Abstract
Introduction
We aimed to determine whether a unique, ultra high-field 7 Tesla (T) MRI scanner could detect occult cartilage and meniscal injuries in asymptomatic female dancers.
Materials and Methods
This study had institutional review board approval. We recruited eight pre-professional female dancers and nine non-athletic, female controls. We scanned the dominant knee on a 7T MRI scanner using a 3D-FLASH sequence and a proton density, fast spin-echo sequence to evaluate cartilage and menisci, respectively. Two radiologists scored cartilage (International Cartilage Repair Society classification) and meniscal (Stoller classification) lesions. We applied two-tailed z- and t-tests to determine statistical significance.
Results
There were no cartilage lesions in dancers or controls. For the medial meniscus, the dancers compared to controls demonstrated higher mean MRI score (2.38±0.61 vs. 1.0±0.97, p<0.0001) and higher frequency of mean grade 2 lesions (88% vs. 11%, p<0.01). For the lateral meniscus, there was no difference in score (0.5±0.81 vs. 0.5±0.78, p=0.78) in dancers compared to controls.
Discussion
Asymptomatic dancers demonstrate occult medial meniscal lesions. Because this has been described in early osteoarthritis, close surveillance of dancers’ knee symptoms and function with appropriate activity modification may help maintain their long-term knee health.
Keywords: Dancers, Knee, Meniscus, MRI, 7 Tesla
INTRODUCTION
Dancers are unique athletes who are devoted to an artistic practice with intensive physical demands. The complex movements specified by a dancer’s choreographer or teacher require extreme ranges of motion, excellent static and dynamic strength, and superb balance and proprioception. These physical demands are amplified by an intensive schedule that includes frequent dance classes, rehearsals, and performances; limited breaks from dance activities (“off-season”); and restricted medical benefits and support as compared with professional athletes. Dancers incur musculoskeletal injuries at a relatively high rate, which is comparable to that seen in other athletes.
In their recent survey of dance injuries, Shah et al. studied 184 professional modern dancers while providing a review of the current literature on injury in dance.(Shah et al. 2012) Shah et al. found an annual incidence of injury of 81%, which is similar to what has been found in other forms of dance (75–85% for ballet) and in other sports (81% for football).(Meeuwisse & Fowler 1988) Injuries in dancers have been found to more commonly occur in the lower extremity, including the knee. Because of high competition for professional positions, dancers may ignore their injuries and only bring them to medical attention when the injuries have reached a more advanced stage. These injuries can result in lost performance time and financial strain on both the dancer and the dance company (Garrick & Lewis 2001; Ojofeitimi & Bronner 2011). Despite what is known about the incidence of injuries in dancers, little is known about the mechanism or time course of progression of these injuries.
Magnetic resonance imaging (MRI) is considered to be the best test to evaluate injuries to soft tissues of the musculoskeletal system.(Resnick et al. 2006) A number of studies have utilized MRI to systematically examine the knee joints of asymptomatic athletes including basketball, football, and soccer players, as well as swimmers and gymnasts,(Jerosch et al. 1994; Ludman et al. 1999; Major & Helms 2002; Soder et al. 2012; Soder et al. 2011; Walczak et al. 2008) but no such investigations have yet been reported in dancers. These studies have utilized a variety of MRI scanners, ranging in field strength from 0.35 to 3 Tesla (T). Since the arrival of MRI scanners in the 1980s, there has been steady progress in both MRI software (such as pulse sequences) and hardware (such as coils) that has allowed improved visualization of joint structures including cartilage, menisci, ligaments, and tendons. One of the most important hardware advancements over the last decade has been the arrival of high field (3 T) and ultra high field (≥7 T) MRI scanners.(Robitaille & Berliner 2006) The advantage of scanning at higher field strength is the greater signal-to-noise ratio, which can permit imaging with higher spatial resolution and/or faster scanning speed.(Gold et al. 2004; Krug et al. 2009; Regatte & Schweitzer 2007) Over the last few years, there have been an increasing number of publications related to ultra high field 7 T MRI of the knee, with the potential for early disease detection or improved monitoring of disease progression becoming more evident.(Banerjee et al. 2008; Chang et al. 2012; Chang et al. 2008; Krug et al. 2007; Trattnig et al. 2010)
The goal of this study was to use ultra high field, 7 T MRI to assess the status of knee cartilage and menisci in a group of pre-professional, female contemporary dancers and a group of nonathletic, female controls. We were interested in examining whether early morphological lesions or changes could be detected in the knees of dancers at a relatively early stage of their career. We hypothesized that dancers would exhibit a higher degree of occult cartilage and meniscal injuries, compared with controls, and that we would be able to detect these changes with 7 T MRI.
MATERIALS AND METHODS
Subject Recruitment
This study had institutional review board approval and we obtained written informed consent from all subjects. The dancers (n=8) were advanced, pre-professional modern (contemporary) dance students (and one subject was their teacher) at a school that specializes in modern dance. The mean age, height, and weight of dancers were 25.7±5.8 years, 1.6±0.1 meters, and 57.1±4.6 kg, respectively. The mean years of dance participation was 15.7±6.1 years; the subjects’ dance participation in prior years included both ballet and modern dance. The dancers participated in dance training activities totaling approximately 20 hours per week at the time of the study. We recruited physically inactive, healthy female controls (n=9) similar in age, height, and weight by placing ads around the university campus. The mean age, height, and weight for the female controls were 32±4.6 years, 1.6±0.0 meters, 55.8±5.9 kg, respectively. The controls did not participate in sports regularly and described their only significant physical activity as walking to and from class/work.
MRI Scanning
The dominant lower extremity of each subject (those who were unsure were asked to identify the lower extremity used to kick a ball) was scanned on a 7 T whole-body MRI scanner (Siemens, Erlangen, Germany) using a birdcage-transmit, 28-channel receive array coil (Quality Electrodynamics, Mayfield Village, Ohio). We employed a high-resolution, 3-dimensional fast low-angle shot sequence to image cartilage (TR/TE = 26 ms/5.06 ms, matrix = 512 × 512, FOV = 12 cm, in-plane resolution = 0.234 mm × 0.234 mm, slice thickness = 1 mm, 80 sagittal slices, acquisition time = 7 minutes 9 seconds) (Chang et al. 2012) and a standard proton-density weighted sequence to evaluate the meniscus (TR/TE = 3270/26, matrix = 448 × 448, FOV = 16 cm, in-plane resolution = 0.357 mm × 0.357 mm, slice thickness = 3 mm, 25 sagittal images, acquisition time = 4 minutes 23 seconds).(Peterfy et al. 2004)
Scoring of Injury to Cartilage and Menisci
All images were de-identified. Two musculoskeletal radiologists scored each subject’s images for cartilage injury using the International Cartilage Repair Society grading system (0 = normal, 1 = superficial fissures or cracks, 2 = lesions extending down to < 50% of cartilage depth, 3 = lesions extending down to > 50% of cartilage depth but not through subchondral bone, 4 = lesions extending through subchondral bone).(Brittberg & Winalski 2003) The musculoskeletal radiologists also scored each subject’s images for meniscal injury using the Stoller MRI grading system (0 = normal, 1 = intrasubstance globular signal not extending to the articular surface, 2 = intrasubstance linear signal not extending to the articular surface, 3 = abnormal signal that extends to the articular surface).(Stoller et al. 1987) An arithmetic mean of the two radiologists’ scores was calculated. There was good agreement between radiologists’ scores, as determined by a kappa value of 0.7.
Statistics
We used two-tailed z-tests and t-tests (SPSS 18.0, Somers, New York) to compare the proportions and scores for cartilage and meniscus injuries between groups (p < 0.05 for statistical significance).
RESULTS
There were no cartilage lesions in the dancer group (mean score = 0) or the control group (mean score = 0) in either the medial or lateral compartments. Representative images of normal articular cartilage from a control are shown in Figure 1.
Figure 1.
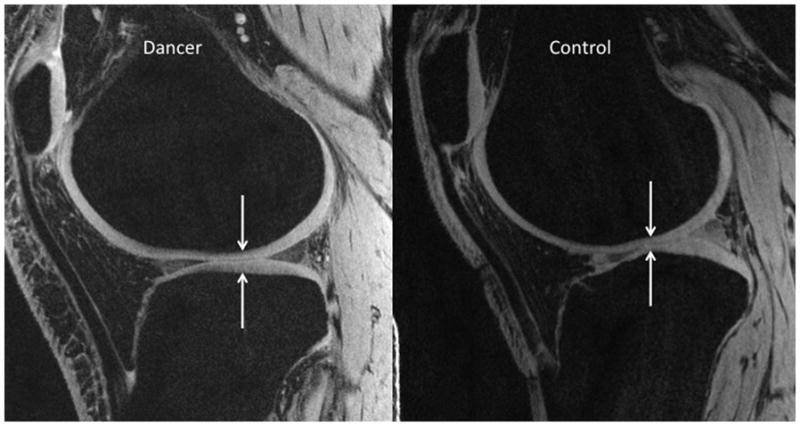
Sagittal 7T MR images from a dancer (left panel) and a control (right panel) demonstrating normal articular cartilage along both the femoral and tibial articular surfaces (TR/TE = 26 ms/5.06 ms, 0.234 mm × 0.234 mm × 1 mm).
For the medial meniscus, the dancers demonstrated a higher mean MRI score (2.4±0.6) compared to the control group (1.0±1.0, p<0.0001). The medial meniscal findings in the dancers were all identified within the posterior horn. There was a greater proportion of medial meniscal lesions of mean grade 2 or higher in the dancer group (7/8 subjects, 88%) compared to the control group (1/9 subjects, 11%, p<0.01).
There was no significant difference in the mean lateral meniscus MRI score in the dancer group (0.5±0.8) compared to the control group (0.5±0.8, p=0.78). Figure 2 shows an example of a grade 2 MRI signal within the posterior horn of the medial meniscus of a dancer.
Figure 2.
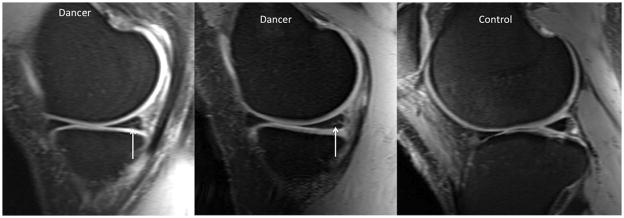
Sagittal 7T MR image (TR/TE = 3270 ms/26 ms, 0.357 mm × 0.357 mm × 3 mm) demonstrating Stoller grade 3 (left panel) and grade 2 (middle panel) signal within the posterior horn of the medal meniscus in asymptomatic dancers. The meniscus from a healthy control is shown for comparison (right panel).
DISCUSSION
In this study, we used an ultra high field, 7 T MRI scanner to evaluate and compare knee cartilage and menisci in a group of contemporary female dancers and a group of nonathletic, female controls. Interestingly, even with ultra high field MRI there were no observed injuries to the articular cartilage in the dancers. This is in contrast to what has been described for other athletes. Walczak et al. in 2008 described a study of the knees of 14 male NBA basketball players (mean age 26.3), where he found a high frequency (approximately 50%) of articular cartilage abnormalities.(Walczak, McCulloch 2008) Walczak’s findings were consistent with previous studies of basketball players, by Major et al.(Major & Helms 2002) and Kaplan et al.(Kaplan et al. 2005), who showed a frequency of 41.5% and 45% of articular cartilage abnormalities, respectively. Ludman et al.’s 1999 study of gymnasts only focused on meniscal findings rather than articular cartilage(Ludman, Hough 1999), and Soder et al.’s 2011 and 2012 studies of soccer players(Soder, Simoes 2011) and swimmers(Soder, Mizerkowski 2012), respectively, involves only adolescents and is limited by the 0.35 open MRI scanner that was used. Whether the lack of articular cartilage abnormalities seen in our dancers, despite the use of higher resolution imaging, is due to a protective effect of dance training, the demands of dance vs. other sports, or to the characteristics of the specific subjects involved in our study, including gender, is not known.
With regard to meniscal abnormalities, the 7 T MRI detected a significantly higher proportion and severity of meniscal injury in the dancers as compared with controls. These findings are consistent with previous reports of a correlation between athletic activity and meniscal abnormalities seen on MRI, including that of Jerosch et al.(Jerosch, Hoffstetter 1994) They likely reflect the high physical demands endured by dancers who are training for professional positions. The presence of meniscal degeneration or tears in the asymptomatic dancers is not necessarily surprising. Englund et al. found that 61% of middle-aged and elderly adults with meniscal tears had no pain, aching or stiffness in the previous month.(Englund et al. 2008) However, the same authors also note that meniscal damage is frequently seen in knee osteoarthritis and meniscal degeneration is often considered a sign of early-stage knee osteoarthritis.(Englund et al. 2009; Englund et al. 2009) Therefore, the results of this study raise the question of whether the dancers are at a higher risk for developing osteoarthritis as compared to the control group. In a nested, case-control study of middle-aged and elderly adults, knees with meniscal lesions but without cartilage lesions were at greater risk for developing radiographic osteoarthritis compared to knees with intact menisci.(Englund et al. 2009) Because the meniscus functions for shock absorption and load transmission, damage to meniscal tissue may lead to increased mechanical stress on underlying cartilage, and subsequent cartilage degeneration (Englund, Guermazi 2009).
In this study, all medial meniscal findings in the dancers were identified within the posterior horn. This is different than what was found in studies of other athletes. In Jerosch et al.’s study of the correlation between athletic activity and meniscal findings on MRI, it was the lateral meniscus, and to the greatest extent its anterior horn, where the highest correlation was seen; no correlation was observed at the posterior horn of the medial meniscus.(Jerosch, Hoffstetter 1994) In Ludman et al.’s study, meniscal findings were preferentially seen in the lateral meniscus of gymnasts as compared with controls; Ludman’s study was performed with a younger, predominantly male population of athletes (10 male, 4 female; average age of 20 years) who had a lower overall frequency of meniscal abnormalities.(Ludman, Hough 1999) The posterior horn of the menisci, a common site of damage, are believed to transmit greater loads than the anterior horns, with the degree of load transmission also depending on the amount of knee flexion.(Resnick, Kang 2006) Knowledge of the specific location of meniscal injury in different sports, including dance, could potentially help influence sport-specific training to be more mindful of the loading of the knee in each sport. In addition, knowledge of dancers’ knee alignment (for example, determination of valgus or varus positioning on weight-bearing radiographs) may also influence physical activity recommendations as knee malalignment is a known risk factor for the later development of osteoarthritis (Sharma et al. 2001).
This study was facilitated by the use of a 7 T MRI scanner. As described previously, the advantage of imaging at higher field strength is the increased signal-to-noise ratio available, which permits imaging with higher spatial resolution and/or faster scanning speeds compared to scanning at lower field strength.(Gold, Suh 2004; Krug, Stehling 2009; Regatte & Schweitzer 2007) Though we did not detect any cartilage injuries in the dancers or the control group, the spatial resolution of the cartilage images in this study (0.234 mm × 0.234 mm × 1 mm) is higher than the spatial resolutions listed for previous cartilage imaging studies performed at 1.5 T and 3 T.(Eckstein et al. 2006) Given that the sensitivity and specificity of 1.5 T MRI for the detection of cartilage defects in the knee is as high as 93% and 94,(Disler et al. 1995) respectively, we believe that it is unlikely that we missed any cartilage lesions. In the future, the inclusion of biochemical cartilage imaging techniques (sodium MRI, T2 mapping, chemical exchange saturation transfer, delayed gadolinium enhance MRI of contrast) may allow further insight into early cartilage or knee joint changes in modern dancers and other types of athletes.
This study has limitations. First, the overall number of subjects is low, which was due to budget limitations and time constraints. Nevertheless, the findings were statistically significant. Second, as this is a cross-sectional study, longitudinal follow-up is needed in order to determine whether the dancers will actually develop osteoarthritis or if their joint status will remain stable. Third, the 7 T MRI scanner is not widely available, with only a handful of whole-body installations in the United States. However, this was the scenario when manufacturers introduced 3 T MRI scanners approximately ten years ago, and 3 T MRI scanners are now becoming the standard-of-care in radiology departments. Fourth, we do not have surgical confirmation of the MRI findings. However, arthroscopy would not have been justified in this population. In addition, the criteria used in this study to evaluate the MRI findings have been in existence for two decades and have already been validated in pathologic and arthroscopic studies.(Disler, McCauley 1995; Stoller, Martin 1987) Finally, the age of the controls in this study was significantly different than that of the dancers. Because meniscal injury would be expected to increase with age, and since the dancers in our study were younger but had more injury, this seems only to strengthen our results.
In conclusion, we have used an ultra high-field 7 T MRI scanner to evaluate and compare the status of knee cartilage and menisci in pre-professional female contemporary dancers and matched nonathletic female controls. The dancers demonstrated no cartilage injuries, but did demonstrate a higher frequency and severity of meniscal abnormalities compared to the controls, which were clustered at posterior horn of the medial meniscus. Whether the data from this small sample of dancers is reflective of injuries in the larger population of dancers is yet to be determined, but this study suggests that further work is necessary to evaluate early signs of joint disease in dancers. The clinical significance of these abnormalities are not fully understood, but because these type of meniscal findings are commonly seen in early, degenerative osteoarthritis in middle-aged and the elderly adults, we believe that it is important to closely monitor dancers’ knee symptoms and function and institute appropriate activity modification if necessary.
PERSPECTIVE.
The knee is a common site of injury in dancers, but the precise anatomic and temporal characteristics of these injuries remains unknown. Several studies have utilized magnetic resonance imaging (MRI) to examine the knee joints of athletes, but no such investigations have been reported in dancers. We aimed to determine whether an ultra high-field 7 Tesla (T) MRI scanner could detect occult cartilage and meniscal injuries in asymptomatic female dancers. We found that high-resolution 7T MRI detects a higher frequency and severity of medial meniscal lesions in asymptomatic dancers compared to healthy controls. Because such meniscal lesions have been described in early osteoarthritis, close surveillance of dancers knee symptoms and function, with appropriate activity modification, may help maintain dancers’ long-term knee health.
Acknowledgments
This study was funded by the United States National Institutes of Health/National Institutes of Arthritis and Musculoskeletal and Skin Diseases (NIH/NIAMS K-23AR059748). The authors have no competing interests.
References
- Banerjee S, Krug R, Carballido-Gamio J, Kelley DA, Xu D, Vigneron DB, Majumdar S. Rapid in vivo musculoskeletal MR with parallel imaging at 7T. Magn Reson Med. 2008;59:655–660. doi: 10.1002/mrm.21455. [DOI] [PubMed] [Google Scholar]
- Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85-A(Suppl 2):58–69. doi: 10.2106/00004623-200300002-00008. [DOI] [PubMed] [Google Scholar]
- Chang G, Madelin G, Sherman OH, Strauss EJ, Xia D, Recht MP, Jerschow A, Regatte RR. Improved assessment of cartilage repair tissue using fluid-suppressed (2)(3)Na inversion recovery MRI at 7 Tesla: preliminary results. Eur Radiol. 2012;22:1341–1349. doi: 10.1007/s00330-012-2383-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang G, Pakin SK, Schweitzer ME, Saha PK, Regatte RR. Adaptations in trabecular bone microarchitecture in Olympic athletes determined by 7T MRI. J Magn Reson Imaging. 2008;27:1089–1095. doi: 10.1002/jmri.21326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang G, Wiggins GC, Xia D, Lattanzi R, Madelin G, Raya JG, Finnerty M, Fujita H, Recht MP, Regatte RR. Comparison of a 28-channel receive array coil and quadrature volume coil for morphologic imaging and T2 mapping of knee cartilage at 7T. J Magn Reson Imaging. 2012;35:441–448. doi: 10.1002/jmri.23506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Disler DG, McCauley TR, Wirth CR, Fuchs MD. Detection of knee hyaline cartilage defects using fat-suppressed three-dimensional spoiled gradient-echo MR imaging: comparison with standard MR imaging and correlation with arthroscopy. AJR Am J Roentgenol. 1995;165:377–382. doi: 10.2214/ajr.165.2.7618561. [DOI] [PubMed] [Google Scholar]
- Eckstein F, Burstein D, Link TM. Quantitative MRI of cartilage and bone: degenerative changes in osteoarthritis. NMR Biomed. 2006;19:822–854. doi: 10.1002/nbm.1063. [DOI] [PubMed] [Google Scholar]
- Englund M, Guermazi A, Gale D, Hunter DJ, Aliabadi P, Clancy M, Felson DT. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008;359:1108–1115. doi: 10.1056/NEJMoa0800777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Englund M, Guermazi A, Lohmander LS. The meniscus in knee osteoarthritis. Rheum Dis Clin North Am. 2009;35:579–590. doi: 10.1016/j.rdc.2009.08.004. [DOI] [PubMed] [Google Scholar]
- Englund M, Guermazi A, Lohmander SL. The role of the meniscus in knee osteoarthritis: a cause or consequence? Radiol Clin North Am. 2009;47:703–712. doi: 10.1016/j.rcl.2009.03.003. [DOI] [PubMed] [Google Scholar]
- Englund M, Guermazi A, Roemer FW, Aliabadi P, Yang M, Lewis CE, Torner J, Nevitt MC, Sack B, Felson DT. Meniscal tear in knees without surgery and the development of radiographic osteoarthritis among middle-aged and elderly persons: The Multicenter Osteoarthritis Study. Arthritis Rheum. 2009;60:831–839. doi: 10.1002/art.24383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrick JG, Lewis SL. Career hazards for the dancer. Occup Med. 2001;16:609–618. iv. [PubMed] [Google Scholar]
- Gold GE, Suh B, Sawyer-Glover A, Beaulieu C. Musculoskeletal MRI at 3.0 T: initial clinical experience. AJR Am J Roentgenol. 2004;183:1479–1486. doi: 10.2214/ajr.183.5.1831479. [DOI] [PubMed] [Google Scholar]
- Jerosch J, Hoffstetter I, Reer R, Assheuer J. Strain-related long-term changes in the menisci in asymptomatic athletes. Knee Surg Sports Traumatol Arthrosc. 1994;2:8–13. doi: 10.1007/BF01552647. [DOI] [PubMed] [Google Scholar]
- Kaplan LD, Schurhoff MR, Selesnick H, Thorpe M, Uribe JW. Magnetic resonance imaging of the knee in asymptomatic professional basketball players. Arthroscopy. 2005;21:557–561. doi: 10.1016/j.arthro.2005.01.009. [DOI] [PubMed] [Google Scholar]
- Krug R, Carballido-Gamio J, Banerjee S, Stahl R, Carvajal L, Xu D, Vigneron D, Kelley DA, Link TM, Majumdar S. In vivo bone and cartilage MRI using fully-balanced steady-state free-precession at 7 tesla. Magn Reson Med. 2007;58:1294–1298. doi: 10.1002/mrm.21429. [DOI] [PubMed] [Google Scholar]
- Krug R, Stehling C, Kelley DA, Majumdar S, Link TM. Imaging of the musculoskeletal system in vivo using ultra-high field magnetic resonance at 7 T. Invest Radiol. 2009;44:613–618. doi: 10.1097/RLI.0b013e3181b4c055. [DOI] [PubMed] [Google Scholar]
- Ludman CN, Hough DO, Cooper TG, Gottschalk A. Silent meniscal abnormalities in athletes: magnetic resonance imaging of asymptomatic competitive gymnasts. Br J Sports Med. 1999;33:414–416. doi: 10.1136/bjsm.33.6.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Major NM, Helms CA. MR imaging of the knee: findings in asymptomatic collegiate basketball players. AJR Am J Roentgenol. 2002;179:641–644. doi: 10.2214/ajr.179.3.1790641. [DOI] [PubMed] [Google Scholar]
- Meeuwisse WH, Fowler PJ. Frequency and predictability of sports injuries in intercollegiate athletes. Can J Sport Sci. 1988;13:35–42. [PubMed] [Google Scholar]
- Ojofeitimi S, Bronner S. Injuries in a modern dance company effect of comprehensive management on injury incidence and cost. J Dance Med Sci. 2011;15:116–122. [PubMed] [Google Scholar]
- Peterfy CG, Guermazi A, Zaim S, Tirman PF, Miaux Y, White D, Kothari M, Lu Y, Fye K, Zhao S, Genant HK. Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage. 2004;12:177–190. doi: 10.1016/j.joca.2003.11.003. [DOI] [PubMed] [Google Scholar]
- Regatte RR, Schweitzer ME. Ultra-high-field MRI of the musculoskeletal system at 7.0T. JMagn Reson Imaging. 2007;25:262–269. doi: 10.1002/jmri.20814. [DOI] [PubMed] [Google Scholar]
- Resnick D, Kang HS, Pretterklieber ML. Internal derangements of joints. 2. Vol. 2. Philadelphia: Saunders/Elsevier; 2006. p. xvi. 2284, liv. [Google Scholar]
- Robitaille P-M, Berliner LJ. Ultra high-field magnetic resonance imaging. New York, NY: Springer; 2006. p. xxiii.p. 475. [Google Scholar]
- Shah S, Weiss DS, Burchette RJ. Injuries in professional modern dancers: incidence, risk factors, and management. J Dance Med Sci. 2012;16:17–25. [PubMed] [Google Scholar]
- Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- Soder RB, Mizerkowski MD, Petkowicz R, Baldisserotto M. MRI of the knee in asymptomatic adolescent swimmers: a controlled study. Br J Sports Med. 2012;46:268–272. doi: 10.1136/bjsm.2010.083345. [DOI] [PubMed] [Google Scholar]
- Soder RB, Simoes JD, Soder JB, Baldisserotto M. MRI of the knee joint in asymptomatic adolescent soccer players: a controlled study. AJR Am J Roentgenol. 2011;196:W61–65. doi: 10.2214/AJR.10.4928. [DOI] [PubMed] [Google Scholar]
- Stoller DW, Martin C, Crues JV, 3rd, Kaplan L, Mink JH. Meniscal tears: pathologic correlation with MR imaging. Radiology. 1987;163:731–735. doi: 10.1148/radiology.163.3.3575724. [DOI] [PubMed] [Google Scholar]
- Trattnig S, Welsch GH, Juras V, Szomolanyi P, Mayerhoefer ME, Stelzeneder D, Mamisch TC, Bieri O, Scheffler K, Zbyn S. 23Na MR imaging at 7 T after knee matrix-associated autologous chondrocyte transplantation preliminary results. Radiology. 2010;257:175–184. doi: 10.1148/radiol.10100279. [DOI] [PubMed] [Google Scholar]
- Walczak BE, McCulloch PC, Kang RW, Zelazny A, Tedeschi F, Cole BJ. Abnormal findings on knee magnetic resonance imaging in asymptomatic NBA players. J Knee Surg. 2008;21:27–33. doi: 10.1055/s-0030-1247788. [DOI] [PubMed] [Google Scholar]


