The focus of the World Health Day (WHD) this year is on one of the main non-communicable disease (NCD) risk factors, hypertension. It is currently the leading risk resulting in considerable death and disability worldwide and accounted for 9.4 million deaths and 7 per cent of disability adjusted life years (DALYs) in 20101. Hypertension is increasing rapidly in most low and middle income countries (LMICs) driven by diverse health transitions. In 2001, it accounted for 10 per cent of global healthcare expenditure underlining the considerable economic implications to resource constrained health systems, particularly those in LMICs2. Apart from health implications it has huge societal, developmental and economic costs. There is also noteworthy income loss to families affected by hypertension not only due to illness but also due to care giving and premature death. In 2004, the annual income loss from NCDs among working adults in India was  251 billion (about US$ 50 billion) and that due to hypertension alone amounted to
251 billion (about US$ 50 billion) and that due to hypertension alone amounted to  43 billion. Further, hypertension was also a leading cause for hospitalizations and outpatient visits3.
43 billion. Further, hypertension was also a leading cause for hospitalizations and outpatient visits3.
Rising burden of hypertension in India
In India, hypertension is the leading NCD risk and estimated to be attributable for nearly 10 per cent of all deaths4. Adult hypertension prevalence has risen dramatically over the past three decades from 5 per cent to between 20-40 per cent in urban areas and 12-17 per cent in rural areas5,6. The number of hypertensive individuals is anticipated to nearly double from 118 million in 2000 to 213 million by 20256. It is estimated that 16 per cent of ischaemic heart disease, 21 per cent of peripheral vascular disease, 24 per cent of acute myocardial infarctions and 29 per cent of strokes are attributable to hypertension underlining the huge impact effective hypertension prevention and control can have on reducing the rising burden of cardiovascular disease (CVD)7.
Sub-optimal treatment and control
Though national data on treatment and control are not available, multiple cross-sectional studies conducted across various regions of India such as north (Delhi 10.5%), south (Chennai 7.5%, Thiruvananthapuram 8.6%), east (Assam 18.1%), and west (Mumbai 13.6%) indicate sub-optimal blood pressure control8. Besides once hypertension-related CVD occurs, the use of evidence-based secondary prevention therapies is also very low in primary and secondary care, leading to a large and escalating burden of avoidable and premature mortality9.
Against the milieu of increasing NCDs in India, the gap between what is known and actually done for hypertension prevention, detection and management is disconcerting and requires to be addressed as a public health priority. Further, effectively addressing it assumes critical importance in light of the recent World Health Organization (WHO)-United Nations (UN) targets for reduction of NCDs by 2025 with explicit targets for hypertension and its chief modifiable determinant salt intake10.
Pathways for prevention and control
The increasing hypertension and NCD burden presents a formidable challenge to the Indian health system, which will need strengthening at all levels (primary, secondary, tertiary) incorporating prevention, surveillance, screening and appropriate management, along with re-training, regular enhancement and updating skills of the health professionals in providing hypertension related care. India cannot afford the resource intensive model of healthcare to address hypertension and NCDs and should, therefore, prioritize population based prevention approaches requiring multi-sectoral actions across non-health sectors to minimize population risk factor exposure in tandem with evidence based clinical approaches focussed on early detection and treatment, which can maximize the gains for population health.
Population based approaches
Population based prevention strategies have high impact, are cost-effective as these target lifestyle change, entail working with non-health sectors and are likely sustainable over the long term. Interventions utilizing the power of public policies for reducing salt, fat, sugar and alcohol intakes through regulatory and consumer education approaches; increasing physical activity through sound urban planning and creation of activity promoting environments; increasing fruit-vegetable intake through appropriate agricultural and pricing mechanisms and implementing comprehensive tobacco control have the potential to prevent a large proportion of disease events in the whole population, given that most disease events occur at modest elevations of multiple risk factors rather than at marked elevation of a single risk factor. For example, a 2 per cent population-wide decrease of diastolic blood pressure, such as that easily achievable by modest salt reduction, was estimated to avert 300,000 coronary heart disease and stroke deaths in India, with larger blood pressure decreases yielding higher reductions11.
Limited available data point to high salt intake (9-12 g/day) which exceeds current WHO recommended levels12. The recent global burden of disease study reports excess salt intake to be the 7th leading cause of mortality in South East Asia Region which is much higher than in rest of the world (11th globally), highlighting the adverse impact of high intake in countries like India1. A 15 per cent reduction in salt intake through voluntary reduction by the food industry and consumer education to encourage dietary change was estimated to cost (in 2005) just  2 per person/year13. Given the rising burden of hypertension and high salt consumption, the priority intervention of choice for hypertension prevention and control is population-wide salt reduction. However, its potential has yet to be tapped in India with efforts being initiated only recently. The Public Health Foundation of India (PHFI) conducted a national research consultation to identify salt reduction strategies for India and initiated studies to gather current evidence to facilitate national salt reduction policy development12. Recently, the HEART study was initiated in Tamil Nadu and an early report indicated a salt intake of 12 g/day14. The South East Asia Regional Office of the WHO (SEARO) had conveyed an Expert Group Meeting on population salt reduction to discuss regional salt reduction strategies and the methods to monitor population intake. The participants agreed on setting a regional target of 10 per cent relative reduction in population salt intake in the next five years and successive reductions thereafter with the aim of achieving 30 per cent relative reduction in population salt intake by 2025 in consonance with the global WHO-United Nations targets15.
2 per person/year13. Given the rising burden of hypertension and high salt consumption, the priority intervention of choice for hypertension prevention and control is population-wide salt reduction. However, its potential has yet to be tapped in India with efforts being initiated only recently. The Public Health Foundation of India (PHFI) conducted a national research consultation to identify salt reduction strategies for India and initiated studies to gather current evidence to facilitate national salt reduction policy development12. Recently, the HEART study was initiated in Tamil Nadu and an early report indicated a salt intake of 12 g/day14. The South East Asia Regional Office of the WHO (SEARO) had conveyed an Expert Group Meeting on population salt reduction to discuss regional salt reduction strategies and the methods to monitor population intake. The participants agreed on setting a regional target of 10 per cent relative reduction in population salt intake in the next five years and successive reductions thereafter with the aim of achieving 30 per cent relative reduction in population salt intake by 2025 in consonance with the global WHO-United Nations targets15.
Evidence based clinical approaches
Hypertension is easily diagnosable and treatable with lifestyle modifications and effective medicines. Thus, hypertension control provides an entry point to deal with other NCDs as any intervention will help concomitantly address other NCDs as well. This has been taken into cognizance in the newly launched National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) which has hypertension and diabetes as the main focus areas. NPCDCS offers great potential for both health systems strengthening as well as improving hypertension management if leveraged appropriately16.
The opportunistic screening planned in NPCDCS at the sub-centre level could be strengthened with provision of electronic decision support tools for the health workers to detect, refer and follow up patients as well as facilitate reporting utilizing appropriate data templates and thereby contribute to surveillance and the development of a health information system to track hypertension and its outcomes. The NCD clinics mandated under NPCDCS could be leveraged to facilitate guidelines based hypertension management with emphasis on generic drugs and those recommended by the Indian Public Health Standards/National List of Essential Medicines as well as capacity building of health staff in the system around delivery of hypertension related services. Existing training guidance for physicians and health workers under the NPCDCS can be used, incorporating regular evidence updates where and when required16,17.
Given the limited availability of physicians, task sharing as well as task shifting of existing primary health workforce, particularly training of non-physician health workers (NPHW) is a possible strategy. There is evidence from developing countries on the feasibility and effectiveness of this approach in improving outcomes18,19. The LMIC specific WHO cardiovascular risk management package has also been demonstrated to be suitable for assessing and managing CVD risks by NPHW in primary care settings (including India) which have limited numbers of physicians20.
Given the high prevalence of hypertension in India6, blood pressure assessment in all adults at every opportunity is both prudent and justified. In addition, simple non-laboratory based risk scores previously validated in India, based on simple assessment of age, waist circumference, physical activity, and family history could be used to assess total cardiovascular risk as well as co-morbidities and refer those requiring further detailed evaluation to the health system21,22. The WHO - International Society of Hypertension (ISH) risk chart adapted for countries like India and also recommended by the NPCDCS can be utilized for assessing total cardiovascular risk23. Further, the WHO's Package of Essential Noncommunicable Disease Interventions (WHO-PEN) which has been specifically developed for promoting prioritized, cost-effective, equitable delivery and universal coverage of NCD interventions in primary care of LMICs should be adopted24.
Given the continued care required for hypertension, appropriate referral and follow up pathways across various levels of care as well as public and private sectors are warranted. Properly validated devices to measure blood pressure should be provided at all health facilities and made available to all healthcare providers. As most expenses related to hypertension care are on medicines, ensuring affordable, accessible and uninterrupted drug supply is necessary. Medicines contribute to 45 per cent of out of pocket expenses for NCDs in India, while for hypertension it is as high as 64 per cent3. A 36-country WHO study found that in most countries including India, a month's treatment with just one antihypertensive medication costs 1.8 day's wages which becomes even more unaffordable if multiple drugs are necessary for attaining treatment targets and if more than one family member has hypertension25. Thus, effective financial risk protection measures should be adopted to reduce financial burden on individuals.
Given the low levels of awareness and detection, blood pressure measurement and possibly non-laboratory risk assessment among adults should be mandated as part of all national health programmes. To increase the awareness on hypertension, information about prevention and control of hypertension can be incorporated in the information education and communication (IEC) components of all national programmes. This can complement overall efforts to increase societal awareness through other approaches. In this regard, the World Hypertension League (WHL) aims to improve public awareness through World Hypertension Day, conducted on May 17 every year with specific themes (Table)26. The theme for 2013 World Hypertension Day is “Healthy heart beat – healthy blood pressure” emphasizing on the importance of blood pressure control and control of arrhythmias (www.worldhypertensionleague.org).
Table.
The World Hypertension League Call to Action
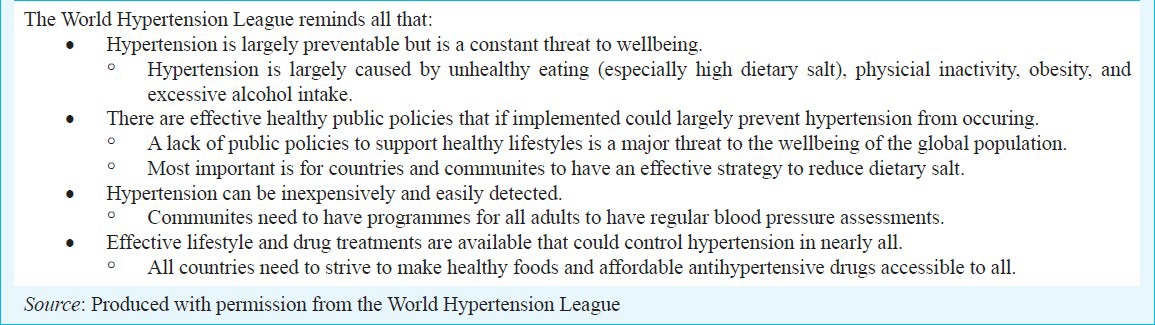
Health professionals, including physicians, nurses and other health workers as well as their professional organizations, civil society and academia should be catalyzed to assume leadership for focussed advocacy efforts to raise the priority of hypertension prevention and control as well as to build multi-sectoral partnerships for population based risk reduction and modification approaches.
The rising burden of hypertension, associated CVD and NCDs in India needs to be addressed as a public health priority employing an optimal context specific resource sensitive combination of the population and the clinical approach. There are numerous challenges ahead but also promising opportunities to galvanize efforts towards attaining the WHO-UN goal of 25 per cent reduction in NCD related mortality and associated reduction in hypertension and salt intake by 2025.
Footnotes
This editorial is published on the occasion of World Health Day - April 7, 2013.
References
- 1.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gaziano TA, Bitton A, Anand S, Weinstein MC International Society of Hypertension. The global cost of nonoptimal blood pressure. J Hypertens. 2009;27:1472–7. doi: 10.1097/HJH.0b013e32832a9ba3. [DOI] [PubMed] [Google Scholar]
- 3.Mahal A, Karan A, Engelgau M. Health Nutrition and Population (HNP) discussion paper. Washington: The World Bank; 2010. The economic implications of non-communicable disease for India. [Google Scholar]
- 4.Patel V, Chatterji S, Chisholm D, Ebrahim S, Gopalakrishna G, Mathers C, et al. Chronic diseases and injuries in India. Lancet. 2011;377:413–28. doi: 10.1016/S0140-6736(10)61188-9. [DOI] [PubMed] [Google Scholar]
- 5.Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens. 2004;18:73–8. doi: 10.1038/sj.jhh.1001633. [DOI] [PubMed] [Google Scholar]
- 6.Reddy KS, Shah B, Varghese C, Ramadoss A. Responding to the threat of chronic diseases in India. Lancet. 2005;366:1744–9. doi: 10.1016/S0140-6736(05)67343-6. [DOI] [PubMed] [Google Scholar]
- 7.Mohan S, Reddy KS, Prabhakaran D. Reversing the tide. New Delhi: Public Health Foundation of India; 2011. Chronic non-communicable diseases in India. [Google Scholar]
- 8.Devi P, Rao M, Sigamani A, Faruqui A, Jose M, Gupta R, et al. Prevalence, risk factors and awareness of hypertension in India: a systematic review. J Hum Hypertens. 2013;27:281–7. doi: 10.1038/jhh.2012.33. [DOI] [PubMed] [Google Scholar]
- 9.Yusuf S, Islam S, Chow CK, Rangarajan S, Dagenais G, Diaz R, et al. Prospective Urban Rural Epidemiology (PURE) Study Investigators. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet. 2011;378:1231–43. doi: 10.1016/S0140-6736(11)61215-4. [DOI] [PubMed] [Google Scholar]
- 10.Revised Draft Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013-2020 (version dated 11 February 2013. World Health Organization. 2013. [accessed on March 2, 2013]. Available from: http://www.who.int/nmh/events/2013/revised_draft_ncd_action_plan.pdf .
- 11.Rodgers A, Lawes C, MacMahon S. Reducing the global burden of blood pressure related cardiovascular disease. J Hypertens. 2000;18(Suppl):S3–6. [PubMed] [Google Scholar]
- 12.Mohan S, Prabhakaran D. Review of salt and health: situation in South-East Asia Region. New Delhi: WHO SEARO; 2012. Background paper for the Expert Meeting on Population Sodium Reduction Strategies for Prevention and Control of Noncommunicable Diseases in the South-East Asia Region. [Google Scholar]
- 13.Asaria P, Chisholm D, Mathers C, Ezzati M, Beaglehole R. Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet. 2007;370:2044–53. doi: 10.1016/S0140-6736(07)61698-5. [DOI] [PubMed] [Google Scholar]
- 14.Chidambaram N, Sethupathy S, Saravanan N, Taguchi T, Mori M, Garg A, et al. Nutritional factors for hypertension in India; the first report of the heart study based on biological marker estimation of 24-hour urine samples. J Hyperten. 2012;1:e49. [Google Scholar]
- 15.Mohan S, Prabhakaran D, Krishnan A. Promoting population-wide salt reduction in South East Asia Region: current status and future directions. Regional Health Forum. 2013;17:72–9. [Google Scholar]
- 16.Manual for medical officers. New Delhi: Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India; 2011. National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke. [Google Scholar]
- 17.A guide for health workers. New Delhi: Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India; 2011. National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke. [Google Scholar]
- 18.Coleman R, Gill G, Wilkinson D. Noncommunicable disease management in resource-poor settings: a primary care model from rural South Africa. Bull World Health Organ. 1998;76:633–40. [PMC free article] [PubMed] [Google Scholar]
- 19.Farzadfar F, Murray CJ, Gakidou E, Bossert T, Namdaritabar H, Alikhani S, et al. Effectiveness of diabetes and hypertension management by rural primary health-care workers (Behvarz workers) in Iran: a nationally representative observational study. Lancet. 2012;379:47–54. doi: 10.1016/S0140-6736(11)61349-4. [DOI] [PubMed] [Google Scholar]
- 20.Abegunde DO, Shengelia B, Luyten A, Cameron A, Celletti F, Nishtar S, et al. Can non-physician health-care workers assess and manage cardiovascular risk in primary care? Bull World Health Organ. 2007;85:432–40. doi: 10.2471/BLT.06.032177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chaturvedi V, Reddy KS, Prabhakaran D, Jeemon P, Ramakrishnan L, Shah P, et al. Development of a clinical risk score in predicting undiagnosed diabetes in urban Asian Indian adults: a population based study. CVD Prev Control. 2008;3:141–51. [Google Scholar]
- 22.Mohan V, Deepa R, Deepa M, Somannavar S, Datta M. A simplified Indian Diabetes Risk Score for screening for undiagnosed diabetic subjects. J Assoc Physicians India. 2005;53:759–63. [PubMed] [Google Scholar]
- 23.Mendis S, Lindholm LH, Anderson SG, Alwan A, Koju R, Onwubere BJ, et al. Total cardiovascular risk approach to improve efficiency of cardiovascular prevention in resource constrain settings. J Clin Epidemiol. 2011;64:1451–62. doi: 10.1016/j.jclinepi.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 24.WHO. Geneva: World Health Organization; 2010. Package of essential noncommunicable (PEN) disease interventions for primary health care in low-resource settings. [Google Scholar]
- 25.van Mourik MS, Cameron A, Ewen M, Laing RO. Availability, price and affordability of cardiovascular medicines: a comparison across 36 countries using WHO/HAI data. BMC Cardiovasc Disord. 2010;10:25. doi: 10.1186/1471-2261-10-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chockalingam A. World Hypertension Day and global awareness. Can J Cardiol. 2008;24:441–4. doi: 10.1016/s0828-282x(08)70617-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


