Abstract
Objective
The health status and life experiences of older diabetes patients may be highly heterogeneous, thus making their perspectives particularly relevant for developing individualized self-management plans for this population. Our earlier research showed older diabetes patients’ healthcare goals and self-management behaviors are frequently shaped through social comparisons with peers/family members. The present paper explores this role of social comparison in their self-management practices and develops a conceptual model depicting the process.
Methods
Data were collected using open-ended, semi-structured interviews to elicit 28 older, type 2 diabetes patients’ healthcare goals and self-management practices. Qualitative techniques were used to extract salient themes.
Results
Social comparison plays a salient role in routinizing older patients’ self-management practices. Almost all patients assess their self-management by making “downward” comparisons with individuals doing worse than them; “upward” comparisons are rarely invoked. Occasionally patients’ social comparisons lead them to adopt “normalizing” behaviors resulting in deviations from medically recommended self-care.
Conclusion
The findings formed the basis for developing a conceptual model delineating the role of social comparison in self-management that can be beneficial for providers in tailoring educational interventions for self-management.
Practice implications
Fostering these comparisons can help providers enhance communication on initiating and sustaining self-management practices.
Keywords: Diabetes mellitus, Self-management, Social comparison
1. Introduction
Quote A: “……… my diabetes is under such excellent control because I know my friends; they eat such horrible things…” (Interview 16)
Quote B: “…. my aunt never drank,… never smoked, … never kept late hours…… ate well….and it’s paying off for her….she’s in excellent health for her age….and I mostly want to be independent (like her)….” (Interview 14)
The above quotes illustrate the ways in which patients invoke social comparison processes in the self-management of type 2 diabetes. In the first, the patient attributes her excellent diabetes control to her better eating habits compared to those of her friends. In contrast, in the second, the patient compares herself with a family member doing better than her at self-managing—a goal the patient aspires to.
Medical providers know that self-management is a critical factor for achieving and maintaining optimal blood glucose levels [1]. And since more than 95% of diabetes care needs to be performed by the patient [2], educating the patient is paramount for diabetes self-management [3,4]. Over the years diabetes education material has begun to acknowledge priorities, goals, resources, culture and lifestyles of individual patients when developing self-management plans [5-10]. A recent position statement by the American Association of Diabetes Educators (AADE) emphasizes: “The effectiveness of information (given patients) increases when it evolves from and is related to the participants’ experiences, beliefs and priorities” [11]. Since the health status and life experiences of older diabetes patients may be highly heterogeneous, seeking their perspectives is particularly germane for providers in efforts to develop effective self-management plans for them.
Our earlier research explored older diabetes patients’ healthcare goals, motivations shaping their goals, and actual self-care practices [12,13]. The main findings of the study [12] were: (1) older patients express their healthcare goals in a social and functional language, and (2) healthcare goals are shaped by providers as well as by social comparison with peers/family members.
Social comparison is defined as behavior through which individuals assess themselves, and is generally invoked when “reality” cannot be measured by conventional physical devices, and thus needs to be socially defined [14]. Two underlying conditions are: (1) when “objective” means are not available, individuals evaluate their opinions and abilities through comparisons with those of others [15,16] and (2) they are more likely to compare their attitudes with others similar on socio-demographic attributes rather than with those widely discrepant from themselves [17]. Social comparison has been shown to have a significant role in chronic pain and chronic diseases [18], and in Latino patients with diabetes [19]. However, its role in self-management in older diabetes patients has yet to be explored.
The specific goals of this paper are to examine: (1) how patients use social comparisons with peers/family members to construct their healthcare goals and self-management routines, (2) what functions are served by these comparisons and (3) develop a conceptual model to delineate how social comparison influences older diabetes patients’ self-management.
2. Methods
2.1. Sample and design
The present study is a secondary data analysis [20] of the sample detailed in a prior publication [12] and only a brief summary is delineated here. The sample of 28 older patients with diabetes was drawn from the general internal medicine, geriatrics and endocrinology clinics of The University of Chicago. IRB approval was obtained before patient recruitment.
This is an exploratory study using in-depth, one-on-one, semi-structured interviews with older type 2 diabetes patients (65 and over). A lack of research on older patients’ perceptions of, and language in which they report their healthcare goals, and factors influencing those goals, prompted the use of grounded theory [21] to inductively extract salient themes and analyze them for building situation specific theory. Following guidelines of field research [22], this study neither purports to test hypotheses nor build theory. Rather, it draws exclusively on patients’ self-reports, elicited in one-time interviews, to examine how and why older patients cite peers/family members as being instrumental in developing their self-management practices.
In the original study, interview transcripts were coded by all three investigators in a two-step process. First, each investigator independently reviewed a set of three transcripts, recorded patients’ healthcare goals, factors influencing goals and actual self-care practices, and made a summary of salient themes in the form of a face sheet. Second, discrepancies in themes were discussed, modified by consensus, and subsequently arranged into a Final Summary Sheet for all 28 transcripts. One investigator (RGB) used these Final Summary Sheets and original transcripts to conduct the present secondary data analysis. Two investigators (ESH and MHC) provided critical reviews that led to documenting emergent themes in the present format.
2.2. Operationalization of self-management
The Interview Guide included querying patients on: (1) self-management practices; (2) current diet and exercise practices and (3) experiences and challenges in managing diabetes. Patients’ self-management practices were captured through their capacity to incorporate four major dimensions of self-care: (1) taking medications; (2) monitoring blood glucose; (3) following dietary recommendations and (4) incorporating exercise routines into their daily regimen. Self-management practices were scored as follows:
Patient incorporates ≥3 dimensions of self-care in daily routine scored high.
Patient incorporates ≤2 dimensions of self-care in daily routine scored low.
Salient themes along with illustrative quotes extracted from patients’ transcripts are reported (Interview 10) in the following sections.
3. Results
3.1. Patient characteristics
The average age of patients was 74.3 (range: 66–87 years). They had lived with diabetes for an average of 9.1 years (range: 0.33–40 years). The sample was predominantly African-American (79%) and female (57%). The mean Charlson Comorbidity Index Score was 3.9 [12].
3.2. Stressful life-changing event and healthcare goals
Quote C: “….you go through your life, you retire, and then everything in your body breaks down, and you get hit with something like….you are diabetic….and now your entire life is about to change, and not for the better …. It’s….disheartening…. Cause, right now I don’t have control over my life in terms of what I can eat, where I can go (and when), and it just takes the joy out of life, ….so if you ask me, it’s frightening…it’s absolutely frightening….” (Interview 10)
The above quote captures commonly expressed frustrations of older patients on being diagnosed with type 2 diabetes. For an individual who may have lived a full life, the diagnosis of diabetes in later life is a stressful life-changing event; it forces an awareness of an irreversible condition, and brings about the need to adopt self-management practices that are perceived to be as burdensome as the disease itself.
3.3. Motivations for self-management
Patients often described their motivations for self-management couched in aspects of life goals, and in functional rather than biomedical terms, such as the need to “remain independent,” and “being able to walk.” Further, two major types of self-management behaviors emerged in our sample that were either “external” or “internal” to the patient.
The “external” category is illustrated in Quote D and depicts how the patient invokes the case of her sister and makes a social comparison to guide her diabetes self-care practices.
Quote D: “…. I could go blind…. I could have an amputee…. like my sister had diabetes ….she had (to have) her legs amputated….So I know those things can happen (to me…) (Interview 5).
Patients who compare themselves with similar others to help them navigate healthcare goals and self-care practices are termed “externally motivated” and constitute three-fourths of the sample population (21 of 28). In contrast, the patient in Quote E is illustrative of a small number of patients (7 of 28) who use predominantly internal factors in motivating themselves towards self-management, and are characterized as “internally motivated.”
Quote E: “. I wanna control (to the) maximum, and….slow the process….so, every three/four months I go, I measure …and I try to lower the levels (blood glucose) below the 8… (Interview 12)
Both externally and internally motivated patients expressed affirmative statements in taking prescribed medications. However, on the three remaining self-management routines, externally motivated patients did notably better than internally motivated patients: monitoring blood glucose (79% versus 57%), following dietary recommendations (61% versus 28%), and incorporating exercise regimens into daily routines (61% versus 14%).
3.4. Types and functions of social comparison
Invoking experiences of family members/peers plays a vital role in motivating older patients in self-managing their diabetes. Two types of social comparison emerged in our sample:
Quote F: “…. sometimes I be in my car, and I be thinking “gee…. “where am I going,” and I got to think a minute, …. but you know….some people’s minds is worse than mine…. (comparing herself to her friends with diabetes)… (Interview 7)
Quote F presents a patient comparing herself to her friends doing poorly in comparison to herself. The majority of externally motivated patients – 20 of 21 (95%) – made this type of comparison, termed “downward” social comparison in the literature [23]. In contrast, the patient in Quote B makes a comparison with a family member that continues to do better than the patient; this genre of comparison is rare in our sample (1 of 21) and is defined as an “upward” social comparison [24,25].
Both upward and downward comparisons can be used to improve health behaviors. However, caution should be exercised to avoid taking this stance to an extreme, because it can become a source of stress by making patients feel chronically outperformed, as illustrated:
Quote G: “…and then I eat, and then do my exercise, and I do the exercise, no, I do the exercise before I eat, …. then I have to wait an hour before I can do my exercise, so I do the exercise 30 minutes, I said “30 minutes is all you get” and …. then I eat, and I look up and the day’s gone, particularly if I woke up late… My day is completely gone doing things to keep up…the whole day is diabetes” (Interview 10)
Three examples given below serve to illustrate the functions served by social comparisons. First, patients define and alert themselves to the risks of developing complications of diabetes, by comparing friends’ experiences with theirs, thus serving to promote their awareness and understanding of risks.
Quote H: “…. he had to retire because of diabetes, his vision was going, his legs and feet were going, and I look at him and I could see what could happen, you know, for myself, if I don’t take care of myself….and it’s really difficult…. (Interview 12)
Quote I highlights the second function of how making comparisons can translate into lessons on setting goals (“keep my blood sugars ….”), labeled as adjusting to living with a chronic disease.
Quote I: “….the things that can happen to me….I have a friend in the hospital with a wound in her leg that they can’t close, and they’re finding they want to go back in and do something they did when they were trying to save her foot….I don’t even want to talk about it…. it’s frightening, it’s absolutely frightening….so you see, it’s very important to me that I keep my blood sugars (under control) (Interview 10)
Quote J illustrates how downward comparison can be instrumental for patients in developing a sense of empowerment.
Quote J: “….I don’t let it (diabetes) press on my mind and keep me from doin’ things….. if you got diabetes, whatever complaints you have, don’t think about it…. some people’s mind is worse than mine…and keep on going and you just take care of yourself….….” (Interview 7)
The cross-sectional nature of this study precludes us from knowing if each patient chooses to invoke functions of: (a) understanding risks, (b) adjusting to living with diabetes, and (c) feeling empowered, specifically in the above sequence, or if they occur in random sequence depending on patients. The study sample is a conglomeration of patients who have endured diabetes over a range of 0.33–40 years; however, the analysis is based on a one-time interview of these patients and thus does not lend itself to ascertain specific progression of the three functions described above.
3.5. Self-management and social comparison
Of those making social comparisons (21 of 28), the majority of older diabetes patients made “downward” comparisons (15 of 21) and scored “high” on the self-management scale (12 of 15). In this secondary data analysis based on one-time interviews of a comparatively small sample population, we did not find any relationship between self-management and duration of diabetes.
3.6. Normalizing behavior—comparison with “Normal” others?
Our data show that some older diabetes patients have a limited capacity to perform recommended self-management tasks on an extended basis:
Quote K: “…….If I feel like I want some beer, I get beer…. but when I take my beer, I just don’t take my medications…..I just live my life as best as I possibly can, and if I get up in the morning and I be dragging and ragging around, maybe I just do somethin’ regular….I go in the shopping center and eat lunch….you’ve got to do normal things for yourself and make yourself feel good……Before I got diabetes, I used to be eatin’ sweets, but ever since I had diabetes, you know, don’t nothin’ satisfy me unless I have somethin’ sweet, so I eat what I want …” (Interview 7)
The above example captures a range of related behaviors going against medical advice, but which patients report as essential to their overall well-being (9 of 28). The patient in the above example knows that sweets are not on the recommended diet; nonetheless his indulgence is justified because it “satisfies me.”
4. Discussion and conclusion
Older patients perceive the diagnosis of type 2 diabetes and consequent self-management recommendations as stressful life-changing events (Quote C). Also, they express their healthcare goals in functional terms, and it is conceivable that these might serve as precursors to making comparisons with others. While many factors (including media) may influence a patient’s self-care practices, social comparison with peers/family members and education and counseling by healthcare providers emerged as dominant factors [12]. The discussion section below draws insights from the social comparison literature to interpret these results by: (A) highlighting the nature of the relationship between self-management and social comparison; (B) developing a conceptual model of self-management and social comparison and (C) delineating limitations of the study.
4.1. Discussion
(A) Nature of relationship between self-management and social comparison: The salience of social comparison – in a largely African-American sample – highlighted in this paper is consistent with studies on other medically threatening illnesses (e.g. rheumatoid arthritis, multiple sclerosis and cancer) in which patients – when under stressful conditions – engage in social comparisons for the reception, adoption and maintenance of health behaviors [18,26]. Further, patients motivated by external factors (especially social comparison) did better on self-management than did internally motivated patients. This finding differs from earlier theorizing that intrinsic motivation “(enables patients)… to make and sustain changes in their behavior” [2]. Differences in socio-demographic factors (e.g. education, income, and race) of the samples may contribute to these observed differences. The salience of social comparison for self-management in our predominantly African-American sample is consistent with earlier studies showing the salience of external factors for African-American samples—e.g. social support as a key factor in the desire and ability to exercise [27], and in subjective well-being [28]. Future research should investigate the role of social comparison and self-management in other populations.
In making social comparisons, the higher frequency of “downward” in contrast to “upward” comparison noted in this study is consistent with the literature in eating disorders, chronic pain, infertility, smoking cessation and depression [29], and in cardiac patients [30]. The reason may be that in comparing themselves to others who rank lower, patients afford themselves a sense of subjective well-being [25]. Downward comparisons also serve self-empowering and coping functions[23,31]. And, empowering feelings are efficacious for patients in initiating and sustaining self-management in the long run [32].
The concept of empowerment as being vital for sustaining self-management over the long term is emphasized in diabetes research [33,34] and in clinical practice [35-37] because diabetes occurs in the context of patients’ lives and calls for patients to self-manage [32]. Especially when emanating from downward social comparison, empowerment can improve the quality of life for institutionalized disabled patients. For instance, the Dutch Health Insurer – VGZ – in sponsoring pilgrimages to Lourdes, France for its most disabled clients – “to improve the company’s image by helping people,”[38] – surreptitiously may have helped patients feel empowered. The present authors believe that during the pilgrimage to Lourdes, the forced juxtaposition of similar others, some in a far worse plight, facilitated patients making downward comparisons with others worse off than themselves, thus leading to patients’ acceptance of their disability.
Very few patients made comparisons with people who were doing (or did) better; nonetheless these comparisons can inspire hope and/or provide information on improving oneself [31,32]. Through invoking the example of her aunt, the patient in Quote B implies a similar lifestyle is attainable for her. It is important to note that this patient’s score on self-management was at the highest level (four on self-management scale).
Older diabetes patients also incorporate seemingly contradictory behaviors in their routines alongside invoking social comparisons and empowering themselves. How can these be explained? Despite physicians’ recommended self-management routines, patients show the need to continue with their usual social roles while seeking ways to incorporate recommendations within their life context. Thus, from patients’ perspectives, leading the life of a diabetes patient calls for choosing not only physician recommended behaviors, but also a range of (seemingly contrary) behaviors that are perceived as essential to their overall well-being. In doing so, patients may be comparing themselves to “normal” others (those not bearing the burden of diabetes), thus expanding the definition of self-management to balance their daily lives. Our finding is consistent with patients’ “relapse” behaviors in the diabetes literature [39] and in the chronic illness literature [40,41].
Ironically, we found that patients who scored high on self-management also reported more frequent instances of “normalizing” behavior. It is conceivable that these patients were more forthcoming in articulating both achievements and challenges of self-care behavior. In contrast, patients who may not have established a self-management routine may also not have constructed the positives and negatives of self-care and hence did not express normalizing behaviors.
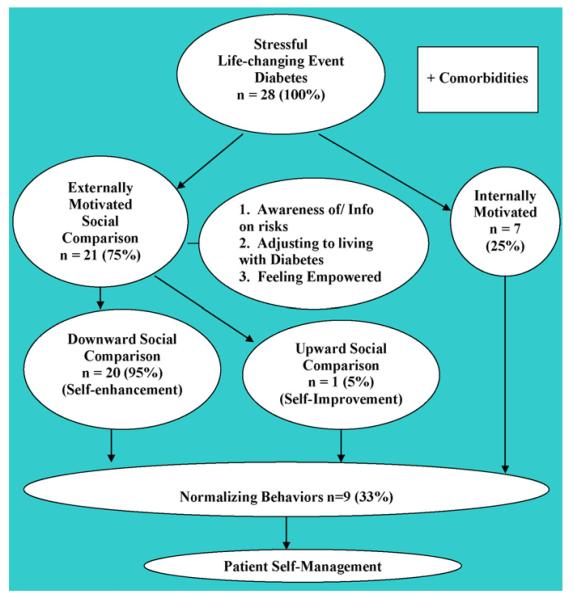
(B) A Conceptual Model of Social Comparison and Self-management in Older Diabetes Patients has been developed on the basis of the above findings and analysis (Fig. 1). While social comparison and the model developed may be applicable for all segments of the patient population they are particularly salient for older patients for several reasons. First, research in elders’ quality of life shows social contacts and health status constitute major components of good quality of life [42]. Therefore, the elderly may have greater desire and time to watch (and reflect on) family members’/friends’ self-care behaviors and their consequences. Second, the onslaught of age-related stressful life events, e.g. serious medical illnesses and dwindling of life-long support networks leave older patients as sole survivors among peers leading them to seek comfort in making comparisons. It is no surprise that the majority of older type 2 diabetes patients in our sample compared themselves vis-à-vis others on self-management behaviors. Social comparison is a significant factor in chronic diseases, and some research has been conducted in older adults [18]; however, there is, to our knowledge, no research highlighting older patients’ reliance on social comparison in diabetes self-management. The present study is one of the first to make this contribution.
Fig. 1.
Social comparison and self-management in older diabetes patients.
The model (Fig. 1) is conceptualized as comprising four domains that patients traverse, either as distinct, or in tandem with one or more domains. The numerical results of the cross-sectional data analyses from the present sample are listed to illustrate the domains and social processes involved in self-management. The first domain delineates patients passing through a stressful life event – being diagnosed with type 2 diabetes – and deciphering providers’ recommended practices (Section 3.2). In the second domain patients motivate themselves to self-manage—through external or internal motivation (Section 3.3). The third domain includes two distinct types of social comparison processes and salient functions invoked—self-enhancement and self-improvement (Section 3. 4). The fourth domain presents patients acting on their desires to live a socially “normal” life – comparing themselves to “normal” others – by adopting “normalizing” behaviors amidst their efforts to self-manage (Section 3.6).
Three cautionary points are noteworthy. First, the emphasis in this paper – social aspects of self-management – should not be construed as a substitute for biomedical recommendations. Second, although the model is conceptualized as four domains, patients do not traverse them in a linear progression—they can be at one or more domains at any given time. And, third, the model is developed from analyses of a cross-sectional sample, and sequential patterns can only be assessed through longitudinal research.
The main advantage of the model is that providers can recognize the four domains that older patients traverse during self-management. They can use the model to identify the domain(s) the patient is at and effectively tailor relevant counseling and educational interventions. Intervention(s) would constitute actively encouraging patients to make comparisons on self-management practices with their friends/family members—“upward” comparisons to encourage emulating role models and “downward” comparisons to empower patients. However, making “downward” comparisons can have a negative side in that they can potentially desensitize patients to risks. Therefore, to avoid building a false sense of security in patients, providers should use discretion on when biomedical goals need to supersede the social aspects of self-management. Behavioral interventions should always complement the biomedical goals by bringing the two to focus on suggesting adaptive comparisons for self-management. Providers should periodically monitor for improvement, and expect occasional lapses of self-management (normalizing behaviors). Since social comparison is a common routine of older diabetes patients, it may be efficacious for providers to reinforce the informal systems of naturally occurring social comparison processes to encourage the adoption of desired actions, or identify ways of persuading patients to select better comparison references [43].
(C) Limitations of the study include: (1) small sample size drawn from community dwelling, predominantly African-American individuals attending an urban academic medical center. Further research needs to be extended to other settings and populations to better understand the influence of social comparison; (2) the role of socio-demographic factors such as race, education and income could not be assessed in this small sample; (3) this research focuses on patients’ perspectives, and the nature of patient–provider relationships or providers’ perspectives are not known; (4) the study used patients’ self-reports that may be clouded by social desirability artifacts [44]; (5) our qualitative study did not start with a priori theory, rather elaborated only on those themes that surfaced as salient to respondents. Other theories of behavior change, e.g. theory of reasoned action [45] and/or stages of change model [46] may be implicated in patients’ self-management practices and (6) results from this study should be interpreted keeping in mind the limitations of cross-sectional research [47].
4.2. Conclusion
Social comparisons are often invoked by older diabetes patients in routinizing self-management. Providers would benefit by exploring the salience of comparisons for patients, and where applicable, foster these comparisons to enhance communication on initiating and sustaining self-management practices.
4.3. Practice implications
Older patients’ self-reports lay grounds for providers to strengthen and reinforce naturally occurring social comparisons, exploit their benefits, and build a foundation for self-management behavior. Providers could use informal social comparison networks to encourage diffusion of self-care information. Opinion leaders identified from patients’ social networks could be used to create persuasive interventions [48]. Educational and/or informational interventions such as group visits could provide a venue for fostering new social comparison networks with similar others. Additionally, group medical visits can be used to better understand patients’ perceived barriers and “normalizing” behavior patterns since they can have important consequences for self-management. Providers can subsequently identify incremental steps in routinizing self-care practices. Providers could encourage “downward” comparisons to foster well-being and empower patients and, “upward” comparisons could uphold a model for goal-setting for self-management.
Acknowledgements
The research reported in this paper was supported by The Section of Geriatrics (RGB), a Hartford Center of Excellence Pilot Grant (ESH), a National Institute on Aging Geriatric Academic Program Award (K12 AG000488 ESH), a National Institute on Aging Career Development Award (K23 AG021963 ESH), a National Institute of Diabetes and Digestive and Kidney Diseases Diabetes Research and Training Center (P60 DK20595—RGB, ESH and MHC) and a Mid-Career Investigator Award in Patient-Oriented Research (MHC) from the National Institute of Diabetes and Digestive and Kidney Diseases (K24 DK071933). The investigators retained full independence in the conduct of this research.
The authors wish to thank investigators in the Diabetes Research and Training Center Prevention and Control Core at the University of Chicago for participating in a fruitful discussion and providing constructive comments on a prior draft.
Footnotes
An earlier version of this research was presented at the 2007 International Conference on Communication in Healthcare, Charleston, South Carolina, USA.
Conflict of interest statement
This is to certify that all three of the above named authors do not have any actual or potential conflict of interest including any financial, personal or other relationships with other people or organizations within three (3) years of beginning the submitted work that could inappropriately influence, or be perceived to influence their work.
References
- [1].Funnell MM, Kruger DF, Spencer M. Self-management support for insulin therapy in type 2 diabetes. Diabetes Educ. 2004;30:274–80. doi: 10.1177/014572170403000220. [DOI] [PubMed] [Google Scholar]
- [2].Funnell MM, Anderson RM. The problem with compliance in diabetes. J Am Med Assoc. 2000;284:1709–11. [PubMed] [Google Scholar]
- [3].Burnet D, Plaut A, Courtney R, Chin MH. A practical model for preventing type 2 diabetes in minority youth. Diabetes Educ. 2002;28:779–95. doi: 10.1177/014572170202800519. [DOI] [PubMed] [Google Scholar]
- [4].Anderson RM. Taking diabetes self-management education to the next level. Diabetes Spectr. 2007;20:202–3. [Google Scholar]
- [5].Fain JA, Nettles A, Funnell MM, Prochownik DC. Diabetes patient education research: an integrative literature review. Diabetes Educ. 1999;25:7–15. doi: 10.1177/014572179902500618. [DOI] [PubMed] [Google Scholar]
- [6].Funnell MM, Anderson RM. Working toward the next generation of diabetes self-management education. Am J Prev Med. 2002;22:3–5. doi: 10.1016/s0749-3797(02)00431-2. [DOI] [PubMed] [Google Scholar]
- [7].Glasgow RE, Funnell MM, Bonomi AE, Davis C, Beckham V, Wagner EH. Self-management aspects of improving chronic issues care break-through series: implementation with diabetes and heart failure teams. Ann Behav Med. 2002;24:80–7. doi: 10.1207/S15324796ABM2402_04. [DOI] [PubMed] [Google Scholar]
- [8].Funnell MM, Anderson RM. Empowerment and self-management of diabetes. Clin Diabetes. 2004;22:123–7. [Google Scholar]
- [9].Fisher L, Glasgow E. A call for more effectively integrating behavioral and social science principles into comprehensive diabetes care. Diabetes Care. 2007;30:2746–9. doi: 10.2337/dc07-1166. [DOI] [PubMed] [Google Scholar]
- [10].Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Maryniuk M, Piette JD, Siminerio LM, Weinger K, Weiss MA. National standards for diabetes selfmanagement education. Diabetes Care. 2007;30:1630–7. doi: 10.2337/dc07-9923. [DOI] [PubMed] [Google Scholar]
- [11].American Association of Diabetes Educators (AADE) AADE position statement: individualization of diabetes self-management education. Diabetes Educ. 2007;33:45–9. doi: 10.1177/0145721706298308. [DOI] [PubMed] [Google Scholar]
- [12].Huang ES, Gorawara-Bhat R, Chin MH. Self-reported goals of older patients with type 2 diabetes. J Am Geriatr Soc. 2005;53:306–11. doi: 10.1111/j.1532-5415.2005.53119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Huang ES, Gorawara-Bhat R, Chin MH. Practical challenges of individualizing diabetes care in older patients. Diabetes Educ. 2004;30:558. doi: 10.1177/014572170403000407. [DOI] [PubMed] [Google Scholar]
- [14].Festinger L. A theory of social comparison processes. Hum Relat. 1954;7:117–40. [Google Scholar]
- [15].DeVellis RF, Blalock SJ, Holt K, Renner BR, Blanchard LW, Klotz ML. Arthritis patients’ reactions to unavoidable social comparisons. Pers Soc Psychol B. 1991;17:392–9. [Google Scholar]
- [16].Kulik JA, Mahler HIM. Stress and affiliation in a hospital: preoperative roommate preferences. Pers Soc Psychol B. 1989;15:183–93. [Google Scholar]
- [17].Hornstein H, Fisch E, Holmes M. Influence of a model’s feelings about his behavior and his relevance as a comparison other on observers’ helping behavior. J Pers Soc Psychol. 1968;10:220–6. [Google Scholar]
- [18].Tennen H, McKee TE, Affleck G. Social comparison processes in health and illness. In: Suls J, Wheeler L, editors. Handbook of social comparison: theory and research. Kluwer/Plenum Publishers; New York: 2000. pp. 443–83. [Google Scholar]
- [19].Caballero AE. Diabetes in the Hispanic or Latino population: genes, environment, culture and more. Curr Diabetes Rep. 2005;5:217–25. doi: 10.1007/s11892-005-0012-5. [DOI] [PubMed] [Google Scholar]
- [20].McCaston KM. Partnership and Household Livelihood Security Unit (PHLS Unit), CARE. Tips for collecting, reviewing and analyzing secondary data. 1998:1–11. [Google Scholar]
- [21].Strauss AL, Corbin JM. Basics of qualitative research: grounded theory procedures and techniques. Sage Publications; Newbury Park, CA: 1990. [Google Scholar]
- [22].Gorawara-Bhat R. The social and spatial ecology of work: the case of a survey research organization. Plenum/Kluwer Academic; New York: 2000. pp. 25–40. [Google Scholar]
- [23].Gibbons FX, Gerrard M. Downward comparison and coping with threat. In: Suls J, Wills TA, editors. Social comparison: contemporary theory and research. Lawrence Erlbaum; Hillsdale, NJ: 1991. pp. 317–46. [Google Scholar]
- [24].Collins RL. Among the better ones: upward assimilation in social comparison. In: Suls J, Wheeler L, editors. Handbook of social comparison. Kluwer Academic/Plenum; New York: 2000. pp. 159–72. [Google Scholar]
- [25].Lockwood P, Kunda Z. Superstars and me: predicting the impact of role models on the self. J Pers Soc Psychol. 1997;73:91–103. [Google Scholar]
- [26].Suls J. Contributions of social comparison to physical illness and well-being. In: Suls J, Wallston KA, editors. Social psychological foundations of health and illness. Blackwell Publishing; Ames, IA: 2003. pp. 226–55. [Google Scholar]
- [27].Walcott-McQuigg JA, Prohaska TR. Factors influencing participation of African American elders in exercise behavior. Public Health Nurs. 2001;18:194–203. doi: 10.1046/j.1525-1446.2001.00194.x. [DOI] [PubMed] [Google Scholar]
- [28].Taylor RJ, Cahtters LM, Hardison CB, Riley A. Informal social support networks and subjective well-being among African Americans. J Black Psychol. 2001;27:439–63. [Google Scholar]
- [29].Buunk BP, Gibbons FX, editors. Health and coping: perspectives from social comparison theory. Lawrence Erlbaum; Mahwah, NJ: 1997. pp. 299–328. [Google Scholar]
- [30].Helgeson VS, Taylor SE. Social comparisons and adjustment among cardiac patients. J Appl Soc Psychol. 1993;23:1171–95. [Google Scholar]
- [31].Wills TA. Downward comparison as a coping mechanism. In: Snyder CR, Ford CE, editors. Coping with negative life events: clinical and social psychological perspectives. Plenum; New York: 1987. pp. 243–68. [Google Scholar]
- [32].Weiss MA. Empowerment: a patient’s perspective. Diabetes Spectr. 2006;19:116–8. [Google Scholar]
- [33].Anderson RM, Funnell MM. Patient empowerment: reflections on the challenge of fostering the adoption of a new paradigm. Patient Educ Couns. 2004;57:153–7. doi: 10.1016/j.pec.2004.05.008. [DOI] [PubMed] [Google Scholar]
- [34].Feste C, Anderson RM. Empowerment: from philosophy to practice. Patient Educ Couns. 1995;26:139–44. doi: 10.1016/0738-3991(95)00730-n. [DOI] [PubMed] [Google Scholar]
- [35].Anderson RM, Funnell MM. The art of empowerment: stories and strategies for diabetes educators. American Diabetes Association; Alexandria, VA: 2000. [Google Scholar]
- [36].Luban-Plozza B. Empowerment techniques: from doctor-centered to patient-centered discussion groups. Patient Educ Couns. 1995;26:257–63. doi: 10.1016/0738-3991(95)00756-p. [DOI] [PubMed] [Google Scholar]
- [37].Arnold MS, Butler PM, Anderson RM, Funnell MM, Feste C. Guidelines for facilitating a patient empowerment program. Diabetes Educ. 1995;21:308–12. doi: 10.1177/014572179502100408. [DOI] [PubMed] [Google Scholar]
- [38].Miller JW. A different take on health care: A trip to Lourdes. Wall Street J. 2007;1:15. Sect: A. [Google Scholar]
- [39].Burnet DL, Elliott LD, Quinn MT, Plaut AJ, Schwartz MA, Chin MH. Preventing diabetes in the clinical setting. J Gen Intern Med. 2006;21:84–93. doi: 10.1111/j.1525-1497.2005.0277.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Royer A. Life with chronic illness: social and psychological dimensions. Praeger; Westport, Connecticut: 1998. [Google Scholar]
- [41].Knafl KA, Deatrick JA. How families manage chronic conditions: an analysis of the concept of normalization; Proceedings of the paper presented at the Midwest Sociological Association Meeting; 1984. [Google Scholar]
- [42].Farquhar M. Elderly people’s definitions of quality of life. Soc Sci Med. 1995;41:1439–46. doi: 10.1016/0277-9536(95)00117-p. [DOI] [PubMed] [Google Scholar]
- [43].Funnell MM, Tang TS, Anderson RM. From DSME to DSMS: developing empowerment-based diabetes self-management support. Diabetes Spectr. 2007;20:221–6. [Google Scholar]
- [44].Fisher RJ. Social desirability bias and the validity of indirect questioning. J Consum Res. 1993;20:303–15. [Google Scholar]
- [45].Fishbein M. The theory of reasoned action and healthcare behavior. In: Terry D, Gallois M, McCamish M, editors. The theory of reasoned action: its application to AIDS preventive behavior. Pergamon Press; New York: 1993. pp. 1–27. [Google Scholar]
- [46].Prochaska JO, Velicer WF. Behavior change: the transtheoretical model of health behavior change. Am J Health Promot. 1998;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- [47].Rindfleisch A, Malter AJ, Ganesan S, Moorman C. Cross-sectional versus longitudinal survey research: concepts, findings and guidelines. Institute for the Study of Business Markets; University Park, PA: 2007. ISBM Report # 2-2007. [Google Scholar]
- [48].Suls J, Martin R, Wheeler L. Three kinds of opinion comparison: the triadic model. Pers Soc Psychol Rev. 2000;4:219–37. [Google Scholar]