Abstract
Background
Recently, the number of thyroid surgery cases has been increasing; consequently, the number of patients who visit plastic surgery departments with a chief complaint of swallowing deformity has also increased. We performed a scar correction technique on post-thyroidectomy swallowing deformity via platysma flap with Z-plasty and obtained satisfactory aesthetic and functional outcomes.
Methods
The authors performed operations upon 18 patients who presented a definitive retraction on the swallowing mechanism as an objective sign of swallowing deformity, or throat or neck discomfort on swallowing mechanism such as sensation of throat traction as a subjective sign after thyoridectomy from January 2009 till June 2012. The scar tissue that adhered to the subcutaneous tissue layer was completely excised. A platysma flap as mobile interference was applied to remove the continuity of the scar adhesion, and additionally, Z-plasty for prevention of midline platysma banding was performed.
Results
The follow-up results of the 18 patients indicated that the definitive retraction on the swallowing mechanism was completely removed. Throat or neck discomfort on the swallowing mechanism such as sensation of throat traction also was alleviated in all 18 patients. When preoperative and postoperative Vancouver scar scales were compared to each other, the scale had decreased significantly after surgery (P<0.05).
Conclusions
Our simple surgical method involved the formation of a platysma flap with Z-plasty as mobile interference for the correction of post-thyroidectomy swallowing deformity. This method resulted in aesthetically and functionally satisfying outcomes.
Keywords: Cicatrix, Thyroidectomy, Neck muscles
INTRODUCTION
Recently, the number of thyroid surgery cases has been increasing. Consequently, the number of patients who visit plastic surgery departments with a chief complaint of surgery-related scar formation, particularly swallowing deformity as a definitive retraction on swallowing mechanism, has also increased. The various methods of thyroidectomy include endoscopic surgery, robotic surgery, and thyroidectomy via cervical incision. Among these methods, thyroidectomy via cervical incision is the most frequently used; however, it leaves the longest scar and has the highest potential for swallowing deformity formation. Flat linear surgical scars can usually be concealed with makeup or along wrinkle lines, and a hypertrophic or depressed skin scar could be easily corrected by scar revision. However, if the scar adhesion is continuous from the skin surface through the subcutaneous tissue layer, muscle layer, and thyroid cartilage, a swallowing deformity may be formed (Fig. 1). A swallowing deformity cannot be corrected by simple skin scar revision as scar excision from the skin to the subcutaneous tissue layer only. Moreover, it could cause discomfort in patients' swallowing function; thus, it can cause not only aesthetic but also psychological problems and, therefore, definitely requires correction [1].
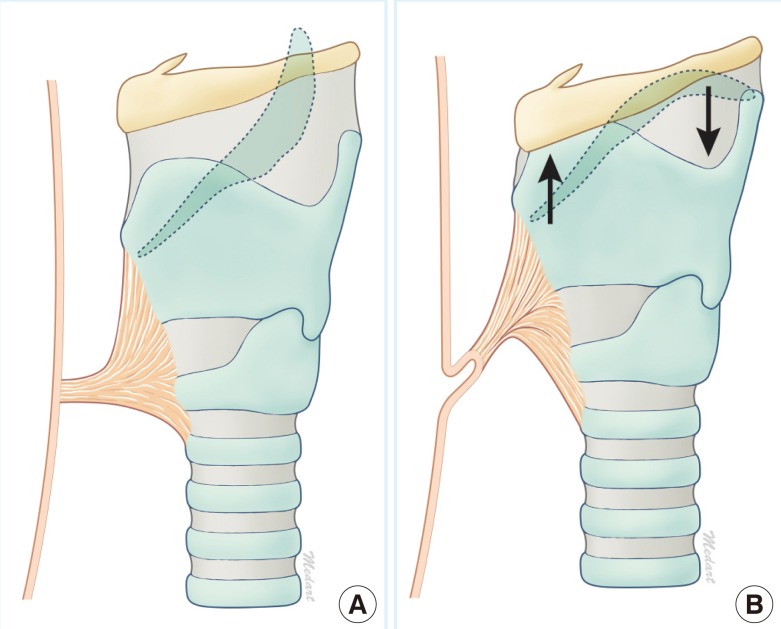
Fig. 1.
Schematic illustration of scar adhesion
(A) The scar adhesion from the skin surface, dermis, subcutaneous tissue, and muscle layer to the thyroid cartilage forms a continuity during wound healing. (B) Scar adhesion transfers the force generated by the thyroid cartilage's movement by the swallowing mechanism (black arrow) to the scar on the skin and thus pulls the scar in an internal and superior direction and eventually causes a swallowing deformity.
Although many thyroid operations have been conducted and many patients have presented with complaints of swallowing deformity-related discomfort in recent times, few studies, if any, on scar correction techniques for post-thyroidectomy swallowing deformity have been published. For post-thyroidectomy swallowing deformity, in this study we performed a scar correction technique using a platysma flap, which functions as mobile interference, and also performed Z-plasty to prevent midline platysma banding and obtained functionally and aesthetically satisfactory outcomes. Therefore, we describe in this paper our present cases, with references to support our findings.
METHODS
Subjects
The authors performed surgery upon 18 patients who presented a definitive retraction on the swallowing mechanism as an objective sign of swallowing deformity, or throat or neck discomfort on the swallowing mechanism such as sensation of throat traction as a subjective sign after thyoridectomy from January 2009 till June 2012. Out of a total of 18 patients, 3 were males and 15 were females. The ages of the patients ranged from 25 to 53 years, with a mean of 48.5 years. All 18 patients had both objective and subjective signs. Furthermore, 3 of them had a history of previous simple scar revision, and they visited this hospital due to a relapse of the symptoms.
The mean interval between the time of thyroidectomy and the time of operation via platysma flap with Z-plasty was 10.2 months. The follow-up period after scar correction was 6 to 20 months, with a mean of 11.4 months (Table 1).
Table 1.
Summary of patient characteristics and results
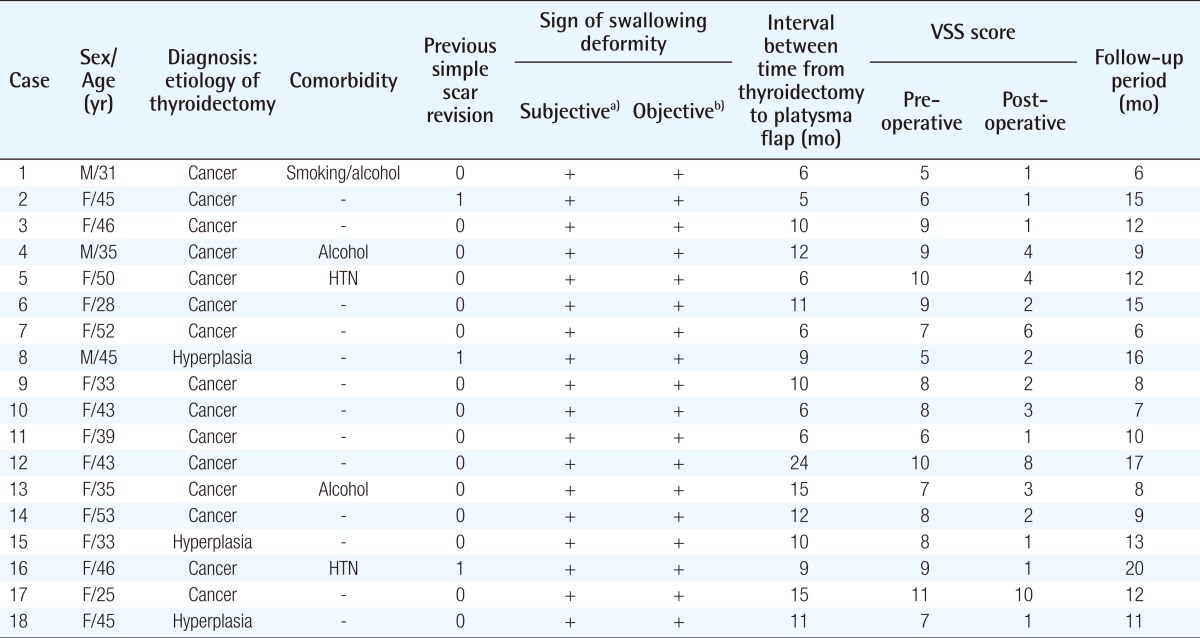
VSS, vancouver scar scale; HTN, hypertension.
a)Throat or neck discomfort on swallowing mechanism such as sensation of throat traction; b)Definitive retraction on swallowing mechanism.
Methods
The patients underwent surgery in the supine position, under local anesthesia. The cervical area was sterilized, and the surgical plan was established 2 mm from the scar margin, according to the shape of the scar. During swallowing, the site of the most severe tethering due to the scar band was determined, after which local anesthesia was induced with 2% lidocaine and 1:100,000 diluted epinephrine.
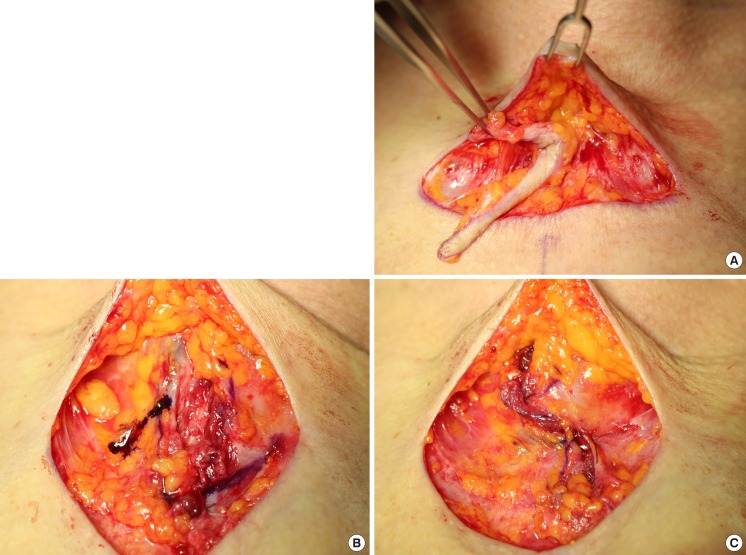
Along with the incision line that had been drawn, an incision was made up to the subcutaneous tissue level, and the scar tissue was completely excised from the skin surface to the subcutaneous tissue layer. Once the scar tissue, which had adhered to the subcutaneous tissue layer, was completely excised within 2 cm of the incision margin, the scar band was incised to release the tethering as the patient was instructed to swallow each time to locate the scar band (Fig. 2A). The platysma flap was then obtained by dissecting above and below the platysma, including the platysma fascia, at a total distance of 2 cm above the previous thyroid incision line.
Fig. 2.
Intraoperative photographs of a case
(A) When the patient is asked to swallow, the location of the scar band, as indicated, can be seen precisely. (B) After checking the medical border of the platysma flap, the design is made in a Z-plasty shape. This is how it looks when the B and D sites are initially sutured. (C) Platysmaplasty with Z-plasty.
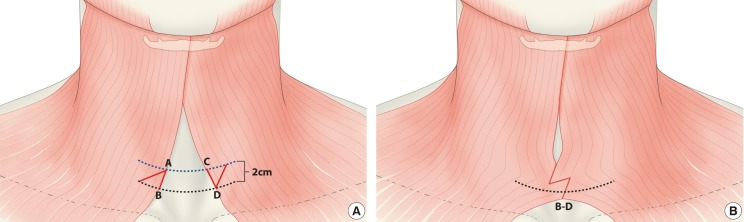
The point 2 cm above the previous incision line on the medial border of the right platysma flap was denoted as point A, and the point on the previous incision line was designated as point B. The same spots on the left side were labeled points C and D, respectively. Accordingly, the surgical plan was designed so that points A to B and C to D would become the central member, with a length of 2 cm and a 60-degree Z angle from the central member (Figs. 2B, 3A) [2]. However, the angle or length of the Z-plasty incision could vary according to the anatomy of the platysma. First, the B-D spot was approximated, and a horizontal mattress suture (Vicryl 5-0) was made. Then, an incision was made along the drawn Z line, and horizontal mattress and simple interrupted sutures were made by approximation according to the Z shape, forming the platysma flap barrier (Figs. 2C, 3B). The dermis was sutured subcuticularly (Prolene 5-0), and the skin incision was closed using a simple interrupted suture (Prolene 6-0). Drainage was not performed, and light-pressure dressing was applied. The patient was instructed not to cough and to wear a neck splint made of a sponge for a week to prevent tension on the sutured site. The skin suture was removed on the seventh postoperative day, and a Steri Strip was placed on the wound. The subcuticular suture was removed 21 days after the operation. For scar management, massage was done and Cica Care (Smith & Nephew, London, UK) or Kelo-cote (Enaltus, Suwanee, GA, US) were applied for at least 6 months.
Fig. 3.
Schematic illustration of surgical methods
(A) The Z-plasty design (red line) is made after designating the spots 2 cm above the incision line as as AC (blue dotted line), and the incision line as BD (black dotted line, previous operation incision line). (B) Schema illustration after Z-plasty is performed.
In order to objectively compare the results of the surgery, the authors used the Vancouver scar scale (VSS) to measure all of the 18 patients before surgery and 6 months after surgery. The VSS contains 4 variables: pigmentation (0-2), vascularity (0-3), pliability (0-5), and height (0-3). The measured VSS scores were statistically analyzed using a Wilcoxon signed-rank test, which is a non-parametric testing method in SPSS Statistics ver. 21 (IBM, Armonk, NY, USA).
RESULTS
The follow-up results of the 18 patients indicated that the definitive retraction on swallowing mechanism was completely removed. Furthermore, throat or neck discomfort on the swallowing mechanism such as the sensation of throat traction was also alleviated in all 18 patients.
When the preoperative and postoperative Vancouver scar scale values were compared to each other, the scale had decreased significantly after surgery (P<0.05). If the comparison were done by item, pigmentation, vascularity, pliability, and height decreased significantly (P<0.05) (Table 2).
Table 2.
Preoperative and postoperative score using the Vancouver scar scale
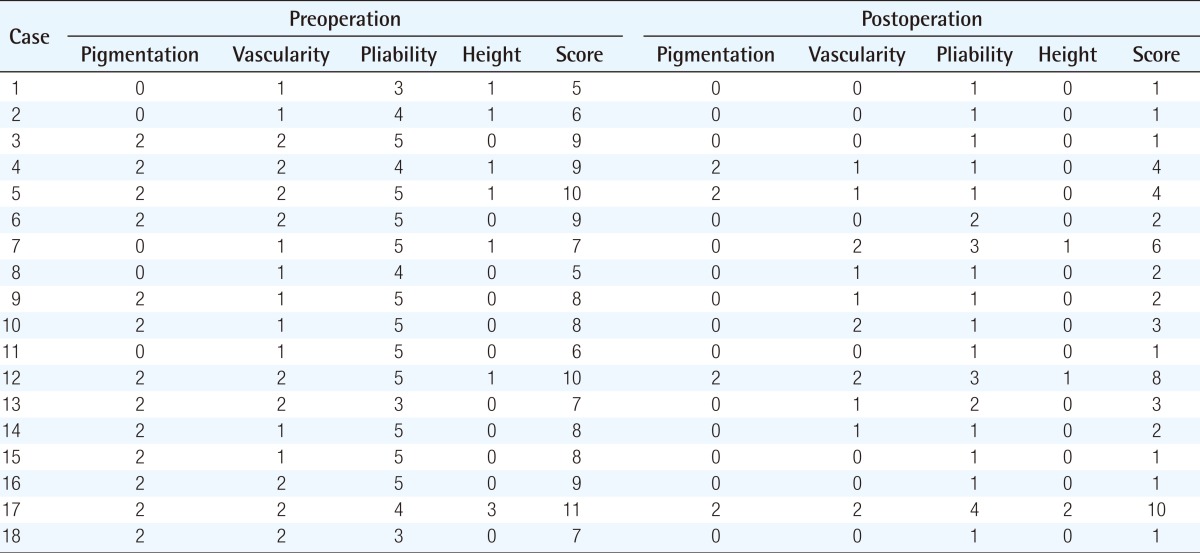
The difference in the scar location change is significant (P < 0.05); Wilcoxon signed-rank test.
None of the 18 patients presented inflammation, hematoma, or wound dehiscence. 2 patients showed hypertrophic scars and 1 patient showed keloid formation. As an outcome of follow-up observation after additionally prescribing Accolate (AstraZeneca, London, UK) to these 3 patients, the degree of scarring of all 3 patients improved to the point that the patients themselves were satisfied.
Case 10
A 43-year-old female had the chief complaint of depressed depressed scar on swallowing and neck discomfort on swallowing. She had undergone surgery for a near total thyroidectomy with central node dissection under general anesthesia. The biopsy showed papillary microcarcinoma with metastatic lymph node.
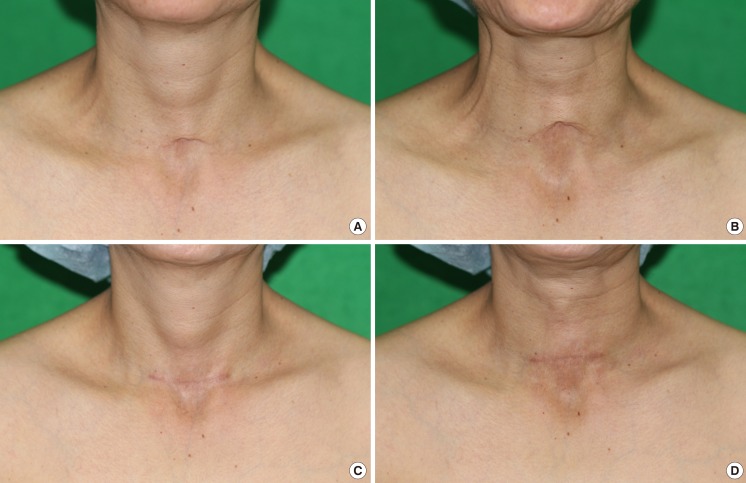
The interval between the time of thyroidectomy and the time of operation via platysma flap with Z-plasty was 6 months. Before surgery, she had objective and subjective signs. The VSS score was 8 points: pigmentation 2, vascularity 1, pliability 5, and height 0 (Fig. 4A, B).
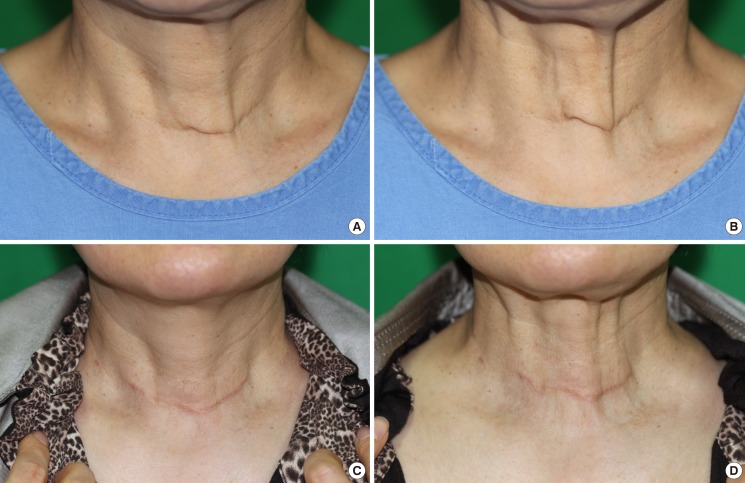
Fig. 4.
Preoperative and postoperative photographs of a patient
(A) Preoperative photograph in a static state. (B) Preoperative photograph in a swallowing state. Definitive retraction on swallowing is present. (C) Seven month postoperative photograph in a static state. (D) Seven month postoperative photograph in a swallowing state. Definitive retraction on swallowing is not present.
The scar tissue was completely excised from the skin surface to the subcutaneous tissue layer and platysma flap with Z-plasty was performed.
Six months after surgery, objective and subjective signs had disappeared. The VSS score was 3 points: pigmentation 0, vascularity 2, pliability 1, and height 0. Follow-up lasted for 7 months after surgery was performed (Fig. 4C, D).
Case 14
A 53-year-old female had a chief complaint of a striking neck scar on swallowing and throat discomfort on swallowing. She had undergone total thyroidectomy with modified node dissection under general anesthesia. The biopsy showed papillary microcarcinoma. The interval between the time of thyroidectomy and the time of operation via platysma flap with Z-plasty was 12 months.
Before surgery, she had objective and subjective signs. The VSS score was 8 points: pigmentation 2, vascularity 1, pliability 5, and height 0 (Fig. 5A, B).
Fig. 5.
Preoperative and postoperative photographs of a patient
(A) Preoperative photograph in a static state. (B) Preoperative photograph in a swallowing state. Definitive retraction on swallowing is present. (C) Nine month postoperative photograph in a static state. (D) Nine month postoperative photograph in a swallowing state. Definitive retraction on swallowing is not present.
The scar tissue was completely excised from the skin surface to the subcutaneous tissue layer and a platysma flap with Z-plasty was performed.
Six months after surgery, the objective and subjective signs had disappeared. The VSS score was 2 points: pigmentation 0, vascularity 1, pliability 1, and height 0. Follow-up was performed until 9 months after surgery (Fig. 5C, D).
DISCUSSION
The thyroid cancer incidence rate in Korea has been gradually increasing. According to data released by the Central Cancer Registration Center in Korea, thyroid cancer topped the list of types of cancer at an incidence rate of 17.8%, with an annual mean of 36,021 cases, regardless of sex. Thyroid cancer ranked first place in women and sixth place in men. The overall incidence of thyroid cancer according to sex was highest among 15-year-old to 34-year-old [3].
As a result, the number of surgical procedures performed has also increased, including endoscopic surgery, robotic surgery, and thyroidectomy via cervical incision, which are the surgical methods currently used in Korea. Currently, the most frequently used surgical method is conventional thyroidectomy via cervical incision, in which an incision is made from the sterna notch through the neck wrinkle 2 fingerbreadths above the sterna notch. The subcutaneous tissue and platysma are then divided via cauterization [4]. Among the methods, this one leaves the longest scar and has the highest possibility of swallowing deformity formation.
A swallowing deformity causes a significant amount of aesthetic and functional discomfort to patients. In more severe cases, functional disability such as dysphasia or limited cervical area extension could occur owing to continuous contraction of the thyroid cartilage by the scar [5]. Therefore, surgical correction of a swallowing deformity is important in terms of aesthetic and functional purposes and is absolutely necessary to improve the patient's quality of life.
However, there have been few studies on post-thyroidectomy swallowing deformity or its surgical method. Studies on post-tracheostomy tethered scar, which has similar signs, and its surgery method have already been published. Through comparative analysis of these studies, therefore, the authors embarked upon planning this study. In many prior studies, reports on the post-tracheostomy tethered scar and its surgery method have been as follows.
In 1918, Poulard [6] reported a correction method for post-tracheostomy retracted scars; however, the method failed to correct tracheal contraction, although it successfully corrected the retraction by making an incision around the scar, desquamatizing the scar tissue, and then adequately dividing and suturing the adjacent skin flap.
In 1961, Pressman [7] corrected a post-tracheostomy tethered scar by excising the scar and filling the retracted scar with sternocleidomastoid muscle. However, some problems were encountered with the use of the method, such as extension of the incision around the scar and difficulty in controlling bleeding due to the deep dissection wound.
In 1975, Vecchione and Pickering [8] were able to correct a patient's scar retraction by performing Z-plasty alone on the subcutaneous tissue; however, the patient developed a complication of skin contraction during swallowing due to readhesion to the trachea.
In 1972, Kulber and Passy [1] sutured a retracted scar with a tracheal fistula by advancing the suture up to the center using strap muscle. Furthermore, Carlson et al. [5] reported a method involving the removal of the scar and subcutaneous tissue underneath the scar and placement of the sternocleidomastoid muscle and fascia in the center, covered with the allogeneic dura.
As described above, post-tracheostomy tethered scar is a depression scar caused by volume loss as an anatomical defect because the scar was left as it was without primary suture so that it could heal by secondary adhesion. Therefore, volume restoration will be necessary, and many methods for it are being reported.
However, what causes post-thyroidectomy swallowing deformity of the normal anatomy is the continuity of scar adhesion. The scar adhesion from the skin surface, dermis, subcutaneous tissue, and muscle layer to the thyroid cartilage forms in continuity during wound healing. This scar adhesion transfers the force which is generated by the thyroid cartilage's movement by the swallowing mechanism to the scar on the skin and thus pulls the scar in an internal and superior direction and eventually causes a swallowing deformity [9,10].
In other words, in the case of post-thyroidectomy swallowing deformity, surgery not for volume restoration but for interference with scar adhesion is needed.
Therefore, we blocked the continuity of scar adhesion by using a platysma flap, which functions as mobile interference and additionally performed Z-plasty to prevent midline platysma banding.
Our surgical method has the following merits: First, the platysma flap was used for correction of the swallowing deformity. The reason the platysma was used is that it allows better manipulation during surgery than other muscles. Because it is located immediately below the subcutaneous layer, it allows for easy access and elevation. In addition, handling is easy because of its thinness and elasticity and the resulting aesthetic deformity is rare owing to the change in anatomical location [11]. When elevating the platysma, the platysma fascia must be included to improve the elasticity of the platysma, which in turn improves mobility and prevents tearing during the suture.
Second, Z-plasty was used on the platysma flap. Primary repair of platysma causes a platysma midline scar and thus could cause midline platysma banding. Therefore, Z-plasty was performed so that midline platysma banding formation could be prevented [12]. In addition, Z-plasty made the extension of the length possible and thus could narrow down the range of dissection.
Third, the cost could be low, as additional surgical procedures are not required because of the use of the patient's own tissue, which is safe to use and not likely to be absorbed. In barrier-forming methods for interference in scar adhesion, injection of filler agents such as collagen and hyaluronic acid is administered and autologous fat grafting is performed. However, the results of these methods are not permanent because the grafts become absorbed over time. They are also only effective for small scars, although the methods are simple per se [13,14].
Platysma flap with Z-plasty, as a result, brought significant improvement to definitive retraction on the swallowing mechanism, pigmentation, vascularity, pliability, and height. In addition, good outcomes from aesthetic and functional perspective were gained due to Z-plasty. Therefore, it is safe to say that Z-plasty is a meaningful surgical method for correction of post-thyroidectomy swallowing deformity.
However, the authors also pity the fact that there the number of cases was insufficient and consider this to be a limitation, such that further long-term studies will be necessary in the future.
Also, the authors did studies on the method that will solve post-thyroidectomy swallowing deformity in this article. However, to ultimately prevent the swallowing deformity in thyroidectomy, it is important that denuded thyroid cartilage is covered by adjacent muscles or soft tissue and that the scar adhesion between the thyroid cartilage and neighboring tissue is prevented by minimization of the use of electrocautery or dissection on thyroid cartilage or neighboring tissue, and studies on this are also necessary.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Kulber H, Passy V. Tracheostomy closure and scar revisions. Arch Otolaryngol. 1972;96:22–26. doi: 10.1001/archotol.1972.00770090060006. [DOI] [PubMed] [Google Scholar]
- 2.Rohrich RJ, Zbar RI. A simplified algorithm for the use of Z-plasty. Plast Reconstr Surg. 1999;103:1513–1517. [PubMed] [Google Scholar]
- 3.National Cancer Information Center. Statics of thyroid cancer [Internet] Goyang (KR): National Cancer Information Center; c2012. [cited 2013 Jul 4]. Available from: http://www.cancer.go.kr/mbs/cancer/subview.jsp?id=cancer_040102000000. [Google Scholar]
- 4.Mathur AK, Doherty GM. Thyroidectomy and neck dissection. In: Minter RM, Doherty GM, editors. Current procedures surgery. 1st ed. Michigan: McCraw-Hill; 2010. pp. 1–7. [Google Scholar]
- 5.Carlson ER, Marx RE, Jones GM. Tracheostomy scar revision using allogeneic dura. J Oral Maxillofac Surg. 1991;49:315–318. doi: 10.1016/0278-2391(91)90232-b. [DOI] [PubMed] [Google Scholar]
- 6.Poulard A. Traitement des cicatrices faciales. Pres Med. 1918;26:221. [Google Scholar]
- 7.Pressman JJ. The repair of depressed tracheotomy scars. Arch Otolaryngol. 1961;74:150–152. doi: 10.1001/archotol.1961.00740030155005. [DOI] [PubMed] [Google Scholar]
- 8.Vecchione TR, Pickering PP. The subcutaneous Z-plasty: case report. Plast Reconstr Surg. 1975;56:579–580. doi: 10.1097/00006534-197511000-00023. [DOI] [PubMed] [Google Scholar]
- 9.Singer AJ, Clark RA. Cutaneous wound healing. N Engl J Med. 1999;341:738–746. doi: 10.1056/NEJM199909023411006. [DOI] [PubMed] [Google Scholar]
- 10.Mast BA, Diegelmann RF, Krummel TM, et al. Scarless wound healing in the mammalian fetus. Surg Gynecol Obstet. 1992;174:441–451. [PubMed] [Google Scholar]
- 11.de Castro CC. The anatomy of the platysma muscle. Plast Reconstr Surg. 1980;66:680–683. doi: 10.1097/00006534-198011000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Biggs TMJ, Steely RL. The male neck and T-Z-plasty: 28 years later. Aesthet Surg J. 2000;20:31–34. [Google Scholar]
- 13.Kontis TC. Scar revision and skin resurfacing. In: Snow JB, Wackym PA, editors. Ballenger's otorhinolaryngology head and neck surgery. Connecticut: People's Medical Publishing House; 17th ed. pp. 707–716. [Google Scholar]
- 14.Shiffman MA. Subcison with fat transfer. In: Shiffman MA, editor. Autologus fat transfer, art, science and clinical practice. Heidelberg: Springer; 2009. pp. 65–68. [Google Scholar]