Abstract
Methanol is a highly toxic alcohol resembling ethanol in smell and taste. Methanol poisoning is a lethal form of poisoning that can cause severe metabolic acidosis, visual disturbances, and neurological deficit. Brain lesions typically described in methanol toxicity are in the form of hemorrhagic and non-hemorrhagic necrosis of the basal ganglia and sub-cortical white matter. To our knowledge, lesions in the parietal, temporal, or frontal areas of cerebrum and cerebellar hemispheres have been rarely reported so far. We herewith report this rare presentation.
Keywords: Basal ganglia, intoxication, methanol, necrosis, putamen
Introduction
Methanol is a toxic alcohol readily available in household and industrial products. Methanol toxicity may be seen due to its unintentional or intentional abuse. It is associated with serious complications like metabolic acidosis, visual disturbances and neurological deficit. Diagnosis is based upon the typical clinical picture, metabolic acidosis, neuroimaging and high osmolar gap. Neuroimaging typically described in the literature involves the basal ganglia and sub-cortical white matter. However, brain lesions at other sites may occur as we describe in this case. This knowledge is necessary as prompt diagnosis and timely institution of treatment by administration of ethanol or fomepizole besides other adjuvant therapy can be life-saving.
Case Report
A 51-year-old male presented with abdominal pain, nausea, and vomiting for 1 day with altered mentation, decreased urine output, and sudden onset blurring of vision since 12 h. The patient was a chronic alcoholic and smoker for last 10 years and there was history of consumption of unquantified amount of country liquor 1 day back. There was no history of fever, blood in urine, seizures, weakness, decreased sensations, or bowel disturbances. Other history was not significant. On examination, the patient was conscious but confused. His vitals were normal. General physical examination revealed mild pallor. On central nervous system examination, the Glasgow coma scale was E4M5V3; there was diminished light perception in both the eyes; pupils were normal sized bilaterally but sluggishly reacting to light. Other cranial nerves were normal. There was no motor or sensory deficit. Cerebellar signs like finger nose test, dysdiadochokinesis, and heel-shin tests were abnormal on the right side. The patient had a wide based gait. Rest of his examination was normal. His complete blood count and liver function tests at the time of presentation were normal. Random blood sugar was 6.1 mmol/L. Kidney function tests showed blood urea nitrogen of 27 mmol/L, creatinine of 238 mmol/L, serum sodium 146 mmol/L, and potassium 4.2 mmol/L. Arterial blood gas revealed pH of 7.21, bicarbonate of 10 mmol/L, paCo2 of 18 mm Hg. With clinical possibility of methanol toxicity, serum osmolar gap was calculated. It was found to be 74; serum methanol levels were sent which were high with value of 8.04 mmol/L. Magnetic resonance (MR) imaging of the brain revealed hemorrhagic conversion of infarct in bilateral parasagittal, parieto-occipital region. An acute infarct was seen in right cerebellum. There were punctate infarcts in bilateral frontal regions [Figures 1 and 2]. Visual-evoked response revealed prolonged bilateral (R > L) P100 and bilateral (R>>L) demylination of optic nerve. Serum levels of ammonia, vitamin B12, folate, amylase, and lipase were normal. The ultrasonography of the abdomen and the thyroid function tests were normal. In view of methanol poisoning, hemodialysis was done and ethanol was given through the naso-gastric tube since the patient could not afford fomepizole. The patient responded to treatment. Patient’s visual acuity improved. Initially at presentation, it was finger-counting (FC+) at 1 m. Now the patient has visual acuity of 6/36 in both eyes without visual aids with minimal focal neurologic deficit and is on regular follow-up.
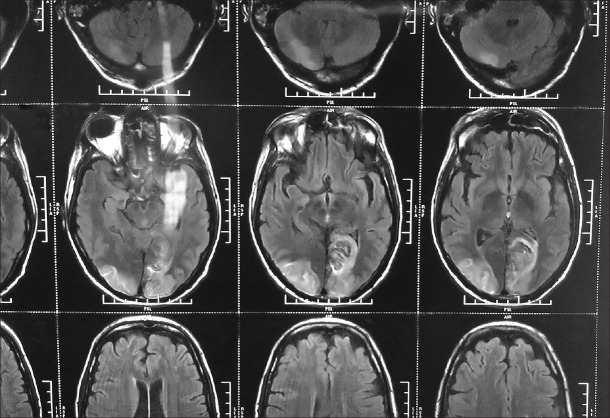
Figure 1.
Infarct in rt. cerebellum and b/l parieto–occipital region
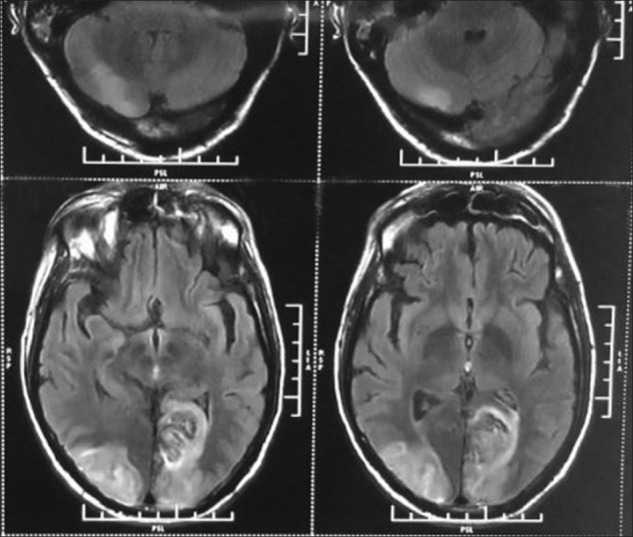
Figure 2.
Hemorrhagic infarct in b/l parieto – occipital region
Discussion
Methanol is a clear, colorless solvent used in anti-freeze solutions, varnishes, paint, and fuel. Methanol poisoning may occur due to accidental or suicidal ingestion of these, or it may occur due to consumption of adulterated alcoholic beverages. The lethal dose of methanol is around 1 g/kg.[1] Methanol by itself is largely non-toxic and toxicity results due to its metabolism into formaldehyde and formic acid in the liver. This also accounts for the time lag between substance ingestion and clinical manifestation which is considered to be around 6-24 h.
Patient may present with non-specific symptoms as nausea, vomiting, headache, dizziness, and weakness. Clinically, the patient may present with several complications like high anion gap metabolic acidosis, visual disturbances, and neurologic deficit. If not treated early, the patient may develop coma and succumb to the poisoning.
Cerebral infarction-ischemic as well as hemorrhagic, selectively affecting the putamen and sub-cortical white matter is known to occur in methanol poisoning.[2,3] The reason for cerebral infarction in these selective regions is not known although many theories have been proposed.
According to some, this is attributed to the venous drainage pattern of the lenticular nucleus. Accumulation of methanol in high concentrations may occur in this region causing direct toxicity.[4] Relative ischemia due to the high metabolic rates of basal ganglia and optic nerves has also been proposed.[5] Anti-coagulation during hemodialysis may contribute to the hemorrhage in the infarcted areas of the brain. Apart from basal ganglionic involvement, lesions of the pontine tegmentum and peripheral white matter may also be seen.[6–8] However, apart from these, lesions in other parts of the cerebrum and cerebellum have rarely been reported so far.[9] In our case, the typical clinical features and laboratory parameters suggested methanol intoxication. MR imaging of brain revealed hemorrhagic infarcts in bilateral parasagittal, parieto-occipital region and an acute infarct was seen in right cerebellum. The possible mechanism could be methanol-induced cerebral vasospasm resultant of a large rise in intra-cytosolic calcium in cerebrovascular smooth muscle cells, as proposed by Li et al.,[10] in his recent study. The patient improved clinically on administration after renal replacement therapy and ethanol. Recovery of vision is common with treatment in methanol poisoning and permanent visual impairment is only rarely seen.[11–13] Fomepizole, an alcohol dehydrogenase inhibitor, which is usually preferred in such cases over use of ethanol, could not be administered in our case due to patient’s unaffordability.
This case report emphasizes the need to consider the possibility of methanol poisoning in patients presenting with altered mentation, visual disturbances, and brain lesions at atypical sites since timely institution of treatment can save the life.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Buller F, Wood CA. Cases of death and blindness from Columbian spirits and other methylated preparations. JAMA. 1904;43:972–7. [Google Scholar]
- 2.Pelletier J, Habib MH, Khalil R, Salamon G, Bartoli D, Jean P. Putaminal necrosis after methanol intoxication. J Neurol Neurosurg Psychiatry. 1992;55:234–5. doi: 10.1136/jnnp.55.3.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arora V, Nijjar IB, Multani AS, Singh JP, Abrol R, Chopra R, et al. MRI findings in methanol intoxication: A report of two cases. Br J Radiol. 2007;80:e243–6. doi: 10.1259/bjr/40137535. [DOI] [PubMed] [Google Scholar]
- 4.Koopmans RA, Li DK, Paty DW. Basal ganglia lesions in methanol poisoning: MR appearance. J Comput Assist Tomogr. 1988;12:168–9. doi: 10.1097/00004728-198801000-00039. [DOI] [PubMed] [Google Scholar]
- 5.Sharpe JA, Hostovsky M, Bilbao JM, Rewcastle NB. Methanol optic neuropathy: A histopathological study. Neurology. 1982;32:1093–100. doi: 10.1212/wnl.32.10.1093. [DOI] [PubMed] [Google Scholar]
- 6.Gaul HP, Wallace CJ, Auer RN, Fong TC. MR findings in methanol intoxication. AJNR Am J Neuroradiol. 1995;16:1783–6. [PMC free article] [PubMed] [Google Scholar]
- 7.Blanco M, Casado R, Vázquez F, Pumar JM. CT and MR imaging findings in methanol intoxication. AJNR Am J Neuroradiol. 2006;27:452–4. [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson CA, Rubinstein D, Filley CM, Stears JC. MR enhancing brain lesions in methanol intoxication. J Comput Assist Tomogr. 1997;21:834–6. doi: 10.1097/00004728-199709000-00034. [DOI] [PubMed] [Google Scholar]
- 9.Askar A, Al-Suwaida A. Methanol intoxication with brain hemorrhage: Catastrophic outcome of late presentation. Saudi J Kidney Dis Transpl. 2007;18:117–22. [PubMed] [Google Scholar]
- 10.Li W, Zheng T, Wang J, Altura BT, Altura BM. Methanol elevates cytosolic calcium ions in cultured canine cerebral vascular smooth muscle cells: Possible relation to CNS toxicity. Alcohol. 1999;18:221–4. doi: 10.1016/s0741-8329(99)00007-5. [DOI] [PubMed] [Google Scholar]
- 11.Chew WB, Berger EH. Alkali treatment of methyl alcohol poisoning. J Am Med Assoc. 1946;130:61–4. doi: 10.1001/jama.1946.02870020005002. [DOI] [PubMed] [Google Scholar]
- 12.Hovda KE, Hunderi OH, Tafjord AB, Dunlop O, Rudberg N, Jacobsen D. Methanol outbreak in Norway 2002-2004: Epidemiology, clinical features and prognostic signs. J Intern Med. 2005;258:181–90. doi: 10.1111/j.1365-2796.2005.01521.x. [DOI] [PubMed] [Google Scholar]
- 13.Paasma R, Hovda KE, Tikkerberi A, Jacobsen D. Methanol mass poisoning in Estonia: Outbreak in 154 patients. Clin Toxicol (Phila) 2007;45:152–7. doi: 10.1080/15563650600956329. [DOI] [PubMed] [Google Scholar]