Abstract
Emotional dysregulation and impaired attachment are seen by many clinical researchers as central aspects of borderline personality disorder (BPD). Alternatively, these constructs may represent general impairments in personality that are nonspecific to BPD. Using multitrait-multimethod models, we examined the strength of associations among preoccupied attachment, difficulties with emotion regulation, BPD features, and features of two other personality disorders (i.e., antisocial and avoidant) in a combined psychiatric outpatient and community sample of adults. Results suggested that preoccupied attachment and difficulties with emotion regulation shared strong positive associations with each other and with each of the selected personality disorders. However, preoccupied attachment and emotional dysregulation were more strongly related to BPD features than to features of other personality disorders. Our findings suggest that although impairments in relational and emotional domains may underlie personality pathology in general, preoccupied attachment and emotional dysregulation also have specificity for understanding core difficulties in those with BPD.
Borderline personality disorder (BPD) is a painful and debilitating disorder characterized by affective instability, identity disturbance, chaotic relationships, and impulsive self-destructive behaviors such as repeated suicide attempts and non-suicidal self-injury (Diagnostic and Statistical Manual of Mental Disorders, 4th ed. [DSM-IV-TR]; American Psychiatric Association [APA], 2000). Interpersonal and emotional dysregulation are central to many theories of BPD (e.g, Gunderson & Lyons-Ruth, 2008; Kernberg, 1984; Levy, 2005; Linehan, 1993), and evidence suggests that these features are among the most prevalent and stable of BPD symptoms (McGlashan et al., 2005). Both clinical experience and empirical evidence suggest that negative affective states and mood-dependent behaviors among individuals with BPD are often evoked by upsetting interpersonal events (Herpertz, 1995; Stiglmayr et al., 2005). Patients with this disorder are frequently acutely sensitive and reactive to interpersonal rejection or abandonment, often leading to intense negative emotion and difficulties regulating affective experiences, which may further exacerbate relational instability.
Attachment theory (Bowlby 1969) offers a developmental perspective and organizing theoretical framework for understanding both interpersonal and emotional dysregulation in BPD. According to Bowlby, attachment styles are relatively stable relational patterns, beliefs, and expectancies about self and others that are rooted in early experiences with caregivers and that act as prototypes or heuristic guides for later interpersonal interactions. Secure attachment promotes the ability to regulate one’s emotions effectively through the use of strategies such as reappraisal, problem-solving, and self-soothing, as well as the ability to seek out and obtain support from important others (Shaver & Mikulincer, 2007). Thus, “attachment theory is fundamentally about emotional experiences and their regulation” (Tidwell, Reis, & Shaver, 1996, p. 731).
Although there does not appear to be any single category of insecure attachment that encompasses all individuals with BPD, several studies support a strong association between attachment anxiety and BPD (for reviews, see Agrawal, Gunderson, Holmes, & Lyons-Ruth, 2004; Levy, 2005; Meyer & Pilkonis, 2005). Attachment anxiety is characterized by intense desires for closeness coupled with acute sensitivity to rejection and threats of abandonment, patterns that are exemplified by the preoccupied form of insecure attachment. Preoccupied attachment is associated with hyperactivation of the attachment system in the face of emotional distress or threat and hypervigilance to the possibility of rejection or abandonment (Shaver & Mikulincer, 2007). Hyperactivation hinders attempts at problem solving and is associated with distress-intensifying appraisals (i.e., perceiving threats as more serious than they are, and perceiving oneself as unable to cope), emotion-focused coping strategies, excessive rumination, and other maladaptive behaviors that intensify and perpetuate the experience of negative emotions. These difficulties parallel the dysfunctional emotion regulation strategies seen in those with BPD (Glenn & Klonsky, 2009; Selby, Ward, & Joiner, 2010). We therefore focus our investigation on preoccupied attachment, which we believe best characterizes the relational ambivalence and instability, rejection sensitivity, and emotional reactivity seen in many individuals with BPD.
Nonetheless, the specificity of preoccupied attachment and emotional dysregulation to BPD versus their associations with personality pathology more generally are unclear. Multivariate analyses of both normative personality traits and pathological personality features often produce a broad, robust factor related to neuroticism, negative affectivity, or emotional dysregulation (Livesley & Jang, 2000; Wright et al., in press). Hence, emotional dysregulation may represent a central characteristic of all or most personality disorders (PDs), which may explain in part the extensive overlap among PD diagnoses (Zimmerman, Rothschild, & Chelminski, 2005). Similarly, theory and research suggest that all PDs are defined by chronic interpersonal dysfunction (Pincus & Wiggins, 1990; Livesley, 2011). Livesley (1998) has described PDs as adaptive failures in attachment and affiliation. The specificity of insecure attachment and emotional dysregulation to BPD versus their relevance to personality pathology more generally has importance for proposed revisions to diagnostic criteria for PDs in DSM-5, in which general impairments in personality (i.e., interpersonal and self functioning) are seen as the defining feature of PD, with specific phenotype manifestations captured by malaptive trait profiles. Hence, for the empirically based development of these criteria, there is a need to identify general markers of PDs and indicators that differentiate among individual PDs.
However, most studies of the relations among attachment, affective processes, and psychopathology have been limited by the use of only one assessment method, usually self reports or interviews. Method error (i.e., the variance attributable to the method of measurement rather than the construct of interest) can artificially attenuate or inflate relations among variables. With only a single method of measurement, it is impossible to disentangle the variance associated with measurement procedures from that associated with the traits of interest. Because no single method is free from bias, researchers have argued in favor of a multi-method and multi-informant approach to personality assessment (Kraemer, Measelle, Ablow, Essex, Boyce, & Kupfer, 2003; Vazire, 2006). Multi-method assessment allows for the decomposition of sources of variance in measures, thereby enhancing construct validity and interpretability of findings (Fiske, 1987). In the case of PD, shared method variance could contribute to the appearance of general shared impairments that are in fact more methodological artifact than substantive associations.
Despite the compelling evidence for emotional dysregulation and preoccupied attachment as central to BPD, it remains unknown whether these features are differentially represented in BPD relative to other PDs. The primary aim of this study is to examine the degree to which preoccupied attachment and difficulties with emotion regulation are associated with BPD features relative to the strength of their associations with other PD features. As “other PDs”, we selected antisocial and avoidant PDs (ASPD and AVPD, respectively) for comparison to BPD for both conceptual and practical reasons. ASPD is a relevant comparison given the evidence for shared biological and environmental risk factors for BPD and ASPD, including difficulties with both attachment and emotion regulation, which have led some to suggest that these disorders reflect multifinal outcomes of a shared etiology (Beauchaine, Klein, Crowell, Derbridge, & Gatzke-Kopp, 2009). Similarly, data indicate that individuals with AVPD demonstrate intense rejection sensitivity (similar to preoccupied attachment styles) and temperamental vulnerability to emotional dysregulation (Meyer, Ajchenbrenner, & Bowles, 2005). In addition, clinical experience and empirical evidence suggest that individuals with BPD tend to oscillate between interpersonal extremes, sometimes appearing more hostile and antisocial while at other times more submissive and avoidant in their interpersonal styles (e.g., Horowitz, 2004; Russell, Moskowitz, Zuroff, Sookman, & Paris, 2007). Finally, BPD, ASPD, and AVPD features are prevalent in general psychiatric and forensic settings (Kendall et al., 2009; Zimmerman et al., 2005), and both ASPD and AVPD show high rates of comorbidity with BPD (Grant, Chou, Goldstein, et al., 2008; Lieb, Zanarini, Schmahl, Linehan, Bohus, 2004). Hence, it is theoretically and clinically important to examine what these disorders share versus how they differ in terms of attachment and emotion regulation difficulties.
Each construct was measured using clinician ratings, self-reports, and informant reports, allowing us to use a multitrait-multimethod (MTMM) confirmatory factor analysis (CFA) approach, thereby ensuring that shared variance is the result of substantive associations as opposed to methodological design. We hypothesized that emotional dysregulation and preoccupied attachment would be significantly positively related to all three PDs, reflecting general personality impairment; however, we hypothesized that these constructs would be more strongly related to BPD than to the other two PDs, reflecting specificity to BPD.
Methods
Participants and Recruitment Procedures
The study sample consisted of 100 adult participants recruited for a study of interpersonal and emotional functioning among individuals with BPD (Mean age = 45.9, SD = 10.6, Range = 24 to 61 years old; 65% female). To sample a full range of PD features in both treatment-seeking and non-treatment seeking populations, the sample included 45 patients in treatment at a general outpatient psychiatric clinic and 55 community residents who were not receiving mental health care. The patient sample was recruited via promotional flyers in outpatient psychiatric treatment facilities and through research networking systems such as the psychiatric hospital research registry, research coordinator meetings, and/or direct referrals from outpatient clinics. Recruitment flyers targeted men and women between the ages of 21 and 60 with symptoms such as “intense and stormy relationships” or “self-injury”. The community sample was recruited by telephone through the use of a random digit dialing (RDD) method. All potential participants completed an initial screening interview (by phone or in person) to determine eligibility. Potential participants were screened using the McLean Instrument for Borderline Personality Disorder (MSI-BPD; Zanarini, Vujanovic, Parachini, Boulanger, Frankenburg, & Hennen, 2003). Our recruitment criteria were intended to capture the full spectrum of BPD features within both clinical and community populations by categorizing participants based on three strata (0–2, 3–4, or 5 or more diagnostic criteria endorsed on the MSI-BPD) and two groups (community and psychiatric). After the initial eligibility was established, participants were placed in one of the six cells determined by their MSI-BPD score and psychiatric service use.
In the total sample (N = 100), forty-five participants were single and never married, 35 were married, 19 were separated or divorced, and one was widowed. Fifty-nine participants identified as Caucasian, 36 as African American, four as more than one race, and one as Asian. Forty-eight participants were employed and 69 reported some educational attainment beyond high school, although 20 participants reported an annual household income of less than $10,000. Table 1 illustrates clinical characteristics of the clinic and community subsamples.
Table 1.
Axis I and II diagnostic information
| Clinic (n = 45) | Community (n = 55) | |||
|---|---|---|---|---|
| Current Axis I disorders | n | % | n | % |
| Mood | 27 | 60.0 | 8 | 14.5 |
| Anxiety | 16 | 35.6 | 12 | 21.8 |
| Substance-related | 13 | 28.9 | 7 | 12.7 |
| Eating | 1 | 2.2 | 0 | 0.0 |
| Somatoform | 2 | 4.4 | 1 | 1.8 |
| Other Axis I | 2 | 4.4 | 1 | 1.8 |
| Any Axis I diagnosis (1 or more) | 39 | 86.7 | 23 | 41.8 |
| Current Axis II disorders | ||||
| Paranoid | 1 | 2.2 | 4 | 7.3 |
| Schizoid | 2 | 4.4 | 0 | 0.0 |
| Schizotypal | 2 | 4.4 | 0 | 0.0 |
| Histrionic | 1 | 2.2 | 2 | 3.6 |
| Narcissistic | 2 | 4.4 | 0 | 0.0 |
| Antisocial | 7 | 15.6 | 0 | 0.0 |
| Borderline | 12 | 26.7 | 4 | 7.3 |
| Avoidant | 10 | 22.2 | 3 | 5.5 |
| Dependent | 1 | 2.2 | 0 | 0.0 |
| Obsessive-compulsive | 5 | 11.1 | 2 | 3.6 |
| PD-NOS | 10 | 22.2 | 4 | 7.3 |
| Any Axis II diagnosis (1 or more) | 36 | 80.0 | 14 | 25.5 |
Note. Axis I and II diagnoses were rated by the consensus team based on all available intake information, including the Structured Clinical Interview for DSM-IV Axis I disorders (SCID-I; First, Spitzer, Gibbon, & Williams, 1997) and the Structured Interview for DSM-IV Personality (SIDP-IV; Pfohl, Blum, & Zimmerman, 1997). “Other Axis I” disorders include adjustment, dissociative, and sexual disorders. No participants in this sample met criteria for a bipolar disorder. Several participants met criteria for more than one disorder, particularly within the clinic sample. The mean numbers of Axis I and II diagnoses in the clinic sample were 1.38 (SD = 0.81) and 1.18 (SD = 0.94), respectively; 20 (44.4%) clinic participants met criteria for more than one Axis I disorder, and 11 (24.4%) met criteria for more than one Axis II disorder. The mean numbers of Axis I and II diagnoses in the community sample were 0.55 (SD = 0.79) and 0.35 (SD = 0.73), respectively; 5 (9.1%) community participants met criteria for more than one Axis I disorder, and 3 (5.5%) met criteria for more than one Axis II disorder.
Participants were asked to identify up to three people that they knew well to serve as informants. For the sake of simplicity, we will refer to the informants as significant others (SO). We received at least one SO report for 86 research participants. Three SO reports were received from 52 participants (60%), two SO reports from 24 participants (28%) and one SO report from 10 participants (12%). Hence, the SO sample consisted of 214 individuals, of whom 151 (71%) were female (two SOs did not report gender). One hundred and fourteen (53%) of the SOs were relatives (89 of the 114 were first-degree relatives), 71 (33%) were friends, 27 (13%) were romantic partners (18 of the 27 were spouses), and the remaining two (1%) SO reports were received from a roommate and a co-worker. Of the 190 SOs who provided further information on their relationship with the research participant, 39 (20.5%) reported living with the research participant and having known the participant for an average of 27 years (SD = 16.2, Range = 3 months to 59 years). In order to provide a best estimate of each participants’ functioning based on these various sources of information,1 SO data were aggregated by calculating the mean of SO reports for each participant.
Assessment Procedures
At the initial assessment meeting, clinicians described the study in detail and obtained written, informed consent. Participants completed a battery of self-report questionnaires and clinical interviews, and SOs completed questionnaires about the participant. Interviewers were trained clinicians who had a Master’s or doctoral degree and at least five years of assessment/clinical experience. Clinical interviewers were blind to participants’ community or patient status and MSI-BPD scores. At the conclusion of each participant’s interviews, a consensus diagnostic case conference was conducted by a research team comprised of at least three individuals. At the case conferences, interviewers presented all historical and concurrent information collected during the intake process. Consensus-rated measures were completed in the case conference sessions. A complete description of the consensus rating process used in this research program has been provided in previous reports (e.g., Pilkonis et al., 1995; Stepp, Smith, Morse, Hallquist, & Pilkonis, 2011).
Measures
Preoccupied Attachment
Clinician-rated preoccupied attachment was assessed using the ambivalent and reverse-scored secure prototype scales from the Adult Attachment Prototype Ratings (AAPR; Pilkonis, 1988). The process used to create the AAPR and specific details of each prototype are described in previous reports (e.g., Pilkonis, 1988; Stepp et al., 2008). Additionally, we used the preoccupied and reverse-scored secure prototype scales from the Q-Sort for rating attachment interviews devised by Kobak (1989). The Q-sort (Kobak, 1989) was rated by the consensus team based on the Interpersonal Relations Assessment Interview (IRA; Heape, Pilkonis, Lambert, & Proietti, 1989), which asks about important relationships and attachment figures from childhood through adulthood. Self-reported and SO-reported preoccupied attachment was assessed using the attachment anxiety scale from the Experiences in Close Relationships-Revised (ECR-R; Fraley, Waller, & Brennan, 2000), a 36-item self-report questionnaire intended to assess two latent dimensions of attachment in romantic relationships (anxiety and avoidance). Internal consistency alphas (α) for the ECR-R anxiety scale (n = 18 items) were high for both self-reports (α = .94) and SO reports (α = .95).
Difficulties with Emotion Regulation
Clinician-rated difficulties with emotion regulation were assessed using the Emotional Experiencing and Regulation Interview (EERI; Reynolds, Yaggi, Morse, Stepp, & Pilkonis, 2006), which was developed by the research team to assess emotional reactivity and impairment in regulation strategies across four emotional states: anger, sadness, shame/embarrassment, and joy/happiness. Respondents are asked to provide a detailed description of a recent instance in which they experienced each emotion, including antecedents to the event and a step-by-step narrative of the chain of events. These narratives were written as a vignette for each emotion and the consensus team used the vignettes to rate participants on a number of salient dimensions of emotional functioning, including difficulties recognizing and labeling emotional reactions, difficulties accepting emotions, and emotional lability. Severity of impairment was measured on a 9-point scale where higher scores indicate dysfunctional emotion regulation. Consensus team members were blind to the diagnostic and attachment information collected throughout the intake process when scoring the EERI. In this analysis, we used the global level of emotional regulation functioning, which summarized the level of general impairment in emotion regulation across emotional states. This scale was highly correlated with other measures of emotion regulation difficulties (see Table 3). Thirty-four participants were rated using the EERI by multiple judges for evaluation of interrater reliability, with 11 participants rated by two judges, one by three, one by five, 12 by six, and 9 by seven judges. The interrater reliability coefficient (ICC) for the global EERI scale, calculated based on a one-way random effect model for the unequal number of raters per case, was very strong (ICC = .94).
Table 3.
Correlations and Descriptive Statistics for Manifest Variables Used in Confirmatory Factor Analysis Models
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. PA-CR | - | ||||||||||||||
| 2. PA-SR | .43*** | - | |||||||||||||
| 3. PA-SO | .59*** | .57*** | - | ||||||||||||
| 4. DER-CR | .61*** | .45*** | .55*** | - | |||||||||||
| 5. DER-SR | .60*** | .58*** | .44*** | .57*** | - | ||||||||||
| 6. DER-SO | .64*** | .53*** | .77*** | .60*** | .63*** | - | |||||||||
| 7. BPD-CR | .65*** | .51*** | .45*** | .67*** | .63*** | .48*** | - | ||||||||
| 8. BPD-SR | .66*** | .67*** | .54*** | .67*** | .83*** | .66*** | .72*** | - | |||||||
| 9. BPD-SO | .59*** | .53*** | .78*** | .63*** | .55*** | .85*** | .57*** | .68*** | - | ||||||
| 10. ASPD-CR | .39*** | .22* | .15 | .25* | .29** | .25* | .40*** | .38*** | .28* | - | |||||
| 11. ASPD-SR | .37*** | .39*** | .24* | .32** | .42*** | .21* | .44*** | .52*** | .40*** | .46*** | - | ||||
| 12. ASPD-SO | .52*** | .42*** | .63*** | .52*** | .46*** | .66*** | .54*** | .57*** | .85*** | .40*** | .45*** | - | |||
| 13. AVPD-CR | .33*** | .28** | .29** | .30** | .40*** | .31** | .23* | .41*** | .24* | −.06 | −.00 | .13 | - | ||
| 14. AVPD-SR | .40*** | .28** | .31** | .40*** | .64*** | .48*** | .34*** | .54*** | .31** | .01 | −.18† | .17 | .48*** | - | |
| 15. AVPD-SO | .42*** | .54*** | .68*** | .41*** | .54*** | .77*** | .36*** | .54*** | .73*** | .11 | .17 | .53*** | .53*** | .44*** | - |
| N | 100 | 100 | 83 | 99 | 100 | 86 | 100 | 100 | 85 | 100 | 100 | 86 | 100 | 100 | 85 |
| M | 0.00 | 3.46 | 3.53 | 4.48 | 0.00 | 70.69 | 2.60 | 0.00 | 0.01 | 1.52 | 241.99 | 3.52 | 1.61 | 161.78 | 4.17 |
| SD | 0.78 | 1.45 | 1.08 | 1.30 | 0.57 | 22.21 | 3.41 | 13.91 | 0.95 | 2.52 | 32.13 | 3.11 | 2.70 | 28.72 | 3.17 |
| Skewness | −0.41 | 0.43 | −0.07 | 0.58 | 0.54 | 0.50 | 1.46 | 0.31 | 0.80 | 1.87 | −0.35 | 1.09 | 2.38 | 0.20 | 1.13 |
| Kurtosis | −0.86 | −0.67 | −0.17 | −0.13 | 0.03 | −0.45 | 1.16 | −0.70 | 0.72 | 2.73 | 1.07 | 0.77 | 6.34 | 0.22 | 1.63 |
Note. CR = Clinician-rated, SR = Self-report, SO = Significant other-rated, PA = Preoccupied Attachment, DER = Difficulties with Emotion Regulation, BPD = Borderline Personality Disorder, ASPD = Antisocial Personality Disorder, AVPD = Avoidant Personality Disorder.
p < .10.
p < .05.
p < .01.
p < .001.
Self-reported emotion regulation was assessed using the reverse-scored subscales comprising the Effortful Control factor of the Adult Temperament Questionnaire (ATQ; Rothbart, Ahadi, & Evans, 2000), the reverse-scored reappraisal scale of the Emotion Regulation Questionnaire (ERQ; Gross & John, 2003), and the sum total of five scales from the Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004). The ATQ (Rothbart et al., 2000) Effortful Control factor contains 35 items and three subscales: attentional control (12 items; α = .88), inhibitory control (11 items; α = .73), and activation control (12 items; α = .87). The ERQ (Gross & John, 2003) reappraisal scale is comprised of six items (α = .78) and is intended to gauge the ability to change the way a situation is interpreted or understood in order to lessen the emotional impact of the situation, capacities that are often impaired in those with preoccupied attachment (Shaver & Mikulincer, 2007). The DERS (Gratz & Roemer, 2004) contains 36 items and produces six subscales: lack of emotional clarity, limited access to emotion regulation strategies, lack of emotional awareness, impulse control difficulties, difficulties engaging in goal-directed behavior, and nonacceptance of emotional responses. In this analysis, we used the sum of scores for five of the six DERS subscales (30 items; α = .96). The lack of emotional awareness subscale of the DERS was not used because it led to decrements in goodness-of-fit of the measurement model, and previous studies have found this scale to be less strongly related to BPD than other DERS subscales (e.g., Selby et al., 2010). SO ratings on the same fives subscales of the DERS were also used in this analysis as an informant measure of emotion regulation (α = .97).
PD symptoms
Clinician-rated PD symptoms were assessed using a DSM checklist that was rated by the consensus team using all available information from intake, including responses from administration of the Structured Interview for DSM-IV Personality (SIDP-IV; Pfohl, Blum, & Zimmerman, 1997). The individual DSM-IV diagnostic criteria for each PD were rated on a 0–2 scale (0 = absent, 1 = present, 2 = strongly present). The clinician-rated PD dimensional scores were calculated by summing these scores for the corresponding PD criteria. Twenty percent of participants’ SIDP-IV interviews were videotaped and rated by at least one independent rater for calculation of interrater reliability. Three participants’ interviews were rated by six judges, 16 were rated by five judges, and one was rated by two judges. ICC’s were calculated based on one-way random effect models for the unequal number of raters per case, and demonstrated adequate interdiagnostician agreement for BPD (ICC = .84), ASPD (ICC = .86), and AVPD (ICC = .78) dimensional scores.
To derive scores for self-reported PD features, we used Miller’s method (Miller, Bagby, Pilkonis, Reynolds, & Lynam, 2005) for scoring PDs based on the Revised NEO Personality Inventory (NEO-PI-R; Costa & McCrae, 1992). The NEO-PI-R is a widely used measure of the personality traits that comprise the five factor model (FFM) of personality (Neuroticism, Extraversion, Openness to Experience, Agreeableness, and Conscientiousness). Miller et al.’s (2005) method for assessing PDs based on the NEO-PI-R involves taking the simple sum of selected FFM facets (for details and scoring procedures, see Miller et al., 2005). Evidence supports the clinical utility of this approach for assessing self-reported PD features. We used the BPD (9 items; α = .80), ASPD (17 items; α = .64), and AVPD (10 items; α = .74) scales.
Additional self-report measures of BPD features included the Personality Assessment Inventory Borderline Features Scale (PAI-BPD; Morey, 1991), McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD; Zanarini et al., 2003), and selected items from the Interpersonal Inventory of Personal Problems (IIP; Horowitz, Rosenberg, Baer, Ureno, & Villasenor, 1988). The PAI-BOR (Morey, 1991) comprises 24 items (α = .94) that are rated on a 4-point scale (0 = false, 3 = very true). The MSI-BPD (Zanarini et al., 2003) contains 10 true-false questions (α = .87), with each endorsed item receiving a score of 1. Total MSI-BPD scale scores 7 have been shown to have good sensitivity (.81) and specificity (.85) relative to a BPD diagnosis (Zanarini, et al, 2003). We also obtained self- and SO-reported BPD features using a subset of items from the 90-item version of the IIP (Horowitz et al., 1988), which is a self-report questionnaire intended to assess interpersonal difficulties and associated distress. In a separate sample from a previous research protocol, we identified eight items that correlated most highly with dimensional BPD scores from clinical interviews, and calculated the sum of these items to create scales used for both self-reported (α = .88) and SO-rated (α = .90) BPD.
SOs also rated participants’ personality features on the Multi-source Assessment of Personality Pathology (MAPP; Oltmanns, Turkheimer, & Strauss, 1998; Thomas, Turkheimer, & Oltmanns, 2003), an informant measure of personality developed by translating the DSM-IV personality disorder criteria into more simplified, layman’s terms. The measure contains 103 items rated on a 4-point scale (0 = never like this, 3 = always like this), and generates scores for all ten personality disorders included in the DSM-IV. The BPD scale is comprised of nine items (α = .91), the ASPD scale is comprised of 7 items (α = .86), and the AVPD scale is comprised of 7 items (α = .86).
Statistical Procedures
Preliminary data analyses were conducted using SPSS 19.0 (SPSS Inc., Chicago, IL) and latent variable models were tested using Mplus Version 6.1 for Windows (Muthén & Muthén, 2010). Given the modest sample size, we estimated two separate confirmatory factor analysis (CFA) models to test study hypotheses. Each model included four latent constructs corresponding to preoccupied attachment, difficulties with emotion regulation, BPD symptoms, and one other PD (i.e., ASPD or AVPD). Each latent variable had three manifest indicators representing three methods (i.e., clinician ratings, self reports, and SO reports). In order to account for measurement error and method variance in our models, we specified correlated uniqueness CFA models (Kenny, 1979; Marsh, 1989) to the MTMM correlation matrices of the 12 observed variables. Each indicator was specified to load on only one trait factor. Correlations among trait factors were freely estimated. Method effects were estimated by specifying correlated errors among indicators sharing the same assessment method.
Prior to conducting our primary analyses, we first constructed latent variable models for constructs that were assessed through multiple measures of the same method (e.g., clinician-rated preoccupied attachment, which was assessed using four clinician-rated subscales) and extracted factor scores from well-fitting measurement models (i.e., from CFAs estimated in Mplus), which were then used as manifest variables in our primary analyses. Measures used to construct the variables included in the primary analyses are listed in Table 2. Further details on these preliminary models and scale construction are available by request from the first author.
Table 2.
Measures Used to Create Manifest Variables for Multitrait Multimethod Models
| Trait Construct and Manifest Variables | Measures/Scales Used |
|---|---|
| Preoccupied Attachment | |
| Clinician Report | Latent factor score from four observed variables:
|
| Self Report | ECR-R -Attachment Anxiety |
| Significant Other Report | ECR-R - Attachment Anxiety |
| Difficulties with Emotion Regulation | |
| Clinician Report | EERI - Global Functioning |
| Self Report | Latent factor score from five observed variables:
|
| Significant Other Report | DERS – Total of 5 subscales |
| Borderline Personality Disorder (BPD) | |
| Clinician Report | DSM Consensus Checklist |
| Self Report | Latent factor score from four observed variables:
|
| Significant Other Report | Latent factor score from two observed variables:
|
| Antisocial and Avoidant Personality Disorders | |
| Clinician Report | DSM Consensus Checklist |
| Self Report | NEO-PI-R |
| Significant Other Report | MAPP |
Note. AAPR = Attachment Adult Attachment Prototype Ratings; ECR-R = Experiences in Close Relationships Scale-Revised; ATQ = Adult Temperament Questionnaire; EERI = Emotional Experiencing and Regulation Interview; ERQ = Emotion Regulation Questionnaire; DERS = Difficulties in Emotion Regulation Scale; NEO-PI-R = Revised NEO Personality Inventory; PAI-BPD = Personality Assessment Inventory Borderline Features Scale; MSI-BPD = McLean Screening Instrument for Borderline Personality Disorder; IIP = Interpersonal Inventory of Personal Problems; MAPP = Multi-source Assessment of Personality Pathology.
All latent variable models were tested using full-information maximum likelihood estimation with robust standard errors (MLR estimator), which can include missing data and produces unbiased parameter estimates and standard errors that are robust to non-normality. A variety of fit indices reflecting diverse criteria of overall model fit were evaluated, including the adjusted χ2, root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR), comparative fit index (CFI), and Tucker Lewis Index (TLI). Indications of adequate model fit included a non-significant (p < .05) adjusted chi-square (χ2) value [or χ2 over degrees of freedom ratio (χ2/df) < 3]; SRMR < .08; CFI and TLI > .90, and RMSEA < .08 (Kline, 1998). We examined differences in strength of associations between latent variables using the Wald χ2 statistic.
Results
Preliminary Analyses
Descriptive statistics and intercorrelations between manifest variables used in the primary analyses are presented in Table 3. Based on independent samples t-tests (corrected for inhomogeneity of variance when indicated), there were few significant sex or racial differences on manifest variables. However, men were higher than women in self-reported antisocial PD features at trend levels (ps = .08). Women were higher than men in self-reported avoidant PD features at a trend level (p = .08). Additionally, white participants had higher SO-reported avoidant PD features (p = .03) and lower clinician-rated antisocial PD features than non-white participants at a trend level (p = .06).
There were significant differences between the community and patient samples for all manifest variables (all p’s < .05), with patients reporting more preoccupied attachment, emotion dysregulation, and PD symptoms than community participants. To evaluate the appropriateness of combining the two samples in subsequent measurement models, we conducted a series of multiple-group CFAs to test the equivalence (i.e., invariance) of the factor structure (i.e., measurement model) between the community and patient participants. Results demonstrated strong invariance of measurement parameters (e.g., factor loadings, intercepts, residual covariances) between the community and patient samples for all constructs, with no significant degradation in model fit when constraining these parameters to equality. We therefore considered it appropriate to combine the two samples in subsequent analyses.
Primary Analyses
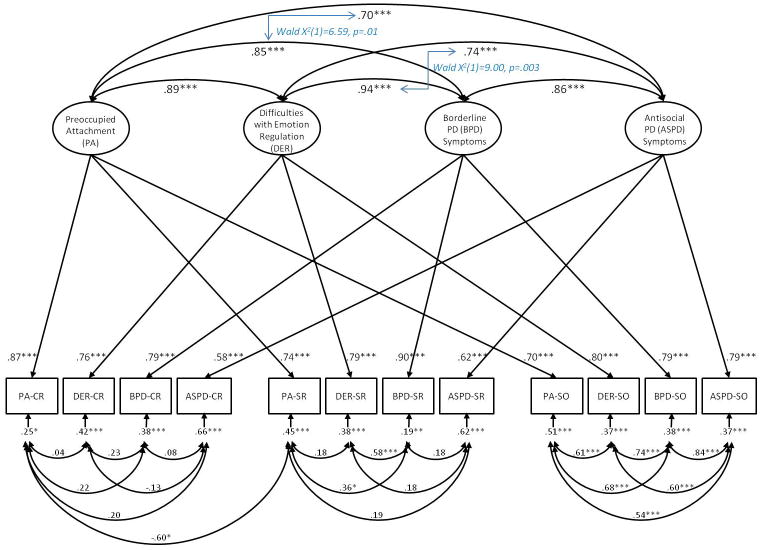
In both CFA models, modification indices suggested that residuals of clinician- and participant-rated attachment should be correlated. The addition of this correlated error significantly improved each model’s fit based on adjusted χ2 difference tests, and was therefore included in final reported models. The first model included preoccupied attachment (PA), difficulties with emotion regulation (DER), BPD, and ASPD features. Standardized parameter estimates are portrayed in Figure 1. This model fit the data well (χ2 [29] = 38.08, p = .12; χ2/df = 1.31; RMSEA = .06; SRMR = .04; CFI = .99; TLI = .97). Trait factor loadings were all highly significant (ps < .001), demonstrating good convergent validity among measures of each trait. The magnitude of correlated errors among SO-reported constructs was high, demonstrating substantial method effects for SO reports. This suggests a halo effect (i.e., where ratings of one trait tend to influence ratings on another trait) for informant-rated measures, with little differentiation between SO-rated constructs. There were only modest correlations between errors for self-report measures and even lower correlated errors for clinician-rated measures, suggesting that these assessments are less susceptible to halo effects than are informant-rated assessments. However, the positive error covariances among participant-rated DER and BPD and between PA and BPD suggest a halo effect for participant reports of these specific constructs. In other words, participants who rated themselves high on BPD features also tended to rate themselves high on PA and DER. Interestingly, the negative error covariance for clinician- and participant-rated PA indicates a lack of agreement between clinician-reports and self-reports of participants’ attachment patterns.
Figure 1.
Multitrait-multimethod confirmatory factor analysis model of Preoccupied Attachment (PA), Difficulties with Emotion Regulation (DER), Borderline Personality Disorder (BPD), and Antisocial Personality Disorder (ASPD). Completely standardized robust maximum likelihood parameter estimates. Wald χ2 values represent tests of significant differences between parameter estimates. Residual variance components (error variances) indicate the amount of unexplained variance. Thus, for each observed variable, R2 = (1 – error variance). CR = Clinician-rated; SR = Self-report; SO = Significant other-rated. *p < .05. **p < .01. ***p < .001.
Of primary relevance to our hypotheses, the correlations among latent traits of PA, DER, BPD, and ASPD were high (ranging from r = .70 to r = .94, all ps < .001), which is consistent with our hypothesis that PA and DER would be associated to some degree with all three PDs. BPD features were also highly correlated with ASPD features (r = .86, p < .001), demonstrating the high degree of overlap between PDs. Most importantly to our hypothesis of added specificity of PA and DER to BPD relative to other PDs, Wald χ2 tests demonstrated that PA shared significantly more variance with BPD than with ASPD (R2 = .72 vs. R2 = .49, respectively; Wald χ2 (1) = 6.59, p = .01) and DER shared more variance with BPD than with ASPD (R2 = .88 vs. R2 = .55, respectively; Wald χ2 (1) = 9.00, p = .003).
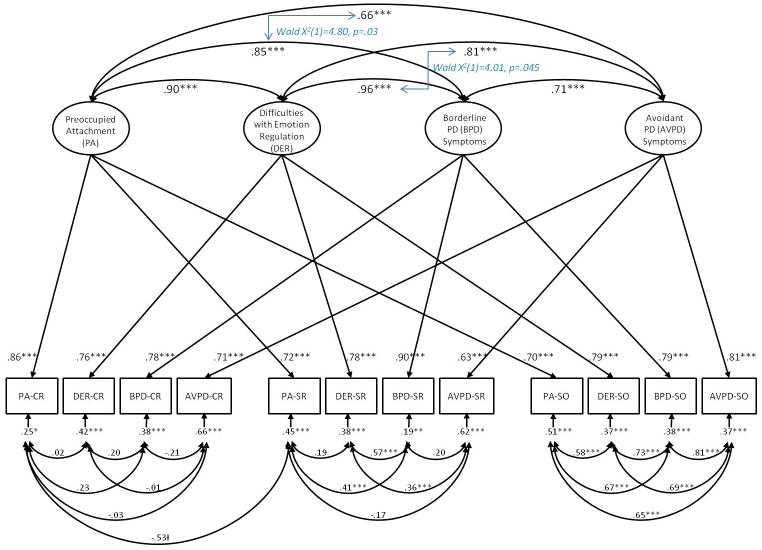
The second model included PA, DER, BPD, and Avoidant PD (AVPD) features. The standardized solution is illustrated in Figure 3. The model fit the data adequately according to most fit indices (χ2 [29] = 53.70, p = .004; χ2/df = 1.85; RMSEA = .09; SRMR = .04; CFI = .97; TLI = .93). Method effects in this model were similar to those observed in the first model, with a strong halo effect observed for SO-reported constructs, moderate method effects for participant-rated constructs, and relatively no method effects for clinician-rated constructs. Despite strong correlations between all latent variables, Wald χ2 tests indicated that PA shared significantly more variance with BPD than with AVPD (R2 = .81 vs. R2 = .73, respectively; Wald χ2 (1) = 4.80, p = .03) and DER shared more variance with BPD than with AVPD (R2 = .92 vs. R2 = .66, respectively; Wald χ2 (1) = 4.01, p = .045). Hence, our results demonstrated some specificity of PA and DER to BPD in comparison to AVPD, although somewhat higher correlations were observed between PA/DER and AVPD relative to those between PA/DER and ASPD.
Discussion
Using a MTMM latent variable approach, we examined the degree to which preoccupied attachment and difficulties with emotion regulation were associated with BPD features as compared to the strength of their associations with two other PDs (i.e., ASPD and AVPD). Our findings suggested that preoccupied attachment and difficulties with emotion regulation were strongly related to all three PDs we examined, and that BPD was also strongly related to both ASPD and AVPD. This finding supports the notion of a general PD factor and the proposed DSM-5 conceptualization of general impairments in personality (i.e., interpersonal and self functioning) as central characteristics of several PDs. However, both preoccupied attachment and difficulties with emotion regulation were more strongly associated with BPD than with ASPD and AVPD, despite the fact that BPD was so highly related to these other PDs. Our results therefore also indicate that preoccupied attachment and difficulty regulating emotions are particularly good specific markers for BPD.
Our results suggest that general impairments in attachment and emotion regulation may have utility for assessing the dimensional severity of global personality pathology. The high degree of overlap between these constructs and all three PDs, as well as the strong correlations observed between BPD and both ASPD and AVPD, are consistent with a dimensional representation of PD severity as suggested by several researchers and theorists (e.g., Bornstein, 1998; Kernberg, 1984; Livesley, 1998) and supported in recent empirical work (e.g., Hopwood et al., 2011; Jahng et al., 2011; Morey et al., 2011). For example, in a recent study with the Collaborative Longitudinal Personality Study sample (Hopwood et al., 2011), a generalized personality pathology severity dimension explained the majority of variance in current and prospective social, work, and leisure dysfunction. Additionally, studies suggest that a higher-order general PD factor may account for much of the covariance among all PDs (Jahng et al., 2011; Wolf, Miller, & Brown, 2011). It is possible that preoccupied attachment and emotional dysregulation are highly related to all PDs because difficulties with interpersonal and emotional functioning are common to these disorders. Moreover, the strong associations between BPD and both ASPD and AVPD provide additional empirical evidence of a general PD factor that cuts across these disorders.
Despite the high correlations between these constructs and all three PDs examined here, our results also suggest that a specific manifestation of impaired attachment (i.e., preoccupied attachment) and difficulties with emotion regulation (particularly those reflecting intense emotionality and behavioral dyscontrol) show specificity as diagnostic markers of BPD. Thus, these constructs may help to distinguish between individuals with BPD and those with ASPD or AVPD. These findings provide empirically grounded documentation of interpersonal and emotional patterns that have long been observed clinically in those with BPD. Preoccupied attachment patterns, which are characterized by intense desires for closeness accompanied by equally intense fears of rejection or abandonment, may not be as descriptive of those with prominent ASPD features, who are often interpersonally hostile, domineering, and uncomfortable with dependency (Pincus & Wiggins, 1990). Accordingly, several studies document associations between dismissive/avoidant attachment patterns and ASPD (e.g., Gacano & Meloy, 1991; Gacano, Meloy, & Berg, 1992; Rosenstein & Horowitz, 1996). In addition, those with ASPD features, as well as those with dismissive or avoidant attachment patterns, tend to demonstrate emotional coldness and denial of distress (e.g., Rosenstein & Horowitz, 1996; Austin & Deary, 2000), which is antithetical to the emotional intensity and reactivity that is often observed in those with BPD.
Likewise, although individuals with AVPD features may be similar to those with BPD in their desire for close relationships coupled with intense fears of rejection, those with AVPD tend to be more socially avoidant and detached (Pincus & Wiggins, 1990; Skodol et al., 2011). Because of their actively avoidant strategies to prevent potential rejection or embarrassment, those with AVPD tend to demonstrate more fearful rather than preoccupied attachment patterns (Meyer & Pilkonis, 2005). Further, the stronger association between difficulties with emotion regulation and BPD as compared to the association between these difficulties and AVPD is consistent with evidence of greater negative emotionality (Meyer et al., 2005) and functional impairment (Skodol et al., 2002) in those with BPD than in those with AVPD. Nonetheless, results suggest that AVPD is still strongly associated with difficulties regulating emotions, and this finding is consistent with evidence that AVPD is associated with high levels of neuroticism (Samuel & Widiger, 2008), disability (Cramer, Torgersen, & Kringlen, 2006; Grant et al., 2004), and comorbid anxiety disorders (for a review, see Skodol et al., 2011).
The surprisingly large correlations between all latent variables in our analyses are noteworthy, especially considering the rather moderate bivariate correlations that were observed between most of the manifest variables. For example, the correlation between BPD and ASPD latent factors (r = .86) is strikingly larger in magnitude than the bivariate correlations between clinician ratings of these disorders (r = .40) and greater than reported associations in other studies (e.g., Ekselius, Lindström, von Knorring, Bodlund, & Kullgren, 1994). This may be at least partially attributed to the disattenuation of correlations between variables that occurs when measurement error and method effects are controlled in a latent variable modeling context. Alternatively, it is possible that correlations between traits (i.e., trait-trait covariances) in this study are somewhat inflated as a result of similarities between the methods that are not represented in the models, which is a potential bias that can occur in correlated uniqueness MTMM models when correlations between distinct methods of measurement are nontrivial (Kenny & Kashy, 1992). Nonetheless, this bias would likely have resulted in the inflation of all trait-trait covariances and underestimation of discriminant validity between traits, which was not the focus of this study. Thus, the results of this study, which concern comparisons of trait-trait covariances within the same model, are not likely to be biased by this phenomenon. Some caution should be used, however, in interpreting the absolute strength of correlations between these constructs considering this potential source of bias in correlated uniqueness MTMM models.
In addition, the considerable method effects observed for SO reports of these constructs suggests that, although these are valuable sources of information, they are subject to halo effects more than other assessment methods. Specifically, SOs tend to rate participants high or low on all scales, with little differentiation between constructs, which is a well-known source of bias in informant reports of personality constructs (Nisbett & Wilson, 1977; Srivastava, Guglielmo, & Beer, 2010). This finding may reflect the relatively limited information available to SOs for rating participants, because SOs cannot report on participants’ internal experiences unless they are overtly expressed. The self-report measures were also somewhat susceptible to halo effects, albeit at a much more moderate level, which might reflect the high degree of demoralization experienced by many patients with PDs, leading them to report high levels of distress and impairment across domains. Clinician-rated measures appeared least susceptible to such method effects, which is a potential strength of the consensus-team rating process in which all information is used to derive clinical formulations and to better distinguish between domains. Nonetheless, the strong factor loadings for each trait suggest that all methods contributed valuable information to the assessment of these constructs.
It is also noteworthy that there was a significant negative error covariance between clinician- and participant-rated attachment, which we accounted for in our models. This result may indicate a lack of agreement between clinicians and participants in how they view their attachment patterns. This finding could reflect distinct aspects of attachment assessed by clinician-rated interviews and self-report instruments. Several authors have discussed how interviews and other clinician-rated measures of attachment may tap into a combination of implicit and explicit attachment-related representations, whereas, self-report instruments assess explicit attachment-related cognitions, feelings, and beliefs of which participants are consciously aware (Collins & Read, 1994; Shaver, Belsky, & Brennan, 2000). This finding is consistent with the idea that different methods of measuring attachment reflect unique components of the attachment system, which supports multi-method approaches to assessing attachment.
Accordingly, one of the greatest strengths of this study is the multi-method, multi-informant approach, which allowed us to control for method effects and examine the utility of various methods of measuring these constructs. This approach enhances the validity and interpretability of our results. In addition, our mixed clinic and community sample is advantageous in that a full range of PD symptom severity was represented, particularly with regard to cluster B and C disorders that are commonly seen in outpatient psychiatric clinic settings. The specific PDs we examined in this study have particular clinical relevance because they are often seen in either clinical or forensic settings. Although previous multivariate analyses of PD traits indicate that difficulties with attachment and emotion regulation consistently factor together and that the resulting factor is distinct from both antisocial and avoidant features (Livesley, 2007), other evidence suggests that ASPD and AVPD are near-neighbor disorders that are likely to have a similar underlying structure to BPD. Specifically, BPD was strongly correlated with both ASPD and AVPD in the current study, high rates of comorbidity have been observed in previous studies between BPD and both ASPD and AVPD, and similar etiological risk factors have been identified for these disorders. Hence, these near-neighbor PDs provide a stringent test for our hypotheses regarding the specificity of preoccupied attachment and difficulties with emotion regulation to BPD as compared to other PDs that show a high degree of overlap with BPD.
The most notable limitation of this study is the modest sample size relative to typical recommendations for latent variable modeling. Obtaining large samples is difficult with an intensive, multi-method clinical assessment protocol such as ours. However, the strength of correlations between variables in our study mitigates the need for large samples to obtain sufficient power. Another limitation to this study is that, due to the nature of our sample, only two PDs were examined for comparison to BPD, and Cluster A PDs are not represented in these analyses due to their low base-rate in our patient population. Therefore, results may not generalize to all Axis II disorders. We also did not examine distinct relations among these measures and PDs versus Axis I-related dysfunction. Our findings suggest the utility of conducting studies with large and clinically diverse samples to shed further light on the specificity of preoccupied attachment and emotional dysregulation to BPD as compared to other types of Axis I and II psychiatric disorders. Additionally, we did not incorporate attachment patterns other than preoccupied attachment into our models. Future studies should examine whether dismissive, fearful, or disorganized attachment might further elucidate impairments that are common to all PDs and those that are unique to individual PDs.
These findings have implications for the assessment of PDs in DSM-5 and for future research attempts to model such constructs. This study is timely because the development of methods for optimally assessing global PD severity as well as delineating the specific criteria that distinguish between individual PD types is a prominent debate in the field with direct implications for both clinical and research efforts. Our results are consistent with dimensional models of personality traits and suggest that impaired interpersonal and affective processes may represent global dimensions of general personality pathology severity. Accordingly, measures of these constructs may be effective for assessing Criterion A (i.e., impairments in self and interpersonal functioning) for PD diagnosis in DSM-5. However, our results also indicate that preoccupied attachment, as a specific form of insecure attachment, and difficulties regulating emotions, appear to have specificity for describing the BPD “type” and may distinguish BPD from other PDs. These findings support proposed DSM-5 criteria for BPD such as elevations in the trait domain of negative affectivity characterized by emotional lability, anxiousness, depressivity, and separation insecurity, as these specific traits are closely related to difficulties with emotion regulation and preoccupied attachment. Our results also underscore the importance of utilizing multiple measurement methods and controlling for measurement error in future studies in order to accurately capture the common and unique features of PDs.
Figure 2.
Multitrait-multimethod confirmatory factor analysis model of Preoccupied Attachment (PA), Difficulties with Emotion Regulation (DER), Borderline Personality Disorder (BPD), and Avoidant Personality Disorder (AVPD). Completely standardized robust maximum likelihood parameter estimates. Wald χ2 values represent tests of significant differences between parameter estimates. Residual variance components (error variances) indicate the amount of unexplained variance. Thus, for each observed variable, R2 = (1 – error variance). CR = Clinician-rated; SR = Self-report; SO = Significant other-rated. †p < .10. *p < .05. **p < .01. ***p < .001.
Acknowledgments
This research was supported by a grant from the National Institute of Mental Health (PI: Pilkonis; R01 MH056888, PI: Pilkonis). Dr. Scott’s effort was supported by T32 MH018269. Dr. Stepp’s effort was supported by K01 MH086713.
Footnotes
As expected given the range of relationships represented in our informant sample, as well as evidence from previous studies that multiple informants often provide discordant information about psychosocial functioning (Kraemer et al., 2003), SO ratings in this study were only moderately concordant (ICCs across SOs ranging from .44 to .59). Considering that participants likely function differently in different relationships and in different contexts, we did not expect nor desire perfect concordance between multiple informant ratings; however, the average of these informant reports should provide the best estimate of participants’ functioning across relational and situational contexts.
References
- Agrawal H, Gunderson J, Holmes B, Lyons-Ruth K. Attachment studies with borderline patients: A review. Harvard Review of Psychiatry. 2004;12:94–104. doi: 10.1080/10673220490447218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. rev. [Google Scholar]
- Austin EJ, Deary IJ. The ‘four as’: A common framework for normal and abnormal personality? Personality and Individual Differences. 2000;28(5):977–995. [Google Scholar]
- Beauchaine TP, Klein DN, Crowell SE, Derbidge C, Gatzke-Kopp L. Multifinality in the development of personality disorders: A Biology × Sex × Environment interaction model of antisocial and borderline traits. Development and Psychopathology. 2009;21:735–770. doi: 10.1017/S0954579409000418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornstein RF. Reconceptualizing personality disorder diagnosis in the DSM-V: The discriminant validity challenge. Clinical Psychology: Science and Practice. 1998;5:333–343. [Google Scholar]
- Bowlby J. Attachment. Vol. 1. New York: Basic Books; 1969. Attachment and loss. [Google Scholar]
- Collins NL, Read SJ. Cognitive representations of attachment: The structure and function of working models. In: Bartholomew K, Perlman D, editors. Attachment processes in adulthood. London: Kingsley; 1994. pp. 53–90. [Google Scholar]
- Costa PT, Jr, McCrae RR. Revised NEO Personality Inventory (NEO–PI–R) and NEO Five-Factor Inventory (NEO–FFI) professional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Cramer V, Torgersen S, Kringlen E. Personality disorders and quality of life. A population study. Comprehensive Psychiatry. 2006;47:178–184. doi: 10.1016/j.comppsych.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Ekselius L, Lindström E, von Knorring L, Bodlund O, Kullgren G. Comorbidity among the personality disorders in DSM-III-R. Personality and Individual Differences. 1994;17(2):155–160. [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- Fiske DW. Construct invalidity comes from method effects. Educational and Psychological Measurement. 1987;47:285–307. [Google Scholar]
- Fraley RC, Waller NG, Brennan KA. An item response theory analysis of self-report measures of adult attachment. Journal of Personality and Social Psychology. 2000;78:350–365. doi: 10.1037//0022-3514.78.2.350. [DOI] [PubMed] [Google Scholar]
- Gacano CB, Meloy JR. A Rorschach investigation of attachment and anxiety in antisocial personality disorder. Journal of Nervous and Mental Disease. 1991;179:546–552. doi: 10.1097/00005053-199109000-00005. [DOI] [PubMed] [Google Scholar]
- Gacano CB, Meloy JR, Berg JL. Object relations, defensive operations, and affective states in narcissistic, borderline, and antisocial personality disorder. Journal of Personality Assessment. 1992;59:32–49. doi: 10.1207/s15327752jpa5901_4. [DOI] [PubMed] [Google Scholar]
- Glenn CR, Klonsky ED. Emotion dysregulation as a core feature of borderline personality disorder. Journal of Personality Disorders. 2009;23:20–28. doi: 10.1521/pedi.2009.23.1.20. [DOI] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, Ruan WJ. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69(4):533–450. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Prevalence, correlates, and disability of personality disorders in the united states: Results from the national epidemiologic survey on alcohol and related conditions. Journal of Clinical Psychiatry. 2004;65:948–958. doi: 10.4088/jcp.v65n0711. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. [Google Scholar]
- Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology. 2003;85:348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Lyons-Ruth K. BPD’s interpersonal hypersensitivity phenotype: A gene-environment-developmental model. Journal of Personality Disorders. 2008;22:22–41. doi: 10.1521/pedi.2008.22.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heape CL, Pilkonis PA, Lambert J, Proietti JM. Unpublished manuscript. 1989. Interpersonal Relations Assessment. [Google Scholar]
- Herpertz S. Self-injurious behaviour: Psychopathological and nosological characteristics in subtypes of self-injurers. Acta Psychiatrica Scandinavica. 1995;91:57–68. doi: 10.1111/j.1600-0447.1995.tb09743.x. [DOI] [PubMed] [Google Scholar]
- Hopwood CJ, Malone JC, Ansell EB, Sanislow CA, Grilo CM, McGlashan TH, Morey LC. Personality assessment in DSM-5: Empirical support for rating severity, style, and traits. Journal of Personality Disorders. 2011;25:305–320. doi: 10.1521/pedi.2011.25.3.305. [DOI] [PubMed] [Google Scholar]
- Horowitz LM. Split identity and instability: Borderline personality disorder and related conditions. In: Horowitz LM, editor. Interpersonal foundations of psychopathology. Washington, DC: American Psychological Association; 2004. pp. 205–220. [Google Scholar]
- Horowitz LM, Rosenberg SE, Baer BA, Ureno G, Villasenor VS. Inventory of Interpersonal Problems: Psychometric properties and clinical applications. Journal of Consulting and Clinical Psychology. 1988;56:885–892. doi: 10.1037//0022-006x.56.6.885. [DOI] [PubMed] [Google Scholar]
- Jahng S, Trull TJ, Wood PK, Tragesser SL, Tomko R, Grant JD, Sher KJ. Distinguishing general and specific personality disorder features and implications for substance dependence comorbidity. Journal of Abnormal Psychology. 2011;120:656–669. doi: 10.1037/a0023539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall Tim, Pilling Stephen, Tyrer Peter, Duggan Conor, Burbeck Rachel, Meader Nicholas, Taylor Clare. Borderline and antisocial personality disorders: summary of NICE guidance. BMJ. 2009:338. doi: 10.1136/bmj.b93. [DOI] [PubMed] [Google Scholar]
- Kenny DA. Correlation and causality. New York: Wiley; 1979. [Google Scholar]
- Kenny DA, Kashy DA. Analysis of the multitrait-multimethod matrix by confirmatory factor analysis. Psychological Bulletin. 1992;112:165–172. [Google Scholar]
- Kernberg OF. Severe personality disorders: Psychotherapeutic strategies. New Haven, CT: Yale University Press; 1984. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York: Guilford Press; 1998. [Google Scholar]
- Kobak RR. The Attachment Interview Q-set. Newark, DE: University of Delaware; 1989. Unpublished manuscript. [Google Scholar]
- Kraemer HC, Measelle JR, Ablow JC, Essex MJ, Boyce T, Kupfer DJ. A new approach to integrating data from multiple informants in psychiatric assessment and research: Mixing and matching contexts and perspectives. American Journal of Psychiatry. 2003;160:1566–1577. doi: 10.1176/appi.ajp.160.9.1566. [DOI] [PubMed] [Google Scholar]
- Levy KN. The implications of attachment theory and research for understanding borderline personality disorder. Development and Psychopathology. 2005;17:959–986. doi: 10.1017/s0954579405050455. [DOI] [PubMed] [Google Scholar]
- Lieb K, Zanarini MC, Schmahl C, Linehan MM, Bohus M. Borderline personality disorder. Lancet. 2004;364(9432):453–461. doi: 10.1016/S0140-6736(04)16770-6. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- Livesley WJ. A framework for integrating dimensional and categorical classifications of personality disorder. Journal of Personality Disorders. 2007;21(2):199–224. doi: 10.1521/pedi.2007.21.2.199. [DOI] [PubMed] [Google Scholar]
- Livesley WJ. An empirically-based classification of personality disorder. Journal of Personality Disorders. 2011;25:397–420. doi: 10.1521/pedi.2011.25.3.397. [DOI] [PubMed] [Google Scholar]
- Livesley WJ. Suggestions for a framework for an empirically based classification of personality disorder. Canadian Journal of Psychiatry. 1998;43:137–147. doi: 10.1177/070674379804300202. [DOI] [PubMed] [Google Scholar]
- Livesley WJ, Jang KL. Toward an empirically based classification of personality disorder. Journal of Personality Disorders. 2000;14:137–151. doi: 10.1521/pedi.2000.14.2.137. [DOI] [PubMed] [Google Scholar]
- Marsh HW. Confirmatory factor analyses of multitrait-multimethod data: Many problems and a few solutions. Applied Psychological Measurement. 1989;13:335–361. [Google Scholar]
- McGlashan TH, Grilo CM, Sanislow E, Ralevski LC, Morey LC, Gunderson JG, et al. Two-year prevalence and stability of individual DSM-IV criteria for schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders: Toward a hybrid model of axis II disorders. American Journal of Psychiatry. 2005;162:883–889. doi: 10.1176/appi.ajp.162.5.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer B, Pilkonis PA. An attachment model of personality disorders. In: Lenzenweger MF, Clarkin JF, editors. Major theories of personality disorder. 2. New York: Guilford Press; 2005. pp. 231–281. [Google Scholar]
- Meyer B, Ajchenbrenner M, Bowles DP. Sensory sensitivity, attachment experiences, and rejection responses among adults with borderline and avoidant features. Journal of Personality Disorders. 2005;19:641–658. doi: 10.1521/pedi.2005.19.6.641. [DOI] [PubMed] [Google Scholar]
- Miller JD, Bagby RM, Pilkonis PA, Reynolds SK, Lynam DR. A simplified technique for scoring DSM-IV personality disorders with the five-factor model. Assessment. 2005;12:404–415. doi: 10.1177/1073191105280987. [DOI] [PubMed] [Google Scholar]
- Morey LC. Personality Assessment Inventory: Professional manual. Tampa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- Morey LC, Berghuis H, Bender DS, Verheul R, Krueger RF, Skodol AE. Toward a model for assessing level of personality functioning in DSM-5, part II: Empirical articulation of a core dimension of personality pathology. Journal of Personality Assessment. 2011;93:347–353. doi: 10.1080/00223891.2011.577853. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. MPLUS user’s guide. 6. Los Angeles, CA: Muthén & Muthén; 2010. [Google Scholar]
- Nisbett RE, Wilson TD. The halo effect: Evidence for unconscious alteration of judgments. Journal of Personality and Social Psychology. 1977;35:250–256. [Google Scholar]
- Oltmanns TF, Turkheimer E, Strauss ME. Peer assessment of personality traits and pathology in female college students. Assessment. 1998;5:53–65. doi: 10.1177/107319119800500108. [DOI] [PubMed] [Google Scholar]
- Pfohl B, Blum N, Zimmerman M. Structured interview for DSM-IV personality. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- Pilkonis PA. Personality prototypes among depressives: Themes of dependency and autonomy. Journal of Personality Disorders. 1988;2:144–152. [Google Scholar]
- Pilkonis PA, Heape CL, Proietti JM, Clark SW. The reliability and validity of two structured diagnostic interviews for personality disorders. Archives of General Psychiatry. 1995;52:1025–1033. doi: 10.1001/archpsyc.1995.03950240043009. [DOI] [PubMed] [Google Scholar]
- Pincus AL, Wiggins JS. Interpersonal problems and conceptions of personality disorders. Journal of Personality Disorders. 1990:342–352. [Google Scholar]
- Reynolds S, Yaggi K, Morse JQ, Stepp SD, Pilkonis PA. Emotional Experiencing and Regulation Interview (EERI): Guidelines for Administration and Coding. Pittsburgh, PA: University of Pittsburgh; 2006. Unpublished manual. [Google Scholar]
- Rosenstein DS, Horowitz HA. Adolescent attachment and psychopathology. Journal of Consulting and Clinical Psychology. 1996;64:244–253. doi: 10.1037//0022-006x.64.2.244. [DOI] [PubMed] [Google Scholar]
- Rothbart MK, Ahadi SA, Evans DE. Temperament and personality: Origins and outcomes. Journal of Personality and Social Psychology. 2000;78:122–135. doi: 10.1037//0022-3514.78.1.122. [DOI] [PubMed] [Google Scholar]
- Russell JJ, Moskowitz DS, Zuroff DC, Sookman D, Paris J. Stability and variability of affective experience and interpersonal behavior in borderline personality disorder. Journal of Abnormal Psychology. 2007;116(3):578–588. doi: 10.1037/0021-843X.116.3.578. [DOI] [PubMed] [Google Scholar]
- Samuel DB, Widiger TA. A meta-analytic review of the relationships between the five-factor model and DSM-IV-TR personality disorders: A facet level analysis. Clinical Psychology Review. 2008;28:1326–1342. doi: 10.1016/j.cpr.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby EA, Ward AC, Joiner TE., Jr Dysregulated eating behaviors in borderline personality disorder: Are rejection sensitivity and emotion dysregulation linking mechanisms? International Journal of Eating Disorders. 2010;43:667–670. doi: 10.1002/eat.20761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaver PR, Mikulincer M. Adult attachment strategies and the regulation of emotion. In: Gross JJ, editor. Handbook of emotion regulation. New York: Guilford Press; 2007. pp. 446–465. [Google Scholar]
- Shaver PR, Belsky J, Brennan KA. The Adult Attachment Interview and self reports of romantic attachment: Associations across domains and methods. Personal Relationships. 2000;7:25–43. [Google Scholar]
- Skodol AE, Bender DS, Morey LC, Clark LA, Oldham JM, Alarcon RD, Siever LJ. Personality disorder types proposed for DSM-5. Journal of Personality Disorders. 2011;25:136–169. doi: 10.1521/pedi.2011.25.2.136. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Gunderson JG, McGlashan TH, Dyck IR, Stout RL, Bender DS, Oldham JM. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. American Journal of Psychiatry. 2002;159:276–283. doi: 10.1176/appi.ajp.159.2.276. [DOI] [PubMed] [Google Scholar]
- Srivastava S, Guglielmo S, Beer JS. Perceiving others’ personalities: Examining the dimensionality, assumed similarity to the self, and stability of perceiver effects. Journal of Personality and Social Psychology. 2010;98:520–534. doi: 10.1037/a0017057. [DOI] [PubMed] [Google Scholar]
- Stepp SD, Hallquist MN, Morse JQ, Pilkonis PA. Multimethod investigation of interpersonal functioning in borderline personality disorder. Personality Disorders: Theory, Research, and Treatment. 2011;2:175–192. doi: 10.1037/a0020572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepp SD, Morse JQ, Yaggi KE, Reynolds SK, Reed I, Pilkonis PA. The role of attachment styles and interpersonal problems in suicide-related behaviors. Suicide and Life-Threatening Behavior. 2008;38:592–607. doi: 10.1521/suli.2008.38.5.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiglmayr CE, Grathwol T, Linehan MM, Ihorst G, Fahrenberg J, Bohus M. Aversive tension in patients with borderline personality disorder: A computer-based controlled field study. Acta Psychiatrica Scandinavica. 2005;111:372–379. doi: 10.1111/j.1600-0447.2004.00466.x. [DOI] [PubMed] [Google Scholar]
- Thomas C, Turkheimer E, Oltmanns TF. Factorial structure of pathological personality as evaluated by peers. Journal of Abnormal Psychology. 2003;112:81–91. [PMC free article] [PubMed] [Google Scholar]
- Tidwell MO, Reis HT, Shaver PR. Attachment, attractiveness, and social interaction: A diary study. Journal of Personality and Social Psychology. 1996;71:729–745. doi: 10.1037//0022-3514.71.4.729. [DOI] [PubMed] [Google Scholar]
- Vazire S. Informant reports: A cheap, fast, and easy method for personality assessment. Journal of Research in Personality. 2006;40:472–481. [Google Scholar]
- Wolf EJ, Miller MW, Brown TA. The structure of personality disorders in individuals with posttraumatic stress disorder. Personality Disorders: Theory, Research, and Treatment. 2011;2:261–278. doi: 10.1037/a0023168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Thomas KM, Hopwood CJ, Markon KE, Pincus AL, Krueger RF. The hierarchical structure of DSM-5 pathological personality traits. Journal of Abnormal Psychology. doi: 10.1037/a0027669. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Vujanovic AA, Parachini EA, Boulanger JL, Frankenburg FR, Hennen J. A screening measure for BPD: The Mclean Screening Instrument for Borderline Personality Disorder (MSI-BPD) Journal of Personality Disorders. 2003;17:568–573. doi: 10.1521/pedi.17.6.568.25355. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Rothschild L, Chelminski I. The prevalence of DSM-IV personality disorders in psychiatric outpatients. American Journal of Psychiatry. 2005;162:1911–1918. doi: 10.1176/appi.ajp.162.10.1911. [DOI] [PubMed] [Google Scholar]