30AI042853).
Thank you to the following individuals and organisations for assistance in completing this review: Mary Kumvaj, National Drug and Alcohol Research Centre, University of New South Wales, for assistance with developing search strings and locating literature; Paul Nelson, National Drug and Alcohol Research Centre, University of New South Wales, for methodological advice; Christine Reavis, student intern, for assisting with the literature search; and Annette Verster, HIV/AIDS Department, World Health Organization, for funding support and assisting with identification of grey literature. We thank the following individuals for providing data used in this study: Frederick Altice; Bradley Brockmann; Silviu Ciobanu; Svetlana Doltu; Joumana Hermez; Saliya Karymbaeva; Ruth Zimmerman.
Abbreviations
- HCV
hepatitis C virus
- IDU
injecting drug use
- HIV
human immunodeficiency virus
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- py
person-years
Contributor Information
Sarah Larney, Email: s.larney@unsw.edu.au.
Hannah Kopinski, Email: hannah_kopinski@brown.edu.
Curt G. Beckwith, Email: cbeckwith@lifespan.org.
Nickolas D. Zaller, Email: nzaller@lifespan.org.
Don Des Jarlais, Email: ddesjarlais@cphnet.org.
Holly Hagan, Email: hh50@nyu.edu.
Josiah D. Rich, Email: jrich@lifespan.org.
Brenda J. van den Bergh, Email: bvb@euro.who.int.
Louisa Degenhardt, Email: l.degenhardt@unsw.edu.au.
References
- 1.Hanafiah KM, Groeger J, Flaxman AD, Wiersman ST. Global epidemiology of hepatitis C virus infection: New estimates of age-specific antibody to hepatitis C virus seroprevalence. Hepatology. doi: 10.1002/hep.26141. in press. [DOI] [PubMed] [Google Scholar]
- 2.Hutin Y, Kitler ME, Dore GJ, Perz JF, Armstrong GL, Dusheiko G, Ishibashi H, et al. Global Burden of Disease (GBD) for Hepatitis C. Journal of Clinical Pharmacology. 2004;44:20–29. doi: 10.1177/0091270003258669. [DOI] [PubMed] [Google Scholar]
- 3.Lavanchy D. The global burden of hepatitis C. Liver International. 2009;29 (suppl 1):74–81. doi: 10.1111/j.1478-3231.2008.01934.x. [DOI] [PubMed] [Google Scholar]
- 4.Mathers B, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee SA, Wodak A, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: A systematic review. The Lancet. 2008;372:1733–1745. doi: 10.1016/S0140-6736(08)61311-2. [DOI] [PubMed] [Google Scholar]
- 5.Nelson PK, Mathers BM, Cowie B, Hagan H, Des Jarlais D, Horyniak D, Degenhardt L. Global epidemiology of hepatitis B and hepatitis C in people who inject drugs: Results of systematic reviews. The Lancet. 2011;378:571–583. doi: 10.1016/S0140-6736(11)61097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United Nations Office on Drugs and Crime. HIV prevention, treatment and care in prisons and other closed settings: A comprehensive package of interventions. United Nations Office on Drugs and Crime; 2012. [Google Scholar]
- 7.Dolan K, Kite B, Black E, Aceijas C, Stimson GV. HIV in prison in low-income and middle-income countries. The Lancet Infectious Diseases. 2007;7:32–41. doi: 10.1016/S1473-3099(06)70685-5. [DOI] [PubMed] [Google Scholar]
- 8.Hayashi K, Milloy MJ, Fairbairn N, Kaplan K, Suwannawong P, Lai C, Wood E, et al. Incarceration experiences among a community-recruited sample of injection drug users in Bangkok, Thailand. BMC Public Health. 2009:9. doi: 10.1186/1471-2458-9-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kinner SA, Jenkinson R, Gouillou M, Milloy MJ. High-risk drug-use practices among a large sample of Australian prisoners. Drug and Alcohol Dependence. 2012 doi: 10.1016/j.drugalcdep.2012.05.008. in press. [DOI] [PubMed] [Google Scholar]
- 10.Pollini RA, Alvelais J, Gallardo M, Vera A, Lozada R, Magis-Rodriquez C, Strathdee SA. The harm inside: Injection during incarceration among male injection drug users in Tijuana, Mexico. Drug and Alcohol Dependence. 2009;103:52–58. doi: 10.1016/j.drugalcdep.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Post JJ, Dolan K, Whybin LR, Carter IW, Haber P, Lloyd A. Acute hepatitis C virus infection in an Australian prison inmate: Tattooing as a possible transmission route. Medical Journal of Australia. 2001;174:183–184. doi: 10.5694/j.1326-5377.2001.tb143214.x. [DOI] [PubMed] [Google Scholar]
- 12.Tsang TH, Horowitz E, Vugia DC. Transmission of hepatitis C through tattooing in a United States prison. American Journal of Gastroenterology. 2001;96:1304–1305. doi: 10.1111/j.1572-0241.2001.03728.x. [DOI] [PubMed] [Google Scholar]
- 13.Taylor LE, Swan T, Mayer KH. HIV coinfection with hepatitis C virus: Evolving epidemiology and treatment paradigms. Clinical Infectious Diseases. 2012;55 (Suppl 1):S33–S42. doi: 10.1093/cid/cis367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ghany MG, Nelson DR, Strader DB, Thomas DL, Seeff LB. An update on treatment of genotype 1 chronic hepatitis C virus infection: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 2012;54:1433–1444. doi: 10.1002/hep.24641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gane E. Future perspectives: Towards interferon-free regimens for HCV. Antiviral Therapy. 2012;17:1201–1210. doi: 10.3851/IMP2431. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-analyses: The PRISMA Statement. PLoS Medicine. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gough E, Kempf MC, Graham L, Manzanero M, Hook EW, Bartolucci A, Chamot E. HIV and hepatitis B and C incidence rates in US correctional populations and high risk groups: A systematic review and meta-analysis. BMC Public Health. 2010;10:art. no. 777. doi: 10.1186/1471-2458-10-777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Macalino GE, Hou JC, Kumar MS, Taylor LE, Sumantera IG, Rich JD. Hepatitis C infection and incarcerated populations. International Journal of Drug Policy. 2004;15:103–114. [Google Scholar]
- 19.Vescio MF, Longo B, Babudieri S, Starnini G, Carbonara S, Rezza G, Monarca R. Correlates of hepatitis C virus seropositivity in prison inmates: A meta-analysis. Journal of Epidemiology and Community Health. 2008;62:305–313. doi: 10.1136/jech.2006.051599. [DOI] [PubMed] [Google Scholar]
- 20.Stern RK, Hagan H, Lelutiu-Weinberger C, Des Jarlais D, Scheinmann R, Strauss S, Pouget ER, et al. The HCV Synthesis Project: Scope, methodology and preliminary results. BMC Medical Research Methodology. 2008;8:62. doi: 10.1186/1471-2288-8-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ali H, Calabria B, Phillips B, Singleton J, Sigmundsdottir L, Congreve E, Roberts A, et al. Searching the grey literature to access information on drugs, alcohol and HIV/AIDS research: An update. Sydney: National Drug and Alcohol Research Centre; 2010. [Google Scholar]
- 22.WHO. Assessment of compulsory treatment of people who use drugs in Cambodia, China, Malaysia and Vietnam: An application of selected human rights principles. Manila: World Health Organization Western Pacific Regional Office; 2009. [Google Scholar]
- 23.Harris RJ, Bradburn MJ, Deeks JJ, Harbord RM, Altman DG, Sterne JAC. metan: Fixed- and random-effects meta-analysis. The Stata Journal. 2008;8:3–28. [Google Scholar]
- 24.Harbord RM, Higgins JPT. Meta-regression in Stata. The Stata Journal. 2008;8:493–519. [Google Scholar]
- 25.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. British Medical Journal. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hagan H, Pouget ER, Des Jarlais D, Lelutiu-Weinberger C. Meta-regression of hepatitis C virus infection in relation to time since onset of illicit drug injection: The influence of time and place. American Journal of Epidemiology. 2008;168:1099–1109. doi: 10.1093/aje/kwn237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mahfoud Z, Kassak K, Kreidieh K, Shamra S, Ramia S. Prevalence of antibodies to human immunodeficiency virus (HIV), hepatitis B and hepatitis C and risk factors in prisoners in Lebanon. Journal of Infection in Developing Countries. 2010;4:144–149. doi: 10.3855/jidc.517. [DOI] [PubMed] [Google Scholar]
- 28.Chu F-Y, Chiang S-C, Su F-H, Chang Y-Y, Cheng S-H. Prevalence of human immunodeficiency virus and its association with hepatitis B, C, and D virus infections among incarcerated male substance abusers in Taiwan. Journal of Medical Virology. 2009;81:973–978. doi: 10.1002/jmv.21481. [DOI] [PubMed] [Google Scholar]
- 29.Kheirandish P, Seyedalinaghi S, Jahani M, Shirzad H, Seyed Ahmadian M, Majidi A, Sharifi A, et al. Prevalence and correlates of hepatitis C infection among male injection drug users in detention, Tehran, Iran. Journal of Urban Health. 2009;86:902–908. doi: 10.1007/s11524-009-9393-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Popov GT, Plochev KS, Chervenyakova TP. Prevalence of hepatitis C virus infection among juvenile prisoners. Journal of Hepatology. 2012;56:S546. [Google Scholar]
- 31.Ogilvie EL, Veit F, Crofts N, Thompson SC. Hepatitis infection among adolescents resident in Melbourne Juvenile Justice Centre: risk factors and challenges. Journal of Adolescent Health. 1999;25:46–51. doi: 10.1016/s1054-139x(98)00086-x. [DOI] [PubMed] [Google Scholar]
- 32.Walmsley R. World Prison Population List. 9. 2011. [Google Scholar]
- 33.Hagan H, Pouget ER, Des Jarlais DC. A systematic review and meta-analysis of interventions to prevent hepatitis C virus infection in people who inject drugs. Journal of Infectious Diseases. 2011;20:474–483. doi: 10.1093/infdis/jir196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.WHO. Guidance on prevention of viral hepatitis B and C among people who inject drugs. Geneva: World Health Organization; 2012. [PubMed] [Google Scholar]
- 35.Jurgens R, Ball A, Verster A. Interventions to reduce HIV transmission related to injecting drug use in prison. The Lancet Infectious Diseases. 2009;9:57–66. doi: 10.1016/S1473-3099(08)70305-0. [DOI] [PubMed] [Google Scholar]
- 36.Larney S, Toson B, Burns L, Dolan K. Effect of prison-based opioid substitution treatment and post-release retention in treatment on risk of re-incarceration. Addiction. 2012;107:372–380. doi: 10.1111/j.1360-0443.2011.03618.x. [DOI] [PubMed] [Google Scholar]
- 37.WHO. Interventions to address HIV in prisons: Needle and syringe programmes and decontamination strategies. Geneva: World Health Organization; 2007. [Google Scholar]
- 38.Larney S, Dolan K. A literature review of international implementation of opioid substitution treatment in prisons: Equivalence of care? European Addiction Research. 2009;15:107–112. doi: 10.1159/000199046. [DOI] [PubMed] [Google Scholar]
- 39.Boesecke C, Wedemeyer H, Rockstroh JK. Diagnosis and treatment of acute hepatitis C virus infection. Infectious Disease Clinics of North America. 2012:26. doi: 10.1016/j.idc.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 40.Allen SA, Spaulding AC, Osei AM, Taylor LE, Cabral AM, Rich JD. Treatment of chronic hepatitis C in a state correctional facility. Annals of Internal Medicine. 2003;138:187–190. doi: 10.7326/0003-4819-138-3-200302040-00010. [DOI] [PubMed] [Google Scholar]
- 41.Boonwaat L, Haber PS, Levy MH, Lloyd AR. Establishment of a successful assessment and treatment service for Australian prison inmates with chronic hepatitis C. Medical Journal of Australia. 2010;192:496–500. doi: 10.5694/j.1326-5377.2010.tb03605.x. [DOI] [PubMed] [Google Scholar]
- 42.United Nations. Joint statement: Compulsory drug detention and rehabilitation centres. United Nations: [accessed March 5, 2013]. 2012. Available from http://www.unaids.org/en/media/unaids/contentassets/documents/document/2012/JC2310_Joint%20Statement6March12FINAL_en.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.