Abstract
Background/Aims
Screening for hepatitis B virus (HBV) is recommended in populations with anticipated prevalence ≥2%. This study surveyed HBV screening and vaccination practices of Asian American primary care providers (PCPs).
Methods
Approximately 15,000 PCPs with Asian surnames in the New York, Los Angeles, San Francisco, Houston, and Chicago areas were invited to participate in a web-based survey. Asian American PCPs with ≥25% Asian patients in their practice were eligible.
Results
Of 430 (2.9%) survey respondents, 217 completed the survey. Greater than 50% followed ≥200 Asian patients. Although 95% of PCPs claimed to have screened patients for HBV, 41% estimated that ≤25% of their adult Asian patients had ever been screened, and 50% did not routinely screen all Asian patients. In a multivariable analysis, the proportion of Asian patients in the practice, provider geographic origin and the number of liver cancers diagnosed in the preceding 12 months were significantly associated with a higher likelihood of screening for HBV. Over 80% of respondents reported that ≤50% of their adult Asian patients had received the HBV vaccine.
Conclusions
Screening and vaccination for HBV in Asian American patients is inadequate. Measures to improve HBV knowledge and care by primary-care physicians are critically needed.
Keywords: Hepatitis B virus, Chronic hepatitis B
INTRODUCTION
Chronic hepatitis B (CHB) is a serious global healthcare problem and a major cause of liver disease including hepatocellular carcinoma (HCC). Worldwide, 350 million to 400 million people have CHB, of whom approximately 1 million per year die of complications.1 In the United States, where around 2 million Americans have CHB, an estimated 3,000 to 6,000 people die annually of complications.2,3 Despite wide availability of hepatitis B virus (HBV) vaccine programs, new hepatitis infections are common, particularly in high endemic regions, such as eastern Asia, India, and Pakistan. Although the World Health Organization reports having implemented universal HBV vaccination in 84% (162/193) of its member countries as of 2006, the morbidity and mortality associated with prevalent cases of CHB will continue for decades to come.4
In the United States, CHB disproportionately affects the Asian and Pacific Islander communities and Asian Americans are 2 to 3 times more likely to develop and die from HCC than Caucasian Americans.5 HBV screening and vaccination was shown to be cost effective in Asian and Pacific islander Americans.6 In September 2008, the Centers for Disease Control and Prevention updated recommendations for HBV screening to include persons born in countries with HBV infection prevalence ≥2%.7 However, fewer than 25% of Asian American CHB patients have been diagnosed, and 40% to 65% go unscreened.8
To enhance screening, diagnosis, referral, and treatment as well as prevention of HBV, essential data are needed to understand the current status of HBV care in the United States. Whereas modern therapeutic agents have been shown to provide potent and reliable suppression of HBV, lack of implementation of appropriate screening in high-risk individuals constitutes a critical barrier to reducing the burden of HBV in the United States. In this work, we investigate HBV screening and vaccination practices among Asian American primary care physicians (PCPs) who provides care to predominantly Asian American patients and determine factors that influence these practices.
MATERIALS AND METHODS
A web-based survey was conducted to evaluate HBV screening and vaccination practices of Asian American PCPs treating Asian patients living in the United States in 2008. Approximately 15,000 PCPs with Asian surnames and medical practices in the New York, Los Angeles, San Francisco, Houston, and Chicago metropolitan areas were invited to participate. Asian-surnamed PCPs were identified from an existing market research database and lists obtained from the American Medical Association, as well as online search of providers practicing within selected zipcodes. Common Asian surnames were determined from a reference for six major Asian American ethnic groups.9 The surname Lee was excluded, because of commonality with non-Asian individuals.
The study was approved by a central Institutional Review Board (the Copernicus Group) and survey respondents provided electronic informed consent. Eligible study respondents met all inclusion criteria: 1) self-reported Asian descent; 2) licensed United States physician in internal medicine, family medicine, or general practice; 3) ≥25% practice patients of Asian descent; and 4) willingness and ability to provide informed consent and complete the web-based survey in English.
A web-based survey was designed by a collaboration of clinical experts in HBV and a research organization experienced in epidemiologic research and web-based surveys. The survey asked questions about demographics of the respondent and patients in his/her care, proportion of Asian patients in the given practice ever screened or vaccinated for HBV. In addition, information about reasons and motivators for HBV screening was collected as well as barriers that prevent appropriate screening. Lastly, survey respondents were asked to answer a series of eight true-false questions that assess general knowledge about HBV. These last questions were presented in a random order asking about HBV in general, risk factors, complications and treatment. The survey was designed to be completed in less than 20 minutes.
The survey link was emailed to PCPs by an independent research organization. Respondents were compensated for time to complete the survey. As an additional incentive for the PCP to participate in the study, links to websites that provides information about CHB, including opportunities for independent CHB continuing medical education were provided at the end of the survey. Furthermore, respondents were offered the opportunity, by telephone or email, for 1:1 contact with expert hepatologist mentors.
Results were anonymous and data pooled for analysis. Electronic safeguards prevented double entry from a single user name and password. The goal was to receive at least 200 completed surveys. Initial descriptive statistics included frequency tables and mean summaries. Counts and percentages were calculated for each survey question. Univariate and multivariate logistic regression analysis was performed to identify factors associated with screening practice-variables with univariate significance were included in the multivariable model in which the stepwise variable selection method was employed to develop the final model. All analyses were performed using JMP or SAS statistical software version 9.1 (SAS Institute Inc., Cary, NC, USA).
RESULTS
1. Demographics of the Asian primary care providers and patients
Of 14,948 PCPs invited to participate, 430 (2.9%) entered the survey, 270 (1.8%) met study eligibility criteria, and 217 (1.5%) completed the survey. The most common reason for exclusion was ≤25% Asian patients in the respondent's practice (n=109). Table 1 summarizes the demographics and characteristics of survey respondents. New York and Los Angeles areas represented two-thirds of geographic location of practice. Although the majority of the respondents had been born outside the United States, more than half graduated from a United States medical school.
Table 1.
Demographics and Characteristics of Survey Respondents
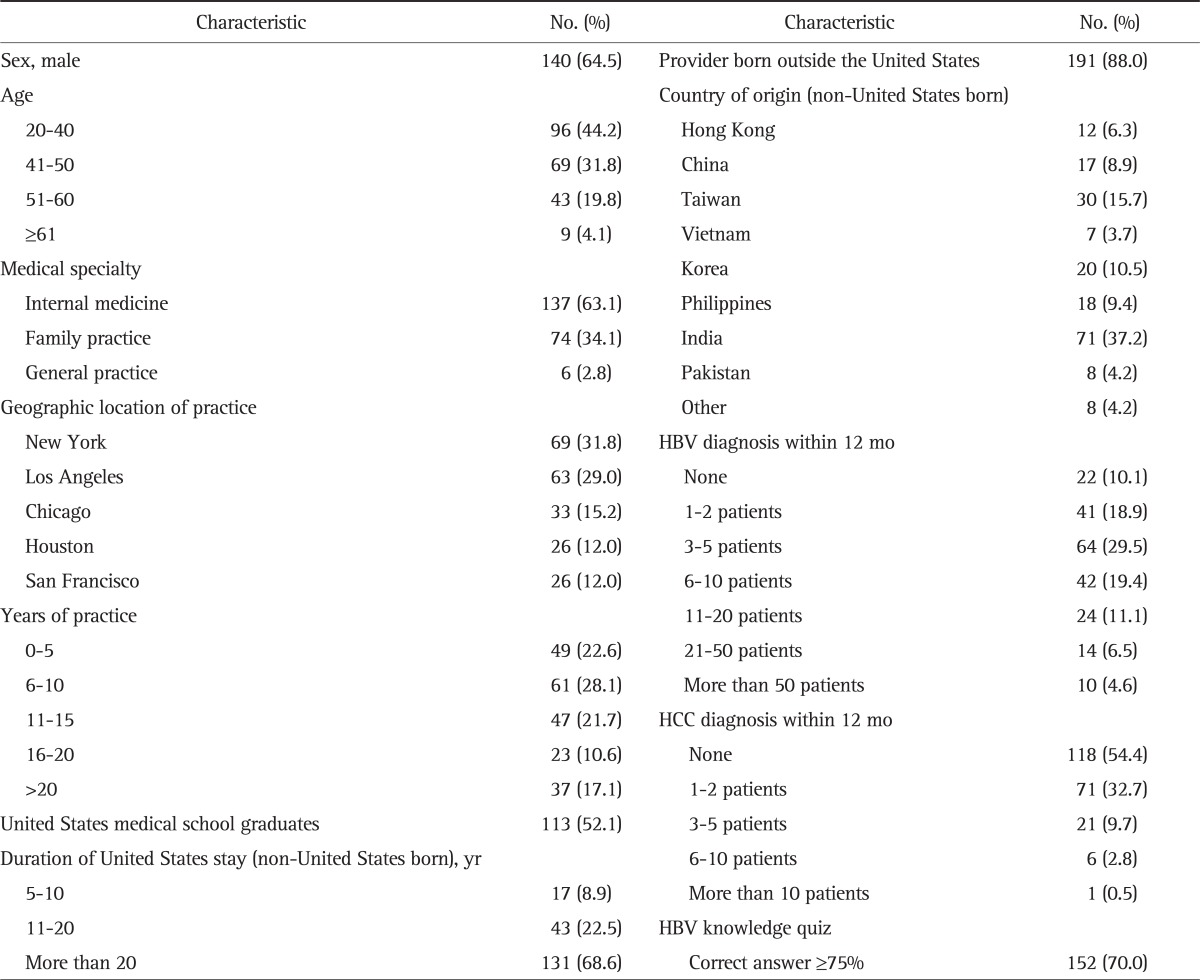
HBV, hepatitis B virus; HCC, hepatocellular carcinoma.
Ninety percent of respondents reported having diagnosed at least one patient with CHB in the past year and 46% having diagnosed at least one liver cancer in the past year. The survey included eight questions to assess the respondent's general knowledge about hepatitis B. The proportion of correct answers ranged from 25% to 100%.
Table 2 describes the characteristics of patient population of survey respondents. Overall, the mean proportion of the patient population being Asians was 35% (range, 25% to 100%). More than half (55%) of the respondents reported following more than 200 adult Asian patients, most of whom were foreign-born. Hong Kong, China, Taiwan (27%), and India (37%) were the most common countries of origin. As expected, there was a significant concordance in the country of origin between the physician and patients (p<0.05 for Chinese, Indian, Japanese, Korean, Vietnamese, Filipino, Pakistani, and Thai respondents). Only one-third of respondents indicated that majority (range, 76% to 100%) of their Asian patients carried prescription drug coverage, whereas an average of 11% of patients did not have any type of insurance.
Table 2.
Demographics of Patient Population of Survey Respondents
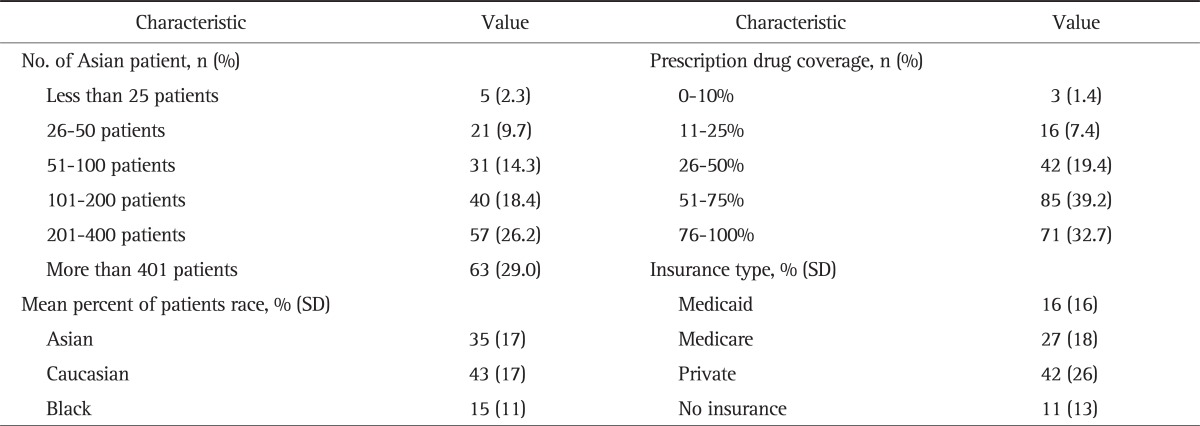
SD, standard deviation.
2. HBV screening practices and predictors
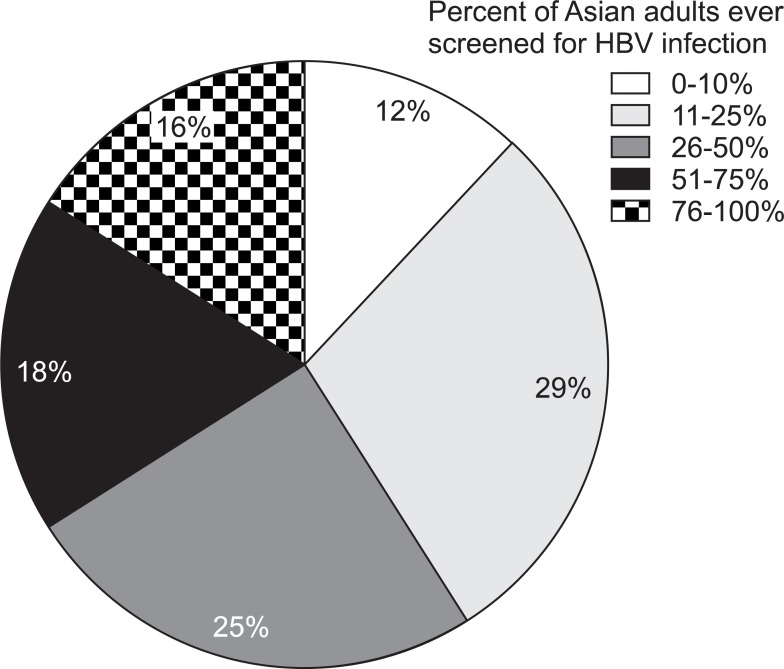
Essentially all (95.4%, n=207) respondents reported having screened for HBV in at least one patient, whereas routine screening for HBV was reported by only 35.9% (n=78). In Fig. 1, 41% providers estimated that ≤25% of their adult Asian patients had ever been screened. Similarly, 71% of the respondents estimated that they had screened 25% or less of adult Asian patients for the first time in the preceding 6 months.
Fig. 1.
Percentage of adult Asian patients that have ever been screened for hepatitis B virus (HBV). Example: 66% (12%+29%+25%) of Asian American primary care provider respondents reported that ≤50% of their Asian adult patients had ever been vaccinated.
Table 3 summarizes univariable and multivariable logistic regression analysis predicting more than 50% of adult Asian patients having been screened for hepatitis B (in the respondent's practice or elsewhere). In the univariate analysis, high-volume of Asian patients; the proportion of foreign born Asian patients, particularly from China and Vietnam; providers from Hong Kong or Taiwan; number of new HBV or HCC diagnosis within the preceding 12 months; and the proportion of patients with prescription drug coverage were associated with screening, whereas providers from India was associated with lack of screening. With regard to geographic factors, those practicing on the West coast were more likely to screen for HBV, whereas higher proportion of non-Asian patients or providers from India and Pakistan; providers practice location in Chicago or Houston metropolitan area were associated with lower likelihood of screening. Finally, HBV knowledge correlated with likelihood of screening.
Table 3.
Hepatitis B Virus-Screening Model
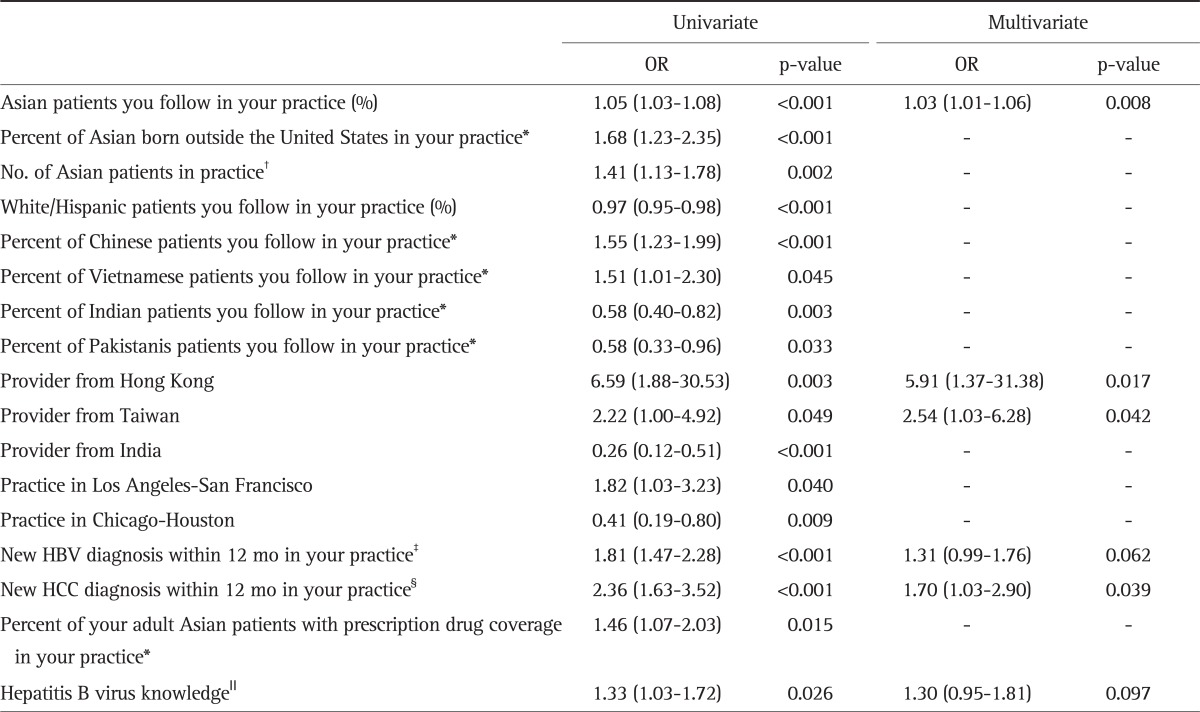
Outcome: >50% of adult Asian patients who have ever been screened for hepatitis B virus at your practice or elsewhere.
OR, odds ratio; CI, confidence interval.
*1: 0% to 10%, 2: 11% to 25%, 3: 26% to 50%, 4: 51% to 75%, 5: 76% to 100%; †1: <25 patients, 2: 26 to 50 patients, 3: 51 to 100 patients, 4: 101 to 200 patients, 5: 201 to 400, 6: >401 patients; ‡1: 0 patients, 2: 1 to 2 patients, 3: 3 to 5 patients, 4: 6 to 10 patients, 5: 11 to 20 patients, 6: 21 to 50 patients; §1: 0 patients, 2: 1 to 2 patients, 3: 3 to 5 patients, 4: 6 to 10 patients, 5: >10 patients; ∥Number of correct responses.
The multivariate analysis presented in Table 3 was constructed based on the variables selected in the univariate analysis. The following were found to be independently correlated with screening for HBV: the proportion of Asian patients in the practice, providers from Hong Kong or Taiwan, and having patients with new HCC diagnosis within the prior 12 months (Table 3).
3. Reasons to/not to screen
Respondents reporting to have screened patients for HBV were further queried regarding specific screening practices. Firstly, respondents were asked how likely they were to screen certain patients for HBV (Table 4). Although most respondents indicated always screening Asian patients with sign or symptom of liver disease, only 62% providers always screen for HBV in Asian patients with a family member with hepatitis B or liver cancer. When asked about the one most important reason for screening, most than half of the respondents selected suspicion for liver disease such as: 1) abnormal liver tests (25%); 2) abnormal liver tests plus a family history of hepatitis B or liver disease (22%); and 3) symptoms suggestive of hepatitis B/liver disease (11%). Less common was screening for purely preventative purposes such as: 1) birth outside the United States (18%); and 2) having a family member with hepatitis B and/or liver cancer (5%).
Table 4.
Reasons for Screening Asian Patients for Hepatitis B Virus Infection
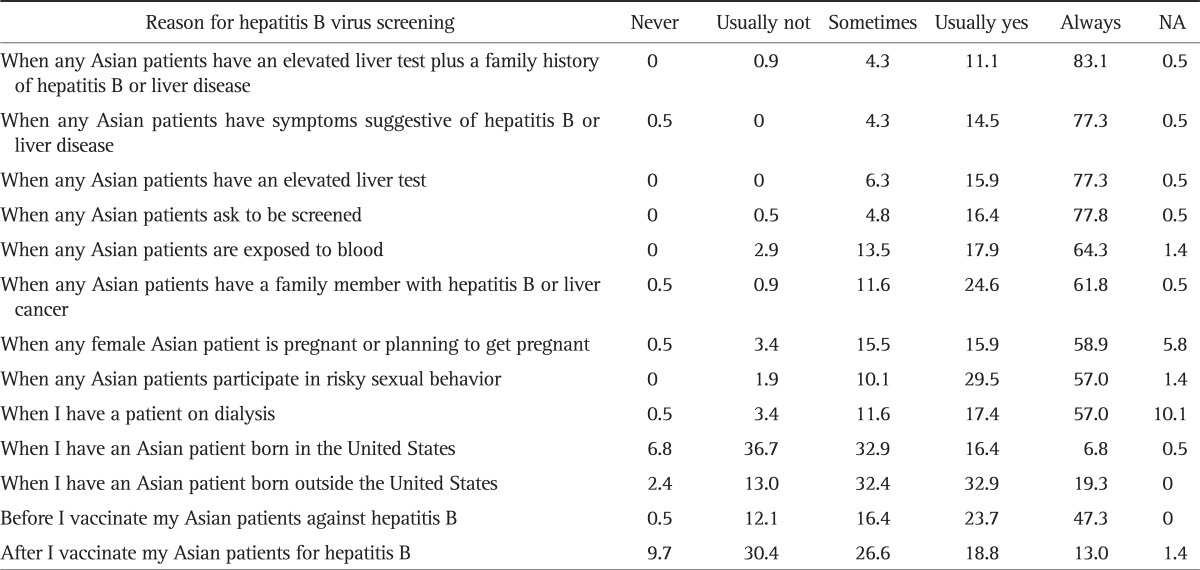
Data are presented as percentage.
NA, not applicable.
Reasons cited for not ordering screening included: 1) a perception that the patient was not at risk for hepatitis B (47%); 2) history of previous HBV vaccination (41%); 3) prior screening (35%); 4) patient refusal of screening (38%); 5) absence of symptoms of hepatitis B/liver disease (36%); and 6) lack of insurance (33%). Provider financial considerations (e.g., practice is too busy, 9%; working with insurance companies is too cumbersome or time consuming, 4%; too expensive for their practice, 3%) were cited as reasons for not screening, but infrequently. Eight respondents (4%) indicated not ordering HBV screening tests because they felt uncomfortable treating CHB.
4. HBV vaccination practices
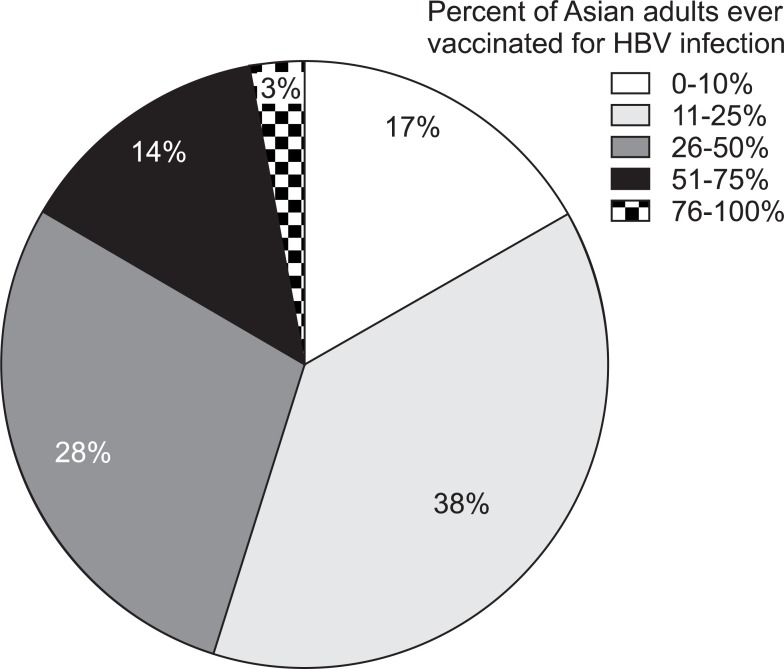
More than half of respondents reported ≤25% of their adult Asian patients had received the HBV vaccination series, and 83% reported ≤50% had been vaccinated (Fig. 2). Not surprisingly, there was strong correlation between HBV screening and vaccination practices (p<0.0001). A total of 47% of respondents reported always screening patients for HBV before vaccination; however, 13% usually did not screen, or never screened, before vaccination.
Fig. 2.
Percentage of adult patients that have had the hepatitis B virus (HBV) vaccine series. Example: 54% (17%+37%) of Asian American primary care provider respondents reported that ≤25% of their Asian adult patients have ever been vaccinated.
DISCUSSION
This study highlights a large chasm between the current recommendations and self-reported practices for hepatitis B screening and vaccination by Asian American PCPs who treat Asian Americans living in the United States. While some degree of discrepancy was anticipated at the outset of the study, some of the responses were surprising, such as only 36% of the respondents routinely screen for HBV in their practice and 41% reporting less than a quarter of their adult Asian patients having ever been screened. In terms of the factors that were associated with higher likelihood of screening, the positive feedback loop of physicians with common exposure to HBV or HCC patients being more likely to screen was expected. Also important was physician knowledge of HBV as was reflected in the quiz. On the other hand, where the practice is located or the propensity for patients to have insurance coverage, which were an important factor in the univariate analysis, were found not significant in the multivariable analysis, indicating that provider exposure and knowledge about HBV may be the primary driver of screening.
In January 2010, the Institute of Medicine (IOM) issued a report on "hepatitis and liver cancer."10 The report indicated that lack of knowledge and awareness about chronic viral hepatitis on the part of health-care and social service providers, and insufficient understanding about the extent and seriousness of this public health problem impede current efforts to prevent and control viral hepatitis in the United States. The results of this study is consistent with the findings of the IOM study in that a major barrier to screening is insufficient provider knowledge of the epidemiology, clinical presentations and complications of hepatitis B infection. Previous studies have shown that lack of knowledge is a significant barrier to physicians screening for HBV-factors such as: 1) physician and/or patient's knowledge about Asians being at high risk of CHB, how HBV is spread, and CHB potentially leading to HCC; 2) patient having a family member or friend with HBV infection; or 3) having a regular source of healthcare.10-18
Obviously, lack of physician's recommendation is a critical barrier to HBV screening, with up to 75% of patients reporting their physician not recommending HBV screening.16 Since this study specifically selected providers of Asian decent whose practice consisted of a large proportion of Asian patients, the level of nonadherence to screening recommendations was somewhat unexpected. For example, in our survey, only 62% providers reported to always screen for HBV in Asian patients with a family member with hepatitis B or liver cancer and only 5% of our respondents listed the patient having a family member with hepatitis B and/or liver cancer as the most important reason for screening. Screening of close contacts with HBV-positive persons has been recommended since 1982, based in part on data that the risk of HBV infection from a household contact or sexual partner is between 14% and 60%.7
Our results are also helpful in identifying provider characteristics that could lead to improved screening. For example, the geographic location of the practice was an important univariate predictor of screening-physicians in Chicago and Houston were less likely to screen. The fact that these factors were not found to be significant in the multivariable analysis suggests that the association was attributable to other more direct determinants such as frequency of exposure to patients with HBV and HCC and knowledge level about HBV, compared to their counterparts located on either coast. Thus, one may construe our data to indicate that increasing the knowledge level of the practitioners, perhaps by means of continuing education, may be able to overcome the lower adherence to screening. Similarly, we interpret the more frequent screening by providers from Hong Kong and Taiwan may also be explained by their familiarity with CHB. Thus, physician education may target providers of other ethnic origin to improve their knowledge level and thus screening.
Other factors that had no impact on screening practices may deserve some comments. Provider characteristics such as their age, medical specialty, years of practice, or graduation from United States medical school had no demonstrable impact on screening. In a study of cancer screening practices including screening for HCC, Asian American PCPs who serve largely Asian populations in New York City were surveyed. More than 90% of the respondents reported to recommend HBV vaccination to Asian patients; however, only two-thirds reported screening patients for hepatitis B surface antibody (immunity) or antigen (infection). The study identified barriers to the implementation of preventive measures including lack of patients understanding of the concept of preventive medicine and physician's time constraints. Surprisingly, in our study, few respondents cited reasons along these lines as barriers to HBV screening, including time constraints, difficulties working with insurance companies, screening expense, or not feeling comfortable treating HBV infection.
Limitations of this web-based survey study included possible selection bias, required computer proficiency and internet access, and geographic reach. The requirement for internet access and computer proficiency may have biased against inclusion of older physicians; however, 25% of respondents were aged >50 years and 5% were aged >60 years. Similarly, despite the multiple sources of the invitees, there is no guaranty that they truly represent the Asian American PCP population. Further, patient demographics and HBV knowledge, screening and vaccination practices of Asian American PCPs living in large cities may not be representative of other United States geographic regions. It is also possible that eligible PCPs who participated in this study may be a biased group who are more aware of CHB and our results represent the best case scenario. Finally, as with all surveys, respondents were assumed to be who they claimed (i.e., Asian American PCPs), to read and correctly interpret the questions, respond accurately, and answers reflect actual practice.
In conclusion, although respondents of this study were aware that hepatitis B affects Asian Americans, our data suggest that many Asian patients followed by Asian American PCPs in the United States are not being screened or appropriately vaccinated. A major barrier to screening and vaccination seems to be a lack of familiarity and knowledge on the part of the provider about hepatitis B in Asian patients. Factors such as time constraints, difficulties working with insurance companies, screening expense, or not feeling comfortable treating HBV infection, were not commonly cited as barriers to HBV screening. These data identify provider education as a key component in improving provider HBV awareness and adherence to screening and vaccination recommendations in United States Asian patients. These findings are consistent with the recent IOM recommendations. As engaging busy primary care providers in educational initiatives is often a challenge, innovative approaches to incentivize appropriate screening and preventive practices are needed with an emphasis on adherence to current CDC HBV screening guidelines as well as follow-up care.
ACKNOWLEDGEMENTS
The authors thank the Asian American primary care physicians who completed the survey and TNS Healthcare for assistance with conducting the study.
Footnotes
Funding source: Gilead Sciences, Inc.
Chu: consultant/speaker-Gilead, Bristol-Myers-Squibb
Lok: advisory panel-Roche, Gilead, Bristol-Myers Squibb; research grants-GlaxoSmithKline, Roche, Schering, Gilead, Bristol-Myers Squibb, Novartis
Kim: consultant-Gilead, Bristol-Myers Squibb, Roche
Tran: advisor/speaker-Gilead, Bristol-Myers Squibb; research grants-Bristol-Myers Squibb
Martin, Fagan, Rousseau: employees and stockholders of Gilead Sciences, Inc.
All authors had access to the study data and participated in writing the manuscript.
References
- 1.Wright TL. Introduction to chronic hepatitis B infection. Am J Gastroenterol. 2006;101(Suppl 1):S1–S6. doi: 10.1111/j.1572-0241.2006.00469.x. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Disease burden from viral hepatitis A, B, and C in the United States [Internet] Atlanta: Centers for Disease Control and Prevention; 2009. [cited 2009 Nov 18]. Available from: http://www.cdc.gov/hepatitis/PDFs/disease_burden.pdf. [Google Scholar]
- 3.Manos MM, Leyden WA, Murphy RC, Terrault NA, Bell BP. Limitations of conventionally derived chronic liver disease mortality rates: results of a comprehensive assessment. Hepatology. 2008;47:1150–1157. doi: 10.1002/hep.22181. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Implementation of newborn hepatitis B vaccination: worldwide, 2006. MMWR Morb Mortal Wkly Rep. 2008;57:1249–1252. [PubMed] [Google Scholar]
- 5.Chang ET, Keegan TH, Gomez SL, et al. The burden of liver cancer in Asians and Pacific Islanders in the Greater San Francisco Bay Area, 1990 through 2004. Cancer. 2007;109:2100–2108. doi: 10.1002/cncr.22642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hutton DW, Tan D, So SK, Brandeau ML. Cost-effectiveness of screening and vaccinating Asian and Pacific Islander adults for hepatitis B. Ann Intern Med. 2007;147:460–469. doi: 10.7326/0003-4819-147-7-200710020-00004. [DOI] [PubMed] [Google Scholar]
- 7.Weinbaum CM, Williams I, Mast EE, et al. Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. MMWR Recomm Rep. 2008;57(RR-8):1–20. [PubMed] [Google Scholar]
- 8.Lin SY, Chang ET, So SK. Why we should routinely screen Asian American adults for hepatitis B: a cross-sectional study of Asians in California. Hepatology. 2007;46:1034–1040. doi: 10.1002/hep.21784. [DOI] [PubMed] [Google Scholar]
- 9.Coronado GD, Taylor VM, Tu SP, et al. Correlates of hepatitis B testing among Chinese Americans. J Community Health. 2007;32:379–390. doi: 10.1007/s10900-007-9060-x. [DOI] [PubMed] [Google Scholar]
- 10.Colvin HM, Mitchell AE Institute of Medicine (U.S.) Committee on the Prevention and Control of Viral Hepatitis Infections; Institute of Medicine (U.S.) Board on Population Health and Public Health Practice. Hepatitis and liver cancer: a national strategy for prevention and control of hepatitis B and C. Washington DC: National Academies Press; 2010. [PubMed] [Google Scholar]
- 11.Hwang JP, Huang CH, Yi JK. Knowledge about hepatitis B and predictors of hepatitis B vaccination among Vietnamese American college students. J Am Coll Health. 2008;56:377–382. doi: 10.3200/JACH.56.44.377-382. [DOI] [PubMed] [Google Scholar]
- 12.Lai CJ, Nguyen TT, Hwang J, Stewart SL, Kwan A, McPhee SJ. Provider knowledge and practice regarding hepatitis B screening in Chinese-speaking patients. J Cancer Educ. 2007;22:37–41. doi: 10.1007/BF03174373. [DOI] [PubMed] [Google Scholar]
- 13.Ma GX, Shive SE, Fang CY, et al. Knowledge, attitudes, and behaviors of hepatitis B screening and vaccination and liver cancer risks among Vietnamese Americans. J Health Care Poor Underserved. 2007;18:62–73. doi: 10.1353/hpu.2007.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen TT, Taylor V, Chen MS, Jr, Bastani R, Maxwell AE, McPhee SJ. Hepatitis B awareness, knowledge, and screening among Asian Americans. J Cancer Educ. 2007;22:266–272. doi: 10.1007/BF03174128. [DOI] [PubMed] [Google Scholar]
- 15.Taylor VM, Yasui Y, Burke N, et al. Hepatitis B testing among Vietnamese American men. Cancer Detect Prev. 2004;28:170–177. doi: 10.1016/j.cdp.2004.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taylor VM, Yasui Y, Burke N, Choe JH, Acorda E, Jackson JC. Hepatitis B knowledge and testing among Vietnamese-American women. Ethn Dis. 2005;15:761–767. [PubMed] [Google Scholar]
- 17.Thompson MJ, Taylor VM, Jackson JC, et al. Hepatitis B knowledge and practices among Chinese American women in Seattle, Washington. J Cancer Educ. 2002;17:222–226. doi: 10.1080/08858190209528842. [DOI] [PubMed] [Google Scholar]
- 18.Upadhyaya N, Chang R, Davis C, Conti MC, Salinas-Garcia D, Tang H. Chronic hepatitis B: perceptions in Asian American communities and diagnosis and management practices among primary care physicians. Postgrad Med. 2010;122:165–175. doi: 10.3810/pgm.2010.09.2213. [DOI] [PubMed] [Google Scholar]